Abstract
Background
With an increase in the incidence of childhood obesity and body awareness among adolescents, there has been a rise in the number of reduction mammaplasties being performed in this group of patients. Our study aims to review the indications, complications, and long-term outcomes of reduction mammaplasty in this subgroup of patients.
Methods
A retrospective review included female patients under 19 years old undergoing reduction mammaplasty. Data was obtained on patient demographics, mechanical and psychological symptoms and postoperative complications. A qualitative prospective questionnaire study was performed between 5 to 13 years following surgery. Responses were rated using the standardized Likert Scaling system to assess subjective benefits of the procedure.
Results
Thirty-six females had unilateral or bilateral reduction mammaplasty at a mean age of 17.40 years. Primary mechanical symptoms included back/neck pain, difficulty sleeping, and intertrigo. The principal psychological complaints were increased self-consciousness, low self-esteem, depression, and bullying. Sixty-seven percent agreed there was an immediate resolution of mechanical symptoms, and 47 % reported an improvement in psychological symptoms following surgery.
Conclusions
Reduction mammaplasty is especially beneficial in this group of patients as they suffer increased psychological comorbidities versus their adult counterparts. Patients need to be adequately assessed and counseled for optimal outcome.Level of Evidence: Level IV, therapeutic study.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Reduction mammaplasty is regarded as the mainstay of treatment in the management of macromastia [1]. This is defined as the massive enlargement of the female breast disproportionate to the growth of the remainder of the body. It mainly occurs in females who are either pubertal or pregnant. In the pubertal and para-pubertal groups, the causes include endocrine changes, childhood obesity, and juvenile (virginal) hypertrophy [2]. The breast often grows to an enormous position rapidly with little chance of spontaneous remission [3].
The number of cases of reduction mammaplasty being performed in adolescents is on the rise. In the past 10 years, there has been a mean of 2 to 5,000 procedures done per year in patients between 13 and 19 years old in the USA. Furthermore, this group accounts for about 2.5 % of all reduction mammaplasties on a yearly basis [4]. This can be attributed to the increasing prevalence of childhood obesity [5], adolescent macromastia, and a lower threshold for surgical intervention.
The development of macromastia in adolescents can be distressing in a very crucial part of a girl’s life. During puberty, a teenager experiences rapid and major changes in appearance and maybe displeased with elements of her new body. It is at this age when body image, peer pressure, and a desire to fit into the norms of society come into play. Adolescents can be psychologically affected due to this condition. Social issues known to occur include inability to attain proper fitting clothes, avoidance of swimming, exercises, and physical activity, and teasing and bullying from peers. This results in a loss of confidence and low self-esteem that can ultimately lead to clinical depression and social isolation.
It is also associated with mechanical symptoms like mastalgia, ulceration, and maceration of the breast folds, postural problems, back and neck pain, shoulder notching, and traction injury to the fourth and fifth intercostal nerves with, in some cases, impairment of nipple sensation [6].
The potential benefits of reduction mammaplasty especially in this subgroup of patients include resolution of physical symptoms, improved quality of life, and emotional stability [7–9].
Despite this, controversy exists when performing bilateral breast reduction in adolescents. This had led to a sense of caution among plastic surgeons. Factors like optimal age to operate, proven benefit, and long-term implications are likely to contribute to this. These include regrowth, need for revision surgery, potential for decreased nipple sensation, and future ability to breastfeed.
Subjective outcome measures would be invaluable in this area; however, the use of validated questionnaires remains a challenge. For example, the Breast-Q, a patient-reported outcome measure, developed and validated for different types of breast surgery, including reduction mammaplasty is only used for patients between the ages of 18 and 34 years of age [10]. Additionally, questionnaire items that deal with sexual behaviors may not be applicable to all members of this age group.
There are a number of studies that report the benefit of bilateral breast reduction in the resolution of both mechanical and psychological symptoms in adults, but there are few studies especially from the European region that investigate the effect of this procedure on adolescents.
The aim of our study is to review the indications, complications, and long-term outcomes of adolescent reduction mammaplasty in our population and compared it with published literature.
Material and methods
A retrospective case-note analysis was conducted between 1997 and 2009 in a regional plastic surgery unit after approval from the clinical effectiveness department. Inclusion criteria included all female patients undergoing unilateral and bilateral reduction mammaplasty for symptomatic macromastia who were less than 19 years old at the time of surgery. Patients that met the inclusion criteria were analyzed for demographics, including body mass index (BMI), smoking, and underlying medical comorbidities. The main indication(s) for surgery were classified into physical and/or psychological presentations and captured from the preoperative clinical consultation.
