Abstract
Aims
The purpose of this study is to investigate the regulation of adipose tissue insulin resistance with DPP-4 inhibitors in treatment-naive subjects with T2DM and to examine its relation to other diabetic parameters.
Subjects and methods
A total of 147 subjects were treated with alogliptin 12.5–25 mg/day (n = 55), sitagliptin 25–50 mg/day (n = 49), or teneligliptin 10–20 mg/day (n = 43) monotherapy for 3 months. Changes in adipo-IR, a mathematical model used to evaluate adipose tissue insulin resistance, and various diabetic parameters were analyzed in this prospective, non-randomized observational study.
Results
Among these three drugs, only alogliptin significantly reduced adipo-IR (−25.9%, p < 0.004) and some lipid parameters, such as LDL-C, T-C/HDL-C, log(TG)/HDL-C, non-HDL-C/HDL-C, and LDL-C/HDL-C. Subjects in the alogliptin group were divided into two groups with distinct changes in adipo-IR. Group A had a significant decrease in adipo-IR (−56.5%, p < 0.00001, n = 28), whereas group B had an insignificant increase (19.1%, p = 0.055, n = 27). Significant reductions in FBG or HbA1c were observed in groups A and B, respectively. Group A also showed significant reductions in HOMA-R, T-C/HDL-C, TG, log(TG)/HDL-C, non-HDL-C/HDL-C, LDL-C/HDL-C, and FFA, as well as increases in QUICKI or HDL-C. In contrast, group B showed significant reductions in QUICKI or LDL-C, and increases in HOMA-R, insulin, HOMA-B, C-peptide, or CPR-index.
Conclusions
In contrast to other tested DPP-4 inhibitors, alogliptin demonstrated the ability to down-regulate insulin resistance in adipose tissue, as well as certain atherogenic lipids. This study provides the initial evidence of a DPP-4 inhibitor’s potential to regulate adipose tissue insulin resistance. Furthermore, adipo-IR is associated with non-LDL-C lipid parameters instead of glycemic control in those receiving alogliptin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dipeptidyl peptidase-4 (DPP-4) inhibitors are oral hypoglycemic agents that belong to incretin-based therapy and are extensively utilized in the management of type 2 diabetes mellitus (T2DM) [1]. Although all drugs in this class inhibit the same enzyme (DPP-4) and exhibit similar glucose-lowering efficacies, they exhibit distinct chemical structures and pharmacological properties, implying differential non-glycemic efficacies [2, 3].
Some researchers have referred to T2DM as diabetes lipidus [4, 5], given that many patients with T2DM have disrupted lipid profiles. Current guidelines advocate aggressive treatment of low-density lipoprotein cholesterol (LDL-C) with statins [6]. In addition to LDL-C, T2DM is often associated with non-LDL dyslipidemia (such as decreased high-density lipoprotein cholesterol [HDL-C], elevated triglycerides [TG], or non-HDL-C), which has been demonstrated to increase cardiovascular risks, even when LDL-C is low [7, 8]. Although DPP-4 inhibitors are generally considered neutral with respect to lipid or body weight [2, 3], our previous report demonstrated that alogliptin, a quinazolinone-based, non-covalent drug in this class, can down-regulate some atherogenic lipids and increase body weight in lean subjects [7].
One organ that links glucose metabolism with lipid and weight is adipose tissue, where insulin enhances triglyceride synthesis and/or suppresses the release of free fatty acids (FFA) and glycerol into circulation [8]. This insulin-mediated lipolysis suppression is down-regulated in the presence of increased insulin resistance [8]. Enhanced FFA release has been demonstrated to impair beta-cell function (lipotoxicity), insulin signal transduction, or glucose-stimulated insulin response [9, 10]. Such metabolic dysregulations may further contribute to the impairment of whole-body insulin sensitivity and metabolism. Previous research has shown that adipose tissue insulin resistance increases from healthy to impaired glucose tolerance to T2DM in association with declining beta-cell function [11, 12]. Nevertheless, it remains to be determined whether adipose tissue insulin resistance is directly responsible for glycemic efficacy during diabetes treatment. The methods of measuring adipose tissue insulin resistance are based on insulin-mediated suppression of adipose tissue lipolysis [12, 13]. The inhibition of FFA during the multi-step euglycemic-hyperinsulinemic clamp may be considered the “gold standard” to measure adipose tissue insulin sensitivity in vivo. However, adipo-IR, a simple equation of “fasting plasma FFA x insulin,” has been shown to possess good correlation with multi-step euglycemic-hyperinsulinemic clamp [12, 13].
