Abstract
Background
Rhinoplasty continues to be among the most popular surgical cosmetic treatments around the world. This is often a reflection of the significance of nose shapes in sociocultural, ethnic, and psychological contexts. Despite developments in the therapeutic field of cosmetic surgery, there is scarce information available within current literature concerning the effects of cosmetic procedures on quality of life (QOL), particularly in Iran. The purpose of this study was to survey QOL among Iranian adults before and after rhinoplasty.
Methods
From July 2015 to July 2016, 83 patients over 16 years of age seeking cosmetic rhinoplasty were included in this study. Demographic information such as age, sex, marital status, education, occupation, and monthly income of patients were recorded. SF-36 version 2, Rosenberg self-esteem scale (RSES), and WHOQOL-BREF questionnaires were completed by a single trained interviewer for all patients, before and 6 months after rhinoplasty. Data analysis was conducted using SPSS ver. 16. Results before and after surgery were compared.
Results
The mean age of the subjects was 24.87 ± 5.8 years, with a median of 24 years. The female-to-male ratio was 4.53:1. In all cases and all questionnaires, QOL was improved after rhinoplasty. Significant differences were observed on six subscales of SF-36 comprised bodily pain (p = 0.003), general health (p = 0.002), vitality (p = 0.005), social functioning (p < 0.001), emotional role (p = 0.02), and mental health state (p = 0.012). According to RSES and WHOQOL-BREF questionnaires, self-esteem (p = 0.002), psychological health (p < 0.001), social relationships (p < 0.001), and general quality of life (p = 0.011) indicated significant differences.
Conclusions
Our data suggest that QOL can be improved after rhinoplasty in Iranian adult patients. With proper patient selection and a successful operation, improvement of QOL can be expected.
Level of Evidence: Level III, risk / prognostic study
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cosmetic rhinoplasty is a surgical procedure aimed at reshaping the nose for aesthetic reasons [1]. Initially, rhinoplasty was exclusively performed for repairing tissue damage, or performing what is known as reconstructive rhinoplasty. However, in recent times, rhinoplasty is also being used for aesthetic reshaping of noses, or what is identified as Elective Cosmetic Surgery (ECS). In 2013, it was considered the fifth most common cosmetic surgical procedure worldwide, accounting for 8.8% of the total surgical procedures worldwide [2]. While there is often a social status attached to rhinoplasty—that is—it is often considered reserved for wealthy young Caucasian women, there has been an increase in the diversity of demographics seeking the procedure across ethnic, gender, age, and socioeconomic backgrounds [3]. According to the International Society of Aesthetic Plastic Surgery, 15.4% of the total number of surgical procedures in the world take place in the USA, followed by 13.9% in Brazil, 3.4% in Japan, and 4.6% in South Korea respectively. In the USA, other prevalent cosmetic surgeries consist of breast augmentation, liposuction, eyelid surgery, and rhytidectomy [4]. According to the American Plastic Surgery Association, a total of 12.1 million plastic surgeries have been performed on females since 2011—that is—92 % of the total number of the plastic surgeries performed [5]. In Iran, for instance, 95% of the patients aged 14–45 years are females willing to have either rhinoplasty or hair transplants, while the other 5% consist of males undertaking cosmetic rhinoplasty procedures [6]. In addition, 41 % of the patients from Iran are under 25 years of age while 65% have been under 35 years of age [6].
The increasing prevalence of cosmetic surgery in both Western and non-Western societies has brought increasing interest among medical researchers into examining the internal and external factors that motivate a wide demographic toward undertaking surgical procedures [7]. While previous literature have attributed the increasing availability of plastic surgeons, the role of the media [7, 8] and personal factors (such as level of religiosity, history of previous violent relationships, and belief system factors) [9,10,11,12] as contributing to the increasing prevalence of cosmetic surgeries worldwide, other factors such as technological advances in cosmetic surgery making it safer and less recovery time have been suggested [13]. One key factor which has been amply discussed is the impact of an awareness of a “beauty bias” [8]. Physical attractiveness is considered one of the most effective factors in social interaction, and facial attraction is a critical subtype of physical attractiveness given its immediate noticeability. In certain cases, issues like low life satisfaction are arguably brought about by a pre-conceived “beauty bias,” wherein self-rated attractiveness is shown to be strongly correlated with increased likelihood of cosmetic surgery [14]. Additionally, stereotypes about the beautiful having higher moral standards and having higher perceived quality of life become key assumptions in social interactions [15].
