Abstract
Purpose
The study aims to evaluate the impact of recipients’ and donors’ polymorphisms in multidrug resistance-associated protein 2 (MRP2) gene ABCC2 -24C>T and 1249G>A on disposition of mycophenolic acid (MPA) and their interaction with cyclosporine (CsA) (compared to tacrolimus, TAC) in stable de novo adult renal transplant patients of Croatian origin.
Methods
A total of 68 recipient-donor pairs were genotyped. Steady-state pharmacokinetics of MPA was assessed by the model-independent method.
Results
Adjusted for MPA formulation, renal function, type of calcineurin inhibitor and recipients’ and donors’ genotypes at the two loci, donors’ A-allele at 1249G>A was associated with a reduced peak (29%) and early (AUC0–2, 33%) exposure and increased MPA clearance (26%). Donors’ A-allele combined with CsA was associated with 78% higher MPA clearance, 49% lower early and 48% lower total exposure as compared to wild type homozygosity + TAC. Recipients’ SNPs per se did not reflect on MPA disposition. However, A-allele at 1249G>A + CsA (compared to wild type + TAC) was associated with a numerically greater increase in MPA clearance (59 vs. 41%), reduction in total exposure (36 vs. 27%) and increase in absorption rate (C max/AUC) (56 vs. 37%) than observed for the main effect of CsA. Less pronounced effects were observed for the combination of variant allele at -24C>T and CsA.
Conclusion
Considering MPA disposition, data indicate: donors’ ABCC2 1249G>A polymorphism increases clearance and reduces exposure; CsA increases clearance and reduces exposure by inhibiting MRP2 in the gut, the liver, and the kidney; donors’ ABCC2 1249G>A polymorphism enhances the renal CsA effect, while recipients’ polymorphism seems to enhance the liver and the gut CsA effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mycophenolic acid (MPA) is an antimetabolite immunosuppressant of choice in solid organ transplantation. Regardless of the (oral) formulation (immediate-release ester pro-drug mycophenolate mofetil, MMF, or enteric-coated sodium salt, EC-MPS), pharmacokinetics (PK) of MPA is complex and variable; hence, MPA is subject to therapeutic drug monitoring (TDM) [1, 2].
MPA is extensively metabolized in the liver by glucuronidation to inactive MPA-phenyl-glucuronide (MPAG) and a minor acyl-MPAG. Glucuronides are largely excreted into the bile, deglucuronidated in the gut, and contributed to MPA enterohepatic re-circulation accounting for 10–61% of total MPA exposure (a second increase in concentration 6–12 h after dosing). Final elimination is by the kidney apparently by active secretion (MPAG) involving organic anion transporters [1]. Reduced renal function reduces MPAG/MPA elimination and increases total circulating MPA. Exposure to MPA is strongly related to its effects in renal transplant recipients: low(er) area under the concentration-time curve over dosing interval and pre-dose levels increase the risk of acute rejections [3, 4].
Variability in MPA PK is due to a number of factors including gender, serum albumin, renal function, co-medication, and genetics [1]. Regarding the latter two, calcineurin inhibitors (CNIs) included in standard immunosuppressant protocols in renal transplantation, cyclosporine A (CsA) and tacrolimus (TAC), affect exposure to MPA with more profound effects of CsA [1, 5]. CsA increases MPA clearance and reduces pre-dose levels. Inhibition of the multidrug resistance-associated protein 2 (MRP2/ABCC2) resulting in a reduced enterohepatic re-circulation of MPAG/MPA is considered to be the main CsA effect [5,6,7]. MRP2, a member of the ATP-binding cassette (ABC) transporter superfamily, is expressed at the apical hepatocyte membrane, the luminal membrane of the proximal renal tubular cells, in the intestinal epithelium, placenta, and some other organs. Both MPA and MPAG are substrates for MRP2, and MRP2 is considered the main transporter in MPAG excretion in the liver [8], although this role was suggested also for the breast cancer resistance protein (BCRP/ABCG2) [9]. Animal studies indicate the role of MRP2 in MPAG/MPA transport in the kidneys. In vitro, CsA potently inhibits MRP2-mediated MPAG transport, while TAC has no effect [10].
Several SNPs in the ABCC2 gene encoding MRP2 might partly explain variability in MPA PK. In vitro, ABCC2 -24C>T variant (rs717620) decreases the ABCC2 promoter activity [11]. Recipients’ variant allele carriage at this locus had no major impact on MPA disposition in several studies in solid organ transplant patients [12,13,14,15,16], but an “additive” effect to the effect of SNPs in glucuronidation enzymes has been suggested [17]. Moreover, the ABCC2 -24C>T might modify the effect of CsA on MRP2 [18,19,20]. The ABCC2 1249G>A SNP in exon 10 (rs2273697) (valine-to-isoleucine at position 417) in vitro has no effect on MRP2 expression or activity [21] but appears associated with a reduced expression of MRP2 in preterm placenta [22]. To our knowledge, there have been no reports to indicate relevance of this SNP for disposition of MPA.
