Abstract
Osteocyte produced fibroblast growth factor 23 (FGF23) is the key regulator of serum phosphate (Pi) homeostasis. The interplay between parathyroid hormone (PTH), FGF23 and other proteins that regulate FGF23 production and serum Pi levels is complex and incompletely characterised. Evidence suggests that the protein product of the SOST gene, sclerostin (SCL), also a PTH target and also produced by osteocytes, plays a role in FGF23 expression, however the mechanism for this effect is unclear. Part of the problem of understanding the interplay of these mediators is the complex multi-organ system that achieves Pi homeostasis in vivo. In the current study, we sought to address this using a cell line model of the osteocyte, IDG-SW3, known to express FGF23 at both the mRNA and protein levels. In cultures of differentiated IDG-SW3 cells, both PTH1-34 and recombinant human (rh) SCL remarkably induced Fgf23 mRNA expression dose-dependently within 3 h. Both rhPTH1-34 and rhSCL also strongly induced C-terminal FGF23 protein secretion. Secreted intact FGF23 levels remained unchanged, consistent with constitutive post-translational cleavage of FGF23 in this cell model. Both rhPTH1-34 and rhSCL treatments significantly suppressed mRNA levels of Phex, Dmp1 and Enpp1 mRNA, encoding putative negative regulators of FGF23 levels, and induced Galnt3 mRNA expression, encoding N-acetylgalactosaminyl-transferase 3 (GalNAc-T3), which protects FGF23 from furin-like proprotein convertase-mediated cleavage. The effect of both rhPTH1-34 and rhSCL was antagonised by pre-treatment with the NF-κβ signalling inhibitors, BAY11 and TPCK. RhSCL also stimulated FGF23 mRNA expression in ex vivo cultures of human bone. These findings provide evidence for the direct regulation of FGF23 expression by sclerostin. Locally expressed sclerostin via the induction of FGF23 in osteocytes thus has the potential to contribute to the regulation of Pi homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibroblast growth factor family member 23 (FGF23) is a protein hormone produced by osteoblasts and osteocytes, and is a potent regulator of blood levels of Pi [1, 2]. The expression of both FGF receptor 1 (FGFR1) and αKlotho forms a receptor complex allowing responsiveness to FGF23 in organs remote from its synthesis, most notably the renal proximal tubule epithelium [3,4,5]. Both Pi and the active hormonal form of vitamin D, 1α,25-dihydroxyvitamin D3 (1,25D) have been shown to stimulate the synthesis of FGF23 in vivo and in vitro [6,7,8,9,10,11,12], and FGFR1 expression by osteocytes has been shown to play a pivotal role in sensing the serum Pi level [13]. Furthermore, other gene products are clearly implicated in regulating the synthesis of FGF23, since mutations of these genes leads to its dysregulation. Specifically, mutations in the genes phosphate regulating endopeptidase homolog, X-linked (PHEX), dentin matrix protein 1 (DMP1) and ectonucleotide pyrophosphatase/phosphodiesterase I (ENPP1) result in hypophosphatemic rickets with inappropriately high FGF23 levels, in both humans and genetically modified mice, however the mechanism by which they do so is unknown [5].
In addition to regulating serum calcium levels, parathyroid hormone (PTH) is also known to suppress serum Pi levels via the down regulation of the sodium phosphate co-transporters NaPi-2a and Na-Pi-2c, in renal proximal tubules, albeit with differing kinetics [14]: these molecules are also targets of FGF23 [15]. PTH also stimulates the synthesis of 1,25D by increasing the expression of CYP27B1 and decreasing the expression of CYP24A1 [16, 17]. In contrast, FGF23 down-regulates 1,25D by decreasing CYP27B1 and increasing CYP24A1 [18]. PTH and FGF23 are therefore now regarded as the dominant regulators of serum 1,25D. In addition to the interaction of FGF23 and PTH in regulating serum Pi and calcium levels, there is accumulating evidence that they regulate each other’s production. Lavi-Moshayoff et al. [19] showed that parathyroidectomy prevented the increase of FGF23 with high Pi levels seen in the adenine high-phosphorus diet-induced early kidney failure mouse model, which supports the hypothesis that PTH can directly stimulate FGF23 production. In the same report, it was shown that PTH increased Fgf23 mRNA levels in the rat osteoblastic cell line, UMR-106. Subsequently, Rhee et al. [20] reported that mice, in which a specific constitutively active PTH receptor 1 (PTHR1) was over-expressed specifically in osteocytes (Dmp1-caPTHR1), displayed high serum levels of intact FGF23, together with high bone levels of Fgf23 mRNA and of the gene Galnt3. The significance of the latter finding is that the protein product of Galnt3, N-acetylgalactosaminyl-transferase 3 (GalNAc-T3), is critical in the FGF23 regulatory pathway, as it protects intact FGF23 protein from inactivation by cleavage, by initiating O-glycosylation adjacent to the cleavage site [21,22,23]. These authors also showed that PTH increased levels of Fgf23 mRNA in primary osteoblast/osteocyte cultures [20]. In addition, they showed that PTH or PTHR1 signalling down-regulated Sost mRNA expression in rat UMR-106 cells, in the bone of Dmp1-caPTHR1 mice, and in primary osteoblasts and osteocytes, consistent with the findings of others [24, 25]. The effects of PTH or PTHR1 signalling on FGF23 expression were antagonised by co-treatment with sclerostin, the product of the Sost gene, in UMR-106 cells or by co-overexpression of Sost in osteocytes (Dmp1-SOST tg) in Dmp1-caPTHR1 mice [19, 20].
