Abstract
Purpose
Despite evidence for macrostructural alteration in epilepsy patients later in life, little is known about the underlying pathological or compensatory mechanisms at younger ages causing these alterations. The aim of this work was to investigate the impact of pediatric epilepsy on the central nervous system, including gray matter volume, cerebral blood flow, and water diffusion, compared with neurologically normal children.
Methods
Inter-ictal magnetic resonance imaging data was obtained from 30 children with epilepsy ages 1–16 (73% F, 27% M). An atlas-based approach was used to determine values for volume, cerebral blood flow, and apparent diffusion coefficient in the cerebral cortex, hippocampus, thalamus, caudate, putamen, globus pallidus, amygdala, and nucleus accumbens. These values were then compared with previously published values from 100 neurologically normal children using a MANCOVA analysis.
Results
Most brain volumes of children with epilepsy followed a pattern similar to typically developing children, except for significantly larger putamen and amygdala. Cerebral blood flow was also comparable between the groups, except for the putamen, which demonstrated decreased blood flow in children with epilepsy. Diffusion (apparent diffusion coefficient) showed a trend towards higher values in children with epilepsy, with significantly elevated diffusion within the thalamus in children with epilepsy compared with neurologically normal children.
Conclusion
Children with epilepsy show statistically significant differences in volume, diffusion, and cerebral blood flow within their thalamus, putamen, and amygdala, suggesting that epilepsy is associated with structural changes of the central nervous system influencing brain development and potentially leading to poorer neurocognitive outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is a chronic neurological disorder that affects approximately 1% of all children [1, 2]. The type and frequency of seizures can range from mild to severe, with heterogeneous impacts on a child’s life [1, 3]. Specifically, epilepsy can have considerable impact on children across multiple domains, including academic and social challenges [4,5,6]. Individuals with childhood onset epilepsy have been observed to have poorer functional outcomes as adults, including deficits in learning and mental health, when compared with individuals without epilepsy [7]. These findings also include children with uncomplicated epilepsy whose seizures are well controlled on anti-epileptic medication [7].
Childhood is an essential period of significant brain development, in particular the first year of life, during which significant motor and cognitive milestones are achieved and brain volume doubles [8]. As brain development continues, initially synaptic connections are formed at a rapid rate, reflected by an increase in gray matter volume [9] followed by a subsequent increase in white matter volume [10], which continues to increase until approximately age 10. Eventually, unused connections are pruned, with gray matter volumes remaining stable or decreasing from age 10 onwards [11]. Despite the prevalence and impact of epilepsy on pediatric patients, little is known about the effects of epilepsy on the developing brain. However, it is understood from animal models of epilepsy that seizure activity in the developing brain has negative consequences for neural connectivity [12]. Additionally, epilepsy has been shown to affect neurocognitive development, impacting cognitive performance in children [13].
Neuroimaging of children with epilepsy has previously revealed decreased gray and white matter volumes compared with controls, the degree of which has been correlated with cognitive outcomes [13, 14]. Reduced cortical thickness has also been observed in epilepsy syndromes considered to be relatively benign, such as rolandic epilepsy, although the clinical significance is poorly understood [15]. There are also age-specific differences in seizure probability and seizure type based on the stage of brain development, which may influence the long-term consequences of seizures on neuronal structures and behavior in the developing brain [16]. In adults with genetic generalized epilepsies, volume reductions have been noted in the thalamus, putamen, caudate, pallidum, and supplementary motor areas, as well as diffusely across the whole brain [17]. Furthermore, epilepsy has been shown to affect subcortical brain volumes in adults, specifically in the thalamus and hippocampus, as well as reducing cortical gray matter thickness [18]. Interestingly, these changes were observed across multiple types of epilepsy, suggesting that epilepsy may have a “neuroanatomical signature” [18].
Despite the overwhelming evidence for macrostructural alteration in epilepsy patients later in life, evidenced by reduced regional volumes, little is known about the underlying pathological or compensatory mechanisms at younger ages causing these alterations. Previous research investigating microstructural properties in the brain of children with epilepsy is sparse with some evidence for diffusion abnormalities in the hippocampus and thalamus in children with temporal lobe epilepsy [19] as well as diffusion changes in the frontal lobe and putamen in children with juvenile myoclonic epilepsy [20]. Likewise, previous research has not investigated inter-ictal cerebral perfusion in children with epilepsy in detail so far, despite some evidence for altered macrovascular blood flow [21].
