Abstract
Objective
Adverse Drug Reactions (ADR) add a significant clinical and economic burden to the healthcare system of a country. We present an overview of the different approaches of ADR reporting systems worldwide and their evolution over time.
Methods
A systematic review of the literature was made based on PubMed and the Cochrane database of systematic reviews. The articles searched for included original articles, WHO and FDA reports and institute of medicine reports.
Summary
Reporting ADRs is the cornerstone of detecting uncommon ADRs once the drugs are on the market. In many countries, ADR reporting is regulated by national regulatory bodies and various methods are employed to report ADRs. Direct reporting by healthcare professionals has been adopted by many developed and developing countries. With emerging new technologies in the field of medicine, there is a great potential to develop better ADR reporting systems in the countries where they have poor reporting.
Conclusion
Development and acquisition of newer technologies to promote ADR monitoring and reporting is a necessity for an effective pharmacovigilance system in a country.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
ADRs are defined by the World Health Organization (WHO) as responses to a drug which are noxious and unintended and which occur at doses normally used to treat a patient for diagnosis, prophylaxis, therapy, or the modification of a physiological function [1]. ADRs have a detrimental effect on a healthcare system of a country. It is the sixth leading cause of mortality worldwide [2]. A meta-analysis that includes 69 studies around the world showed that 6.7% of all hospital admissions are due to ADRs. In addition, it is found that the median prevalence of ADR-related hospital admission in developed and developing countries was 6.3–5.5%, respectively [3].
Furthermore, prolonged hospital stays and additional laboratory investigations adversely affect the economy of a country.
Importance of ADR reporting
During the drug development process, only a small number of selected groups of patients are enrolled to experiment with the drug. Thus, some less common ADRs occur in special populations like children, pregnant mothers, and the elderly with several comorbidities that are often undetected. In addition, the trial period may be too brief to detect ADRs. Hence, no drug is safe at the time of marketing. However, drugs are consumed by the people belonging to the above categories once the drug is on the market. Thus, the surveillance system for a post-marketing phase of a drug is necessary to detect, assess, and prevent ADRs which are not identified during the drug development process. Globally, many drugs were withdrawn following severe ADRs, reported during the post-marketing phase, signifying the importance of post-marketing surveillance. A few examples include cisapride, gemtuzumab, and aceclofenac [4]. Even the known ADRs of the particular drug should be detected and reported without any negligence to take necessary actions.
History of ADR reporting
The activities related to the detection, assessment, understanding, and prevention of drug reactions or any other problems related to medicinal products are known as pharmacovigilance [5].
When considering ADR reporting around the world, the national pharmacovigilance systems of most countries depend on spontaneous reporting. Spontaneous reporting means voluntary reporting of ADR data by health professionals, pharmaceutical companies, or directly by patients to a national or regional ADR database. The collected data is screened regularly for detection of the signal. Information suggesting a new potential association or new aspects of a known association between medicines and ADR that warrant further investigation are known as signals [6].
The importance of spontaneous reporting is early identification of the ADRs at the lowest cost. This helps further investigate ADRs, make necessary warnings, and change the products. Furthermore, drugs can be withdrawn based on this information. Still, spontaneous reporting is the cornerstone of pharmacovigilance.
Many countries have understood the importance of pharmacovigilance after the thalidomide tragedy. Thalidomide was found to be an effective antiemetic for nausea and vomiting in pregnancy, and it was prescribed for pregnant women where thousands of deformed infants were born subsequent to its exposure [7, 8]. This incident highlighted the necessity of an active surveillance system for a country to report ADRs. Hence, a formal way of spontaneous reporting system was first introduced following the thalidomide tragedy.
Most of the countries’ national pharmacovigilance centers are ruled by medicine regulatory authorities. Some countries have regional centers which are established and governed by the national center, and they serve as centers for local data collection. Different methods are used to report ADRs by these centers. A study conducted in 2002 to investigate and compare the different ADR reporting systems shows that all schemes are operated on the same basic principle to collect ADR data to prevent possible drug hazards, but the approaches are different [9].