In humans, SOST is the causative gene for high bone mass condition Sclerosteosis (#269500) [26]. Sclerostin is expressed in bone predominantly by osteocytes [27], and has been shown to have a number of key autocrine/paracrine effects on osteoblast/osteocyte activity [28,29,30]. Sclerostin was shown to block canonical Wnt signalling by binding to the Wnt co-receptors low density lipoprotein receptor-related proteins (LRP)-5 and -6 [31]. Therefore, it was hypothesised that FGF23 production is directly stimulated by canonical Wnt signalling and indirectly by PTH via its suppressive effect on SOST gene expression. Ren et al. [32] treated hypophosphatemic Dmp1 knockout mice with neutralising antibody to SCL, which improved osteomalacia in these animals without attenuating the hypophosphatemia or the high levels of circulating FGF23. However, Ryan et al. [33] reported that serum intact FGF23 levels in Sost gene knock-out mice were reduced, consistent with a positive rather than a negative effect of sclerostin on FGF23 expression. Also, we have reported that Sost mRNA levels are elevated in the long bones of Phex deletion (Hyp) mice [28], which show hypophosphatemic rickets with increased serum intact FGF23 when compared with normal controls, although others have reported decreased levels in neonatal animals [34].
Clearly, interpretation of regulatory pathways of FGF23 production in vivo, is made complex due to the multi-organ and hormonal contributions, and an in vitro cell line model offers a simplified and ‘cleaner’ system to address these questions. To date, in vitro studies to investigating the regulation of FGF23 have been conducted in UMR-106 or primary bone cells, as the only cells expressing detectable FGF23 in vitro [11, 19, 35]. Recently, the mouse osteoblast-like cell line, IDG-SW3, was established, which differentiates into osteocyte-like cells expressing FGF23 [12, 36, 37]. To further investigate the regulation of FGF23 by PTH and sclerostin, we used differentiated IDG-SW3 cells, in which PTH and sclerostin both induced robust up-regulation of Fgf23 mRNA expression.
Materials and Methods
IDG-SW3 Cells
IDG-SW3 cells were cultured as described previously [12, 36, 37] and differentiated into cells that were morphologically osteocyte-like and expressed an osteocytic gene profile over a 35-day period. All further experiments were performed on IDG-SW3 cells differentiated for 35 days.
Recombinant PTH and Sclerostin Treatment
Differentiated IDG-SW3 cells were treated for the indicated time intervals with rhPTH1-34 (Tocris Bioscience) at concentrations between 1 and 100 nM or recombinant human sclerostin (rhSCL) (R&D Systems) at concentrations between 1 and 50 ng/ml [28, 29] for the time periods indicated. Media were also collected from differentiated IDG-SW3 cells treated for 24 h with rhPTH1-34 (100 nM) or rhSCL (50 ng/ml) for FGF23-specific ELISA. To determine the effects of rhPTH1-34 and rhSCL on Fgf23 or other related mRNA expression, differentiated IDG-SW3 cells treated with rhPTH1-34 (100 nM) or rhSCL (50 ng/ml) were harvested at 3, 6, 12 and 24 h. In some experiments, cells were also treated with the NF-κβ signalling inhibitor, BAY11 (Sigma) at 100 μM or N-Tosyl-L-Phenylalanine Chloromethyl Ketone (TPCK) (Sigma) at 100 μM one hour before the addition of rhPTH1-34 (100 nM) or rhSCL (50 ng/ml) and harvested after 6 h.
Human Bone Samples
All human experimentation was performed with the approval of our institutional Human Research Ethics Committee (Approval No. RAH 140216a). Human cancellous bone samples were obtained with written consent from patients undergoing total hip replacement surgery. Bone samples were digested twice with collagenase (10 mg/ml) at 37 °C for 30 min to remove marrow and lining cells [38], and then cut into pieces (~ 1 mm in diameter) using a sterile scalpel before being placed evenly in 12-well tissue culture plates in αMEM medium (Sigma) containing 2% FCS [37].
RNA Purification and Quantitative Real-Time PCR (qPCR)
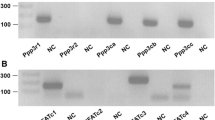
RNA was extracted from IDG-SW3 cells and human bone samples with TRIzol (Invitrogen) and then cDNA was synthesised with iScript (Bio-Rad). Real-Time PCR (CFX Connect™; Bio-Rad) was used to quantitate mRNA levels by qPCR, as described previously [29]. cDNA specific primers for qPCR were designed to amplify mRNA for murine glyceraldehyde-3-phosphate dehydrogenase (Gapdh), Fgf23, Sost, Phex, Dmp1, Enpp1, Galnt3, IL-6 and human GAPDH, FGF23, PHEX, DMP1 and ENPP1. All qPCR measurements were normalised to the expression of Gapdh/GAPDH mRNA (Supplementary Table S1).
FGF23 ELISA
FGF23 protein levels in the media and cell lysates were analysed by two different types of ELISA: the FGF-23 (C-Term) ELISA Kit (Immutopics, San Diego, CA, USA) utilises two epitopes, both detecting the C-terminal side of the cleavage point such that this kit detects both full-length FGF23 and its C-terminal fragment. On the other hand, the Intact FGF-23 ELISA Kit (Kainos, Tokyo, Japan) has epitopes N and C terminal to the physiological cleavage point (amino acid 179–180), and therefore exclusively detects functional, full-length FGF23 [39].
Statistical Analysis
All experiments were performed in triplicate. All data shown represent the mean ± standard error of the mean (SEM). Statistical analyses were performed by using One-Way Analysis of Variance (ANOVA) followed by Tukey’s post-hoc test or Student’s t test (two-tailed). Data were analysed using GraphPad Prism software (GraphPad Prism, CA, USA). The significance level is indicated by asterisks: *p < 0.05; **p < 0.01; ***p < 0.001.
Results
Effect of PTH 1-34 and Sclerostin on FGF23 Expression and Secretion
Differentiated IDG-SW3 cells expressed abundant Fgf23 mRNA, as reported previously [36]. When treated with rhPTH1-34 and rhSCL, Fgf23 mRNA levels increased markedly, in a dose-dependent manner. Fgf23 mRNA levels increased by more than 700-fold in response to rhPTH1-34 (100 nM) and by more than 200-fold in response to rhSCL (50 ng/ml), compared to untreated controls, in 24 h (Fig. 1a, b). Time-course studies revealed that Fgf23 mRNA levels peaked at more than 2,000 and 3,000-fold for rhPTH1-34 100 nM and rhSCL 50 ng/ml, respectively, within 3 to 12 h of treatment (Fig. 1c, d). RhPTH1-34 and rhSCL also both induced FGF23 mRNA expression in human cancellous bone samples cultured ex vivo, although to a lesser extent due possibly to the inefficient diffusion of these agents into the lacunocanalicular pores by passive diffusion (Suppl Fig. S1).