Cosmetic rhinoplasty is believed to have a remarkable effect on a patient’s physical and mental health when investigated from an evidence-based medicine approach [16,17,18]. The effect of cosmetic rhinoplasty has largely been evaluated from both objective and subjective outcomes. Patient-reported outcome measures (PROMs) are increasingly used in examining changes in the quality of life of patients undergoing aesthetic procedures. Several health-related quality of life domains covering physical, psychosocial, and sexual well-being are used. Some of the specific instruments used in evaluating cosmetic rhinoplasty involve the 36-item health-surgery questionnaire (SF-36 version 2) [19], the Rosenberg self-esteem scale (RSES) [20], Rhinoplasty Outcome Evaluation (ROE) [21], Nasal Obstruction Symptoms Evaluation Scale (NOSE Scale) [22], Glasgow Benefit Inventory (GBI) [23], FACE-Q Rhinoplasty Module (FACE-Q RM) [24], and the Evaluation of Aesthetic Rhinoplasty Scale (EARS) [25] just to mention a few. Significant improvement in perceived quality of life is commonly observed in patients from studies examining the short-term and intermediate-term outcomes following cosmetic surgeries. For instance, facial cosmetic surgery candidates demonstrated improved quality of life in patients as early as 2 months to 1 year post-operation when using the SF-36 measure [26, 27]. Other studies on rhinoplasty patients have reported a positive conclusion for up to 3 years post-operative when using Nasal Obstruction Symptom Evaluation and Rhinoplasty Outcomes Evaluation questionnaires [28]. A systematic review of the aforementioned patient-reported outcome measures (PROMs) after rhinoplasty, however, identified the need for a new self-assessment tool to emphasize the functional, psycho-relational, and aesthetic properties of satisfaction and quality of life in patients undertaking rhinoplasty [29].
Alternatively, the World Health Organization Quality of Life (WHO-QoL) is a cross-culturally developed instrument used to assess the general quality of life based upon a person’s positive satisfaction by socioeconomic status, cultural and political systems in which they live, objectives, expectations, standards, and concerns [30]. The WHO-QoL measures quality of life across physical health, psychological, social relationships, and environmental domains. The World Health Organization defines quality of life as an individual’s perception of their position in life in terms of the culture and value systems they live in and in terms of their goals, expectations, standards, and concerns [31]. Previous studies using the WHO-QoL instrument have reported mixed outcomes. One study assessing quality of life in patients undergoing rhinoseptoplasty found that turbinate reduction did not improve short-term quality of life outcomes, although both intervention groups presented higher post-operative WHO-QoL-brief scores [32].
Rhinoplasty continues to be the most common form of plastic surgeries performed in Iran, followed only second by crest and wrinkle surgeries [6]. Approximately 180 in 100,000 (a ratio of 2.75%) people perform rhinoplasties in Iran, making it ranked seventh among the fifty most common invasive surgical procedures in Iran, preceded only by natural birth, cataract surgery, caesarian sections, coronary angiography, varicocele surgery, and appendectomy from first to sixth places respectively [6]. The demand for plastic surgery in Iran has had an 80% increase since the early 1990s, with an increased demand for these types of procedures among mature aged people [6]. In Iran, the majority of clients are women, but recently, the number of men applying for cosmetic surgery has increased [6]. A study in 2012 reported that Iranian males alone spend more than fifty million dollars annually for surgical rhinoplasty and twice as much for Botox procedures [6]. However, the specified expenditure mentioned is only a small fraction of the total price that is contributed toward cosmetic surgery [6].
Only a small amount of quality of life research has been investigated in Iran concerning cosmetic rhinoplasty. Previous studies have attempted to validate the WHOQOL-BREF questionnaire in Iran with reasonable success [6]. Previous studies in Iran have shown a variety of outcomes ranging from positive [6] to negative [33] quality of life. One study suggested that rhinoplasty surgery was not found to have any beneficial impact on mental health [6], while other studies have suggested a reduction in the quality of life post-rhinoplastic surgery [6]. In contrast to both previous studies, one study using SF-36, NOSE, and Rosenberg questionnaires saw significant differences in pre- and post-operative quality of life scores [34]. Given the high prevalence of rhinoplasty in Iran, the high costs associated with this operation for both people and the health system, the conflicting results obtained from the various studies on the impact of surgery on quality of life, and the little overall research that has already been carried out in this field, this study will attempt to examine the quality of life of patients pre- and post-rhinoplasty surgery in accordance with the several standardized questionnaires.
