Abstract
Purpose
Effective and efficient medication reporting processes are essential in promoting patient safety. Few qualitative studies have explored reporting of medication errors by health professionals, and none have made reference to behavioural theories. The objective was to describe and understand the behavioural determinants of health professional reporting of medication errors in the United Arab Emirates (UAE).
Methods
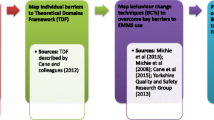
This was a qualitative study comprising face-to-face, semi-structured interviews within three major medical/surgical hospitals of Abu Dhabi, the UAE. Health professionals were sampled purposively in strata of profession and years of experience. The semi-structured interview schedule focused on behavioural determinants around medication error reporting, facilitators, barriers and experiences. The Theoretical Domains Framework (TDF; a framework of theories of behaviour change) was used as a coding framework. Ethical approval was obtained from a UK university and all participating hospital ethics committees.
Results
Data saturation was achieved after interviewing ten nurses, ten pharmacists and nine physicians. Whilst it appeared that patient safety and organisational improvement goals and intentions were behavioural determinants which facilitated reporting, there were key determinants which deterred reporting. These included the beliefs of the consequences of reporting (lack of any feedback following reporting and impacting professional reputation, relationships and career progression), emotions (fear and worry) and issues related to the environmental context (time taken to report).
Conclusion
These key behavioural determinants which negatively impact error reporting can facilitate the development of an intervention, centring on organisational safety and reporting culture, to enhance reporting effectiveness and efficiency.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Effective and efficient medication reporting systems and processes are essential in promoting patient safety. A key goal of the US National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP) is stimulating the ‘development and use of reporting and evaluation systems by individual health care organisations’ [1]. These systems should promote staff engagement; quality, timely and consistent reporting; and feedback to impact organisations and practitioners.
Whilst several systematic reviews have reported medication error prevalence and causality, these did not focus specifically on medication error reporting [2–5]. A number of studies have employed quantitative approaches (mainly cross-sectional surveys) to research the perspectives of health professionals around medication error reporting [6–14]. Key findings are that many factors appear to influence sub-optimal reporting including lack of awareness of reporting policies, lack of visibility of the reporting processes, disagreement on what constitutes an error worthy of reporting, the effort required to report, lack of any senior role models and poor communication following reporting.
Fewer qualitative studies (employing methods of semi-structured interviews and focus groups) have been reported, with barriers to reporting errors comprising time constraints and burden of reporting, selective reporting depending on error severity, anxieties of reporting, lack of feedback following reporting and cultural norms [15–17]. One key limitation of the studies published to date is the absence of application of behavioural theories to processes of research data collection and generation, analysis or interpretation.
The UK Medical Research Council (MRC) guidance on ‘developing and implementing complex interventions’ highlights the role of cognitive, behavioural and organisational theories [18]. Theory is a key aspect of the development phase, ‘…you also need to be aware of the relevant theory, as this is more likely to result in an effective intervention than is a purely empirical or pragmatic approach’. A recent systematic review highlighted the lack of and poor use of theory in implementation research [19]. Prior to developing an intervention to enhance and optimise the medication error reporting systems and processes, it is important to define and characterise behavioural determinants associated with the behaviour in question (i.e. medication error reporting).
The Theoretical Domains Framework was developed through expert panel consensus and validation by a group of psychological theorists, health service researchers and health psychologists to overcome the challenge of selecting the most appropriate behavioural change theory from the vast number available [20, 21]. The framework was derived from 33 psychological theories and 128 theoretical constructs which are organised into 14 overarching domains, as described in Table 1. TDF can be used in research to understand and characterise the domains of behaviour which need to be targeted in any intervention. TDF has been used extensively within health care-related research; areas of study have included smoking cessation, physical activity, hand hygiene, acute low back pain and schizophrenia [21].
The aim of this study was to describe and understand the behavioural determinants of health professional reporting of medication errors in the United Arab Emirates (UAE). Describing and understanding their perspectives on error reporting would provide an opportunity to generate novel data which could be used to develop an intervention to impact the effectiveness and efficiency of the medication error reporting systems and processes.
Methods
Research design
A qualitative design of face-to-face, semi-structured interviews was employed, with the phenomenon in question being health professional reporting of medication errors.
