Abstract
Aim
This study aimed to reveal the current status of the literature on rational prescribing training in undergraduate medical education.
Methods
This study followed the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. An online search using 50 keywords in four databases was performed to access the studies published between 2008 and 2020. Specific features of the training such as aims or objectives of teaching, methods or model, and evaluation of effectiveness were extracted. Kirkpatrick levels were used to evaluate the effectiveness of teaching.
Results
Of 74 studies included in the full review, 16 (21.6%) of them reported the use of WHO 6-Step Model for Rational Prescribing in their educational interventions. In terms of effectiveness, only two of the studies investigated changes in learner behavior in the context for which they are being trained, and only one study showed the effect of training on patient outcomes.
Conclusion
The evidence on the effectiveness of rational prescribing training has been presented mostly by using student satisfaction surveys and test of knowledge and skills. A higher level of evidence such as patient outcomes of the training needs to be reported.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rational prescribing is one of the important skills that physicians use throughout their professional life. Although the number is expected to change from a country to another country, a nationwide study conducted in Turkey showed that a family physician writes 47 prescriptions per day on average [1]. Considering its importance along with the high frequency, it is evident that lacking this skill could cause severe consequences frequently. More specifically, a recent systematic review on prescribing errors revealed that the median rate of medication errors following discharge is 53% [2]. A more recent systematic review showed that the percentage of preventable adverse drug reactions in primary care settings is between 12 and 37% [3]. These preventable errors and reactions cause a great burden of morbidity and mortality both in hospital settings [4] and primary care settings [3].
The problem does not exist only for experienced physicians, but also newly graduated doctors suffer from it [5]. Moreover, a recent multinational study showed that there is a “lack of essential prescribing competencies among final-year students in Europe” [6]. These facts direct us to focus on the effectiveness of rational prescribing training in undergraduate medical education.
The last comprehensive systematic review studies on the effectiveness of rational prescribing training were published in 2009 by screening the studies published up to 2008 [7, 8]. One of these reviews showed that most of the studies have been conducted with “small numbers of participants in single centres” [8]. Therefore, they concluded that there is a need “to produce high-quality educational interventions” and “to systematically test why interventions do or do not work” in terms of rational prescribing [7, 8]. After these studies, several systematic reviews were carried out with limited scope or were not focusing on undergraduate medical education. In these systematic review studies, geriatric pharmacology education [9], new prescribers’ behavioral changes after educational interventions [10], educational interventions to improve prescribing competency in medical and non-medical prescribers [11], simulation methods to teach pharmacotherapy in health professions education [12], educational interventions targeting rational prescribing of opioids [13], digital learning for rational prescribing [14], and human‐simulation‐based learning for prescribing [15] have been studied.
We can conclude that a systematic review focused on investigating the effectiveness of rational prescribing training in undergraduate medical education is needed. Following the last comprehensive review [8], we aimed to reveal the current status of the literature including the studies from 2008 to 2020 on rational prescribing training in undergraduate medical education.
The research questions of this study are as follows:
-
1.
Which educational years have rational prescribing training been implemented?
-
2.
What are the methods/models used to teach rational prescribing?
-
3.
How effective is rational prescribing training?
Methods
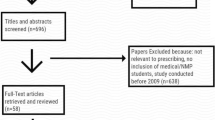
Our study is a systematic review that follows the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [16]. Figure 1 summarizes the screening process.
Search strategy
We conducted an online search using 50 keywords with “[AND]” or “[OR]” operators (see the Appendix, Table 1). The search terms were extracted from the relevant literature. The period that we included to search was 2008–2020 (both years included) since the last systematic reviews on teaching rational prescribing were published in 2009 [7, 8]. Search was carried out between March 18, 2021, and July 27, 2021, by one reviewer.
We searched the keywords through four databases: PubMed, Scopus, Web of Science, and Education Resources Information Center (ERIC). All records were downloaded and imported into a reference management tool (Endnote X9.2) to make the screening process easier.
Inclusion and exclusion criteria
Inclusion criteria was defined as a PICO [17].
