Abstract
Background
Burn injuries are a significant global health burden, with critically ill patients requiring intensive care unit (ICU) admission. The present study aimed to investigate burn characteristics, management strategies, and mortality trends of burn patients admitted to the ICU at a tertiary care center.
Methods
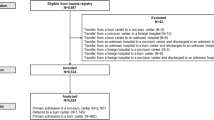
A six-year retrospective analysis was conducted on patients admitted to the burn ICU between 2016 and 2021. Data on demographics, burn characteristics, management, and mortality were collected from medical records. Descriptive statistics and survival analysis were employed to analyze trends over the six-year period.
Results
A total of 312 patients were included in the study with a mean age of 38.0 ± 15.2 years. Flame burn was observed in 57.7% of the patients and 16% had scald burns. The average total body surface area (TBSA) was 27% ± 25%. The majority of admitted patients had at least one operative intervention (79%). The type of burn (p < 0.001), having a third-degree burn (p < 0.001), having one or more comorbid conditions (p = 0.03), TBSA (p < 0.001), and inhalation injury (p = 0.015) were found to be significantly associated with mortality.
Conclusion
The overall mortality rate was 9.9%. Most of the admitted cases were for flame burns followed by scald burns. The majority of admitted patients had at least one operative intervention. TBSA, inhalation injury, type of burn, having a third-degree burn, and having one or more comorbid conditions were found to be significantly associated with mortality.
Level of Evidence:
Level III, Therapeutic; Risk/Prognostic; Diagnostic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Burns are dynamic injuries that can lead to a reduction in the affected person’s quality of life in the physical and mental domains, leading to pain and deformities that are sometimes lifelong [1]. These injuries tend to be spread disproportionately among different populations, as it is estimated that the around 95% of deaths due to burns are in people of ethnic minorities especially in low to middle-income countries [2]. Overall, the incidence of burns in 2017 significantly decreased in numerous regions of the world, including the Middle East, compared to 1990 [3]. However, the numbers could be grossly underestimated since the vast majority of burn injuries are normally managed conservatively by the patients themselves or be treated in a non-hospital setting [4].
Burns also represent a heavy financial burden to the affected individuals and the system that supports them due to the nature of the injury which necessitates the involvement of a multidisciplinary team of specialists, potential intensive care admission, surgical management, post-injury physiotherapy, and any potential sequelae of the trauma. In such cases, the costs can rise rapidly with costs estimated to be over $125,000 per patient [5].
There have been marked reductions in mortality due to burns in recent years. This is mainly due to better understanding of burns and their pathophysiology, advances in surgical techniques, improved resuscitation and nutritional support, early interventions, and better infection control [6, 7]. Certain factors such as an older age, as well as deeper and a more extensive burn body area increase the likelihood of death [8, 9]. Burn mortality in Saudi Arabia is estimated to have fallen by around 59% in 2017 compared to 1990 [3]. However, most deaths reported in the literature focus on in-hospital mortality and thus represent a very small fraction of the true disease burden, considering that a significant proportion of patients pass away before reaching and being admitted into a hospital [10]. In the present study, we aimed to highlight epidemiological and clinical characteristics, and management strategies of patients with burn injuries at a tertiary care center in Riyadh, Saudi Arabia.
Material and methods
This was a retrospective chart review of all adults (≥ 18 years) patients admitted to the burns unit of King Abdulaziz Medical City (KAMC), Riyadh, between January 2016 to December 2021. KAMC is a tertiary care hospital and level 1 trauma center that was established in 1982. It has a bed capacity of around a thousand and nine-hundred beds. Its burns unit has eight beds dedicated to patients with burn injuries.
All adult patients who were admitted to the unit during the specified period were included in the study after gaining the approval of the Institutional Review Board of King Abdullah International Medical Research Center (approval number NRC22R/186/04). The data was entered using Microsoft Excel sheet for the following variables: age, gender, body mass index (BMI), admission and discharge dates, length of stay, type and degree of burn, injured body part, the total body surface area (TBSA), whether the patient was managed conservatively or operatively, any comorbid conditions, and the cause of death where applicable. Statistical Package for Social Sciences (SPSS) Statistics version 23 (IBM Corp., Armonk, NY, USA) was used for data analysis. The numerical variables are presented as mean and standard deviation and as median and interquartile range (IQR). The categorical variables are presented as frequencies and percentages. The independent samples t-test and Mann Whitney U-test were used to compare the numerical variables with surgical intervention (Yes/No) and mortality (Yes/No). The categorical variables were compared with mortality (Yes/No) using the Chi-Square test and Fisher Exact test. A p-value < 0.05 was considered to show a statistically significant difference.