Although some hypoglycemic drugs, such as thiazolidinedione (TZD, pioglitazone) or sodium-glucose cotransporter 2 (SGLT-2) inhibitors, have been shown to regulate adipose tissue insulin resistance evaluated with adipo-IR [13,14,15], no DPP-4 inhibitor has been demonstrated to regulate this parameter thus far. In this report, we demonstrate that alogliptin, but not other drugs in this class (sitagliptin or teneligliptin), can down-regulate adipo-IR as well as some atherogenic lipids. Further investigations will be carried out to establish the link between adipose tissue insulin resistance and glycemic/non-glycemic parameters.
Subjects and methods
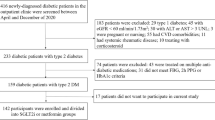
Subjects
Inclusion criteria for this study comprised of individuals who were either newly diagnosed with type 2 diabetes mellitus (T2DM) or previously diagnosed but untreated. These individuals did not receive any prescribed medications within the last 6 months prior to the study. Exclusion criteria included clinically significant renal impairment (serum creatinine > 1.5 mg/dl), hepatic dysfunction (glutamic oxalacetic transaminases/glutamic pyruvic transaminases [AST/ALT] > 70/70 IU/L), history of heart disorders, severe hypertension (systolic blood pressure > 160 mm Hg and/or diastolic blood pressure > 100 mm Hg), type 1 diabetes mellitus (T1DM), and pregnancy. The subjects received either 12.5 mg/day (for females, n = 13) or 25 mg/day (for males, n = 42) of alogliptin, 25 mg/day (for females, n = 13) or 50 mg/day (for males, n = 36) of sitagliptin, or 10 mg/day (for females, n = 14) or 20 mg/day (for males, n = 29) of teneligliptin as monotherapy. No other drugs were administered. The subjects were not strictly randomized; hence, this study was non-randomized and observational, comparing the effects of three different dipeptidyl peptidase-4 (DPP-4) inhibitors. All patients gave their informed consent, which was stored in the electronic medical record system. The study protocol was approved by the Ethical Committee/Institutional Review Board of Gyoda General Hospital and Kumagaya Surgical Hospital. This study was conducted following the principles of the Helsinki Declaration and Good Clinical Practice.
Laboratory measurements
The primary endpoint of this study was to investigate changes in adipose tissue insulin resistance (assessed with adipo-IR) from baseline to 3 months. The secondary endpoints included changes in fasting blood glucose (FBG), glycated hemoglobin (HbA1c), insulin, C-peptide, homeostatic model assessment of insulin resistance (HOMA-R), homeostatic model assessment of beta-cell function (HOMA-B), quantitative insulin sensitivity check index (QUICKI), C-peptide response index (CPR-index), total cholesterol (T-C), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), T-C/HDL-C ratio, non-HDL-C, non-HDL-C/HDL-C ratio, log(TG)/HDL-C ratio, non-LDL-C, LDL-C/HDL-C ratio, uric acid (UA), free fatty acid (FFA), and body mass index (BMI) from baseline to 3 months. Blood samples were collected in the morning hours after an overnight fast. HbA1c and FBG levels were measured once a month, whereas TC, TG, HDL-C, LDL-C, insulin, C-peptide, and FFA levels were measured at baseline and at the end of the study. Non-HDL-C was calculated as T-C minus HDL-C. Antiglutamic acid decarboxylase (GAD) antibody was measured in some patients to exclude those with T1DM. HOMA-R, HOMA-B, QUICKI, CPR-index, and adipo-IR were calculated as described previously [16,17,18].
Data analyses
The statistical analysis was conducted using the PAST program, which is available from the University of Oslo (https://folk.uio.no/ohammer/past/). An analysis of variance (ANOVA) was utilized to investigate differences in baseline characteristics among the three drug groups. For within-group differences, paired Student’s t-tests were employed when the data were normally distributed, whereas the Wilcoxon signed-rank test was utilized when the data did not follow a normal distribution. If applicable, an analysis of covariance (ANCOVA) was conducted to investigate inter-group differences. Multiple regression analysis was performed to identify factors associated with changes in adipose tissue insulin resistance, as measured by adipo-IR, after alogliptin administration. Throughout the statistical analyses, p-values less than 0.05 were considered statistically significant. Results with p-values between 0.05 and 0.1 were deemed statistically insignificant but suggestive of possible differences or correlations [19].