-
Population: undergraduate medical students
-
Intervention: rational prescribing training
-
Comparison: none
-
Outcome: the effectiveness in terms of Kirkpatrick levels [18]
Studies that reported any kind of rational prescribing teaching activity in an undergraduate medical education setting were included. The settings that include other health professions students along with undergraduate medical students were also included if the focus of the study is to teach rational prescribing. These studies were excluded:
-
Studies that were not published in English
-
Studies that did not include a research report such as correspondence and commentary
-
Studies that reported a rational prescribing teaching activity in a postgraduate or continuous medical education setting, or the other health professions education settings without the participation of undergraduate medical students
-
Studies that focused on improving interprofessional education rather than teaching rational prescribing
-
Studies that focused only on “basic” pharmacology teaching (the studies only from the perspective of “basic sciences” without vertical integration [19])
Screening of the studies
The titles that were imported into the reference management tool were independently screened by two reviewers. The titles that create uncertainty by means of relevance were included to be screened during the abstract screening. The same process was carried out for the abstract screening, and the disagreements were solved by discussing together with a third reviewer during the full-text screening.
Extraction of the data
A data extraction form that consists of a table with 11 columns was developed. The columns were titled as follows: authors and year, country, undergraduate year, number of participants, type of course, course manager, aims or objectives of teaching, methods or model, evaluation of effectiveness, result, and the highest level of Kirkpatrick levels. To fill in these columns with the relevant data extracted from the studies, each study has been assigned to two reviewers. Subsequently, the reviewers gathered to discuss and reach a consensus to be consistent. The disagreements lasted after this discussion were solved by two lead reviewers (IİB and ÖC) by reaching an agreement.
Assessment of the results
To assess the effectiveness of the interventions, Kirkpatrick evaluation levels [18] have been used. Two reviewers evaluated each study using Kirkpatrick levels by discussing and reaching a consensus.
Results
Descriptive statistics
Out of 74 studies included for full review, the distribution of the studies in terms of publication years is presented in the graphic in the Appendix (see the Appendix, Fig. 1).
The studies were carried out in 18 different countries. The UK had the most of the studies with 19 (25.6%) studies among these countries. The USA followed the UK with 10 (13.5%) studies. India had 9 (12.1%), the Netherlands had 6 (8.1%), Germany had 5 (6.7%), and Turkey had 4 (5.4%) studies. Apart from those, there were two (2.7%) multinational studies that have been conducted in more than one country [20, 21]. The number of studies that include compulsory teaching was 31 (41.9%), voluntary was 41 (55.4%), and two (2.7%) were unspecified.
Out of 74 studies, 70 of them reported participant numbers. The mean value of participant numbers in these 70 studies was 214 ± 308 (max, 1727; min, 1). Leading two studies with maximum participants had 1727 [22] and 1652 [23]. The first one reported usage of online self-assessment tool for drug dose calculations to teach rational prescribing in order to reduce serious medical incidents [22]. The second one reported long-term effect of a training based on WHO 6-Step Model for Rational Prescribing in medical curriculum [23]. The study conducted with the least number of participants had only one participant [24]. In this study, a medical student described the personal experiences in the use of a workplace training system for rational pharmacotherapy called “Check and Correct” [24].
Which educational years have rational prescribing training been implemented?
Table 1 shows the distribution of the undergraduate medical student participants in terms of years. Since some studies had participants from more than one undergraduate year, the total number is higher than 74. The least number of studies were conducted with first-year medical students compared to other 5 years of undergraduate medical education. However, it is worth to note that undergraduate medical education lasts various number of years in different countries.
What are the methods/models used to teach rational prescribing?
Out of reviewed 74 studies, 16 (21.6%) of them reported that they used or partially adopted WHO 6-Step Model for Rational Prescribing in their educational interventions [20, 23, 25,26,27,28,29,30,31,32,33,34,35,36,37,38]. In 15 studies, teaching method was described as case-based (case based; learning, discussion, online simulation, assignments). However, most of the studies have utilized cases even if they did not describe the method as case-based.