Results
Age, gender, and admissions
Three hundred and twelve patients were included in the study. Males made up 76% (n = 238) of the sample, and the mean age was 38.0 ± 15.2 years. The highest number of admissions came during the months of September to November. The average length of stay (LOS) was 27.4 ± 30.7 (median = 16, IQR = 8, 34).
Burn characteristics
Most of the admitted cases were for flame burns (n = 180; 57.7%), and most had second-degree injuries (n = 115; 40%). The upper limbs were affected most often (n = 244; 78%) (Table 1). The average total body surface area (TBSA) was 27% ± 25%. TBSA was found to be significantly associated with mortality (p ≤ 0.001).
Operative vs. conservative management
The majority of admitted patients had at least one operative intervention (n = 248; 79%). Neither the gender (p = 0.95) nor the type of burn (p = 0.16) were associated with surgical intervention. However, the degree of burn had a statistically significant association (p < 0.001) (Table 2).
Mortality
Throughout the duration of the study, 31 patients (9.9%) passed away. Generally, the deceased had a much higher TBSA compared to the survivors (71.6% compared to 22.3%); this difference was statistically significant (p < 0.001). BMI, LOS, and age were not associated with mortality (Table 3).
The type of burn (p < 0.001), having a third-degree burn (p < 0.001), and having one or more comorbid conditions (p = 0.03) were all found to be significantly associated with mortality (table 4). Furthermore, those who had died were more likely to have undergone a surgical intervention compared to the survivors (p = 0.02), 96.7% for the former group compared to 77.5% for the latter. Additionally, the TBSA of the patients who had passed away within 48 h of admission was significantly higher than those who had died over a longer period (p = 0.05). Those with inhalation injury reported a significantly higher mortality rate compared to individuals without inhalation injury (p = 0.015)
Discussion
The relative lack of recent studies on burn patients in Saudi Arabia prompted the initiation of the present study, as the latest published epidemiological papers were either conducted in regions other than Riyadh [11], or were solely focused on the pediatric age group [12]. The described gender distributions were comparable to other regional studies, whether they involved only pediatric patients [12,13,14], had a mixture of adults and children [15,16,17,18,19], or were exclusive to adults [20]. However, there are other local [21,22,23] and international studies in the United States [24] and Bangladesh [25] where the proportions were much closer together. Men are generally more affected than females provided that, in accordance with local culture, there are fewer women working in the factory industry [26]. Moreover, men are disproportionately represented in Saudi Arabia’s armed forces, which could increase their risk of occupation-related burn injuries.
Comparing the ages distribution in our sample to others would prove difficult considering that the majority of other studies include both adults and children. The reason behind our focus on adults only was because the burn intensive care unit (BICU) only admits adult patients while pediatric patients get admitted to a separate ICU. Seasonal variation was noted among studies. Jamal et al’s study in Jeddah shares similar results to ours, where burn incidence was at its highest in autumn [27], whereas another paper by Ali and colleagues which was conducted in Al-Baha had markedly different findings compared to ours as autumn scored the lowest amount of burn admissions [28]. This could be explained by the significant differences in the climates of Riyadh and Jeddah compared to Al-Baha and thus varying social behaviors that could increase the risk of incurring burn injuries in different times of the year. Based on the different types of burns, exposure to flames was the most common cause of burn injuries (57.5%); scald burns (16%) were the second most common cause. These findings align with earlier research from industrialized and developing nations [29, 30]. Flame burn was mostly seen in our sample possibly due to the fact that the center where this study was conducted is a major referral center in the country receiving more complicated and extensive cases.
Most admitted patients underwent at least one operative intervention (79%). Those who had passed away were more likely to have undergone operative management. This is no surprise as patients with more extensive burn injury in terms of TBSA and burn depth require more frequent serial wound debridement and skin grafting. Neither gender nor type of burn affected the decision of surgical intervention in our study. The decision to push the patient to the operating room or pursue non-surgical management was mainly based on the degree of burn. Those with deeper burns in our sample were more likely to receive surgical intervention. Burns involving the epidermal or superficial dermal layers will heal spontaneously, but deep second degree and third-degree burns require surgical debridement and subsequent coverage [31].