Little is known about potential effects of the donors’ ABCC2 SNPs in renal transplantation. Certain variant alleles, but not -24C>T or 1249G>A, were reported associated with delayed graft function [23]. However, there have been no reports on effects of donors’ ABCC2 SNPs on exposure to MPA. Here, we investigate the impact of recipients’ and donors’ ABCC2 -24C>T and 1249G>A on steady-state exposure to MPA and their interaction with CsA, an inhibitor of several transporter proteins [24] in stable de novo renal transplant patients.
Patients and methods
Study outline
This prospective observational study was approved by the institutional Ethics Committee and is outlined in Fig. 1. Study procedures were described in detail previously [25]. Briefly, renal transplant recipients on a standard immunosuppressant treatment including MPA, a CNI (CsA or TAC), and corticosteroids for 5–8 days (i.e., 4–7 days after transplantation) (attained steady-state of MPA, CsA, and TAC) were included if meeting the predefined criteria: (1) informed consent; (2) stable clinical condition based on a close monitoring over the pre-study days (Fig. 1): (a) no surgical complications, (b) no signs of graft dysfunction/rejection, (c) no severe comorbidity (cardiovascular, hepatic, metabolic, infections, gastrointestinal), (d) low immunological risk, (e) serum creatinine ≤300 μmol/L (or estimated glomerular filtration rate ≥14 mL/min/1.73 m2) and by at least 1/3 lower than the initial value (first postoperative day) and stable diuresis at around 60 mL/h, (f) serum albumin >31 g/L; (3) not treated with proton pump inhibitors, antacids, phosphate binders, oral iron, magnesium or calcium, rifampicin, or any antibiotics during the pre-study and study days. A standard immunosuppressive protocol consisted of (a) EC-MPS (Myfortic®, Novartis, Switzerland) or MMF (CellCept®, Roche, Switzerland), (b) CsA (microemulsion formulation, Neoral®, Novartis, Switzerland) or TAC (Prograf®, Astellas Pharma Ireland), (c) prednisone (Decortin®, Merck, Germany) or methylprednisolone (Medrol®, Pfizer, Italy) starting post transplantation at 60 mg/day prednisone-equivalent dose for 3 days with a rapid reduction to 30 mg/day. All drugs were obtained commercially and their assignment was at the discretion of the attending physician.
Study flow. See “Patients and Methods” for details. Renal transplant recipients on immunosuppressive therapy (based on mycophenolic acid and cyclosporine or tacrolimus) for 5–8 days meeting predefined criteria were included in the present analysis of steady-state pharmacokinetics of mycophenolic acid during a dosing interval based on data obtained through routine therapeutic drug monitoring. EC-MPS enteric-coated myocophenolate sodium, MMF mycophenolate mofetil immediate-release formulation, CsA cyclosporine, TAC tacrolimus, MPA mycophenolic acid
Bioanalytical methods
Blood samples were drawn immediately before 08:00 H to determine trough concentrations of CsA, TAC, and MPA, followed by drug administration and six serial blood samples for determination of the MPA profile during the dosing interval at 0.5, 1, 2, 3, 8, and 12 h post-dose (Fig. 1). Whole blood CsA and TAC were determined by a validated affinity column-mediated immunoassay (Siemens, Germany). Total plasma MPA was determined by high pressure liquid chromatography (HPLC) with UV/VIS spectrophotometric detector and Turbochrom software (Perkin Elmer, USA) using a commercially available HPLC kit and reverse-phase column for MPA in plasma (Chromsystems, Germany). All analytes were included in the external proficiency testing scheme (RfB and UK NEQUAS). Serum creatinine and estimated glomerular filtration rate (eGFR) were determined as previously described [25].
Genotyping
Genomic DNA was isolated from whole blood using BioSprint 15 DNA Blood Kit (Qiagen, Hilden, Germany) on KingFisher mL System (Thermo Labsystems, Vantaa, Finland). Analysis of the ABCC2 -24C>T and 1249G>A was performed on an Applied Biosystems 7500 Real-Time PCR System according to the manufacturer’s instructions (Applied Biosystems, CA, USA) using a validated TaqMan® Drug Metabolism Genotyping Assays (Applied Biosystems, CA, USA). Assay IDs were for ABCC2 -24C>T C_2814642_10 and for 1249G>A C_22272980_20.
