Abstract
Purpose
Examine SSRIs’ efficacy in treating depression, anxiety, PTSD, and substance use in individuals with addiction.
Methods
From their inception until August 6, 2021, we searched Google Scholar, PubMed, Scopus, OVID MEDLINE, and Academic Search Complete. We included randomized controlled trials (RCTs) and omitted open-label studies. Bayesian analysis was performed. Bayes factor (BF) established efficacy and tau (τ) statistical heterogeneity. The RoB2 method assessed potential biases. Subgroup analysis was carried out to determine SSRI performance. Treatment duration, SSRI dosage, and attrition rate were all examined in meta-regression.
Results
We investigated 64 RCTs with 6128 participants. SSRIs reduced depressive symptoms in opioid, alcohol, cocaine, cannabis, and nicotine use disorders (d = 0.353, BF > 99); social anxiety symptoms in alcohol use disorder (d = 0.875, BF > 99); and generalized anxiety symptoms in opioid, alcohol, cocaine, marijuana, and nicotine use disorders (d = 0.346, BF = 4.236). Evidence for PTSD was inconclusive. SSRIs facilitated abstinence for opioid, alcohol, cocaine, cannabis, and nicotine use (d = 0.325, BF > 99); reduced craving for alcohol, cocaine, and nicotine use (d = 0.533, BF = 24.129); and reduced alcohol use (d = 0.452, BF > 99) and cocaine use (d = 0.255, BF = 3.87). Fluoxetine showed the highest antidepressant effect. There was no effect of attrition rate, SSRI dosage, or treatment length on SSRI's efficacy.
Conclusions
Results support the use of SSRIs to treat substance use, depression, and anxiety in individuals with addiction.
Protocol registration
PROSPERO registration number: CRD42020164944.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Substance use disorders (SUDs) and psychiatric disorders are linked to relapse, financial and social problems [1], and high medical costs [2]. SUDs co-occur in roughly 32% of people with mood disorders. 16.5% of people with mood disorders have an alcohol use disorder, and 18.5% have a SUD [3]. SUDs, mood disorders, suicide, and impulsive and self-destructive acts are linked. Suicide is common in depressed patients who use alcohol or other SUDs [3]. A 12-year prospective study found that comorbid alcohol or other SUDs reduced the recovery rate of generalized anxiety disorder (GAD) by about fivefold (risk ratio = 0.20, p = 0.01) and increased the likelihood of relapse by over threefold (risk ratio = 3.09, p = 0.05) [4]. The most common co-occurring disorders among combat veterans and civilians with post-traumatic stress disorder (PTSD) were alcohol use, depression, anxiety, conduct disorder, and non-alcohol substance abuse or dependence [5].
Chronic alcohol, nicotine, and other SUDs reduce serotonin (SERT) levels in the brain. Studies on SUDs’ neurochemical changes have shown SERT’s role from initial exposure to tolerance, withdrawal, abstinence, or relapse [6]. Most addictive drugs involve SERT. For example, in the prefrontal cortex, cannabinoid receptor 1 (cb1) stimulation reduces the effect of citalopram. Selective reuptake inhibitor (SSRI) blockade of the cb1 receptor can increase SERT levels in the prefrontal cortex [7]. Nicotine’s mechanism of action is partly related to SERT (5-HT2C) receptor agonists. 5-HT2C agonists reduce drugs’ discriminative and reinforcing effects in the midbrain [8]. Studies suggest that alcohol causes low cerebrospinal fluid 5-hydroxyindoleacetic acid and low plasma tryptophan. Different opioid receptor subtypes regulate serotonergic neurotransmission in the central nervous system (CNS). For example, mu- and delta-opioid receptor agonists increase 5-HT efflux in the dorsal raphe nucleus (DRN) [9]. However, kappa agonists reduce extracellular 5-HT in the DRN, median raphe nucleus, and forebrain [10]. Among stimulants, SERT modulates cocaine’s locomotor action [11]. Cocaine and amphetamine are controlled by the balance of dopamine (DA) and SERT release [12].
Tolerability, adherence to treatment, cost-effectiveness, general safety in overdose, and a more comprehensive range of therapeutic activities make SSRIs one of the best pharmacotherapy approaches for people with mental illnesses and addiction. In this context, research on their therapeutic benefits is limited and inconclusive.
The term “antidepressants” was used in frequentist meta-analyses to look at how well they worked to treat depression in people with SUDs. A few of these studies focused on SSRIs’ efficacy. Torrens et al. [13] concluded that SSRIs have no clinical advantages over tricyclics in SUDs. Tricyclics and nefazodone were recommended by Iovieno et al. [14], but not SSRIs. Stokes et al. [15] found no difference in treatment effects between SSRIs and non-SSRIs in individuals with depression and SUDs. Two more studies supported SSRIs. Nunes and Levin [16] suggested that antidepressants exert a modest beneficial effect on individuals with depression and SUDs. A study published in 2021 found that SSRIs may be associated with a reduction in the risk of substance misuse compared to 1 month before treatment initiation [17]. There is conflicting data regarding improving clinical outcomes when the SERT system is modulated in patients with a psychiatric disorder and comorbid SUDs. Further investigation is essential to clarify the extent of the evidence and guide therapy. Therefore, a meta-analysis of randomized controlled trials (RCTs) was undertaken using a Bayesian approach to explore SSRIs’ efficacy in treating depression, anxiety, PTSD, and substance use in individuals with SUDs.
Methods
Criteria for considering studies
This meta-analysis follows PRISMA guidelines [18] and is registered under PROSPERO registration (CRD42020164944). RCTs comparing an SSRI to a placebo or an active drug in various clinical settings were included if they involved participants of various ages, genders, and races. Open trials and laboratory experiments were excluded. The outcome of interest was efficacy as measured by SSRIs’ ability to treat depression, anxiety, and PTSD (symptom reduction on clinician rating or self-report scales) and facilitate drug abstinence, manage craving, and reduce drug use.
