Abstract
Purpose
The aim of this study was to examine the age of onset for increased dose-adjusted serum concentrations (C/D ratio) of common antidepressant drugs and to explore the potential association with sex and CYP2C19/CYP2D6 genotype.
Methods
Serum concentrations and prescribed daily doses for citalopram, escitalopram, sertraline, venlafaxine and mirtazapine, and CYP genotypes, were obtained from a therapeutic drug monitoring (TDM) service. Segmented linear regression analysis was used to examine the relationship between age and antidepressant log C/D ratio in (i) all individuals, (ii) men and women, and (iii) CYP2D6/CYP2C19 normal metabolizers (NMs) and CYP2D6/CYP2C19 intermediate or poor metabolizers (IMs/PMs).
Results
A total of 34,777 individuals were included in the study; CYP genotype was available for 21.3%. An increase in C/D ratio started at 44‒55 years of age. Thereafter, the increase progressed more rapidly for citalopram and escitalopram than for venlafaxine and mirtazapine. A doubled C/D ratio was estimated to occur at 79 (citalopram), 81 (escitalopram), 86 (venlafaxine), and 90 years (mirtazapine). For sertraline, only modest changes in C/D ratio were observed. For escitalopram and venlafaxine, the observed increase in C/D ratio started earlier in women than in men. The results regarding CYP genotype were inconclusive.
Conclusion
The age-related increase in C/D ratio starts in middle-aged adults and progresses up to more than twofold higher C/D ratio in the oldest old. Sertraline seems to be less prone to age-related changes in C/D ratio than the other antidepressants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment with antidepressants is common in current healthcare, and older people are a major user group. When antidepressants are administered to people aged 65 years or older, they have on average 1.5–2 times higher serum concentrations than younger people using equal doses [1, 2]. Furthermore, serum concentrations above the recommended reference range have been reported to be twice as common in older people, despite being prescribed lower doses [3].
Therapeutic reference ranges of antidepressants are generally based on healthy adult populations, and may not be valid for older patients [4]. As older people, especially the frail, are particularly vulnerable to side effects of drugs, elevated serum concentrations may be problematic in this patient group [5]. We have recently reported that only modest dose reductions occur among patients ≥ 65 years over a 10-year period and that more than one third of these patients have serum concentrations above the recommended reference range [6]. However, using an age cut-off of 65 can be questioned, as it reflects the traditional age of retirement rather than age-related physiological changes, such as altered fat/muscle ratio and decreased kidney function [7]. Indeed, it may be reasonable to assume that increasing concentrations with the same dose can be a continuous process with increasing age. Yet, as far as we are aware, it is not known at which age a change in antidepressant concentration-to-dose (C/D) ratio appears, and how the C/D ratio develops over time with increasing age.
Furthermore, one could speculate that sex and genetic prerequisites may have implications for the concentrations achieved. Indeed, an association between sex and antidepressant pharmacokinetics has been described [8], and progressive age–related changes in C/D ratio could therefore be suspected to differ between men and women. Regarding pharmacogenetics, polymorphic cytochrome P450 (CYP) enzymes are important for the metabolism of antidepressants. For instance, CYP2C19 is involved in the metabolism of citalopram, escitalopram, and sertraline; CYP2D6 is one of several CYP enzymes involved in the metabolism of mirtazapine; and for venlafaxine, both CYP2D6 and CYP2C19 are important for the serum concentration of the drug and the active moiety [9,10,11,12]. The Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline provides dose recommendations according to CYP2D6 and CYP2C19 genotype for all the abovementioned drugs except mirtazapine [9].
In this study, we aimed to examine the age of onset for increased dose-adjusted serum concentration (C/D) of antidepressant drugs and to explore the potential association with sex and CYP2C19/CYP2D6 genotype.
Methods
Patients and samples
Data were obtained from a therapeutic drug monitoring (TDM) database at Diakonhjemmet Hospital, Oslo, Norway. This database contains information on serum concentration measurements from patients that are clinically followed up in primary or secondary health care. Serum concentration measurements from the period 2010–2020 were extracted for individuals, 18 years or older, referred to TDM for one of the following antidepressants: citalopram, escitalopram, sertraline, venlafaxine, and mirtazapine. Patient age, sex, prescribed antidepressant dose, and sampling time were also extracted from the TDM database. For the subgroup of patients who had performed CYP2D6 and CYP2C19 pharmacogenetic analyses, these results were also obtained. Finally, when TDM of interacting drugs was requested concurrently with the included antidepressants, this information was extracted. The interacting drugs included the CYP inducers phenobarbital, phenytoin, and carbamazepine, and the CYP inhibitors bupropion, fluvoxamine, fluoxetine, levomepromazine, and paroxetine. Information regarding comedication with other drugs than the abovementioned was not available.