Microstructural and cerebral perfusion changes are typically considered to precede macrostructural effects [22, 23] and might, therefore, shed light on the effects of pediatric epilepsy on neurodevelopment manifesting as macrostructural changes later in life. Thus, the aim of this study was to investigate the presence of macro- and microstructural alterations as well as cerebral perfusion changes in the brain of children with epilepsy compared with neurologically normal children. Additionally, we sought to examine similar changes between localization-related epilepsy and generalized epilepsy in subgroup analyses.
Material and methods
Patient identification
Patients treated for epilepsy at the Lucile Packard Children’s Hospital (Stanford, CA) from May 2006 to October 2017 were retrospectively reviewed after approval by the institutional review board (IRB protocol 28,674). All study protocols and procedures were conducted in compliance with the Declaration of Helsinki. As this was a retrospective review, the IRB waived the requirement of informed consent.
Patients were retrospectively identified using ICD-9 and ICD-10 codes containing the terms “epilepsy” or “seizure.” Once identified, all patients had to meet the most recent International League Against Epilepsy (ILAE) criteria for a diagnosis of epilepsy [24]. For ease of evaluation, all patients were classified according to “basic” ILAE criteria as having focal onset epilepsy (with or without alterations in awareness), generalized epilepsy, motor onset epilepsy, or unknown epilepsy.
Following the classification of the epilepsy type, additional inclusion criteria were applied and included: acquisition of arterial spin labeling (ASL) perfusion magnetic resonance imaging (MRI) and diffusion-weighted MRI (DWI) at 3T (standard protocol), and age less than 18 years at the time of neuroimaging. Patients could be on anticonvulsant therapy at the time of imaging although were not required to be. Exclusion criteria included inadequate data or image registration quality, history of prematurity (defined as gestational age < 36 weeks at birth), evidence for underlying cardiac or pulmonary disease, hemorrhage, vascular lesions (aneurysms, AVMs, fistulas, or steno occlusive disease), or prior strokes given their potential impact on cerebral blood flow (CBF) and diffusion. Patients with known cortical malformations or cerebral dysgenesis were excluded from this study and the MRI was read as negative in all cases in the patient group, including any hippocampal signal abnormality or morphologic changes that would indicate the presence of hippocampal sclerosis.
The control group consisted of children without known neurological, neurocognitive, developmental, or behavioral deficits, and had normal-appearing brain on MRI. Children that are part of the control group underwent MR imaging as a standard of care for several reasons, such as syncope, nausea, family history of aneurysm or cancers, scalp nevus, isolated facial lesions, orbital strabismus, cholesteatoma of the ear, isolated headaches, sinus disease or inflammatory nasal obstruction, and familial short stature. This control group population has been previously described in more detail [11].
EEG
Once the patient cohort was identified, EEG findings containing any of the following phrases were collected for review: diffuse slowing, focal slowing, focal amplitude decrease, epileptiform activity, electrographic seizure, frequent seizure, periodic epileptiform discharge, pseudo-periodic epileptiform discharge, stimulus-induced rhythmic periodic ictal or interictal discharge, rhythmic delta, evolving rhythmic discharge, or breach rhythm. All EEGs were reviewed by board-certified pediatric neurologists with fellowship level experience in epilepsy or neurophysiology and certified by the American Board of Clinical Neurophysiology.
MR imaging
MR imaging was performed in all cases using a 3T Discovery 750 scanner (GE Healthcare, Milwaukee, Wisconsin) in all subjects, including the inter-ictal epilepsy and control groups, with an eight-channel head coil. Among others, an ASL MRI and DWI dataset was acquired in all subjects using identical scanning parameters.
Whole-brain ASL datasets were acquired in all cases using the method described by Dai et al. [25] applying a pseudo-continuous labeling period of 1525 ms, 1500 ms post-label delay, 4632 ms repetition time (TR), 10.5 ms echo time (TE), and 111° flip angle with an in-plane resolution of 3.0 × 3.0 mm2 and slice thickness of 4.0 mm. Quantitative CBF datasets were generated based on the acquired ASL datasets using the microsphere methodology described by Buxton et al. [26].
DWI datasets were acquired using TR = 1500 ms, TE = 37 ms, flip angle 90°, FOV = 24 × 24 cm, with an in-plane resolution of 0.94 × 0.94 mm2 and slice thickness of 4.0 mm. Two diffusion weightings of b = 0 s/mm2 and b = 1000 s/mm2 were acquired, with diffusion gradients applied in three directions averaged for the latter. The imaging parameters are described in more detail in Li et al. [27].
