Abstract
Arsenic is successfully used in cancer chemotherapy and several cancer treatments on account of its apoptogenic effects. However, it is environmentally hazardous with potential for toxicity when distributed in the soil, water, and food, and long exposure to water contaminated with Arsenic may induce cancers. Some research studies have reported that liver is the storage site and an important target organ for Arsenic toxicity. In the present work, a new kind of organic arsenic compound, 4-(2-nitrobenzaliminyl) phenyl arsenoxide (NPA), was synthesized, and its potential involvement of mitochondria was explored. The results presented that the toxicology of NPA, at least in part, mediated mitochondrial function and may thoroughly destroy mitochondrial membrane physiological functions. NPA induced mitochondrial permeability transition pore (mtPTP) opening that induces mitochondrial biochemical abnormalities as evidenced by mitochondrial swelling, mitochondrial membrane potential breakdown, membrane fluidity alterations, and the strikingly remarkable protection of CsA. Meanwhile, both the decreased respiration rate of state 4 and the increased inner membrane H+ permeabilization revealed that the inner membrane function regarding important energy production chain was destroyed. The toxicity of NPA is due to its interaction with mitochondrial membrane thiol protein. This conclusion is based on the protective effects of RR, DTT, and MBM+.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arsenic has been used therapeutically for more than 2,400 years (Wu et al. 2010), which is an effective therapeutic agent for the treatment of several types cancers, such as lymphoma, esophageal cancer, promyelocytic leukemia, due to its ability of apoptosis induction (Zhang et al. 2001). Paradoxically, high concentration of naturally occurring Arsenic in drinking water is a serious environmental problem worldwide (Nordstrom 2002), and epidemiologic evidence implicated that exposure to drinking water contaminated with Arsenic has been linked to several human cancers (National Research Council (NRC) 2001). According to some researches, these different actions of Arsenic may result in the induction of apoptosis depending on cell type, exposure concentration, and exposure time (Miller et al. 2002).
Arsenic induces cell apoptosis and necrosis maybe through induction of mitochondrial permeability transition, alteration of mitochondrial function in proteins, and oxidative stress (Miller et al. 2002; Bustamante et al. 2005). As we all know, mitochondria are critical modulators of cell death, particularly in the initiation of apoptosis and necrosis (Kroemer and Reed 2000). It has also been reported that Arsenic induces the breakdown of mitochondrial membrane potential (Δψ) which is a crucial event commonly occurring in a variety of cell lines (Rojewski et al. 2004). Arsenic targets mitochondria through the permeability transition pore (PTP) opening, reactive oxygen species (ROS) generation, and then mitochondrial membrane depolarization leading to the initiation of cell death subsequently (Han et al. 2008).
It has been estimated that liver is the primary site for bio-transformation, accumulation, and excretion of Arsenic in mammals. Recent publications suggest that liver is a potential target organ for Arsenic toxicity (Liu and Waalkes 2008). Mitochondria are not only essential for providing energy for the cell but can also unleash “machineries of death” (Newmeyer and Ferguson-Miller 2003). In addition, it has been suggested that hepatic toxicity of Arsenic could be caused by the impairment of liver mitochondria (Hosseini et al. 2013).
Arsenic has two biologically important oxidation states: Arsenic (III) and Arsenic (V). Arsenic (III) species is widely used in biological system. In general, inorganic arsenic compound is more toxic than its organic counterpart (Choong et al. 2007). Organic arsenic compounds have greater affinity toward biological macromolecules, subcellular organelles, and cells (Chen et al. 2013). Our group synthesized a new kind of organic arsenic compound, 4-(2-nitrobenzaliminyl) phenyl arsenoxide (NPA) which is an Arsenic (III)-containing Schiff base derivative (Fig. 1). Due to the key roles mitochondria play in Arsenic toxicity, we try to explore NPA toxicity on mitochondria in this study. The result demonstrated that NPA induced mtPTP opening which can induce apoptosis. Besides, the increased inner membrane permeabilization to K+ may be another factor. We postulated that the increased inner membrane permeabilization to H+ and the stimulated respiration state 4 revealed that the inner membrane function was destroyed. In a manner similar to inorganic arsenic compound, NPA targets –SH protein to modify PTP conformation which leads to an alteration of mitochondrial function.
