Abstract
Purpose
STOPPFrail criteria highlight instances of potentially inappropriate medications (PIMs) in frailer older adults with poor 1-year survival prognosis. The objectives of this study were to (i) determine the proportion of older adults requiring long-term nursing care in whom STOPPFrail criteria are applicable, (ii) measure the prevalence of STOPPFrail PIMs, and (iii) identify risk factors for PIMs in this cohort.
Methods
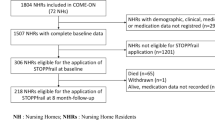
We retrospectively reviewed applications for long-term nursing care to nursing homes in the Cork area over a 6-month period. We recorded diagnoses, medications, functional status, cognitive ability, frailty status, and applied STOPPFrail criteria as appropriate.
Results
We reviewed 464 applications; 38 were excluded due to incomplete information and 274 patients (64.3%) met STOPPFrail eligibility criteria (median age 83 years (IQR 77.25–88); 233 (54.7%) female). Those STOPPFrail eligible were prescribed 2194 medications (mean 8, (SD 4)), of which 828 (37.7%) were PIMs. At least one PIM was identified in 250 eligible patients (91.2%). The median number of PIMs was 3 (IQR 2–4), the most common being (i) medications without clear indication identified in 47.0% (n = 129) of patients, (ii) long-term high-dose proton pump inhibitors in 31.4% (n = 86), and (iii) statins in 29.6% (n = 81). For every additional medication prescribed, the odds of identifying a PIM increased by 58% (odds ratio 1.58, 95% CI 1.32–1.89, p < 0.001).
Conclusion
Almost 65% of patients awaiting long-term care are eligible for the application of STOPPFrail criteria with over 90% prescribed at least one PIM. Transition to nursing home care represents an opportunity to review therapeutic appropriateness and goals of prescribed medications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Older adults requiring admission to long-term care facilities are often frail [1], multi-morbid [2], have a high burden of medication use [3], and poor survival prognosis [4]. These patients are frequently prescribed potentially inappropriate medications (PIMs) [5], which often predispose to adverse drug reactions (ADRs) and excess morbidity and mortality [6]. Many medications prescribed in the last year of life are continued from when they were originally commenced years earlier for the purposes of halting disease progression and/or preventing long-term disease complications [7]. However, therapeutic goals may change over time because of advancing or severe frailty and poor survival prognosis, thus rendering such prescriptions potentially inappropriate. In such instances, physicians are often reluctant to deprescribe long-term preventative medications for various reasons including time constraints, resistance to change by patients and their relatives, fear of causing adverse outcomes, fear of litigation, knowledge deficiency, paucity of clear deprescribing guidelines, and lack of evidence-based research on deprescribing [8,9,10,11].
STOPPFrail (Screening Tool of Older Person’s potentially inappropriate Prescriptions in Frail Older Adults with limited life expectancy) criteria were devised as a deprescribing aid to highlight instances of PIM use in frailer older adults with poor 1-year survival prognosis [12]. Patient eligibility for application of STOPPFrail criteria includes the following variables: (i) the presence of end-stage irreversible pathology, (ii) poor 1-year survival prognosis, (iii) severe functional impairment or severe cognitive impairment or both, and (iv) where symptom control is the priority rather than prevention of disease progression. STOPPFrail content was validated by Delphi consensus in which 17 senior academic clinicians, representing geriatric medicine, clinical pharmacology, palliative medicine, old age psychiatry, primary care, and clinical pharmacy, participated [12]. This resulted in an explicit list of 27 PIMs organised according to physiological systems. The inter-rater reliability of STOPPFrail criteria is good when deployed by physicians practising across different specialties, with its application taking a mean (SD) of 2.7 (0.94) minutes per clinical case [13]. Currently, the prevalence of PIM use, according to STOPPFrail criteria, in frailer older patients awaiting long-term nursing care is unknown.