Material and Methods
In this study, individuals aged 16 years and older were referred to Pars Surgical Centre, Mazandaran University of Medical Science (the University of Medical Sciences in Sari, the Centre of Mazandaran Province), from July 2015 to July 2016 for elective rhinoplasty and were enrolled in this study. Patients younger than 16 years of age, with known psychological disorders or with previous cosmetic rhinoplasty, were excluded from this study. Eighty-three patients were studied (69 patients with 20% for lost to follow-up probability). All 83 patients completed the standard QOL questionnaires in both the first and second phases. A trained interviewer interviewed each patient separately and completed a short form 36-item health-surgery questionnaire (SF-36 version 2), the Rosenberg self-esteem scale (RSES), and the WHOQOL-BREF, which were translated and validated for the Iranian population. Demographic characteristics were also collected at the beginning of the questionnaire.
The SF-36 version 2 questionnaire is a brief and multifunctional health survey from the patient’s point of view and has 36 questions for people aged 14 years and older. The SF-36 version 2 consists of eight scaled scores that are the minimum standards necessary for psychological study in comparing individuals. These eight scales have 40 items from which the mental and physical component scores are obtained. The RSES questionnaire consists of ten questions about self-esteem, and each question has four options for a total score ranging from 10 to 40. The RSES measures global self-esteem and personal worthlessness; higher scores indicate higher self-esteem. The World Health Organization (WHO) has developed a quality of life instrument, the WHOQOL, which captures many subjective aspects of quality of life. The WHOQOL-BREF that contains 26 items is one of the best-known instruments that has been developed for cross-cultural comparisons of quality of life and is available in more than 40 languages. The WHOQOL-BREF covers four different domains of quality of life.
After collecting the data, the patients underwent rhinoplasty. Six months after surgery, the patients were invited for the second interview. Six months was elected as the time for the second interview given the cultural-subjectivity of perceiving time. This time was considered appropriate for patients to appropriately obtain initial attitudes and perceptions of the new experience. The same questionnaires with the same methodology were completed by the same interviewer. Data analysis was conducted using SPSS ver. 16. Paired sample t tests and Wilcoxon signed-ranks tests were used to compare the results before and after rhinoplasty. To increase the accuracy of comparison between different scales of the SF-36 version 2 and other questionnaires, a linear transformation was conducted. The significant p value was set at a value of less than 0.05.
This study was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was given by all participants, who were included in this study.
Results
The mean age of the 83 subjects was 24.87 ± 5.8 years, with a median age of 24 years and range 17 to 48 years. Most subjects (65.1%) were between 16 and 25 years old. The female-to-male ratio was 4.53:1. Most individuals (72.3%) were single, and 25.3% were married. The average number of children that the married subjects had was 0.65 ± 0.64, with a median of 1, and a total number ranging from 0 to 2. 2.4% of the participants were divorced. The most common educational level reached by the patients was university level (49.4%). Those with secondary school education comprised 36.1% and over-secondary school diploma comprised 14.5% of the participants. Subjects were university students (47%), housewives (16.9%), employed (13.3%), students (8.4%), self-employed (7.2%), or unemployed (7.2%). The subjects were categorized into four groups according to monthly income. Those with an income greater than 600 US dollars comprised 48.2% of the study population, while 24.1% had a monthly income 200–400 US dollars, 22.9% had a monthly income 400–600 US dollars, and 4.8% had an income less than 200 US dollars (Table 1).
The results of the SF-36 version 2 questionnaire (Table 2) indicated higher scores (better conditions) for all eight subscales except physical role. In six subscales, including bodily pain (p = 0.003), general health (p = 0.002), vitality (p = 0.005), social functioning (p < 0.001), emotional role (p = 0.02), and mental health state (p = 0.012), there were statistically significant differences before and after rhinoplasty. In the two other subscales, including physical functioning (p = 0.57) and physical role (p = 0.94), no statistically significant differences were observed.
Two scales of the SF-36 version 2 questionnaire (Table 3), physical health (p = 0.03) and mental health (p < 0.001), were improved and statistically significant differences were observed. At the end, final score significantly improved too (p = 0.001).