Materials and Methods
Chemicals
Bovine serum albumin (BSA), rhodamine 123 (Rh123), hematoporphyrin (HP), cyclosporin A (CsA), dithiothreitol (DTT), adenosine diphosphate (ADP), 2,4-dinitrophenol (DNP), ruthenium red (RR), rotenone, oligomycin, ethylene glycol tetraacetic acid (EGTA), and ethylene diamine tetraacetie acid (EDTA) were all purchased from Sigma (St. Louis, MO). All other reagents were of analytic grade, and all solutions were prepared with aseptic double-distilled water.
Isolation of Rat Liver Mitochondria
Mitochondria were isolated from male Wistar rat (about 250 g) liver by differential centrifugation according to conventional methods (Paul et al. 2008). The liver tissue was minced on ice and resuspended in medium A (250 mM sucrose, 2 mM HEPES, 0.1 mM EDTA and 0.1 % fatty acid-free BSA, pH 7.4). The final mitochondrial pellet was preserved in buffer B (220 mM mannitol, 70 mM sucrose, 0.1 mM EDTA, pH 7.4). All the procedures were carried out at 4 °C. The mitochondrial protein concentration was determined by the biuret method (Gornall et al. 1949) using BSA as a standard.
Mitochondrial Swelling Assays
Measurement of mitochondrial swelling was performed using a UNICO 4802 double-beam spectrophotometer at 540 nm. Mitochondrial swelling was estimated by analyzing the change of absorbance as described (Hosseini et al. 2013). Mitochondria (0.5 mg protein/mL) were homogenized in buffer MAB (2 mL) containing 200 mM sucrose, 5 mM succinate, 1 mM Tris-MOPS, 1 μM EGTA-Tris, 2 μM rotenone, and 3 μg/mL oligomycin, pH 7.4 and incubated with different concentrations of NPA. Buffer MAB was mixed with Ca2+ (5 μM) before injecting with NPA.
Estimation of Mitochondrial Transmembrane Potential
Mitochondrial Δψ changes were estimated by fluorescence changes of Rh123 (100 nM) using the LS-55 fluorophotometer (Perkin-Elmer, Norwalk, USA) at λ ex = 488 nm, λ em = 525 nm. Rh123 is a lipophilic cationic dye which can permeate inner membrane and accumulate in the mitochondrial matrix (Ricchelli et al. 2003). Suspended mitochondria (0.5 mg protein/mL) in medium MAB (2 mL) were labeled by Rh123 for 2 min, and then NPA was added to the medium.
Mitochondrial Membrane Fluidity
Mitochondrial membrane fluidity changes were analyzed by the fluorescence anisotropies of HP recorded on LS-55 fluorophotometer (Zhang et al. 2011), operating at excitation and emission wavelengths of 520 and 626 nm, respectively. HP is a kind of membrane lipid-bound dye mostly interacting with mitochondrial inner membrane protein sites. The values of anisotropy (r) could be obtained by measurements of I Π and I ⊥ (i.e., the fluorescence intensities polarized in parallel and perpendicular planes, respectively, to the vertical polarization plane of the excitation beam) in MAB for about 10 min. The anisotropy (r) is defined by the following equation:
where \( G = I_{ \bot } /I_{\Pi} \) is the correction factor for instrumental artifacts.
Measurement of Mitochondrial Inner Membrane Permeabilization
Mitochondrial inner membrane permeabilities to H+ and K+ were measured spectrophotometrically by monitoring the absorbance at 540 nm (Dong et al. 2013). Mitochondrial inner membrane permeability to H+ was detected in K-acetate medium (KAc medium) containing 135 mM KAc, 5 mM HEPES, 0.2 mM EDTA, 0.1 mM EGTA, and 2 μM rotenone, pH 7.1. To detect mitochondrial inner membrane permeability to K+, we used KNO3 medium which is prepared by adding 135 mM KNO3—instead of 135 mM KAc as in the preparation of KAc medium.
