Abstract
Necrotizing fasciitis is a potentially fatal soft tissue infection characterized by generalized necrosis and gas formation in the subcutaneous tissues and fascia. It is rarely seen in the head and neck area. This report presents the case of a 62-year-old diabetic female patient with generalized cervicofacial necrotizing fasciitis extending to the front chest wall. The cause of the disease was the extraction of the infected second molar tooth. Debridement was performed on the generalized necrotic fascia, subcutaneous tissue, and the skin extending from the preauricular area to the front chest wall and nipples. A series of debridement procedures were necessary because of generalized necrosis. The patient received intensive medical supportive treatment. Following the debridement procedures, the defective area from the neck to the front chest wall was closed up with split-thickness skin graft. Abscessed tooth extraction can lead to cervicofacial necrotizing fasciitis. Necrotizing fasciitis still remains as a potentially fatal disease. Early diagnosis, early radical surgical debridement, and a multidisciplinary approach constitute the significant factors in preventing mortality in such patients.
Level of Evidence: Level V, therapeutic study
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Necrotizing fasciitis (NF), brought about by polymicrobial causes and characterized by generalized necrosis and gas formation along the fascias, is frequently seen in the extremities, abdomen, thorax, perineum, and groin [1, 2]. As the disease advances, necrosis is seen in the skin, subcutaneous tissues, and muscles. The involvement of the head and neck area is rare [2]. If the patient does not receive early aggressive surgical debridement and broad-spectrum antibiotherapy, the disease causes systemic toxicity, multiorgan failure, and eventually mortality. Diabetes mellitus, atherosclerosis, chronic kidney failure, systemic steroid use, hypothyroidism, obesity, alcoholism, cirrhosis, drug abuse, malnutrition, and immunodeficiency pose risks for this disease [3, 4]. In this study, we present a successful treatment case of extensive necrotizing fasciitis of the cervicofacial region involving the anterior chest wall and mammarian tissue and literature review.
Case report
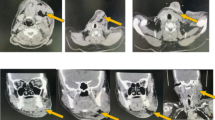
A 62-year-old female patient presented to our clinic with complaints of pain, rash, and open wound on the left side of her face, neck, front chest wall, and nipples. Her lower left second molar tooth had been extracted at a clinic. She had presented with complaints of tooth pain 16 days prior to her presentation at our clinic, and she had also presented infectious diseases to our clinic on day 5 with complaints of pain and rash on her jaw and neck 3 days after the tooth extraction. Although she had received systemic parenteral antibiotherapy for 10 days having been diagnosed with infection at the said clinic, our clinic was consulted because not only she did not show any progress with her complaints but also had spread to her front chest wall and localized necroses on her skin. The patient had diabetes for 15 years and had been using insulin for the regulation of blood sugar, and her physical examination revealed that she had generalized edema, erythema, sensitivity, and temperature rise extending from the left malar and preauricular area to the neck, front chest wall, and both nipples, and localized skin necroses and generalized crepitations at palpation (Fig. 1). The patient’s facial nerve examination revealed zygomatic and frontal branch paralysis. The laboratory results were: leukocyte 17,800 K/μL; CRP, 227 mg/L; albumin 2.1 g/dl; sedimentation 140 mm/h. Broad-spectrum antibiotic (piperacillin-tazobactam) administration was continued. The patient, who was taken into emergency debridement, was seen to have generalized necrosis extending from the left malar area to the nipples in subcutaneous tissues and fascias and received aggressive debridement (Fig. 2). The patient was controlled and followed up closely regarding systemic complications like acute kidney failure, acute respiratory distress syndrome, pneumonia, electrolyte disorders, disseminated intravascular coagulopathy, sepsis, gastrointestinal bleeding, and gastritis which could be caused by the severity and generality of the infection. Since the patient was cachectic and had low levels of protein, she was supported by parenteral and oral nutrition. The patient’s culture results indicated no reproduction. The patient received two more debridement procedures. Wound dressing was made with alginate silver wound dressing. Granulation tissue was formed at the end of 2 weeks having necrotized fascia and subcutaneous tissues completely cleaned up (Fig. 3). Defective areas formed after skin necrosis and debridement were closed up with primary and split-thickness skin graft (STSG) (Fig. 4). The patient was discharged after 26 days with full recovery. No complications like contracture or limitations of the mobility of the neck were seen within her 8-month follow-up period.
Discussion
Necrotizing fasciitis is a significant soft tissue infection characterized by generalized fascia and subcutaneous tissue necrosis caused by aerobic and anaerobic bacteria [5]. Although it is frequently seen in the extremities, the abdomen, and the genital area, it is rarely seen in the head and neck area [2, 6]. Reported literature review studies indicate that the rate of head and neck involvement is between 2.6 and 7.7 % [7, 8].