Results
Baseline characteristics and changes of glycemic/non-glycemic parameters at 3 months with DPP-4 inhibitors; alogliptin, sitagliptin, and teneligliptin
The baseline characteristics of these parameters were similar across the three drug groups, and no significant differences were observed (see Table 1 for details of each value and statistical significance). After 3 months of treatment, all three drug groups exhibited significant reductions in FBG and HbA1c, as well as increases in HOMA-B, CPR-index, and UA (Table 2A–C). However, distinct regulatory patterns were observed in other parameters. Specifically, the alogliptin group exhibited significant reductions in adipo-IR (−25.9%) and several atherogenic lipid parameters, including LDL-C (−7.8%), T-C/HDL-C (−6.8%), log(TG)/HDL-C (−6.8%), non-HDL-C/HDL-C (−8.7%), and LDL-C/HDL-C (−11.2%) (Table 2A). Non-HDL-C also showed a tendency to decrease (−4.8%, p = 0.073). In contrast, no significant changes were observed in these parameters in the sitagliptin or teneligliptin groups (Table 2B, C), except for a non-significant increase in BMI with sitagliptin (p = 0.071, Table 2B).
Regulations of adipose tissue insulin resistance with alogliptin
As mentioned earlier, significant reductions in adipo-IR were observed with alogliptin (Table 2A), whereas no such reductions were observed with sitagliptin or teneligliptin (Table 2B, C). To investigate this issue further, a simple regression analysis was performed between changes (Δ) and baseline adipo-IR. As shown in Fig. 1A, significant negative correlations were observed between these parameters with alogliptin, while no such correlations were noted with sitagliptin or teneligliptin (Fig. 1B, C).
To identify any factors responsible for the changes in adipo-IR during treatment with alogliptin, a multiple regression analysis was performed, as described in the “Subjects and methods” section. The following independent variables, including baseline levels of adipo-IR, age, FBG, BMI, T-C, TG, HDL-C, HOMA-R, HOMA-B, and BMI, were employed. Among these factors, TG was identified as the significant factor responsible for changes in (Δ) adipo-IR with alogliptin (Table 3). Simple regression analysis indicated that insignificant correlations were observed between Δadipo-IR and baseline TG levels (R = 0.232, p = 0.088, results not shown in the table).
Associations between adipose tissue insulin resistance and glycemic/non-glycemic parameters
To examine the associations among adipose tissue insulin resistance and glycemic/non-glycemic parameters while undergoing alogliptin treatment, a straightforward regression analysis was conducted by juxtaposing the baseline and changes (Δ) of adipo-IR with those of glycemic/non-glycemic parameters.
-
(A)
Table 4A: significant correlations were identified between the baseline levels of adipo-IR and HOMA-R (R = 0.96), T-C/HDL-C (R = 0.327), non-HDL-C (R = 0.337), log(TG)/HDL-C (R = 0.323), non-HDL-C/HDL-C (R = 0.327), UA (R = 0.422), insulin (R = 0.997), HOMA-B (R = 0.797), C-peptide (R = 0.829), CPR-index (R = 0.629), and BMI (R = 0.481). Conversely, significant negative correlations were observed between the baseline levels of adipo-IR and age (R = −0.279) or QUICKI (R = −0.811). There were insignificant correlations between the baseline levels of adipo-IR and FBG (R = 0.247, p = 0.069), TG (R = 0.224, p = 0.098), and LDL-C/HDL-C (R = 0.234, p = 0.085).
Table 4 Correlations between adipo-IR and diabetic parameters. Simple regression analysis was performed between adipo-IR and indicated parameters at baseline and at 3 months treatment of alogliptin -
(B)
Table 4B: significant correlations were shown between the changes (Δ) of adipo-IR and HOMA-R (R = 0.691), log(TG)/HDL-C (R = 0.266), insulin (R = 0.797), HOMA-B (R = 0.276), C-peptide (R = 0.398), and FFA (R = 0.407). Conversely, significant negative correlations were observed between the changes (D) of adipo-IR and QUICKI (R = −0.501). Nearly significant correlations were observed between the changes (Δ) of adipo-IR and T-C/HDL-C (R = 0.262, p = 0.053), non-HDL-C/HDL-C (R = 0.262, p = 0.053), or LDL-C/HDL-C (R = 0.247, p = 0.07). There were insignificant negative correlations between the changes (Δ) of adipo-IR and HDL-C (R = −0.231, p = 0.089).