Mitochondrial Respiratory Activities
Mitochondrial respiratory rates under three different states were evaluated by the consumption of oxygen using a Clark-type electrode, in a closed glass chamber equipped with magnetic stirring, at 25 °C (Oxygraph, Hatchtech, Dorchester, UK). Mitochondria (1 mg protein/mL) were added to MRB (1 mL) under stirring, containing 250 mM sucrose, 20 mM KCl, 10 mM HEPES, 5 mM K2HPO4, 2 mM MgCl2, and 1 mM rotenone, pH 7.4 (Robson et al. 2010). Mitochondrial respiratory state 4 was initiated by adding 5 mM succinate. To induce respiration state 3, 5 mM succinate and 100 μM ADP were added. For uncoupled respiration, 30 μM DNP was added instead of ADP. The slope of the oxygen consumption curve given in the oxygraph reflected the rate of oxygen consumption by mitochondria at each state. Respiratory Control Ratio (RCR) was calculated by dividing the rate of oxygen consumption of respiration state 3 by the rate of respiration state 4.
Mitochondrial Membrane Lipid Peroxidation
Mitochondrial membrane lipid peroxidation was assessed by the consumption of oxygen using a Clark-type electrode. Mitochondria (1 mg protein/mL) were injected into stirred lipid peroxidation medium (1 mL), containing 175 mM KCl, 10 Mm Tris–HCl, and 3 μM rotenone, pH 7.4 (Li et al. 2011). Rotenone in the medium could suppress mitochondrial respiration induced by endogenous substrates during the experiment. Membrane lipid peroxidation was initiated by adding 1 mM ADP/0.1 mM Fe2+. Iron (II) solution must be prepared before using.
Results
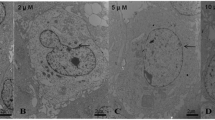
NPA-Induced Mitochondrial Swelling and Inhibited by CsA
Mitochondrial swelling was monitored with changes of absorbance at 540 nm, and the decreased absorbance exhibited an increase in mitochondrial swelling. As shown in Fig. 2a, the absorbance decreased in the presence of NPA, and the decrease rate was proportionate to the testing concentration of NPA. In other words, NPA could induce mitochondrial swelling in a dose-dependent manner. On the other hand, CsA (15 μM) which is a well-established pharmacological inhibitor of MPT totally protected mitochondrial swelling induced by exposure to 500 μM NPA (Fig. 2b).
Mitochondrial Transmembrane Potential Collapse
Rh123 can accumulate in energized mitochondrial matrix due to the mitochondrial inner membrane inside negative Δψ, leading to medium fluorescence quenching of Rh123. Upon membrane depolarization, Rh123 is released into medium, thus causing increase in fluorescence intensity. As shown in Fig. 3, the percentage increase of fluorescence intensity was synchronous with the increasing concentrations of NPA which means NPA induced the breakdown of Δψ.
NPA Induced Alterations of Mitochondrial Membrane Fluidity
HP mainly interacts with protein sites and selectively locates on the mtPTP constituents. The change of fluorescence anisotropy of mitochondria-bound dyes reflects changes in membrane fluidity. The decrease of HP anisotropy corresponds to the increase of membrane fluidity (Fig. 4a), whereas the increase of HP anisotropy corresponds to the decrease of membrane fluidity (Fig. 4b). As shown in Fig. 4a, with low concentration (20–80 μM), NPA induced the increase of membrane fluidity and was inversely proportional to the concentration. On the contrary, with high concentration (120–500 μM), NPA induced the decrease of membrane fluidity to an extent proportional to the concentration.
Mechanism of NPA at High Concentration
RR, a hexavalent polysaccharide stain, is a mitochondrial Ca2+ uniporter inhibitor which can abolish Ca2+ influx effectively (Bae et al. 2003). As shown in Fig. 5, mitochondrial swelling induced by NPA was strikingly suppressed with the addition of RR. It is known that mitochondria are able to reseal after the removal of overmuch Ca2+ by chelator EGTA (Leung et al. 2010). As shown in Fig. 5, mitochondrial swelling was not totally inhibited with addition of EGTA. DTT and MBM+ selectively protect –SH proteins on mitochondrial membrane. DTT can permeate mitochondrial inner membrane, whereas MBM+ is impermeable (Puntel et al. 2010). The results presented in Fig. 5 show that DTT and MBM+ only inhibited mitochondrial swelling partially.
