Abstract
Selective serotonin reuptake inhibitors (SSRIs) have been shown to have a clinically significant impact on bone metabolism. To explore this further, we aimed to determine whether these agents are associated with serum markers of bone turnover utilising a population-based sample of men (n = 1138; 20–96 year) participating in the Geelong Osteoporosis Study. Blood samples were obtained and the bone resorption marker, C-telopeptide (CTx) and formation marker, type 1 procollagen amino-terminal-propeptide (PINP) were measured. Anthropometry and socio-economic status (SES) were determined and information on medication use and lifestyle was obtained via questionnaire. Lifetime mood disorders were assessed using semi-structured clinical interviews. Thirty-seven (3.3%) men reported using SSRIs. Age was an effect modifier in the association between SSRIs and markers of bone turnover. Among younger men (20–60 year; n = 557), adjusted mean CTx and PINP values were 12.4% [16.7 (95% CI 14.6–18.8) vs 19.1 (95% CI 18.7–19.4) pg/ml, p = 0.03] and 13.6% [5.6 (95% CI 4.9–6.3) vs 6.4 (95% CI 6.3–6.6) pg/ml, p = 0.02] lower among SSRI users compared to non-users, respectively. No differences in SSRI use and markers of bone turnover were detected among older men (61–94 year; all p > 0.05). These patterns persisted after further adjustment for activity, alcohol, smoking, SES, depression, bone active medications and other antidepressants. Our data suggest that SSRI use is associated with alterations in bone turnover markers among younger men. The observed decreases in both CTx and PINP are likely to contribute to a low bone turnover state and increased skeletal fragility with this potential imbalance between formation and resorption resulting in subsequent bone loss.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paralleling the high prevalence and disease burden of depression, the global use of antidepressants has increased substantially, such that approximately one in ten are prescribed these agents [1]. Osteoporosis is similarly a common disorder, characterised by impairment in bone quality resulting in an increased susceptibility to fracture [2]. It has been estimated to affect one in three women and one in five men over the age of 50 years [3], with osteoporosis estimated to cause more than 8.9 million fractures annually across the globe [4]. The total cost associated with osteoporosis, osteopenia (low bone mass) and consequent fractures in Australia during 2012 was estimated to be $AUD 2.75 billion, this being in line with other reported international costs [5]. The escalating burden of these diseases is one of the more critical issues facing healthcare systems worldwide.
Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), have been associated with decreases in bone mineral density (BMD) and an increased risk for falls and fractures in both men and women across the age range [6, 7]. Depression itself has been shown to be a vulnerability factor for osteoporosis, being associated with both low BMD and increased fracture risk [8, 9] as well as falls [10, 11]. Both in vitro and in vivo evidence provides further support to the observational findings in humans and mechanistic possibilities [8].
Fundamentally, bone mass and bone strength are determined by continual bone re/modelling that consists of bone generation by osteoblasts and bone resorption by osteoclasts, with osteocytes controlling the functioning of osteoblasts and osteoclasts within the multicellular unit [12]. A failure to balance bone formation with bone resorption results in net bone loss, with this process influenced by both local and systemic factors. Bone turnover markers are products of the re/modelling process and offer a way to assess this process.
Thus, the aim of this study was to investigate the association between SSRIs and serum markers of bone turnover in a population-based sample of men.
Methods
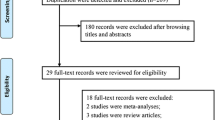
Participants
This study examined data collected from men participating in the Geelong Osteoporosis Study (GOS); a population-based study located in south-eastern Australia. Methodological details of the cohort are published elsewhere [13]. Originally, 1540 men (response 67.0%) were randomly recruited from the electoral rolls for the Barwon Statistical Division between 2001 and 2006. Of 1540 men, participants for whom blood samples were not available were excluded from the analyses, resulting in a final sample of 1138, aged 20–96 year.
Data
Outcome
Blood samples were obtained following an overnight fast and stored at − 80 °C for batch analysis. The serum bone resorption marker, C-telopeptide (CTx) and formation marker, type 1 procollagen amino-terminal-propeptide (PINP) were measured using the automated Roche Modular Analytics E170 analyser [CTx inter-assay coefficient of variation (CV) < 3.8%, detection limit, 10 ng/l: PINP inter-assay CV < 4.9%, detection limit 5 µg/l].
Exposure
Current medication use and duration were ascertained via self-report and categorised according to the Australian index of medications (http://www.mims.com.au/index.php/about-mims/about-mims-overview). Participants were asked to bring in a list of medications or containers to assist with accurate recording of details. Antiresorptive (bisphosphonates and selective oestrogen receptor modulators), calcium and vitamin D supplements, gonadal hormones (hormone replacement therapy), oral glucocorticoids and antidepressant (selective serotonin reuptake inhibitors, serotonin–norepinephrine reuptake inhibitors and tricyclic antidepressants) use were required for these analyses.
Psychiatric history was assessed using the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Non-patient edition (SCID-I/NP) [14]. The SCID-I/NP was used to identify those who had ever experienced a depressive disorder, including major depressive disorder (MDD), minor depression, bipolar disorder, dysthymia, mood disorder due to a general medical condition and substance-induced mood disorder. Participants were classified as having a lifetime history of depression if past or current symptoms met the lifetime and/or current diagnostic criteria for any of the aforementioned DSM-IV depressive disorders. All interviews were conducted by personnel with post-graduate qualifications in psychology, who were trained using live and videotaped interviews under the supervision of a psychiatrist.