Identification of studies
We searched the following electronic databases: Google Scholar, PubMed, Scopus, OVID MEDLINE, and Academic Search Complete from their inception to August 6, 2021. We identified all published RCTs in any language using medical subject headings and terms such as substance use, addictive drugs, drug use, SSRIs, depression, anxiety, craving, abstinence, and SSRIs and SUDs. Here is an example of a Uniform Resource Locator (URL) search strategy: https://PubMed.ncbi.nlm.nih.gov/?term=Selective+serotonin+reuptake+inhibitors+%28SSRI%29+depression+and+other+affective+disorders+in+patients+with+substance+use+disorder.
Data collection
Two independent assessors (DF and PM) screened titles and extracted data, while a third author (AJ) resolved conflicts between DF and PM. We extracted general information such as publication status, title, authors’ names, source, country, year of publication, duplicate publication, and trial characteristics.
Bias risk assessment
We assessed articles’ quality and risk of bias using the Revised Cochrane RCT risk of bias tool [19], focusing on randomization, deviations from intended interventions, missing outcome data, outcome measurement, and reporting results.
Data synthesis
We summarized pooled results as the standardized difference between two means, Cohen’s d (“small, d = .2,” “medium, d = .5,” and “large, d = .8”) [20]. Because the random-effects model assumes that between-study heterogeneity causes the actual effect sizes of studies to differ, we, therefore, included an estimated standard deviation of underlying effects across studies, tau (τ) [21].
Frequentist meta-analysis uses a fixed state of nature to interpret a parameter of interest, while Bayesian analysis allows an unknown quantity to have a probability distribution [22]. We set prior d to 0, width parameter to 0.707, truncated Cauchy because we were 50% confident that the effect size resided somewhere between d = 0 and d = 0 0.707 [23]. We compared how well the alternative hypothesis (HA= SSRIs) or the null hypothesis (H0 = control) predicted the data in the following relationship: Prior d of HA × BF (Bayes factor) = Posterior d of HA, where BF = [Probability (data, given HA)]/[Probability (data, given H0)] postulated the likelihood of evidence of a treatment effect in place of the p-value in frequentist meta-analysis. For this analysis, a BF = 3 = posterior probability (d > 0) = 75%. The larger numbers are essentially non-interpretable; they were stated as BF > 99. The modeling procedure was as follows: adaptation: 1000, burn-in: 5000, number of iterations: 1000, and number of chains: 3. Subgroup analysis was carried out on SSRIs to tease apart the one with the most robust performance. Meta-regression was undertaken to determine whether attrition rate (5–64%), SSRI dosage (citalopram 20–100; escitalopram 10–30; fluoxetine 20–80; fluvoxamine 100–300; paroxetine 20–60; sertraline 20–200), or treatment duration (4–52 weeks) influenced SSRI's efficacy over placebo. Meta-analysis was conducted in Jeffreys’s Amazing Statistics Program, JASP Team (2020). JASP (Version 0.14.1) [Computer software] (University of Amsterdam Nieuwe Achtergracht 129B, Amsterdam, The Netherlands).
Results
The search found 2,921 articles (Fig. 1). Two thousand six hundred sixty of these were deemed irrelevant. Two hundred sixty-one articles were eligible for screening, with 153 being rejected. One hundred eight publications were suitable for data collection, but 38 did not provide data appropriate for analysis. The meta-analysis included 70 of them. One article was omitted due to data duplication [88]. Two articles did not provide statistical data suitable for the analysis [89, 90], and three articles used data from previous RCTs [91,92,93]. Sixty-four RCTs [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87] were included in the Bayesian meta-analysis. Sixty-one of the trials compared an SSRI with a placebo, and three of them used another medication as a control [78, 86, 87]. The investigation used a random sample of 6128 participants (Table 1) (Supp Table 2–15).
More than 80% of participants were male, and over 45% were Caucasian. Ages ranged from 12 to 75. Forty-four of the sixty-three trials were conducted in the USA. Around 30% were university-based, and 17% were outpatient. The treatment lasts from 4 to 52 weeks. We found fluoxetine, sertraline, paroxetine, citalopram, escitalopram, and fluvoxamine data. Fluoxetine (25) and sertraline (17) were the most studied. Twenty-nine trials had an attrition rate of 20% or more. Twelve trials had missing outcome data, while fifteen were deemed at risk of bias in the selection of the reported result.
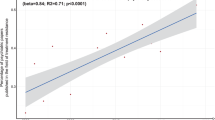
Depression, anxiety, and PTSD
Carried out with a placebo arm, a reduction in depressive symptoms (d = 0.353, BF > 99) was demonstrated for fluoxetine, sertraline, paroxetine, citalopram, escitalopram, and fluvoxamine in opioid, alcohol, cocaine, marijuana, and nicotine use disorders. Fluoxetine showed the highest antidepressant effect (Supp Fig. 11). Paroxetine, citalopram, and sertraline combined with naltrexone produced no antidepressant effect (Supp Fig. 3). Citalopram, escitalopram, fluoxetine, and sertraline reduced the severity of GAD symptoms (d = 0.345, BF = 4.236) in alcohol, cocaine, marijuana, and nicotine use disorders. Despite fluoxetine’s advantage, no SSRI outperformed the others. Paroxetine lessened social anxiety symptoms (d = 0.687, BF = 8.726) in alcohol use disorder. Sertraline’s efficacy was inconclusive for PTSD symptoms in alcohol use disorder (Supp Fig. 6). Attrition rate, SSRI dosage, or treatment duration did not show any meta-regression change of SSRI’s response over placebo for depression (n = 29) (β = 0.308, BF = 0.568), GAD (n = 5) (β = 0.389, BF = 0.742), social anxiety (n = 4) (β = 0.988, BF = 1), and PTSD (n = 2) (β = 0.477, BF = 1).