Pharmacokinetic analysis
Steady-state PK parameters of MPA were determined by non-compartmental method (Kinetica 4.1, InnaPhase Corp., USA): peak concentration (C max,ss) (mg/L); time to peak concentration (T max,ss) (hours); area under the concentration-time curve (AUCτ, ss by the log-linear method) (mg × h/L); pre-dose concentrations (C 0, C 12) (mg/L); apparent total body clearance (CLT/F,ss) (mL/min/kg), and peak-trough fluctuation (%PTF). Partial area under the curve AUC0–2 and C max/AUCτ ratio as an indicator of the absorption rate [26] were also determined. The analysis was based on dose-normalized concentrations accounting for the fact that 1000 mg of MMF corresponded to 739 mg of MPA and 1000 mg of EC-MPS corresponded to 936 mg of MPA.
Sample size and data analysis
No exact a priori sample size calculation was done since assignment of CNI (CsA or MPA) was not directed and variability of the PK outcomes and prevalence of variant alleles in the population were largely unknown. The enrollment continued until the smallest CNI (CsA or MPA)-by-genotype subset (wild-type or variant allele carriage) attained 12 subjects. A comparison between any two 12 vs. 12 patients subset has 80% power to detect a difference of at least 50% (geometric means ratio ≥1.5 or ≤0.67) at two-sided alpha level assuming a relatively conservative coefficient of variation of 35%. Such a difference could be reasonably considered as potentially clinically relevant. Ln-transformed PK parameters were analyzed by fitting general linear models to obtain the adjusted effects of CsA (vs. TAC), recipients’ and donors’ genotype, and their interactions. Results are expressed as geometric mean ratios (GMRs). Adjustment for multiple comparisons was by the simulation method. We used SAS 9.4 (SAS Inc., Cary, NC).
Results
Patient characteristics
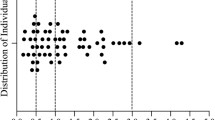
A total of 68 patients were included. Recipients’ and donors’ ABCC2 genotypes indicated no departure from Hardy-Weinberg equilibrium and no linkage disequilibrium between the loci (electronic supplementary material Table S1). Table 1 summarizes demographic, renal function, and other characteristics in respect to recipients’ and donors’ genotypes.
Effects of MPA formulation, CNI, and recipients’ and donors’ ABCC2 SNPs on steady-state pharmacokinetics of MPA
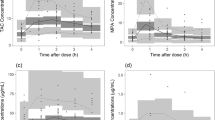
Concentration-time MPA profiles by formulation, CNI, and ABCC2 genotypes are depicted in electronic supplementary material (Fig. S1). Table 2 summarizes pharmacokinetic parameters by genotype.
PK parameters were analyzed with the following effects: MPA formulation, CNI type, eGFR, recipients’ and donors’ ABCC2 genotypes (both loci) dichotomized as minor allele carriage vs. wild type. The adjusted main effects are depicted in Fig. 2. There appeared no effect of MPA formulation except for a trend of lower troughs (C 0, C 12) with MMF. CsA-treated patients had significantly lower C 0 (45%), AUCτ (27%), and AUC0–2 (24%) and higher CLT/F (41%), %PTF (54%), and C max/AUCτ (38%) than those of TAC-treated patients. The CsA effect was consistent by MPA formulation (not shown). Recipients’ minor allele carriage at either locus had no apparent effect except for a tendency of lower C 12 in A-allele carriers at 1249G>A, but the estimate was imprecise (GMR=0.637, 95% CI 0.378–1.073). Donors’ T-allele carriage at -24C>T was associated with a tendency of lower C 0, but the estimate was imprecise (GMR=0.650, 95% CI 0.414–1.019). However, donors’ A-allele at 1249G>A was associated with a significantly lower C max (29%) and a lower AUC0–2 (33%) (Fig. 2).