In the present study, the overall mortality rate was reported to be 9.9% which, coming from a burn center in a developing country, is deemed acceptable. Compared to other developing countries, mortality rates in hospitalized patients were 12.2% and 60.8% in Malysia and India, respectively [32, 33]. Like other studies, we found that TBSA was significantly associated with mortality. The body of research generally agrees that a higher death rate is linked to larger affected TBSA [34]. Patients with higher TBSA involvement are expected to die from burn shock in the early stages, whereas sepsis and multiple organ failure are the main reasons of death in the long run [34]. Moreover, third-degree burns were associated with mortality in our sample. This is in agreement with the current literature [35, 36]. Increases in the surface area affected and depth of the burn led to higher mortality, according to Temiz et al. [37]. Yazıcı et al. conducted a study among burn patients admitted in the ICU and found a significant association between full thickness burns and mortality [38].
The association between the mortality rate and comorbidities of burn patients was the subject of conflicting findings in previous research. [39]. For example, in the elderly patients with burn injury, Lionelli et al. [40] and Wibbenmeyer et al. [41] found no association between comorbidities and mortality, whereas Akhtar el al. [42] reported that a number of comorbid conditions, such as neurological, hepatic, renal, cardiac, and pulmonary disorders, had a significant effect on mortality. Brandão et al. used the Charlson Comorbidity Index (CCI) score to predict the probability of mortality in burn patients and found that preexisting comorbidities have a significant impact on mortality where the index score was reported to precisely predict the probability of mortality within 1 year [39]. Moreover, a large study including records of 31,338 patients with burns retrieved from the United States National Burn Repository demonstrated multiple pre-existing commodities to be correlated with mortality using the CCI score and the Elixhauser methods for comorbidity assessment [43]. These data are in agreement with our findings as we found having one or more comorbid conditions to be significantly associated with mortality.
In our study, the type of burn was significantly associated with mortality. Flame and electrical burns reported the highest mortality rates compared to other types of burn injuries, 15% and 14% respectively. Flame burns are associated with more extensive, deeper burns and the presence of inhalation injury, contributing to increased mortality rate [44]. Kraft et al. reported higher rates of multi-organ failure and sepsis among pediatric patients with flame burn injuries [45]. It is well known in the literature that electrical burns are generally associated with high mortality rate [46,47,48]. Electrical burns can result in internal tissue damage that is unnoticed from the outside, and affects different types of tissue such as muscles, internal organs, and the heart; subsequently contributing to increased morbidity and mortality [49]. Moreover, electrical injury can have delayed complications such as compartment syndrome or rhabdomyolysis, which can further increase mortality [49].
Among burn victims, inhalation injury is an independent indicator of mortality. Up to 77% of the fatalities are caused by pulmonary complications following burns and inhalation injuries, most of which are attributed to carbon monoxide poisoning [50]. In the present study, the mortality rate of patients with inhalation injury was 16%, while it was only 7% in those with no evidence of inhalation injury. This difference was statistically significant. Colohan et al. [51] found that the mortality rate (27.6%) increased in burn patients with inhalation injuries in a meta-analysis of prognostic variables in burn patients. Inhalation injury increases the incidence of burn patient mortality by causing major airway, pulmonary, and systemic complications [52].
Limitations
The present study has some limitations. First, it was a retrospective single-center study, which introduces the risk of bias. However, our center is considered a level 1 trauma center in Saudi Arabia to whom major burn patients from all around the country are referred, hence possibly increasing the representativeness of our data. Second, given the retrospective nature of the study, missing data could not be retrieved, and some variables were not collected. Lastly, long-term outcomes such as functional status, quality of life, and mortality after discharge were not included in the analysis given the retrospective nature of the study.
Conclusions
This six-year retrospective analysis of burn patients admitted to the ICU provided valuable insights into burn characteristics, management strategies, and mortality trends. We found that the overall mortality rate was 9.9%. Most of the admitted cases were for flame burns followed by scald burns. The majority of admitted patients had at least one operative intervention. TBSA, inhalation injury, type of burn, having a third-degree burn, and having one or more comorbid conditions were found to be significantly associated with mortality. These findings contribute to our understanding of factors associated with burn outcomes in critically ill patients.