Blood samples were excluded if not collected within 10–26 h after last drug intake, and if the serum concentration was outside the limits of quantification. Samples where no metabolite was detected were also excluded as this probably reflects poor compliance. Furthermore, to avoid TDM results affected by drug interactions, samples were excluded if the abovementioned CYP inducers/inhibitors were analyzed and detected in the sample. Also, for some patients, there were multiple samples, and to maximize data at older ages, all but the most recent sample were excluded.
Drug analyses
Serum concentrations of the antidepressants, including the main metabolites, were determined by validated and certified analytical methods developed for routine TDM analyses at the Center for Psychopharmacology, Diakonhjemmet Hospital, Norway. During the inclusion period, the analytical assays were modified due to renewal of the analytical instruments, and all modifications were cross-validated. Briefly, in the current ultra-performance liquid chromatography high-resolution MS (UPLC-HRMS) method, protein precipitation was performed with an acetonitrile-methanol mix. Purified serum samples were injected into a Vanquish UPLC system (Thermo Fisher Scientific, Waltham, MA, USA). Chromatographic separation of all compounds was achieved with an XBridge BEH C18 column (2.6 µm, 2.1 × 75 mm; Waters Corporation, Milford, MA, USA) by gradient elution with acetonitrile and ammonium acetate (pH = 4.8).
Using a QExactive Hybrid Quadropole-Orbitrap MS (Thermo Fisher Scientific), full scan data was acquired at a resolution of 70,000 within the 100–1500-Da scan range. The compounds were quantified in a full-scan acquisition mode, and m/z values were 325.17107 for citalopram and escitalopram, 311.15542 for desmethylcitalopram and desmethylescitalopram, 306.08108 for sertraline, 292.0654 for desmethylsertraline, 278.21146 for venlafaxine, 264.19581 for O-desmethylvenlafaxine, 266.16517 for mirtazapine, and 252.14952 for desmethylmirtazapine. The limits of quantification were 8–1000 nmol/L for citalopram/escitalopram, 5–400 nmol/L for desmethylcitalopram/escitalopram, 10–600 nmol/L for sertraline, 20–1200 nmol/L for desmethylsertraline, 10–800 nmol/L for mirtazapine, 10–500 nmol/L for desmethylmirtazapine, 50–4000 nmol/L for venlafaxine, and 75–4000 nmol/L for O-desmethylvenlafaxine. Intra- and inter-day validation parameters of imprecision and inaccuracy showed less than 15% deviation for all compounds. For venlafaxine, the serum concentration is presented as the active moiety, i.e., the sum of parent drug and active metabolite.
Genotyping
Genotyping of CYP2D6 included identification of the no function variant alleles CYP2D6*3 (rs35742686), CYP2D6*4 (rs3892097), CYP2D6*5 (gene deletion), and CYP2D6*6 (rs5030655); the decreased function alleles CYP2D6*9 (rs5030656), CYP2D6*10 (rs1065852), and CYP2D6*41 (rs28371725); and allele multiplication. Genotyping of CYP2C19 included the no function alleles CYP2C19*2 (rs4244285), CYP2C19*3 (rs4986893), and CYP2C19*4 (rs28399504), and the increased function allele CYP2C19*17 (rs12248560). Analysis of variant alleles was performed using the TaqMan-based real-time PCR assays implemented for routine pharmacogenetic analyses at the Center for Psychopharmacology, Diakonhjemmet Hospital. To detect deletion or multiplication of CYP2D6, copy number analysis was performed with TaqMan Copy Number Assay targeting exon 9, using RNase P as endogenous control.