Preoperative counseling and any formal psychological input were reviewed. The technique, amount of breast tissue removed intraoperatively, postoperative complications, length of hospital stay and follow-up including patient’s satisfaction on discharge from clinic were also assessed. All patients consented to participating in the follow-up survey. A qualitative prospective questionnaire was then conducted on these patients postoperatively. The seven-item survey evaluated immediate and long-term (>1 year postsurgery) resolution of symptoms, improvement in relationships, and patient satisfaction and whether the patients would have surgery again at that age. The responses were rated using the standardized Likert scaling system (1 = strongly disagree to 5 = strongly agree). Cumulative frequencies were calculated for the percentage agreed for each item in the questionnaire. Additional data on episodes of pregnancy, breastfeeding, recurrence of macromastia, and any revision surgery were captured.
No human or animals were used experimentally in this study.
Results
Between 1997 and 2009, 36 patients underwent unilateral or bilateral breast reduction mammaplasty in our institution. Overall mean age at the time of surgery was 17.40 years (range, 14–19 years). Patients had a mean recorded BMI of 22.5 (range, 16–32), 8 % being obese (BMI >30). Six patients were active smokers with a mean of one pack year (range, 0–2). Medical comorbidities included asthma (two patients) and fetal alcohol syndrome (one patient) (Table 1).
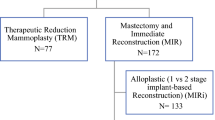
All patients had a mean of two consultations preoperatively before proceeding to surgery (range, 1–2). One or both parents (the mother in single parent cases) were documented to be present at all consultations, i.e., initial, counseling with the specialist nurse and a preoperative consenting clinic. Consent was obtained from the parent or countersigned if the child was less than 16 years of age and Gillick competent. Indications for surgery included both mechanical and psychological presenting complaints. The most frequent mechanical symptoms identified included back/neck pain (27/36), breast pain (4/36), shoulder grooving (3/36), and intertrigo (2/36) (Fig. 1). The most frequent psychological features were found to be increased self-consciousness (10/36), low self-esteem (10/36), depression (7/36), bullying by peers at school (5/36), and relationship difficulties (4/36) (Fig. 2).
A clinical psychologist did not formally assess patients in this cohort; however, all were counseled by a specialist breast reconstruction nurse preoperatively. There were 17 bilateral and 19 unilateral breast reductions. Contralateral mastopexy was performed in combination with a unilateral reduction in 42 % of cases. The functional and psychological presentations of unilateral versus bilateral cases are compared in Table 2. All reductions were performed using a single vascular pedicle (inferior) wise pattern technique by two consultant surgeons (Figs. 3 and 4). Histopathology records revealed no sinister features in any specimens.
The median amount of breast tissue resected was 593 g (range, 190–1,230) and 574 g (range, 135–1,100) for the right and left breasts respectively in bilateral cases. In unilateral cases, the median weight of breast tissue excised was 352.46 g (range, 100–1,300).
Postoperative complications included superficial cellulitis (2/36), infected seroma (1), and hypertrophic scars (3). These were all treated conservatively. The length of hospital stay had a mean of 1.6 days (range, 1–3), and all patients attended a 2-month follow-up clinic appointment following surgery (Table 3). Mean follow-up time from the date of surgery to closure of the study was 7 years (range, 5–13). Of the patients, 94 % (34/36) were documented to be satisfied with the procedure in the last postoperative visit, 8 weeks following surgery.
Qualitative analysis
There was a 67 % response rate in the survey (24/36). We analyzed the questions separately to obtain patient satisfaction rates for various key aspects of their result. The cumulative frequencies for each item are shown in Table 4.
Sixty-seven percent of the patients agreed that they experienced resolution of physical symptoms, which lasted for at least 1-year postoperatively. None of the patients reported significant regrowth, recurrence of symptoms, or revision surgery at the time of the survey, which had a mean of 7 years following surgery.
Forty-six percent of the patients stated a resolution of their psychological problems, which continued at least a year following surgery. Seventy-five percent of the patients agreed that they experienced an improvement in their personal relationships, and 92 % agreed that the surgery overall positively impacted their life. Ninety-six percent of the patients were in agreement that they would still undergo the procedure at the same age. Furthermore just over 50 % of our responders (15) went on to have children and nine were able to successfully breastfeed. There were no reported cases of recurrence of symptoms or episodes of revision breast reduction surgery.
