Abstract
Introduction
The aim of this study was to analyze brain functional connectivity and its relationship to cognition in patients with mild traumatic brain injury (mTBI).
Methods
Twenty-five patients with mTBI and 25 healthy control subjects were studied using resting-state functional MRI (rs-fMRI). Amplitudes of low-frequency fluctuations (ALFFs) and functional connectivity (FC) were calculated and correlated with cognition.
Results
Compared with the normal control group, the mTBI patients showed a significant decrease in working memory index (WMI) and processing speed index (PSI), as well as significantly decreased ALFFs in the cingulate gyrus, the middle frontal gyrus and superior frontal gyrus. In contrast, the mTBI patients’ ALFFs in the left middle occipital gyrus, the left precuneus, and lingual gyrus increased. Additionally, FC significantly decreased in the thalamus, caudate nucleus, and right hippocampus in the mTBI patients. Statistical analysis further showed a significant positive correlation between the ALFF in the cingulate gyrus and the WMI (R 2 = 0.423, P < 0.05) and a significant positive correlation between the FC in the left thalamus and left middle frontal gyrus and the WMI (R 2 = 0.381, P < 0.05).
Conclusion
rs-fMRI can reveal the functional state of the brain in patients with mTBI. This finding differed from observations of the normal control group and was significantly associated with clinical cognitive dysfunction. Therefore, rs-fMRI offers an objective imaging modality for treatment planning and prognosis assessment in patients with mTBI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As the traffic and construction industries have expanded, there has been a gradual yearly increase in traumatic brain injury (TBI), especially mild traumatic brain injury (mTBI) [1]. mTBI presents with only minor clinical symptoms and is easily ignored by conventional imaging modalities, which typically produce negative results; therefore, difficulties arise regarding follow-up treatment and forensic identification [2, 3]. Approximately 30 % of all mTBI patients experience some degree of residual neurologic or cognitive deficit [4]. The cognitive domains of memory, executive function, and processing speed are commonly affected [5, 6]. The underlying pathophysiology of these cognitive impairments remains poorly understood. To provide accurate and comprehensive information to facilitate the clinical diagnosis and treatment of mTBI, thereby improving its prognosis, it is necessary to thoroughly delineate the pathogenic mechanisms underlying mTBI. To accomplish this, the use of novel functional imaging methods provides an attractive option.
Task-based blood-oxygen-level-dependent functional magnetic resonance imaging (BOLD-fMRI) can be used to determine whether a given region of the brain is active based on its oxygen consumption, with high levels of oxygen consumption corresponding to increased neuronal activity. In recent years, resting-state fMRI (rs-fMRI) technology has become increasingly used to study brain function. rs-fMRI can accurately identify signals in various brain regions that spontaneously arise because of self-regulation within the brain rather than in response to external stimulation [7–11]. In 1995, Biswal et al. [7] reported that activity within the motor area of the bilateral brain was highly synchronized under resting-state conditions, producing a signal characterized by low-frequency fluctuations (LFFs). Subsequent studies have proposed and confirmed the existence of a default network under resting-state conditions [12], thus popularizing the use of rs-fMRI technology. One significant advantage of rs-fMRI technology is its simple design, which places few requirements on subjects and thus offers a convenient means of collecting data. Johnson et al. [10] used rs-fMRI to evaluate the default mode network (DMN) present in the subacute phase of mTBI. The resting-state DMN showed reductions in the number and strength of connections in the posterior cingulate and lateral parietal cortices; however, an increase in these parameters was noted in the medial prefrontal cortex. Mayer et al. [11] found that patients with mTBI exhibited decreased functional connectivity (FC) within the DMN and hyper-connectivity between the DMN and the lateral prefrontal cortex. Measures of FC exhibited high levels of sensitivity and specificity for patient classification and predicted cognitive complaints during the semi-acute injury stage. Zang et al. [13] found that patients with attention deficit hyperactivity disorder (ADHD) showed decreased amplitudes of low-frequency fluctuations (ALFFs) in the right inferior frontal cortex, left sensorimotor cortex, bilateral cerebellum, and vermis and increased ALFFs in the right anterior cingulate cortex, left sensorimotor cortex, and bilateral brainstem. This finding suggests that changes in spontaneous neuronal activity in these regions may be implicated in the underlying pathophysiology affecting children with ADHD. Moreover, the authors suggested that ALFF values can reflect the intensity of spontaneous neuronal activity (SNA) in a given region of the brain and that the presence of functional lesions in the brain would cause a corresponding change in SNA. Matthew et al. [14] evaluated ALFFs to study low-frequency oscillations (LFOs) under resting-state conditions in patients with schizophrenia and found that these patients possessed abnormally decreased ALFFs in the lingual gyrus, cuneus, and precuneus areas. In contrast, abnormally increased ALFFs were found in the left subiculum hippocampi, which indicated the presence of abnormal LFOs in the brains of patients with schizophrenia.