The actual mechanism in the pathogenesis of the rapidly spreading gangrenous infection in NF has not been clearly defined yet. It has been shown that the secretion of enzymes like hyaluronidase and the proteolytic parts of cell membranes participated in necrosis [9].
The infections of the head and neck area based on teeth problems are polymicrobial. Many bacteria like β-hemolytic streptococcus, staphylococcus, bacteroides, proteus, enterobacter, and pseudomonas can be isolated [10]. Therefore, following the collection of culture samples, broad-spectrum antibiotics should be started, and the treatment should be modified depending on culture antibiogram results. Although culture samples were collected from the case, there was no reproduction. The fact that there was no culture reproduction, it was thought to be based on previous antibiotics administration before presentation at our clinic.
Klabacha et al. classified this inflammatory process anatomically according to the depth of tissues it covers: type I—extending to the epidermis; type II—extending to the dermis; type III—extending to the superficial musculoaponeurotic layer of the face and superficial layer of the deep cervical fascia; type IV—extending to the musculature [11]. Since our patient’s necrosis extended to the muscles, her case is type IV according to this staging. Literature stresses that cervical NF is most frequently seen in patients with immune system deficiencies, and they have one or more enfeebling systemic diseases in more than half of them [7]. The case of our patient, who has diabetes for 15 years, is in line with previous cases in this perspective.
The early diagnosis of this life-threatening disease is very important for the success of treatment. Since the first symptoms of the disease are not specific, patients can be diagnosed with routine tooth infection or it can frequently be confused with acute cellulitis or abscess. However, the existence of a tooth-based infection extending to the neck and front chest wall, abnormal gas formation in the tissues, rapid spread of infection, and orange peel appearance on the skin held should draw attention to NF [4]. Fifty-five to sixty-seven percent of gas collection is formed in the affected tissues [12]. Sometimes, crepitation cannot be obtained because of the edema of the upper tissue. Collected gas is best imaged by computerized tomography (CT). We did not consider imaging with CT because the physical examination of our patient indicated skin crepitations with localized necroses.
Mortality rates for NF between 1924 and 1994 were reported as between 6 and 76 % [7]. In literature review studies conducted between 2003 and 2010, the said rates vary between 4 and 29 % [8]. While mortality is 24 % for patients with additional systemic diseases, it is reported to be 9 % for patients with no disease at all [7]. This rate was found to be between 18 and 22 % for head and neck NF cases [4, 7]. The existence of accompanying diseases like diabetes and alcoholism, delay in surgery, and mediastinitis development account for the most significant clinical factors determining mortality rates. Out of a total of 125 reported cases of tooth-based NF until 1993, 70 were found to have accompanying diseases and 31 of these cases had diabetes [4]. Although bad prognosis criteria (diabetes, delayed surgery, malnutrition) coexist, as with the case of our patient, multidisciplinary approaches prevent mortality.
Baerge et al. reported that 44 % of 59 cases had mediastinum involvement and 34 % of these died [13]. Mediastinum involvement in patients with cervical NF affects prognosis negatively. Our case had no mediastinum involvement.
Airway patency is important in neck NF cases. Edema and necrosis in the neck not only complicate intubation but also require tracheostomy [4]. Although our case had extensive neck involvement, no tracheostomy was needed.
Early aggressive surgical intervention, parenteral antibiotics, and supportive therapy is the most accepted treatment modality for the successful management of NF. Researchers underlined that early debridement was very important and mortality risks increased in the case of delays [6, 7]. Extensive debridement and drainage of necrotic skin, fascia, and muscles constitute the most significant parts of treatment [6]. Not only does the early execution of this procedure control the primary infectious process but also enables the cleansing of necrotic tissues causing toxin production and secondary infections. After debridement, wound dressing was made with alginate silver wound dressing instead of conventional wound dressing. After debridement, wound dressing was made with alginate silver wound dressing instead of conventional wound dressing. Highly absorbent, biodegradable alginate dressings are derived from seaweed. Alginates, which form a gel upon contact, promoting moist interactive healing, are ideal for exudative and infected wounds. Alginate silver wound dressing incorporates the barrier effectiveness of ionic silver with the absorbency capabilities of calcium alginate and polyurethane foam. They contributed to good wound healing rates when compared to the traditional treatment [14].
When healthy granulation tissue is present, reconstruction of the defect must be considered. The reconstructive procedures after debridement are a very important aspect of NF treatment for survivors. If vital structures such as neurovascular structures are not exposed and the granulation tissue is satisfactory, STSG should be carried out. If these vital structures are exposed, and if a dead space occurs after the debridement, coverage with flaps should be considered. The reconstructive method should be planned with regard to the final defect. Wound closure should not be the only aim of the reconstruction; the functional and aesthetic outcomes should also be considered. We did not find any communication between the neck and the oral cavity, and the great vessels in the neck were not exposed. For these reasons, a split-thickness skin graft seemed to be the best option for our patient.