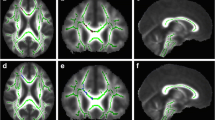
Image processing
Extraction of quantitative volumetric, diffusion, and perfusion measurements was performed using an in-house developed pipeline previously described in Forkert et al. [11]. Briefly described, rigid registration was performed to align the ASL cerebral blood flow and b = 1000 s/mm2 DWI datasets with the corresponding T2-weighted DWI dataset (b = 0 s/mm2). The registered DWI datasets (to correct for potential patient motion) were then used to calculate each individual apparent diffusion coefficient (ADC) map making use of the Stejskal-Tanner equation [28]. In the next step, non-linear registration was used to align the MNI brain atlas [29] with each T2-weighted DWI dataset, which was then used to transform the Harvard-Oxford subcortical atlas brain regions to the patient space according to the non-linear transformation. Two experienced observers (SM, NF) visually checked all registration results to ensure suitable data and registration quality. The registered atlas brain regions were used for volumetric analysis as well as extraction of median ADC and CBF values for each subject within the whole cerebral cortex (gray matter), cerebral hippocampus, thalamus, caudate, putamen, globus pallidus, amygdala, and nucleus accumbens.
Statistical analysis
Quantile local piecewise regression analysis (LOESS) described by Sakov et al [30] was used to generate plots with the age-related 5th, 10th, 25th, 50th, 75th, 90th, and 95th quantile curves extracted from the neurologically normal control group individually for each brain structure and for the three parameters (volume, median ADC, and median CBF) along with the corresponding data points extracted from the children with epilepsy. The plots were generated using the R statistical software package of The R Foundation of Statistical Computing (www.r-project.org, version 3.2.2).
Additionally, multivariate analysis of covariance (MANCOVA) was used for group comparison of the neurologically normal children and pediatric epilepsy patients using the volumetric, median ADC, and median CBF values as dependent variables, age and sex as covariates, and the class (control vs. epilepsy) as the fixed factor. Pairwise comparisons of the dependent variables with Bonferroni correction (n = 24 - volume, ADC, and CBF for the eight structures: cerebral cortex, cerebral hippocampus, thalamus, caudate, putamen, globus pallidus, amygdala, and nucleus accumbens) were performed post hoc to identify significant parameters.
The same MANCOVA setup was used to compare children with localized and generalized epilepsy as well as for a comparison of children with focal EEG signal vs. other epilepsy forms (negative EEG, generalized epilepsy, and multi-focal EEG signs). Pairwise comparisons of the dependent variables with Bonferroni correction (n = 24 variables) were also applied in these cases. No correction for multiple testing across the three models (n = 3) was applied because the second and third MANCOVA analyses were conducted only as an exploratory analysis given the smaller sample sizes. IBM SPSS Statistics (Version 22.0, IBM, Armonk, NY) was used for MANCOVA statistical analyses. A p value < 0.05 was considered significant.
Results
Cohort demographics
Thirty-seven datasets of pediatric patients with epilepsy matching the inclusion criteria were retrospectively identified. Seven patient datasets had to be excluded due to inadequate data or image registration quality. Thus, a total of 30 children with epilepsy (mean age 7.7 years, range 1 to 16 years) and 100 neurologically normal children without epilepsy (mean age 8.2 years, range 0 to 17 years) were included in this study. In the epilepsy group, 73% (n = 22/30) were female and 27% (n = 8/30) were male, and in the control group, 61% (n = 61/100) were female and 39% (n = 39/100) were male. Of the children with epilepsy, 27% (n = 8/30) were diagnosed with generalized epilepsy and 73% (n = 22/30) were diagnosed with focal epilepsy based on EEG findings and clinical history. No patients with motor or unknown types of epilepsy met inclusion criteria in this study. All patients in the epilepsy group were on treatment at the time of imaging, and all patients have been seizure free for > 3 months at the time of imaging although many went on later to experience additional seizures. Further data on inter-ictal EEG, seizure semiology, and neurologic status is compiled in Table 1.
Neuroimaging differences in children with epilepsy vs. neurologically normal children
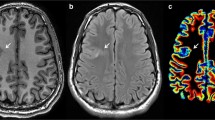
Figure 1 shows the normal distribution plots for three selected brain structures and all three parameters (volume, diffusion, perfusion) generated based on the data from the control group as well as the corresponding data points extracted from the children with epilepsy. A more detailed figure showing the graphs for all parameters and brain regions can be found in the Electronic Supplementary Material.
