Abstract
Purpose
Hypergastrinaemia induced by proton pump inhibitor (PPI) therapy may cause ECL-cell and parietal-cell hyperplasia and rebound hyperacidity and dyspepsia after PPI withdrawal. The aim of the study was to assess the effect of different dosage-regimens of netazepide, a gastrin/CCK2 receptor antagonist, on PPI-induced hypergastrinaemia and elevated chromogranin A (CgA).
Methods
Six groups of eight healthy subjects participated in a randomised, double-blind study of esomeprazole 40 mg daily for 28 days, in combination with netazepide 1, 5 or 25 mg or placebo, daily, during the last 14 days of esomeprazole or during 14 days after treatment withdrawal. Fasting serum gastrin and plasma CgA were measured during treatment and after withdrawal, as biomarkers of acid suppression and ECL-cell activity, respectively. Dyspepsia was monitored throughout the study.
Results
Esomeprazole increased gastrin and CgA. Netazepide increased gastrin, but not CgA, and inhibited dose dependently the CgA response to esomeprazole. Gastrin and CgA returned to baseline within 2–3 days of esomeprazole withdrawal; netazepide did not shorten that time. There was no rebound dyspepsia after esomeprazole withdrawal.
Conclusions
Esomeprazole and netazepide each increase gastrin, consistent with a secondary effect of gastric acid suppression, but by different mechanisms. Esomeprazole-induced hypergastrinaemia stimulates ECL cells and thereby increases CgA. Netazepide-induced hypergastrinaemia does not increase CgA, because netazepide blocks gastrin/CCK2 receptors on ECL cells. Co-administration of netazepide 5 mg abolishes the effect of esomeprazole-induced hypergastrinaemia on ECL cells. The quick return to baseline of gastrin and CgA and absence of dyspepsia after esomeprazole withdrawal do not support the concept of rebound hyperacidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastrin controls gastric acid secretion and has a trophic effect on cells in the gastric mucosa, especially enterochromaffin-like (ECL) cells, which possess gastrin (CCK2) receptors [1–3]. Stimulation of CCK2 receptors by gastrin causes release of histamine, which in turn stimulates histamine H2 receptors on parietal cells and secretion of acid via H+/K+-ATPase (proton pump) into the stomach lumen. CCK2 receptors are expressed on parietal cells [4] but are not thought to be involved in acid secretion [5]. Reduced acid production by disease or an acid suppressant, such as a proton pump inhibitor (PPI), causes secondary hypergastrinaemia [6].
In rats, omeprazole reduced acid secretion and induced hypergastrinaemia, but 1 week after omeprazole withdrawal, acid production had increased above baseline [7]. The effect lasted ≥70 days [8]. YM022, a gastrin/CCK2 receptor antagonist, prevented the rebound hyperacidity response to omeprazole withdrawal in rats, whereas in control animals rebound hyperacidity lasted for ≥56 days [9].
Withdrawal of omeprazole 40 mg daily after 12 and 8 weeks in patients with gastro-esophageal reflux disease (GORD) and healthy subjects, respectively, also resulted in increased basal and pentagastrin-stimulated acid output 2 weeks afterwards [10, 11]. However, a literature review concluded that clinical evidence for PPI withdrawal causing rebound hyperacidity was weak, mainly because the studies were done in few subjects and were not well controlled [12]. In two subsequent studies in healthy subjects, both of which were placebo controlled and involved many more subjects, PPI withdrawal was followed by dyspepsia. In one study, 60 subjects received esomeprazole 40 mg daily for 8 weeks followed by placebo daily for 4 weeks, and 60 subjects received placebo daily for 12 weeks. During the last 3 weeks of placebo treatment, there was a significant difference between esomeprazole and placebo (44 vs 15 %) with respect to symptoms of heartburn, acid reflux or dyspepsia after treatment withdrawal [13]. In the other study [14], of 48 subjects who took pantoprazole 40 mg or placebo daily for 4 weeks, significantly more developed dyspepsia after pantoprazole withdrawal than after placebo (44 vs 9 %).
The main indications for treatment with a proton pump inhibitor are peptic ulcer disease or GORD [15]. After Helicobacter pylori eradication was introduced, the need for maintenance therapy for peptic ulcer disease was largely eliminated, and GORD became the main indication for prolonged gastric acid inhibition. PPIs are also used empirically for treatment of non-ulcer dyspepsia. The prevalence of long-term PPI treatment is rising, and there is increasing concern that PPIs are overprescribed [16]. The above studies in healthy subjects and patients suggest that attempts to withdraw PPI treatment in patients who originally responded might fail because of rebound dyspepsia. In other words, PPI withdrawal might cause the very symptoms for which the PPI was first prescribed [17].