Genotype-predicted phenotype
Patients who carried two no function alleles were defined as poor metabolizers (PMs). Patients carrying a no function allele combined with a decreased function allele, a normal function allele, or an increased function allele, and patients carrying two decreased function alleles, were defined as intermediate metabolizers (IMs). Those who presented two increased function alleles (CYP2C19*17/*17) or more than two CYP2D6*1 alleles were defined as ultrarapid metabolizers (UMs). For CYP2D6, individuals with gene duplication and a no function or decreased function allele were classified as having unknown CYP2D6 genotype, due to lacking information regarding which allele was duplicated. The remaining individuals were classified as normal metabolizers (NMs). Individuals with the CYP2C19*1/*17 genotype were merged into the NM phenotype group in concordance with guidelines from the Dutch Pharmacogenetics Working Group [13].
Statistics
The distribution of concentration-to-dose (C/D) ratios of the examined drugs were right skewed and therefore log transformed to better approach the normality assumption in linear regression analyses. For the same reason, C/D ratios are presented as geometric means.
Segmented linear regression analysis was used to examine the relationship between age and log C/D ratio for the studied antidepressants. This regression technique performs piecewise linear regressions, allowing estimation of the point where the regression line changes direction, i.e., the “breakpoint” (B) [14]. A starting value for age was chosen for the estimation of one potential breakpoint and two piecewise relations for each antidepressant. The starting values were obtained using Davies test evaluated at k = 100 points [14]. Sex and blood sampling time were included as covariates in the segmented regression analysis. The regression coefficients for the slope before and after the breakpoint B were denoted R1 and R2, respectively. Furthermore, we used 95% confidence interval as a measure of uncertainty for all estimates of B, R1, and R2.
The segmented regression analyses were performed for (1) all individuals, (2) men and women separately, and (3) CYP2D6/CYP2C19 NMs and CYP2D6/CYP2C19 IM/PMs separately. That is, for citalopram, escitalopram, and sertraline, segmented regression analyses were performed for CYP2C19 NMs and CYP2C19 IMs/PMs separately, while for mirtazapine, segmented regression analyses were performed for CYP2D6 NMs and CYP2D6 IMs/PMs separately. Since metabolism of venlafaxine depend on both CYP2D6 and CYP2C19, individuals with normal vs reduced CYP-metabolism were separated into combined CYP2D6 and CYP2C19 NMs and individuals with all combinations of CYP2D6 and CYP2C19 NM/IM/PM, except for CYP2D6 and CYP2C19 NMs. UMs of the respective CYP enzyme(s) for each antidepressant were excluded, because the UM subgroups were too small to be included in the segmented regression analyses.
Median with interquartile range (IQR) was used to describe central tendency of age, dose, and sampling time because of extreme values in the study sample.
Stata IC version 16 (StataCorp llc, Statistical Software, College Station, TX, USA) was used for descriptive analyses, while R was used for estimation of breakpoint (B) and regression coefficients (R1 and R2) by segmented regression analyses, including Davies test.
Ethical considerations
The study was approved by the Regional Committee for Medical and Health Research Ethics (ref. 2018/655) and the Hospital Investigational Review Board.
Results
Patients and samples
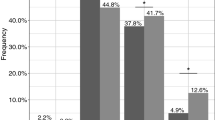
In all, 34,777 unique individuals were included in the analyses, where 12,385 (36%) were men. In the subgroup analysis according to genotype, 7,396 unique individuals were included, whereof 2740 (37%) were men. A flowchart of the inclusion and exclusion process is presented in Fig. 1, and patient characteristics for the different antidepressants are presented in Table 1.
Changes in C/D ratio related to age
For the five examined antidepressants, the change in the C/D ratio started between the age of 44 to 55 years (Table 2). The age of onset for an increased C/D ratio is denoted B (breakpoint in the segmented regression analysis) and is illustrated in Fig. 2. R1 and R2 show the annual change in log C/D ratio before and after age B, respectively. For all studied antidepressants, the log C/D ratio before age B did not change with increasing age, except for sertraline where a small decline in log C/D ratio with increasing age was observed, followed by an increase in slope after age B (Fig. 2). After B, the C/D ratio increased more rapidly for citalopram and escitalopram than for venlafaxine and mirtazapine, and a doubled C/D ratio was estimated at 79 and 80 years of age, respectively (Table 2; Appendix 1). For venlafaxine and mirtazapine, a doubled C/D ratio was estimated at 86 and 90 years of age. The yearly increase in C/D ratio was smaller for sertraline than for the other antidepressants.
