Abstract
Purpose
To search for the risk factors closely related to cerebral cavernous malformation associated with developmental venous anomaly (CCM-DVA) lesions rupture, laying foundations for the development of reasonable individual treatment plans for patients.
Methods
In this retrospective study, we collected CCM-DVA patients who met the inclusion criteria in our outpatient department from 2014 to 2017, MRI scans were performed including susceptibility-weighted imaging (SWI) and contrast-enhanced imaging, characteristics and basic clinical information were collected then statistically analyzed, CCM-DVA lesions were divided into 3 types according to the location and quantitative relationship between CCM and DVA.
Results
A total number of 319 adult patients were identified with 41.2±11.9 years on average, though univariate and multivariate regression analysis, ruptured presentations were more common in patients with prior hemorrhage (p=0.003), type III CCM-DVA lesions (p=0.001), lesions volume>1 cm3 (p<0.001), infratentorial lesions especially located in midbrain (p=0.019), pontine (p=0.007), medulla (p=0.015). Caplan-Meier curve shows a lower Hemorrhage-free survival rate on patients with type III CCM-DVA lesions (log-rank, p=0.0222), functional area lesions (log-rank, p<0.001), lesions volume>1 cm3 (log-rank, p<0.001), infratentorial lesions (log-rank, p=0.0002).
Conclusion
The classification based on the relationship between CCM and DVA may be meaningful to predict the risk of lesion rupture and CCM lesions next to DVA distal branches showed a higher risk of rupture.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cerebral cavernous malformation (CCM) is a common cerebral vascular malformation with a prevalence about 0.5% in the population biopsy [1], accounting for about 5–13% of the total number of vascular malformation patients [2]. CCM mostly occurring in supratentorial, recurrent intracranial hemorrhage can be one of its main manifestations. The average hemorrhage rate of unruptured lesions was about 0.4–0.6% per year, and the re-hemorrhage rate of ruptured lesions was significantly increased, about 4.5–22.9% per year [3,4,5,6]. Compared with other forms of cerebrovascular malformations such as arteriovenous malformation (AVM) and CCM, developmental venous anomaly (DVA) has a higher prevalence rate of about 3% [1]. It is considered having a benign natural history, most patients have no obvious clinical symptoms and the hemorrhage rate is as low as 0.22–0.68% per year [7, 8], but when combined with other intracranial vascular malformations such as CCMs, it often speeds up its progression.
CCM associated with DVA (CCM-DVA) is thought to be the most common type of intracranial vascular malformation, which first reported by Roberson in 1974 then classified by McCormick in 1984 [1, 9]. About 8–33% of DVA and CCMs exists in combination [10,11,12,13,14], and CCM-DVA is more common in a sporadic patient than familial cases. Previous studies and analyses on the rupture factors of CCM indicated that female sex [2, 3, 15, 16], young age [17, 18], infratentorial location [17], eloquent location [19], and the presence of a DVA [10, 11, 17, 20,21,22,23] are associated with a higher risk of hemorrhage.
Since a considerable part of CCM was associated with DVA, different positional structural relationships may have different effects on lesion rupture at the hemodynamic level. In prior studies, the combined DVA was more discussed as a potential risk factor for CCM rupture, but there is no large-scale study on the patient population in which CCM and DVA are combined, and few studies have used the relationship as an indicator of hemorrhage occur. Taking these into consideration, we decided to discuss the CCM-DVA relationships including the number and structural characters in adult patients based on risk factors discussed in previous studies, primarily expected to predict the risk of hemorrhage under the premise of covering the most comprehensive influencing factors and provide evidence for future clinical decisions.
We retrospectively reviewed 319 adult patients suffering from CCMs associated with DVAs in our institute, by analyzing the neuroimaging features (ruptured/unruptured, multiplicity, location, lesion volume, CCM-DVA relationship, etc.) and basic characteristics of the patient (gender, age, chief complaint, prior hemorrhage history), mainly to identify risk factors for rupture of CCM-DVAs and lay the foundation for subsequent long-term prognosis and natural history studies.