In 1968, WHO started the drug monitoring process by incorporating a few countries. The ten founding members of the WHO programme in 1968 were Australia, Canada, Czechoslovakia, Federal Republic of Germany, Ireland, Netherlands, New Zealand, Sweden, the UK, and the USA [10, 11]. Later, in 1978, this was organized as a separate international drug monitoring center known as Uppsala Monitoring Center (UMC). The primary objective of this programme was a developing international collaboration to identify and take actions for ADRs which were not detected during clinical trials (Programme for International Drug Monitoring (PIDM)) [12]. Currently, it works collaboratively with 143 countries and annually receives 150,000–200,000 reports of suspected ADRs from different countries.
However, the urgent need to rationalize and harmonize the drug regulation process around the world was first recognized by the Europe. In 1990, the International Council for Harmonisation (ICH), formerly the International Conference on Harmonisation, was established by Europe, together with Japan and the USA. ICH has gradually evolved in pharmacovigilance activities on a number of important multidisciplinary topics, including drug safety, quality, and efficacy [13].
Paper-based ADR reporting
With time, many countries around the world implemented ADR reporting systems in which healthcare professionals were supposed to report ADRs voluntarily to a national center. In the beginning, the reporting process was mainly driven by the ADR reporting forms. Different names were given to these ADR reporting forms by their countries. For example, the UK has a yellow card scheme, the USA has a MedWatch reporting form, Australia has a blue card, and India has its own Central Drugs Standard Control Organization (CDSCO) form [14,15,16]. However, there is no internationally accepted standard format to report ADRs to UMC or national centers. Furthermore, a study carried out to compare different ADR forms around the world emphasizes the need of developing a uniform ADR reporting system globally [17]. This study has comparatively evaluated 13 different ADR forms and concluded significant variability in the content of the ADR forms in different countries.
Web-based ADR reporting
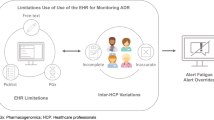
As the ADR reporting process has been largely paper-based, there were many instances of problems with delaying reports, their quality of recording, and poor accessibility. Furthermore, as it is a time-consuming process, encouraging health personnel to report ADR was another concern. However, developing a global electronic ADR reporting system was not that easy as it takes a lot of effort to implement, validate, and manage such a system.
In 1991, a specially designed computer programme known as Adverse Drug Reaction Online Information Tracking system (ADROIT) was introduced by the MHRA and it consisted of all the ADR data received through the yellow card scheme since 1964 [18].The data which is entered into the system are prioritized by their seriousness and the fatal reports are generated within a day where serious and non-serious reports are generated within 72 h and 7 days, respectively [19].
The members of UMC have national pharmacovigilance centers that collect Individual Case Safety Reports (ICSR) and these reports are transferred electronically to VigiBase, the WHO global database of ICSRs [20]. It is the world’s largest database and it is continuously updated with incoming reports of ADR. Currently, all the members of the UMC share their ADR data with the VigiBase [21].
Furthermore, UMC introduced a Web-based ADR reports management system known as VigiFlow in 2004 [22]. This system helps to analyse the ADR data effectively and efficiently, allowing identifying potential medicine safety hazards. Currently, VigiFlow is used by more than 90 members of UMC and is harmonious with international standards. This process also allows healthcare personnel to report ICSR directly to VigiBase [23].
EudraVigilance is the pharmacovigilance database established in 2001 for the collection and analysis of suspected ADRs in European Union (EU) countries [24]. The European Medicine Agency is the regulatory body that operates the system, and it enables the electronic exchange, management, and scientific evaluation of ICSRs related to all medicinal products. Since 2015, the EMA collaboratively has worked with the UMC-WHO by sharing all suspected ADRs with the UMC.
The USA is one of the ten founding members of the International Drug Monitoring Program of WHO. The Food and Drug Administration (FDA) is the responsible authority for the regulation of foods, medicines, cosmetics, and medical devices in the USA. Since 1968, they have been maintaining an ADR reporting system that consists of collecting suspected ADR data from healthcare professionals, consumers, and pharmaceutical companies [25]. Currently, it receives about half a million reports per year, which is a huge number compared to other countries. The collected ADR reports by FDA are sent to the Web-based data tool known as FDA Adverse Event Reporting System [26, 27]. Then they are continually screened for new signals.