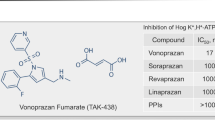
Non-clinical studies have shown that netazepide (YF476) is a potent, highly selective, competitive and orally active gastrin/CCK2 receptor antagonist [18]. We have characterised the clinical pharmacology of netazepide in healthy subjects. Single oral doses caused dose-dependent inhibition of pentagastrin-stimulated gastric acid secretion, which persisted after repeated doses [19]. Rabeprazole alone and netazepide alone for 6 weeks were similarly effective in reducing acid and increasing serum gastrin. A combination of rabeprazole and netazepide increased serum gastrin and reduced basal acid secretion more than did either treatment alone, suggesting more effective acid suppression. Rabeprazole alone increased plasma CgA—a sign of ECL-cell hyperactivity—whereas netazepide alone reduced plasma CgA—a sign of ECL-cell hypoactivity. When combined with rabeprazole, netazepide prevented the increase in CgA resulting from rabeprazole-induced hypergastrinaemia, which is consistent with blockade of gastrin/CCK2 receptors on ECL cells [20]. Circulating gastrin is a biomarker for gastric acid secretion [21, 22], and CgA is a biomarker for ECL-cell activity [23–25]. However, stopping rabeprazole after 6 weeks led neither to rebound hyperacidity nor dyspepsia. Two limitations of the study were that the number of subjects (10 per treatment group) was small, and we measured neither serum gastrin nor plasma CgA during the withdrawal period. We concluded that PPI withdrawal should be studied in an adequately powered trial in patients on long-term PPI treatment. If PPI withdrawal really can lead to rebound hyperacidity, a gastrin/CCK2 receptor antagonist, such as netazepide, should prevent it. But, first a study was required to establish a suitable dose regimen of netazepide, and the time course of the response to PPI withdrawal. Hence, the study we report here.
Objectives
The primary aims were to assess the effect of different dose regimens of netazepide on esomeprazole-induced increases in circulating gastrin and CgA in healthy subjects and to choose a dose regimen for future studies of PPI withdrawal in patients.
The secondary aims were to assess if esomeprazole withdrawal leads to dyspepsia, and if so, whether netazepide can prevent it, and to assess the likelihood of an interaction between esomeprazole and netazepide.
Methods
We complied with the ICH Guideline for Good Clinical Practice. The Medicines and Healthcare products Regulatory Agency and Brent Medical Ethics Committee (REC reference 09/H0717/73) approved the study on 2 and 13 November 2009, respectively, and a protocol amendment on 9 June 2010 and 18 May 2010, respectively. Subjects gave written, informed consent. We did the study during November 2009–September 2010 and registered it with EudraCT (2009-016201-42) and ClinicalTrials.gov (NCT02620696).
Materials
The sponsor, Trio Medicines Ltd., London, England, provided capsules of netazepide 1, 5 and 25 mg and matching placebo; esomeprazole (Nexium®; Astra Zeneca) 40 mg tablets; and an antacid (Gastrocote tablets, Actavis Group) for subjects to take after treatment withdrawal, if needed.
Study design
The study was randomised, double blind and parallel group in design, and in two parts. The protocol required 48 healthy adults (6 groups of 8; 3 groups in each part), who were H. pylori negative (13C–urea breath test), non-smoking men or women, with normal serum gastrin and no history of dyspepsia, and were taking no medicines. Pre-menopausal women at risk of pregnancy were excluded. Subjects were deemed healthy by medical history and examination; ECG; tests for drugs of abuse, hepatitis B and C and HIV 1 and 2; and blood and urine safety tests. A statistician generated the random allocation sequence.
Part 1
In part 1, we assessed the impact of the timing of netazepide 25 mg on the response to esomeprazole. Eligible subjects were randomised to one of 3 treatment groups (Fig. 1).
Group 1
-
Esomeprazole 40 mg for 28 days (Days 1–28); and
-
Netazepide placebo for 42 days (Days 1–42)
Group 2
-
Esomeprazole 40 mg for 28 days (Days 1–28);
-
Netazepide 25 mg for 14 days (Days 15–28); and
-
Netazepide placebo for 28 days (Days 1–14 and Days 29–42)
Group 3
-
Esomeprazole 40 mg for 28 days (Days 1–28);
-
Netazepide 25 mg for 14 days (Days 29–42); and
-
Netazepide placebo for 28 days (Days 1–28)
Subjects took their treatment by mouth once daily for 42 days, and attended the clinic at weekly intervals, on Days −1, 7, 14, 21, 28, 35, 42, 49 and 56. They were resident overnight on Day −1 only. At visits when they were taking treatment, we dosed them circa 0900 hours, after an overnight fast. They took all other doses at home, with breakfast. At 0, 2 and 4 h after dosing in the clinic, or at equivalent times when there was no dosing, we drew blood for measurement of serum gastrin and plasma CgA. At 0, 2 and 4 h after dosing on Days 21, 28, 35 and 42 only, we also drew blood for measurement of plasma netazepide.
On Days 1–56, subjects used a diary card to record adverse events and treatment compliance and completed the short form of the validated Nepean questionnaire, which uses 4- or 5-point Likert scales to measure frequency and severity of 15 upper gastrointestinal symptoms, and the bother they cause [26]. On Days 29–56, subjects recorded antacid usage in the diary card.