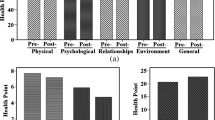
As seen in Chart 1, in the Rosenberg self-esteem scale, the mean score before rhinoplasty was 22.6 ± 4.66. After surgery, the mean score increased to 24.01 ± 3.73. These results indicate that there were statistically significant differences observed in the RSES self-esteem scale (p = 0.002).
The result of WHOQOL-BREF indicated higher scores (better conditions) for all domains (Table 4). In two domains including physical health (p = 0.1) and environmental health (p = 0.36), no statistically significant differences were observed. But other domains including psychological health (p < 0.001), social relationships (p < 0.001), and general quality of life (p = 0.01) significantly improved 6 months after surgery.
Discussion
Patient-reported outcome measures (PROMs) are becoming a relevant tool for studying the success of a procedure in modern clinical outcome research. With the increasing application of evidence-based medicine in medical practice, facial surgeries such as cosmetic procedures in rhinoplasty are being enhanced to ensure patient quality of life is best achieved. Patient-reported outcome measures (PROMs) are an effective qualitative tool with excellent psychometric properties developed from patient stories to ensure content validity [29]. This study was among the very few in Iran and around the world to have employed the WHOQOL-BREF instrument in examining quality of life in patients undergoing rhinoplasty. Quality of life (QoL) assessments are important indicators of overall health in the growing literature on evidence-based medicine in cosmetic surgery. The importance of quality of life as an outcome measure is particularly appreciated by plastic surgeons, given the inability to measure aesthetic procedures merely by using mortality and morbidity as outcome measurements. However, despite the growing importance of quality of life in evidence-based medicine, there have been little attempts toward implementing this outcome measurement in rhinoplasty. According to a systematic review, Barone et al. [29] identified three different categories for surgery-specific questionnaires for rhinoplasty: (1) functional self-assessment, (2) aesthetic self-assessment, and (3) aesthetic and functional self-assessment. The conclusion drawn from Baron et al.’s [29] systematic review was the need for a PROM that collectively encompassing the functional, psycho-relational, and aesthetic properties to measure quality of life in patients undergoing rhinoplasty.
Given current limitation in rhinoplasty-specific PROMs, we employed the WHOQOL-BREF, SF-36 version 2, and the Rosenberg questionnaires to effectively examine quality of life in Iranian patients undergoing rhinoplasty. Reasons for why quality of life measures have not been employed into rhinoplasty-specific PROMs may be due to two reasons: firstly, the mechanistic model of medicine, and secondly, the difficulty in translating the cultural-sensitivity of perceiving quality of life into a generalized one-fit all model. The mechanistic model of medicine is focused on the eradication of disease and associated symptoms before considering the humanistic element associated with health care. Quality of life is a humanistic assessment concerned with the ultimate purpose of health care—that is—in what way the proposed solution to the problem, i.e., rhinoplasty, has contributed to the functional and emotional well-being of the person. In contrast, rhinoplasty-specific questionnaires such as the Rhinoplasty Outcomes Evaluation (ROE) have yet been produced to address this humanistic facet. For instance, according to Baron et al.’s [29] study, contents such as “self-perception of nose appearance,” “looking younger,” “self-concept,” “feeling normal,” “feeling attractive,” “concern regarding others’ negative perception of self,” “psychological functions,” “concern/excessive worry,” “social network appearance,” “appearance in photos,” and “physical function” were all missing in current rhinoplasty-specific PROMs. This raises the issue of which best method exists for quantitatively accounting for humanistic factors.
Secondly, most other measures of health status have been developed in North America and UK, thereby making the translation of these measures for use in other cultural contexts extremely difficult. Any attempt to translate the concept of quality of life would require an appreciation of the cultural context of the patient rather than producing a generalized one-fit all model. In the case of this study, it would be difficult to quantify the specifically Iranian cultural influences shaping post-operative rhinoplasty satisfaction using rhinoplasty-specific questionnaires which do not consider the Iranian sociocultural context which can explain why many Iranian youths—either female or male—are seeking aesthetic rhinoplasty. In contrast, generic questionnaires have been widely used across various cultures, legitimizing its internal validity. For instance, WHOQOL-BREF was developed through an exploration of the quality of life in 15 diverse cultures. Given that the subjects of this study involved a single cultural group, i.e., Iranians, a generic questionnaire addresses the two aforementioned problems—the mechanistic model of medicine and cultural-specificity of population being targeted better than rhinoplasty-specific measurement tools.