In Africa, most of the countries have manual reporting systems rather than electronic methods compared to other developing and developed countries. Furthermore, 200 or more ADR reports per million population are expected by WHO, while some African countries were able to provide fewer than 20 ADR reports per million population in 2010 [28]. At the end of 2015, the majority of African countries (35 of 54) were full members of the PDIM. Although the ICSR submitted from African countries has improved substantially, still the total reports from African countries are < 1% of the global count in VigiBase [29].
Meanwhile, as a solution to the safety issues, another safety surveillance, known as cohort event monitoring (CEM), was introduced by WHO. This method is introduced to capture ADRs that occurred due to selected medications. A simple and user-friendly new software, known as CemFlow, was designed by WHO to manage and analyze all the data collected from CEM. This software is introduced as a pilot project to collect ADR data in African countries. Furthermore, the PaniFlow software, a specially designed extension of the UMC’s ICSR management tool VigiFlow, was introduced to African countries by WHO to detect adverse events following immunization (2009 H1N1-pandemic influenza) [30, 31].
However, various organizations and institutions including WHO-UMC are working together to strengthen the ADR reporting systems in African countries which are unsatisfactory compared to other developing countries.
The Asian pharmaceutical market is the third-largest pharmaceutical market in the world after Europe and the USA, and a lot of pharmaceutical companies are emerging with successful drug developments. Japan and China owned the majority, while other countries belong to the minority. In China, Korea, and India, government-approved ADR reporting regional centers have been established across the countries that held the responsibility for monitoring and collecting ADRs [32,33,34,35,36]. Furthermore, Indian authorities are planning to increase the Adverse Drug Reaction Monitoring Centres (AMC) up to 350 across the country. In that case, India will have one of the largest ADR monitoring programs among the Asian countries. By establishing various networks and bodies, these countries keep working on strengthening pharmacovigilance programs without giving up the effort.
In Sri Lanka currently, an existing method to report ADRs is spontaneous reporting by healthcare professionals. The National Medicine Regulatory Authority (NMRA) has introduced a national ADR reporting form together with a set of guidelines that entail all the details concerned regarding the monitoring and reporting of ADRs in Sri Lanka [37, 38]. Furthermore, a Google form of ICSR has been introduced to report ADR, which can be filled by logging in to the website of NMRA. Safety and Risk Evaluation Sub Committee (SAFRESC) is an expert committee appointed by the NMRA which provides advice and technical assistance to the pharmacovigilance division of NMRA pertaining to the subject. To enhance the number of ADR reports to the national center, a step was taken to establish regional foci in identified areas. Accordingly, the first focus was established in 2014. In order to reduce the missing ADR data, a separate ICSR has been introduced for suspected anaphylactic reactions by NMRA to report anaphylactic reactions, which could collect all the important information. Finally, all the appropriate data are entered in the global database (VigiFlow) [39].
However, studies based on electronic ADR reporting systems are lacking in Sri Lanka. Furthermore, measures to promote ADR reporting are not being given appropriate attention and the practical problems associated with the ADR reporting are not being properly addressed.
Since the beginning, spontaneous reporting of ADRs mostly depends on the healthcare professionals. However, some countries (the USA, Canada, and Australia) have permitted patients to report ADRs since the initial stages of the pharmacovigilance programs. In 2003, Denmark and the Netherlands, followed by Italy, the UK, Sweden, and Croatia, allowed patients to report directly to their regulatory agency [40]. After adopting new pharmacovigilance legislation in 2012, EU countries have empowered their patients to report ADRs directly to the national pharmacovigilance center [41]. A study conducted using 44 countries that have patients’ reporting systems shows 9% of reports represent coming from direct patient reporting. Out of them, 27 countries have a patient-specific reporting form, while 31 countries provide a form to complete online [42]. Few studies found that patient reporting of suspected ADRs has the potential to add value to pharmacovigilance [43].