Abstinence, craving, and substance use reduction
Carried out with a placebo arm, citalopram, escitalopram, sertraline, fluvoxamine, fluoxetine, and paroxetine improved abstinence for opioid, alcohol, cocaine, cannabis, or nicotine use (d = 0.325, BF > 99). On subgroup analysis, sertraline fared better (Supp Fig. 12). A reduction in the severity of craving was noticeable for fluoxetine, citalopram, sertraline, fluvoxamine, and paroxetine in alcohol, cocaine, or nicotine use (d = 0.513, BF = 12.331). Fluoxetine showed the highest anti-craving efficacy. Fluoxetine, sertraline, paroxetine, or citalopram significantly reduced alcohol use (d = 0.438, BF > 99). Fluoxetine had the superior outcome among them. Fluoxetine, citalopram, and sertraline reduced cocaine use (d = 0.255, BF = 3.87). SSRIs had no effect on reducing opioid, nicotine, or cannabis use (Supp Fig. 13–15). Attrition rate, SSRI dosage, or treatment duration did not show any meta-regression change for abstinence (n = 22) (β = 0.401, BF = 0.192), craving (n = 8) (β = 0.489, BF = 0.381), or alcohol use reduction (n = 21) (β = 0.596, BF = 0.350). However, based on SSRI dosage, there was a trend that SSRIs had no effect in reducing cocaine use (n = 10) (β = 0.139, BF = 2,012).
Discussion
SSRIs effectively treat depression, GAD, and social anxiety in individuals with SUDs. SSRIs can also help with alcohol abstinence and craving, as well as the reduction of alcohol and cocaine use. Fluoxetine performs better than the other SSRIs. The findings of this meta-analysis agree with those of Nunes and Levin (2004) [16], indicating a beneficial, albeit modest, effect of antidepressants in the treatment of depression in patients with SUDs. The effect size in Nunes’s study was 0.20. Our investigation found 0.3, with a BF > 99. This analysis agrees with Virtanen et al. 2022 [17] and supports the author’s finding of an association between SSRIs and substance risk reduction. This investigation, however, contradicts Iovieno et al.’s conclusions [14], which indicated that SSRIs failed to treat depression in alcohol use disorder.
SSRIs do not reduce opioid, nicotine, or cannabis consumption. An unfavorable outcome resulted from the intricate interactions between SERT and the three psychoactive substances. Mu, delta, and kappa opioid receptors differently influence SERT neurotransmission in the CNS [10]. It is difficult to predict how 5-HT receptor subtypes respond to this complex interface. Similarly, subtle and varied responses to nicotine with different 5-HT receptor subtypes have been reported [6]. The cannabis system has a specific colocalization pattern with DA and SERT receptors. For example, in low-CB1-expressing cells (principal projecting neurons), CB1 colocalizes with DA receptors, D1, D2, and 5-HT1B, while in high-CB1-expressing cells, primarily gamma-aminobutyric acid (GABAergic cells), CB1 colocalizes with 5-HT3 [94]. These reactions are convoluted and unpredictable since SERT subtypes influence or target cannabinoid receptors. Albeit a small number of RCTs, no prediction can be made about SSRIs’ capacity to reduce PTSD symptoms. Unexpected PTSD symptoms may modulate the benefits of SSRIs. Targeting numerous receptors at once may help treat this complex illness. 5-HT1B receptors are essential because they control fear and anxiety [95].
More than 20% of the overall trials had elevated attrition rates or did not provide data on attrition, which raises critical questions about their study design, confounders, or other issues inherent to the population studied. Nevertheless, judging by the review authors, all the trials underwent a controlled process, and there is no deviation from ethical or scientific standards. A behavioral intervention was undertaken in more than 50% of the trials. Although their purpose was not therapeutically oriented, their impact on the expected outcomes remains unclear.
There are limitations inherent to the design of this investigation. The protocol included only RCTs, which already overemphasized potential beneficial effects, a priori, in addition to publication bias. Also, in a small number of trials, their study design was not explicitly geared toward understanding the benefit of SSRIs in SUDs. Still, the authors could extract valuable data that fit into the Bayesian model. Furthermore, this analysis is not devoid of between-study statistical heterogeneity. A tentative explanation of heterogeneity veered attention to issues related to the use of distinctive and heterogeneous scales, nonspecific outcome measures from some trials, bias in reporting results, or low sample size. Thus, there is a need for a more homogeneous method to measure the treatment effect. Increasing power seems more difficult due to the problematic nature of treating addiction with high recidivism.
SUD is linked to antidepressant resistance [96]. The symptom overlaps between GAD and substance use, or withdrawal complicates GAD diagnosis. Clinicians are hesitant to prescribe SSRIs to substance-abusing patients due to misdiagnosis and poor treatment response [97]. Around half individuals with SUDs have PTSD. They had worse results [98]. The best treatment for them is unknown. There are no therapeutic guidelines for depression, anxiety, or PTSD unique in SUDs. What works for depression, anxiety, or PTSD in the absence of SUDs may or may not work in the presence of SUDs. This study analyzes these limitations since SUDs and mental diseases should be treated in concert, not separately. There are a lot of possible outcomes that are not covered in this meta-analysis, but they still need to be investigated. These include decreased risk behaviors; social, economic, and family functioning; hospitalizations; and suicide rates.
Research may focus on the interaction between SERT and other neurotransmitters such as GABA, N-methyl-d-aspartate, cannabinoids, opioids, or norepinephrine to better and perhaps mitigate dropouts and facilitate retention in treatment for SUDs and to better understand the neurobiology of SUDs comorbid with psychiatric disorders. Overall, fluoxetine seems to be a promising candidate. One might have to weigh risks and benefits before prescribing an SSRI constantly. One might preemptively attempt to mitigate potential adverse events such as QT prolongation, serotonin syndrome, bleeding, and suicide risk.
Conclusions
SSRIs appear promising as pharmacological interventions in treating depression and anxiety in individuals with SUDs and maintaining abstinence, facilitating, and reducing substance use. There was no effect of attrition rate, SSRI dosage, or treatment length on SSRI's efficacy. This is a preliminary work that may guide treatments in diverse clinical settings. Further research could help determine how much SSRIs should be taken, how well they work, and how safe they are for individuals with SUDs and psychiatric disorders.