Overall, the graphs suggest that children with epilepsy have similar brain volumes compared with neurologically normal children. Likewise, the perfusion measurements are similar to those found in the control group. However, the plots indicate slightly reduced cerebral blood flow values in the putamen in children with epilepsy compared with the control children. In contrast to these findings, median ADC values seem to be generally elevated in children with epilepsy in all brain structures analyzed, with the most pronounced differences in the thalamus.
The results of the statistical analysis of the quantitative parameters generally support the qualitative findings based on the plots. More precisely, the MANCOVA analysis using the volume and median ADC and CBF values in the different brain structures analyzed as dependent variables, age and sex as covariates, and the class as a fixed factor revealed a statistically significant difference between children with epilepsy and neurologically normal children (p = 0.001). Pairwise comparisons revealed Bonferroni-corrected significant differences between the groups for the putamen volume (p = 0.037), the amygdala volume (p = 0.045), the median ADC in the thalamus (p < 0.001), and CBF in the putamen (p = 0.027). More precisely, children with epilepsy showed increased sex- and age-adjusted (96.5 months) volumes of the putamen (4.69 ± 0.08 ml vs. 4.48 ± 0.05 ml) and amygdala (1.6 ± 0.03 ml vs. 1.53 ± 0.02 ml) compared with the neurologically normal children. The age-adjusted (96.5 months) mean ADC value in the thalamus with 830.0 × 10−6 mm2/s (standard error ± 3.9 × 10−6 mm2/s) in children with epilepsy was significantly higher compared with 812.7 × 10−6 mm2/s (± 2.2 × 10−6 mm2/s) in the control cohort. With respect to the CBF in the putamen, children with epilepsy were found to have a significantly decreased blood flow compared with the control group (50.0 ± 1.7 vs. 54.3 ± 0.9 mL/100 g/min). None of the other parameters investigated in this study was found to differ significantly between the groups in pairwise comparisons (p > 0.05).
Subgroup analysis: localization-related vs. generalized epilepsy
The MANCOVA analysis using the volume and median ADC and CBF values of the different brain structures analyzed as dependent variables, age and sex as covariates, and the epilepsy type as a fixed factor revealed no statistically significant difference between children with generalized and localized epilepsy (p = 0.162). Despite the small sample size of children with generalized epilepsy (n = 8), pairwise comparisons were performed, even though multivariate statistics did not reveal a significant difference, in order to generate hypotheses for future studies. This pairwise analysis revealed significantly decreased ADC values in the hippocampus (generalized: 915.4 ± 12.6 × 10−6 mm2/s; localized: 956.2 ± 7.6 × 10−6 mm2/s; p = 0.012) in children with generalized epilepsy compared with children with localized epilepsy. No significant differences were found for any other parameter tested.
The MANCOVA analysis using the volume and median ADC and CBF values of the different brain structures analyzed as dependent variables, age and sex as covariates, and the seizure type as a fixed factor also revealed no statistically significant difference (p = 0.053) between pediatric epilepsy patients with focal EEG signal (n = 17) and other epilepsy forms (negative EEG, generalized epilepsy, and multi-focal EEG signs; n = 13). None of the parameters investigated reached statistical significance in subsequent pairwise statistical analysis comparing the two groups.
Discussion
The results of this study suggest that children with epilepsy exhibit inter-ictal macro- and microstructural and cerebral perfusion changes in the thalamus, putamen, and amygdala when compared with children without epilepsy.
The most striking and highly significant finding in this study is the elevated ADC values in the thalamus, which indicates dramatic microstructural changes in this critical area of the brain [31,32,33,34,35]. The thalamus is a central communication hub for normal and abnormal electrical impulses within the brain and is essential in cortical functioning and network relay, and as such, is critical for seizure control [36, 37]. This brain region has been described to be dysfunctional in generalized epilepsy syndromes where generalized spike wave discharges are started in synchrony and is commonly implicated as a pathologic region in childhood absence epilepsies [38,39,40]. However, studies focusing on focal seizures and other types of genetic epilepsies have also found that the thalamus is a key player spreading seizure activity, leading to the secondary generalization of seizures as well as alterations in consciousness during seizure events [41, 42]. The multiple roles of the thalamus in cortical networks and its interface with most areas of the central nervous system might make it especially vulnerable to microstructural changes from excessive activation/excitability. Early and chronic injury to this region is hypothesized to be the initial step in macrostructural changes later in life, as previously described in volumetric studies in adult epilepsy patients [18]. However, it should be noted that altered imaging parameters found could also reflect compensatory effects or an epiphenomenon rather than pathologic findings. The significantly decreased ADC values in the hippocampus in children with generalized epilepsy compared with children with localized epilepsy are also an interesting finding. The hippocampus is known to be an epileptogenic focus, which can become sclerotic with chronic and refractory epilepsy, which further potentiates seizures from this region [18]. Furthermore, this may be interrelated to the patient’s long-term neurocognitive issues later in life [43].