In the Republic of Ireland, the majority of older adults requiring long-term nursing care are assessed by the Nursing Home Support Scheme (NHSS) operated by the National Health Service Executive. Over a 5-year period, the average number of NHSS applications per year, nationally, was 10,482 (range 9323 to 12,697) [14]. Prior to NHSS application, a comprehensive care needs assessment is performed by a multi-disciplinary team led by geriatricians or psychiatrists of old age. Through this standardised assessment, an applicants’ medical, functional, cognitive, social status and medication prescription details are documented. Therefore, the NHSS application contains comprehensive information about applicants’ clinical, functional and prescription details to facilitate reliable application of STOPPFrail criteria to identify PIMs in eligible patients.
The objectives of this study were to (i) determine the proportion of adults requiring long-term nursing care eligible for application of STOPPFrail criteria and (ii) determine the prevalence and risk factors for STOPPFrail PIMs in these patients.
Methods
Study design, setting, and participants
The application for long-term nursing care incorporates a comprehensive multi-disciplinary assessment of patients’ comorbidities, concurrent medications, activities of daily living, and functional and cognitive status. These are presented using a Common Summary Assessment Report (CSAR). All CSARs are submitted to the local NHSS office from the relevant placement panel, i.e., a multi-disciplinary panel led by a consultant geriatrician that reviews the comprehensive multi-disciplinary assessment for long-term care. Once the application is approved by this panel, it is then sent to the local NHSS office for processing. Adults of all ages and all socioeconomic backgrounds are eligible to apply for long-term care through this scheme. All CSARs submitted to the local NHSS office between January 1 and June 30, 2016, were retrospectively reviewed by one senior physician in geriatric medicine, who was a member of the research team and was not involved in the care of these patients. At the time of application, patients applying for long-term care resided either at home, in hospital, or were already in emergency nursing home accommodation.
The local NHSS office is part of the health service executive (HSE) responsible for the administration side of long-term care applications for the Cork area and is located in Cork City. All applications for the time frame above were reviewed on site at the NHSS office, from December 1, 2016, to February 15, 2017. The local Clinical Research Ethics Committee at University College Cork (UCC) approved the study protocol. Consent was not required as all CSARs were anonymised with only a unique patient identifier available to the research team.
All persons 65 years and older applying for nursing home care were eligible for study inclusion. Comparison was made between those eligible for the application of STOPPFrail criteria and those not. Using an estimated 20% prevalence of ≥ 1 PIM, a margin of error of 5% and a 95% level of confidence, a minimum sample of 246 patients was required to assess the rate of STOPPFrail PIMs in the STOPPFrail cohort.
Data collection
We extracted the following details from patients’ CSARs: (i) standard demographic details, (ii) medical diagnoses, (iii) medications and doses, (iv) Barthel Index score [15], (v) mini-mental state examination (MMSE) score [16], and (vii) frailty status using the Rockwood Clinical Frailty Scale [17]. Supplementary clinical information was present in the form of a clinical letter by the treating consultant, clarifying medical diagnoses and severity of conditions for some applications.
Recorded medications were those prescribed at the time of NHSS application. Short-term medications documented on the CSAR were excluded from evaluation, e.g. heparinoids for deep vein thrombosis prophylaxis. Polypharmacy was defined as the daily intake of ≥ 6 drugs and major polypharmacy as the daily consumption of ≥ 11 drugs [18]. Comorbidity burden was quantified using the Cumulative Illness Rating Scale (CIRS) [19].
Determination of potentially inappropriate prescribing practices using STOPPFrail criteria
STOPPFrail eligibility was determined, by a senior physician in geriatric medicine, based on the four eligibility criteria: (i) the presence of end-stage irreversible pathology, (ii) poor 1-year survival prognosis, (iii) severe functional impairment or severe cognitive impairment or both, and (iv) where symptom control is the priority rather than prevention of disease progression. This was based on clinical judgement from all the information provided. Uncertainty regarding STOPPFrail eligibility was treated conservatively; i.e., the patient was deemed not to be STOPPFrail eligible in such circumstances. For some applications, a paucity of information was evident and these persons were excluded.