References
Jeschke MG, van Baar ME, Choudhry MA et al (2020) Burn injury. Nat Rev Dis Prim. https://doi.org/10.1038/S41572-020-0145-5. 6:
Sasor SE, Chung KC (2019) Upper extremity burns in the developing world: a neglected epidemic. Hand Clin 35:457. https://doi.org/10.1016/J.HCL.2019.07.010
James SL, Lucchesi LR, Bisignano C et al (2020) Epidemiology of injuries from fire, heat and hot substances: global, regional and national morbidity and mortality estimates from the global burden of disease 2017 study. Inj Prev 26. https://doi.org/10.1136/INJURYPREV-2019-043299
Schaefer TJ, Tannan SC (2023) Thermal burns. Environ Emergencies Inj Nat 41–47. https://doi.org/10.5005/jp/books/12720_94
Saavedra PAE, Leal JVDO, Areda CA, Galato D (2021) The costs of burn victim hospital care around the world: a systematic review. Iran J Public Health 50:866. https://doi.org/10.18502/IJPH.V50I5.6104
Żwierełło W, Piorun K, Skórka-Majewicz M et al (2023) Burns: classification, pathophysiology, and treatment: a review. Int J Mol Sci 24. https://doi.org/10.3390/IJMS24043749
García-Díaz A, Durán-Romero AJ, PurificaciónGacto-Sánchez et al (2021) Trends in burn injury mortality in Spain (1979–2018): sex-specific age-cohort-period effects. Burns 47:714–720. https://doi.org/10.1016/J.BURNS.2020.08.001
Yen CI, Chiou MJ, Kuo CF, Liao HT (2018) Determination of risk factors for burn mortality based on a regional population study in Taiwan. Burns 44:1591–1601. https://doi.org/10.1016/J.BURNS.2018.02.030
Angulo M, Aramendi I, Cabrera J, Burghi G (2020) Mortality analysis of adult burn patients in Uruguay. Rev Bras Ter Intensiva 32:43. https://doi.org/10.5935/0103-507X.20200008
Hussain A, Dunn K (2015) Burn related mortality in greater manchester: 11-year review of regional coronial department data. Burns 41:225–234. https://doi.org/10.1016/J.BURNS.2014.10.008
Alshammari S, Almarzouq S, Alghamdi A, Shash H (2022) Mortality and survival analysis of burn patients admitted in a critical care burn unit, Saudi Arabia. Saudi J Med Med Sci 10:216. https://doi.org/10.4103/SJMMS.SJMMS_618_21
Alnjeidi Z, Alharthy N, Alghnam S, Badri M (2022) Factors associated with mortality and morbidity among pediatrics with burn injuries in Riyadh, Saudi Arabia. Saudi Med J 43:508–513. https://doi.org/10.15537/SMJ.2022.43.5.20210923
Gari AA, Al-Ghamdi YA, Qutbudden HS et al (2012) Pediatric burns in western Saudi Arabia. Saudi Med J 33
Alsalman AK, Algadiem EA, Alalwan MA, Farag TS (2015) Epidemiology of infant burn in eastern Saudi Arabia. Saudi Med J 36:324. https://doi.org/10.15537/SMJ.2015.3.10683
Alajmi MM, Aldosari KH, Al-Ghamdi S (2021) Clinical, epidemiological, and management aspects of burn injuries in Saudi Arabia – A cross-sectional study. Saudi J Biol Sci 28:4342. https://doi.org/10.1016/J.SJBS.2021.04.021
Mater ME, Yamani AE, Aljuffri AA, Binladen SA (2020) Epidemiology of burn-related infections in the largest burn unit in Saudi Arabia. Saudi Med J 41:726–732. https://doi.org/10.15537/SMJ.2020.7.25141
Al-Shlash S, Warnasuriya ND, Al Shareef Z et al (1996) Eight years experience of a regional burns unit in Saudi Arabia: clinical and epidemiological aspects. Burns 22:376–380. https://doi.org/10.1016/0305-4179(95)00169-7
El Danaf A (1995) Burn variables influencing survival: a study of 144 patients. Burns 21:517–520. https://doi.org/10.1016/0305-4179(95)00035-A
Al-Hoqail RA, Fadaak H, Wafa AW (2011) Burn injuries at a University Hospital in Saudi Arabia: an audit and concept of total quality management, 1997–2003. J Craniofac Surg 22:404–408. https://doi.org/10.1097/SCS.0B013E3182077F84
Althunayan TA, Alqarni SM, Mohsenh WA et al (2019) Risk factors for thromboembolism in burn patients admitted to the burn unit at King Abdulaziz Medical City, Riyadh, Kingdom of Saudi Arabia. Saudi Med J 40:1027. https://doi.org/10.15537/SMJ.2019.10.23955