Stevens et al. [9] identified multiple abnormalities in resting-state network FC in patients with mTBI using independent component analysis (ICA) of rs-fMRI data. These FC abnormalities were found in various areas within the brain, including in regions associated with visual processing, motor function, and limbic system function, as well as in numerous circuits believed to underlie executive cognition. By conducting ICA of rs-fMRI data, Iraji et al. [8] also found reduced FC in both the posterior cingulate cortex and the precuneus regions in patients with acute mTBI. Salvador et al. [15] initially established a whole-brain FC network under resting-state conditions in normal subjects. To accomplish this, they divided the brain into 90 regions (excluding the cerebellum) according to an automated anatomical labeling (AAL) template. Following this, they calculated the correlation coefficients of BOLD-fMRI signals between specific brain areas for each subject and finally used statistical analysis to identify existing connectivity networks. The network constructed using the above method was dependent on an a priori brain anatomy template to enable the division of brain areas, a process that can simplify the necessary calculations [15, 16].
The relationship between cognitive impairment following mTBI and FC within the brain is likely to be complex. The purposes of the current study were to assess FC in patients with mTBI and to investigate differences between FC in a group of patients with chronic mTBI and an age-matched control group using rs-fMRI. The secondary objective was to examine the relationship between FC and cognitive impairment following mTBI. We hypothesized that decreased FC following mTBI is associated with greater cognitive impairment.
Materials and methods
Between Feb. 2012 and May 2014, 25 patients (16 male and 9 female; mean age ± SD, 32.5 ± 10.4 years) with chronic mTBI were recruited from Daping Hospital, Third Military Medical University, Chongqing, China. All of the recruited patients had suffered injuries caused by motor vehicle accident. During the post-injury recovery stage, lasting from 26 to 40 days (average, 32.08 ± 3.62 days), all of the patients continued to complain of dizziness, headache, impaired concentration, insomnia, palpitations, forgetfulness, and other symptoms. All of the patients had a history of brief coma of 13 to 15 points as assessed by the Glasgow coma scale (GCS). Conventional computed tomography (CT) or MRI examinations showed no abnormalities, excluding previous disease history, brain trauma, surgery, or other brain lesions. Additionally, patients with epilepsy; patients with severe heart, liver, or renal dysfunction; and patients with blood disorders were excluded. Twenty-five healthy subjects who were matched to the 25 mTBI patients with respect to age, gender, and education level were recruited as controls. The control group included 15 males and 10 females, who ranged in age from 18 to 45 years (average, 31.5 ± 9.5 years).
Neuropsychological assessment
Intelligence quotient (IQ) was assessed using the Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV). The WAIS provides an estimate of general intelligence and is the most standardized intelligence test currently in use. The WAIS consists of 11 subtests. From these subtests, total IQ, verbal comprehension index (VCI), working memory index (WMI), perceptual reasoning index (PRI), and processing speed index (PSI) scores were obtained. The VCI included similarities, vocabulary, and information; the WMI included arithmetic and digit span; the PRI included block design, matrix reasoning, and visual puzzles; and the PSI included digit symbol coding and symbol search. The mini-mental state examination (MMSE) [17] is the most widely used screening measure for cognitive impairment because of its brevity and ease of administration. It has high retest reliability and is useful as a screening test for dementia and delirium. In this study, the MMSE was used to evaluate cognitive impairment: a score of less than 27 was considered cognitively impaired.