Two studies used games, a board game [39] and a serious game [40], to teach infection related pharmacotherapy. Four studies used formative assessment to support learning rational prescribing [21, 22, 41,42,43]. Pharmacist-led teaching for prescribing was presented in five studies [44,45,46,47,48]. Team-based learning has been utilized in three studies [49,50,51] and task-based learning in one study [52]. Peer or near-peer education was another method that has been used in other three studies [43, 53,54,55]. Some specific tools also have been used such as “The Systematic Tool to Reduce Inappropriate Prescribing (STRIP)” [56], “Check and Correct” [24], and “Patient Education Checklist” [57]. Apart from all these methods, there were some more common methods that have been used: lecture, seminar, small-group discussion, patient encounter, clinical rotation, clerkship, workshop, e-learning, and virtual patients.
How effective is rational prescribing training?
In the studies, the effectiveness of training has been assessed using various tools and methods: survey, focus-group interview, written assessment, objective structured clinical examination (OSCE) [25, 32, 37, 38, 53, 58, 59], objective structured performance evaluation (OSPE) [41, 60,61,62], direct observation of procedural skills (DOPS) [48], mini clinical evaluation exercise (mini-CEX) [58], and assessment by patients [28].
In Table 2, we reported the highest level that educational interventions reached. Of 56 studies in level Kirkpatrick level two, 29 assessed only knowledge, 21 assessed only skills, and six assessed both knowledge and skills (see the Appendix, Table 2). There was a substantial and statistically significant agreement between the raters (Cohen kappa value: 0.749, p < 0.001).
In the study that reaches Kirkpatrick’s fourth level by showing an improved patient outcome [63], students participated in a medication safety curriculum that comprised of a workshop, case-based assignments, and patient encounters. Three to 6 months after the student-led medication encounters, patients felt more knowledgeable and reported that “students helped them overcome barriers to medication adherence (e.g. cost, transportation, side effects)” [63].
Two studies [28, 34] that reached Kirkpatrick’s third level by reporting changes in learner behavior in daily clinical context have utilized WHO 6-Step Model for Rational Prescribing. On the effectiveness of the training, one of them stated that students provided satisfying care in a student-run clinic [28]. The other one conducted a semi-structured interview with former students who had participated in the training [34]. The finding of the study was that these students have an awareness about rational use of medicine but they do not use the knowledge in daily clinical practice.
Discussion
The findings showed that the prominent model to teach rational prescribing is, as it was in 2009 [8], WHO 6-Step Model for Rational Prescribing since it has been utilized in 21.6% of the studies. Apart from that, various teaching methods have also been used in other studies.
The studies generally showed positive outcomes in terms of student satisfaction and test of knowledge and skills (Kirkpatrick’s first and second levels). However, the effectiveness of rational prescribing training still needs a higher level of evidence such as behavior change in a real context (third level) and increased patient outcomes (fourth level). Out of 74 studies, only one study has shown increased patient outcomes [63], and only two studies investigated evidence from the context for which the students are being trained [28, 34]. The findings of our study are aligned with the previous two reviews published in 2009 that point out a need for robust evaluations regarding the effectiveness of educational interventions to teach rational prescribing [7, 8].
Rational prescribing training has been carried out in various undergraduate years, but it was held least in the first year of undergraduate medical education, and more often in the clinical years. Considering the importance of early clinical experience in cultivating skills [64], an inclination for rational prescribing training to be carried out starting from the first year would be helpful. In this kind of attempt, it is crucial to keep in mind that the content of training should be adjusted and simplified according to the levels of first-year students if we do not want to lead to a cognitive overload [65].
Regarding countries, the literature mentioned that the Netherlands has a pioneering role due to the high use of the WHO 6-Step Model for Rational Prescribing [66]. Along with that, our findings showed that researchers from the UK have also significant contribution to the rational prescribing training literature with 19 studies. Even if quantitative results showed these countries have a prominent role, reaching the higher levels of evaluation in terms of Kirkpatrick levels is more valuable. From this perspective, the two studies that reached the third level were from the Netherlands [28] and Brazil [34], and the one that reached the fourth level was from the USA [63]. In 2009, there were seven different countries that implemented rational prescribing training, while our study showed 18 different countries (when multinational studies were not included). Even if the previous study had a narrower scope than ours, this still is a hopeful sign that rational prescribing training spreads to different contexts, which is an important step for improvement.