Material and methods
Patient population
We analyzed 319 consecutive adult CCM-DVA patients’ outpatient records and imaging data admitted to our institution from 2014 to 2017 retrospectively. All patients received MRI examination at 1.5 t or 3.0 t field strength, including T1- and T2-weighted images + susceptibility-weighted imaging (SWI); additional contrast-enhanced T1-weighted images were performed in 243 patients. Among them, 32 patients received surgical treatment because of recurrent symptomatic hemorrhage, progressive aggravation of neurological dysfunction, or epileptic seizure, and the remaining patients received a conservative observation. Patient’s demographic information including age, sex, initial symptoms, prior hemorrhage history, lesions location, and multiplicity were collected. The CCM lesion location was classified as supratentorial and infratentorial. Supratentorial included frontal lobe, temporal lobe, parietal lobe, occipital lobe, insula, corpus callosum, ventricle, basal ganglia, and thalamus. Infratentorial group includes cerebellum, midbrain, pontine, and medulla. CCM lesion volume was calculated from the T2 images of the sagittal, coronal, and axial positions. Al-shahi et al. raised standard published in 2008 were used to evaluate whether the CCM-DVA lesion was ruptured [24]. For patients with multiple CCM lesions confirmed by imaging, only symptomatic lesions/ruptured lesions were selected to include in the study. For asymptomatic and unruptured lesions, the analysis was conducted according to the order of priority from a close relationship with DVA to lesion size.
Diagnostic criteria using MRI
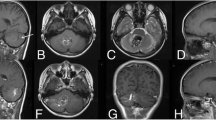
Contrast-enhanced T1-weighted images (T1WI) have long been used as the gold standard for diagnosing CCM-DVAs. With the application of SWI sequence, a non-invasive neuroimaging tool to identify DVA, the higher sensitivity to identify microhemorrhage of CCM lesions is gradually valued [25]. The main advantage of SWI is that it can detect the presence of microbleeds more sensitively and small CCM lesions could be visualized directly; this is especially important for finding and observing DVA-related CCM lesions because the associated recurrent microhemorrhage are considered to be the beginning stage of CCM formation [26, 27]. Therefore, an MRI examination with a contrast-enhanced T1WI + SWI sequence were used in our study to provide the greatest extent diagnosis of existing lesions and a clear relationship between CCM lesions and DVA. (Fig. 1).
Patient with multiple CCM-DVA, right cerebellar cavernous malformation has the closest relationship with DVA. DVA can not be recognized on T2WI (c), but can be clearly identified in SWI (b) and T1-enhanced images (a), multiple microhemorrhages at DVA distal branches can be seen by SWI scan and CCMs were highly suspected, which cannot found in enhanced images
Depending on types, DVA can be expressed in a variety of forms on MRI: the most common feature is the stellate or linear abnormal vein that can be discerned on the contrast-enhanced T1WI and/or SWI sequence, which merges into the central vein and flows into the cortical vein or deep.
According to different Zabramski types, CCM also presents different imaging features. The most classical features are sponge-like structures, and the central area on T2-weighted images is the mixed signal, surrounded by low-signal hemosiderin deposition area, namely, “popcorn” sign. Traces of bleeding at different stages can be seen within the contour of the lesion and related hemorrhages can be more sensitively observed in the SWI sequence.
In addition, before the diagnosis of CCM, imaging features and previous medical history characteristics should be used to identify and exclude the diagnosis of similar intracranial space-occupying lesions/hemorrhagic lesions such as AVM and tumor stroke hemorrhage by enhanced scanning when necessary.
Image analysis
All patients’ image data were gathered in picture archiving and communication systems (PACS) and evaluated by experienced neuroradiologist. The lesions were divided into ruptured/unruptured group according to the characteristics of the lesions presents on MRI images, and the lesions location, number, and maximum diameter of each axis were determined then calculated by volume formula.
Supratentorial deep location refers to CCM located around thalamus, basal ganglia. Location was divided into two groups: supratentorial and infratentorial. Zabramski scale were used for the imaging classification of CCM, and the classification of the hematoma outside the lesion was classified separately and ranked as the third group; however, since the CCM classification based on Zabramski and the exlesional hemorrhage had an obvious direction for the lesions hemorrhage, it was not included in the major discussion affecting the lesions rupture.