Furthermore, the putamen was not only found to be larger in children with epilepsy compared with controls but also associated with a significantly reduced perfusion. The clinical significance of this finding is unclear although it could suggest early-stage macro- and microstructural changes to this area, which has been noted by others, specifically in juvenile myoclonic epilepsy [20]. Similar to the thalamus, the putamen is a highly interconnected structure involved in the regulation and execution of movement and cognition [44]. This suggests that the putamen may be particularly vulnerable in pediatric patients with epilepsy, and therefore is one of the first brain areas affected by childhood seizures. This is supported by previously described evidence suggesting that the degree of damage in the putamen is correlated with earlier age of onset and longer duration of epilepsy in pediatric patients [20]. The enlarged putamen volume is in agreement with previous research in pediatric patients with new-onset benign epilepsy with centrotemporal spikes [45], which suggested that this hypertrophy might be a result of an adaptive response whereas the exact causality was not discussed. Based on the results of this work, it might be argued that the putamen enlargement and hypoperfusion are associated. However, further research is needed to investigate this relation in more detail.
Interestingly, CBF and diffusion were not significantly different between children with epilepsy and neurologically normal children in other areas of the brain. Together, these data suggest that the thalamus, putamen, and to some extent the hippocampus are particularly affected by seizure activity in the developing brain, potentially due to their diffuse interconnectivity. Within this context, it is also interesting to highlight that these three brain regions together with the precuneus, superior frontal, and superior parietal cortex, which were not analyzed in detail in this work, form the so-called rich club [46]. These brain regions are highly connected and central neocortical hub regions that integrate information from other regions of the brain network and might, therefore, be especially relevant for spreading seizure activity in patients with epilepsy.
Apart from these three “rich club” brain regions, the only other brain region analyzed in this work with a significant difference between children with epilepsy and neurologically normal children was the amygdala, for which a significant enlargement was found in children with epilepsy. The amygdala is a central brain structure related to the experience and perception of fear. Previous electrophysiological studies suggest that the amygdala is also an important seizure source in patients with temporal lobe epilepsy, which might be related to the larger amygdala volumes found [47]. Overall, the finding of increased amygdala volumes is well in line with previous research in adult patients with epilepsy [47, 48].
In contrast to other volumetric studies in adult and pediatric patients with epilepsy, no regional volumetric differences apart from the amygdala and putamen compared with healthy children were found in this study. One potential explanation for this conflicting result is that the pediatric epilepsy cohort studied in this work is younger (average age of 7.7 years) compared with the pediatric patient cohorts used in previous studies (e.g., 10.5 in Lee et al.) [13]. This difference is especially important as the age-related normal data (see Fig. 1) suggest that the brain regions investigated increase in volume until the age of 10. Within this context, the finding of generally increased ADC values in children with epilepsy compared with neurologically normal subjects throughout all brain regions analyzed suggest increased microstructural impairment. Although only hypothetical, children with epilepsy may be accruing microstructural insults over time, which in turn may contribute to the poorer long-term outcomes observed within this population. Thus, it would be of interest to study diffusion changes longitudinally in adults with epilepsy, to investigate if diffusion changes progress with duration of epilepsy as pediatric patients’ age.
When comparing focal and generalized seizures, none of the parameters investigated showed significant differences, including CBF and diffusion. However, there was a trend towards increased diffusion in focal epilepsy, specifically with an increased ADC in the hippocampus, and a tendency towards increased brain volumes and increased CBF measurements in generalized epilepsy compared with children with focal epilepsy. Nevertheless, the sample size for this group comparison was small, preventing any specific conclusions.