Medical curricula and pathways vary in different countries according to specific conditions of each country [67], and as a result, it is reasonable to expect that the approaches utilized to teach rational prescribing also differ. For example, in the UK, Prescribing Safety Assessment (PSA) is used to ensure that newly graduates are prepared to prescribe [68]. The use of the PSA has influenced the way in which rational prescribing is taught, as demonstrated by research on the effectiveness of teaching approaches specifically designed to prepare students for the PSA [50, 69]. Although it is difficult to classify a country as a whole, in some countries, the teaching of rational prescribing may be more focused on the use of evidence-based guidelines, while in other countries, the emphasis may be more on developing the ability to consider a range of factors when making prescribing decisions. Regardless of the specific focus of the medical curriculum in a country, it is important for medical students to understand the principles of rational prescribing.
As a well-established method with more than 25 years of implementation in various settings, WHO 6-Step Model for Rational Prescribing would be considered as the safest option among others to teach rational prescribing. Since the guide for the utilization of this model has currently 24 translations or local editions [66], it can be used in different countries speaking different languages. More recently, the attempts to update the guide have started by evaluating its use and impact and considering the demands [66].
This review offers three specific benefits. The first benefit is that it offers a foundation for future research by revealing the current situation regarding rational prescribing training. The second benefit would be for medical educators who would like to embark on developing rational prescribing training in the undergraduate years. The table in the Appendix could be a rich source for them to explore previous training experiences. By taking a look at it, they may decide to review some studies further to utilize some methods in their local context. The third benefit would be for the researchers who deliver rational prescribing training in their institutions. Our study could raise awareness to evaluate the effectiveness of their training by using some methods that are aimed to show the effect on patient outcomes.
This study has some limitations. The first limitation is that even if it is a strength to focus on undergraduate medical education, it limits the generalizability of this study in the meantime. It is also possible that some studies relevant to the topic would not be identified. Another limitation is that, since the reviewed studies do not always clearly report the methods that they have used, the data about the methods/models may have some problems. It heavily depended on their own description and understanding that may not completely reflect what they have actually done.
Conclusion
In this study, we reviewed the published literature on rational prescribing training in undergraduate settings. We found that WHO 6-Step Model for Rational Prescribing is the most prominent and well-established method to teach rational prescribing. Apart from that, many different teaching methods have been utilized. However, the evidence for the effectiveness has been presented mostly by using student satisfaction surveys and test of knowledge and skills. There are a limited number of studies that report a higher level of evidence such as patient outcomes of the training. Rational prescribing training needs more robust evidence on its effectiveness.
Data Availability
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Change history
22 January 2023
Supplementary Materials are missing and it is included in the re-published proof.