Effect of PTH and rhSCL treatment on Fgf23 mRNA expression and FGF23 secretion. IDG-SW3 cells differentiated for 5 weeks were treated with a rhPTH1-34 and b rhSCL for 24 h at the concentrations indicated and Fgf23 mRNA levels measured by real time RT-PCR. Fgf23 mRNA levels were also measured in a time course in response to c rhPTH1-34 (100 nM), and d rhSCL (50 ng/ml). Gene expression was normalised to Gapdh mRNA levels and data described as mean fold-change ± standard error of the mean (SEM) relative to the untreated normal control (NC) or the time zero level. Media from IDG-SW3 cells differentiated for 5 weeks and treated with rhPTH1-34 (100 ng/ml) or rhSCL (50 ng/ml) for 24 h were measured using e FGF23 (C-Term) and f Intact FGF23 ELISA kits. Data shown are means ± SEM of quadruplicate readings. Significant difference to the reference level is depicted by *p < 0.05; **p < 0.01; ***p < 0.001
Treatment with either rhPTH1-34 or rhSCL for 24 h resulted in abundant secretion of FGF23 measured by the C-terminal FGF23 ELISA kit (Fig. 1e) confirming that the effects on Fgf23 mRNA levels by both rhPTH1-34 and rhSCL resulted in new FGF23 protein synthesis. However, there was no significant change in the levels of secreted intact FGF23 in response to these treatments (Fig. 1f). This is consistent with our previous observations, that the IDG-SW3 model exhibits constitutively active furin-like proprotein convertase activity and/or a deficiency in the ability to protect newly translated FGF23 protein by O-glycosylation [37].
Effect of PTH and SCL on FGF23 Regulatory Gene Expression
The expression of genes implicated in control of FGF23 levels was also investigated. In differentiated IDG-SW3 cells, Phex (Fig. 2a, b), Dmp1 and Enpp1 mRNA levels were significantly decreased by both rhPTH1-34 and rhSCL at several concentrations (Suppl Fig. S2, S3), although Dmp1 mRNA levels were up-regulated at lower concentrations of rhPTH1-34 (1 nM) and rhSCL (1 nM) (Suppl Fig. S2A&B). Suppression of Phex, Dmp1 and Enpp1 mRNA by rhPTH1-34 and rhSCL was seen by 3 to 6 h of treatment and persisted for at least 24 h for Phex and Dmp1 (Fig. 2c, d, Suppl Fig. S2 C&D, S3 C&D). A clear although variable increase of Galnt3 mRNA levels was observed in response to either rhPTH1-34 or rhSCL by 3–6 h of treatment (Fig. 3a–d).
Effect of PTH and rhSCL treatment on Phex mRNA expression. IDG-SW3 cells differentiated for 5 weeks were treated with a rhPTH1-34 and b rhSCL for 24 h at the concentrations indicated and Phex mRNA levels measured by real time RT-PCR. Phex mRNA levels were also measured in a time course in response to c rhPTH1-34 (100 nM), and d rhSCL (50 ng/ml). Gene expression was normalised to Gapdh mRNA levels and data described as mean fold-change ± SEM relative to the untreated normal control (NC) or the time zero level. Significant difference to the reference level is depicted by *p < 0.05; **p < 0.01; ***p < 0.001
Effect of PTH and rhSCL treatment on Galnt3 mRNA expression. IDG-SW3 cells differentiated for 5 weeks were treated with a rhPTH1-34 and b rhSCL for 24 h at the concentrations indicated and Galnt3 mRNA levels measured by real time RT-PCR. Galnt3 mRNA levels were also measured in a time course in response to c rhPTH1-34 (100 nM), and d rhSCL (50 ng/ml). Gene expression was normalised to Gapdh mRNA levels and data described as mean fold-change ± SEM relative to the untreated normal control (NC) or the time zero level. Significant difference to the reference level is depicted by *p < 0.05; **p < 0.01; ***p < 0.001
Effect of NFκB Inhibition
We reported recently that pro-inflammatory factors, including tumour necrosis factor alpha (TNFα) and interleukin-1β (IL-1β) stimulated the synthesis of Fgf23 mRNA via NF-κβ signalling [37], and it was also reported by others that PTH stimulates NF-κβ signalling in bone cells and in renal tubular cells [40,41,42]. In the current study, the induction of IL-6 mRNA, a well-known readout of NF-κβ signalling, was observed in response to rhPTH1-34 and rhSCL (Fig. 4a–d). To investigate the involvement of NF-κβ signalling in PTH and sclerostin mediated regulation on Fgf23 expression, differentiated IDG-SW3 cells were treated with the NF-κβ inhibitors, BAY11 or TPCK, one hour prior to rhPTH1-34 or rhSCL treatments. Both BAY11 and TPCK significantly antagonised the effect of both rhPTH1-34 and rhSCL on Fgf23 mRNA expression (Fig. 4e, f).