There are many countries around the world where patients are still not incorporated into the spontaneous ADR reporting system. However, the reports obtained from patients may require further evaluation and investigations. It is questionable whether the reports obtained from the patients whose health literacy is poor, add any value to the system.
Although the ADR reporting and providing safety information during clinical trials by pharmaceutical companies to regulatory authorities has been mandatory for many years, the requirements of each authority are different [44]. In some countries, spontaneous reports are submitted to relevant pharmaceutical companies, and those companies have legal obligations to forward those reports to the national centers. Germany and the USA provide a considerable number of reports from the industry compared to other countries.
Worldwide, many interventions have been tried to facilitate spontaneous ADR reporting. Still, the major drawback is underreporting [3]. To facilitate the ADR reporting, in most cases, educational interventions were tested [45,46,47]. Furthermore, some countries have employed Web-based methods while others have employed electronic health record systems [48]. With time as new technologies are emerging, the field of pharmacovigilance was looking for a more user-friendly and efficient way of reporting ADRs. Introducing mobile applications in the different fields of medicine is a recent development [49].
Mobile application to report ADRs
Introducing mobile applications in the field of pharmacovigilance is a new transformation, and it enables easy ADR reporting as this helps lower the barriers to reporting. In 2014, European Union’s Innovative Medicines Initiative and WHO, in collaboration with Uppsala Monitoring Centre, launched a project known as WEB-Recognizing Adverse Drug Reactions (WEB-RADR) [50]. The main pinnacle of this project was to employ new technologies for pharmacovigilance purposes. Under this project, a mobile application known as Med Safety was introduced as a pilot project in the UK, the Netherlands, and Croatia. Later, this mobile application was introduced to the low- and middle-income countries, and permission was given to adopt a personalized version according to the country. This application allows healthcare professionals and even patients to report ADRs directly to the national center and they receive immediate acknowledgment.
By 2020, this mobile app was introduced in eight countries as a pilot project and some countries have shown a greater increment in ADR reporting rate during this period [51]. As an example, the number of ADR reports received in the first 9 months of the pilot exceeded the total number of reports submitted before the app was launched.
Furthermore, the USA introduced a mobile application in 2012 to report ADRs to FDA known as MedWatcher which allows healthcare professionals and patients to report ADRs voluntarily [52]. In France, several other mobile applications were introduced and allowed users to report ADRs directly to the national centers since 2015 [53]. VigiBip, My e-Report, and Medisafe are those mobile applications that showed increased ADR reports than classical methods. Similarly, India has introduced a mobile application since 2017 to report ADRs to their national pharmacovigilance center [54]. They have shown that the percentage of reports received through consumers and healthcare professionals has been increased up to 96.45%.
Furthermore, some countries have tested integrated methods to promote ADR reporting. Several studies have done combining traditional methods to promote ADR reporting. Few systematic reviews showed multiple interventions have more impact on promoting ADR reporting than doing a single intervention [55, 56]. Some studies have shown the effectiveness of combining new technologies to facilitate the detection of safety signals. A study conducted by integrating drug safety signals from US FDA Adverse Event Reporting System and posts from Twitter showed social media can be used to improve signal detection [57].
Conclusion
Monitoring drug safety is a continuous process and it should be an essential component in the field of medicine, in which some countries are way behind compared to other developed countries. When considering the evolution of the ADR reporting systems, especially during the last 10 years, some countries have put major effort to strengthen their ADR reporting systems while others are in the initial stages where it started. Paper-based processes are time-consuming and labor-intensive. Overworked healthcare personnel in the healthcare setting may not see the importance of reporting ADRs. If the reporting processes are more complicated and time-consuming, they may even fail to report. Hence, an ADR reporting process needs to be user-friendly and easily accessible to the healthcare provider. Furthermore, new approaches of reporting ADRs should be safer and faster, and should be involved in preventing ADRs.
With emerging new technologies in the field of medicine, there is a great potential to develop better ADR reporting systems in the countries where they have poor reporting.
New technology should be employed to gain positive outcomes, including increasing the number and the quality of the ADR reports. The final goal should be the earlier detection of the ADRs and getting appropriate actions to minimize the risk.