We assessed safety and tolerability by medical examination, ECG, blood and urine tests and adverse events throughout the study.
Part 2
After reviewing the data from part 1, we amended the protocol to test lower doses of netazepide, 1 and 5 mg, and to change the study design in part 2. Eligible subjects were randomised to one of three treatment groups (Fig. 1).
Group 4
-
Esomeprazole 40 mg for 28 days (Days 1–28); and
-
Netazepide placebo for 28 days (Days 1–28)
Group 5
-
Esomeprazole 40 mg for 28 days (Days 1–28);
-
Netazepide 1 mg for 14 days (Days 15–28); and
-
Netazepide placebo (Days 1–14)
Group 6
-
Esomeprazole 40 mg for 28 days (Days 1–28);
-
Netazepide 5 mg for 14 days (Days 15–28); and
-
Netazepide placebo (Days 1–14).
Subjects took their treatment by mouth once daily for 28 days. They attended the clinic on Days −1, 7, 14, 21 and 28. They were resident overnight on Day −1 only. After completion of dosing, they attended the clinic on Days 29, 30, 31, 32, 33, 34 and 35. At visits when they were taking treatment, we dosed them circa 0900 hours, after an overnight fast. They took all other doses at home, with breakfast. At 0, 2 and 4 h after dosing in the clinic, or at equivalent times when there was no dosing, we drew blood for measurement of serum gastrin and plasma CgA. At 0, 2 and 4 h after dosing on Days 21 and 28 only, we also drew blood for measurement of plasma netazepide. On Days 1–35, subjects recorded adverse events, treatment compliance and dyspepsia symptoms, as in part 1. On Days 29–35, they recorded any antacid usage, as in part 1. We assessed safety and tolerability, as in part 1.
Measurement of gastrin, CgA and netazepide
We separated serum or plasma from blood and stored samples at −20 °C until assay by ELISA (serum gastrin: Immulite 2000, DPC (CV ≤3.1 %); plasma CgA: DAKO (CV ≤10.8 %)) and validated HPLC/MS method (plasma netazepide: lower limit of quantification, 0.5 ng/mL) [27].
Assessment of compliance
We assessed compliance by diary card and capsule counts. Subjects wore a wristwatch with an alarm, and we telephoned them weekly, to remind them to take their treatment.
Statistics
Sample size
The study was exploratory in nature. The sample size was based on feasibility and data from our previous study which showed significant suppression by netazepide of rabeprazole-induced increases in circulating CgA [20]. The sample size was not expected to be big enough to show significant differences between treatment groups for dyspepsia symptoms.
Fasting serum gastrin and plasma CgA
We compared treatments by analysis of covariance, with baseline (Day −1) values as covariates, treatment and visit as fixed effects, time-point as a repeated variable and the interaction term treatment × visit. We transformed data before analysis, as appropriate.
Plasma netazepide
We plotted plasma netazepide concentrations versus time for all subjects who took netazepide in groups 2, 3, 5 and 6 and who completed the study.
Dyspepsia scores and antacid usage
We summarised the number of subjects per group with dyspepsia symptoms during each week and compared groups informally. Likewise, we summarised the number of doses of antacid taken by each subject in each week after esomeprazole withdrawal and compared treatment groups informally.
Results
Demography
Of 53 subjects who entered the study, 5 (3 in part 1; and 2 in part 2) withdrew for reasons unrelated to treatment. As required by the protocol, 48 subjects (groups 1–6; 8 subjects per group) completed the study. Mean (range) age, weight and height of subjects who completed the study in groups 1–3 in part 1 were 33 years (21–74), 67 kg (49–88) and 167 cm (156–179), respectively. Mean (range) age, weight and height of groups 4–6 in part 2 were 31 years (20–69), 68 kg (49–94) and 168 cm (151–184), respectively. Treatment compliance at home was 96 %.
Statistical analyses
Analysis of data from parts 1 and 2 showed a significant (p < 0.05) treatment by visit interaction, indicating that the time profiles of the different treatments were non-parallel, making it impossible to compare the effects of netazepide 1, 5 and 25 mg on the esomeprazole-induced changes in gastrin and CgA. Nor was it possible to explore the effect of esomeprazole withdrawal on gastrin and CgA, or whether that effect was altered by previous dosing with netazepide. Therefore, we did a post hoc analysis.