STOPPFrail prescribing criteria were applied to eligible patients. The presence or absence of a PIM was categorised as a dichotomous variable; i.e., a medication was either potentially inappropriate according to STOPPFrail criteria or not. Some prescriptions could pertain to one or more STOPPFrail criteria (e.g. a drug may have no clear indication and also be listed elsewhere in the criteria as being inappropriate) but for the purpose of this study the identification of one drug was categorised as being inappropriate, regardless of whether or not it fulfilled one or more STOPPFrail criteria. Uncertainty regarding the appropriateness of a prescription was treated conservatively; i.e., the prescribing decision was deemed to be appropriate in such circumstances.
Statistical analysis
Statistical analysis was performed using SPSS© software version 22. Descriptive data were reported using the mean and standard deviation (SD) for normally distributed variables and median and interquartile range (IQR) for non-parametric variables. Differences in the distribution of categorical variables were compared using the Pearson chi-square (χ2) test and continuous variables using the independent t test. The Mann-Whitney U and Kruskal-Wallis tests were used to determine independence of two or more non-parametric variables respectively. Comparison was made between those eligible for the application of STOPPFrail criteria and those not. Multivariate logistic regression was used to examine the influence of gender, age, dementia, number of medical conditions, and number of medications on PIM occurrence. The Hosmer & Lemeshow statistic was used to test the goodness-of-fit of the regression model. A probability value of < 0.05 was considered statistically significant.
Results
General population demographics
Four hundred sixty-four long-term care applications were retrospectively reviewed, of which 38 were excluded due to incomplete information. Of the remaining 426 patients, 233 (55%) were female. The median age of all applicants was 83 (IQR 77.25–88) years with a mean MMSE score of 16.6 (SD 7) and a mean Barthel score of 9.2 (SD 4.7). Per Rockwood’s clinical frailty 0.7% (n = 1) were terminally ill, 18.8% (n = 80) were very severely frail, 63.6% (n = 271) were severely frail, 16% (n = 68) were moderately frail, 0.5% (n = 2) mildly frail, 0.5% (n = 2) were vulnerable, 0.2% (n = 1) were managing well, and 0.2% (n = 1) were well. Patients had a mean of 7.3 (SD 2.6) diagnoses, with a mean CIRS score of 12.7 (SD 4.4). The most common diagnoses were dementia (62.4%), hypertension (46%), constipation (41.3%), depression (35.9%), and dyslipidaemia (26.3%).
A total of 3332 medications were prescribed to all 426 applicants (mean 7.8 (SD 3.9)); Polypharmacy and major polypharmacy were identified in 46% and 23%, respectively. The most frequently prescribed medications were proton pump inhibitors (PPIs) prescribed to 47.9% of patients, paracetamol (38.2%), osmotic laxatives (36.9%), anti-platelets (33.3%), beta-blockers (31.2%), neuroleptic antipsychotics (30.5%), vitamin D (30%), and selective serotonin re-uptake inhibitors (23.7%).