Image acquisition
A Siemens E3.0T superconductive MR scanner (Magnetom Verio, Siemens Medical Solutions, Erlangen, Germany) with a 16-channel phased-array head coil was used. All of the patients in the experimental group received cranial MRI in the supine position and with the head entering first.
Anatomical imaging was performed using conventional MRI SE sequence scanning (T1WI, T2WI) and gradient-echo T1-weighted scanning to obtain whole-brain MRI anatomical images. Spin-echo T1-weighted anatomical image scanning (repetition time/echo time (TR/TE) = 500/12 ms, field of view (FOV) = 230 mm, thickness spacing = 3.0 mm/1.0 mm, matrix = 320 × 256) was used to align and build these images. Gradient-echo T1-weighted 3D anatomical image scanning (FOV = 240 mm, thickness of 1.0 mm, no spacing, matrix = 512 × 512, TR/TE/Flip = 1900/3 93/15°) was used for the Talairach transformation of the images and to visualize the morphology of brain structures.
Resting-state echo-planar imaging was accomplished using a single-shot gradient-echo weighted sequence to obtain BOLD brain signals (thickness/spacing = 3.0/1.0 mm, TR/TE/Flip = 2000 ms/50 ms/90°, FOV = 220 mm, matrix = 64 × 64). During the resting-state scanning, all of the lights were turned off, and exposure to sounds was avoided. The subjects were asked to close their eyes and to lie down, relax, stay awake, and try not to think about anything. The scanning process lasted for 8 min.
Resting-state fMRI data analysis
Raw resting-state fMRI data were preprocessed using the Data Processing Assistant for Resting-State fMRI (DPARSF; State Key Laboratory of Cognitive Neuroscience and Learning in Beijing Normal University; http://rfmri.org/DPARSF) [18] and the Statistical Parametric Mapping software package (SPM5; Department of Neurology, London, UK. Http://www.fil.ion.ucl.ac.uk/spm). The following process was used: removal of the first 10 time points, time-level correction, head movement correction, and spatial normalization.
ALFF calculation was accomplished by using DPARSF to perform spatial smoothing with a Gaussian kernel with full-width half-maximum (FWHM), followed by filtering (passband frequency of 0.01–0.08 Hz) and linear trend removal for the preprocessed data.
FC analysis was accomplished using the following procedure. First, we divided each hemisphere of the brain into 45 anatomical brain regions based on the AAL template and then averaged the time sequence of all voxels in each brain area for all subjects. This ultimately allowed us to obtain the time series signals of 90 brain regions. For the time sequence of each brain region, we used linear regression to remove the effects of various interference factors, such as brain movement, white matter signal, and cerebrospinal fluid signal. The regressed voxel time series signals were band-pass filtered (0.01–0.1 Hz) to eliminate the impact of low-frequency drift and high-frequency noise associated with breathing and heartbeat. Finally, we used Pearson correlation analysis to compute correlation coefficients between two brain areas, obtained a correlation coefficient matrix, and then transformed the correlation coefficients into Fisher Z values to bring the matrix closer to a normal distribution. A P value of less than 0.05 (FDR-corrected) was considered to indicate a statistically significant difference.
Statistical analysis
A cognitive functional score was initially calculated for each subject using Excel 2007 and then reanalyzed using SPSS for Windows v17.0 (SPSS Inc., Chicago, IL, USA). Simple linear regression analyses were performed to investigate the relationships between the ALFF and FC values of the peak voxels of significant clusters of interest (independent variable) and the cognitive functional scores of total IQ, VCI, WMI, PRI, PSI, and MMSE (dependent variable) of the mTBI patients. All results were quoted as two-sided; P < 0.05 was considered statistically significant.