To compare the effect of co-administration of netazepide 1, 5 and 25 mg on plasma CgA with that of placebo, we analysed the percentage changes on Days 21–28 for groups 1, 2, 4, 5 and 6 relative to the pre-dose time-point on Day 14, before the start of netazepide treatment. A repeated measures analysis was done on percentage change from pre-dose on Day 14 in plasma CgA concentration, with terms fitted for treatment, patient within treatment, study day and time within study day plus interactions with treatment. Interaction terms which were not significant were removed from the model. There were no significant interactions with treatment, i.e. the effect of treatment was approximately the same at each time, so treatment least square means were calculated and the differences from placebo calculated (Table 1). To assess the effect of netazepide 1 and 5 mg on CgA after treatment withdrawal, we used data from part 2 (groups 4, 5 and 6) at 0 h on each of Days 28–35. One-way ANOVA was used to analyse the data, and, as there was a statistically significant treatment difference, two-sample t tests were used to compare pairs of treatments at the 0-h time-points from Day 28 onwards, until there was no longer a statistically significant difference between treatments (Table 2). Also, we plotted mean concentrations of serum gastrin and plasma CgA with respect to day and time of day for each group at each visit. Given the many data points, we assessed the effect of treatments from the plots and did not do a formal analysis. However, we did explore the relationship between gastrin and CgA concentrations in individual subjects during esomeprazole dosing. We used gastrin and CgA concentration data on days when subjects had received esomeprazole alone (Days 1–28 of treatments 1, 3 and 4, and Days 1–14 of treatments 2, 5 and 6) and used linear regression to select an appropriate model. In each model, subject and day were factors, CgA was the dependent variable and serum gastrin was a covariate. The model that best fitted the data (R 2 = 0.9534) had one line per subject per day with individual slopes and intercepts.
Fasting serum gastrin and plasma CgA
The results are illustrated in Figs. 2, 3, 4 and 5, each of which has a caption describing the effect of treatment and interpretation of the results, so only a summary follows.
a Part 1. Mean (n = 8; ±SEM) fasting serum gastrin (pmol/L) before (0 h) and after (2 and 4 h) treatment of groups 1, 2 and 3 on Days −1 to 56. All groups took esomeprazole 40 mg daily on Days 1 to 28. All treatments increase fasting gastrin on Days 1–28, consistent with a secondary response to gastric acid suppression; the response to esomeprazole alone resolves within 7 days of its withdrawal whether or not netazepide 25 mg is co-administered with esomeprazole on Days 15–28. Netazepide 25 mg alone on Days 29–42 (group 3), after withdrawal of esomeprazole, increases fasting gastrin, consistent with a secondary response to acid suppression via antagonism of gastrin/CCK2 receptors on ECL cells. b Part 2. Mean (n = 8; ±SEM) fasting serum gastrin (pmol/L) before (0 h) and after (2 and 4 h) treatment of groups 4, 5 and 6 on Days −1 to 35. All groups took esomeprazole 40 mg daily on Days 1 to 28. Esomeprazole alone on Days 1–28 increases fasting gastrin; the response resolves within 2–3 days of esomeprazole withdrawal, whether or not netazepide 1 or 5 mg is co-administered with esomeprazole on Days 15–28. The disproportionate increase in gastrin in group 6 reflects a large effect of esomeprazole in three of the eight subjects
a Part 1. Mean (n = 8; ±SEM) fasting plasma CgA (U/L) before (0 h) and after (2 and 4 h) treatment of groups 1, 2 and 3 on Days – 1 to 56. All groups took esomeprazole 40 mg daily on Days 1 to 28. Hypergastrinaemia induced by esomeprazole alone increases fasting CgA. In groups 1 and 3, the response resolves within 7 days of esomeprazole withdrawal, whether or not netazepide 25 mg is administered after esomeprazole withdrawal. However, co-administration of netazepide with esomeprazole on Days 15–28 (group 2) abolishes the increase in fasting CgA. Netazepide 25 mg alone on Days 29–42 (group 3) does not increase CgA, despite increasing gastrin during that time (Fig. 2a), because netazepide blocks gastrin/CCK2 receptors on ECL cells. b Part 2. Mean (n = 8; ±SEM) fasting plasma CgA (U/L) before (0 h) and after (2 and 4 h) treatment of groups 4, 5 and 6 on Days −1 to 35. All groups took esomeprazole 40 mg daily on Days 1 to 28. Hypergastrinaemia induced by esomeprazole alone (group 4) increases fasting CgA; the response resolves within 2–3 days of esomeprazole withdrawal. Co-administration of netazepide 1 mg (group 5) and 5 mg (group 6) on Days 15–28 inhibits the CgA response, which is consistent with antagonism of gastrin/CCK2 receptors on ECL cells. The disproportionate increase in CgA in group 6 reflects the marked esomeprazole-induced hypergastrinaemia in three of the eight subjects
a Parts 1 and 2. Mean (n = 8 or 16; ±SEM) fasting serum gastrin (pmol/L) before (0 h) and after (2 and 4 h) treatment of groups 1, 2, 4, 5 and 6 on Day −1 (baseline) and Days 14 to 35. All groups took esomeprazole 40 mg daily on Days 1 to 28. All treatments increase serum gastrin; the response returns to baseline (Day −1) within 7 days of the end of all treatments. The disproportionate increase in gastrin in group 6 reflects the large effect of esomeprazole in three of the eight subjects (as evidenced by mean serum gastrin concentration on Day 7 of esomeprazole treatment; see Fig. 2b). b Parts 1 and 2. Mean (n = 8 or 16; ±SEM) fasting plasma CgA (U/L) before (0 h) and after (2 and 4 h) treatment of groups 1, 2, 4, 5 and 6 on Day −1 (baseline) and Days 14 to 35. All groups took esomeprazole 40 mg daily on Days 1 to 28. Co-administration of netazepide 1, 5 and 25 mg on Days 15–28 inhibits in a dose-dependent manner the increase in CgA by esomeprazole-induced hypergastrinaemia, which is consistent with gastrin/CCK2 receptor antagonism. CgA returns to baseline (Day −1) within 7 days of the end of all treatments. The disproportionate increase in CgA in group 6 reflects the marked esomeprazole-induced hypergastrinaemia in three of the eight subjects (as evidenced by mean CgA concentration on Day 7 and at 0 h on Day 14 of esomeprazole treatment; see Fig. 3b)
Analysis of covariance of fasting gastrin and fasting CgA concentrations within subjects in groups 1–6 during periods of treatment with esomeprazole alone. Using our statistical model, there was no evidence of a linear relationship between gastrin and CgA concentrations within individual subjects (based on 425 observations from 47 subjects)
Effect of esomeprazole alone on gastrin and CgA
Groups 1–3 and 4–6 were evenly matched for gastrin and CgA at baseline (Day −1). Esomeprazole increased gastrin and CgA on Days 7, 14, 21 and 28 in groups 1, 3 and 4 and Days 7 and 14 in groups 2, 5 and 6. Gastrin increased with time at 0, 2 and 4 h after dosing, whereas CgA was similar at each time-point. Gastrin and CgA responses to esomeprazole varied among subjects and groups.