There are several limitations to this study. The retrospective nature and relatively small sample size are notable limitations, especially given the heterogeneity of the patient population. As a result of this, there are also only a small number of children with each subtype of epilepsy (focal and generalized) so that the results of these subgroup comparisons should be considered purely exploratory. For this reason, subgroup analysis of focal epilepsy with and without alterations in awareness was not feasible. Additionally, no patients with focal motor seizures or unknown types of epilepsy met our strict inclusion criteria. The retrospective nature of this study might also bias the imaging findings towards patients with more complex genetic epilepsy, for example, because patients selected for MRI might be less likely to show well-characterized electro-clinical syndromes but also less likely to exhibit good seizure control with drug treatment. Patients with seizures related to lesions or other severe pathologies such as arteriovenous malformations were excluded because it would not be possible to differentiate brain alterations related to the primary diseases or associated seizures. It should also be noted that any epilepsy patient group is rather heterogeneous with respect to disease duration, onset age, medication response, epilepsy subtype, etc. Seizure burden in this cohort was assessed subjectively and retrospectively making exact quantifications difficult. Furthermore, seizure burden can fluctuate on a frequent basis, making it less relevant at the time of imaging. The patients included in this study were treated with a variety of anticonvulsant medications. Previous studies suggest that at least some anti-epileptic drugs, such as valproate and lamotrigine, lead to a cerebral blood flow reduction [49, 50] while experiments using animal models have shown that anticonvulsant medications can trigger neuronal apoptosis [51]. Thus, it is possible that the regional brain alterations found are also influenced by treatment with anticonvulsant medication, but it remains speculative if and how the results of the limited previous studies in adults are translatable to children. All children were imaged with a standardized imaging protocol so that intravenous propofol sedation, with or without mask induction using a halogenated anesthetic, was generally used for all children aged 3 months to approximately 6 years. A previous statistical analysis of the children with and without sedation in the overlapping age range of 6 to 9 years in this control group showed no significant differences [11]. Nevertheless, it is possible that anesthesia used during imaging can affect the imaging parameters in children with epilepsy, especially the cerebral blood flow measurement. Given the sample size in this study, it is not possible to correct for all potential covariates. However, the most important findings and trends found in this pediatric epilepsy study are well in line with adult epilepsy patient studies. Another limitation of our study is that there are more girls than boys represented in our experimental sample. The reason for this is not known, but may be related in part to exclusion of children with autism in our study, as autism has a higher prevalence in boys. For this reason, we included sex as a covariate in the statistical analyses and all reported group-wise average results were corrected for age and sex.
Finally, it should be highlighted the T2-weighted DWI datasets (b = 0 s/mm2) were used as the basis for the atlas-based analysis. These datasets exhibit a lower spatial resolution compared with typical high-resolution T1-weighted datasets. This was necessary as high-resolution T1-weighted datasets were not available in all cases. A rigorous quality assessment by two independent observers was performed to ensure optimal registration results. More precisely, every segmented brain region, with a special focus on deep gray matter structures and areas in the frontal cortex, was visually inspected and patients with insufficient results of the atlas-based analysis were excluded from the analysis. As a result of this, no patients younger than 1 year were included in the final study cohort as the atlas-based analysis is more error-prone in very young patients.
Finally, it should be highlighted that due to the single time point MRI analysis used in this cross-sectional study, the observed differences may be pathologic, compensatory, or an epiphenomenon, which will require further prospective studies to investigate in more detail.
Conclusions
Children with epilepsy demonstrate microstructural alterations within their central nervous system, specifically in highly interconnected regions of the brain such as the thalamus and putamen. These brain areas may be particularly affected by seizure activity and are likely most susceptible as an effect of their connectivity to multiple other brain regions. As childhood is a significant time for brain development and maturation, microstructural alterations to these areas may contribute to the developmental challenges experienced by children with epilepsy and play a role in poorer neuro-psycho-social outcomes in adulthood.