Comparison between STOPPFrail eligible patients and others
Of the 426 NHSS application assessed, 274 (64.3%) met STOPPFrail eligibility criteria. Differences between older adults that met STOPPFrail eligibility criteria and those that did not are displayed in Table 1. Patients STOPPFrail eligible were older (83.5 (IQR 78.75–88) vs 80 (IQR 70.25–86) years; p < 0.001), had lower mean MMSE scores (14.6 (SD 7.0) vs 21.0 (SD 5.6); p < 0.001), and had lower mean Barthel Index scores (7.6 (SD 4.3) vs 12.0 (SD 3.9); p = 0.03). As expected, STOPPFrail eligible patients had higher levels of frailty on the Rockwood Clinical Frailty Scale (χ2 (7) ≥ 93.616, p ≤ 0.001); i.e., they were more likely to be severely frail (68.2% vs 55.3%; p = 0.008) or very severely frail (26.3% vs 5.3%; p ≤ 0.001). Patients eligible for STOPPFrail assessment had a higher mean number of conditions (7.3 (SD 2.6) vs 6.4 (SD 2.5); p < 0.001) and were more likely to have dementia (73.4% vs 42.8%; p < 0.001), faecal incontinence (55.8% vs 30.9%; p < 0.001), urinary incontinence (81% vs 54.6%; p < 0.001), and osteoporosis (25.2% vs 15.1%; p < 0.016), as well as higher comorbidity burden (CIRS scores 13.6 (SD 4.4) vs 10.9 (SD 3.8); p < 0.001).
A life-limiting diagnosis was required for the application of STOPPFrail criteria. Of those STOPPFrail eligible, 51% had advanced dementia and a further 19% had advanced dementia with another life-limiting diagnosis. Those who had dementia as a life-limiting illness were either experiencing recurrent infections or of maximum dependency with significant dysphagia. In comparison, dementia was present in 42.8% of patients in whom STOPPFrail criteria were not applicable, but in its earlier stages. Cancer was the life-limiting diagnosis in 5.7% of patients, stroke in 4.7%, chronic lung disease in 3.8%, heart failure in 0.9%, and Parkinson’s disease in 0.9%. Among the 6.6% classified as “others,” life-limiting diagnoses included end-stage liver disease, multi-system atrophy, motor neuron disease, and multiple sclerosis.
A total of 2194 medications were prescribed to the 274 STOPPFrail eligible patients. Differences identified in medication use between adults that met STOPPFrail eligibility criteria and those that did not are displayed in Table 2. There was no difference in the mean number of medications prescribed to those STOPPFrail eligible and others (8 (SD 4) vs 7.5 (SD 3.7); p = 0.183). In addition, there was no significant difference in the prevalence rates of polypharmacy (67.1% vs 69%; p = 0.526) and major polypharmacy (24.8% vs 19.7%, p = 0.233) between those STOPPFrail eligible and others. Patients eligible for STOPPFrail assessment had more prescriptions for aldosterone antagonists (5.8% vs 1.3%; p = 0.026), laxatives (40.1% vs 30.9%; p = 0.005), and nutritional supplements (26.3% vs 17.1%; p = 0.029). Consistent with a higher prevalence of dementia, they also had more prescriptions for acetyl cholinesterase inhibitors (21.9% vs 11.2%; p = 0.023) and memantine (19.0% vs. 10.5%; p = 0.006). In contrast, anti-coagulants were less frequently prescribed to STOPPFrail eligible patients (15.0% vs 23.0%; p = 0.037).
PIMs as determined by STOPPFrail criteria
Among those patients eligible for STOPPFrail criteria, 828 of 2512 (37.7.0%) prescriptions were potentially inappropriate. These were identified in 250 of 274 patients (91.2%). One STOPPFrail PIM was identified in 38 patients (13.9%), 2 PIMs in 55 patients (20.1%), 3 PIMs in 48 patients (17.5%), 4 PIMs in 50 patients (18.2%), 5 PIMs in 34 patients (12.4%), 6 PIMs in 17 patients (6.2%), 7 PIMs in 4 patients (1.5%), 8 PIMs in 2 patients (0.7%), 10 PIMs in 1 patient (0.4%), and 11 PIMs in 1 patient (0.4%). Males and females were equally likely to be prescribed 1, 2, or ≥ 3 PIMs (χ2 (3) ≥ 0.567, p = 0.904). The median number of PIMs per patient was 3 (IQR 2–4).