Segmented regression analysis of patient age versus concentration-to-dose (CD)-ratio ((nmol/L)/mg) for citalopram (n = 2275), escitalopram (n = 16652), sertraline (n = 4461), venlafaxine (n = 5869), and mirtazapine (n = 5520). The break point identifies the age (years) where the C/D ratio starts to change direction, while the regression slopes identify the average annual change in C/D ratio before and after the break point on a log scale. CI, confidence interval
Differences between men and women
For escitalopram and venlafaxine, the age-related change in C/D ratio was observed 5–6 years earlier for women when compared with men. However, the increase in C/D ratio after age B was smaller in women when compared with men for both escitalopram and venlafaxine. Similar findings were observed for citalopram, despite somewhat overlapping confidence intervals (Table 3). For sertraline, the increase in C/D ratio seems to start later for women compared with men, but this finding is uncertain due to wide confidence intervals (Table 3). No difference between men and women was observed for mirtazapine (Table 3).
Differences related to genotype
For individuals with genotype available, the results regarding age of onset for increased C/D ratio were inconclusive. However, in spite of overlapping confidence intervals, a trend towards 6 to 9 years earlier increase in C/D ratio was observed for CYP2C19 IMs/PMs on escitalopram and combined CYP2C19/CYP2D6 IMs/PMs on venlafaxine (Table 4).
Discussion
Examining almost 35,000 serum concentration measurements from unique individuals in a TDM service in Norway, we observed that the C/D ratio for the studied antidepressants started to increase between the age 44 to 55 years. For citalopram, escitalopram, venlafaxine, and mirtazapine, the C/D ratio was increased with 100% at the age of 79 to 90 years. For sertraline, only modest changes in C/D ratio were observed, indicating that age is less important for the pharmacokinetics of sertraline than the other examined antidepressants.
The steepest annual increase in C/D ratio was found for citalopram and escitalopram, which were estimated to have threefold higher serum concentration at the age of 97 compared with middle-aged adults receiving the same doses. Currently, among the antidepressants examined, citalopram and escitalopram are the only drugs where recommendations on dose reduction for older people are included in the summary of product characteristics (SPC). In 2011, a recommendation was added to reduce the daily dose of citalopram/escitalopram by 50% to people ≥ 65 years, after post-marketing reports of cardiotoxic effects and increased attention regarding dose-related risk of QT-prolongation [15, 16]. Our results show that increasing concentration with the same dose is a continuous process and that instead of a cut-off at 65 years, dose reductions could be considered continuously, in particular at the oldest ages.
At present, for venlafaxine and mirtazapine, there are no recommendations regarding dose reduction in older people. Studies that examined the correlation between antidepressant doses and QT-prolongation concluded that the effect for venlafaxine and mirtazapine was negligible [17, 18]. However, an association between QTc prolongation and high serum concentration has been demonstrated for older people using venlafaxine, and cardiotoxic effect is reported in CYP2D6 PMs and in patients using CYP2D6 inhibitors [19, 20]. A case report of mirtazapine-induced long QT syndrome has also been described in an older patient using low-dose (15 mg) mirtazapine, and both venlafaxine and mirtazapine are classified as drugs with possible increased risk of QT time [21, 22]. It has been reported that a prolonged QT interval of ≥ 500 ms is associated with considerably increased mortality in hospitalized patients independent of comorbidity [23]. Older people are at increased risk not only because of the higher age but also because of the higher occurrence of hypokalemia and use of antiarrhythmic drugs [24]. Additionally, old age and high serum concentrations are risk factors for side effects such as hyponatremia and serotonin syndrome, as well as side effects that are more difficult to quantify [25,26,27]. Side effects of antidepressants may be difficult to unveil because of the similarity with the disease for which they are prescribed for, i.e., increased restlessness, anxiety, and aggression. Based on our findings of an increasing C/D ratio with increasing age, combined with the general higher risk of side effects in older people, TDM may be a valuable tool to personalize treatment with venlafaxine and mirtazapine for older patients.
When examining differences between men and women, the age-related change in C/D ratio started 5 to 6 years earlier for women compared with men using venlafaxine or escitalopram. However, when the C/D ratio starts to increase, the annual age-related increase in C/D ratio for venlafaxine seems to be higher in men compared with women. This indicates that eventually, within the oldest old, perhaps because of age-related pharmacokinetic effects, differences in C/D ratio related to sex may even out [28]. Furthermore, this also means that age may have an independent effect on the C/D ratio of antidepressants and that older people are in general at increased risk of high serum concentration. Sex hormones play a role in the pharmacokinetic variability of psychotropic drugs [29]. Potential use of contraceptives, menopausal changes in estrogen, and possible estrogen substitution make the assessments of age-related changes in C/D ratios more complex in women than in men.