Results
Statistical analysis of clinical data from and cognitive function in mTBI patients
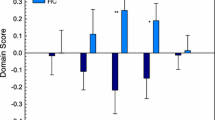
The average length of education was 12.84 ± 3.05 years in the mTBI group and 13.89 ± 3.22 years in the control group, with no significant differences between the groups. Compared with the normal control group, the mTBI group exhibited decreases in total IQ, VCI, and PRI scores, but there were no significant differences between the groups. In contrast, WMI and PSI did significantly differ between the groups: Both parameters were significantly decreased in the mTBI group (Table 1). There were no significant differences in MMSE score between the groups.
ALFF results
Compared with the healthy control group, the mTBI group exhibited significantly decreased ALFFs in the cingulate gyrus, the middle frontal gyrus, and superior frontal gyrus (Fig. 1). In contrast, the mTBI group exhibited significantly increased ALFFs in the left middle occipital gyrus, left precuneus, and lingual gyrus (Table 2).
Functional network analysis
Compared with the healthy control group, 15 FC pairs were significantly decreased in the brains of the mTBI patients (Table 3). The affected regions primarily included the thalamus, left caudate nucleus, and right hippocampus (Fig. 2).
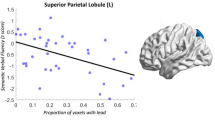
Correlation analysis
General linear regression analysis showed that the ALFF in the cingulate gyrus was significantly positively related to WMI in the mTBI patients (R 2 = 0.423, P < 0.05; Fig. 3). The results also showed that the FC between the left thalamus and the left middle frontal gyrus had a significantly positive correlation with WMI in the mTBI patients (R 2 = 0.381, P < 0.05; Fig. 4). However, these correlations did not exist in the control group, and there were no significant correlations between other abnormalities in FC and the various assessed intelligence indices.
Discussion
Physiological significance of changes in ALFFs under resting-state conditions
Previous study suggested that ALFFs can reflect spontaneous brain activation and can be used to reflect abnormal brain function under resting-state conditions [7, 14, 19–23]. The current study demonstrated that patients with mTBI exhibit notably decreased ALFFs in various brain regions, including the cingulate gyrus, the middle frontal gyrus, and superior frontal gyrus. In contrast, these patients exhibited notably increased ALFFs in the left middle occipital gyrus, left precuneus, and lingual gyrus. Linear regression analysis also indicated that the ALFF in the cingulate gyrus had a significantly positive relationship with WMI in mTBI patients (R 2 = 0.42, P < 0.05). Brain structures such as the frontal lobe and cingulate gyrus are considered to be closely involved in functions such as cognition and memory, and decreased ALFFs in these areas may signify weakened cerebration. The cingulate gyrus is a part of the brain’s limbic system, which functions to regulate emotions, learning, and memory. The current study found that the ALFF in the cingulate gyrus was significantly positively correlated with WMI, which suggests that decreased ALFFs in the cingulate gyrus may contribute to working memory dysfunctions in mTBI patients. The rs-fMRI results in this study also showed that mTBI patients exhibit increased ALFFs in the left middle occipital gyrus, left precuneus, and lingual gyrus, possibly indicating the presence of a functional compensation mechanism.