Effect of NPA on Mitochondrial Inner Membrane Permeabilization to H+ and K+
As shown in Fig. 6a, mitochondria underwent a slight swelling rate in KAc medium without NPA. With the addition of NPA, mitochondria swelling rate significantly increased in a concentration-dependent manner. So, NPA promoted inner membrane permeabilization to H+. The H+ gradient across the mitochondrial membrane was disrupted by the addition of NPA. The same conclusion could be drawn from Fig. 6b: NPA promoted inner membrane permeabilization to K+. NPA disturbed the H+ and K+ balance between mitochondrial matrix and intermembrane space. Its influence on inner membrane permeabilization to K+ was more obvious and intensive. The results of Fig. 6b show a platform as the time lapsed over the duration of the test which means NPA-promoted swelling in KNO3 medium was more rapid.
Mitochondrial Oxygen Consumption
Mitochondrial oxygen consumption was monitored in the presence of varying concentrations of NPA. The parameters assessed were mitochondrial different respiratory states (state 3, state 4, and uncoupled state) and mitochondrial membrane lipid peroxidation.
A high rate of state 3 indicates an intact respiratory chain and ATP synthesis, while a low rate of state 4 indicates an intact mitochondrial inner membrane (Adlam et al. 2005). At the tested concentration, NPA stimulated mitochondrial respiratory state 4 explicitly at concentrations from 10 to 50 μM (Fig. 7a); the degree of stimulation increased in a concentration-dependent manner, showing that NPA acted as an uncoupler (Robson et al. 2010). NPA clearly did not have any influence over mitochondrial respiration state 3 and uncoupled state at the tested concentrations. NPA caused a net decrease of RCR ratio, suggestive of extensive mitochondrial damage in the presence of NPA (Fig. 7b).
a NPA induced alterations of mitochondrial respiratory activities at different states. b Effects of different concentrations of NPA on RCR. c Changes of mitochondrial membrane lipid peroxidation induced by NPA. Lipid peroxidation was induced by the pro-oxidant pair, ADP/Fe2+, and evaluated by oxygen consumption. c (NPA)/μM: a–e: 0, 10, 20, 30, 50
Mitochondrial membrane lipid peroxidation was evaluated by measuring mitochondrial oxygen consumption without respiratory state and induced by the pro-oxidant pair ADP/Fe2+. Under this condition, oxygen consumption increased due to the polyunsaturated fatty acid acyl chain of membrane phospholipids oxidation by ROS (Niki et al. 2005). Oxygen consumption rate was reduced with the addition of NPA reflecting the decreased lipid peroxidation level (Fig. 7c).
Discussion
Mitochondrial dysfunction is a fundamental pathogenic mechanism that leads to several significant toxicities in mammals especially those associated with liver (Castanha Zanoli et al. 2012). To assess the potential involvement of mitochondria in NPA-related toxicity, we assessed its effects using isolated rat liver mitochondria as model. The presented results could indicate the toxicology of NPA to some extent.
It is well known that mitochondrial membrane permeability is a major regulative factor of mitochondrial function, and mtPTP has a key role in the control of apoptosis. As shown in our results, the first aim in this study was to investigate some parameters of mtPTP opening. Our observation indicated that NPA caused mitochondrial swelling in a concentration-dependent manner and Δψ disruption indicating change in membrane permeability transition. In addition, CsA effectively inhibited the NPA- induced swelling. It is concluded that NPA stimulated the mtPTP opening. mtPTP is a high-conductance channel located between mitochondrial inner and outer membranes, and formed by adenine nucleotide translocase (ANT), voltage-dependent anion channel (VDAC), and cyclophilin D (CyP-D) (Vaseva et al. 2012). The mtPTP opening is always accompanied with the changes of membrane fluidity, and this mitochondrial factor could reflect the dynamic properties of mitochondrial membranes. In this study, we used HP as probe which can accumulate in the boundary lipids area surrounding some inner-mitochondrial carriers specifically. The data presented in the study suggested that NPA induced alterations of mitochondrial membrane fluidity, which confirmed the conclusion that NPA stimulated the opening of mtPTP.