References
Bulut S, Yıldız A, Kaya S (2019) Evaluation of transition to electronic prescriptions in Turkey: perspective of family physicians. Int J Health Policy Manag 8:40–48. https://doi.org/10.15171/ijhpm.2018.89
Alqenae FA, Steinke D, Keers RN (2020) Prevalence and nature of medication errors and medication-related harm following discharge from hospital to community settings: a systematic review. Drug Saf 43:517–537. https://doi.org/10.1007/s40264-020-00918-3
Insani WN, Whittlesea C, Alwafi H et al (2021) Prevalence of adverse drug reactions in the primary care setting: a systematic review and meta-analysis. PLoS One 16:e0252161. https://doi.org/10.1371/journal.pone.0252161
Oscanoa TJ, Lizaraso F, Carvajal A (2017) Hospital admissions due to adverse drug reactions in the elderly. A meta-analysis Eur J Clin Pharmacol 73:759–770. https://doi.org/10.1007/s00228-017-2225-3
Ross S, Bond C, Rothnie H et al (2009) What is the scale of prescribing errors committed by junior doctors? A systematic review. Br J Clin Pharmacol 67:629–640. https://doi.org/10.1111/j.1365-2125.2008.03330.x
Brinkman D, Tichelaar J, Schutte T et al (2017) Essential competencies in prescribing: a first European cross-sectional study among 895 final-year medical students. Clin Pharmacol Ther 101:281–289. https://doi.org/10.1002/cpt.521
Ostini R, Hegney D, Jackson C et al (2009) Systematic review of interventions to improve prescribing. Ann Pharmacother 43:502–513. https://doi.org/10.1345/aph.1L488
Ross S, Loke YK (2009) Do educational interventions improve prescribing by medical students and junior doctors? A systematic review. Br J Clin Pharmacol 67:662–670. https://doi.org/10.1111/j.1365-2125.2009.03395.x
Keijsers CJPW, van Hensbergen L, Jacobs L et al (2012) Geriatric pharmacology and pharmacotherapy education for health professionals and students: a systematic review: Geriatric pharmacology and pharmacotherapy education. Br J Clin Pharmacol 74:762–773. https://doi.org/10.1111/j.1365-2125.2012.04268.x
Brennan N, Mattick K (2013) A systematic review of educational interventions to change behaviour of prescribers in hospital settings, with a particular emphasis on new prescribers: systematic review of behaviour change interventions. Br J Clin Pharmacol 75:359–372. https://doi.org/10.1111/j.1365-2125.2012.04397.x
Kamarudin G, Penm J, Chaar B, Moles R (2013) Educational interventions to improve prescribing competency: a systematic review. BMJ Open 3:e003291. https://doi.org/10.1136/bmjopen-2013-003291
Aura SM, Sormunen MST, Jordan SE et al (2015) Learning outcomes associated with patient simulation method in pharmacotherapy education: an integrative review. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare 10:170–177. https://doi.org/10.1097/SIH.0000000000000084
Moride Y, Lemieux-Uresandi D, Castillon G et al (2019) A systematic review of interventions and programs targeting appropriate prescribing of opioids. Pain Physician 22:229–240
Bakkum MJ, Tichelaar J, Wellink A et al (2019) Digital learning to improve safe and effective prescribing: a systematic review. Clin Pharmacol Ther 106:1236–1245. https://doi.org/10.1002/cpt.1549
Sarfati L, Ranchon F, Vantard N et al (2019) Human-simulation-based learning to prevent medication error: a systematic review. J Eval Clin Pract 25:11–20. https://doi.org/10.1111/jep.12883
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34. https://doi.org/10.1016/j.jclinepi.2009.06.006
Cook DA, West CP (2012) Conducting systematic reviews in medical education: a stepwise approach: conducting systematic reviews. Med Educ 46:943–952. https://doi.org/10.1111/j.1365-2923.2012.04328.x
Frye AW, Hemmer PA (2012) Program evaluation models and related theories: AMEE Guide No. 67. Med Teach 34:e288–e299. https://doi.org/10.3109/0142159X.2012.668637
Brauer DG, Ferguson KJ (2015) The integrated curriculum in medical education: AMEE Guide No. 96. Med Teach 37:312–322. https://doi.org/10.3109/0142159X.2014.970998