To conclude, the development and acquisition of newer technologies to promote ADR monitoring and reporting is a necessity for an effective pharmacovigilance system in a country.
References
World Health Organization (2002) Quality A, Safety of Medicines T. Safety of medicines: a guide to detecting and reporting adverse drug reactions: why health professionals need to take action. (WHO/EDM/QSM/2002.2). https://apps.who.int/iris/handle/10665/67378
Sultana J, Cutroneo P (2013) Trifirò G J J of pharmacology, pharmacotherapeutics. Clinical and economic burden of adverse drug reactions 4(Suppl1):S73
Lazarou J, Pomeranz BH, Corey PN (1998) Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 279(15):1200–1205. https://doi.org/10.1001/jama.279.15.1200
Onakpoya IJ, Heneghan CJ, Aronson JK (2016) Post-marketing withdrawal of 462 medicinal products because of adverse drug reactions: a systematic review of the world literature. BMC Med 14(1):10
Organization WH (2006) The safety of medicines in public health programmes: pharmacovigilance, an essential tool. Published online
Insani WN, Pacurariu AC, Mantel-Teeuwisse AK, Gross-Martirosyan L (2018) Characteristics of drugs safety signals that predict safety related product information update. Pharmacoepidemiol Drug Saf 27(7):789–796
Von Moos R, Stolz R, Cerny T, Gillessen SJS (2003) Thalidomide: from tragedy to promise. Medical Weekly 133(5/6):77–87
Kim JH, Scialli AR JT (2011) Thalidomide: the tragedy of birth defects and the effective treatment of disease. Sciences 122(1):1–6
Hughes ML, Whittlesea CMC (2002) Luscombe DK J A drug reactions, reviews toxicological. Review of national spontaneous reporting schemes 21(4):231–241
Centre, Uppsala Monitoring. “Get to Know UMC.” UMC. https://who-umc.org/about-uppsala-monitoring-centre/
Centre UM (nd) Members of the WHO programme for International Drug Monitoring. UMC. Retrieved July 4, 2022, from https://who-umc.org/about-the-who-programme-for-international-drug-monitoring/member-countries/
Lindquist M (2001) Edwards IR J TJ of rheumatology. The WHO Programme for International Drug Monitoring, its database, and the technical support of the Uppsala Monitoring Center 28(5):1180–1187
Harmonisation ICH. Histroy of ICH 17 May 2022. Available from: https://www.ich.org/page/safety-guidelines
Welcome to the New Yellow Card Reporting Site. YellowCard (nd) Retrieved July 4, 2022, from https://yellowcard.mhra.gov.uk/
Australian Government Department of Health. Therapeutic Goods Administration (nd) Blue card adverse reaction reporting form. Therapeutic Goods Administration (TGA). Retrieved July 4, 2022, from https://www.tga.gov.au/form/blue-card-adverse-reaction-reporting-form
Home (nd) Retrieved July 4, 2022, from https://cdsco.gov.in/opencms/opencms/en/Home
Singh A (2012) Bhatt P J J of pharmacology, pharmacotherapeutics. Comparative evaluation of adverse drug reaction reporting forms for introduction of a spontaneous generic ADR form 3(3):228
Clarkson A (2002) Choonara I J A of disease in childhood. Surveillance for fatal suspected adverse drug reactions in the UK 87(6):462–466
Waller PC, Coulson RA (1996) Wood SM J P, safety drug. Regulatory pharmacovigilance in the United Kingdom: current principles and practice 5(6):363–375
Lindquist M (2008) J DIJ. VigiBase, the WHO global ICSR database system: basic facts 42(5):409–419
Centre UM (nd) VigiBase: Who's global database signalling harm and pointing to safer use. UMC. Retrieved July 4, 2022, from https://www.who-umc.org/vigibase/vigibase/vigibase-signalling-harm-and-pointing-to-safer-use/
Centre UM (nd) A mine of information on potential safety risks. UMC. Retrieved July 4, 2022, from https://who-umc.org/pv-products/vigiflow/