Adjusted effects of mycophenolic acid (MPA) formulation (mycophenolate mofetil, MMF vs. enteric-coated sodium salt, EC-MPS), cyclosporine (CsA) compared to tacrolimus (TAC) and recipients’ and donors’ ABCC2 genotypes at locus -24C>T and locus 1249G>A on steady-state pharmacokinetics of MPA. Ln-transformed data for each pharmacokinetic parameter were analyzed in a separate general linear model (effects, MPA formulation, calcineurin inhibitor, estimated glomerular filtration rate, recipients’ genotype at ABCC2 locus −24 dichotomized as CC or T-allele carriage, recipients’ genotype at ABCC2 locus 1249 dichotomized as GG or A-allele carriage and donors’ genotypes at the two loci dichotomized in the same way) and derived contrasts are expressed as geometric means ratios (GMR) with 95% confidence intervals. C max,ss peak plasma concentration at steady-state, C 0 morning pre-dose trough, C 12 evening trough, AUC t,ss area under the concentration-time curve during dosing interval at steady-state, %PTF peak-trough fluctuation, AUC 0–2 partial AUC over the first 2 h
Joint effects of CsA and recipients’ ABCC2 SNPs
PK parameters were analyzed with the same effects as in Fig. 2 plus interactions between recipients’ -24C>T or 1249G>A genotype and CNI. The adjusted effects of the recipients’ minor allele carriage (vs. wild type), CsA (vs. TAC), and of minor allele combined with CsA (vs. wild type + TAC) are depicted in Fig. 3. A combination of CsA and 1249A was associated with a reduction in AUCτ and an increase in clearance that were numerically greater than the main effects of CsA (36 vs. 27, 59 vs. 41%, respectively). Similar additive effects were observed regarding increased C max/AUCτ and %PTF, whereas the effect on AUC0–2 appeared numerically “opposing” to the main CsA effect (Fig. 3). CsA and -24T combination effect appeared numerically “opposing” to the main CsA effect regarding AUCτ, clearance and AUC0–2, and additive regarding increased C max/AUCτ and %PTF (Fig. 3).
Joint effects of the recipients’ minor allele carriage at locus -24 or locus 1249 in ABCC2 and treatment with cyclosporine (CsA) on steady-state pharmacokinetics of mycophenolic acid. Ln-transformed data for each pharmacokinetic parameter were analyzed in a separate general linear model (effects, MPA formulation, calcineurin inhibitor (CNI; CsA or tacrolimus, TAC), estimated glomerular filtration rate, donors’ genotypes at ABCC2 locus -24 dichotomized as CC or T-allele carriage, donors’ genotype at ABCC2 locus 1249 dichotomized as GG or A-allele carriage, recipients’ genotypes at the two loci dichotomized in the same way and an interaction term between the recipients’ minor allele carriage (each locus) and calcineurin inhibitor) and derived contrasts are expressed as geometric means ratios (GMR) with 95% confidence intervals. Adjustments for multiple comparisons were by the simulation method. C max,ss peak plasma concentration at steady-state, T max,ss time of peak concentration, AUC t,ss area under the concentration-time curve during dosing interval at steady-state, %PTF peak-trough fluctuation, AUC 0–2 partial AUC over the first 2 h
Joint effects of CsA and donors’ ABCC2 SNPs
PK parameters were analyzed with the same effects as in Fig. 3, but interactions were between donors’ -24C>T or 1249G>A genotype and CNI. The adjusted effects of the donors’ minor allele carriage (vs. wild type), CsA (vs. TAC), and of minor allele combined with CsA (vs. wild type + TAC) are depicted in Fig. 4. A combination of CsA and 1249A was associated with a reduction in AUCτ (38%) and AUC0–2 (49%) and an increase in clearance (78%) that were numerically greater than the main effects of CsA (28, 28, and 40%, respectively), while the effects of the combination appeared numerically “opposing” to the main CsA effects regarding C max/AUCτ and %PTF (Fig. 4). A combination of CsA and -24T was associated with a reduction in AUCτ (35%) and increase in clearance (50%) that was numerically greater than the main CsA effects (24 and 37%, respectively). Similar additivity was observed regarding C max/AUCτ and %PTF (increase), but not regarding AUC0–2 (Fig. 4).