In group 1, gastrin and CgA returned to baseline (Day −1) by Day 35, the first sampling day after withdrawal of esomeprazole.
Effect of netazepide on esomeprazole-induced increases in gastrin and CgA
In groups 5, 6 and 2, co-administration of netazepide 1, 5 and 25 mg, respectively, with esomeprazole on Days 15–28 suppressed the CgA response in a dose-dependent manner. Netazepide 5 and 25 mg both abolished the CgA response to esomeprazole. Netazepide 1 mg suppressed it only partially. Table 1 shows that, on Days 21 and 28, netazepide significantly reduced the high circulating CgA concentrations resulting from esomeprazole. The effect was dose dependent: 5 and 25 mg doses reduced CgA to a similar extent; 1 mg was less effective.
In group 2, after treatment withdrawal, the gastrin responses returned to baseline by Day 35, as they did in group 1 subjects, who received esomeprazole alone.
In groups 4, 5 and 6, daily measurements after treatment withdrawal showed that gastrin and CgA returned to baseline within 2–3 days in all groups, regardless of whether they had received esomeprazole alone or combined with netazepide.
Effect of netazepide alone on gastrin and CgA
In group 3, netazepide 25 mg alone on Days 29–42 increased gastrin, but not in a time-dependent manner, and did not increase CgA. Indeed, CgA returned to baseline by Day 35, the first sampling day after the start of netazepide alone.
Relationship between gastrin and CgA concentrations in individual subjects
There was no evidence of a linear relationship between gastrin and CgA within subjects: the slope term in the model was not significant (p > 0.05).
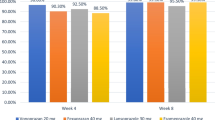
Dyspepsia questionnaire
No subject recorded dyspepsia symptoms in the questionnaire on Day −1, before starting treatment. However, 29 subjects (17 in part 1 and 12 in part 2) reported dyspepsia symptoms in their questionnaires on one or more visits thereafter. The most common symptom was discomfort in stomach, followed by pain/ache in stomach, nausea and bloating. Subjects in part 1 (groups 1–3) reported dyspepsia symptoms 45 times during Days 1–28, when esomeprazole was administered, and 23 times during Days 29–56, the period after withdrawal of esomeprazole. Subjects in part 2 (groups 4–6) reported dyspepsia symptoms 41 times during Days 1–28 and 6 times during Days 29–35. Thus, there were about twice as many reports per week during esomeprazole treatment than after its withdrawal.
Dyspepsia symptoms were reported during all treatments: esomeprazole, netazepide and placebo. There was no obvious relationship to treatment; dyspepsia symptoms were reported after Day 42 in part 1 and after Day 28 in part 2, when all treatments had stopped.
Antacid usage
Three subjects took the antacid for dyspepsia: one subject in group 2 took a total of 11 doses during the weeks before Days 35 and 42 visits, while taking placebo and after he had finished taking esomeprazole and netazepide; one subject in group 3 took one dose on Day 31, after finishing esomeprazole but while taking netazepide, and one subject in group 6 took 18 doses between Days 30 and 34, after she had finished taking esomeprazole and netazepide.
Netazepide concentrations
Mean plasma concentrations of netazepide in groups 2, 3, 5 and 6 at 0, 2 and 4 h after dosing are listed in Table 3. Figure 6a, b shows mean concentrations at 0, 2 and 4 h after dosing with netazepide for 7 and 14 days, respectively. The concentrations at 0 h (pre-dose) were below the limit of quantification. Concentrations at 2 and 4 h after dosing were dose proportional and similar for the common dose of 25 mg.