As mentioned above, NPA indeed induced mitochondrial dysfunction through mtPTP opening. In order to investigate the association between NPA and mtPTP, we conducted tests to investigate the actions of each of the most important PTP inhibitors (RR, EGTA, DTT, and MBM+) at high (120 μM) concentration. As illustrated in Fig. 5, NPA-produced swelling was hampered by the inhibitors partly or totally. NPA-induced swelling is only partially reversed with the addition of DTT and MBM+. DTT and MBM+ are thiol reagents that can prevent –SH oxidation involved in the control of mtPPT opening (Leung et al. 2008). Besides, MBM+ is impermeable to mitochondrial inner membrane, whereas DTT is permeable (Puntel et al. 2010). It is quite possible that NPA-induced mitochondrial dysfunction involves mitochondrial inner membrane outer and inner proteins. RR is a noncompetitive inhibitor of mitochondrial Ca2+ uniporter and preserves Ca2+ influx (Bae et al. 2003). Thus, it is reasonable to suggest that NPA-induced mtPTP opening may be monitored by the Ca2+ uniporter because with the addition of RR, a marked suppression was observed. During the mtPTP opening, the free Ca2+ was not the only factor because EGTA also prevented NPA-stimulated swelling partially. EGTA (a Ca2+ chelator) is impermeable to mitochondrial inner membrane and presumably does not enter mitochondrial matrix. Hence, Ca2+ uniporter was attacked resulting in mitochondria-accumulated free Ca2+. Meanwhile, we speculated Ca2+ channel was opened. Taken together, all these indicated that NPA probably acted through interaction with a Ca2+ trigger site(s) and via oxidation of –SH groups (Belyaeva and Korotkov 2003).
The most prominent roles of mitochondria are to produce energy currency (adenosine triphosphate, ATP) for cells, as reflected by respiration electron train located in the mitochondrial membrane for this task (Newmeyer and Ferguson-Miller 2003). H+ can travel across the mitochondrial inner membrane and dissociate in mitochondrial matrix, producing a proton gradient which enables ATP Synthase to synthesize ATP (Liu et al. 2011). During mitochondrial respiration state 4, most of the oxygen consumed is derived from H+ leakage across the mitochondrial membrane (Murphy 2001). Taken together, the results (Figs. 6a, 7a) indicated that NPA stimulated respiration state 4 due to the change of mitochondrial inner membrane permeabilization to H+. Although there is no literature available about NPA toxicology, it is reasonable to suggest that mitochondrial inner membrane function about respiration would be influenced when NPA induced the mitochondrial dysfunction, at least to a certain degree.
Although mtPTP opening is always considered as a general mechanism during cell apoptosis, it is not the only way. In cells, intracellular K+ acts as a repressor of apoptotic effectors, and the loss of K+ may serve as a distress signal to allow apoptosis (Eliseev et al. 2003). Our results have shown that the K+ gradient across the mitochondrial membrane got disrupted with the addition of NPA. A huge influx of K+ into mitochondrial matrix and water occurs following the osmolarity changes causing mitochondrial swelling (Yu 2003). Excessive K+ efflux over the water movement can lead to a significant decrease in concentrations of K+. Therefore, it is assumed that there is another way to trigger apoptosis, i.e., dissipate K+ gradient across the mitochondrial inner membrane. Arsenic targets mitochondria by the generation of ROS—lipid peroxidation is one of the main oxidative alterations by ROS in biological membrane system, which is initiated by iron chelated by substances such as ADP (Gill and Tuteja 2010). However, lipid peroxidation was inhibited in the presence of different concentrations of NPA. We feel that more studies are necessary to better understand the toxicology of NPA.
In summary, we studied the effects of NPA on isolated rat mitochondria. NPA induced the mitochondrial swelling, Δψ disruption, and membrane fluidity alterations as the result of mtPTP opening as confirmed by the marked suppression of CsA. Incidentally, the increased inner membrane permeabilization to K+ may contribute to apoptosis. At the same time, mitochondrial respiration system was influenced by the addition of NPA. We have hypothesized that not only the Ca2+ trigger site(s) plays a substantial role in NPA-induced mitochondrial dysfunction. Besides, thiol site(s) oxidation is profound too.