The most frequently encountered PIMs identified by STOPPFrail criteria are detailed in Table 3. These include (i) medications without clear indication (47.0%), (ii) long-term high-dose proton pump inhibitors (31.4%), (iii) lipid-lowering therapies (29.6%), (iv) nutritional supplements (25.5%), and (v) neuroleptics (24.5%). Females were more likely to be inappropriately prescribed medications without clear indication (52.6% vs 24.1%; p = 0.05), anti-platelets for primary prevention (23.3% vs 5.5%; p = 0.002), calcium supplementation (33.5% vs 6%; p < 0.001), and anti-resorptive therapy for osteoporosis (16.3% vs 2.5%; p = 0.002). Males were more likely to be prescribed alpha-adrenergic blockers for hypertension (3.5% vs 0.65%; p = 0.011), neuroleptics (19.6% vs 18%; p = 0.005), and alpha-adrenergic blockers with concurrent long-term urinary catheters (1.5% vs 0%; p = 0.047).
Risk factors for STOPPFrail PIMs
Logistic regression was used to determine the influence of age, gender, dementia, number of conditions, and number of medications on the risk of receiving a STOPPFrail PIM (Table 4). The number of prescribed medications was significantly associated with an increased risk of receiving a STOPPFrail PIM, controlling for gender, age, presence of dementia, and the number of medical conditions. For every additional medication prescribed, the odds of receiving a STOPPFrail PIM increased by 58%% (odds ratio 1.58, 95% CI 1.32–1.89; p < 0.001).
Discussion
This study identified that 64.3% of older adults who applied for long-term nursing care, through the NHSS application process, between January 1 and June 30, 2016, from one area in Ireland, met STOPPFrail eligibility criteria. As expected, STOPPFrail eligible patients were older, more cognitively impaired, more functionally dependent, and measurably frailer than those who were not STOPPFrail eligible. In addition, STOPPFrail eligible patients had significantly more medical conditions. The most prevalent life-limiting condition in these STOPPFrail eligible was advanced dementia, identified in 70% of cases.
Despite the fact that STOPPFrail eligible patients had a poor 1-year survival prognosis, they received similar amounts of daily medications as all other patients applying for long-term care. PIM use was highly prevalent among STOPPFrail patients with 37.7% of prescriptions identified as potentially inappropriate affecting 91.2% of patients. Previous studies by O’Sullivan et al. and Ryan et al. have reported PIM prevalence rates, using STOPP criteria, of 13.7% in 70% of nursing home residents and 12.9% in 59.8% of nursing home residents, respectively [20, 21]. Lower prevalence rates reported in these studies are accounted for by the fact that STOPP criteria were developed to identify PIMs in the general older adult population and not PIMs in frailer multi-morbid older adults with a poor survival prognosis. Prescribing needs for these patients differ from those of the general population. STOPP criteria do not suggest discontinuing major drug classes that are least likely to have benefits in the last year of life, e.g. statins [22]. Therefore, the population at the highest risk of inappropriate prescribing (IP) is the group where there is the least clear guidance on prescribing and deprescribing for physicians. STOPPFrail criteria aim to address this.
The most common STOPPFrail PIMs identified in this study were medications without clear indication (47.0%), long-term high-dose PPIs (31.4%), and lipid-lowering therapies (29.6%). Fifty-one percent of the population studied had advanced dementia; therefore unsurprisingly, neuroleptics were prescribed potentially inappropriately to 24.5% of those studied. They are commonly prescribed for the treatment of behavioural and psychological symptoms of dementia, despite their limited effectiveness and risk profile. Varying daily neuroleptic prescription prevalence rates in nursing homes have been reported worldwide: 11% in Hong Kong, 26–27% in Canada, 34% in Switzerland, 38% in Finland [23], 32.8% in Europe [24], and 22 to 25% in the USA [25, 26]. In Ireland, one study focusing on PIM use in nursing home residents reported that 14.4% of PIMs were neuroleptic agents [20]. The higher prescription rate of neuroleptics in this study suggests that their prescription often precedes nursing home placement in frailer, older people in Ireland. Therefore, STOPPFrail criteria could be used by physicians at points of care transition, such as hospital discharge and admission to nursing homes for long-term care to identify inappropriate prescriptions and optimise medication use.