Joint effects of the donors’ minor allele carriage at locus -24 or locus 1249 in ABCC2 and treatment with cyclosporine (CsA) on steady-state pharmacokinetics of mycophenolic acid. Ln-transformed data for each pharmacokinetic parameter were analyzed in a separate general linear model (effects, MPA formulation, calcineurin inhibitor (CNI; CsA or tacrolimus, TAC), estimated glomerular filtration rate, recipients’ genotypes at ABCC2 locus −24 dichotomized as CC or T-allele carriage, recipients’ genotype at ABCC2 locus 1249 dichotomized as GG or A-allele carriage, donors’ genotypes at the two loci dichotomized in the same way and an interaction term between the donors’ minor allele carriage (each locus) and calcineurin inhibitor) and derived contrasts are expressed as geometric means ratios (GMR) with 95% confidence intervals. Adjustments for multiple comparisons were made by the simulation method. C max,ss peak plasma concentration at steady-state, T max,ss time of peak concentration, AUC t,ss area under the concentration-time curve during dosing interval at steady-state, %PTF peak-trough fluctuation, AUC 0-2 partial AUC over the first 2 h
Discussion
The effects of CNIs and of genetic factors have attracted much attention in investigations of the variability of MPA pharmacokinetics. Currently, only UGT1A9 genotype is considered a relevant biomarker to predict initial dosing of MPA in patients co-treated with TAC [27]. However, ABCC2 variants have been extensively evaluated as potential sources of MPA PK variability, per se, as well as molecular basis for the effects of CsA. Present study is specific in that it accounted for both the recipients’ and donors’ genotypes, bearing in mind MRP2-mediated renal MPAG/MPA transport. The study has limitations; as it was observational (routine TDM), it did not include MPAG measurements and did not account for glucuronidation enzyme or other transporter genotypes. The PK blood sampling schedule was guided by the TDM requirement of an AUCτ based on at least six sampling points and might have been suboptimal for detection of t max. However, it has several strengths—by inclusion/exclusion criteria and simultaneous adjustments for renal function and recipients’ and donors’ genotypes at both loci, a fair control of confounding was achieved; all treatment-by-genotype subsets were large enough to detect potentially relevant effects (the smallest compared subsets contained 16 vs. 12 patients, Fig. 4). Under these circumstances, there appeared no major main effect of the donors’ variant allele -24T on PK of MPA. However, donors’ variant allele 1249A was associated with a reduced peak (C max, 29%) and early exposure (AUC0–2, 33%) co-incident with an increased clearance (26%, p = 0.091) (Fig. 2). These findings are indicative of an increased renal elimination. The fact that total exposure and trough values were not proportionally reduced (15–20% lower AUCτ, C0 and C 12, p > 0.05) might be explained by the (assumed) “second wave of MPA exposure” due to MPAG/MPA enterohepatic re-circulation—AUCτ might have been reduced less than AUC0–2 on the account of an “input” occurring after the 2nd post-dose hour. Unfortunately, “late partial AUC” was not informative since there were only three sampling points over 10 later hours (Fig. S1). Still, a trend towards lower %PTF (by 20%, p > 0.05) indirectly supports such a possibility as it reflects a difference between C max (reduced) and C min (reduced, but less so). In mechanistic terms, this is in line with the role of MRP2 as a major efflux protein and with association of the variant allele with lower MRP2 expression [22]. In such a scenario, MPAG/MPA would be more available for tubular secretion resulting in an increased clearance. Indirectly, this possibility is supported by additive effects of CsA (an MRP2 inhibitor as opposed to TAC) and variant allele carriage: reductions in AUCτ and AUC0–2 and increase in clearance were all numerically greater in 1249A carriers co-treated with CsA (vs. wild-type homozygosity + TAC) than the main effects of CsA (Fig. 4). Similar effects regarding AUCτ (reduction) and clearance (increase) were observed also for the combination of CsA and donors’ variant allele carriage at ABCC2 -24C>T but are difficult to interpret since no main effect of the T-allele was observed (Fig. 4). However, the differences between the T-allele + CsA combination and CC + TAC combination were numerically greater than the main CsA effects suggesting a greater MRP2 inhibition by CsA when variant allele was present. Overall, data suggest that the donors’ ABCC2 polymorphisms may affect exposure to MPA per se and/or by increasing susceptibility to inhibition of tubular MRP2 by CsA.