Most of the quality of life studies using other scales have also rendered positive results in QoL. In one study by Kotzampasakis et al. [35] using GBI, a significant difference in quality of life before and after rhinoplasty was observed. This is further supported in a previous study by Chauhan, Warner, and Adamson [36] where a significant positive benefit was reported in the general subscale, physical health, social support, and total scales, although no significant difference was found in the early and late post-operative periods. In contrast to Chauhan, Warner, and Adamson’s study with GBI [36], other studies using SF-36 scales have suggested an improved post-operative score in physical and mental health domains [37]. In measures using FACE-Q on patients of rhinoplasty, improvements in appearance, social functioning, and psychological well-being have also been observed [3]. One point of concern raised by previous studies on quality of life was that a difference in instruments used may be the cause for difference in outcomes obtained [6]. Hence, a study using the WHOQOL-BREF instrument is arguably important for mounting preliminary evidences when assessing these concerns.
The results of our study based on the SF-36 version 2, RSES, and WHOQOL-BREF questionnaires indicate that QoL improves up to 6 months following rhinoplasty. According to SF-36 questionnaire, six subscales including bodily pain, general health, vitality, social functioning, emotional role, and mental health state indicated statistically significant differences before and after rhinoplasty. Additionally, scales for the SF-36 version 2 questionnaire, physical health and mental health, and final scores were found to be significantly improved. In the Rosenberg self-esteem scale, our results indicated that there were statistically significant differences observed in the participants’ self-esteem pre- and post-operatively. These findings are consistent with previous studies that have demonstrated that quality of life evaluated with the SF-36 version 2 and RSES questionnaire improved significantly in all eight subscales, and even in a group showing no changes in quality of life, four subscales, i.e., physical performance, role of emotion, social performance, and mental health, showed statistically significant differences before and after surgery [24]. The results obtained from the SF-36 subscales, however, showed differences from previous studies in the domains of general health and social functioning, where no significant differences were obtained for those domains.
In addition, our results also show discrepancies with other previous Iranian studies. A study by Zojaji et al. [6] using WHOQOL-BREF instrument found no significant improvement in quality of life across all domains except for psychological health. Our study upon using WHOQOL-BREF, however, found a significant improvement in quality of life in not only psychological health, but also in social relationships and general quality of life domains. It was suggested that a fundamental difference between two conflicting results obtained by Fatemi et al. [34] and Zojaji et al. [6] may have been a difference in the instruments employed; Zojaji et al.’s [6] study used WHOQOL-BREF whereas Fatemi et al.’s [34] study used SF-36, ROSE, and RSES. However, this study confirms that even upon employing the WHOQOL-BREF instrument, discrepancy was imminent between our findings and Zojaji et al.’s [6] study. There are a few reasons for the different results obtained: firstly, the follow-up period and the sample population examined in Zojaji et al.’s [6] study. In contrast to our study which followed up after 6 months, Zojaji et al.’s [6] study followed up after 3 months. Our reason for this was that a reasonable time frame is required when providing a qualitative response to one’s perception of quality of life following rhinoplasty. This could be one source that may justify the discrepancy in our findings. Secondly, our study recruited 83 patients in contrast to Zojaji et al.’s [6] 50 patients. Despite losing 20% of our patients at follow-up, it is unclear whether Zojaji et al.’s [6] study was able to recruit the entire 50 patients for a follow-up. Our findings also go against a previous study by Mohammadshahi et al. [33] which suggested a decrease in quality of life in patients undergoing rhinoplasty. Reasons for differences between our findings and the findings ascertained in Mohammadshahi et al.’s [33] study could be that there was no specific time frame the study kept to when carrying out the follow-up interview. While our study ensured 6-month follow-up interviews, Mohammadshahi et al.’s [33] study statistically recorded interviews from 3 to 18 months following surgery. It is unknown what proportion of Mohammadshahi et al.’s [33] study examined patients after 3, 6, and 12 months for instance, although it is acknowledged that there existed a positive correlation between length of time since surgery and quality of life measured.