Mean (±SD) plasma netazepide concentrations (ng/mL) by time-point. a Mean (±SD) plasma netazepide concentrations (ng/mL) on Day 21 (groups 2, 5 and 6) or Day 35 (group 3), 7 days after starting netazepide. b Mean (±SD) plasma netazepide concentrations (ng/mL) on Day 28 (groups 2, 5 and 6) or Day 42 (group 3), 14 days after starting netazepide. Netazepide concentrations at 2 and 4 h after dosing are dose dependent. Co-administration with esomeprazole does not affect netazepide concentrations
Adverse events
Of 53 subjects who entered the study, 42 reported one or more adverse events, such as headache and upper respiratory tract infection, which were all minor and resolved spontaneously. Fewer subjects reported adverse events when taking esomeprazole plus netazepide or netazepide alone than when taking esomeprazole alone.
Discussion
Despite the finding of a significant treatment by visit interaction in parts 1 and 2, and the variability of the fasting gastrin and CgA responses to esomeprazole in our subjects, it was still possible to interpret the results.
Esomeprazole alone increased circulating gastrin and CgA in all subjects in groups 1–6. The increase in gastrin is consistent with inhibition of gastric acid secretion [20–22]. Co-administration of netazepide suppressed the CgA response to esomeprazole in a dose-dependent manner. Those results, which are in accord with the results from our previous study of rabeprazole and netazepide, alone and in combination [20], are consistent with esomeprazole-induced hypergastrinaemia stimulating gastrin/CCK2 receptors on ECL cells and releasing CgA into the circulation, and with netazepide inhibiting gastrin/CCK2 receptors and thereby blocking the CgA response. In 1920, patients from 16 studies of patients on long-term PPI therapy, mean gastrin levels increased by one to three times the upper limit of the normal range (~100 pg/mL) [28].
Others have shown a positive correlation between gastrin and CgA in single blood samples taken from patients during short-, medium- and long-term acid suppression [23, 24]. In our previous study, 24-h serum gastrin increased after a single dose of rabeprazole, whereas 24-h plasma CgA required longer, which supports the concept that gastrin drives the increase in CgA [20]. In this study, we explored the relationship between gastrin and CgA in individual subjects during 2–4 weeks of esomeprazole treatment, using concentration data obtained at 3 time points (0, 2 and 4 h) on several study days. In general, CgA and gastrin were substantially higher in individual subjects during esomeprazole treatment than at baseline; however, there was no direct relationship between their concentrations within individual subjects.
We were surprised that in part 1, both gastrin and CgA had returned to baseline by 7 days, the first sampling point, after esomeprazole withdrawal in groups 1–3, regardless of whether or not netazepide 25 mg had been taken in the period before esomeprazole withdrawal. That finding is contrary to that of Reimer et al. who reported that CgA was still significantly raised 4 weeks after esomeprazole withdrawal in healthy subjects, whereas gastrin was back to normal at that time [13]. However, an earlier study showed that serum gastrin and CgA had decreased significantly at 5 days after withdrawal of 6 months’ PPI therapy in GORD patients [29], which is in accord with our results in healthy subjects.
After reviewing the results from part 1, we amended the protocol for part 2, to measure fasting gastrin and CgA daily after esomeprazole withdrawal and to test the effect of lower doses of netazepide 1 and 5 mg compared with placebo on the gastrin and CgA responses to esomeprazole (Fig. 1). Like netazepide 25 mg daily, netazepide 5 mg daily completely suppressed the CgA response to esomeprazole, whereas the 1-mg regimen had only a modest effect. After esomeprazole withdrawal, both gastrin and CgA returned to baseline within 2–3 days, whether or not esomeprazole had been co-administered with netazepide, confirming the finding in part 1 that both gastrin and CgA returned to baseline within 7 days of esomeprazole withdrawal.
Although no subject reported a history of dyspepsia before entry to the study, 29 of the 48 who completed the study reported dyspepsia symptoms one or more times during treatment. However, there was no increase in incidence of dyspepsia following esomeprazole withdrawal—indeed, dyspepsia symptoms were more frequent during esomeprazole treatment than after its withdrawal. Thus, esomeprazole withdrawal did not lead to dyspepsia. That finding, plus the return to baseline of circulating gastrin and CgA within 2–3 days of esomeprazole withdrawal, excludes the possibility of rebound hyperacidity in this study. We also failed to demonstrate rebound hyperacidity and dyspepsia after withdrawal of rabeprazole treatment for 6 weeks in a previous study in healthy subjects [20]. Retrospective analysis of data from 287 patients with erosive oesophagitis who participated in a trial of dexlansoprazole therapy for 4–8 weeks also revealed no worsening of heartburn symptoms after treatment withdrawal [29].
The results of our study of esomeprazole withdrawal after 4 weeks’ dosing, and our previous study of rabeprazole withdrawal after 6 weeks of dosing [20], are contrary to reports of rebound hyperacidity after withdrawal of 12 weeks of omeprazole therapy in GORD patients [10] and 8 weeks of omeprazole in healthy subjects [11] and dyspepsia after withdrawal of 8 weeks of esomeprazole [13] and 4 weeks of pantoprazole [14] in healthy subjects.