De Vries TPGM, Daniels JMA, Mulder CW et al (2008) Should medical students learn to develop a personal formulary?: An international, multicentre, randomised controlled study. Eur J Clin Pharmacol 64:641–646. https://doi.org/10.1007/s00228-008-0465-y
Likic R, White C, Cinti S et al (2013) Online learning applied to a course on rational therapeutics: an international comparison between final year students of two medical schools: Online learning applied to a course on rational therapeutics. Br J Clin Pharmacol 75:373–380. https://doi.org/10.1111/j.1365-2125.2012.04370.x
McQueen DS, Begg MJ, Maxwell SRJ (2010) eDrugCalc: an online self-assessment package to enhance medical students’ drug dose calculation skills: improving dose calculation skills. Br J Clin Pharmacol 70:492–499. https://doi.org/10.1111/j.1365-2125.2010.03609.x
Keijsers CJPW, Segers WS, de Wildt DJ et al (2015) Implementation of the WHO-6-step method in the medical curriculum to improve pharmacology knowledge and pharmacotherapy skills: effect of WHO-6-step implemented in a medical curriculum. Br J Clin Pharmacol 79:896–906. https://doi.org/10.1111/bcp.12575
Conroy-Smith E, Herring R, Caldwell G (2011) Learning safe prescribing during post-take ward rounds. Clin Teach 8:75–78. https://doi.org/10.1111/j.1743-498X.2011.00432.x
Sikkens JJ, Caris MG, Schutte T et al (2018) Improving antibiotic prescribing skills in medical students: the effect of e-learning after 6 months. J Antimicrob Chemother 73:2243–2246. https://doi.org/10.1093/jac/dky163
Tichelaar J, den Uil SH, Antonini NF et al (2016) A ‘SMART’ way to determine treatment goals in pharmacotherapy education: improving treatment goal setting, step 2 of the WHO Guide to Good Prescribing. Br J Clin Pharmacol 82:280–284. https://doi.org/10.1111/bcp.12919
Desai M, Panchal J, Shah S, Iyer G (2016) Evaluation of impact of teaching clinical pharmacology and rational therapeutics to medical undergraduates and interns. Int J App Basic Med Res 6:205. https://doi.org/10.4103/2229-516X.186967
Dekker RS, Schutte T, Tichelaar J et al (2015) A novel approach to teaching pharmacotherapeutics—feasibility of the learner-centered student-run clinic. Eur J Clin Pharmacol 71:1381–1387. https://doi.org/10.1007/s00228-015-1916-x
Dikici MF, Yaris F, Artiran Igde F, et al (2014) Effect of a workshop in rational pharmacotherapy for interns during family medicine clerkship in Samsun-Turkey. Pak J Med Sci 30:. https://doi.org/10.12669/pjms.302.4285
Krishnaiah V, Ramaiah V, Ramakrishna R (2013) Comparison of rational pharmacotherapy approach by medical students with and without Guide to Good prescribing guidelines. Natl J Physiol Pharm Pharmacol 3:53. https://doi.org/10.5455/njppp.2013.3.53-56
Khanal S, Buckley T, Harnden C et al (2013) Effectiveness of a national approach to prescribing education for multiple disciplines: a national prescribing curriculum in Australia. Br J Clin Pharmacol 75:756–762. https://doi.org/10.1111/j.1365-2125.2012.04399.x
Gelal A, Gumustekin M, Ma A, Gidener S (2013) Rational pharmacotherapy training for fourth-year medical students. Indian J Pharmacol 45:4. https://doi.org/10.4103/0253-7613.106426
Kamat SK, Marathe PA, Patel TC et al (2012) Introduction of case based teaching to impart rational pharmacotherapy skills in undergraduate medical students. Indian Journal of Pharmacology 44:634
Patrício KP, Alves NAB, Arenales NG, Queluz TT (2012) Teaching the rational use of medicines to medical students: a qualitative research. BMC Med Educ 12:56. https://doi.org/10.1186/1472-6920-12-56
Rakanovic-Todic M, Mulabegovic N, Kusturica J et al (2011) Role-play in the rational pharmacotherapy training: is it suitable. Technologies Education Management 6:535–540
Baskett K (2011) Using e-learning to improve prescribing practice in emerging prescribers. Teaching English with Technology 11:98–109