STOPPFrail criteria have the potential to assist physicians with deprescribing across all healthcare settings, and not just those attending patients awaiting nursing home care or those residing in nursing homes. A recent study by Curtin et al. reports that the use of STOPPFrail criteria to address inappropriate prescribing in multi-morbid older hospitalised patients with advanced frailty and poor survival prognosis had moderate agreement with gold standard specialist geriatrician-led deprescribing (Cohen’s Kappa 0.60) [27], suggesting that it could be a reasonable alternative to a specialist review. Physicians are frequently under time pressure where completing medication reviews and using criteria like STOPPFrail can encourage identification of medications that can potentially be deprescribed in a time-efficient structured fashion [13]. Studies have shown that the application of STOPP criteria, when applied by an experienced geriatrician, improve medication appropriateness [28, 29] and reduce incident in-hospital ADRs [30]. Similarly, through appropriate deprescribing, STOPPFrail criteria could potentially reduce IP, ADRs, and their associated morbidity and mortality. However, randomised controlled trials (RCTs) need to be undertaken to assess whether the application of STOPPFrail criteria can improve prescribing and improve patient outcomes. One such RCT looking at the discontinuation of PIMs according to STOPPFrail criteria in older adults entering long-term care is currently under way in Cork (ClinicalTrials.gov Identifier: NCT03501108).
O’Connor et al. showed that the application of STOPP/START criteria to hospitalised inpatients reduced the median medication cost at discharge significantly from €90.62, IQR €49.38–162.53 in the control group to €73.16, IQR €38.68–121.72) in the intervention group [30]. Similarly, by providing explicit deprescribing criteria in a subpopulation of older people, STOPPFrail criteria offer the potential to lower drug treatment costs. This study identified that more than one in three medications prescribed at the time of nursing home application were potentially inappropriate. If those medication were deemed inappropriate by their treating physician and consequently stopped, the number of daily medication prescribed to these patients could be reduced, reducing the burden and potentially reducing medication costs for patients. In most developed nations, adults aged ≥ 85 years are the fastest growing cohort of the population [31] and multi-morbidity is most prevalent in this population cohort, with prevalence rates of over 80% reported [32] and correspondingly high levels of polypharmacy and inappropriate prescribing (IP). Several studies demonstrate the extent of health budget wastage resulting from ADRs [33, 34]. In tandem, overall expenditure on prescription medications for older people is one of the fastest growing areas of all healthcare expenditure. In recent years in Ireland, Europe, and the USA, annual medication expenditure continues to rise [35,36,37].
This study has limitations. STOPPFrail eligibility and the prevalence of PIMs were made based on patients’ CSAR applications without a clinical review. Therefore, uncertainty regarding STOPPFrail eligibility and the appropriateness of a prescription were treated conservatively. In view of this, IP could be higher than what is reported here. In addition, CSAR applications are often completed during an acute admission and it is possible that medication changes occurred after the application was made; i.e., some mediations deemed inappropriate in patients in this study may have been stopped prior to nursing home placement. CSARs are often completed by the most junior staff member on the medical team and it is possible that some information was inadvertently excluded or that some information on the CSARs was inaccurate. One senior physician specialising in geriatric medicine with experience in the clinical assessment of older adults and experience applying STOPPFrail criteria completed all assessments. This could have been strengthened by two clinicians working independently to verify assessments.
In summary, this study of older adults’ medications, while awaiting long-term care, identified that more than one in three medications were potentially inappropriate. STOPPFrail can assist physicians in identifying inappropriate prescriptions in patients awaiting long-term care and can be applied prior to nursing home admission to improve medication appropriateness in older frailer multi-morbid adults with a poor 1-year survival prognosis.