Physiological significance of changes in brain functional connectivity
Our study identified 15 FC pairs that were significantly decreased in mTBI patients. Additionally, we identified that the functional connection between the left thalamus and the left middle frontal gyrus had a significantly positive correlation with WMI (R 2 = 0.38, P < 0.05). Tang et al. [24] used a resting-state FC analysis method to demonstrate that the thalamus network connection becomes damaged in mTBI patients and that thalamus network connection intensity significantly correlates with clinical cognitive function, a finding that is consistent with the results of our study. However, Iraji et al. [8] reported that patients with acute mTBI exhibit significantly higher FC in several regions of the thalamus, including the anterior prefrontal cortex and the supramarginal gyrus, suggesting that the thalamocortical network becomes upregulated in response to acute brain injury. The differences in imaging findings that Iraji et al. identified between the two groups may indicate that a temporal memory recovery process occurs after mTBI. Other studies have shown that the prefrontal cortex is involved in maintaining working memory (i.e., short-term memory) and can assemble emotional information from other brain regions for further processing and handling. A large number of basic and clinical studies have confirmed that the left frontal gyrus is a key component in information processing and can coordinate working memory and other sources of information that are especially important for working memory (e.g., short-term memory) and attention sustaining [25–27]. Iraji et al. [8] also revealed decreased intrinsic connectivity in the inferior frontal gyrus in acute mTBI. Therefore, the functional connection between the left thalamus and the left middle frontal gyrus is weakened, potentially indicating that patients with mTBI may have insufficient memory capacity and judgment ability.
The current study has some limitations. We used an a priori anatomical template of the brain to divide it into 90 separate regions, and the establishment of our whole-brain FC network relied on this template. Although this approach simplified our calculations, it also led to the following disadvantages [28–31]. First, as each network node was defined using this a priori template, our brain network analysis results may differ if a whole-brain functional connection network map is established using a different template. Second, the establishment of a brain functional network using nodes from different brain regions can only be used to describe relationships between specific brain regions and will not provide in-depth analysis of whole-brain relationships.
Conclusion
The current study advances our understanding of mTBI using data obtained from rs-fMRI. Notably, we found that patients with mTBI exhibit abnormal ALFFs in several brain regions and that the ALFF of the cingulate gyrus had a significantly positive correlation with WMI in these patients. Additionally, these patients showed significantly decreased FC in the thalamus, caudate nucleus, and right hippocampus and a significantly positive correlation between FC in the left thalamus and the left middle frontal gyrus and WMI. These features may serve as a biomarker for the diagnosis of functional deficits in mTBI. A longitudinal study of a larger cohort is warranted to further reveal the physiological basis underlying the neurocognitive symptoms associated with mTBI.
References
Langlois JA, Rutland-Brown W, Wald MM (2006) The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil 21:375–378
Belanger HG, Vanderploeg RD, Curtiss G, Warden DL (2007) Recent neuroimaging techniques in mild traumatic brain injury. J Neuropsychiatry Clin Neurosci 19:5–20
Nolin P, Heroux L (2006) Relations among sociodemographic, neurologic, clinical, and neuropsychologic variables, and vocational status following mild traumatic brain injury: a follow-up study. J Head Trauma Rehabil 21:514–526
Whitnall L, McMillan TM, Murray GD, Teasdale GM (2006) Disability in young people and adults after head injury: 5–7 year follow up of a prospective cohort study. J Neurol Neurosurg Psychiatry 77:640–645
Scheid R, Walther K, Guthke T, Preul C, von Cramon DY (2006) Cognitive sequelae of diffuse axonal injury. Arch Neurol 63:418–424
Draper K, Ponsford J (2008) Cognitive functioning ten years following traumatic brain injury and rehabilitation. Neuropsychology 22:618–625
Biswal B, Yetkin FZ, Haughton VM, Hyde JS (1995) Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn Reson Med 34:537–541