References
Carey KB, Purnine DM, Maisto SA, Carey MP, Simons JS (2000) Treating substance abuse in the context of severe and persistent mental illness: clinicians’ perspectives. J Subst Abuse Treat 19(2):189–198. https://doi.org/10.1016/s0740-5472(00)00094-5
Dickey B, Azeni H (1996) Persons with dual diagnoses of substance abuse and major mental illness: their excess costs of psychiatric care. Am J Public Health 86(7):973–977. https://doi.org/10.2105/ajph.86.7.973
Quello SB, Brady KT, Sonne SC (2005) Mood disorders and substance use disorder: a complex comorbidity. Sci Pract Perspect 3(1):13–21. https://doi.org/10.1151/spp053113
Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, Shea MT, Keller MB (2005) Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am J Psych 162(6):1179–1187. https://doi.org/10.1176/appi.ajp.162.6.1179
Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB (1995) Post-traumatic stress disorder in the National Comorbidity Survey. Arch Gen Psych 52(12):1048–1060. https://doi.org/10.1001/archpsyc.1995.03950240066012.
Kirby LG, Zeeb FD, Winstanley CA (2011) Contributions of serotonin in addiction vulnerability. Neuropharmacology 61(3):421–432. https://doi.org/10.1016/j.neuropharm.2011.03.022
Kleijn J, Cremers TI, Hofland CM, Westerink BH (2011) CB-1 receptors modulate the effect of the selective serotonin reuptake inhibitor, citalopram on extracellular serotonin levels in the rat prefrontal cortex. Neurosci Res 70(3):334–337. https://doi.org/10.1016/j.neures.2011.03.004
Fletcher PJ, Le AD, Higgins GA (2008) Serotonin receptors as potential targets for modulation of nicotine use and dependence. Prog Brain Res 172:361–383. https://doi.org/10.1016/S0079-6123(08)00918-7
LeMarquand D, Pihl RO, Benkelfat C (1994) Serotonin and alcohol intake, abuse, and dependence: clinical evidence. Biol Psychiat 36(5):326–337. https://doi.org/10.1016/0006-3223(94)90630-0
Tao R, Auerbach SB (2002) Opioid receptor subtypes differentially modulate serotonin efflux in the rat central nervous system. J Pharmacol Exp Ther 303(2):549–556. https://doi.org/10.1124/jpet.102.037861.2002Nov1;303(2):549-56
Carey RJ, DePalma G, Damianopoulos E (2001) Cocaine and serotonin: a role for the 5-HT(1A) receptor site in the mediation of cocaine stimulant effects. Behav Brain Res 126(1–2):127–133. https://doi.org/10.1016/s0166-4328(01)00253-4
Rothman RB, Baumann MH (2006) Balance between dopamine and serotonin release modulates behavioral effects of amphetamine-type drugs. Ann N Y Acad Sci 1074:245–260. https://doi.org/10.1196/annals.1369.064
Torrens M, Fonseca F, Mateu G, Farré M (2005) Efficacy of antidepressants in substance use disorders with and without comorbid depression. A systematic review and meta-analysis. Drug Alcohol Depend 78(1):1–22. https://doi.org/10.1016/j.drugalcdep.2004.09.004
Iovieno N, Tedeschini E, Bentley KH, Evins AE, Papakostas GI (2011) Antidepressants for major depressive disorder and dysthymic disorder in patients with comorbid alcohol use disorders: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry 72(8):1144–1151. https://doi.org/10.4088/JCP.10m06217
Stokes PRA, Jokinen T, Amawi S, Qureshi M, Husain MI, Yatham LN, Strang J, Young AH (2020) Pharmacological treatment of mood disorders and comorbid addictions: a systematic review and meta-analysis: Traitement Pharmacologique des Troubles de L'humeur et des Dépendances Comorbides: Une Revue Systématique et une Méta-Analyse. Can J Psych. Revue canadienne de psychiatrie 65(11):749–769. https://doi.org/10.1177/0706743720915420
Nunes EV, Levin FR (2004) Treatment of depression in patients with alcohol or other drug dependence: a meta-analysis. JAMA 291(15):1887–1896. https://doi.org/10.1001/jama.291.15.1887
Virtanen S, Lagerberg T, Khemiri L, Suvisaari J, Larsson H, Lichtenstein P, Chang Z, Latvala A (2022) Association of selective serotonin reuptake inhibitor (SSRI) treatment with acute substance misuse outcomes. Addiction (Abingdon, England) 117(1):234–242. https://doi.org/10.1111/add.15625
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann T, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical research ed) 372:n71. https://doi.org/10.1136/bmj.n71
Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ (Clini Res ed) 366
Borenstein M, Cohen J (1988). Statistical power analysis: a computer program. Lawrence Erlbaum Associaties, Incorporated
Harrer M, Cuijpers P, Furukawa TA, Ebert DD (2021) In: Doing Meta-Analysis with R. Chapman & Hall/CRC, Boca Raton, FL
Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR (1999) Methods in health service research. An introduction to Bayesian methods in health technology assessment. BMJ Clin Res Ed 319(7208):508–512. https://doi.org/10.1136/bmj.319.7208.508
van Doorn J, van den Bergh D, Böhm U, Dablander F, Derks K, Draws T, Etz A, Evans NJ, Gronau QF et al (2021) The JASP guidelines for conducting and reporting a Bayesian analysis. Psychon Bull Rev 28(3):813–826. https://doi.org/10.3758/s13423-020-01798-5