CCM-DVAs relationship was valued using contrast-enhanced T1-weighted images and SWI sequences and was classified into three types according to the structural position and quantity relationship between CCM and DVA:
Type I: CCM associated with a single abnormally thickened and distort venous drainage.
Type II: CCM located in the trunk of the DVA with multiple abnormal vein drainage surrounded.
Type III: Typical DVA of the caput medusa-like appearance especially on the SWI/T1-enhanced images, CCM located around the distal radical branch of DVA. (Fig. 2)
Different CCM-DVA relationship classification. a (Type I) CCM located in occipital lobe with a single drainage vein to the cortex. b, c (Type II) CCM located in the DVA trunk, surrounded by multiple veins drainage. d (Type III): DVA composed of multiple tortuous draining veins that eventually converge into a collecting vein, CCM is located at the turning point of the DVA distal branch, and multiple drainage veins eventually merge into the collecting vein
Statistical analysis
Statistical analysis was performed using the IBM SPSS version 22.0; univariate analysis using X2 test (Fisher’s exact test when necessary) and independent t tests were used in continuous data, then multivariate analysis confirming the independent risk factors using logistic regression and confirmed by Cox regression. We determined that the CCM-DVA lesion was congenital; Kaplan-Meier curve was drawn to evaluate the relationship between certain risk factors and Hemorrhage-free survival with years. Continuous variables are presented as the mean ± SD, p values less than 0.05 were considered statistically significant.
Result
Demographics of CCMs associated with DVAs
A total number of 319 patients with CCM-DVA were enrolled, with an average age of 41.2±11.9 years (range 18–77 years), of which 176 (55%) were female patients. Eighty-four patients had a prior hemorrhage history (84/319.26%), chief complaint of patients including symptomatic hemorrhage (n=148, 46%), epileptic seizure (n=48, 15%), non-hemorrhage headache/dizziness (n=50, 15%), neurologic deficit (n=54, 17%), and asymptomatic (n=19, 6%). Among them, there were 78 patients with multiple CCMs (n=78, 24%) and 161 patients with infratentorial lesions (n=161, 50%). One hundred ninety-nine patients had lesions adjacent to the eloquent area (n=199, 62%); the lesions diameter measured using T2WI, SWI, and T1-enhanced scan were 15.64±8.56 mm, 18.43±8.27 mm, and 15.53±8.26 mm. The relationship between CCM and DVA is most seen in type III (n=230, 72%), and more detailed demographics are described in Table 1.
We assume that all CCM-DVA lesions are present at birth, there were totally 13,143 patient-years of follow-up of 319 patients (41.2 years average); 140 patients who had 197 ruptured lesions were included, among them, 53 patients had a prior hemorrhage history; the estimated first time hemorrhaging rate was about 0.93% per patient-years.
Risk factors for hemorrhage
Tables 2, 3, and 4 list the following possible hemorrhage-related factors: gender, age, multiple lesions, infratentorial lesions, eloquent lesions, and the diameter of the lesion as well as the type of CCM-DVA. Through univariate analysis and then multivariable analysis, patients with prior hemorrhage history shows a significant higher rupture risk than those ruptured lesions first discovered (p=0.003 [OR] 2.5, [HR] 2.3), which presents more significant in infratentorial lesions (p=0.002, [OR] 4.0) but no differences was found in supratentorial lesions. Compared to CCM-DVA lesions type I and II, type III has a significant higher rupture rate (p=0.001 [OR] 2.8; p=0.026 [HR] 1.6), which was effective for both supratentorial and infratentorial lesions. Besides, CCM lesion volume>1 cm3 (p<0.001 [OR] 3.3, [HR] 2.2) were presented to be the independent risk factor of CCM-DVA lesions hemorrhage. On the other hand, female sex, multiple lesions, functional zone, and left side lesion did not show any differences between ruptured/unruptured lesions.