It is important to note that the present results are exclusively based on the observed changes in the systemic serum concentrations with increasing age. Both differences in the distribution of drugs into the central nervous system (CNS) and pharmacodynamic differences between older and younger individuals may result in altered effects, or risk of side effects, despite similar serum concentrations. For instance, increased permeability of the blood–brain barrier and decreased activity of the P-glycoprotein may contribute to a higher CNS drug disposition and risk of side effects despite stable serum levels [30,31,32,33,34]. Concerning pharmacodynamic changes at old age, a general reduction in homeostatic mechanisms, as well as changes in levels of neurotransmitters, serotonin receptors, and transporters, is associated with a higher risk of side effects [30, 35, 36]. Altogether, based on the existing knowledge of age-related changes in pharmacokinetics and pharmacodynamics and the increased risk of side effects in older people, dose reductions to older people seem reasonable.
There are some limitations of this study that should be considered. The observed increase in C/D ratio with increasing age may be associated with impaired renal function. For example, the clearance of O-desmethylvenlafaxine is reported to decrease in renally impaired patients [37]. However, we did not have information regarding renal function for the patients. For the same reason, frailty and potential reductions in hepatic clearance could not be considered [7, 38]. Furthermore, smoking may increase CYP1A2 metabolism of mirtazapine, but smoking status was not available for the included patients [39]. Also, despite exclusion of samples to avoid interference caused by drug interactions, we cannot guarantee that such bias is avoided as drugs for which TDM had not been requested could not be taken into account. Unfortunately, we did not have access to complete medication lists of the included patients. Increasing age is associated with increasing number of drugs, which could lead to more drug interactions. However, we were not able to separately describe the effect that reduced renal and hepatic function, comorbidities, or increased number of concomitant drugs may have had on the increase in C/D ratio. Indeed, the regression slopes for citalopram and escitalopram were particularly steep, and it cannot be excluded that the extensive use of the CYP2C19 inhibitor omeprazole at high ages may have contributed to this finding [40]. Furthermore, when considering differences between individuals with normal versus reduced metabolic capacity, the sample sizes were not large enough to perform separate analyses for individuals with IM and PM genotype-predicted phenotype. Nevertheless, a strength of the present study is the large number of individuals which made it possible to examine not only differences in C/D ratio between older and younger individuals but also the age where these changes begin and how these changes proceed with increasing age.
Conclusion
The present study, based on TDM data, shows that the age-related increase in antidepressant C/D ratio on average appeared already in middle-aged adults and progressed up to more than doubled C/D ratios in the oldest old. Sertraline seems to be less prone to age-related changes in C/D ratio than the other antidepressants. Although the therapeutic reference range is large for these substances, the increasing C/D ratio by age could be worthwhile considering in the treatment of older patients.
Data availability
The data of this study are available from the corresponding author upon reasonable request.
References
Waade RB et al (2012) Serum concentrations of antidepressants in the elderly. Ther Drug Monit 34(1):25–30
Hansen MR et al (2017) Therapeutic drug monitoring of venlafaxine in an everyday clinical setting: analysis of age, sex and dose concentration relationships. Basic Clin Pharmacol Toxicol 121(4):298–302
Hermann M, Waade RB, Molden E (2015) Therapeutic drug monitoring of selective serotonin reuptake inhibitors in elderly patients. Ther Drug Monit 37(4):546–549
Hiemke C et al (2018) Consensus Guidelines for Therapeutic Drug Monitoring in Neuropsychopharmacology: Update 2017. Pharmacopsychiatry 51(1–02):9–62
Fried LP et al (2021) The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging 1(1):36–46