References
Adlam VJ, Harrison JC, Porteous CM, James AM, Smith RAJ, Murphy MP, Sammut IA (2005) Targeting an antioxidant to mitochondria decreases cardiac ischemia-reperfusion injury. FASEB J 19(9):1088–1095
Bae JH, Park JW, Kwon TK (2003) Ruthenium red, inhibitor of mitochondrial Ca2+ uniporter, inhibits curcumin-induced apoptosis via the prevention of intracellular Ca2+ depletion and cytochrome c release. Biochem Biophys Res Commun 303(4):1073–1079
Belyaeva EA, Korotkov SM (2003) Mechanism of primary Cd2+-induced rat liver mitochondria dysfunction: discrete modes of Cd2+ action on calcium and thiol-dependent domains. Toxicol Appl Pharm 192(1):56–68
Bustamante J, Nutt L, Orrenius S, Gogvadze V (2005) Arsenic stimulates release of cytochrome c from isolated mitochondria via induction of mitochondrial permeability transition. Toxicol Appl Pharmacol 207(2):110–116
Castanha Zanoli JC, Maioli MA, Medeiros HC, Mingatto FE (2012) MingattoAbamectin affects the bioenergetics of liver mitochondria: a potential mechanism of hepatotoxicity. Toxicol In Vitro 26(1):51–56
Chen XY, Hu XL, Xia CF, Qin CQ, Liu Y (2013) Antibacterial evaluation of novel organoarsenic compounds by the microcalorimetric method. Biol Trace Elem Res 153(1–3):382–389
Choong TSY, Chuah TG, Robiah Y, Gregory Koay FL, Azni I (2007) Arsenic toxicity, health hazards and removal techniques from water: an overview. Desalination 217:139–166
Dong JX, Zhao GY, Yu QLY, Li R, Yuan L, Chen J, Liu Y (2013) Mitochondrial dysfunction induced by Honokiol. J Membr Biol 246(5):375–381
Eliseev RA, Salter JD, Gunter KK, Gunter TE (2003) Bcl-2 and tBid proteins counter-regulate mitochondrial potassium transport. Biochim Biophys Acta 1604(1):1–5
Gill SS, Tuteja N (2010) Reactive oxygen species and antioxidant machinery in abiotic stress tolerance in crop plants. Plant Physiol Biochem 48(12):909–930
Gornall AG, Bardawill CJ, David MM (1949) Determination of serum proteins by means of the biuret reaction. J Bioenerg Biomenbr 177(2):751–766
Han YH, Kim SZ, Kim SH, Park WH (2008) Arsenic trioxide inhibits the growth of Calu-6 cells via inducing a G2 arrest of the cell cycle and apoptosis accompanied with the depletion of GSH. Cancer Lett 270(1):40–55
Hosseini MJ, Shaki F, Ghazi-Khansari M, Pourahmad J (2013) Toxicity of Arsenic (III) on isolated liver mitochondria: a new mechanistic. Appr Iran J Pharmaceut Res 12:121–138
Kroemer G, Reed JC (2000) Mitochondrial control of cell death. Nat Med 6(5):513–519
Leung AW, Varanyuwatana P, Halestrap AP (2008) The mitochondrial phosphate carrier interacts with cyclophilin D and may play a key role in the permeability transition. J Biol Chem Bioenergy 283(39):26312–26323
Li JH, Zhang Y, Xiao Q, Tian FF, Liu XR, Li R, Zhao GY, Jiang FL, Liu Y (2011) Mitochondria as target of quantum dots toxicity. J Hazard Mater 194:440–444
Liu J, Waalkes MP (2008) Liver is a target of arsenic carcinogenesis. Toxicol Sci 105(1):24–32
Liu XR, Li JH, Zhang Y, Ge YS, Tian FF, Dai J, Jiang FL, Liu Y (2011) Mitochondrial permeability transition induced by different concentrations of Zinc. J Membr Biol 244(3):105–112
Miller WH Jr, Schipper HM, Lee JS, Singer J, Waxman S (2002) Mechanisms of action of arsenic trioxide. Cancer Res 62(14):3893–3903
Murphy MP (2001) How understanding the control of energy metabolism can help investigation of mitochondrial dysfunction, regulation and pharmacology. BBA-Bioenergetics 1504(1):1–11