Effect of PTH and rhSCL on the IL-6/NF-κB pathway. IDG-SW3 cells differentiated for 5 weeks were treated with a rhPTH1-34 and b rhSCL for 24 h at the concentrations indicated and Il6 mRNA levels measured by real time RT-PCR. Il6 mRNA levels were also measured in a time course in response to c rhPTH1-34 (100 nM), and d rhSCL (50 ng/ml). Differentiated (5 wk) IDG-SW3 cells were pre-treated with NF-κβ signal inhibitors Bay11 (100 μM) or TPCK (100 μM) for 1 h before treatment with e rhPTH1-34 (100 nM) or f rhSCL (50 ng/ml) for 24 h and Fgf23 mRNA levels were quantified by real-time RT-PCR. Gene expression was normalised to Gapdh mRNA levels and data described as mean fold-change ± SEM relative to the untreated normal control (NC) or the time zero level. Significant difference to the reference level is depicted by *p < 0.05; **p < 0.01; ***p < 0.001
The effects of inhibitors on rhPTH1-34 and rhSCL regulation of other regulators of FGF23 was also examined (Suppl Fig. 4). NF-κβ inhibition with Bay11 did not reverse the inhibitory effects of PTH on Phex, Dmp1 and Enpp1 mRNA levels. TPCK had a similar effect although the PTH inhibition of Dmp1 was reversed. Overall, the effects of PTH on these genes appeared NF-κβ independent. The apparent exacerbation of the PTH inhibitory effect may have been due to altered kinetics of expression in the presence of the inhibitors. Similarly, the reduction of Phex and Enpp1 mRNA expression by rhSCL was largely unaffected by NF-κβ inhibition. Inhibition of Dmp1 expression by rhSCL however, like Fgf23 expression, exhibited NF-κβ-dependence (Suppl Fig. 4).
Discussion
PTH has been a long time candidate regulator of FGF23 levels. It has been shown that injection of rhPTH1-34 increased serum intact FGF23 levels within 18 h [43] with no significant change in serum Pi levels. However, in that study, the effect on FGF23 levels was preceded by an increase in 1,25D levels, and, as stated, 1,25D is a known positive regulator of FGF23. Brown et al. [44] reported high intact FGF23 levels in a patient with Jansen’s metaphyseal chondrodysplasia (#156400), a condition caused by a gain of function mutation of the PTH1R gene resulting in the constitutive activation of the PTH and PTH related protein (PTHrP) signalling pathway. As this patient also showed low serum Pi and normal serum 1,25D levels, this finding implied a direct stimulatory effect of PTH on FGF23 expression [44]. These observations illustrate the complexity of unravelling the in vivo regulation of Pi, Ca and 1,25D levels, and whether PTH stimulates FGF23 directly or indirectly. Rhee et al. and Lavi-Moshayoff et al., respectively, showed the direct positive effect of PTH on Fgf23 mRNA production possibly via the down-regulation of Sost expression in mouse primary osteoblast/osteocyte cultures and the rat osteoblast-like cell line UMR-106, which was previously the only cell line known to express Fgf23 [19, 20, 35]. SOST is considered to be one of the key target genes when PTH1-34 is administered in an intermittent fashion as a pro-anabolic treatment for osteoporosis. We recently showed that sclerostin targets cells at the late osteoblast/pre-osteocyte and osteocyte stages, target populations to those of PTH, and acts as an autocrine/paracrine regulator of matrix mineralisation [28, 29, 45] and of osteocyte support of osteoclast activity [30]. It was possible, therefore, that the actions of PTH and sclerostin were overlapping, bisynchronous or conflicting, with respect to FGF23 production.
The murine osteoblast-like cell-line, IDG-SW3, has emerged as a promising cell model, with which to examine the regulation of FGF23 expression, in particular when it is differentiated to a mature osteocyte-like stage [12, 36]. Here, Fgf23 mRNA expression was strongly stimulated by PTH in these cells, up to more than 2000-fold 6 h after treatment, which is considerably greater than previous studies using UMR-106 cells where 4 to 5-fold induction was reported [19], perhaps reflective of the more osteocyte-like qualities of differentiated IDG-SW3 cells. Importantly, synthesis of Fgf23 mRNA was also induced by rhSCL, to a similar extent to rhPTH1-34. Under the experimental conditions employed, despite other osteocytic genes, including Dmp1, Phex, Mepe and Fgf23 itself, being relatively abundantly expressed, the endogenous Sost mRNA levels were detectable but low and were unchanged further by rhPTH1-34 exposure (data not shown). The reasons for this variation in cell line behaviour are currently unknown, however PTH has been demonstrated to suppress SOST expression in a number of rodent and human cell line and primary osteoblast/osteocyte models [19, 20, 24, 25, 36, 38, 46].
PHEX, DMP1 and ENPP1 proteins are thought to constitutively suppress serum intact FGF23 levels in healthy subjects [5]. Here, the observed down-regulation of expression of Phex, Dmp1 and Enpp1 mRNA and the increase of Galnt3 mRNA levels in response to rhPTH1-34 or rhSCL, could all constitute part of the mechanism for the increase of Fgf23 mRNA and/or FGF23 protein levels in response to rhPTH1-34, or indeed sclerostin in vivo, given the results of the loss of function mutation of these genes [22, 23, 39, 47,48,49,50,51,52].
PTH/PTHR1 signalling is mediated by the classical cyclic AMP (cAMP)/protein kinase A (PKA) pathway [53] and has also been long known to activate NF-κβ [54]. We reported previously that pro-inflammatory mediators increased Fgf23 expression via an NF-κβ-dependent pathway [37]. The downstream target gene of NF-κβ, IL6 [55], was strongly induced by both rhPTH1-34, consistent with a previous report [56], and rhSCL. Two NF-κβ signalling pathway inhibitors, Bay11 and TPCK, significantly reversed the effect of both rhPTH1-34 and rhSCL on Fgf23 mRNA levels. These findings are consistent with previous studies implicating the NF-κβ signalling pathway in regulating FGF23 expression in osteoblasts and osteocytes [57, 58]. However, further detailed studies are warranted to fully elucidate the signalling pathways, by which PTH and sclerostin regulate FGF23 expression.
The dramatic increase in Fgf23 mRNA levels observed in response to both PTH1-34 and rhSCL, was reflected in the amount of secreted C-terminal fragments of FGF23 protein in the media. However, similar to our previous findings with pro-inflammatory mediators [37], intact FGF23 secreted in the media were unchanged, confirming that the levels of the intact hormone are finally determined by the level of protective post-translational O-glycosylation and Furin/Furin-like protein convertase activity, which mediates cleavage or protection of FGF23 protein [22, 23, 59,60,61,62,63]. This post-translational regulatory mechanism also functions as the terminal rate-limiting step to define the amount of active FGF23 secreted in response to serum Pi levels in vivo [60, 61, 63]. Consistent with the importance of this mechanism and with findings here, PTH1-34 was shown to elicit C-terminal FGF23 in vivo in mice without altering intact hormone levels, unless a furin inhibitor was also administered [64]. Although the rhPTH1-34 and rhSCL failed to increase intact FGF23 levels in IDG-SW3 cultures despite increased Galnt3 mRNA expression, IDG-SW3 might be a promising tool to investigate the detailed mechanism of the Pi sensing system in FGF23 transcription, which remains to be fully elucidated. We have reported previously that Fgf23 mRNA levels are sensitive to Pi using this cell model [12].