References
Guerrini R (2006) Epilepsy in children. Lancet 367:499–524
Hauser WA, Annegers JF, Kurland LT (1993) Incidence of epilepsy and unprovoked seizures in Rochester, Minnesota: 1935-1984. Epilepsia 34:453–468
MacEachern SJ, D'Alfonso S, McDonald RJ et al (2017) Most children with epilepsy experience postictal phenomena, often preventing a return to normal activities of childhood. Pediatr Neurol 72(42–50):e43
Danguecan AN, Smith ML (2017) Academic outcomes in individuals with childhood-onset epilepsy: mediating effects of working memory. J Int Neuropsychol Soc:23(7):594–604
Hamiwka LD, Wirrell EC (2009) Comorbidities in pediatric epilepsy: beyond “just” treating the seizures. J Child Neurol 24:734–742
Ottman R, Lipton RB, Ettinger AB, Cramer JA, Reed ML, Morrison A, Wan GJ (2011) Comorbidities of epilepsy: results from the epilepsy comorbidities and health (EPIC) survey. Epilepsia 52:308–315
Berg AT, Baca CB, Rychlik K et al (2016) Determinants of social outcomes in adults with childhood-onset epilepsy. Pediatrics 137
Gilmore JH, Lin W, Prastawa MW, Looney CB, Vetsa YS, Knickmeyer RC, Evans DD, Smith JK, Hamer RM, Lieberman JA, Gerig G (2007) Regional gray matter growth, sexual dimorphism, and cerebral asymmetry in the neonatal brain. J Neurosci 27:1255–1260
Knickmeyer RC, Gouttard S, Kang C et al (2008) A structural MRI study of human brain development from birth to 2 years. J Neurosci 28:12176–12182
Sampaio RC, Truwit CL (2001) Myelination in the developing human brain. Handbook of developmental cognitive neuroscience:35–44
Forkert ND, Li MD, Lober RM, Yeom KW (2016) Gray matter growth is accompanied by increasing blood flow and decreasing apparent diffusion coefficient during childhood. AJNR Am J Neuroradiol 37:1738–1744
Holmes GL, Ben-Ari Y (2001) The neurobiology and consequences of epilepsy in the developing brain. Pediatr Res 49:320–325
Lee JH, Kim SE, Park CH et al (2015) Gray and white matter volumes and cognitive dysfunction in drug-naive newly diagnosed pediatric epilepsy. Biomed Res Int 2015:923861
O'Muircheartaigh J, Vollmar C, Barker GJ, Kumari V, Symms MR, Thompson P, Duncan JS, Koepp MJ, Richardson MP (2011) Focal structural changes and cognitive dysfunction in juvenile myoclonic epilepsy. Neurology 76:34–40
Overvliet GM, Besseling RM, Jansen JF et al (2013) Early onset of cortical thinning in children with rolandic epilepsy. Neuroimage Clin 2:434–439
Baram TZ (2012) The brain, seizures and epilepsy throughout life: understanding a moving target. Epilepsy Curr 12:7–12
Nuyts S, D'Souza W, Bowden SC, Vogrin SJ (2017) Structural brain abnormalities in genetic generalized epilepsies: a systematic review and meta-analysis. Epilepsia 58:2025–2037
Whelan CD, Altmann A, Botia JA et al (2018) Structural brain abnormalities in the common epilepsies assessed in a worldwide ENIGMA study. Brain 141:391–408
Kimiwada T, Juhasz C, Makki M et al (2006) Hippocampal and thalamic diffusion abnormalities in children with temporal lobe epilepsy. Epilepsia 47:167–175
Keller SS, Ahrens T, Mohammadi S, Möddel G, Kugel H, Ringelstein EB, Deppe M (2011) Microstructural and volumetric abnormalities of the putamen in juvenile myoclonic epilepsy. Epilepsia 52:1715–1724
Nehlig A, Vergnes M, Waydelich R, Hirsch E, Charbonne R, Marescaux C, Seylaz J (1996) Absence seizures induce a decrease in cerebral blood flow: human and animal data. J Cereb Blood Flow Metab 16:147–155
Le Bihan D (2013) Apparent diffusion coefficient and beyond: what diffusion MR imaging can tell us about tissue structure. Radiology 268:318–322
Le Bihan D, Johansen-Berg H (2012) Diffusion MRI at 25: exploring brain tissue structure and function. Neuroimage 61:324–341
Fisher RS, Cross JH, French JA, Higurashi N, Hirsch E, Jansen FE, Lagae L, Moshé SL, Peltola J, Roulet Perez E, Scheffer IE, Zuberi SM (2017) Operational classification of seizure types by the international league against epilepsy: position paper of the ILAE Commission for Classification and Terminology. Epilepsia 58:522–530
Dai W, Garcia D, de Bazelaire C, Alsop DC (2008) Continuous flow-driven inversion for arterial spin labeling using pulsed radio frequency and gradient fields. Magn Reson Med 60:1488–1497