The lack of the main effects of either ABCC2 -24C>T or ABCC2 1249G>A recipients’ SNPs on MPA is in line with previous reports [9, 12,13,14,15,16], but present data suggest that the recipients’ ABCC2 SNPs could moderate the effect of CsA on MRP2. The observed main effects of CsA (compared to TAC) are generally consistent with the reported [6, 24] increased clearance and reduced exposure to MPA. Increased clearance (41%) is in agreement with reduced morning trough (45%) total (AUCτ, 27%) and early (AUC0–2, 24%) exposure (Fig. 2). This is consistent with the reported CsA inhibition of the MRP2-mediated hepatic MPAG excretion and inhibited enterohepatic re-circulation of MPAG/MPA [6, 7]. As already discussed, present data suggest a relevant contribution of the renal MRP2 inhibition to the increased MPA clearance. The fact that C max was not affected should be viewed in parallel with the increased C max/AUCτ (38%) (Fig. 2)—increased absorption rate suggests MRP2 inhibition at the intestinal level and could have “compensated” for the effect of increased clearance on peak exposure. The increased %PTF (53%) (Fig. 2) is an understandable consequence of an increased clearance and unchanged peak exposure. Therefore, the present observations appear plausible when viewed in the light of the (assumed) simultaneous effects of CsA on MRP2 at the intestinal, hepatic, and renal levels. Such a view is further supported by the apparent additive effects of the recipients’ variant allele 1249A and CsA (Fig. 3): The differences between the A-allele + CsA combination and wild-type homozygosity + TAC combination in respect to clearance, total exposure, absorption rate, and %PTF were all numerically greater than the main CsA effects. Lack of such an effect on AUC0–2 should be viewed in the light of the (additively) increased C max/AUCτ—additionally increased absorption rate might have “compensated” for the effect of an increased clearance not only in respect to C max but also, in part, in respect to early exposure. To our knowledge, this is the first indication that the recipients’ ABCC2 1249G>A polymorphism might moderate the effects of CsA on MRP2 since previous studies in renal transplant recipients [18,19,20] focused on the -24C>T SNP. The results have been in part conflicting. In a study in patients co-treated with TAC [19], variant allele was associated with higher MPA trough, while in a study in CsA co-treated patients, no such effect was seen [20]. One study included [18] both genetic and co-treatment patient subsets (CsA vs. TAC or sirolimus). Raw AUC0–12 values on day 7 for T-allele overall (50.0, n = 14) were similar to wild type overall (46.6, n = 23); for CsA overall (40.2, n = 22) were 27% lower (p = 0.009) than for TAC/sirolimus overall (55.2, n = 17); whereas values for CsA+T-allele (51.9, n = 7) were 17% lower than those of TAC/sirolimus + wild type (62.8, n = 9). The present data also suggest that the recipients’ -24Tallele could actually “act in opposition” to CsA regarding MPA clearance/disposition (Fig. 4): Adjusted differences between T-allele carriers co-treated with CsA and wild-type homozygotes co-treated with TAC regarding clearance, AUCτ, and AUC0–2 were all numerically smaller than the main CsA effects indicating a reduced CsA effect. The seemingly additive effect on C max/AUCτ (consistent with a trend of increased C max for the T-allele + CsA combination vs. wild-type homozygosity + TAC combination, 34%, p = 0.163; Fig. 3) suggests a possibility of a different CsA–T-allele interaction at the intestinal vs. the hepatic level.
High inter-individual variability in MPA pharmacokinetics in renal transplant recipients is largely due to genetic factors: polymorphisms of MPA metabolizing enzymes (UGT1A9 [27], UGT2B7 [14, 16]) and various transporter proteins (MRP2 [8, 10], BCRP [9], SLCO1B3 or 1B1 [12, 28]); CNIs are substrates of polymorphic CYP3A4/5 and P-glycoprotein/ABCB1 [29]; CsA in particular inhibits CYPs and UGTs and a range of drug transporters [7, 8, 10, 30] where the extent of CsA effects might be affected by their polymorphisms. Hence, a polygenic approach is needed to achieve a comprehensive understanding of the gene-drug and gene-moderated drug-drug interactions. In this respect, the present study is clearly limited and its results should be viewed within these limitations.
Conclusions
The present study is an initial exploration of a potential interaction between effects of CsA and of recipients’ and donors’ ABCC2 gene variants on disposition of MPA in renal transplant recipients. Since it is based only on plasma MPA pharmacokinetics, arising inferences are largely indirect. With these limitations in mind, the present results are in agreement with the view that CsA reduces MPA disposition by inhibiting enterohepatic cycle (MRP2 inhibition). However, they indicate that the recipients’ ABCC2 -24T>C and 1249G>A SNPs might moderate the effects of CsA on MRP2. Data also indicate that CsA might reduce MPA disposition at the renal level as well, by inhibiting MRP2. Finally, to our knowledge, the present results are first to indicate that the donors’ ABCC2 genotype may influence disposition of MPA—variant allele carriage at 1249G>A per se appears to reduce the exposure to MPA (likely by increasing renal MPAG/MPA clearance) and apparently acts in the “same direction” as CsA at the renal level.