Setting
The research was conducted in the three major medical/surgical hospitals (412, 451 and 461 beds) of Abu Dhabi, the UAE. All hospitals within the Health Authority of Abu Dhabi have adopted the NCCMERP definition of medication error, ‘any preventable event that may cause or lead to inappropriate medication use or patient harm, whilst the medication is in the control of the health care professional, patient or consumer. Such events may be related to professional practice, health care products, procedures and systems including prescribing; order communication; product labelling, packaging and nomenclature; compounding; dispensing; distribution; administration; education; monitoring; and use’ [1]. All health professionals are mandated to report all medication errors, including those which ‘been detected and corrected through intervention by another health care professional or patient, before actual medication administration’ [22].
Recruitment and sampling
As part of a related study, nurses, pharmacists and physicians in the participating hospitals were sent an e-mail by the human resources department, containing full study information and an invitation from the research team to participate. Those interested completed an online sampling survey providing demographic information. Purposive sampling was employed, with strata of profession and years of experience. Those selected for interview were contacted individually via telephone to organise the date, time and location of the interview, with informed consent obtained prior to commencement of the interview.
Sample size
Sampling and data generation were continued to the point of data saturation. The approach to determining the point of saturation recommended by Francis et al. [23] was employed with an initial analysis sample of five from each profession, and interviews progressing until no new themes were identified from three further consecutive interviews.
Data generation
A semi-structured interview schedule was developed with questions focusing on medication error reporting, facilitators, barriers, experiences and suggestions for improving effectiveness and efficiency. The schedule was reviewed for credibility by four individuals in the UK with expertise in patient safety and qualitative research. Three pilot interviews were conducted (one nurse, pharmacist and physician) prior to finalising the interview schedule. Interviews were conducted in English by MA (as part of her doctoral studies) who had extensive work experience in hospital settings in the UAE and training in qualitative interviewing. The interviews took place between July and September 2014, with each lasting around 45 min. The interviews were audio-recorded and transcribed in full, using a naturalistic approach in which every utterance is transcribed in as much detail as possible. All interviewees were afforded the opportunity to review their transcripts prior to analysis. DS reviewed the first five audio-recordings to ensure high-quality interviewing skills and thus promote data credibility and checked the reliability of transcribing of each interview. Furthermore, a very clear audit trail was maintained with documented details of data gathering to promote dependability.
Data analysis
Data analysis followed the framework approach of familiarisation, identifying a thematic framework, indexing, charting and mapping and interpretation [24]. The Theoretical Domains Framework (TDF) was used as a thematic coding framework.
Two researchers (MA and DS) coded each interview independently, with consensus reached by discussion at a meeting of the research team. NVivo 10 (QSR International) was used to support data management.
Governance
The study was approved by the ethical review panel of a university in the UK and the ethics committee of each participating hospital in the UAE.
Results
Forty-three health professionals agreed to be interviewed, with data saturation being achieved after interviewing ten nurses, ten pharmacists and nine physicians. The demographics of the 29 interviewees are given in Table 2.
Emerging themes were mapped to the TDF domains as follows, with each interviewee being allocated an individual code. Table 3 provides a summary of the themes mapped to the TDF domains. The following TDF domains were not represented in the thematic analysis: skills; beliefs about capabilities; optimism; memory, attention and decision processes; and behavioural regulation.
Goals
-
i)
Patient safety
All commented on the improvement in patient safety which could be achieved through reporting medication errors,
“Yeah, the good point of having [a] reporting system is that it lessens the number of errors and improves the quality of patient care”. [physician S2]
-
ii)
Developing and improving health care systems and practises
Most described additional aims around highlighting issues or flaws in either professional practise, systems or processes. Once these had been identified, corrective action could be implemented,
“You want to see where are the gaps that are hidden maybe and then try to improve our processes, our system, our policies, through investigating and checking what was the reason behind these incidents. So the main purpose is to improve, of course”. [pharmacist A5]
Knowledge
-
i)
General lack of knowledge of medication error reporting policy and systems
Interviewees were generally unaware of the medication error reporting policies and systems in their hospitals. Whilst this lack of awareness was widespread, it appeared to be more marked in relation to physicians,
“No, to be honest I did not, have not seen policy in this hospital clarifying what to report. I have not seen any reporting form or tools yet”. [physician S2]
Indeed, several were adamant that there was no system or policy,
“I have an error. I need to report it. Can you give me guidelines on doing it?” [nurse K2]
-
ii)
Need for education and training to improve knowledge
Interviewees across all of the health professions, and at all levels of seniority, highlighted the need for enhanced education and training as one step in improving medication error reporting,
“I believe there is lack of communication and awareness in the implementation policy of medication management and use, especially the part related to the reporting error process. There is definitely [a] problem with education to implement such a practice [error reporting]”. [pharmacist S2]
Several, however, had contrasting views and experiences of the education and training providing around reporting policy, systems and practise,
“It is part of the staff orientation programme, the quality and patient’s safety and I think, everyone, when they are recruited are trained how to use the PSN [Provider Service Network, established and organised by health care provider] and how to report”. [physician S2]
Social professional and role identity
-
i)
Professional obligation
Whilst many considered it their professional obligation to report errors, a pharmacist commented that physicians never reported errors,
“Usually, the reporting comes from nurses and pharmacists. I never saw a physician reporting anything”. [pharmacist H2]
Intentions
-
i)
Selectivity of errors reported
Several explained that they were more likely to report certain types of errors or those committed by certain individuals.