Tveit K et al (2020) Use of antidepressants in older people during a 10-year period: an observational study on prescribed doses and serum levels. Drugs Aging 37(9):691–701
Mangoni AA, Jackson SH (2004) Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol 57(1):6–14
Bigos KL et al (2009) Sex differences in the pharmacokinetics and pharmacodynamics of antidepressants: an updated review. Gend Med 6(4):522–543
Bousman CA et al (2023) Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6, CYP2C19, CYP2B6, SLC6A4, and HTR2A genotypes and serotonin reuptake inhibitor antidepressants. Clin Pharmacol Ther 114(1):51–68
Störmer E et al (2000) Metabolism of the antidepressant mirtazapine in vitro: contribution of cytochromes P-450 1A2, 2D6, and 3A4. Drug Metab Dispos 28(10):1168–1175
Kringen MK et al (2020) The influence of combined CYP2D6 and CYP2C19 genotypes on venlafaxine and O-desmethylvenlafaxine concentrations in a large patient cohort. J Clin Psychopharmacol 40(2):137–144
Karlsson L et al (2015) Influence of CYP2D6 and CYP2C19 genotypes on venlafaxine metabolic ratios and stereoselective metabolism in forensic autopsy cases. Pharmacogenomics J 15(2):165–171
Brouwer JM et al (2022) Dutch Pharmacogenetics Working Group (DPWG) guideline for the gene-drug interaction between CYP2C19 and CYP2D6 and SSRIs. Eur J Hum Genet 30(10):1114–1120
Muggeo V (2008) Segmented: An R package to fit regression models with broken-line relationships. R News 8(1)
Safety concerns: escitalopram — risk of QT interval prolongation. Monthly report : 1111 2011 24. November [cited 2019 15 Mar]; Available from: https://www.ema.europa.eu/en/documents/report/monthly-report-pharmacovigilance-working-party-phvwp-november-2011-plenary-meeting_en.pdf.
Safety concerns: citalopram — risk of QT interval prolongation. Monthly report : 1110 2011 27. Oct [cited 2019 15 Mar]; Available from: https://www.ema.europa.eu/en/documents/report/monthly-report-pharmacovigilance-working-party-phvwp-october-2011-plenary-meeting_en.pdf.
Castro VM et al (2013) QT interval and antidepressant use: a cross sectional study of electronic health records. BMJ 346:f288
Jasiak NM, Bostwick JR (2014) Risk of QT/QTc prolongation among newer non-SSRI antidepressants. Ann Pharmacother 48(12):1620–1628
Hefner G et al (2019) QTc time correlates with amitriptyline and venlafaxine serum levels in elderly psychiatric inpatients. Pharmacopsychiatry 52(01):38–43
Lessard É et al (1999) Influence of CYP2D6 activity on the disposition and cardiovascular toxicity of the antidepressant agent venlafaxine in humans. Pharmacogenetics 9(4):435–443
Matsuda Y et al (2020) Mirtazapine-induced long QT syndrome in an elderly patient: a case report. Psychogeriatrics 20(4):536–537
Danielsson B et al (2016) Antidepressants and antipsychotics classified with torsades de pointes arrhythmia risk and mortality in older adults-a Swedish nationwide study. Br J Clin Pharmacol 81(4):773–783
Gibbs C et al (2019) QT prolongation predicts short-term mortality independent of comorbidity. EP Europace 21(8):1254–1260
Vandael E et al (2017) Risk factors for QTc-prolongation: systematic review of the evidence. Int J Clin Pharm 39(1):16–25
Davies E, Mahony MO (2015) Adverse drug reactions in special populations—the elderly. Br J Clin Pharmacol 80(4):796–807
Filippatos TD et al (2017) Hyponatremia in the elderly: challenges and solutions. Clin Interv Aging 12:1957–1965
Wang RZ et al (2016) Serotonin syndrome: preventing, recognizing, and treating it. Cleve Clin J Med 83(11):810–817
Unterecker S et al (2012) The effect of age, sex, smoking and co-medication on serum levels of venlafaxine and O-desmethylvenlafaxine under naturalistic conditions. Pharmacopsychiatry 45(06):229–235
Brand BA et al (2022) Antipsychotic medication for women with schizophrenia spectrum disorders. Psychol Med 52(4):649–663
Trifiro G, Spina E (2011) Age-related changes in pharmacodynamics: focus on drugs acting on central nervous and cardiovascular systems. Curr Drug Metab 12(7):611–620
Bauer M et al (2009) Age dependency of cerebral P-gp function measured with (R)-[11C] verapamil and PET. Eur J Clin Pharmacol 65(9):941–946
van Assema DM et al (2012) P-glycoprotein function at the blood–brain barrier: effects of age and gender. Mol Imag Biol 14(6):771–776