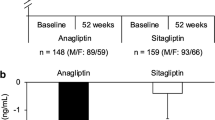
Differential regulations of glycemic/non-glycemic parameters between subjects with distinct changes of adipo-IR with alogliptin
To investigate the physiological implications of changes in adipose tissue insulin resistance following treatment with alogliptin, this study compared the alterations in glycemic and non-glycemic parameters between two distinct groups classified by their changes in adipo-IR (Δ). The subjects were divided into two groups with similar sample sizes, namely group A (Δadipo-IR = −56.5%, p < 0.00001, n = 28) and group B (Δadipo-IR = 19.1%, p = 0.055, n = 27), as shown in Fig. 2. Both groups exhibited significant reductions in FBG (−14.1%, −15.5%) or HbA1c (10.26 to 8.93%, 11.04 to 9.08%), and increases in UA (9.8%, 13.8%) for groups A and B, respectively (refer to Table 5A, B). No significant inter-group differences were observed in these parameters (results not shown in the table).
In group A (refer to Table 5A), significant reductions were observed in HOMA-R (−25.7%), T-C/HDL-C ratio (−10.3%), TG (−18.1%), log(TG)/HDL-C (−11.3%), non-HDL-C/HDL-C (−13.1%), LDL-C/HDL-C ratio (−12.8%), and FFA (−28.9%). Moreover, increases in QUICKI (5.9%) and HDL-C (6.9%) were observed. There were insignificant reductions in LDL-C (−6.68%, p = 0.064) and increases in C-peptide (19.4%, p = 0.072).
In group B (refer to Table 5B), significant reductions were observed in QUICKI (−3.8%) and LDL-C (−9.2%), while increases were observed in HOMA-R (28.4%), insulin (55.1%), HOMA-B (106.3%), C-peptide (16.5%), and CPR-index (39.8%). LDL-C/HDL-C ratio tended to decrease (−9.1%, p = 0.067), while FFA tended to increase (13.8%, p = 0.07).
Discussion
Regulation of atherogenic lipids with alogliptin
Alogliptin demonstrated the ability to down-regulate atherogenic lipids, including log(TG)/HDL-C, T-C/HDL-C, or LDL-C/HDL-C, as well as LDL-C, non-HDL-C, or non-HDL-C/HDL-C, which has been previously established (Table 1, reference 7). However, other DPP-4 inhibitors, such as sitagliptin or teneligliptin, tested in Table 2B, C, did not exhibit the same effect. The residual cardiometabolic risks and loss of beta-cell function have been linked to log(TG)/HDL-C [20, 21], whereas T-C/HDL-C and LDL-C/HDL-C have been deemed as strong predictors of cardiovascular events [22]. Recent studies on the cardiovascular safety of DPP-4 inhibitors have raised concerns about an increased risk of hospitalization for heart failure [23]. However, alogliptin did not increase the risk of hospitalization for heart failure [24, 25]. Additionally, alogliptin has been shown to reduce atherosclerosis, inflammation, and coronary plaque [26, 27]. While not yet proven, the down-regulation of atherogenic lipids by alogliptin may have contributed to its neutral results on the risk of heart failure [24, 25]. Further investigation is required to provide a definitive answer to this question.
Regulation of adipose tissue insulin resistance with alogliptin
The results demonstrate that alogliptin significantly reduced adipo-IR (Table 2A), while sitagliptin or teneligliptin did not show the same effect (Table 2B, C). To date, no reports have investigated the impact of DPP-4 inhibitors on adipose tissue insulin resistance. Moreover, significant negative correlations were observed between the changes (Δ) and baseline adipo-IR (Fig. 1A) for alogliptin, but not for sitagliptin or teneligliptin (Fig. 1B, C). These findings suggest that the regulation of adipo-IR by alogliptin is specific and dependent on the baseline adipo-IR level. In summary, alogliptin is a unique DPP-4 inhibitor that regulates adipose tissue insulin resistance, and further research is needed to evaluate its clinical significance in relation to other clinical measures.