“I think they will report any serious incidents, but they don’t really see that near misses are more important or errors that about to be happen are more important”. [pharmacist A2]
Others described their intentions to report only those errors where blame could not be attributed to an individual,
“Nurses can report an incident where there is nobody to blame. But if there is a clear error from a specific person, they don’t report these things”. [pharmacist L5]
Belief of consequences
Many themes emerged within the domain of beliefs of consequences.
-
i)
Lack of feedback following reporting
One key recurring theme was the absence of feedback following submitting a report, which was major barrier to reporting further errors. This perception of lack of feedback was apparent across the different health professions,
“I have found that my expectation has not been made. It has not been made in that I have written a report, it has gone to Quality [department] and I have not heard anything about it”. [nurse P2]
“I reported two or three times, there was no action taken. I won’t report anymore. It is a non-efficient system”. [pharmacist C1]
-
ii)
Impacting professional reputation
Many were concerned over the impact on their professional reputation, a concern which was heightened by the lack of anonymity in the reporting process,
“They will not think actually what happened, how they can improve. Instead of that, in a meeting, in the ward meeting, they are telling it to all, you feel shame sometimes. They may publish it like that”. [physician Y2]
-
iii)
Impacting professional relationships
As well as impacting their professional reputation, another recurring theme was how reporting errors could impact professional working relationships. Many described their reluctance to report errors committed by their colleagues and friends. These concerns existed at both interprofessional and intraprofessional levels,
“If it is like a physician, it could at least get negative comments, maybe harsh interaction, and maybe uncooperative interaction in the future, maybe just waiting for them to make a mistake in order to really get back to them”. [pharmacist A5]
“But it is there, abrasive, repercussion in that ‘why did you report, you know? You did not have to report me. You could have come in and just told me, you know. You don’t have to put on a piece of paper. Now it is going to another department’. So I think that is, it is abrasive”. [nurse J2]
-
iv)
Impacting career progression
Many discussed concerns over the how reporting could impact their career and indeed, in some instances, their job security,
“…I have heard other people talking, I reported this and now I am battling, you know. I have been transferred…” [nurse K2]
“Only they [management] will concentrate about this first one incident only and he will lose the job. That is why, maybe, they are not reporting”. [physician F1]
Emotion
-
i)
Fear and worry
The behavioural determinant domain of ‘emotions’ emerged as a key theme in relation to reporting errors and was described by physicians, nurses and pharmacists as generating fear and worry,
”…because, I was shocked and I was afraid, and I was afraid that she will inform the unit manager and everybody”. [pharmacist B1]
“That goes back to trust. Fear of losing job. Fear of ‘no performance’”. [physician M5]
Environmental context and resources
Several themes emerged relating to the environment in which they were practising and the resources available to them.
-
i)
Time commitment
Many described a lack of time to report medication errors and many other competing priorities,
“But sometimes I have reasons to not report, just like one afternoon I am alone, I will do the IVs. I have incidents to report, but no time…so that is time limit and I am alone”. [nurse M2]
Some linked the time taken to report to the paper based system and issues around access to reporting forms,
“….reporting error takes a lot of time and consumption. There are no forms that are readily available for everybody”. [physician Y2]
Some, however, expressed contrary views in relation to the time commitment,
“It is not time consuming. If we are used to it is not consuming. If we are doing first time or like that, you will feel, you know, it is time consuming. For me, it is ok”. [pharmacist N8]
One nurse explained that whilst the reporting form was simple, there was some ambiguity in terms of the actual detail to be recorded and the categorisation of the events,
“Here in the hospital, the documentation is very simple, it is very basic; the questions are asked and the document is filled in. But it also...it is very vague, there are no directions or categorisation for the events”. [nurse P2]
-
ii)
Electronic system
Several commented on the lack of electronic reporting systems in their hospitals and that the paper based system was a major deterrent to reporting,
“Again, the lack of the electronic system is one of our big challenges that we haven’t in our hospital. So in order for us to do a reporting, we have to go through many steps of getting the paperwork, manually reporting and waiting for the results”. [pharmacist C1]
Social influences
Many described the influences of others on their likelihood of reporting errors.