Guney Z, Uluoglu C, Yucel B, Coskun O (2009) The impact of rational pharmacotherapy training reinforced via prescription audit on the prescribing skills of fifth-year medical students. CP 47:671–678. https://doi.org/10.5414/CPP47671
Richir M, Tichelaar J, Stam F et al (2008) A context-learning pharmacotherapy program for preclinical medical students leads to more rational drug prescribing during their clinical clerkship in internal medicine. Clin Pharmacol Ther 84:513–516. https://doi.org/10.1038/clpt.2008.82
Karbownik MS, Wiktorowska-Owczarek A, Kowalczyk E, et al (2016) Board game versus lecture-based seminar in the teaching of pharmacology of antimicrobial drugs—a randomized controlled trial. FEMS Microbiology Letters 363:fnw045. https://doi.org/10.1093/femsle/fnw045
Tsopra R, Courtine M, Sedki K et al (2020) AntibioGame®: A serious game for teaching medical students about antibiotic use. Int J Med Inform 136:104074. https://doi.org/10.1016/j.ijmedinf.2020.104074
Malhotra S, Shah K, Patel V (2013) Objective structured practical examination as a tool for the formative assessment of practical skills of undergraduate students in pharmacology. J Edu Health Promot 2:53. https://doi.org/10.4103/2277-9531.119040
Wallerstedt SM, Wallerstedt M, Wallerstedt S (2013) The specialty clinical pharmacology needs to be examined separately to guarantee a sufficient level of knowledge in medical students. Eur J Clin Pharmacol 69:1331–1334. https://doi.org/10.1007/s00228-012-1461-9
Zollner B, Sucha M, Berg C et al (2013) Pharmacases.de – A student-centered e-learning project of clinical pharmacology. Med Teach 35:251–253. https://doi.org/10.3109/0142159X.2013.759642
Kim S, Willett L, Hughes F et al (2013) Pharmacist-led workshops to enhance pharmacotherapy knowledge for medical students. Teach Learn Med 25:118–121. https://doi.org/10.1080/10401334.2013.770744
Newby DA, Stokes B, Smith AJ (2019) A pilot study of a pharmacist-led prescribing program for final-year medical students. BMC Med Educ 19:54. https://doi.org/10.1186/s12909-019-1486-1
Sandilands EA, Reid K, Shaw L et al (2011) Impact of a focussed teaching programme on practical prescribing skills among final year medical students: Education and prescribing errors. Br J Clin Pharmacol 71:29–33. https://doi.org/10.1111/j.1365-2125.2010.03808.x
Tittle V, Randall D, Maheswaran V et al (2014) Practical prescribing course: a student evaluation. Clin Teach 11:38–42. https://doi.org/10.1111/tct.12106
Ward S, Wasson G (2016) Bridging the gap: improving safe prescribing from university to workplace. Int J Clin Pharm 38:1023–1026. https://doi.org/10.1007/s11096-016-0346-x
Akl IB, Ghaddar F, Sabra R et al (2012) Teaching clinical pharmacology using team-based learning: a comparison between third- and fourth-year medical students. J Clin Pharmacol 52:1806–1814. https://doi.org/10.1177/0091270011428986
Field SM, Burstow NJ, Owen DR, Sam AH (2019) Using team-based revision to prepare medical students for the prescribing safety assessment. Adv Med Educ Pract 10:501–506. https://doi.org/10.2147/AMEP.S204435
Zgheib NK, Simaan JA, Sabra R (2011) Using team-based learning to teach clinical pharmacology in medical school: student satisfaction and improved performance. J Clin Pharmacol 51:1101–1111. https://doi.org/10.1177/0091270010375428
Bilge SS, Akyüz B, Ağrı AE, Özlem M (2017) Rational drug therapy education in clinical phase carried out by task-based learning. Indian J Pharmacol 49:102–109. https://doi.org/10.4103/0253-7613.201009
Gibson KR, Qureshi ZU, Ross MT, Maxwell SR (2014) Junior doctor-led ‘near-peer’ prescribing education for medical students: junior doctor-led prescribing education. Br J Clin Pharmacol 77:122–129. https://doi.org/10.1111/bcp.12147
Haslam P, Yau C, Rutter C (2014) Junior doctor-led practical prescribing course. Clin Teach 11:29–32. https://doi.org/10.1111/tct.12087
Rodrigues J, Sengupta A, Mitchell A et al (2009) The South-east Scotland Foundation Doctor Teaching Programme — is “near-peer” teaching feasible, efficacious and sustainable on a regional scale? Med Teach 31:e51–e57. https://doi.org/10.1080/01421590802520915