National Research Council (NRC) (2001) Subcommittee to update the 1999 arsenic in drinking water report. Arsenic in drinking water 2001 update. National Academy Press, Washington, pp 24–74
Newmeyer DD, Ferguson-Miller S (2003) Mitochondria: releasing power for life and unleashing the machineries of death. Cell 112(4):481–490
Niki E, Yoshida Y, Saito Y, Noguchi N (2005) Lipid peroxidation: mechanisms, inhibition, and biological effects. Biochem Biophys Res Commun 338(1):668–676
Nordstrom DK (2002) Worldwide occurrences of arsenic in ground water. Science 296(5576):2143–2145
Paul MK, Kumar R, Mukhopadhyay AK (2008) Dithiothreitol abrogates the effect of arsenic trioxide on normal rat liver mitochondria and human hepatocellular carcinoma cells. Toxicol Appl Pharm 226(2):140–152
Puntel RL, Roos DH, Folmer V, Nogueira CW, Galina A, Aschner M, Rocha JB (2010) Mitochondrial dysfunction induced by different organochalchogens is mediated by thiol oxidation and is not dependent of the classical mitochondrial permeability transition pore opening. Toxicol Sci 117(1):133–143
Ricchelli F, Beghetto C, Gobbo S, Tognon G, Moretto V, Crisma M (2003) Structural modifications of the permeability transition pore complex in resealed mitochondria induced by matrix-entrapped disaccharides. Arc Biochem Biophys 410(1):155–160
Robson LP, Daniel HR, Vanderlei F, Cristina WN, Antonio G, Michael A, João BTR (2010) Mitochondrial dysfunction induced by different organochalchogens is mediated by thiol oxidation and is not dependent of the classical mitochondrial permeability transition pore opening. Toxicol Sci 117(1):133–143
Rojewski MT, Korper S, Thiel E, Schrezenmeier H (2004) Depolarization of mitochondria and activation of caspases are common features of arsenic(III)-induced apoptosis in myelogenic and lymphatic cell lines. Chem Res Toxicol 17(1):119–128
Vaseva AV, Marchenko ND, Ji K, Tsirka SE, Holzmann S, Moll UM (2012) p53 opens the mitochondrial permeability transition pore to trigger necrosis. Cell 149(7):1536–1548
Wu DD, Xiao YF, Geng Y, Hou J (2010) Antitumor effect and mechanisms of arsenic trioxide on subcutaneously implanted human gastric cancer in nude mice. Cancer Genet Cytogen 198(2):90–96
Yu SP (2003) Regulation and critical role of potassium homeostasis in apoptosis. Prog Neurobiol 70(4):363–386
Zhang TD, Chen GQ, Wang ZG, Zhen YW, Chen SJ, Chen Z (2001) Arsenic trioxide, a therapeutic agent for APL. Oncogene 20(49):7146–7153
Zhang Y, Li JH, Liu XR, Jiang FL, Tian FF, Liu Y (2011) Spectroscopic and microscopic studies on the mechanisms of mitochondrial toxicity induced by different concentrations of cadmium. J Membr Biol 241(1):39–49
Acknowledgments
We gratefully acknowledge the financial support from the National Natural Science Foundation of China (No. 21225313); Hubei Natural Science Foundation of China (No. 3013CFC027); B Plan of Hubei Provincial Education Office of China (No. B20114404) and the Hubei Polytechnic University Program of China (No.14xjz03A).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jiao, YH., Zhang, Q., Pan, LL. et al. Rat Liver Mitochondrial Dysfunction Induced by an Organic Arsenical Compound 4-(2-Nitrobenzaliminyl) Phenyl Arsenoxide. J Membrane Biol 248, 1071–1078 (2015). https://doi.org/10.1007/s00232-015-9818-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00232-015-9818-5