-
i)
Professional hierarchy
The perceived professional hierarchy and power of physicians was a major issue, as described by nurses and pharmacists,
“Especially, when you report physicians in the higher hierarchy and they know who reported. Then they come back to you ‘why did you report that? You did not have to. You should have talked to me. This is small thing. You should be…’ Then you are in a poor situation what the correct action of plan is actually...” [pharmacist A5]
Reinforcement
Several of the more senior interviewees described various incentives which had been implemented to increase the likelihood of reporting medication errors.
-
i)
Incentives to report medication errors
One senior physician described a scheme to reward the member of staff reporting the highest number of medication errors,
“…we are rewarding the highest reporter, so that we say that ‘he is the reporter of the month, not only on numbers, but he has identified an incident that could have caused this and this’, so we try to somehow encourage them”. [physician T5]
Discussion
Main findings
This research has elucidated the key behavioural determinants around medication error reporting in a sample of health professionals in the UAE. Whilst it appeared that patient safety and organisational improvement goals and intentions were determinants which facilitated reporting, there were key determinants which deterred reporting. These included the beliefs of the consequences of reporting, emotions, social influences and issues related to the environmental context.
Strengths and weaknesses
The use of the TDF and the steps taken to promote research trustworthiness, particularly the elements of credibility and dependability [25] (e.g. member checking, the documented operational detail of data gathering and ensuring a skilled interviewer), and hence rigour are key strengths of the research. However, there are several limitations, and as such, the findings should be interpreted with caution. The research was conducted within three major hospitals of the UAE, and the findings may not necessarily be transferable to other settings in the UAE and beyond. Nevertheless, it is likely that the findings will resonate widely, given the acknowledged and demonstrated scale of under-reporting [6–14]. Although there were attempts to promote the credibility (i.e. that the findings were congruent with reality), it is possible that some interviewees may not have described truly their perspectives and experiences. Despite employing purposive sampling, a wider range of participants, for example covering different medical and surgical specialties, may have impacted the findings. It is also possible that those agreeing to participate were not representative of all health professionals.
Interpretation of findings
This research extends the knowledge base, particularly the findings from qualitative research exploring barriers to medication error reporting. Whilst some of the findings, such as selective reporting depending on perceived error severity, anxieties of reporting and lack of feedback, are similar to other qualitative studies [15–17], this research has provided rich detail around specific TDF behavioural determinants which impacted reporting. Three of the key determinants which acted as barriers to reporting were the health professionals’ beliefs of the consequences of reporting, emotional issues and social influences. Overall, there were few key differences identified between the professional groupings, other than perceived hierarchies.
Many interviewees of all professions and years of experience reported their fears and worries of reporting. These in turn were linked to their beliefs of the consequences of reporting impacting their professional standing, interprofessional and intraprofessional relationships and working, and their career progression. There appeared to be a hierarchical, social influence based upon the perceived power of certain physicians by nurses and pharmacists which deterred reporting of physician errors by these other professions. These issues are all complex and related to the culture within which the health professionals are working. Indeed, the entire field of safety culture is complex with an acknowledged lack of consistency in terms such as ‘culture’ and ‘climate’ and no standardised definitions. A recent literature review identified the most common definition of safety culture as, ‘the product of individual and group values, attitudes, competencies and patterns of behaviour that determine the commitment to, and the style and proficiency of, an organisation’s health and safety programmes. Organisations with a positive safety culture are characterised by communications founded on mutual trust, by shared perceptions of the importance of safety and by confidence in the efficacy of preventive measure’ [26]. Mutual trust and confidence are key within this definition, and the findings of this study demonstrate that much work is required to promote a safety culture in relation to medication error reporting. Two systematic literature reviews have explored interventions to promote safety culture in hospitals and acute hospitals specifically [27, 28]. Both reviews noted that studies were generally of poor quality but that interventions may improve perceptions of safety culture. However, none of the studies within these reviews had focus on perceptions of culture around medication error reporting.