The findings of this study beg the question as to their possible physiological relevance. We previously reported that NF-κβ signalling in response to pro-inflammatory cytokines or LPS also induces the transcription of Fgf23 mRNA without changing the intact FGF23 level in IDG-SW3 cells [37]. Therefore, it might be that the activators of osteoclast differentiation and activity, such as the local hypoxia due to low serum Fe [65] or NF-κβ signalling, also enhance the synthesis of FGF23 mRNA for the purpose of increasing intact FGF23 levels in order to decrease excess serum Pi due to bone resorption. We have demonstrated that sclerostin induces mineral release by osteocytes [29, 45], suggesting that local induction of FGF23 production may also occur in response to osteocytic osteolysis. Consistent with this, evidence for increased osteocytic osteolysis was reported in the murine XLH model, Hyp [66]. On the other hand, a continuously high serum level of PTH also has a bone catabolic effect [67] and sclerostin is identified as the inhibitor of osteogenic differentiation [26, 28, 31]. In light of this evidence, an osteoclastic or anti-osteogenic signal might have the ability to induce FGF23 expression with a concomitant suppressive effect on PHEX, DMP1 and ENPP1 mRNA levels and a stimulating effect on GALNT3 expression, partly via the NF-κβ signalling pathway.
There are no reports of human sclerosteosis patients [26, 31] showing disturbances of serum Pi levels. However, Sost KO mice were reported to exhibit low serum intact FGF23 levels with high serum Pi [33]. Also, intriguingly, in Jansen’s metaphyseal chondrodysplasia patients caused by constitutively active PTH1R, both serum intact FGF23 and C-terminal FGF23 were reported to be high, which causes low serum Pi levels [44], and which may imply that sclerostin and PTH are not only inducers of FGF23 mRNA transcription, as observed here, but also involved in the post-translational regulation of FGF23 in vivo to some extent. Consistent with this hypothesis is the observation that in patients with chronic hypoparathyroidism, hyperphosphatemia is not fully corrected by FGF23 action [68]. Interestingly, elevated serum sclerostin levels were reported in a cohort of young adult patients with XLH; unfortunately, FGF23 levels were not measured preventing a direct correlation between the two [69]. It will be of interest to observe the effects that clinical neutralisation of FGF23 in the case of XLH and other hypophosphatemic patient cohorts [70] has on either circulating or bone sclerostin levels.
Other potential regulators of FGF23 expression, FGFR1, FGFR3 and Klotho, were not examined in this study. These are known to form co-receptor complexes for FGF23 on target cells, mainly in kidney and liver but potentially also in osteocytes, as recently reviewed [71].
In summary, here we report the potent induction of FGF23 expression by both PTH and sclerostin. The precise post-translational regulatory mechanism(s) of intact FGF23 levels requires further study in terms of elucidating the Pi sensing mechanisms in osteocytes. To this end, IDG-SW3 is a promising cell model with which to study this. This study extends the known autocrine/paracrine effects of sclerostin on the osteoblast/osteocyte. It also provides the intriguing possibility that the down-regulation of SOST by PTH is required for the anabolic response to intermittent PTH1-34 because sclerostin and PTH have both overlapping and possibly discordant effects.
References
ADHR Consortium (2000) Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. Nat Genet 26:345–348
Shimada T, Mizutani S, Muto T, Yoneya T, Hino R, Takeda S, Takeuchi Y, Fujita T, Fukumoto S, Yamashita T (2001) Cloning and characterization of FGF23 as a causative factor of tumor-induced osteomalacia. Proc Natl Acad Sci USA 98:6500–6505
Urakawa I, Yamazaki Y, Shimada T, Iijima K, Hasegawa H, Okawa K, Fujita T, Fukumoto S, Yamashita T (2006) Klotho converts canonical FGF receptor into a specific receptor for FGF23. Nature 444:770–774
Kurosu H, Ogawa Y, Miyoshi M, Yamamoto M, Nandi A, Rosenblatt KP, Baum MG, Schiavi S, Hu MC, Moe OW, Kuro-o M (2006) Regulation of fibroblast growth factor-23 signaling by klotho. J Biol Chem 281:6120–6123
Ito N, Findlay DM, Atkins GJ (2014) Osteocyte communication with the kidney via the production of FGF23: remote control of phosphate homeostasis. Clin Rev Bone Miner Metab 12:44–58
Perwad F, Azam N, Zhang MY, Yamashita T, Tenenhouse HS, Portale AA (2005) Dietary and serum phosphorus regulate fibroblast growth factor 23 expression and 1,25-dihydroxyvitamin D metabolism in mice. Endocrinology 146:5358–5364
Saito H, Maeda A, Ohtomo S, Hirata M, Kusano K, Kato S, Ogata E, Segawa H, Miyamoto K, Fukushima N (2005) Circulating FGF-23 is regulated by 1alpha,25-dihydroxyvitamin D3 and phosphorus in vivo. J Biol Chem 280:2543–2549