FFA flux is the primary contributor to the VLDL (very low-density lipoprotein)-TG pools for fatty acid metabolism [28, 29]. Therefore, it is plausible that adipose tissue insulin resistance is a contributing factor to TG levels. The baseline TG was identified as a significant contributing factor to the change of adipo-IR with alogliptin (Table 3). To support this result, correlations were observed between the changes in adipo-IR and baseline TG (R = 0.232, p = 0.088, results not presented in the table), indicating that those with higher baseline TG levels have greater potential for lowering adipo-IR with this DPP-4 inhibitor.
Link between adipose tissue insulin resistance and non-LDL atherogenic lipids or other parameters
Significant or near-significant associations between baseline or changes in adipo-IR and non-LDL-C lipids such as T-C/HDL-C, log(TG)/HDL-C, or non-HDL-C/HDL-C (Table 4A, B) suggest that adipose tissue insulin resistance is linked to some of the non-LDL-C atherogenic lipids during treatment with alogliptin. Notably, significant negative correlations between adipo-IR and age indicate that younger subjects exhibit greater degrees of adipose tissue insulin resistance. Furthermore, our data demonstrate a significant correlation between adipo-IR and UA or BMI (Table 4A), highlighting a physiological link between these parameters. Generally, younger patients tend to be more obese, resulting in elevated insulin resistance in adipose tissue. UA has been previously linked to body weight and is also produced in adipose tissue [30]. Surprisingly, we did not observe any correlations between changes in adipo-IR and BMI or UA (Table 4). This contrasts with other medications that have demonstrated links between these three parameters [14, 15]. The physiological significance of this unexpected finding warrants further investigation.
Is reduction of adipo-IR linked to glycemic efficacy during treatment with alogliptin?
Previous reports have demonstrated that glucose uptake in adipose tissues, including both abdominal and subcutaneous regions, has strong correlations with whole-body insulin sensitivity and is decreased in individuals with pre-diabetes or type 2 diabetes [31]. Similarly, in this study, we observed robust positive/negative correlations between adipo-IR and HOMA-R/QUICKI (Table 4A). While certain indexes for insulin resistance such as HOMA-R, QUICKI, or Matsuda index have been commonly used to evaluate the glycemic effectiveness of patients with diabetes, there have only been two reports to date examining adipose tissue insulin resistance in the natural history of type 2 diabetes (the transition from normal glucose tolerance to impaired glucose tolerance/type 2 diabetes in obese adolescent and adult populations) [11, 12]. These reports indicated that adipose tissue insulin resistance increased from healthy to impaired glucose tolerance to type 2 diabetes in association with declining beta-cell function [11, 12]. However, these reports did not directly confirm the role of adipose tissue insulin resistance in glycemic control in individuals with type 2 diabetes. Therefore, in this study, we aimed to investigate whether adipose tissue insulin resistance, as assessed by adipo-IR, is directly involved in glycemic effectiveness during treatment with diabetes drugs.
Our results indicate that (1) no correlations were observed between baseline levels of FBG/HbA1c and adipo-IR (Table 4A); (2) no correlations were observed between changes in FBG/HbA1c and adipo-IR (Table 4B); and (3) similar reductions in FBG/HbA1c were observed in two groups with distinct changes in adipo-IR (groups A and B, Table 5A, B). Although not presented in this manuscript, patients were divided into three groups of similar size based on changes in adipo-IR. The change in glycemic/non-glycemic parameters in the lowest tertile of changes in adipo-IR (−62.6%, p < 0.00002) was compared to that in the highest tertile of changes in adipo-IR (28.9%, p < 0.01). Similar reductions in FBG and HbA1c were observed in these two extreme groups (results not shown). Taken together, these findings suggest that adipose tissue insulin resistance is likely not involved in glycemic effectiveness, at least with this DPP-4 inhibitor. The question of whether adipose tissue insulin resistance provides additional predictive information beyond whole-body insulin resistance needs to be investigated in future studies using tracer protocols (for adipose tissue insulin resistance) and euglycemic-hyperinsulinemic clamp studies (for whole-body insulin sensitivity).