Alharthy N, Al Mutairi M, Alqueflie S et al (2016) Pattern of burns identified in the pediatrics emergency department at King Abdul-Aziz Medical City: Riyadh. J Nat Sci Biol Med 7:16. https://doi.org/10.4103/0976-9668.175019
Akkam AY, Joarder A, Cruz-Marcelino N et al (2020) Epidemiology of pediatric patients admitted to a burns ICU in Saudi Arabia. Burn Open 4:90–93. https://doi.org/10.1016/J.BURNSO.2020.06.001
Mahaluxmivala S, Borkar AS, Mathur A, Fadaak H (1997) A retrospective study of etiopathological and preventive factors in a burns unit in Saudi Arabia. Burns 23:333–337. https://doi.org/10.1016/S0305-4179(96)00122-2
Lee A, Wang Y, Nadarajah CC, Lipner SR (2022) Cross-sectional analysis of national electronic injury surveillance system for burn injuries presenting to United States emergency departments 2000–2018. Burns 48:1347–1354. https://doi.org/10.1016/J.BURNS.2021.11.015
Bailey ME, Sagiraju HKR, Mashreky SR, Alamgir H (2019) Epidemiology and outcomes of burn injuries at a tertiary burn care center in Bangladesh. Burns 45:957–963. https://doi.org/10.1016/J.BURNS.2018.12.011
Bagheri Toolaroud P, Attarchi M, Afshari Haghdoust R et al (2023) Epidemiology of work-related burn injuries: a ten‐year retrospective study of 429 patients at a referral burn centre in the north of Iran. Int Wound J 20:3599. https://doi.org/10.1111/IWJ.14238
Jamal YS, Ardawi MSM, Ashy AA et al (1989) Burn injuries in the Jeddah area of Saudi Arabia: a study of 319 cases. Burns 15:295–298. https://doi.org/10.1016/0305-4179(89)90005-3
Ali MH (1997) Pattern of burn injuries at King Fahad Hospital, Al-Baha: a study of 277 cases. Ann Saudi Med 17:104–107. https://doi.org/10.5144/0256-4947.1997.104
Qader AR (2012) Burn mortality in Iraq. Burns 38:772–775. https://doi.org/10.1016/J.BURNS.2011.12.016
Ibarra Estrada MÁ, Chávez Peña Q, García Guardado DI et al (2014) A 10-year experience with major burns from a non-burn intensive care unit. Burns 40:1225–1231. https://doi.org/10.1016/J.BURNS.2013.12.020
Hettiaratchy S, Papini R (2004) Initial management of a major burn: II–assessment and resuscitation. BMJ 329:101–103. https://doi.org/10.1136/BMJ.329.7457.101
Tan Chor Lip H, Tan JH, Thomas M et al (2019) Survival analysis and mortality predictors of hospitalized severe burn victims in a Malaysian burns intensive care unit. Burn Trauma 7:1–8. https://doi.org/10.1186/S41038-018-0140-1/FIGURES/1
Ganesamoni SR, Kate V, Sadasivan J (2010) Epidemiology of hospitalized burn patients in a tertiary care hospital in South India. Burns 36:422–429. https://doi.org/10.1016/J.BURNS.2009.06.212
Güldoğan CE, Kendirci M, Gündoğdu E, Yastı AÇ (2019) Analysis of factors associated with mortality in major burn patients. Turkish J Surg 35:155. https://doi.org/10.5578/TURKJSURG.4065
Alipour J, Mehdipour Y, Karimi A (2020) Epidemiology and outcome analysis of 3030 burn patients with an ICD-10 approach. Ann Burns Fire Disasters 33:3
Forbinake NA, Ohandza CS, Fai KN et al (2020) Mortality analysis of burns in a developing country: a CAMEROONIAN experience. BMC Public Health 20:1–6. https://doi.org/10.1186/S12889-020-09372-3/FIGURES/2
Temiz A, Albayrak A, Peksöz R et al (2020) Factors affecting the mortality at patients with burns: single centre results. https://doi.org/10.14744/tjtes.2020.37862
Yazıcı H, Uçar AD, Namdaroglu O, Yıldırım M (2022) Mortality prediction models for severe burn patients: which one is the best? Turkish J Trauma Emerg Surg 28:790. https://doi.org/10.14744/TJTES.2021.29540
Brandão C, Meireles R, Brito I et al (2021) The role of comorbidities on outcome prediction in acute burn patients. Ann Burns Fire Disasters 34:323