To further explore the factors associated with lesion bleeding, we conducted a subgroup discussion and analysis of several significant factors as followed:
CCM-DVA lesion types
There was a significant difference between the rupture probabilities of the three CCM-DVA types. Type I and type II lesions had a similar rupture rate, while type III lesions harbor a higher rupture risk (p=0.001 [OR 2.8], p=0.026 [HR 1.6]) (Table 2), which is significant for both supratentorial (p=0.031, [OR 2.8]) and infratentorial (p=0.009, [OR 3.0]); furthermore, a shortened hemorrhage-free survival time was found in type III lesions than the other two types (Fig. 3a).
Functional zone
Unfortunately, the statistical results do not reflect the inevitable risk relationship between the functional area and the lesion rupture. Although lesions located in non-functional areas are more likely to achieve longer hemorrhage-free survival (p=0.002, [HR 1.9], Table 2) (log-rank, p<0.001, Fig. 3b), statistical results are insufficient to support their prediction of lesions rupture.
Size of the lesion
In general, ruptured lesions tend to have a relatively large volume, the volume>1 cm3 was closely related to lesions rupture (p<0.001, [OR 3.3] [HR 2.2]), and a larger lesion volume are associated with a shortened hemorrhage-free survival time (log-rank, p<0.001) (Fig. 3c), this conclusion is still valid when it is divided into separate discussions: supratentorial and infratentorial (Tables 3 and 4).
Infratentorial locations
From the statistical data of 319 consecutive patients, the incidence of infratentorial CCM-DVA was basically the same as that supratentorial, but the infratentorial lesions had a significantly higher rupture ratio (p<0.001; OR 3.1). The Kaplan-Meier curve also shows a higher hemorrhage tendency of infratentorial lesions (p=0.0002, Fig. 3d) Specific to each zone, the patients number of pontine lesions was the highest, so does the probability of lesion rupture (58/95, 61%). In addition, we found it that midbrain lesions (p=0.019), pontine lesions (p=0.007), and medulla lesions (p=0.015) were more likely to present with symptomatic hemorrhage (Table 5).
Discussion
DVA is one of the most common cerebrovascular malformations in the brain. It is thought to be formed during embryonic development [28, 29]; however, CCM-DVA is thought to be acquired and developed. The latest study by Waleed et al. found that the incidence of CCM-DVA increased with age [30]. Meng et al. found that the prevalence of CCM in DVA patients was significantly higher than that in the normal population (11.1% vs 2.3%) [12]. In addition, several studies suggested that CCM with DVA had higher annual hemorrhage rate which is inseparable from the formation mechanism [31, 32]: DVA is thought to be more likely to be a congenital vascular malformation that precedes cavernous vascular malformations. A number of pathological studies suggest that it is abnormally dilated venous plexus interspersed with normal insular brain tissue without arterial or arteriovenous short circuit, the area lacks normal draining veins. For the presence of DVA, changes in hemodynamics resulted in increased venous pressure, vascular torsion, and deformation with times, local thrombosis formed, and vascular lumens were further damaged and stenosis, which affected DVA angioarchitecture, leading to microbleeding and angiogenic proliferation. New blood vessels were less stable and therefore more prone to microhemorrhage, forming a cavernous structure with clustered vascular masses and accompanied by bleeding from different periods [13, 33, 34].
Previous studies have generally agreed that CCM-DVA have a higher rupture risk than those with CCM alone, and that infratentorial lesion is an important risk factor for predicting the bleeding of the lesion, natural history reported that the annual bleeding rate of unruptured CCM around the brain stem was about 2.3–8.7% [35,36,37,38], significantly higher than that of supratentorial lesions. However, it is still unclear whether the hemorrhage event of CCM-DVA is related to the infratentorial location. According to our results, the supratentorial lesions did not present any high incidence but with a lower rupture risk than infratentorial lesions, although some multiple lesions may have been neglected. The reasons may vary. First of all, the distribution of infratentorial functional areas are relatively concentrated and the distribution of drainage veins are dense, any enlargement of the lesion caused by a small amount of bleeding may lead to a sudden neurological dysfunction due to the occupying effect, a same bleeding event may remain asymptomatic at supratentorial or may appear as a headache without detection. In addition, the presence of more complex venous components may keep the CCM lesion in a relatively active state for a long time, further exacerbating the progression of bleeding events.