Competition of insulin resistance and beta-cell function in the glycemic efficacy of alogliptin
Increases in insulin resistance, as evaluated using adipo-IR, HOMA-R, or QUICKI, were observed in group B, while group A showed a decrease. Despite this difference, similar glycemic efficacies were observed in both groups, as evidenced by FBG and HbA1c levels (refer to Table 5A, B). In group B, an enhancement of beta-cell function, assessed by HOMA-B or CPR-index, was observed (refer to Table 5B). An explanation for this unexpected finding could be that beta-cell function is activated in response to the deterioration of insulin resistance in group B, either in adipose tissue or the whole body. This hypothesis is supported by the significant correlations observed between the baseline/changes of adipo-IR and those of HOMA-B (refer to Table 4B). Additionally, significant correlations were observed between the baseline/changes of HOMA-R and those of HOMA-B, even though this information is not presented in the table. These findings suggest that a “brake and accelerator mechanism” is at play simultaneously in group B, with insulin resistance acting as the brake and beta-cell function as the accelerator. As the subjects in this study are still in the early stages of the disease, where beta-cell function is still preserved, it remains to be seen whether this mechanism will prove to be a burden on beta-cell function in the long term. In light of these results, drugs that may reduce this burden could prove useful.
Limitations and strengths of the study
This present study is subject to certain drawbacks and limitations. Firstly, it is an observational study that included a small number of subjects and had a short study duration. However, given the design of the protocol (monotherapy in drug-naive subjects), it is likely that the observed results were caused by the drugs used. To strengthen the findings of this study, randomized, double-blind, placebo-controlled studies with a longer duration and a larger sample size will be necessary. It should be noted that caution may be required when using the adipo-IR index in patients with severe fasting hyperglycemia, in whom marked insulin deficiency may be present. Nevertheless, it is important to highlight that the subjects in this study were mostly newly diagnosed patients with T2DM who had sufficient beta-cell function.
Conclusion
The data presented in this study suggest that alogliptin has the potential to impact adipose tissue insulin resistance (adipo-IR), whereas sitagliptin or teneligliptin did not show such an effect. Notably, a baseline-dependent down-regulation of adipo-IR was observed with alogliptin, which is the first report to demonstrate that a DPP-4 inhibitor regulates adipose tissue insulin resistance. Additionally, this drug was found to decrease atherogenic lipids, such as LDL-C, log(TG)/HDL-C, T-C/HDL-C, LDL-C, or non-HDL-C/HDL-C, and significant or nearly significant correlations were observed between the baseline/changes of adipo-IR and those of T-C/HDL-C, log(TG)/HDL-C, or non-HDL-C/HDL-C (but not LDL-C), indicating a potential link between adipose tissue insulin resistance and the metabolism or regulation of non-LDL-C parameters. Conversely, the lack of correlations between the baseline/changes of adipo-IR and glycemic parameters (FBG/HbA1c) suggests that adipo-IR is not involved in the glycemic efficacy of alogliptin treatment. Furthermore, the division of subjects into two groups with distinct changes of adipo-IR revealed that the glycemic efficacy of alogliptin is determined by modulation of insulin resistance and beta-cell function.
Data availability
Data underlying the findings described in this manuscript may be obtained from the first author (EK) upon reasonable request.