O’Brien FE et al (2012) Interactions between antidepressants and P-glycoprotein at the blood–brain barrier: clinical significance of in vitro and in vivo findings. Br J Pharmacol 165(2):289–312
Dalla C et al (2022) Sex differences in blood–brain barrier transport of psychotropic drugs. Front Behav Neurosci 16
Lotrich FE, Pollock BG (2005) Aging and clinical pharmacology: implications for antidepressants. J Clin Pharmacol 45(10):1106–1122
Fidalgo S, Ivanov DK, Wood SH (2013) Serotonin: from top to bottom. Biogerontology 14(1):21–45
Nichols AI et al (2011) The pharmacokinetics and safety of desvenlafaxine in subjects with chronic renal impairment. Int J Clin Pharmacol Ther 49(1):3–13
Mangoni AA, Jarmuzewska EA (2021) Incorporating pharmacokinetic data into personalised prescribing for older people: challenges and opportunities. Eur Geriatr Med 12(3):435–442
Lind AB et al (2009) Steady-state concentrations of mirtazapine, N-desmethylmirtazapine, 8-hydroxymirtazapine and their enantiomers in relation to cytochrome P450 2D6 genotype, age and smoking behaviour. Clin Pharmacokinet 48(1):63–70
Wallerstedt SM et al (2017) Long-term use of proton pump inhibitors and prevalence of disease- and drug-related reasons for gastroprotection-a cross-sectional population-based study. Pharmacoepidemiol Drug Saf 26(1):9–16
Funding
Open access funding provided by Diakonhjemmet Hospital. Kristine Hole was supported by a grant from the ERA PerMed to the ArtiPro project (ERAPERMED2021-357).
Author information
Authors and Affiliations
Contributions
KT, MH, and EM designed the study. KH extracted the data from the TDM database. KT and RMN analyzed the data. KT drafted the manuscript. All authors contributed to the interpretation of the results and the revision of the manuscript for intellectual content. All authors gave their final approval for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The use of pseudonymized patient data for the purpose of this study was approved by the Regional Committee for Medical and Health Research Ethics (ref. 2018/655) and the Diakonhjemmet Hospital Investigational Review Board.
Consent to participate and consent to publish
Since the study was based on existing data retrospectively retrieved from a routine TDM service, ethical approval was granted without the requirement of patient consent.
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1
Appendix 1
Formula for calculation of increase in dose-adjusted serum concentration (C/D ratio).
-
1.
Let \(B\) represent the age where the C/D ratio starts to change direction on the log scale in the segmented regression (the breakpoint). At any age \(x\le B\) (first segmented line), we have the following regression line describing the log C/D ratio:
$$\log{(Y_1)}=A+R1\cdot x$$(1)where \(A\) is the intercept and \(R1\) is the slope coefficient for age \(x\).
-
2.
We use Eq. 1 to estimate the log C/D ratio at the breakpoint age \(B\):
$${\text{log}}\left({Y}_{B}\right)= A + R1\cdot B$$(2) -
3.
At any age \(x \ge B\) (second segmented line), we have the following regression line describing the log C/D ratio:
$$\log{(Y_x)} = A + R1\:\cdot B\: + R2 \cdot (x-B)$$(3)where \(R2\) is the slope coefficient for age \(x\).
-
4.
We then subtract Eq. 2 from 3, which provides us with the difference in log C/D ratio between age x and the breakpoint age B. The subtraction of equations further simplifies to:
$${\text{log}}(\frac{{Y}_{x}}{{Y}_{B}})=R2\cdot (x-B)$$(4)where age \(x \ge B\)
-
5.
Because the ratio \(\frac{{Y}_{x}}{{Y}_{B}}\) is always \(\ge 1\) in our data, we can write this ratio as \(1 +\frac{pct}{100}\), where \(pct\) is the percentage increase in C/D ratio from age \(B\) on the standard C/D ratio scale. Solving Eq. 4 for age \(x\), we obtain the following expression:
$$x=\frac{{\text{log}}\left(1+\frac{pct}{100}\right)+R2\cdot B}{R2}$$(5)Hence, using Eq. 5, we can estimate the age \(x\) at which the C/D ratio is increased by a given \(pct\) (on the standard scale) from breakpoint \(B\).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tveit, K., Hermann, M., Nilsen, R.M. et al. Age of onset for increased dose-adjusted serum concentrations of antidepressants and association with sex and genotype: An observational study of 34,777 individuals. Eur J Clin Pharmacol 80, 435–444 (2024). https://doi.org/10.1007/s00228-023-03611-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-023-03611-3