Barriers such as knowledge gaps around the reporting policies, specifically what to report, and issues relating to the environmental context and resources (time commitment and burden) have been described in quantitative [6–14] and qualitative studies [15–17]. Similarly, selective reporting of errors perceived by the health professional to be more serious has been highlighted previously. Whilst this may be understandable to some extent, it is not congruent with the reporting policy in place in the Health Authority of Abu Dhabi, which requires all errors and near misses to be reported [22]. Reporting and learning from near misses may be particularly valuable in providing feedback at practitioner and organisation levels to develop safer systems of practise. However, one further key theme which emerged in this study was the lack of feedback following reporting which deterred further reports being submitted.
One of the many benefits of using TDF to identify key behavioural domains is that these can then be used as intervention targets, as suggested by the MRC [18]. The Behaviour Change Wheel highlights which domains promote optimal strategies and designing of interventions mapped to behavioural determinants [29]. Interventions are described as seven categories of education; persuasion; incentivisation; coercion; training; restriction; and environmental restructuring, modelling and enablement. Determinants of knowledge, intentions (selectivity of reporting) and environmental context (time taken to report) may be enhanced via effective modes of education, training and persuasion and determinants of beliefs of consequences relating to the lack of feedback by modelling the process. Determinants of beliefs of the consequences of reporting (impacting reputation, relationships and career progression) and emotional issues (worry) are much more likely to be entrenched and difficult to undo. This may require specific modes of intervention possibly at all levels of an organisation from policy makers to practitioners. These interventions may be more likely to be implemented successfully and sustained by considering Normalisation Process Theory (NPT), which explains ‘…the social processes through which new or modified practices of thinking, enacting and organising work are operationalised in health care and other institutionalised settings’ [29]. NPT is concerned with the following three core problems: implementation—the social organisation of bringing practises into action, embedding—the process through which practises become incorporated routinely into everyday work and integration—the process by which practises are reproduced and sustained [30, 31]. The theory proposes that
-
1.
practises become embedded routinely in social contexts as the result of people working, individually and collectively, to implement them;
-
2.
the work of implementation is operationalised through four generative constructs of coherence, cognitive participation, collective action and reflexive monitoring; and
-
3.
the production and reproduction of a practise requires continuous investment.
Further research
Applying NPT to developing, implementing and sustaining interventions to alter behaviours in medication error reporting will require involvement and enablement at all levels of the organisation. Further research should therefore focus on these aspects, using robust and rigorous mixed method research methodologies, covering all stakeholder perspectives.
Conclusion
This qualitative study has identified key behavioural determinants of the beliefs of the consequences of reporting, emotions and issues related to the environmental context, which all negatively impact medication error reporting. These determinants can be mapped to behaviour change strategies facilitating the development of an intervention, centring on organisational safety and reporting culture, to enhance medication error reporting effectiveness and efficiency with implications for health care practise and patient safety.
References
National Coordinating Council for Medication Error Reporting and Prevention. 2016 Available at http://www.nccmerp.org [accessed January 2016].
