Abstract
Fibro-adipose vascular anomaly (FAVA) is a new entity characterized by fibro-adipose infiltration of muscle, pain, and contracture. The main differential diagnosis includes venous malformation and intramuscular hemangioma. Early treatment and physical therapy are of paramount importance to prevent severe contractures, muscle fibrosis, and limb atrophy. We present a case report of a 24-year-old female patient with FAVA in the volar aspect of left arm, presented with limitation to pronation and supination and pain. The patient was operated in 2017 in our center, performing a total resection of the mass and 2-year follow-up. We describe the criteria that we performed to diagnose the left forearm FAVA in this patient, based on the history; the magnetic resonance imaging, which demonstrated muscle replaced by heterogeneous soft tissue, intramuscular phlebolit, and dilated vessels; and histological images that showed a vascular proliferation associated with adipocytes and dense fibrous tissue replacing and infiltrating the skeletal muscle. En bloc resection of the mass was performed successfully, and it gave excellent results with recovery of limitation and improvement of pain and swelling that were maintained at 2-year follow-up. Surgery is a reliable and curative option in FAVA and could be the only one for long-term control of this entity.
Level of evidence: Level V, therapeutic; diagnostic study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fibro-adipose vascular anomaly (FAVA) is a new delineated disorder included in the International Society for the Study of Vascular Anomalies of 2018, as a provisionally unclassified vascular anomaly. It is associated with pain, contracture of affected extremity, and functional limitations [1], explained by fibro-fatty infiltration of muscle and unusual phlebectasia, constituting a distinct clinical, radiological, and histopathological entity. FAVA most commonly occurs on the calf of middle-aged women, and the main differential diagnosis includes venous malformation and intramuscular hemangioma [2].
Early treatment and physical therapy are of paramount importance to prevent severe contractures, muscle fibrosis, and limb atrophy. Optimal treatment for FAVA has not been fully established due to its recent description. Treatment options have included sclerotheraphy, cryoablation, surgery, or even medical treatment [3].
Case report
We present a case report of a 24-year-old female patient with a 10-year history of a progressive painful mass in volar aspect of the left forearm. The patient was clinically diagnosed of venous malformation without histopathology and treated with sclerotherapy at another center, but without control of pain and progression of the mass. Finally, she was referred to our center.
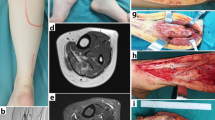
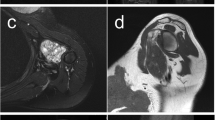
At examination, there was a palpable mass in the forearm with swelling, important limitation to pronation and supination, atrophy of the thenar, hypothenar, and interosseous muscles. Magnetic resonance imaging demonstrated a 12 × 4 × 4 cm mass in the volar aspect of the left forearm. In axial T1-weighted MRI, there was muscle replaced (flexor carpi radialis and flexor digitorum superficialis) by heterogeneous soft tissue with signal intensity higher than adjacent normal muscles. Coronal T1-weighted MRI noted intramuscular phlebolit. Sagittal fat-suppression MRI noted the longitudinal distribution of disease and dilated vessel (Fig. 1).
Magnetic resonance imaging (MRI) of the left forearm evidenced a diffuse fibro-adipose vascular anomaly (FAVA) in the volar aspect. a Axial T1-weighted MRI. Muscle replaced by heterogeneous soft tissue with signal intensity higher than adjacent normal muscles (white arrow). b Coronal T1-weighted MRI, note intramuscular phlebolit (white arrow). c Sagittal fat-suppression MRI, note the longitudinal distribution of disease and dilated vessel (white arrow)
Due to the functional limitation and pain, surgery was proposed, and an en bloc resection was performed. Operative exploration evidenced a fibrotic mass extending into the adjacent fascia and fat planes, in contact with the radial and cubital bone but separated by a delimited plane. The muscular and bone component of the mass was resected completely, without neurolysis (Fig. 2).
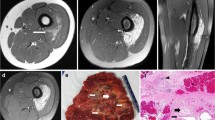
Histological examination (Fig. 3) showed a vascular proliferation associated with adipocytes and dense fibrous tissue replacing and infiltrating the skeletal muscle. The vascular component included clusters of muscularized venous structures intermingled with ectatic thin-walled venous channels and capillary vessels organized in lobular pattern. No organized thrombi were observed. Some of the vascular lobules were surrounded by lymphoplasmacytic aggregates. Lymphatic vascular component was supported by endothelial D2-40 immunopositivity. Furthermore, focal bone metaplasia, atrophic skeletal muscle, and entrapped nerves were also noted.