Abbreviations
- T2DM:
-
Type 2 diabetes
- DPP-4:
-
Dipeptidyl peptidase 4
- adipo-IR:
-
Adipose tissue insulin resistance
- FBG:
-
Fasting blood glucose
- HOMA-R:
-
Homeostasis model assessment-R
- HOMA-B:
-
Homeostasis model assessment-B
- QUICKI:
-
The quantitative insulin sensitivity check
- CPR-index:
-
C-peptide index
- T-C:
-
Total cholesterol
- TG:
-
Triglyceride
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- FFA:
-
Free fatty acids
- UA:
-
Uric acid
- BMI:
-
Body mass index
References
Deacon CF, Holst JJ (2002) Dipeptidyl peptidase IV inhibition as an approach to the treatment and prevention of type 2 diabetes: a historical perspective. Biochem Biophys Res Commun 294(1):1–4
Ceriello A, Sportiello L, Rafaniello C, Rossi F (2014) DPP-4 inhibitors: pharmacological differences and their clinical implications. Expert Opin Drug Saf 13(Suppl 1):S57-68
Filippatos TD, Athyros VG, Elisaf MS (2014) The pharmacokinetic considerations and adverse effects of DPP-4 inhibitors [corrected]. Expert Opin Drug Metab Toxicol 10(6):787–812
Shafrir E, Raz I (2003) Diabetes: mellitus or lipidus? Diabetologia 46(3):433–440
Björntorp P, Shafrir E, Raz I (2003) For debate. Diabetes: mellitus or lipidus? Diabetologia 46(11):1586–1587
Hermans MP, Ahn SA, Rousseau MF (2021) Lipid and cardiometabolic features of T2DM patients achieving stricter LDL-C and non-HDL-C targets in accordance with ESC/EAS 2019 guidelines. Acta Cardiol 76(4):375–383
Kutoh E, Kaneoka N, Hirate M (2015) Alogliptin: a new dipeptidyl peptidase-4 inhibitor with potential anti-atherogenic properties. Endocr Res 40(2):88–96. https://doi.org/10.3109/07435800.2014.952743. (Epub 2014 Sep 10 PMID: 25208188)
Carpentier AC (2021) 100th anniversary of the discovery of insulin perspective: insulin and adipose tissue fatty acid metabolism. Am J Physiol Endocrinol Metab 320(4):E653–E670
Girard J (2003) Rôle des acides gras libres dans la sécrétion et l’action de l’insuline: mécanismes de la lipotoxicité [Contribution of free fatty acids to impairment of insulin secretion and action: mechanism of beta-cell lipotoxicity]. Med Sci (Paris) 19(8–9):827–833
Kutoh E, Wada A, Hayashi J (2018) Regulation of free fatty acid by sitagliptin monotherapy in drug-naïve subjects with type 2 diabetes. Endocr Pract 24(12):1063–1072
Kim JY, Bacha F, Tfayli H, Michaliszyn SF, Yousuf S, Arslanian S (2019) Adipose tissue insulin resistance in youth on the spectrum from normal weight to obese and from normal glucose tolerance to impaired glucose tolerance to type 2 diabetes. Diabetes Care 42(2):265–272
Gastaldelli A, Gaggini M, DeFronzo RA (2017) Role of adipose tissue insulin resistance in the natural history of type 2 diabetes: results from the San Antonio Metabolism Study. Diabetes 66(4):815–822
Gastaldelli A, Harrison SA, Belfort-Aguilar R, Hardies LJ, Balas B, Schenker S, Cusi K (2009) Importance of changes in adipose tissue insulin resistance to histological response during thiazolidinedione treatment of patients with nonalcoholic steatohepatitis. Hepatology 50(4):1087–1093
Kutoh E, Kuto AN, Wada A, Kurihara R, Kojima R (2021) Complementary effects on glycaemic and non-glycaemic parameters between responders and non-responders treated with pioglitazone and canagliflozin in drug-naive subjects with type 2 diabetes. Int J Clin Pract 75(12):e14914
Kutoh E, Kuto AN, Wada A, Kurihara R, Kojima R (2022) Regulations of free fatty acids and diabetic parameters in drug naïve subjects with type 2 diabetes treated with canagliflozin monotherapy. Drug Res (Stuttg) 72(2):86–93
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419
Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, Quon MJ (2000) Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 85(7):2402–2410
Saisho Y, Kou K, Tanaka K, Abe T, Kurosawa H, Shimada A, Meguro S, Kawai T, Itoh H (2011) Postprandial serum C-peptide to plasma glucose ratio as a predictor of subsequent insulin treatment in patients with type 2 diabetes. Endocr J 58(4):315–322
Amrhein V, Korner-Nievergelt F, Roth T (2017) The earth is flat (p > 0.05): significance thresholds and the crisis of unreplicable research. PeerJ 5:e3544
Hermans MP, Ahn SA, Rousseau MF (2010) log(TG)/HDL-C is related to both residual cardiometabolic risk and β-cell function loss in type 2 diabetes males. Cardiovasc Diabetol 14(9):88