Ferrari SL, Bonjour JP, Rizzoli R (2005) Fibroblast growth factor-23 relationship to dietary phosphate and renal phosphate handling in healthy young men. J Clin Endocrinol Metab 90:1519–1524
Yu X, Sabbagh Y, Davis SI, Demay MB, White KE (2005) Genetic dissection of phosphate- and vitamin D-mediated regulation of circulating Fgf23 concentrations. Bone 36:971–977
Burnett SM, Gunawardene SC, Bringhurst FR, Juppner H, Lee H, Finkelstein JS (2006) Regulation of C-terminal and intact FGF-23 by dietary phosphate in men and women. J Bone Miner Res 21:1187–1196
Yamamoto R, Minamizaki T, Yoshiko Y, Yoshioka H, Tanne K, Aubin JE, Maeda N (2010) 1alpha,25-dihydroxyvitamin D3 acts predominately in mature osteoblasts under conditions of high extracellular phosphate to increase fibroblast growth factor 23 production in vitro. J Endocrinol 206:279–286
Ito N, Findlay DM, Anderson PH, Bonewald LF, Atkins GJ (2013) Extracellular phosphate modulates the effect of 1alpha,25-dihydroxy vitamin D3 (1,25D) on osteocyte like cells. J Steroid Biochem Mol Biol 136:183–186
Takashi Y, Kosako H, Sawatsubashi S, Kinoshita Y, Ito N, Tsoumpra MK, Nangaku M, Abe M, Matsuhisa M, Kato S, Matsumoto T, Fukumoto S (2019) Activation of unliganded FGF receptor by extracellular phosphate potentiates proteolytic protection of FGF23 by its O-glycosylation. Proc Natl Acad Sci USA 116:11418–11427
Levi M, Gratton E (2019) Visualizing the regulation of SLC34 proteins at the apical membrane. Pflugers Arch 471:533–542
Gattineni J, Bates C, Twombley K, Dwarakanath V, Robinson ML, Goetz R, Mohammadi M, Baum M (2009) FGF23 decreases renal NaPi-2a and NaPi-2c expression and induces hypophosphatemia in vivo predominantly via FGF receptor 1. Am J Physiol Renal Physiol 297:F282-291
Zierold C, Mings JA, DeLuca HF (2001) Parathyroid hormone regulates 25-hydroxyvitamin D(3)-24-hydroxylase mRNA by altering its stability. Proc Natl Acad Sci USA 98:13572–13576
Zierold C, Mings JA, DeLuca HF (2003) Regulation of 25-hydroxyvitamin D3–24-hydroxylase mRNA by 1,25-dihydroxyvitamin D3 and parathyroid hormone. J Cell Biochem 88:234–237
Shimada T, Hasegawa H, Yamazaki Y, Muto T, Hino R, Takeuchi Y, Fujita T, Nakahara K, Fukumoto S, Yamashita T (2004) FGF-23 is a potent regulator of vitamin D metabolism and phosphate homeostasis. J Bone Miner Res 19:429–435
Lavi-Moshayoff V, Wasserman G, Meir T, Silver J, Naveh-Many T (2010) PTH increases FGF23 gene expression and mediates the high-FGF23 levels of experimental kidney failure: a bone parathyroid feedback loop. Am J Physiol Renal Physiol 299:F882-889
Rhee Y, Bivi N, Farrow E, Lezcano V, Plotkin LI, White KE, Bellido T (2011) Parathyroid hormone receptor signaling in osteocytes increases the expression of fibroblast growth factor-23 in vitro and in vivo. Bone 49:636–643
Topaz O, Shurman DL, Bergman R, Indelman M, Ratajczak P, Mizrachi M, Khamaysi Z, Behar D, Petronius D, Friedman V, Zelikovic I, Raimer S, Metzker A, Richard G, Sprecher E (2004) Mutations in GALNT3, encoding a protein involved in O-linked glycosylation, cause familial tumoral calcinosis. Nat Genet 36:579–581
Frishberg Y, Ito N, Rinat C, Yamazaki Y, Feinstein S, Urakawa I, Navon-Elkan P, Becker-Cohen R, Yamashita T, Araya K, Igarashi T, Fujita T, Fukumoto S (2007) Hyperostosis-hyperphosphatemia syndrome: a congenital disorder of O-glycosylation associated with augmented processing of fibroblast growth factor 23. J Bone Miner Res 22:235–242
Ichikawa S, Sorenson AH, Austin AM, Mackenzie DS, Fritz TA, Moh A, Hui SL, Econs MJ (2009) Ablation of the Galnt3 gene leads to low-circulating intact fibroblast growth factor 23 (Fgf23) concentrations and hyperphosphatemia despite increased Fgf23 expression. Endocrinology 150:2543–2550
Bellido T, Ali AA, Gubrij I, Plotkin LI, Fu Q, O’Brien CA, Manolagas SC, Jilka RL (2005) Chronic elevation of parathyroid hormone in mice reduces expression of sclerostin by osteocytes: a novel mechanism for hormonal control of osteoblastogenesis. Endocrinology 146:4577–4583
Keller H, Kneissel M (2005) SOST is a target gene for PTH in bone. Bone 37:148–158
Brunkow ME, Gardner JC, Van Ness J, Paeper BW, Kovacevich BR, Proll S, Skonier JE, Zhao L, Sabo PJ, Fu Y, Alisch RS, Gillett L, Colbert T, Tacconi P, Galas D, Hamersma H, Beighton P, Mulligan J (2001) Bone dysplasia sclerosteosis results from loss of the SOST gene product, a novel cystine knot-containing protein. Am J Hum Genet 68:577–589
Poole KE, van Bezooijen RL, Loveridge N, Hamersma H, Papapoulos SE, Löwik CW, Reeve J (2005) Sclerostin is a delayed secreted product of osteocytes that inhibits bone formation. FASEB J 19:1842–1844
Atkins GJ, Rowe PS, Lim HP, Welldon KJ, Ormsby R, Wijenayaka AR, Zelenchuk L, Evdokiou A, Findlay DM (2011) Sclerostin is a locally acting regulator of late-osteoblast/preosteocyte differentiation and regulates mineralization through a MEPE-ASARM-dependent mechanism. J Bone Miner Res 26:1425–1436
Kogawa M, Wijenayaka AR, Ormsby RT, Thomas GP, Anderson PH, Bonewald LF, Findlay DM, Atkins GJ (2013) Sclerostin regulates release of bone mineral by osteocytes by induction of carbonic anhydrase 2. J Bone Miner Res 28:2436–2448