Prior hemorrhage history has been recognized by many studies as one of the most important reasons leading to the rupture of CCM lesions [4, 5, 15, 24]. As mentioned earlier, the combination of DVA is also recognized by most researchers as one of the risk factors that increase the hemorrhaging rate of CCM lesions; however, for CCM lesion associated with DVA, there is still no definite conclusion whether the history of prior hemorrhage has an effect on the progression of the lesion. From our statistical result, for patients with infratentorial CCM-DVA lesion, previous hemorrhaging will probably increase the risk of lesion rupture.
Measures of lesion size vary from study to study, and there is no uniform answer whether lesion size is a predictor of rupture [17, 38, 39]. Recently, Sepide et al. found that >1 cm3 was significant in predicting supratentorial lesions rupture, while it was not significant in supratentorial lesions [17]. Similarly, lesion volume>1 cm3 is also an important focal rupture predictor for ruptured lesions in our study, the CCM-DVA lesions volume was larger than unruptured lesions with statistical significance (p<0.001), which effective for both supratentorial and infratentorial lesions.
In previous studies, CCM-DVA was not clearly classified. Ruiz et al. classified it into three types according to the characteristics of DVA in different stages of DSA [40]. Unfortunately, except for a small number of inpatients, most of our subjects did not have the appropriate opportunity to have DSA examination. In addition, the more authoritative CCM classification proposed by Zabramski is only used to describe the statistical data and is not applied to the final risk factor analysis in this study, mainly considering that this classification has a clear tendency for hemorrhage events. The classification methods of CCM-DVAs have been debated differently in previous studies mainly according to the anatomical structure relationship of CCM-DVA and hemodynamics of venous drainage [41, 42]. Hong YJ et al. considered the occurrence of CCM-DVA may be related to anatomical angioarchitectural factors such as stenosis of DVA lumen and degree of vascular tortuosity [43].
Considering these factors, we divided CCM-DVA lesions into three types to evaluate the influence on hemorrhage through careful observation and induction of MRI imaging data of the technicians. From the statistic results, we considered that CCM lesions located around the distal radical branch of typical DVA will possess a relatively high probability of rupture (type III) than CCM associated with single abnormally venous drainage (type I) and CCM located in the trunk of the DVA with multiple abnormal vein drainage surrounded (type II).
As the most common type of CCM-DVAs, DVA-related CCM lesion is often prone to appear in the excessive vascular distortion zone, which is often small distal branches with a poor tolerance to blood flow, as shown in Figs. 1 and 2d. We think it’s mostly due to the special structure of these lesions which have a significant pressure changes and irregular blood flow will consistently impact venous pressure during the running, combined with the high venous pressure existing in DVA itself. Under such unstable hemodynamic conditions, CCM structure developed from abnormal drainage vein lacks integrity and is more prone to rupture.
Limitations
This study is limited to the study and analysis of the patient’s imaging features. It is difficult to completely determine the existence and exact relationship of CCM venous drainage during the screening process. The patients in the group are all clearly defined in the venous drainage component. Some patients will be missed during the statistical process which makes it difficult to carry out statistics on the exact incidence rate. Besides, with 3T MRI, some small DVA cannot be clearly identified and the relationship with CCM cannot be determined; a higher MRI field strengths MRI may improve accuracy to some extent.
Conclusion
CCM combined with DVA is a common form of intracranial vascular malformation; infratentorial lesions with prior hemorrhage history, brainstem lesions, lesion volume>1 cm3, type III lesion are closely related to the rupture of CCM-DVA lesions.
The discovery of these risk factors will provide a basis for subsequent treatment strategies and surgical indications and it is necessary to conduct long-term follow-up of patients to observe disease progression and conduct more research on their natural history.