Hermans MP, Ahn SA, Rousseau MF (2012) The atherogenic dyslipidemia ratio [log(TG)/HDL-C] is associated with residual vascular risk, beta-cell function loss and microangiopathy in type 2 diabetes females. Lipids Health Dis 11:132
Kawamoto R, Tabara Y, Kohara K, Miki T, Kusunoki T, Takayama S, Abe M, Katoh T, Ohtsuka N (2011) Relationships between lipid profiles and metabolic syndrome, insulin resistance and serum high molecular adiponectin in Japanese community-dwelling adults. Lipids Health Dis 10:79
Sano M (2019) Mechanism by which dipeptidyl peptidase-4 inhibitors increase the risk of heart failure and possible differences in heart failure risk. J Cardiol 73(1):28–32
White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, Perez AT, Fleck PR, Mehta CR, Kupfer S, Wilson C, Cushman WC, Zannad F, EXAMINE Investigators (2013) Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med 369(14):1327–1335
Ueki K, Tanizawa Y, Nakamura J, Yamada Y, Inagaki N, Watada H, Shimomura I, Nishimura R, Miyoshi H, Abiko A, Katagiri H, Hayashi M, Shimada A, Naruse K, Fujimoto S, Fujiwara M, Shikata K, Okada Y, Araki E, Yamazaki T, Kadowaki T, J-BRAND Registry Group (2021) Long-term safety and efficacy of alogliptin, a DPP-4 inhibitor, in patients with type 2 diabetes: a 3-year prospective, controlled, observational study (J-BRAND Registry). BMJ Open Diabetes Res Care 9(1):e001787
Okada K, Kikuchi S, Kuji S, Nakayama N, Maejima N, Matsuzawa Y, Iwahashi N, Kosuge M, Ebina T, Kimura K, Tamura K, Hibi K (2022) Impact of early intervention with alogliptin on coronary plaque regression and stabilization in patients with acute coronary syndromes. Atherosclerosis 360:1–7
Shah Z, Kampfrath T, Deiuliis JA, Zhong J, Pineda C, Ying Z, Xu X, Lu B, Moffatt-Bruce S, Durairaj R, Sun Q, Mihai G, Maiseyeu A, Rajagopalan S (2011) Long-term dipeptidyl-peptidase 4 inhibition reduces atherosclerosis and inflammation via effects on monocyte recruitment and chemotaxis. Circulation 124(21):2338–2349
Amigo L, Husche C, Zanlungo S, Lütjohann D, Arrese M, Miquel JF, Rigotti A, Nervi F (2011) Cholecystectomy increases hepatic triglyceride content and very-low-density lipoproteins production in mice. Liver Int 31(1):52–64
Bush NC, Triay JM, Gathaiya NW, Hames KC, Jensen MD (2014) Contribution of very low-density lipoprotein triglyceride fatty acids to postabsorptive free fatty acid flux in obese humans. Metabolism 63(1):137–140
Tsushima Y, Nishizawa H, Tochino Y, Nakatsuji H, Sekimoto R, Nagao H, Shirakura T, Kato K, Imaizumi K, Takahashi H, Tamura M, Maeda N, Funahashi T, Shimomura I (2013) Uric acid secretion from adipose tissue and its increase in obesity. J Biol Chem 288(38):27138–27149
Boersma GJ, Johansson E, Pereira MJ, Heurling K, Skrtic S, Lau J, Katsogiannos P, Panagiotou G, Lubberink M, Kullberg J, Ahlström H, Eriksson JW (2018) Altered glucose uptake in muscle, visceral adipose tissue, and brain predict whole-body insulin resistance and may contribute to the development of type 2 diabetes: a combined PET/MR study. Horm Metab Res 50(8):627–639
Acknowledgements
The authors thank Drs. Kenji Kawashima, Satoshi Yamazaki and Takashi Niida and Kazuki Dohi for discussions and useful comments, and Ms. Keiko Ozawa for her kind assistance during preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
EK and ANK contributed substantially to the study design and concept. EO, MA, and RK were involved in data acquisition. EK and ANK conducted the data analyses and wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethical Committee/Institutional Review Board of Gyoda General Hospital and Kumagaya Surgical Hospital. This study was conducted following the principles of the Helsinki Declaration and Good Clinical Practice. All patients gave their informed consent to participate and to publish, which was stored in the electronic medical record system.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kutoh, E., Kuto, A.N., Akiyama, M. et al. Alogliptin: a DPP-4 inhibitor modulating adipose tissue insulin resistance and atherogenic lipid. Eur J Clin Pharmacol 79, 947–959 (2023). https://doi.org/10.1007/s00228-023-03506-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-023-03506-3