Study limitations
Although applicants were informed that their data would be kept confidential, it is possible that subjects did not provide correct responses to the questionnaires. This could be due to insurance reasons regarding cosmetic surgery. Additionally, given the general issues associated with patients being invited to return for a follow-up assessment, our results were unable to account for demand characteristics which could have been at play in determining their perceived quality of life.
Conclusion
As our study showed, patients who underwent rhinoplasty surgery showed significant improvement in the quality of life after surgery. It seems that rhinoplasty is capable of creating a positive effect on appearance and improves bodily pain, general health, vitality, social functioning, emotional role, mental health state, self-esteem, psychological health, social relationships, and general quality of life according to SF-36, RSES, and WHOQOL-BREF questionnaires. It means that careful patient selection and a successful operation may improve mental and physical health.
References
Davis RE (2006) Rhinoplasty and concepts of facial beauty. Facial Plast Surg 22(03):198–203
Cosmetic Surgery National Data Bank (2014) Statistics 2013. Aesthet Surg J 34(1 suppl):1S–22S
Schwitzer JA, Sher SR, Fan KL, Scott AM, Gamble L, Baker SB (2015) Assessing patient-reported satisfaction with appearance and quality of life following rhinoplasty using the FACE-Q appraisal scales. Plast Reconstr Surg 135(5):830e–837e
ISAPS International Survey on Aesthetic/Cosmetic Procedures Performed in 2014. (2014) International Society of Aesthetic Plastic Surgery. Available from: http://www.isaps.org/Media/Default/global-statistics/2015ISAPS Results.pdf
Gurunluoglu R, Gurunluoglu A, Williams SA, Tebockhorst S (2013) Current trends in breast reconstruction: survey of American Society of Plastic Surgeons 2010. Ann Plastic Surg 70(1):103–110
Zojaji R, Keshavarzmanesh M, Arshadi HR, Mazloum Farsi Baf M, Esmaeelzadeh S (2014) Quality of life in patients who underwent rhinoplasty. Facial Plast Surg 30(5):593–596
Furnham A, Levitas J (2012) Factors that motivate people to undergo cosmetic surgery. Can J Plast Surg 20(4):e47–e50
Sarwer DB, Magee L, Clark V (2003) Physical appearance and cosmetic medical treatments: physiological and socio-cultural influences. J Cosmet Dermatol 2(1):29–39
Schofield M, Hussain R, Loxton D, Miller Z (2002) Psychosocial and health behavioural covariates of cosmetic surgery: Women’s Health Australia Study. J Health Psychol 7(4):445–457
Ozgur F, Tuncali D, Guler Gursu K (1998) Life satisfaction, self-esteem, and body image: a psychosocial evaluation of aesthetic and reconstructive surgery candidates. Aesthetic Plast Surg 22(6):412–419
Alderman A, Chung KC (2013) Measuring outcomes in aesthetic surgery. Clin Plast Surg 40(2):297–304
Ching S, Thoma A, McCabe RE, Antony MM (2003) Measuring outcomes in aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg 111(1):469–480
Edmonds A (2007) ‘The poor have the right to be beautiful’: cosmetic surgery in neoliberal Brazil. J R Anthropol Inst 13(2):363–381
Swami V, Chamorro-Premuzic T, Bridges S, Furnham A (2009) Acceptance of cosmetic surgery: personality and individual difference predictors. Body Image 6(1):7–13
Tsukiura T, Cabeza R (2011) Shared brain activity for aesthetic and moral judgments: implications for the beauty-is-good stereotype. Soc Cogn Affect Neurosci 6(1):138–148
Faria FS, Guthrie E, Bradbury E, Brain AN (1999) Psychosocial outcome and patient satisfaction following breast reduction surgery. Br J Plast Surg 52(6):448–452
Bowling A, Jacobson B, Southgate L (1993) Explorations in consultation of the public and health professionals on priority setting in an inner London health district. Soc Sci Med 37(7):851–857
Margraf J, Meyer AH, Lavallee KL (2013) Well-being from the knife? Psychological effects of aesthetic surgery. Clin Psychol Sci 1(3):239–252