Lionelli GT, Pickus EJ, Beckum OK et al (2005) A three decade analysis of factors affecting burn mortality in the elderly. Burns 31:958–963. https://doi.org/10.1016/J.BURNS.2005.06.006
Wibbenmeyer LA, Amelon MJ, Morgan LJ et al (2001) Predicting survival in an elderly burn patient population. Burns 27:583–590. https://doi.org/10.1016/S0305-4179(01)00009-2
Akhtar M, Basari R, Haq A et al (2014) Burn injury associated with comorbidities: impact on the outcome. Indian J Burn 22:51. https://doi.org/10.4103/0971-653X.147005
Thombs BD, Singh VA, Halonen J et al (2007) The effects of preexisting medical comorbidities on mortality and length of hospital stay in acute burn injury: evidence from a national sample of 31,338 adult patients. Ann Surg 245:629–634. https://doi.org/10.1097/01.SLA.0000250422.36168.67
Tarim MA Factors affecting mortality in burn patients admitted to intensive care unit. East J Med 18:72–75
Kraft R, Kulp GA, Herndon DN et al (2011) Is there a difference in clinical outcomes, inflammation, and hypermetabolism between scald and flame burn? Pediatr. https://doi.org/10.1097/PCC.0B013E31820AC2C5. Crit Care Med 12:
Habouchi S, Bouamra A, Bezzaoucha A, Joucdar S (2020) Estimation of survival rate in electrical injuries, experience in Algerian burn centers. Burn Open 4:141–145. https://doi.org/10.1016/J.BURNSO.2020.07.001
Ghavami Y, Mobayen MR, Vaghardoost R (2014) Electrical burn injury: a five-year survey of 682 patients. Trauma Mon 19:29–33. https://doi.org/10.5812/TRAUMAMON.18748
Mobayen M, Sadeghi M (2022) Prevalence and related factors of electrical burns in patients referred to Iranian Medical Centers: a systematic review and meta-analysis. World J Plast Surg 11:3. https://doi.org/10.52547/WJPS.11.1.3
Bounds EJ, Khan M, Kok SJ (2023) Electrical burns. StatPearls
Inhalation injury from heat, smoke, or chemical irritants - UpToDate. https://www.uptodate.com/contents/inhalation-injury-from-heat-smoke-or-chemical-irritants/print. Accessed 19 Mar 2024
Colohan SM (2010) Predicting prognosis in thermal burns with associated inhalational injury: a systematic review of prognostic factors in adult burn victims. J Burn Care Res 31:529–539. https://doi.org/10.1097/BCR.0B013E3181E4D680
El-Helbawy RH, Ghareeb FM (2011) Inhalation injury as a prognostic factor for mortality in burn patients. Ann Burns Fire Disasters 24:82
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
The authors made substantial contributions to the design and analysis of the present retrospective study. Additionally, they actively took part in the literature review, collecting data and information, data analysis, and writing the manuscript. The entire process of examining and approving the finished manuscript was handled by the authors.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Approval of the Institutional Review Board of King Abdullah International Medical Research Center was acquired prior to the conduction of the present study (approval number NRC22R/186/04).
Consent to participate
Patient confidentiality was ensured, and the patients' data were collected and used by the research team only. Serial numbers were used instead of medical record numbers to ensure anonymity. Due to the retrospective nature of the study, and the use of anonymized patient data, the requirement for informed consent was waived.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ulhaq, M.M., Alkhadhrawi, M.N.H., Qasim, S.S. et al. Burn characteristics, management strategies, and mortality trends of patients admitted in the intensive care unit: a six-year retrospective analysis. Eur J Plast Surg 47, 85 (2024). https://doi.org/10.1007/s00238-024-02233-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00238-024-02233-x