Carpenter KM, Brooks AC, Vosburg SK, Nunes EV (2004) The effect of sertraline and environmental context on treating depression and illicit substance use among methadone maintained opiate dependent patients: a controlled clinical trial. Drug Alcohol Depend 74(2):123–134. https://doi.org/10.1016/j.drugalcdep.2003.11.015
Dean AJ, Bell J, Mascord DJ, Parker G, Christie MJ (2002) A randomised, controlled trial of fluoxetine in methadone maintenance patients with depressive symptoms. J Affect Disord 72(1):85–90. https://doi.org/10.1016/s0165-0327(01)00419-0
Petrakis I, Carroll KM, Nich C, Gordon L, Kosten T, Rounsaville B (1998) Fluoxetine treatment of depressive disorders in methadone-maintained opioid addicts. Drug Alcohol Depend 50(3):221–226. https://doi.org/10.1016/s0376-8716(98)00032-5
Poling J, Pruzinsky R, Kosten TR, Gonsai K., Sofuoglu M, Gonzalez G et al (2007) Clinical efficacy of citalopram alone or augmented with bupropion in methadone-stabilized patients. Am J Addict 16(3):187–194. https://doi.org/10.1080/10550490701375640
Roy A (1998) Placebo-controlled study of sertraline in depressed recently abstinent alcoholics. Biol Psychiat 44(7):633–637. https://doi.org/10.1016/s0006-3223(97)00509-x
Pettinati HM, Volpicelli JR, Luck G, Kranzler HR, Rukstalis MR, Cnaan A (2001) Double-blind clinical trial of sertraline treatment for alcohol dependence. J Clin Psychopharmacol 21(2):143–153. https://doi.org/10.1097/00004714-200104000-00005
Tiihonen J, Ryynänen OP, Kauhanen J, Hakola HP, Salaspuro M (1996) Citalopram in the treatment of alcoholism: a double-blind placebo-controlled study. Pharmacopsychiatry 29(1):27–29. https://doi.org/10.1055/s-2007-979538
Gorelick DA, Paredes A(1992) Effect of fluoxetine on alcohol consumption in male alcoholics. Alcohol Clinic Exp Res 16(2):261–265. https://doi.org/10.1111/j.1530-0277.1992.tb01373.x
Cornelius JR, Salloum IM, Cornelius MD, Perel JM, Ehler JG, Jarrett PJ et al (1995) Preliminary report: double-blind, placebo-controlled study of fluoxetine in depressed alcoholics. Psychopharmacol Bull 31(2):297–303
Cornelius JR, Salloum IM, Ehler JG, Jarrett PJ (1997) Double-blind fluoxetine in depressed alcoholic smokers. Psychopharmacol Bull 33(1):165–170
Kranzler HR, Burleson JA, Korner P, Del Boca FK, Bohn MJ, Brown J et al (1995) Placebo-controlled trial of fluoxetine as an adjunct to relapse prevention in alcoholics. Am J Psychiatry 152(3):391–397. https://doi.org/10.1176/ajp.152.3.391
Janiri L, Gobbi G, Mannelli P, Pozzi G, Serretti A, Tempesta E (1996) Effects of fluoxetine at antidepressant doses on short-term outcome of detoxified alcoholics. Int Clin Psychopharmacol 11(2):109–117
Kranzler HR, Mueller T, Cornelius J, Pettinati HM, Moak D, Martin PR et al (2006) Sertraline treatment of co-occurring alcohol dependence and major depression. J Clin Psychopharmacol 26(1):13–20. https://doi.org/10.1097/01.jcp.0000194620.61868.35
Gual A, Balcells M, Torres M, Madrigal M, Diez T, Serrano L (2003) Sertraline for the prevention of relapse in detoxicated alcohol dependent patients with a comorbid depressive disorder: a randomized controlled trial. Alcohol and alcoholism (Oxford, Oxfordshire) 38(6):619–625. https://doi.org/10.1093/alcalc/agg124
Charney DA, Heath LM, Zikos E, Palacios‐Boix J, Gill KJ (2015) Poorer drinking outcomes with citalopram treatment for alcohol dependence: a randomized, double-blind, placebo-controlled trial. Alcohol Clini Exp Re 39(9):1756–1765. https://doi.org/10.1111/acer.12802
Cornelius JR, Bukstein OG, Wood DS, Kirisci L, Douaihy A, Clark DB (2009) Double-blind placebo-controlled trial of fluoxetine in adolescents with comorbid major depression and an alcohol use disorder. Addict Behav 34(10):905–909. https://doi.org/10.1016/j.addbeh.2009.03.008
Deas D, Randall CL, Roberts JS, Anton RF (2000) A double-blind, placebo-controlled trial of sertraline in depressed adolescent alcoholics: a pilot study. Hum Psychopharmacol 15(6):461–469. https://doi.org/10.1002/1099-1077(200008)15:6%3c461:AID-HUP209%3e3.0.C.O.;2-J
Cornelius JR, Salloum IM, Ehler JG, Jarrett PJ, Cornelius MD, Perel JM, Thase ME, Black A (1997) Fluoxetine in depressed alcoholics. A double-blind, placebo-controlled trial. Arch General Psych 54(8):700–705. https://doi.org/10.1001/archpsyc.1997.01830200024004
Moak DH, Anton RF, Latham PK, Voronin KE, Waid RL, Durazo-Arvizu R (2003) Sertraline and cognitive behavioral therapy for depressed alcoholics: results of a placebo-controlled trial. J Clin Psychopharmacol 23(6):553–562. https://doi.org/10.1097/01.jcp.0000095346.32154.41
Cornelius JR, Salloum IM, Haskett RF, Daley DC, Cornelius MD, Thase ME et al (2000) Fluoxetine versus placebo in depressed alcoholics: a 1-year follow-up study. Addict Behave 25(2):307–310. https://doi.org/10.1016/s0306-4603(99)00065-9
Kabel DI, Petty F (1996) A placebo-controlled, double-blind study of fluoxetine in severe alcohol dependence: adjunctive pharmacotherapy during and after inpatient treatment. Alcohol Clin Exp Res 20(4):780–784. https://doi.org/10.1111/j.1530-0277.1996.tb01686.x
Naranjo CA, Kadlec KE, Sanhueza P, Woodley-Remus D, Sellers EM (1990) Fluoxetine differentially alters alcohol intake and other consummatory behaviors in problem drinkers. Clin Pharmacol Ther 47(4):490–498. https://doi.org/10.1038/clpt.1990.62