References
Tett SE, Saint-Marcoux F, Staatz CE, Brunet M, Vinks AA, Miura M et al (2011) Mycophenolate, clinical pharmacokinetics, formulations and methods for assessing drug exposure. Transplant Rev 25:47–57. doi:10.1016/j.trre.2010.06.001
van Hest R, Mathot R, Vulto A, Weimar W, van Gelder T (2005) Predicting the usefulness of therapeutic drug monitoring of mycophenolic acid: a computer simulation. Ther Drug Monit 27:163–167
van Gelder T, Hilbrands LB, Vanrenterghem Y, Weimar W, de Fijter JW, Squifflet JP et al (1999) A randomized double-blind, multicenter plasma concentration controlled study of the safety and efficacy of oral mycophenolate mofetil for the prevention of acute rejection after kidney transplantation. Transplantation 68:261–266
Kiberd BA, Lawen J, Fraser AD, Keough-Ryan T, Belitsky P (2004) Early adequate mycophenolic acid exposure is associated with less rejection in kidney transplantation. Am J Transplant 4:1079–1083
van Gelder T, Hilbrands LB, Vanrenterghem Y, Weimar W, de Fijter JW, Squifflet JP et al (2001) Comparison of the effects of tacrolimus and cyclosporine on the pharmacokinetics of mycophenolic acid. Ther Drug Monit 23:119–128
Hesselink DA, van Hest RM, Mathot RA, Bonthuis F, Weimar W, de Bruin RW et al (2005) Cyclosporine interacts with mycophenolic acid by inhibiting the multidrug resistance-associated protein 2. Am J Transplant 5:987–994
Cremers S, Schoemaker R, Scholten E, den Hartigh J, König-Quartel J, van Kan E et al (2005) Characterizing the role of enterohepatic recycling in the interactions between mycophenolate mofetil and calcineurin inhibitors in renal transplant patients by pharmacokinetic modelling. Br J Clin Pharmacol 60:249–256
Westley IS, Brogan LR, Morris RG, Evans AM, Sallustio BC (2006) Role of Mrp2 in the hepatic disposition of mycophenolic acid and its glucuronide metabolites: effect of cyclosporine. Drug Metab Dispos 34:261–266
Miura M, Kagaya H, Satoh S, Inoue K, Saito M, Habuchi T et al (2008) Influence of drug transporters and UGT polymorphisms on pharmacokinetics of phenolic glucuronide metabolite of mycophenolic acid in Japanese renal transplant recipients. Ther Drug Monit 30:559–564. doi:10.1097/FTD.0b013e3181838063
El-Sheikh AA, Koenderink JB, Wouterse AC, van den Broek PH, Verweij VG, Masereeuw R et al (2014) Renal glucuronidation and multidrug resistance protein 2-/ multidrug resistance protein 4-mediated efflux of mycophenolic acid: interaction with cyclosporine and tacrolimus. Transl Res 164:46–56. doi:10.1016/j.trsl.2014.01.006
Haenisch S, Zimmermann U, Dazert E, Wruck CJ, Dazert P, Siegmund W et al (2007) Influence of polymorphisms of ABCB1 and ABCC2 on mRNA and protein expression in normal and cancerous kidney cortex. Pharmacogenomics J 7:56–65
Miura M, Satoh S, Inoue K, Kagaya H, Saito M, Inoue T et al (2007) Influence of SLCO1B1, 1B3, 2B1 and ABCC2 genetic polymorphisms on mycophenolic acid pharmacokinetics in Japanese renal transplant recipients. Eur J Clin Pharmacol 63:1161–1169
van Schaik RH, van Agteren M, de Fijter JW, Hartmann A, Schmidt J, Budde K et al (2009) UGT1A9 -275T>A/-2152C>T polymorphisms correlate with low MPA exposure and acute rejection in MMF/tacrolimus-treated kidney transplant patients. Clin PharmacolTher 86:319–327. doi:10.1038/clpt.2009.83
Zhao W, Fakhoury M, Deschênes G, Roussey G, Brochard K, Niaudet P et al (2010) Population pharmacokinetics and pharmacogenetics of mycophenolic acid following administration of mycophenolate mofetil in de novo pediatric renal-transplant patients. J Clin Pharmacol 50:1280–1291. doi:10.1177/0091270009357429
Ruiz J, Herrero MJ, Bosó V, Megías JE, Hervás D, Poveda JL et al (2015) Impact of single nucleotide polymorphisms (SNPs) on immunosuppressive therapy in lung transplantation. Int J Mol Sci 16:20168–20182. doi:10.3390/ijms160920168
Ting LS, Benoit-Biancamano MO, Bernard O, Riggs KW, Guillemette C, Ensom MH (2010) Pharmacogenetic impact of UDP-glucuronosyltransferase metabolic pathway and multidrug resistance-associated protein 2 transport pathway on mycophenolic acid in thoracic transplant recipients: an exploratory study. Pharmacotherapy 30:1097–1108. doi:10.1592/phco.30.11.1097
Fukuda T, Goebel J, Cox S, Maseck D, Zhang K, Sherbotie JR et al (2012) UGT1A9, UGT2B7, and MRP2 genotypes can predict mycophenolic acid pharmacokinetic variability in pediatric kidney transplant recipients. Ther Drug Monit 34:671–679. doi:10.1097/FTD.0b013e3182708f84