Wijenayaka AR, Kogawa M, Lim HP, Bonewald LF, Findlay DM, Atkins GJ (2011) Sclerostin stimulates osteocyte support of osteoclast activity by a RANKL-dependent pathway. PLoS ONE 6:e25900
Li X, Zhang Y, Kang H, Liu W, Liu P, Zhang J, Harris SE, Wu D (2005) Sclerostin binds to LRP5/6 and antagonizes canonical Wnt signaling. J Biol Chem 280:19883–19887
Ren Y, Han X, Jing Y, Yuan B, Ke H, Liu M, Feng JQ (2016) Sclerostin antibody (Scl-Ab) improves osteomalacia phenotype in dentin matrix protein 1(Dmp1) knockout mice with little impact on serum levels of phosphorus and FGF23. Matrix Biol 52–54:151–161
Ryan ZC, Ketha H, McNulty MS, McGee-Lawrence M, Craig TA, Grande JP, Westendorf JJ, Singh RJ, Kumar R (2013) Sclerostin alters serum vitamin D metabolite and fibroblast growth factor 23 concentrations and the urinary excretion of calcium. Proc Natl Acad Sci USA 110:6199–6204
Liu S, Tang W, Fang J, Ren J, Li H, Xiao Z, Quarles LD (2009) Novel regulators of Fgf23 expression and mineralization in Hyp bone. Mol Endocrinol 23:1505–1518
Kolek OI, Hines ER, Jones MD, LeSueur LK, Lipko MA, Kiela PR, Collins JF, Haussler MR, Ghishan FK (2005) 1alpha,25-Dihydroxyvitamin D3 upregulates FGF23 gene expression in bone: the final link in a renal-gastrointestinal-skeletal axis that controls phosphate transport. Am J Physiol Gastrointest Liver Physiol 289:G1036-1042
Woo SM, Rosser J, Dusevich V, Kalajzic I, Bonewald LF (2011) Cell line IDG-SW3 replicates osteoblast-to-late-osteocyte differentiation in vitro and accelerates bone formation in vivo. J Bone Miner Res 26:2634–2646
Ito N, Wijenayaka AR, Prideaux M, Kogawa M, Ormsby RT, Evdokiou A, Bonewald LF, Findlay DM, Atkins GJ (2015) Regulation of FGF23 expression in IDG-SW3 osteocytes and human bone by pro-inflammatory stimuli. Mol Cell Endocrinol 399:208–218
Prideaux M, Schutz C, Wijenayaka AR, Findlay DM, Campbell DG, Solomon LB, Atkins GJ (2016) Isolation of osteocytes from human trabecular bone. Bone 88:64–72
Ito N, Fukumoto S, Takeuchi Y, Yasuda T, Hasegawa Y, Takemoto F, Tajima T, Dobashi K, Yamazaki Y, Yamashita T, Fujita T (2005) Comparison of two assays for fibroblast growth factor (FGF)-23. J Bone Miner Metab 23:435–440
Feyen JH, Elford P, Di Padova FE, Trechsel U (1989) Interleukin-6 is produced by bone and modulated by parathyroid hormone. J Bone Miner Res 4:633–638
Lowik CW, van der Pluijm G, Bloys H, Hoekman K, Bijvoet OL, Aarden LA, Papapoulos SE (1989) Parathyroid hormone (PTH) and PTH-like protein (PLP) stimulate interleukin-6 production by osteogenic cells: a possible role of interleukin-6 in osteoclastogenesis. Biochem Biophys Res Commun 162:1546–1552
Guo Y, Yuan W, Wang L, Shang M, Peng Y (2011) Parathyroid hormone-potentiated connective tissue growth factor expression in human renal proximal tubular cells through activating the MAPK and NF-kappaB signalling pathways. Nephrol Dial Transpl 26:839–847
Burnett-Bowie SM, Henao MP, Dere ME, Lee H, Leder BZ (2009) Effects of hPTH(1–34) infusion on circulating serum phosphate, 1,25-dihydroxyvitamin D, and FGF23 levels in healthy men. J Bone Miner Res 24:1681–1685
Brown WW, Juppner H, Langman CB, Price H, Farrow EG, White KE, McCormick KL (2009) Hypophosphatemia with elevations in serum fibroblast growth factor 23 in a child with Jansen’s metaphyseal chondrodysplasia. J Clin Endocrinol Metab 94:17–20
Kogawa M, Khalid KA, Wijenayaka AR, Ormsby RT, Evdokiou A, Anderson PH, Findlay DM, Atkins GJ (2018) Recombinant sclerostin antagonizes effects of ex vivo mechanical loading in trabecular bone and increases osteocyte lacunar size. Am J Physiol Cell Physiol 314:C53–C61
Prideaux M, Wijenayaka AR, Kumarasinghe DD, Ormsby RT, Evdokiou A, Findlay DM, Atkins GJ (2014) SaOS2 Osteosarcoma cells as an in vitro model for studying the transition of human osteoblasts to osteocytes. Calcif Tissue Int 95:183–193
The HYP Consortium (1995) A gene (PEX) with homologies to endopeptidases is mutated in patients with X-linked hypophosphatemic rickets. HYP Consortium Nat Genet 11:130–136
Yamazaki Y, Okazaki R, Shibata M, Hasegawa Y, Satoh K, Tajima T, Takeuchi Y, Fujita T, Nakahara K, Yamashita T, Fukumoto S (2002) Increased circulatory level of biologically active full-length FGF-23 in patients with hypophosphatemic rickets/osteomalacia. J Clin Endocrinol Metab 87:4957–4960
Lorenz-Depiereux B, Bastepe M, Benet-Pages A, Amyere M, Wagenstaller J, Muller-Barth U, Badenhoop K, Kaiser SM, Rittmaster RS, Shlossberg AH, Olivares JL, Loris C, Ramos FJ, Glorieux F, Vikkula M, Juppner H, Strom TM (2006) DMP1 mutations in autosomal recessive hypophosphatemia implicate a bone matrix protein in the regulation of phosphate homeostasis. Nat Genet 38:1248–1250
Feng JQ, Ward LM, Liu S, Lu Y, Xie Y, Yuan B, Yu X, Rauch F, Davis SI, Zhang S, Rios H, Drezner MK, Quarles LD, Bonewald LF, White KE (2006) Loss of DMP1 causes rickets and osteomalacia and identifies a role for osteocytes in mineral metabolism. Nat Genet 38:1310–1315