All treatments were safe and well tolerated, and there was no relationship between treatments or the number and type of adverse events. Esomeprazole did not affect plasma netazepide concentrations. A formal study is required to assess whether there is a drug-drug interaction between the two treatments.
The limitations of the study were the small groups of subjects, the short course of esomeprazole and the use of biomarkers rather than measurements of gastric acid secretion and histology of gastric biopsies. However, the results were consistent across the groups and have face validity. The proportion of healthy subjects who developed dyspepsia after PPI withdrawal in the above two studies [13, 14] was the same (44 %), despite the difference in duration of dosing. Therefore, we chose to study the effect of esomeprazole for the shorter period of 4 weeks [14].
Conclusions
-
Esomeprazole and netazepide each increase fasting serum gastrin, which is consistent with a secondary response to suppression of gastric acid secretion via inhibition of the proton pump on parietal cells and inhibition of gastrin/CCK2 receptors on ECL cells, respectively.
-
Esomeprazole-induced hypergastrinaemia leads to hyperactivity of ECL cells and an increase in plasma CgA. Gastrin causes the increase in CgA. Netazepide does not increase CgA and suppresses the increase in CgA induced by esomeprazole, because netazepide blocks gastrin/CCK2 receptors on ECL cells.
-
The return to baseline of circulating gastrin and CgA within 2–3 days of esomeprazole withdrawal, and the absence of dyspepsia symptoms after esomeprazole withdrawal in the control groups, are contrary to the findings of others, and show that a standard 28-day course of esomeprazole, and probably all other PPIs, is unlikely to lead to rebound hyperacidity and dyspepsia symptoms. A study in many patients on long-term PPI therapy, randomised to netazepide 5 mg or placebo, is required to establish whether PPI withdrawal really can lead to rebound hyperacidity, and if so its importance.
References
Dockray GJ, Varro A, Dimaline R, Wang T (2001) The gastrins: their production and biological activities. Ann Rev Physiol 63:119–139
Dimaline R, Varro A (2007) Attack and defence in the gastric epithelium—a delicate balance. Exp Physiol 92:591–601
Dimaline R, Varro A (2014) Novel roles of gastrin. J Physiol 592:2951–2958
Schmitz F, Göke MN, Otte JM, Schrader H, Reimann B, Kruse ML, Siegel EG, Peters J, Herzig KH, Fölsch UR, Schmidt WE (2001) Cellular expression of CCK-A and CCK-B gastrin receptors in human gastric mucosa. Reg Pept 102:101–110
Bakke I, Qvigstad G, Sandvik AK, Waldum HL (2001) The CCK2 receptor is located on the ECL cell, but not on the parietal cell. Scand J Gastroenterol 36:1128–1133
Schubert ML, Peura DA (2008) Control of gastric acid secretion in health and disease. Gastroenterology 134:1842–1860
Carlsson E, Larsson H, Mattsson B, Ryberg B, Sundell G (1986) Pharmacology and toxicology of omeprazole—with special reference to the effects on the gastric mucosa. Scand J Gastroenterol 118:31–38
Larsson H, Carlsson E, Håkanson R, Mattsson H, Nilsson G, Seensalu R, Wallmark B, Sundler F (1988) Time-course of development and reversal of gastric endocrine hyperplasia after inhibition of acid secretion. Studies with omeprazole and ranitidine in intact and antrectomised rats. Scand J Gastroenterol 95:1477–1486
Nishida A, Kobayashi-Uchida A, Akuzawa S, Takinami Y, Shishido T, Kamato T, Ito H, Yamano M, Yuki H, Nagakura Y et al (1995) Gastrin receptor antagonist YM022 prevents hypersecretion after long-term acid suppression. Am J Phys 269:G699–G705
Waldum HL, Arnestad JS, Brenna E, Eide I, Syversen U, Sandvik AK (1996) Marked increase in gastric acid secretory capacity after omeprazole treatment. Gut 39:649–653
Gillen D, Wirz AA, Ardill JE, McColl KE (1999) Rebound acid hyper secretion after omeprazole and its relationship to on-treatment acid suppression and H. pylori status. Gastroenterology 116:239–247
Hunfeld NG, Geus WP, Kuipers EJ (2007) Systematic review: rebound acid hypersecretion after therapy with proton pump inhibitors. Aliment Pharmacol Ther 25:39–46
Reimer C, Søndergaard B, Hilsted L, Bytzer P (2009) Proton-pump inhibitor therapy induces acid-related symptoms in healthy volunteers after withdrawal of therapy. Gastroenterology 137:80–87
Niklasson A, Lindström L, Simrén M, Lindberg G, Björnsson E (2010) Dyspeptic symptom development after discontinuation of a proton pump inhibitor: a double-blind placebo-controlled trial. Am J Gastroenterol 105:1531–1537