Lloberas N, Torras J, Cruzado JM, Andreu F, Oppenheimer F, Sánchez-Plumed J, Spanish Pharmacogenetic Symphony Substudy Group et al (2011) Influence of MRP2 on MPA pharmacokinetics in renal transplant recipients-results of the Pharmacogenomic Substudy within the Symphony Study. Nephrol Dial Transplant 26:3784–3793. doi:10.1093/ndt/gfr130
Naesens M, Kuypers DR, Verbeke K, Vanrenterghem Y (2006) Multidrug resistance protein 2 genetic polymorphisms influence mycophenolic acid exposure in renal allograft recipients. Transplantation 82:1074–1084
Baldelli S, Merlini S, Perico N, Nicastri A, Cortinovis M, Gotti E et al (2007) C-440T/T-331C polymorphisms in the UGT1A9 gene affect the pharmacokinetics of mycophenolic acid in kidney transplantation. Pharmacogenomics 8:1127–1141
Hirouchi M, Suzuki H, Itoda M, Ozawa S, Sawada J, Ieiri I et al (2004) Characterization of the cellular localization, expression level, and function of SNP variants of MRP2/ABCC2. Pharm Res 21:742–748
HE M z S, Jedlitschky G, Gratz M, Haenisch S, Linnemann K, Fusch C et al (2005) Variable expression of MRP2 (ABCC2) in human placenta: influence of gestational age and cellular differentiation. Drug Metab Dispos 33:896–904
Grisk O, Steinbach AC, Ciecholewski S, Schlüter T, Klöting I, Schmidt H et al (2009) Multidrug resistance-related protein 2 genotype of the donor affects kidney graft function. Pharmacogenet Genomics 19:276–288. doi:10.1097/FPC.0b013e328328d4e9
Kobayashi M, Saitoh H, Kobayashi M, Tadano K, Takahashi Y, Hirano T (2004) Cyclosporin A, but not tacrolimus, inhibits the biliary excretion of mycophenolic acid glucuronide possibly mediated by multidrug resistance-associated protein 2 in rats. J Pharmacol Exp Ther 309:1029–1035
Trkulja V, Lalić Z, Nađ-Škegro S, Lebo A, Granić P, Lovrić M et al (2014) Effect of cyclosporine on steady-state pharmacokinetics of MPA in renal transplant recipients is not affected by the MPA formulation: analysis based on therapeutic drug monitoring data. Ther Drug Monit 36:456–464. doi:10.1097/FTD.0000000000000052
Endrenyi L, Fritsch S, Yan W (1991) Cmax/AUC is a clearer measure than Cmax for absorption rates in investigations of bioequivalence. Int J Clin Pharmacol Ther Toxicol 29:394–399
Brunet M, Shipkova M, van Gelder T, Wieland E, Sommerer C, Budde K et al (2016) Barcelona consensus on biomarker-based immunosuppressive drugs management in solid organ transplantation. Ther Drug Monit 38(Suppl 1):S1–S20. doi:10.1097/FTD.0000000000000287
Picard N, Yee SW, Woillard JB, Lebranchu Y, Le Meur Y, Giacomini KM et al (2010) The role of organic anion-transporting polypeptides and their common genetic variants in mycophenolic acid pharmacokinetics. Clin Pharmacol Ther 87:100–108. doi:10.1038/clpt.2009.205
Haufroid V, Mourad M, Van Kerckhove V, Wawrzyniak J, De Meyer M, Eddour DC et al (2004) The effect of CYP3A5 and MDR1(ABCB1) polymorphisms on cyclosporine and tacrolimus dose requirements and trough blood levels in stable renal transplant patients. Pharmacogenetics 14:147–154
Picard N, Bergan S, Marquet P, van Gelder T, Wallemacq P, Hesselink DA et al (2016) Pharmacogenetic biomarkers predictive of the pharmacokinetics and pharmacodynamics of immunosuppressive drugs. Ther Drug Monit 38(Suppl1):S57–S69. doi:10.1097/FTD.0000000000000255
Authors’ contributions
BN, LZ, VT and KŽ were responsible for the study concept and design. LZ, NŠS, and KŽ were responsible for acquisition of subjects. BT and LZ performed research. BBA and NŠS analyzed and interpreted the data. TV and BN analyzed and interpreted the data and prepared the manuscript. All authors participated in critical revision of the manuscript, contributed comments, and approved the final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This prospective observational study was approved by the institutional Ethics Committee and was conducted in line with the Declaration of Helsinki (2008 version). Laboratory analyses were performed in line with the lSO-15189 standard of good practice.
Electronic supplementary material
ESM 1
(PDF 400 kb)
Rights and permissions
About this article
Cite this article
Božina, N., Lalić, Z., Nađ-Škegro, S. et al. Steady-state pharmacokinetics of mycophenolic acid in renal transplant patients: exploratory analysis of the effects of cyclosporine, recipients’ and donors’ ABCC2 gene variants, and their interactions. Eur J Clin Pharmacol 73, 1129–1140 (2017). https://doi.org/10.1007/s00228-017-2285-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2285-4