Histopathologic examination. a Variable admixture of dense fibro-fatty tissue and vascular clusters, with ecstasies. Lobular pattern of growth and lymphoplasmacytic aggregates (H&E, × 20). b Clusters of thin-walled, blood-filled venous channels alternated with muscularized vessels in fibro-adipose tissue (H&E, × 100). c Lobular pattern of growth and lymphoplasmacytic aggregates. Focal bone metaplasia (H&E, × 40). d Thin-walled channels and adipose tissue embedded in a fibromyxoid stroma (H&E, × 100)
Follow-up examination 3 months after surgery evidenced an important improvement in pronation and supination, with recovery of limitation and improve of pain in 2-year follow-up.
Discussion
Traditional classification for low-flow vascular malformations includes venous malformation (VM) and lymphatic malformation (LM) [4]. However, FAVA is a newly recognized clinicopathologic and radiologic entity, included in the International Society for the Study of Vascular Anomalies of 2018 as a provisionally unclassified vascular anomaly.
In 2014, Alomari et al. described a cohort of 18 patients with clinical, radiologic, and histopathological features of this new vascular entity [2]. This was categorized like a complex mesenchymal malformation that includes fibro-fatty infiltration of the muscles, phlebectasia and intertwining of anomalous veins, and subcutaneous and cutaneous lymphatic malformation [1].
The clinical features of FAVA include unusual and disproportionately severe pain and contracture, affecting specific anatomic areas (calf and forearm). The constant pain and discomfort seen in these patients are multifactorial. There is a dysfunction and muscular contractility affectation explained by fibro-fatty infiltration of the muscles. The neural and perineural fibrous scarring contributes to the neurogenic pain. The anomalous ectatic veins have stasis and hypertension causing pain, swelling, and discomfort. Pain explains loss of movements of involved extremity, contributing further to dysfunction, constituting a vicious cycle of pain and contracture [1] (Fig. 4).
Similar to the cohort reported by Alomari et al. in 2014, our patient was a young woman who presented with a painful forearm mass, that was initially diagnosed as a VM with muscle involvement on MRI/ultrasound, and firstly treated with sclerotherapy.
On MR imaging, FAVA is of heterogeneous signal intensity on T1-weighted images and of moderately hyperintense, heterogeneous signal intensity on T2-weighted images. It is centered in the musculature, frequently with associated increased fat in the fascial and subcutaneous regions and readily identifiable phlebectasia [5] replacing the normal muscle [2] and sometimes complicated by thrombi [6].
Among the histological findings, similar to other cases previously reported [2, 7], our case showed vascular proliferation associated with adipocytes and dense fibrous tissue replacing and infiltrating the skeletal muscle. The vascular component included clusters of muscularized venous structures intermingled with ectatic thin-walled venous channels and capillary vessels organized in lobular pattern. The presence of phleboliths is more likely to represent venous malformations; however, it is occasionally present in FAVA as in our case [2]. The main differential diagnosis included a venous malformation [2] (see Table 1).
Treatment options for this entity include observation/conservative approach, physical therapy, casts or splints, sclerotherapy, steroid injections, surgical excision, neurolysis or neurectomy [1], cryoablation, and more recently, the use of sirolimus [3].
Sclerotherapy could be performed in the smaller venous component, with less effect in dominant solid fibro-fatty component [2], which explains the poor management of this disease with this treatment.
Shaikh et al. in 2016 reported the percutaneous cryoablation in a retrospective cohort study of 20 patients and 26 sites, concluding that it is a safe and minimally invasive option for symptomatic FAVA lesions. Eighty percent of the patients were satisfied with this treatment, but control of pain, swelling, and functional restriction was achieved in less than 50% of patients [1].
In 2019, Ramaswamy R et al. reported the use of cryoablation as a primary line treatment for 4 cases of FAVA in the foot and calf with control of pain in 3 patients. They concluded that percutaneous cryoablation appears to be safe and effective in the treatment of symptomatic low-flow vascular malformations, including FAVA, either as a primary modality or secondary therapy in addition. However, they only use this procedure in circumscribed focal lesion and localized in muscle and/or subcutaneous region [8].