Naranjo CA, Poulos CX, Bremner KE, Lanctot KL (1994) Fluoxetine attenuates alcohol intake and desire to drink. Int Clin Psychopharmacol 9(3):163–172. https://doi.org/10.1097/00004850-199409000-00004
Chick J, Aschauer H, Hornik K (2004) Efficacy of fluvoxamine in preventing relapse in alcohol dependence: a one-year, double-blind, placebo-controlled multicentre study with analysis by typology. Drug Alcohol Depend 74(1):61–70. https://doi.org/10.1016/j.drugalcdep.2003.11.012
Naranjo CA, Bremner KE, Lanctot KL (1995) Effects of citalopram and a brief psycho-social intervention on alcohol intake, dependence and problems. Addiction (Abingdon, England) 90(1):87–99. https://doi.org/10.1046/j.1360-0443.1995.9018712.x
Coşkunol H, Gökden O, Ercan ES, Bayraktar E, Tuğlular I, Saygılı R (2002) Long-term efficacy of sertraline in the prevention of alcoholic relapses in alcohol-dependent patients: a single-center, double-blind, randomized, placebo-controlled, parallel-group study. Curr Ther Res 63(11):759–771. https://doi.org/10.1016/S0011-393X(02)80096-0
Angelone SM, Bellini L, Di Bella D, Catalano M (1998) Effects of fluvoxamine and citalopram in maintaining abstinence in a sample of Italian detoxified alcoholics. Alcohol and alcoholism (Oxford, Oxfordshire) 33(2):151–156. https://doi.org/10.1093/oxfordjournals.alcalc.a008371
Naranjo CA, Poulos CX, Bremner KE, Lanctôt KL (1992) Citalopram decreases desirability, liking, and consumption of alcohol in alcohol-dependent drinkers. Clin Pharmacol Ther 51(6):729–739. https://doi.org/10.1038/clpt.1992.85
Eriksson M, Berggren U, Blennow K, Fahlke C, Balldin J (2001) Further investigation of citalopram on alcohol consumption in heavy drinkers: responsiveness possibly linked to the DRD2 A2/A2 genotype. Alcohol (Fayetteville, N.Y.) 24(1):15–23. https://doi.org/10.1016/s0741-8329(01)00137-9
Balldin J, Berggren U, Engel J, Eriksson M, Hård E, Söderpalm B (1994) Effect of citalopram on alcohol intake in heavy drinkers. Alcohol Clin Exp Res 18(5):1133–1136. https://doi.org/10.1111/j.1530-0277.1994.tb00093.x
Findling RL, Pagano ME, McNamara NK, Stansbrey RJ, Faber JE, Lingler J et al (2009) The short-term safety and efficacy of fluoxetine in depressed adolescents with alcohol and cannabis use disorders: a pilot randomized placebo-controlled trial. Child Adolesc Psychiatry Ment Health 3(1):11. https://doi.org/10.1186/1753-2000-3-11
Habrat B, Załoga B (2006) Skuteczność i tolerancja tianeptyny w leczeniu zaburzeń depresyjnych u pacjentów uzaleznionych od alkoholu. wieloośrodkowe badanie kontrolowane metoda podwójnie slepej próby z uzyciem fluwoksaminy [A double-blind controlled study of the efficacy and acceptability of tianeptine in comparison with fluvoxamine in the treatment of depressed alcoholic patients]. Psychiatria Polska 40(3):579–597
Moeller FG, Schmitz JM, Steinberg JL, Green CM, Reist C, Lai LY et al (2007) Citalopram combined with behavioral therapy reduces cocaine use: a double-blind, placebo-controlled trial. Am J Drug Alcohol Abuse 33(3):367–378. https://doi.org/10.1080/00952990701313686
Cornelius JR, Salloum IM, Thase ME, Haskett RF (1998) Fluoxetine versus placebo in depressed alcoholic cocaine abusers. Psychopharmacol Bull 34(1):117–121
Schmitz JM, Averill P, Stotts AL, Moeller FG, Rhoades HM, Grabowski J (2001) Fluoxetine treatment of cocaine-dependent patients with major depressive disorder. Drug Alcohol Depend 63(3):207–214. https://doi.org/10.1016/s0376-8716(00)00208-8
Oliveto A, Poling J, Mancino MJ, Williams DK, Thostenson J, Pruzinsky R et al (2012) Sertraline delays relapse in recently abstinent cocaine-dependent patients with depressive symptoms. Addiction (Abingdon, England) 107(1):131–141. https://doi.org/10.1111/j.1360-0443.2011.03552.x
Winstanley EL, Bigelow GE, Silverman K, Johnson RE, Strain EC (2011) A randomized controlled trial of fluoxetine in the treatment of cocaine dependence among methadone-maintained patients. J Subst Abuse Treat 40(3):255–264. https://doi.org/10.1016/j.jsat.2010.11.010
Covi L, Hess JM, Kreiter NA, Haertzen CA (1995) Effects of combined fluoxetine and counseling in the outpatient treatment of cocaine abusers. Am J Drug Alcohol Abuse 21(3):327–344. https://doi.org/10.3109/00952999509002701
Batki SL, Washburn AM, Delucchi K, Jones RT (1996) A controlled trial of fluoxetine in crack cocaine dependence. Drug Alcohol Depend 41(2):137–142. https://doi.org/10.1016/0376-8716(96)01233-1
Mancino MJ, McGaugh J, Chopra MP, Guise JB, Cargile C, Williams DK et al (2014) Clinical efficacy of sertraline alone and augmented with gabapentin in recently abstinent cocaine-dependent patients with depressive symptoms. J Clin Psychopharmacol 34(2):234–239. https://doi.org/10.1097/JCP.0000000000000062
Cornelius JR, Salloum IM, Haskett RF, Ehler JG, Jarrett PJ, Thase ME et al (1999) Fluoxetine versus placebo for the marijuana use of depressed alcoholics. Addict Behav 24(1):111–114. https://doi.org/10.1016/s0306-4603(98)00050-1