Iraji A, Benson RR, Welch RD et al (2015) Resting state functional connectivity in mild traumatic brain injury at the acute stage: independent component and seed-based analyses. J Neurotrauma 32:1031–1045
Stevens MC, Lovejoy D, Kim J, Oakes H, Kureshi I, Witt ST (2012) Multiple resting state network functional connectivity abnormalities in mild traumatic brain injury. Brain Imaging Behav 6:293–318
Johnson B, Zhang K, Gay M et al (2012) Alteration of brain default network in subacute phase of injury in concussed individuals: resting state fMRI study. Neuroimage 59:511–518
Mayer AR, Mannell MV, Ling J, Gasparovic C, Yeo RA (2011) Functional connectivity in mild traumatic brain injury. Hum Brain Mapp 32:1825–1835
Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL (2001) A default mode of brain function. Proc Natl Acad Sci U S A 98:676–682
Zang YF, He Y, Zhu CZ et al (2007) Altered baseline brain activity in children with ADHD revealed by resting-state functional mri. Brain Dev 29:83–91
Hoptman MJ, X-NZ BPD (2010) Amplitude of low-frequency oscillations in schizophrenia: a resting state fMRI study. Schizophr Res 117:13–20
Salvador R, Suckling J, Coleman MR, Pickard JD, Menon D, Bullmore E (2005) Neurophysiological architecture of functional magnetic resonance images of human brain. Cereb Cortex 15:1332–1342
Liu Y, Liang M, Zhou Y et al (2008) Disrupted small-world networks in schizophrenia. Brain 131:945–961
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Chao-Gan Y, Yu-Feng Z (2010) DPARSF: a MATLAB toolbox for “pipeline” data analysis of resting-state fMRI. Front Syst Neurosci 4:13
Pelled G, Goelman G (2004) Different physiological MRI noise between cortical layers. Magn Reson Med 52:913–916
Yin Y, Li L, Jin C et al (2011) Abnormal baseline brain activity in posttraumatic stress disorder: a resting-state functional magnetic resonance imaging study. Neurosci Lett 498:185–189
Fornito A, Zalesky A, Bullmore ET (2010) Network scaling effects in graph analytic studies of human resting-state FMRI data. Front Syst Neurosci 4:22
Wang J, Wang L, Zang Y et al (2009) Parcellation-dependent small-world brain functional networks: a resting-state fMRI study. Hum Brain Mapp 30:1511–1523
Wang JH, Zuo XN, Gohel S, Milham MP, Biswal BB, He Y (2011) Graph theoretical analysis of functional brain networks: test-retest evaluation on short- and long-term resting-state functional MRI data. PLoS One 6:e21976
Tang L, Ge Y, Sodickson DK et al (2011) Thalamic resting-state functional networks: disruption in patients with mild traumatic brain injury. Radiology 260:831–840
Niogi SN, Mukherjee P, Ghajar J et al (2008) Structural dissociation of attentional control and memory in adults with and without mild traumatic brain injury. Brain 131:3209–3221
Salmond CH, Menon DK, Chatfield DA et al (2006) Diffusion tensor imaging in chronic head injury survivors: correlations with learning and memory indices. Neuroimage 29:117–124
Yonelinas AP, Hopfinger JB, Buonocore MH, Kroll NE, Baynes K (2001) Hippocampal, parahippocampal and occipital-temporal contributions to associative and item recognition memory: an fMRI study. Neuroreport 12:359–363
Wig GS, Schlaggar BL, Petersen SE (2011) Concepts and principles in the analysis of brain networks. Ann N Y Acad Sci 1224:126–146
Zalesky A, Fornito A, Harding IH et al (2010) Whole-brain anatomical networks: does the choice of nodes matter? Neuroimage 50:970–983
Hayasaka S, Laurienti PJ (2010) Comparison of characteristics between region-and voxel-based network analyses in resting-state fMRI data. Neuroimage 50:499–508
van den Heuvel MP, Stam CJ, Boersma M, Hulshoff Pol HE (2008) Small-world and scale-free organization of voxel-based resting-state functional connectivity in the human brain. Neuroimage 43:528–539
Acknowledgments
This study was funded by the General Program of National Natural Science Foundation of China (81171866,81571889), the Starting Fund of Overseas Returnees of Ministry of Education (2012) and the National Basic Key Research Program (973) (2014CB541602).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that all human and animal studies have been approved by the Third Military Medical University Ethics Committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed consent prior to inclusion in this study.
Conflict of interest
We declare that we have no conflict of interest.
Rights and permissions
About this article
Cite this article
Xiong, K., Zhang, J., Zhang, Y. et al. Brain functional connectivity and cognition in mild traumatic brain injury. Neuroradiology 58, 733–739 (2016). https://doi.org/10.1007/s00234-016-1675-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-016-1675-0