References
McCormick WF (1984) Pathology of vascular malformations of the brain. In: Wilson CB, Stein BM (eds) Intracranial arteriovenous malformations. Williams & Wilkins, Baltimore, pp 44–63
Robinson JR, Awad IA, Little JR (1991) Natural history of the cavernous angioma. J Neurosurg 75(5):709–714
Salman AS, Hall JM, Horne MA et al (2012) Untreated clinical course of cerebral cavernous malformations: a prospective, population-based cohort study. Lancet Neurol 11(3):217–224
Flemming KD, Link MJ, Christianson TJH, Brown RD (2012) Prospective hemorrhage risk of intracerebral cavernous malformations. Neurology 78(9):632–636
Gross BA, Du R (2016) Hemorrhage from cerebral cavernous malformations: a systematic pooled analysis. J Neurosurg 126(4):1
Kondziolka D, Lunsford LD, Kestle JRW (1995) The natural history of cerebral cavernous malformations. J Neurosurg 83(5):820–824
Garner TB, Curling OD, Kelly DL, Laster DW (1991) The natural history of intracranial venous angiomas. J Neurosurg 75(5):715–722
Mclaughlin MR, Kondziolka D, Flickinger JC et al (1998) The prospective natural history of cerebral venous malformations. Neurosurgery 43(2):195–200
Roberson G (1974) Telangiectases and cavernous angiomas of the brainstem : “cryptic” vascular malformations. Neuroradiology 8:83–89
Clatterbuck RE, Rigamonti D (1999) A comparison of the clinical profile of cavernous malformations with and without associated venous malformations. Neurosurgery 44(1):46–47
Wurm G, Schnizer M, Nussbaumer K, Wies W, Holl K (2003) Recurrent cryptic vascular malformation associated with a developmental venous anomaly. Br J Neurosurg 17(2):188–195
Meng G, Bai C, Yu T, Wu Z, Liu X, Zhang J, zhao J (2014) The association between cerebral developmental venous anomaly and concomitant cavernous malformation: an observational study using magnetic resonance imaging. BMC Neurol 14(1):50
Perrini P, Lanzino G (2006) The association of venous developmental anomalies and cavernous malformations: pathophysiological, diagnostic, and surgical considerations. Neurosurg Focus 21(1):1–4
Ostertun B, Solymosi L (1993) Magnetic resonance angiography of cerebral developmental venous anomalies: its role in differential diagnosis. Neuroradiology 35(2):97–104
Aiba T, Tanaka R, Koike T, Kameyama S, Takeda N, Komata T (1995) Natural history of intracranial cavernous malformations. J Neurosurg 83(1):56–59
Moriarity JL, Wetzel M, Clatterbuck RE et al (1999) The natural history of cavernous malformations: a prospective study of 68 patients. Neurosurgery 44(6):1166–1173
Kashefiolasl S, Bruder M, Brawanski N, Herrmann E, Seifert V, Tritt S, Konczalla J (2018) A benchmark approach to hemorrhage risk management of cavernous malformations. Neurology 90:e856–e863
Barker FG, Amin-Hanjani S, Butler WE et al (2001) Temporal clustering of hemorrhages from untreated cavernous malformations of the central nervous system. Neurosurgery 49(1):15–25
Bertalanffy H (2002) Cerebral cavernomas in adult, review of the literature and analysis of 72 surgically treated patients. Neurosurg Rev 25:1–53
Marasco R, Spagnoli M, Leonardi M (2009) Association between developmental venous anomalies and cavernous angiomas: a retrospective MR study. Neuroradiol J 22(2):179–185
Kamezawa T, Hamada JI, Niiro M, Kai Y, Ishimaru K, Kuratsu JI (2005) Clinical implications of associated venous drainage in patients with cavernous malformation. J Neurosurg 102(1):24–28
Wurm G, Schnizer M, Fellner FA (2007) Cerebral cavernous malformations associated with venous anomalies. Neurosurgery 61(Supplement):SHC-390–SHC-406
Gross BA, Lin N, Du R et al (2011) The natural history of intracranial cavernous malformations. Neurosurg Focus 30(6):E24
Salman AS, Berg MJ, Morrison L et al (2008) Hemorrhage from cavernous malformations of the brain definition and reporting standards. Stroke 39(12):3222–3230