References
Kojima G (2015) Prevalence of frailty in nursing homes: a systematic review and meta-analysis. J Am Med Dir Assoc 16(11):940–945
Moore KL, Boscardin WJ, Steinman MA, Schwartz JB (2014) Patterns of chronic co-morbid medical conditions in older residents of U.S. nursing homes: differences between the sexes and across the age span. J Nutr Health Aging 18(4):429–436
Onder G, Liperoti R, Fialova D et al (2012) Polypharmacy in nursing home in Europe: results from the SHELTER study. J Gerontol A Biol Sci Med Sci 67(6):698–704
Kelly A, Conell-Price J, Covinsky K, Cenzer IS, Chang A, Boscardin WJ, Smith AK (2010) Length of stay for older adults residing in nursing homes at the end of life. J Am Geriatr Soc 58(9):1701–1706
Heppenstall CP, Broad JB, Boyd M, Hikaka J, Zhang X, Kennedy J, Connolly MJ (2016) Medication use and potentially inappropriate medications in those with limited prognosis living in residential aged care. Australas J Ageing 35(2):E18–E24
Tosato M, Landi F, Martone AM, Cherubini A, Corsonello A, Volpato S, Bernabei R, onder G, on behalf of Investigators of the CRIME Study (2014) Potentially inappropriate drug use among hospitalised older adults: results from the CRIME study. Age Ageing 43(6):767–773
Todd A, Husband A, Andrew I, Pearson SA, Lindsey L, Holmes H (2017) Inappropriate prescribing of preventative medication in patients with life-limiting illness: a systematic review. BMJ Support Palliat Care 7(2):113–121
Ailabouni NJ, Nishtala PS, Mangin D, Tordoff JM (2016) Challenges and enablers of deprescribing: a general practitioner perspective. PLoS One 11(4):e0151066
Palagyi A, Keay L, Harper J, Potter J, Lindley RI (2016) Barricades and brickwalls – a qualitative study exploring perceptions of medication use and deprescribing in long-term care. BMC Geriatr 16(1):1–11
Harriman K, Howard L, McCracken R (2014) Deprescribing medication for frail elderly patients in nursing homes: a survey of Vancouver family physicians. B C Med J 56(9)
Schuling J, Gebben H, Veehof LJG, Haaijer-Ruskamp FM (2012) Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC Fam Pract 13:56
Lavan AH, Gallagher P, Parsons C, O'Mahony D (2017) STOPPFrail (Screening Tool of Older Persons Prescriptions in Frail adults with limited life expectancy): consensus validation. Age Ageing 46(4):600–607
Lavan AH, Gallagher P, O'Mahony D (2017) Inter-rater reliability of STOPPFrail [Screening Tool of Older Persons Prescriptions in Frail adults with limited life expectancy] criteria amongst 12 physicians. Eur J Clin Pharmacol 74(3):331–338
The Deparment of Health, Healthy Ireland and the National Patient Safety Office. Review of the Nursing Homes Support Scheme, A Fair Deal
Mahoney FI, Barthel DW (1965) Functional evaluation: the barthel index. Maryland state medical journal 14:61–65
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173(5):489–495
Bushardt RL, Massey EB, Simpson TW, Ariail JC, Simpson KN (2008) Polypharmacy: misleading, but manageable. Clin Interv Aging 3(2):383–389
Linn BS, Linn MW, Gurel LEE (1968) Cumulative illness rating scale. J Am Geriatr Soc 16(5):622–626
O’Sullivan D, O’Mahony D, Parsons C et al (2013) A prevalence study of potentially inappropriate prescribing in Irish long-term care residents. Drugs Aging 30:39–49
Ryan C, O’Mahony D, Kennedy J et al (2013) Potentially inappropriate prescribing in older residents in Irish nursing homes. Age Ageing 42:116–120
Narayan SW, Nishtala PS (2018) Population-based study examining the utilization of preventive medicines by older people in the last year of life. Geriatr Gerontol Int 18(6):892–898