Centre UM (nd) The who programme for International Drug Monitoring. UMC. Retrieved July 4, 2022, from https://who-umc.org/about-the-who-programme-for-international-drug-monitoring/
Postigo R, Brosch S, Slattery J et al (2018) EudraVigilance medicines safety database: publicly accessible data for research and public health protection 41(7):665–675
Waller PC, Coulson RA (1996) Wood SM J P, safety drug. Regulatory pharmacovigilance in the United Kingdom: current principles and practice 5(6):363–375
Harpaz R, DuMouchel W, LePendu P et al (2013) Performance of pharmacovigilance signal-detection algorithms for the FDA adverse event reporting system 93(6):539–546
Food and Drug Administration (2020) Adverse events reporting system(FAERS) public dashboard. https://fis.fda.gov/sense/app/d10be6bb494e-4cd2-82e4-0135608ddc13/sheet/7a47a261-d58b-4203-a8aa6d3021737452/state/analysis. Accessed 26 Jun 2020. No Title
Isah AO, Pal SN, Olsson S, Dodoo A (2012) Bencheikh RS J T advances in drug safety. Specific features of medicines safety and pharmacovigilance in Africa 3(1):25–34
Ampadu HH, Hoekman J, de Bruin ML et al (2016) Adverse drug reaction reporting in Africa and a comparison of individual case safety report characteristics between africa and the rest of the world: analyses of spontaneous reports in VigiBase®. Drug Saf 39:335–345. https://doi.org/10.1007/s40264-015-0387-4
Suku CK, Hill G, Sabblah G, Darko M, Muthuri G, Abwao E, Pandit J, Osakwe AI, Elagbaje C, Nyambayo P, Khoza S, Dodoo AN, Pal SN (2015) Experiences and lessons from implementing cohort event monitoring programmes for antimalarials in four African Countries: results of a questionnaire-based survey. Drug Saf 38(11):1115–1126. https://doi.org/10.1007/s40264-015-0331-7.PMID:26267842;PMCID:PMC4608977
Centre UM (2009) Preparing for influenza pandemic Jerry Labadie. Uppsala Reports 47.32
Biswas PJJ (2013) Pharmacovigilance in Asia. J Pharmacol Pharmacother 4(Suppl1):S7
Kimura T, Matsushita Y, Yang YK, Choi N (2011) Park B J P, safety drug. Pharmacovigilance systems and databases in Korea, Japan, and Taiwan 20(12):1237–1245
Fujiwara M, Kawasaki Y, Yamada HJ (2016) PlO A pharmacovigilance approach for post-marketing in Japan using the Japanese adverse drug event report (JADER) database and association analysis. 11(4):e0154425
Kang DY, Ahn K-M, Kang H-R (2017) Cho S-H J APA. Past, present, and future of pharmacovigilance in Korea 7(3):173–178
Lihite RJ (2015) Lahkar M J F in pharmacology. An update on the pharmacovigilance programme of India 6:194
National Medicines Regulatory Authority (NMRA) Retrieved July 4, 2022, from https://www.nmra.gov.lk/index.php?option=com_content&view=article&id=75&Itemid=185&lang=en
Guideline on pharmacovigilance - NMRA (nd) Retrieved July 4, 2022, from https://nmra.gov.lk/images/PDF/guideline/Guideline-on-Pharmacovigilance.pdf
Jayakody RL (2015) The National Medicines Regulatory Authority Act: its birth, provisions and challenges. Journal of the Ceylon College of Physicians 46:53–56
Avery AJ, Anderson C, Bond C, Fortnum H, Gifford A, Hannaford PC et al (2011) Evaluation of patient reporting of adverse drug reactions to the UK ‘yellow card scheme’: literature review, descriptive and qualitative analyses, and questionnaire surveys. Health Technol Assess
Banovac M, Candore G, Slattery J et al (2017) Patient reporting in the EU: analysis of EudraVigilance data. Drug Saf 40:629–645. https://doi.org/10.1007/s40264-017-0534-137
Margraff F, Bertram D (2014) Adverse drug reaction reporting by patients: an overview of fifty countries. Drug Saf 37:409–419. https://doi.org/10.1007/s40264-014-0162-y