Buxton RB, Frank LR, Wong EC, Siewert B, Warach S, Edelman RR (1998) A general kinetic model for quantitative perfusion imaging with arterial spin labeling. Magn Reson Med 40:383–396
Li MD, Forkert ND, Kundu P et al (2017) Brain perfusion and diffusion abnormalities in children treated for posterior fossa brain tumors. J Pediatr 185:173–180
Stejskal E, Tanner J (1965) Spin diffusion measurements: spin echoes in the presence of a time-dependent field gradient. J Chem Phys 42:288–292
Mazziotta J, Toga A, Evans A et al (2001) A probabilistic atlas and reference system for the human brain: international consortium for brain mapping (ICBM). Philos Trans R Soc Lond Ser B Biol Sci 356:1293–1322
Sakov A, Golani I, Lipkind D et al (2010) High-throughput data analysis in behavior genetics. Ann Appl Stat 4:743–763
Chilla GS, Tan CH, Xu C, Poh CL (2015) Diffusion weighted magnetic resonance imaging and its recent trend-a survey. Quant Imaging Med Surg 5:407–422
Haykin M, Gorman M, van Hoff J et al (2006) Diffusion-weighted MRI correlates of subacute methotrexate-related neurotoxicity. J Neuro-Oncol 76:153–157
Zhang L, Ravdin LD, Relkin N, Zimmerman RD, Jordan B, Lathan WE, Uluğ AM (2003) Increased diffusion in the brain of professional boxers: a preclinical sign of traumatic brain injury? AJNR Am J Neuroradiol 24:52–57
Chappell MH, Ulug AM, Zhang L et al (2006) Distribution of microstructural damage in the brains of professional boxers: a diffusion MRI study. J Magn Reson Imaging 24:537–542
Baliyan V, Das CJ, Sharma R et al (2016) Diffusion weighted imaging: technique and applications. World J Radiol 8:785–798
Sherman SM (2016) Thalamus plays a central role in ongoing cortical functioning. Nat Neurosci 19:533–541
Steriade M, Llinas RR (1988) The functional states of the thalamus and the associated neuronal interplay. Physiol Rev 68:649–742
Timofeev I, Steriade M (2004) Neocortical seizures: initiation, development and cessation. Neuroscience 123:299–336
Blumenfeld H (2005) Cellular and network mechanisms of spike-wave seizures. Epilepsia 46(Suppl 9):21–33
Futatsugi Y, Riviello JJ Jr (1998) Mechanisms of generalized absence epilepsy. Brain and Development 20:75–79
Blumenfeld H (2003) From molecules to networks: cortical/subcortical interactions in the pathophysiology of idiopathic generalized epilepsy. Epilepsia 44(Suppl 2):7–15
Blumenfeld H (2014) What is a seizure network? Long-range network consequences of focal seizures. Adv Exp Med Biol 813:63–70
Nolan MA, Redoblado MA, Lah S, Sabaz M, Lawson JA, Cunningham AM, Bleasel AF, Bye AM (2004) Memory function in childhood epilepsy syndromes. J Paediatr Child Health 40:20–27
Haber SN (2016) Corticostriatal circuitry. Dialogues Clin Neurosci 18:7–21
Lin JJ, Riley JD, Hsu DA, Stafstrom CE, Dabbs K, Becker T, Seidenberg M, Hermann BP (2012) Striatal hypertrophy and its cognitive effects in new-onset benign epilepsy with centrotemporal spikes. Epilepsia 53:677–685
van den Heuvel MP, Sporns O (2011) Rich-club organization of the human connectome. J Neurosci 31:15775–15786
Bower SP, Vogrin SJ, Morris K et al (2003) Amygdala volumetry in “imaging-negative” temporal lobe epilepsy. J Neurol Neurosurg Psychiatry 74:1245–1249
Lv RJ, Sun ZR, Cui T et al (2014) Temporal lobe epilepsy with amygdala enlargement: a subtype of temporal lobe epilepsy. BMC Neurol 14:194
Joo EY, Hong SB, Tae WS, Han SJ, Seo DW, Lee KH, Lee MH (2006) Effect of lamotrigine on cerebral blood flow in patients with idiopathic generalised epilepsy. Eur J Nucl Med Mol Imaging 33:724–729
Gaillard WD, Zeffiro T, Fazilat S, DeCarli C, Theodore WH (1996) Effect of valproate on cerebral metabolism and blood flow: an 18F-2-deoxyglucose and 15O water positron emission tomography study. Epilepsia 37:515–521
Kaushal S, Tamer Z, Opoku F et al (2016) Anticonvulsant drug-induced cell death in the developing white matter of the rodent brain. Epilepsia 57:727–734
Funding
NDF is supported by the Canada Research Chairs program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
MacEachern, S.J., Santoro, J.D., Hahn, K.J. et al. Children with epilepsy demonstrate macro- and microstructural changes in the thalamus, putamen, and amygdala. Neuroradiology 62, 389–397 (2020). https://doi.org/10.1007/s00234-019-02332-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-019-02332-8