Drenth-van Maanen AC, Leendertse AJ, Jansen PAF et al (2018) The systematic tool to reduce inappropriate prescribing (STRIP): combining implicit and explicit prescribing tools to improve appropriate prescribing. J Eval Clin Pract 24:317–322. https://doi.org/10.1111/jep.12787
Gupta S, Shaw J (2019) Development of medication-related counselling skills in senior medical students: a checklist-based approach. BMC Med Educ 19:335. https://doi.org/10.1186/s12909-019-1773-x
Rogers GD, McConnell HW, Jones de Rooy N et al (2014) A randomised controlled trial of extended immersion in multi-method continuing simulation to prepare senior medical students for practice as junior doctors. BMC Med Educ 14:90. https://doi.org/10.1186/1472-6920-14-90
Taylor D, Yuen S, Hunt L, Emond A (2012) An interprofessional pediatric prescribing workshop AJPE 76:111. https://doi.org/10.5688/ajpe766111
Tayem YI, Altabtabaei AS, Mohamed MW et al (2016) Competence of medical students in communicating drug therapy: Value of role-play demonstrations. Indian J Pharmacol 48:37–41. https://doi.org/10.4103/0253-7613.174517
Al Khaja KAJ, James H, Sequeira RP (2013) Effectiveness of an educational intervention on prescription writing skill of preclerkship medical students in a problem-based learning curriculum: The Journal of Clinical Pharmacology. J Clin Pharmacol 53:483–490. https://doi.org/10.1002/jcph.68
Wheeler DW, Degnan BA, Murray LJ et al (2008) Retention of drug administration skills after intensive teaching. Anaesthesia 63:379–384. https://doi.org/10.1111/j.1365-2044.2007.05379.x
Karpa KD, Hom LL, Huffman P et al (2015) Medication safety curriculum: enhancing skills and changing behaviors. BMC Med Educ 15:234. https://doi.org/10.1186/s12909-015-0521-0
Littlewood S, Ypinazar V, Margolis SA et al (2005) Early practical experience and the social responsiveness of clinical education: systematic review. BMJ 331:387–391. https://doi.org/10.1136/bmj.331.7513.387
Young JQ, Van Merrienboer J, Durning S, Ten Cate O (2014) Cognitive load theory: implications for medical education: AMEE Guide No. 86. Med Teach 36:371–384. https://doi.org/10.3109/0142159X.2014.889290
Tichelaar J, Richir MC, Garner S et al (2020) WHO guide to good prescribing is 25 years old: quo vadis? Eur J Clin Pharmacol 76:507–513. https://doi.org/10.1007/s00228-019-02823-w
O’Brien BC, Forrest K, Wijnen-Meijer M, ten Cate O (2018) A global view of structures and trends in medical education. In: Swanwick T, Forrest K, O’Brien BC (eds) Understanding Medical Education. John Wiley & Sons, Ltd, Chichester, UK, pp 7–22
Maxwell SRJ, Cameron IT, Webb DJ (2015) Prescribing safety: ensuring that new graduates are prepared. The Lancet 385:579–581. https://doi.org/10.1016/S0140-6736(14)62339-4
Catling F, Williams J, Baker R (2014) A prescribing e-tutorial for medical students. Clin Teach 11:33–37. https://doi.org/10.1111/tct.12100
Funding
This study has been supported by TÜBİTAK (The Scientific and Technological Research Council of Turkey) under the 1001 program. (project number: 220 K340).
Author information
Authors and Affiliations
Contributions
All authors contributed to the the idea for the article. Literature search and data analysis were performed by Işıl İrem Budakoğlu, Özlem Coşkun, Yavuz Selim Kıyak, and Canan Uluoğlu. The first draft of the manuscript was written by Işıl İrem Budakoğlu, Özlem Coşkun, and Yavuz Selim Kıyak, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Supplementary Materials are missing in the published proof.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Budakoğlu, I.İ., Coşkun, Ö., Kıyak, Y.S. et al. Teaching rational prescribing in undergraduate medical education: a systematic search and review. Eur J Clin Pharmacol 79, 341–348 (2023). https://doi.org/10.1007/s00228-022-03448-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-022-03448-2