Avery AJ, Anderson C, Bond CM, Fortnum H, Gifford A, Hannaford PC, Hazell L, Krska J, Lee AJ, Mclernon DJ, Murphy E (2011) Evaluation of patient reporting of adverse drug reactions to the UK ‘yellow card scheme’: literature review, descriptive and qualitative analyses, and questionnaire surveys. Health Technol Assess
Talbot JC, Nilsson BS (1998) Pharmacovigilance in the pharmaceutical industry. Br J Clin Pharmacol 45(5):427–431. https://doi.org/10.1046/j.1365-2125.1998.00713.x.PMID:9643613;PMCID:PMC1873545
Pagotto C, Varallo F (2013) Mastroianni P J I journal of technology assessment in health care. Impact of educational interventions on adverse drug events reporting 29(4):410–417
Molokhia M (2009) Improving reporting of adverse drug reactions: systematic review. Clin Epidemiol. Published online 75. https://doi.org/10.2147/CLEP.S4775
Herdeiro MT, Ribeiro-Vaz I, Ferreira M, Polónia J, Falcão A, Figueiras A (2012) Workshop- and telephone-based interventions to improve adverse drug reaction reporting. Drug Saf 35(8):655–665. https://doi.org/10.1007/BF03261962
Ribeiro-Vaz I, Silva A-M, Santos CC, Cruz-Correia RJ (2016) How to promote adverse drug reaction reports using information systems–a systematic review and meta-analysis. BMC Med Inform Decis Mak 16(1):27
Ventola CL JP (2014) Mobile devices and apps for health care professionals: uses and benefits. Therapeutics 39(5):356
Bahk CY, Goshgarian M, Donahue K et al (2015) Increasing patient engagement in pharmacovigilance through online community outreach and mobile reporting applications: an analysis of adverse event reporting for the Essure device in the US 29(6):331–340
Oosterhuis I, Taavola H, Tregunno PM et al (2018) Characteristics, quality and contribution to signal detection of spontaneous reports of adverse drug reactions via the WEB-RADR mobile application: a descriptive cross-sectional study. 41(10):969–978
Cano-Sandoval MÁ, López-Armas GC, Perfecto-Avalos Y, Vázquez-Alvarez AO (2020) Brennan-Bourdon LM %J P, Safety D. Opportunities to improve the electronic reporting system for adverse drug reactions in Mexico: a comparative evaluation with the United States of America and the European Union 29(11):1523–1526
Defer G, Le Caignec F, Fedrizzi S et al (2018) Dedicated mobile application for drug adverse reaction reporting by patients with relapsing remitting multiple sclerosis (Vigip-SEP study): study protocol for a randomized controlled trial. 19(1):1–8
Prakash J, Joshi K, Malik D et al (2019) “ADR PvPI” Android mobile app: report adverse drug reaction at any time anywhere in India. 51(4):236
Gonzalez-Gonzalez C, Lopez-Gonzalez E, Herdeiro MT, Figueiras A (2013) Strategies to improve adverse drug reaction reporting: a critical and systematic review. Drug Saf 36(5):317–328. https://doi.org/10.1007/s40264-013-0058-2 (PMID: 23640659)
Molokhia M, Tanna S, Bell D (2009) Improving reporting of adverse drug reactions: systematic review. Clin Epidemiol 9(1):75–92. https://doi.org/10.2147/clep.s4775.PMID:20865089;PMCID:PMC2943157
Li Y, Jimeno Yepes A, Xiao C (2022) Combining social media and FDA adverse event reporting system to detect adverse drug reactions. Drug Saf 43:893–903. https://doi.org/10.1007/s40264-020-00943-2
Author information
Authors and Affiliations
Contributions
T.P. Weerarathna conceived the idea. M.T. Madhushika wrote the first and subsequent drafts. T.P. Weerarathna, P.L.G.C Liyanage, and S.S. Jayasinghe developed the ideas. All the authors read and approved the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Madhushika, M.T., Weerarathna, T.P., Liyanage, P.L.G.C. et al. Evolution of adverse drug reactions reporting systems: paper based to software based. Eur J Clin Pharmacol 78, 1385–1390 (2022). https://doi.org/10.1007/s00228-022-03358-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-022-03358-3