Cornelius JR, Bukstein OG, Douaihy AB, Clark DB, Chung TA, Daley DC et al (2010) Double-blind fluoxetine trial in comorbid MDD-CUD youth and young adults. Drug Alcohol Depend 112(1–2):39–45. https://doi.org/10.1016/j.drugalcdep.2010.05.010
Weinstein AM, Miller H, Bluvstein I, Rapoport E, Schreiber S, Bar-Hamburger R et al (2014) Treatment of cannabis dependence using escitalopram in combination with cognitive-behavior therapy: a double-blind placebo-controlled study. Am J Drug Alcohol Abuse 40(1):16–22. https://doi.org/10.3109/00952990.2013.819362
Covey LS, Glassman AH, Stetner F, Rivelli S, Stage K (2002) A randomized trial of sertraline as a cessation aid for smokers with a history of major depression. Am J Psychiatry 159(10):1731–1737. https://doi.org/10.1176/appi.ajp.159.10.1731
Niaura R, Spring B, Borrelli B, Hedeker D, Goldstein MG, Keuthen N et al (2002) Multicenter trial of fluoxetine as an adjunct to behavioral smoking cessation treatment. J Consult Clin Psychol 70(4):887–896. https://doi.org/10.1037//0022-006x.70.4.887
Saules KK, Schuh LM, Arfken CL, Reed K, Kilbey MM, Schuster CR (2004) Double-blind placebo-controlled trial of fluoxetine in smoking cessation treatment including nicotine patch and cognitive-behavioral group therapy. Am J Addict 13(5):438–446. https://doi.org/10.1080/10550490490512762
Killen JD, Fortmann SP, Schatzberg AF, Hayward C, Sussman L, Rothman M et al (2000) Nicotine patch and paroxetine for smoking cessation. J Consult Clin Psychol 68(5):883–889
Riggs PD, Mikulich-Gilbertson SK, Davies RD, Lohman M, Klein C, Stover SK (2007) A randomized controlled trial of fluoxetine and cognitive behavioral therapy in adolescents with major depression, behavior problems, and substance use disorders. Arch Pediatr Adolesc Med 161(11):1026–1034. https://doi.org/10.1001/archpedi.161.11.1026
Blondal T, Gudmundsson LJ, Tomasson K, Jonsdottir D, Hilmarsdottir H, Kristjansson F et al (1999) The effects of fluoxetine combined with nicotine inhalers in smoking cessation–a randomized trial. Addiction (Abingdon, England) 94(7):1007–1015. https://doi.org/10.1046/j.1360-0443.1999.94710076.x
Shoptaw S, Huber A, Peck J, Yang X, Liu J, Dang J et al (2006) Randomized, placebo-controlled trial of sertraline and contingency management for the treatment of methamphetamine dependence. Drug Alcohol Depend 85(1):12–18. https://doi.org/10.1016/j.drugalcdep.2006.03.005
Brady KT, Sonne S, Anton RF, Randall CL, Back SE, Simpson K (2005) Sertraline in the treatment of co-occurring alcohol dependence and post-traumatic stress disorder. Alcohol Clin Exp Res 29(3):395–401. https://doi.org/10.1097/01.alc.0000156129.98265.57
Hien DA, Levin FR, Ruglass LM, López-Castro T, Papini S, Hu MC et al (2015) Combining seeking safety with sertraline for PTSD and alcohol use disorders: a randomized controlled trial. J Consult Clin Psychol 83(2):359–369. https://doi.org/10.1037/a0038719
Randall CL, Johnson MR, Thevos AK, Sonne SC, Thomas SE, Willard SL et al (2001) Paroxetine for social anxiety and alcohol use in dual-diagnosed patients. Depress Anxiety 14(4):255–262. https://doi.org/10.1002/da.1077
Book SW, Thomas SE, Randall PK, Randall CL (2001) Paroxetine for social anxiety and alcohol use in dual-diagnosed patients. Depress Anxiety 14(4):255–262. https://doi.org/10.1002/da.1077
Book SW, Thomas SE, Smith JP, Randall PK, Kushner MG, Bernstein GA, Specker SM, Miller PM, Randall CL (2013) Treating individuals with social anxiety disorder and at-risk drinking: phasing in a brief alcohol intervention following paroxetine. J Anxiety Disord 27(2):252–258. https://doi.org/10.1016/j.janxdis.2013.02.008
Thomas SE, Randall PK, Book SW, Randall CL (2008) A complex relationship between co-occurring social anxiety and alcohol use disorders: what effect does treating social anxiety have on drinking? Alcohol Clin Exp Res 32(1):77–84. https://doi.org/10.1111/j.1530-0277.2007.00546.x
O’Malley SS, Robin RW, Levenson AL, GreyWolf I, Chance LE, Hodgkinson CA et al (2008) Naltrexone alone and with sertraline for the treatment of alcohol dependence in Alaska natives and non-natives residing in rural settings: a randomized controlled trial. Alcohol Clin Exp Res 32(7):1271–1283. https://doi.org/10.1111/j.1530-0277.2008.00682.x
Farren CK, Scimeca M, Wu R, Malley SO (2009) A double-blind, placebo-controlled study of sertraline with naltrexone for alcohol dependence. Drug Alcohol Depend 99(1–3):317–321. https://doi.org/10.1016/j.drugalcdep.2008.06.006
Petrakis IL, Ralevski E, Desai N, Trevisan L, Gueorguieva R, Rounsaville B et al (2012) Noradrenergic vs serotonergic antidepressant with or without naltrexone for veterans with PTSD and comorbid alcohol dependence. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology 37(4):996–1004. https://doi.org/10.1038/npp.2011.283
Pettinati HM, Oslin DW, Kampman KM, Dundon WD, Xie H, Gallis T et al (2010) A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. Am J Psychiatry 167(6):668–675. https://doi.org/10.1176/appi.ajp.2009.08060852