In 2017, Erickson et al. presented two patients affected with FAVA with severe pain and functional impairment in which sirolimus produced rapid, dramatic improvement. They hypothesized that FAVA may be the result of a somatic activating mutation in PIK3CA, a gene related to overgrowth spectrum that includes a group of disorders with fibro-adipose overgrowth and infiltration into muscle and vascular malformations. They concluded that oral sirolimus was rapidly effective in those two patients, with improvement in the quality of life. On the other hand, they anticipate there will be recurrence after cessation of treatment and a very low dose maintenance therapy would be necessary [3] with the concomitant risk of immunosuppression.
Surgical resection is associated with longer recovery, increased risks, and sequelae [1], but is an effective treatment and the only one for long-term control of FAVA [2]. In cases with extensive muscle involvement and neurovascular entrapment, compartment decompression, partial resection, neurolysis, and tendon lengthening can be very effective [9]. Occasionally, the entire muscles or muscle groups may need to be removed to treat the pain and contracture; in these cases, tendon transfers or free functional muscle reconstruction is often necessary [10]. In our case, surgical resection gave excellent results with recovery of limitation and improvement of pain and swelling that were maintained at 2-year follow-up. There are few cases in literature about surgical treatment of forearm FAVA and therefore, additional studies in a larger cohort are needed to evaluate different management. [1, 2, 7, 9].
Conclusion
To our knowledge, this article presents a case of successful surgical treatment of FAVA in forearm, without recurrence at 2-year follow-up and without sequelae. We consider that surgery is a reliable and curative option in selected cases and could be the only one in for long-term control of FAVA; although, larger studies are needed comparing different treatment options for this disease.
References
Shaikh R, Alomari A et al (2016) Cryoablation in fibro-adipose vascular anomaly (FAVA): a minimally invasive treatment option. Pediatr Radiol 46:1179–1186
Alomari A, Spencer S, Arnold R, Chaudry G, Kasser JR, Burrows PE, Govender P, Padua HM, Dillon B, Upton J, Taghinia AH, Fishman SJ, Mulliken JB, Fevurly RD, Greene AK, Landrigan-Ossar M, Paltiel HJ, Trenor CC 3rd, Kozakewich HP (2014) Fibro-adipose vascular anomaly: clinical-radiologic-pathologic features of a newly delineated disorder of the extremity. J Pediatr Orthop 34:109–117
Erickson J, McAuliffe W, Blennerhassett L, et al. (2017) Fibroadipose vascular anomaly treated with sirolimus: Successful outcome in two patients. Pediatr Dermatol, 34(6), e317–e320
Wassef M, Blei F, Adams D, Alomari A, Baselga E, Berenstein A, Burrows P, Frieden IJ, Garzon MC, Lopez-Gutierrez JC, Lord DJ, Mitchel S, Powell J, Prendiville J, Vikkula M, ISSVA Board and Scientific Committee (2015) Vascular anomalies classification: recommendations from the international society for the study of vascular anomalies. Pediatrics 136:e203–e214
Sheybani E, Eutsler E, Navarro O (2016) Fat-containing soft-tissue masses in children. Pediatr Radiol 46(13):1760–1773
Johnson C, Navarro O (2017) Clinical and sonographic features of pediatric soft-tissue vascular anomalies part 2: vascular malformations. Pediatr Radiol 47(9):1196–1208
Fernandez-Pineda I, Marcilla D, Downey-Carmona F et al (2014) Lower extremity fibro-adipose vascular anomaly (FAVA): a new case of a newly delineated disorder. Ann Vasc Dis 7(3):316–319
Ramaswamy R, Tiwari T, Darcy M et al (2019) Cryoablation of low-flow vascular malformations. Diagn Interv Radiol 25:225–230
Mende K, Vargesson N, Sivakumar B (2018) Vascular anomalies of the upper limb. J Hand Surg Eur Vol 44(3):233–241
Taghinia A, Upton J (2018) Vascular Anomalies. J Hand Surg [Am] 43(12):1113–1121
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Susana López, Andreé Ibarra, Eulalia Baselga, Carmen Vega, Caterina Fumagalli, Sandra Valverde, and Jaume Masia. The first draft of the manuscript was written by Andreé Ibarra, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of informed consent
Informed consent was obtained from the individual participant included in the study. Informed written consent was obtained from the patient in this case report for inclusion of clinical data and photographs.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
López, S., Ibarra, A., Baselga, E. et al. Fibro-adipose vascular malformation (FAVA) in forearm: a successful surgical approach and literature review. Eur J Plast Surg 43, 495–500 (2020). https://doi.org/10.1007/s00238-019-01620-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-019-01620-z