Discussion
Adolescents are more frequently requesting breast reduction surgery. This results from a number of factors, including childhood obesity leading to macromastia and consequent physical and psychological symptoms to peer pressure and media influences, which affects a teenager’s perception of her breasts at a time of heightened vulnerability. Validated subjective outcome measures have been used to demonstrate the substantial negative impact on health-related quality of life, self-esteem, physical symptoms, and eating behaviors in adolescents with macromastia [11].
Preparation for surgery: tips and tricks
The most rewarding outcomes are expected when the adolescent initiates the request, has realistic goals, and has sufficient physical and psychological maturity to undergo the procedure.
In our series, the most common reported psychological disturbance was low self-esteem and increased self-consciousness. Patients reported receiving negative attention from their peers (same and opposite sex), experienced difficulty in sports, e.g., swimming and exercise and were subjected to bullying [12]. This can translate into isolation by peers and poor self-esteem. A significant number of cases were performed for unilateral breast reduction, which additionally had the aim of symmetrization. Our results indicate that psychological comorbidities were the predominant indication for surgery in this particular group of patients compared with their bilateral counterparts (Table 2).
However, despite these features, only patients with a significant psychiatric history, a clinical diagnosis of depression, or those with suicidal ideologies will need a formal psychiatric evaluation before undertaking any surgical procedure [13].
In our series, the psychology department did not formally assess any of our patients, which is in line with most other series in the literature [14]. Nevertheless, all patients were seen and counseled about the procedure by a specialist breast reconstruction nurse. This took place in an additional outpatient appointment whereby the operation, risks, and consequences were discussed with the patients and their parents at length in a relaxed environment. This allowed the patient party to make an informed decision before signing the consent form in a subsequent preoperative clinic.
We found that preoperative counseling is required in this age group as 29 % of patients agreed that they would have benefitted from more contact support prior to the procedure. Clinicians need to ensure that these patients are mentally prepared to undergo a procedure that will result in a change in the appearance of their bodies. This is especially required in patients that undergo unilateral reductions for symmetrization as they may suffer from increased and long-term psychological distress.
Regrowth
Reduction mammaplasty at a young age is associated with the risk of regrowth requiring revision surgery. There is very little data or standard consensus in the literature regarding the age at which to operate. Features like a stable bra and shoe size for 1–2 years may help to identify patients who are still physically developing and may have a higher chance of recurrence. However, this has to be balanced against the benefit of symptom resolution, depending on the severity experienced by the patient.
In our cohort, despite having a younger than average age at the time of operation (16.75 years) compared with published data, we had no reports of regrowth or revision reduction mammaplasty at a mean of 7 years following the procedure. Revision reduction mammaplasty is not without its risks. Death of the nipple areola complex can occur if the initial pedicle is unknown. If the pedicle is known, it should be reused when nipple-areolar complex transposition is planned to maintain perfusion [15]. If it is not known, then the safest option is liposuction reduction or free nipple grafting. Revision reduction mammaplasty therefore is an option in patients that return with regrowth and recurrence of mechanical and psychological symptoms.
Breastfeeding
A review of the literature revealed that there was no difference between patients with reduction mammaplasty and that of the general population in their ability to successfully breast feed. Breast reduction leaves sufficient ductal tissues and neurovascular structures to allow for the successful production of milk [16]. Moreover, there is no association between the pattern of reduction mammaplasty performed and the ability to breastfeed. This supports our finding whereby 13 patients went on to have children and 9 patients were able to successfully breastfeed with 3 patients who chose not as opposed to failed attempts.
Immediate and long-term benefits: resolution of symptoms
Our long-term evaluation highlighted the benefits of reduction mammaplasty in this group of patients. More than 50 % of patients felt an immediate improvement in mechanical symptoms, which was maintained throughout the follow-up period. However, less than 50 % of patients reported resolution of their psychological comorbidities. Other series in the literature have demonstrated the positive impact of reduction mammaplasty in this subgroup of patients. A study by Lee et al. reported 82 % of patients had resolution of their physical symptoms of back, shoulder, and neck pain and 65 % would repeat their adolescent surgical experience [17]. In our series, 94 % of patients were satisfied with their postoperative result and over 90 % of patients agreed that they would undergo the procedure at the same age. Similarly, a 6-year follow-up by Koltz et al. reported overall symptomatic relief and long-term patient satisfaction [18].
It is well known and our data supports the fact that surgery is beneficial to symptom resolution; however, it may not address the additional psychological comorbidities that these patients present with. Access to psychological services should be considered and utilized when needed as these patients may need extra support.