Young A, Poretti A, Bosemani T, Goel R, Huisman TAGM (2017) Sensitivity of susceptibility-weighted imaging in detecting developmental venous anomalies and associated cavernomas and microhemorrhages in children. Neuroradiology 59:797–802
Campeau NG, Lane JI (2005) De novo development of a lesion with the appearance of a cavernous malformation adjacent to an existing developmental venous anomaly. Am J Neuroradiol 26(1):156–159
Cakirer S (2003) De novo formation of a cavernous malformation of the brain in the presence of a developmental venous anomaly. Clin Radiol 58(3):0–256
Pereira VM, Geibprasert S, Krings T, Aurboonyawat T, Ozanne A, Toulgoat F, Pongpech S, Lasjaunias PL (2008) Pathomechanisms of symptomatic developmental venous anomalies. Stroke 39:3201–3215
Saito Y, Kobayashi N (1981) Cerebral venous angiomas: clinical evaluation and possible etiology. Radiology 139(1):87–94
Brinjikji W, Elmasri ER, Wald JT et al (2017) Prevalence of cerebral cavernous malformations associated with developmental venous anomalies increases with age. Childs Nerv Syst 33(9):1539–1543
Roccatagliata L, René van den Berg, Soderman M et al (2012) Developmental venous anomalies with capillary stain: a subgroup of symptomatic DVAs? Neuroradiology 54:475–480
Gross BA, Du R (2015) Cerebral cavernous malformations:natural history and clinical management. Expert Rev Neurother 15(7):771–777
Awad IA, Robinson JR, Mohanty S et al (1993) Mixed vascular malformations of the brain: clinical and pathogenetic considerations. Neurosurgery 33(2):179-88; discussion 188
Sharma A, Zipfel GJ, Hildebolt C, Derdeyn CP (2013) Hemodynamic effects of developmental venous anomalies with and without cavernous malformations. Am J Neuroradiol 34(9):1746–1751
Porter PJ, Willinsky RA, Harper W, Wallace MC (1997) Cerebral cavernous malformations: natural history and prognosis after clinical deterioration with or without hemorrhage. J Neurosurg 87(2):190–197
Petr O, Lanzino G (2015) Brainstem cavernous malformations. J Neurosurg Sci 59(3):271
Kupersmith MJ, Kalish H, Epstein F et al (2001) Natural history of brainstem cavernous malformations. Neurosurgery 49(4):1023–1024
Li D, Hao SY, Jia GJ, Wu Z, Zhang LW, Zhang JT (2014) Hemorrhage risks and functional outcomes of untreated brainstem cavernous malformations. J Neurosurg 121(1):32–41
Jeon JS, Kim JE, Chung YS, Oh S, Ahn JH, Cho WS, Son YJ, Bang JS, Kang HS, Sohn CH, Oh CW (2014) A risk factor analysis of prospective symptomatic haemorrhage in adult patients with cerebral cavernous malformation. J Neurol Neurosurg Psychiatry 85(12):1366–1370
Ruíz DS, Yilmaz H, Gailloud P (2010) Cerebral developmental venous anomalies: current concepts. Ann Neurol 66(3):271–283
Zhang P, Liu L, Cao Y, Wang S, Zhao J (2013) Cerebellar cavernous malformations with and without associated developmental venous anomalies. BMC Neurol 13(1):134–134
Im SH, Han MH, Kwon BJ, Ahn JY, Jung C, Park SH, Oh CW, Han DH (2008) Venous-predominant parenchymal arteriovenous malformation: a rare subtype with a venous drainage pattern mimicking developmental venous anomaly. J Neurosurg 108(6):1142–1147
Hong YJ, Chung TS, Suh SH, Park CH, Tomar G, Seo KD, Kim KS, Park IK (2010) The angioarchitectural factors of the cerebral developmental venous anomaly; can they be the causes of concurrent sporadic cavernous malformation? Neuroradiology 52(10):883–891
Funding
This study was funded by the National Natural Science Foundation of China (81371292) and the National Natural Science Foundation of China (H0906 81801140).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, S., Ma, L., Wu, C. et al. A rupture risk analysis of cerebral cavernous malformation associated with developmental venous anomaly using susceptibility-weighted imaging. Neuroradiology 62, 39–47 (2020). https://doi.org/10.1007/s00234-019-02274-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-019-02274-1