National Institute for Clinical Excellence (2014) Dyspepsia and gastro-oesophageal reflux disease: investigation and management of dyspepsia, symptoms suggestive of gastro-oesophageal reflux disease, or both. NICE guideline
Vakil N (2012) Prescribing proton pump inhibitors: is it time to pause and rethink? Drugs 72:437–445
McColl KE, Gillen D (2009) Evidence that proton-pump inhibitor therapy induces the symptoms it is used to treat. Gastroenterology 137:20–22
Takemoto Y, Yuki H, Nishida A, Ito H, Kobayashi-Uchida A, Takinami Y, Akuzawa S, Ohta M, Satoh M, Semple G, Miyata K (1998) Effects of YF476, a potent and selective gastrin/CCK-B receptor antagonist, on gastric acid secretion in beagle dogs with gastric fistula. Arzneim Forsch 48:403–407
Boyce M, Warrington S, Black J (2013) Netazepide, a gastrin/CCK2 receptor antagonist, causes dose-dependent, persistent inhibition of the responses to pentagastrin in healthy subjects. Br J Clin Pharmacol 76:689–698
Boyce M, Dowen S, Turnbull G, van den Berg F, Zhao CM, Chen D, Black J (2015) Effect of netazepide, a gastrin/CCK2 receptor antagonist, on gastric acid secretion and rabeprazole-induced hypergastrinaemia: a double-blind trial in healthy subjects. Br J Clin Pharmacol 79:744–755
Bonapace ES, Fisher RS, Parkman HP (2000) Does fasting serum gastrin predict gastric acid suppression in patients on proton-pump inhibitors? Dig Dis Sci 45:34–39
Ligumsky M, Lysy J, Siguencia G, Friedlander Y (2001) Effect of long-term, continuous versus alternate-day omeprazole therapy on serum gastrin in patients treated for reflux oesophagitis. J Clin Gastroenterol 33:32–35
Sanduleanu S, Stridsberg M, Jonkers D, Hameeteman W, Biemond I, Lundqvist G, Lamers C, Stockbrügger RW (1999) Serum gastrin and chromogranin a during medium- and long-term acid suppressive therapy: a case-control study. Aliment Pharmacol Ther 13:145–153
Sanduleanu S, De Bruïne A, Stridsberg M, Jonkers D, Biemond I, Hameeteman W, Lundqvist G, Stockbrügger RW (2001) Serum chromogranin a as a screening test for gastric ECL cell hyperplasia during acid-suppressive therapy. Eur J Clin Investig 31:802–811
Pregun I, Herszényi L, Juhász M, Miheller P, Hritz I, Patócs A, Rácz K, Tulassay Z (2011) Effect of proton-pump inhibitor therapy on serum chromogranin a level. Digestion 84:22–28
Talley NJ, Verlinden M, Jones M (2001) Quality of life in functional dyspepsia: responsiveness of the Nepean dyspepsia index and development of a new 10-item short form. Aliment Pharmacol Ther 15:207–216
Redrup MJ, Leaf FC, Miyashita A, Watanabe T, Higuchi S, Chasseaud LF, Cheng KN (2002) Validation of a liquid chromatographic-tandem mass spectrometric method for the measurement of (R)-1-[2,3-dihydro-2-oxo-1-pivaloylmethyl-5-(2-pyridyl)-1H-1,4-benzodiazepin-3-yl]-3-(3methylaminophenyl) urea (YF476) in human plasma. J Chromatography 772:317–325
Lundell L, Vieth M, Gibson F, Nagy P, Kahrilas PJ (2015) Systematic review: effects of PPI on serum gastrin levels and gastric histology. Aliment Pharmacol Ther 42:649–663
Metz DC, Pilmer BL, Han C, Perez MC (2011) Withdrawing proton pump inhibitor therapy after healing esophagitis does not worsen symptoms or cause persistent hypergastrinaemia: analysis of dexlansoprazole MR clinical trial data. Am J Gastroenterol 106:1953–1960
Acknowledgements
We thank the volunteers who took part in the study and our many colleagues who helped carry out the study. In particular, we thank Bhavini Ladwa for data management, Torkjel Matzow and Lucy Ball for the study report and Lauren Garden for Figs. 2, 3, 4, 5 and 6.
Authors’ contributions
MB designed and, together with FvdB and SW, carried out the study. TM did the statistical analyses. MB wrote the manuscript. SW and KD contributed to the final version. All authors approved the final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MB owns HMR and Trio. SW, FvdB, KD and TM are HMR employees.
Funding
The study was funded by Trio Medicines, London, England (Trio), a subsidiary of Hammersmith Medicines Research (HMR).
Rights and permissions
About this article
Cite this article
Boyce, M., van den Berg, F., Mitchell, T. et al. Randomised trial of the effect of a gastrin/CCK2 receptor antagonist on esomeprazole-induced hypergastrinaemia: evidence against rebound hyperacidity. Eur J Clin Pharmacol 73, 129–139 (2017). https://doi.org/10.1007/s00228-016-2150-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2150-x