Keers RN, Williams SD, Cooke J, Ashcroft DM (2013) Prevalence and nature of medication administration errors in health care settings: a systematic review of direct observational evidence. Ann Pharmacother 47(2):237–256
Keers RN, Williams SD, Cooke J, Ashcroft DM (2013) Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf 36(11):1045–1067
Lewis PJ, Dornan T, Taylor D, Tully MP, Wass V, Ashcroft DM (2009) Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review. Drug Saf 32(5):379–389
Ross S, Bond C, Rothnie H, Thomas S, Macleod MJ (2009) What is the scale of prescribing errors committed by junior doctors? A systematic review. Brit J Clin Pharm 67(6):629–640
Wakefield DS, Wakefield BJ, Uden-Holman BMA (1996) Perceived barriers in reporting medication administration errors. Best Pract and Benchmarking Healthc 1:191–197
Uribe CL, Schweikhart SB, Pathak DS, Marsh GB, Fraley RR (2002) Perceived barriers to medical error reporting: an exploratory investigation. J Healthc Manag 47:263–279
McArdle D, Burns N, Ireland A (2003) Attitudes and beliefs of doctors towards medication error reporting. Int J Health Care Qual Assur 16:326–333
Stratton KM, Nlegen MA, Peppper G, Vaughn T (2004) Reporting of medication errors by pediatric nurses. J Pediatr Nurs 19:385–392
Evans SM, Berry JG, Smith BJ, Esterman A, Selim P, O’Shaughnessy J, et al. (2006) Attitudes and barriers to incident reporting: a collaborative hospital study. Qual Saf Health Care 15:39–43
Sanghera IS, Franklin BD, Dhillon S (2007) The attitudes and beliefs of healthcare professionals on the causes and reporting of medication errors in a UK intensive care unit. Anaesthesia 62:53–61
Armitage G, Newell R, Wright J (2010) Improving the quality of drug error reporting. J Eval Clin Pract 16:1189–1197
Sarvadikar A, Prescott G, Williams D (2010) Attitudes to reporting medication error among differing healthcare professionals. Eur J Clin Pharmacol 66:843–853
Castel ES, Ginsburg LR, Zaheer S (2015) Understanding nurses’ and physicians’ fear of repercussions for reporting errors: clinician characteristics, organization demographics, or leadership factors? BMC Health Serv Res 15:326
Kingston MJ, Evans SM, Smith BJ, Berry J (2004) Attitudes of doctors and nurses towards incident reporting: a qualitative analysis. Med J Aus 181:36–39
Hartnell N, MacKinnon N, Sketeris I, Fleming M (2012) Identifying, understanding and overcoming barriers to medication error reporting in hospitals: a focus group study. BMJ Qual Saf 21:361–368
Williams SD, Phipps DL, Ashcroft DM (2013) Understanding the attitudes of hospital pharmacists to reporting medication incidents: a qualitative study. Res Soc Adm Pharm 9:80–89
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M (2008) Developing and evaluating complex interventions: the new Medical Research Council guidance. Brit Med J 337:a1665
Davies P, Walker AE, Grimshaw JM (2010) A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluation. Implement Sci 5:14
Cane J, O’Connor D, Michie S (2012) Validation of the Theoretical Domains Framework for use in behaviour change and implementation research. Implement Sci 7:37
Francis JJ, O’Connor D, Curran J (2012) Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the Theoretical Domains Framework. Implement Sci 7:35
Health Authority Abu Dhabi Medication Error Reporting Policy version 1, 2009. Available at http://www.haad.ae/haad/tabid/58/Mid/417/ItemID/225/ctl/Details/Default.aspx [Accessed January 2016]
Francis JJ, Johnston M, Robertson C, Glidewell L, Entwistle V, Eccles MP, et al. (2010) What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health 25(10):1229–1245
Ritchie J, Spencer L (2002) Qualitative data analysis for applied policy research. Qual Res Companion 305-329
Shenton AK (2004) Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf 22:63–67
Halligan M, Zecevic A (2011) Safety culture in healthcare: a review of concepts, dimensions, measures and progress. BMJ Qual Saf 20(4):338–343
Morello RT, Lowthian JA, Barker AL, McGinnes R, Dunt D, Brand C (2013) Strategies for improving patient safety culture in hospitals: a systematic review. BMJ Qual Saf 22:11–18
Weaver SJ, Lubomksi LH, Wilson RF, Pfoh ER, Martinez KA, Dy SM (2013) Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med 158:369–374
Michie S, van Stralen MM, West R (2011) The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 6:42
May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. (2009) Development of a theory of implementation and integration: normalization process theory. Implement Sci 4:29
May C, Finch T (2009) Implementing, embedding and integrating practices: an outline of normalization process theory. Sociology 43:535–554
Acknowledgments
The authors would like to acknowledge the following for their contribution and support provided throughout this research: Embassy of the United Arab Emirates for funding Mai Alqubaisi; Katie MacLure, Gordon Rushworth, Cristin Ryan, and Anne Watson for reviewing the draught interview schedule; the ethical review panels and Human Resources Departments of all participating hospitals; and all interviewees.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mai Alqubaisi, Antonella Tonna, Alison Strath, and Derek Stewart declare that they have no conflict of interest.
Funding
Funding for Mai Alqubaisi’s doctoral studies was provided by the Embassy of the United Arab Emirates.
Rights and permissions
About this article
Cite this article
Alqubaisi, M., Tonna, A., Strath, A. et al. Exploring behavioural determinants relating to health professional reporting of medication errors: a qualitative study using the Theoretical Domains Framework. Eur J Clin Pharmacol 72, 887–895 (2016). https://doi.org/10.1007/s00228-016-2054-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2054-9