Feng Z, Hirdes JP, Smith TF, Finne-Soveri H, Chi I, du Pasquier JN, Gilgen R, Ikegami N, Mor V (2009) Use of physical restraints and antipsychotic medications in nursing homes: a cross-sectional study. Int J Geriatr Psychiatry 24(10):1110–1118
Foevel AD, Liperoti R, Onder G et al (2014) Use of antipsychotic drugs among residents with dementia in European long-term care facilities: results from the SHELTER study. J Am Med Dir Assoc 15(12):911–917
Briesacher BA, Tjia J, Field T, Peterson D, Gurwitz JH (2013) Antipsychotic use among nursing home residents. JAMA 309(5):440–442
Kamble P, Chen H, Sherer J, Aparasu RR (2008) Antipsychotic drug use among elderly nursing home residents in the United States. Am J Geriatri Pharmacother 6(4):187–197
Curtine D, Dukelow T, James K et al (2018) Deprescribing in multi-morbid older people with polypharmacy: agreement between STOPPFrail explicit criteria and gold standard deprescribing using 100 standardized clinical cases. Eur J Clin Pharmacol
Gallagher P, O’Connor M, O’Mahony D (2011) Prevention of potentially inappropriate prescribing for elderly patients: a randomized controlled trial using STOPP/SART criteria. Clin Pharmacol Ther 89(6):845–854
Dalleur O, Boland B, Losseau C, Henrard S, Wouters D, Speybroeck N, Degryse JM, Spinewine A (2014) Reduction of potentially inappropriate medication use using the STOPP criteria in frail older inpatients: a randomised controlled study. Drugs Aging 31(4):291–298
O’Connor MN, O’Sullivan D, Gallagher PF et al (2016) Prevention of hospital-acquired adverse drug reactions in older people using screening tool of older persons’ prescriptions and screening tool to alert to right treatment criteria: a cluster randomized controlled trial. J Am Geriatr Soc 64(8):1558–1566
National Institue on Ageing and National Institutes of Health (2011) World Health Organisation: Global Health and Ageing
Salive ME (2013) Multimorbidity in older adults. Epidemiol Rev 35:75–83
Moore N, Lecointre D, Noblet C, Mabille M (1998) Frequency and cost of serious adverse drug reactions in a department of general medicine. Br J Clin Pharmacol 45(3):301–308
Leendertse AJ, Van Den Bemt PM, Poolman JB, Stoker LJ, Egberts AC, Postma MJ (2011) Preventable hospital admissions related to medication (HARM): cost analysis of the HARM study. Value Health 14(1):34–40
Barry M, Usher C, Tilson L (2010) Public drug expenditure in the Republic of Ireland. Expert Rev Pharmacoecon Outcomes Res 10(3):239–245
Executive Agency for Health and Consumers – EAHC – European Commission (2012) EU Pharmaceutical expenditure forecast
Aitken M, Berndt ER, Cutler DM (2009) Prescription drug spending trends in the United States: looking beyond the turning point. Health Aff 28(1):w151–w160
Funding
This research has been funded as part of the SENATOR project funded by the European Union’s Seventh Framework Program (EU FP7) programme (grant number 305930). Health Research Board Clinical Research Facility at University College Cork (HRB CRF-C).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The local Clinical Research Ethics Committee at University College Cork (UCC) approved the study protocol.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lavan, A.H., O’Mahony, D. & Gallagher, P. STOPPFrail (Screening Tool of Older Persons’ Prescriptions in Frail adults with a limited life expectancy) criteria: application to a representative population awaiting long-term nursing care. Eur J Clin Pharmacol 75, 723–731 (2019). https://doi.org/10.1007/s00228-019-02630-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02630-3