Adamson SJ, Sellman JD, Foulds JA, Frampton CM, Deering D, Dunn A et al (2015) A randomized trial of combined citalopram and naltrexone for nonabstinent outpatients with co-occurring alcohol dependence and major depression. J Clin Psychopharmacol 35(2):143–149. https://doi.org/10.1097/JCP.0000000000000287
Witte J, Bentley K, Evins AE, Clain AJ, Baer L, Pedrelli P et al (2012) A randomized, controlled, pilot study of acamprosate added to escitalopram in adults with major depressive disorder and alcohol use disorder. J Clin Psychopharmacol 32(6):787–796. https://doi.org/10.1097/JCP.0b013e3182726764
Muhonen LH, Lahti J, Sinclair D, Lönnqvist J, Alho H (2008) Treatment of alcohol dependence in patients with comorbid major depressive disorder--predictors for the outcomes with memantine and escitalopram medication. Substance Abuse Treatment, Prevention Policy 3:20. https://doi.org/10.1186/1747-597X-3-20
Han DH, Kim SM, Choi JE, Min KJ, Renshaw PF (2013) Adjunctive aripiprazole therapy with escitalopram in patients with comorbid major depressive disorder and alcohol dependence: clinical and neuroimaging evidence. Journal of psychopharmacology (Oxford, England) 27(3):282–291. https://doi.org/10.1177/0269881112472563
Muhonen LH, Lönnqvist J, Juva K, Alho H (2008) Double-blind, randomized comparison of memantine and escitalopram for the treatment of major depressive disorder comorbid with alcohol dependence. J Clin Psychiatry 69(3):392–399. https://doi.org/10.4088/jcp.v69n0308
Landabaso MA, Iraurgi I, Jimenez-Lerma JM, Sanz J, Corres BF, Araluce K et al (1998) A randomized trial of adding fluoxetine to a naltrexone treatment programme for heroin addicts. Addiction (Abingdon, England) 93(5):739–744. https://doi.org/10.1046/j.1360-0443.1998.9357399.x
Farren CK, O’Malley S (2002) A pilot double blind placebo-controlled trial of sertraline with naltrexone in the treatment of opiate dependence. Am J Addict 11(3):228–234. https://doi.org/10.1080/10550490290088009
Zorick T, Sugar CA, Hellemann G, Shoptaw S, London ED (2011) Poor response to sertraline in methamphetamine dependence is associated with sustained craving for methamphetamine. Drug Alcohol Depend 118(2–3):500–503. https://doi.org/10.1016/j.drugalcdep.2011.04.015
Bashiri M, Mancino MJ, Stanick VA, Thostenson J, Kosten TR, Oliveto AH (2017) Moderators of response to sertraline versus placebo among recently abstinent, cocaine dependent patients: a retrospective analysis of two clinical trials. Am J Addict 26(8):807–814. https://doi.org/10.1111/ajad.12635
Kranzler HR, Armeli S, Tennen H (2012) Post-treatment outcomes in a double-blind, randomized trial of sertraline for alcohol dependence. Alcohol Clinic Exp Res 36(4):739–744. https://doi.org/10.1111/j.1530-0277.2011.01659.x4
Kelmendi B, Adams TG, Yarnell S, Southwick S, Abdallah C, Krystal JH (2016) PTSD: from neurobiology to pharmacological treatments. Eur J Psychotraumatol 7:31858. https://doi.org/10.3402/ejpt.v7.31858
Hermann H, Marsicano G, Lutz B (2002) Coexpression of the cannabinoid receptor type 1 with dopamine and serotonin receptors in distinct neuronal subpopulations of the adult mouse forebrain. Neuroscience 109(3):451–460. https://doi.org/10.1016/s0306-4522(01)00509-7
Brenner P, Brandt L, Li G, DiBernardo A, Bodén R, Reutfors J (2020) Substance use disorders and risk for treatment resistant depression: a population-based, nested case-control study. Addiction 115(4):768–777
Brady KT, Haynes LF, Hartwell KJ, Killeen TK (2013) Substance use disorders and anxiety: a treatment challenge for social workers. Social work in public health 28(3–4):407–423. https://doi.org/10.1080/19371918.2013.774675
Berenz EC, Coffey SF (2012) Treatment of co-occurring post-traumatic stress disorder and substance use disorders. Curr Psych Rep 14(5):469–477. https://doi.org/10.1007/s11920-012-0300-0
Author information
Authors and Affiliations
Contributions
D.F. initiated the project, developed the protocol, and searched articles in databases. D.F. and P.M. screened titles and extracted data. D.F., P.M., A.J., V.K., and C.P. reviewed the reference lists of retrieved articles for additional reports. D.F. and P.M. reviewed the full texts for selection/exclusion. D.F., P.M., A.J., V.K., and C.P. checked screening and selection. D.F. and P.M. conducted risk of bias assessment. D.F., P.M., A.J., V.K., and C.P. reviewed the outline. D.F. prepared tables and figures and drafted the methods and results sections and the introduction and discussion. D.F., P.M., A.J., and V.K. reviewed and provided intellectual contributions to the draft manuscript. D.F., P.M., A.J., V.K., and C.P. approved the final draft.
Corresponding author
Ethics declarations
Ethics approval
The authors reviewed anonymized data from published literature. Therefore, no informed consent or ethical approval was required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fluyau, D., Mitra, P., Jain, A. et al. Selective serotonin reuptake inhibitors in the treatment of depression, anxiety, and post-traumatic stress disorder in substance use disorders: a Bayesian meta-analysis. Eur J Clin Pharmacol 78, 931–942 (2022). https://doi.org/10.1007/s00228-022-03303-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-022-03303-4