Bulut OC, Wallner F, Plinkert PK, Prochnow S, Kuhnt C, Baumann I (2015) Quality of life after septorhinoplasty measured with the Functional Rhinoplasty Outcome Inventory 17 (FROI-17). Rhinology 53(1):54–58
Kucur C, Kuduban O, Ozturk A, Gozeler MS, Ozbay I, Deveci E, Simsek E, Kaya Z (2016) Psychological evaluation of patients seeking rhinoplasty. Eur J Med 48(2):5–106
Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT (2004) Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg 130(2):157–163
Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT (2004) Development and validation of theNasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg 130(2):157–163
Robinson K, Gatehouse S, Browning GG (1996) Measuring patient benefit from otorhinolaryngological surgery and therapy. Ann Otol Rhinol Laryngol 105(6):415–422
Klassen AF, Cano SJ, East CA, Baker SB, Badia L, Schwitzer JA, Pusic AL (2016) Development and psychometric evaluation of the FACE-Q scales for patients undergoing rhinoplasty. JAMA Facial Plast Surg 18(1):27–35
Naraghi M, Atari M (2016) Development and validation of the expectations of aesthetic rhinoplasty scale. Arch Plast Surg 43(4):365–370
Bensoussan J-C, Bolton MA, Pi S, Powell-Hicks AL, Postolova A, Razani B, Reyes K, IsHak WW (2013) Quality of life before and after cosmetic surgery. CNS Spectr 19(4):282–292
Sarwer DB, Gibbons LM, Magee L, Baker JL, Casas LA, Glat PM, Gold AH, Jewell ML, LaRossa D, Nahai F, Young VL (2005) A prospective, multi-site investigation of patient satisfaction and psychosocial status following cosmetic surgery. Aesthet Surg J 25(3):263–269
Saleh AM, Younes A, Friedman O (2012) Cosmetics and function: quality-of-life changes after rhinoplasty surgery. Laryngoscope 122(2):254–259
Barone M, Cogliandro A, Di Stefano N, Tambone V, Persichetti P (2016) A systematic review of patient-reported outcome measures after rhinoplasty. Eur Arch Otorhinolaryngol 247(4):1807–1811
Group W (1994) Development of the WHOQOL: rationale and current status. Int J Ment Health 23(3):24–56
Orley J, Kuyken W (1994) The development of the World Health Organization Quality of Life Assessment Instrument: preliminary data. Qual Life Res 3(1):53–54
Lavinsky-Wolff M, Camargo HL, Barone CR, Rabaioli L, Wolff FH, Dolci JEL, Polanczyk CA (2013) Effect of turbinate surgery in rhinoseptoplasty on quality-of-life and acoustic rhinometry outcomes: a randomized clinical trial: turbinate surgery in rhinoplasty. Laryngoscope 123(1):82–89
Mohammadshahi M, Pourreza A, Orojlo PH, Mahmoodi M, Akbari F (2014) Rhinoplasty as a medicalized phenomenon: a 25-center survey on quality of life before and after cosmetic rhinoplasty. Aesthetic Plast Surg 38(4):615–619
Fatemi MJ, Rajabi F, Moosavi SJ, Soltani M (2012) Quality of life among Iranian adults before and after rhinoplasty. Aesthetic Plast Surg 36(2):448–452
Kotzampasakis D, Piniara A, Themelis S, Kotzampasakis S, Gabriel E, Maroudias N, Nikolopoulos T (2017) Quality of life of patients who underwent aesthetic rhinoplasty: 100 cases assessed with the Glascow Benefit Inventory. Laryngoscope 127(9):2017–2025
Chauhan N, Warner J, Adamson PA (2010) Adolescent rhinoplasty: challenges and psychosocial and clinical outcomes. Aesthetic Plast Surg 34(4):510–516
Bulut OC, Wallner F, Hohenberger R, Plinkert PK, Baumann I (2017) Quality of life after primary septorhinoplasty in deviated- and non-deviated nose measured with ROE, FROI-17 and SF-36. Rhinology 55(1):75–80
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Mazandaran University of Medical Sciences.
Conflict of interest
Seyed Jaber Mousavi, Jason Abbas Aramideh, Seyedeh Sanam Fattahi, Aminda Amanolahi, and Mohammadhossein Hesamirostami declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Appendices
Appendices
Rights and permissions
About this article
Cite this article
Mousavi, S.J., Aramideh, J.A., Fattahi, S.S. et al. Quality of life before and after rhinoplasty surgery measured with SF-36, RSES, and WHOQOL-BREF. Eur J Plast Surg 41, 535–542 (2018). https://doi.org/10.1007/s00238-018-1392-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-018-1392-5