Cervical NF cases also have complications like aspiration pneumonia, airway obstruction, pulmonary abscess, jugular vein thrombosis, meningitis, mediastinitis, front chest wall necrosis, arterial erosion, and mandibular necrosis [6]. While skin necrosis was seen in almost all of the cases, partial facial palsy was reported in 33 % of the cases [15]. Most of the cases reported in literature on the fasciitis area and skin necroses have been in limited areas, cases with extensive skin necrosis, as with the case of our patient, have been rarely reported [16].
Consequently, NF is rarely seen in the head and neck area, and it is potentially fatal. Despite antibiotic therapy, surgical intervention, and multidisciplinary approach, the morbidity and mortality remain high for NF patients. Multidisciplinary approach incorporating early identification and diagnosis, radical debridement, and supportive medical treatment significantly improve survival and reduce the mortality.
References
Aimioni C, Cilione AR, Grandi E, Lombardi L, Merlo R, Pastore A (1999) Cervical necrotizing fasciitis. Eur Arch Otorhinolaryngol 256:510–513
Arifi HM, Duci SB, Zatriqi VK, Ahmeti HR, Ismajli VH et al (2013) A retrospective study of 22 patients with necrotising fasciitis treated at the University Clinical Center of Kosovo (2005–2010). Int Wound J 10:461–465
Lin C, Yeh FL, Lin JT, Ma H, Hwang CH, Shen BH, Fang RH (2001) Necrotizing fasciitis of the head and neck: an analysis of 47 cases. Plast Reconstr Surg 107:1684–1693
Umeda M, Minamikawa T, Komatsubara H, Shibuya Y, Yokoo S, Komori T (2003) Necrotizing fasciitis caused by dental infection: a retrospective analysis of 9 cases and a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 95:283–290
Bahu SJ, Shibuya TY, Meleca RJ, Mathog RH, Yoo GH, Stachler RJ, Tyburski JG (2001) Craniocervical necrotizing fasciitis: an 11-year experience. Otolaryngol Head Neck Surg 125:245–252
Skitarelić N, Mladina R, Morović M, Skitarelić N (2003) Cervical necrotizing fasciitis: sources and outcomes. Infection 31:39–44
Tung-Yiu W, Jehn-Shyun H, Ching-Hung C, Hung-An C (2000) Cervical necrotizing fasciitis of odontogenic origin: a report of 11 cases. J Oral Maxillofac Surg 58:1347–1352
Tunovic E, Gawaziuk J, Bzura T, Embil J, Esmail A, Logsetty S (2012) Necrotizing fasciitis: a six-year experience. J Burn Care Res 33:93–100
Greinwald JH, Wilson JF, Haggerty PG (1995) Peritonsillar abscess: an unlikely cause of necrotizing fasciitis. Ann Otol Rhinol Laryngol 104:133–137
Antunes AA, Avelar RL, de Melo WM, Pereira-Santos D, Frota R (2013) Extensive cervical necrotizing fasciitis of odontogenic origin. J Craniofac Surg 24:e594–e597
Klabacha ME, Stankiewicz JA, Clift SE (1982) Severe soft tissue infection of the face and neck: a classification. Laryngoscope 92:1135–1139
Becker M, Zbären P, Hermans R, Becker CD, Marchal F, Kurt AM et al (1997) Necrotizing fasciitis of the head and neck: role of CT in diagnosis and management. Radiology 202:471–476
Banerjee AR, Murty GE, Moir AA (1996) Cervical necrotizing fasciitis: a distinct clinicopathological entity? J Laryngol Otol 110:81–86
Opasanon S, Muangman P, Namviriyachote N (2010) Clinical effectiveness of alginate silver dressing in outpatient management of partial-thickness burns. Int Wound J 7:467–471
Lanisnik B, Cizmarevic B (2010) Necrotizing fasciitis of the head and neck: 34 cases of a single institution experience. Eur Arch Otorhinolaryngol 267:415–421
Morioka D, Nakatani K, Watanabe S, Shimizu Y et al (1999) Cervical necrotizing fasciitis with upper trunk extension. Eur J Plast Surg 22:264–266
Conflict of interest
None.
Patient consent
The patient gave her informed consent prior to her inclusion in the study. Details that might disclose the identity of the patient were omitted.
Ethical Standards
For this type of study formal consent is not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Özkan, A., Şentürk, S., Topkara, A. et al. Extensive cervicofacial necrotizing fasciitis of odontogenic origin: case report and literature review. Eur J Plast Surg 38, 143–146 (2015). https://doi.org/10.1007/s00238-014-1036-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-014-1036-3