Conclusion
Adolescent macromastia can be a deforming, distressing, and potentially physically disabling condition. Adolescents compared with their adult counterparts display increased social distress and comorbid psychological conditions. Waiting until the growth of breast tissue is halted must be balanced against the symptoms that these patients present with. A thorough assessment should be undertaken to facilitate careful selection of appropriate patients, who understand the procedure, postoperative pathway, risks, and possible complications. There is no evidence to suggest that operating at such a young age results in rapid regrowth of inability to breastfeed later on in life.
We recommend at least two preoperative clinical consultations to assess and counsel patients about the procedure in addition to a detailed consultation with a nurse specializing in breast reconstruction or a child clinical psychologist if deemed necessary.
Furthermore, collection of subjective outcome measures will serve as a guide not only to clinicians but also to policy makers alike to ensure that this service remains a viable option especially in countries with national health budgets.
Reduction mammaplasty when undertaken in this age group has been found to increase the quality of life in this subgroup of patients.
References
Schnur PL, Hoehn JG, Ilstrup DM et al (1991) Reduction mammaplasty: cosmetic or reconstructive procedure? Ann Plast Surg 27(3):232–237
Griffith JR (1989) Virginal breast hypertrophy. J Adolesc Health Care 10(5):423–432
Ship AG (1971) Virginal and gravid mammary gigantism—recurrence after reduction mammaplasty. Br J Plast Surg 24:396–401
The American Society for Aesthetic Plastic Surgery. Statistics fact sheets. 2003–2013. URL: http://www.surgery.org/media/statistics. Accessed 01 July 2013
National Obesity Observatory. NOO data fact sheet—child weight. February 2013. URL: http://www.noo.org.uk/uploads/doc/vid_17926_ChildWeightFactsheetFeb2013.pdf. Accessed 25 June 2014
Dancey A, Khan M, Dawson J et al (2008) Gigantomastia—a classification and review of the literature. J Plast Reconstr Aesthet Surg 61:493–502
Iwuagwu OC, Walker LG, Stanley PW et al (2006) Randomized clinical trial examining psychosocial and quality of life benefits of bilateral breast reduction surgery. Br J Surg 93(3):291–294
Simis KJ, Hovius SE, de Beaufort ID et al (2002) After plastic surgery: adolescent reported appearance ratings and appearance-related burdens in patient and general population groups. Plast Reconstr Surg 109(1):9–17
McGrath MH, Mukerji S (2000) Plastic surgery and the teenage patient. J Pediatr Adolesc Gynecol 13(3):105–118
Pusic A, Klassen AF, Scott AM et al (2009) Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg 124(2):345–353
Cerrato F, Webb ML, Rosen H et al (2012) The impact of macromastia on adolescents: a cross-sectional study. Pediatrics 130(2):e339–e346
Corriveau S, Jacobs JS (1990) Macromastia in adolescents. Clin Plast Surg 17:151–160
DeSilva N (2010) Tips for clinicians: plastic surgery and the adolescent breast: preliminary patient counseling. J Pediatr Adolesc Gynecol 23:184–186
Xue A, Wolfswinkel E, Weathers W et al (2013) Breast reduction in adolescents: indication, timing and a review of the literature. J Pediatr Adolesc Gynecol 26:228–233
Hudson DA, Skoll PJ (1999) Repeat reduction mammaplasty. Plast Reconstr Surg 104(2):401–408
Aillet S, Watier E, Chevrier S et al (2002) Breast feeding after reduction mammaplasty performed during adolescence. Eur J Obstet Gynecol Reprod Biol 101:79–82
Lee MC, Lehman JA Jr, Tantri MD et al (2003) Bilateral reduction mammaplasty in an adolescent population. J Craniofasc Surg 14(5):691–695
Koltz P, Myers R, Shaw R (2011) Adolescent breast reduction: indications. Techniques and outcomes. Plast Reconstr Surg 127(6):158–159
Conflict of interest
None.
Ethical Standards
This study was approved by the local clinical effectiveness committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The manuscript does not contain experimental studies involving humans or animals.
Author information
Authors and Affiliations
Corresponding author
Additional information
This project was presented orally at the BAPRAS/ESPRAS International Meeting, Edinburgh, 7th–11th July 2014.
Rights and permissions
About this article
Cite this article
Sharma, K.S., Lim, P., Baines, R. et al. Reduction mammaplasty in adolescents: a review of the indications, timing, and outcomes in a regional plastic surgery unit. Eur J Plast Surg 37, 661–666 (2014). https://doi.org/10.1007/s00238-014-1020-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-014-1020-y