Lorenz-Depiereux B, Schnabel D, Tiosano D, Hausler G, Strom TM (2010) Loss-of-function ENPP1 mutations cause both generalized arterial calcification of infancy and autosomal-recessive hypophosphatemic rickets. Am J Hum Genet 86:267–272
Levy-Litan V, Hershkovitz E, Avizov L, Leventhal N, Bercovich D, Chalifa-Caspi V, Manor E, Buriakovsky S, Hadad Y, Goding J, Parvari R (2010) Autosomal-recessive hypophosphatemic rickets is associated with an inactivation mutation in the ENPP1 gene. Am J Hum Genet 86:273–278
Suva LJ, Friedman PA (2020) PTH and PTHrP actions on bone. Handb Exp Pharmacol 262:27–45
Ali NN, Gilston V, Winyard PG (1999) Activation of NF-κB in human osteoblasts by stimulators of bone resorption. FEBS Lett 460:315–320
Libermann TA, Baltimore D (1990) Activation of interleukin-6 gene expression through the NF-kappa B transcription factor. Mol Cell Biol 10:2327–2334
Guillén C, Martı́nez P, de Gortázar AR, Martı́nez MaE, Esbrit P (2002) Both N- and C-terminal domains of parathyroid hormone-related protein increase interleukin-6 by nuclear factor-κB activation in osteoblastic cells. J Biol Chem 277:28109–28117
Ewendt F, Föller M (2019) p38MAPK controls fibroblast growth factor 23 (FGF23) synthesis in UMR106-osteoblast-like cells and in IDG-SW3 osteocytes. J Endocrinol Invest 42:1477–1483
Bär L, Hase P, Föller M (2019) PKC regulates the production of fibroblast growth factor 23 (FGF23). PLoS ONE 14:e0211309
Kato K, Jeanneau C, Tarp MA, Benet-Pages A, Lorenz-Depiereux B, Bennett EP, Mandel U, Strom TM, Clausen H (2006) Polypeptide GalNAc-transferase T3 and familial tumoral calcinosis. Secretion of fibroblast growth factor 23 requires O-glycosylation. J Biol Chem 281:18370–18377
Farrow EG, Yu X, Summers LJ, Davis SI, Fleet JC, Allen MR, Robling AG, Stayrook KR, Jideonwo V, Magers MJ, Garringer HJ, Vidal R, Chan RJ, Goodwin CB, Hui SL, Peacock M, White KE (2011) Iron deficiency drives an autosomal dominant hypophosphatemic rickets (ADHR) phenotype in fibroblast growth factor-23 (Fgf23) knock-in mice. Proc Natl Acad Sci USA 108:E1146-1155
Imel EA, Peacock M, Gray AK, Padgett LR, Hui SL, Econs MJ (2011) Iron modifies plasma FGF23 differently in autosomal dominant hypophosphatemic rickets and healthy humans. J Clin Endocrinol Metab 96:3541–3549
Schjoldager KT, Vester-Christensen MB, Goth CK, Petersen TN, Brunak S, Bennett EP, Levery SB, Clausen H (2011) A systematic study of site-specific GalNAc-type O-glycosylation modulating proprotein convertase processing. J Biol Chem 286:40122–40132
Bhattacharyya N, Wiench M, Dumitrescu C, Connolly BM, Bugge TH, Patel HV, Gafni RI, Cherman N, Cho M, Hager GL, Collins MT (2012) Mechanism of FGF23 processing in fibrous dysplasia. J Bone Miner Res 27:1132–1141
Knab VM, Corbin B, Andrukhova O, Hum JM, Ni P, Rabadi S, Maeda A, White KE, Erben RG, Juppner H, Christov M (2017) Acute parathyroid hormone injection increases C-terminal but not intact fibroblast growth factor 23 levels. Endocrinology 158:1130–1139
Arnett TR (2010) Acidosis, hypoxia and bone. Arch Biochem Biophys 503:103–109
Tokarz D, Martins JS, Petit ET, Lin CP, Demay MB, Liu ES (2018) Hormonal regulation of osteocyte perilacunar and canalicular remodeling in the hyp mouse model of X-linked hypophosphatemia. J Bone Miner Res 33:499–509
Qin L, Raggatt LJ, Partridge NC (2004) Parathyroid hormone: a double-edged sword for bone metabolism. Trends Endocrinol Metab 15:60–65
Gupta A, Winer K, Econs MJ, Marx SJ, Collins MT (2004) FGF-23 is elevated by chronic hyperphosphatemia. J Clin Endocrinol Metab 89:4489–4492
Palomo T, Glorieux FH, Rauch F (2014) Circulating sclerostin in children and young adults with heritable bone disorders. J Clin Endocrinol Metab 99:E920-925
Kinoshita Y, Fukumoto S (2018) X-linked hypophosphatemia and FGF23-related hypophosphatemic diseases: prospect for new treatment. Endocr Rev 39:274–291
Agoro R, Ni P, Noonan ML, White KE (2020) Osteocytic FGF23 and Its Kidney Function. Front Endocrinol 11:592
Acknowledgements
This work was supported by funding from the National Health and Medical Research Council of Australia (NHMRC) Project Grant Scheme (Grant ID 10477960).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Nobuaki Ito, Matthew Prideaux, Asiri R. Wijenayaka, Dongqing Yang, Renee T. Ormsby, Lynda F. Bonewald and Gerald J. Atkins declared no conflicts of interest.
Human and Animal Rights and Informed Consent
Informed consent was obtained from all individual participants included in the study. The study was approved by the Human Research Ethics Committee of the RAH (Protocol no 140216a).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ito, N., Prideaux, M., Wijenayaka, A.R. et al. Sclerostin Directly Stimulates Osteocyte Synthesis of Fibroblast Growth Factor-23. Calcif Tissue Int 109, 66–76 (2021). https://doi.org/10.1007/s00223-021-00823-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-021-00823-6