Weight and height were measured to the nearest 0.1 kg and 0.1 cm, respectively, and body mass index (BMI) calculated as weight/height2 (kg/m2).
Current cigarette smoking was self-reported. Habitual physical activity level was documented by self-report, with those reporting ‘moves, walks and works energetically; participates in vigorous exercise’ or ‘walks at brisk pace, does normal housework or other work; engages in light exercise’ classified as active; otherwise those reporting ‘little walking outside home, but prepares meals and does very light housework or equivalent’ or ‘sits in chair or lies in bed most of the time, walks independently from bed to chair to toilet but requires assistance for greater movement’ were classified as ‘sedentary’.
Calcium intake and alcohol consumption were estimated from a validated food frequency questionnaire [15].
Areal BMD (g/cm2) was measured at the femoral neck using dual-energy X-ray absorptiometry (Prodigy; GE Lunar, Madison, WI, USA). Trained technicians carried out all examinations and performed daily calibrations of the densitometer with equipment-specific phantoms.
Socio-economic status (SES) was ascertained using Socio-Economic Index for Areas (SEIFA) index scores based on the 2006 Australian Bureau of Statistics Census data. SEIFA values were used to derive an Index of relative socio-economic advantage and disadvantage (IRSAD), which account for high and low income, and type of occupation and was categorised into quintiles according to cut-points for the Barwon Statistical Division [16, 17].
Statistics
Differences in characteristics between the groups were determined using t tests for continuous parametric variables, Kruskal–Wallis for non-parametric continuous variables and for discrete variables, Chi-square tests or Fisher’s exact test when expected cell counts were less than five. Serum CTx and PINP concentrations were square root transformed to normalise the data before statistical analysis. Multiple linear regression was used to determine the association between SSRI use and bone turnover markers (CTx and PINP). Known covariates include age, weight, physical activity, smoking status, alcohol consumption, dietary calcium intake, depression, SES, bone active medications and other antidepressants. These were tested sequentially and only included in the final model if significant. All interactions were tested. Statistical analyses were performed using Minitab (version 16; Minitab, State College, PA).
Results
Thirty-seven (3.3%) men reported using SSRIs. Median duration of current SSRI use was 2.7 years (IQR 1.1–4.6 years).
Age was identified as an effect modifier; stratification was undertaken at 60 years at which the direction of the relationship between SSRI use and both markers of bone turnover changed. Characteristics of the whole group (20–94 year; n = 1138) and for the younger (20–60 year; n = 557) and older (61–94 year; n = 581) men according to SSRI use are shown in Table 1. Among younger men, age, weight and dietary calcium-adjusted CTx and PINP were 12.4% [16.7 (95% CI 14.6–18.8) vs 19.1 (95% CI 18.7–19.4) pg/ml, p = 0.03] and 13.6% [5.6 (95% CI 4.9–6.3) vs 6.4 (95% CI 6.3–6.6) pg/ml, p = 0.02] lower among SSRI users compared to non-users, respectively. Associations between SSRI use and both CTx and PINP remained following further adjustment for known risk factors including physical activity, alcohol, smoking, SES, depression, bone active medications and other antidepressants. Among older men, there were no differences in CTx [19.4 (95% CI 17.4–21.4) vs 17.9 (95% CI 17.5–18.3) pg/ml, p = 0.16] or PINP [6.3 (95% CI 5.6–7.0) vs 6.1 (95% CI 6.0–6.2) pg/ml, p = 0.61] among SSRI users compared to non-users.
Discussion
These epidemiological data showed differences in bone turnover markers associated with SSRI use in a large group of community dwelling adult men. Specifically, the serum bone resorption marker, CTx and formation marker, PINP were lower among SSRI users compared to non-SSRI users aged between 20 and 60 years, independent of sociodemographic characteristics, lifetime history of depression, medication use and other lifestyle factors.
In the first study to investigate the association between bone turnover markers and antidepressant use, treatment with the SSRI, escitalopram, increased serum osteocalcin levels and decreased β-CTX levels in a group of premenopausal women newly diagnosed with MDD (n = 50). The effects were more prominent in patients with a HAM-D score below 15 than above 15 at the end of the 3-month study period, suggesting that improvements in the severity of depression influenced the positive changes in bone turnover markers [18]. In a similar, prospective treatment study, serum levels of β-CTX increased, without compensatory increases in PINP, in a group of men and women aged over 60 years whose depression did not remit after 12 weeks of treatment with venlafaxine [19]. In the only other study to investigate this question, escitalopram did not affect PINP and CTX levels, in a randomised controlled trial conducted over an 8-week period, in a group of 141 healthy peri- and postmenopausal women without MDD [20].
Typically, an imbalance between bone formation and bone resorption results in net bone loss. In this study, a reduced bone turnover state (i.e. both formation and resorption reduced) was evident, with concurrent reductions in hip BMD, albeit non-significant following stratification by age. The precise mechanism by which bone mass is decreased among users of antidepressants is still not clear and likely to be multifactorial. For example, it has been proposed that both peripheral and central serotonin signalling have actions on bone [21]. In support of our findings, we have previously shown in vitro, that some but not all SSRIs, potently and dose-dependently inhibit both osteoclast and osteoblast number and function [22]; a result that would be expected to contribute to a low bone turnover state in vivo.
Bone loss and fragility fracture in several clinical conditions have been characterised by a low bone turnover state [23]. Generally, epidemiological studies have shown SSRI use to be associated with lower BMD, increased fracture risk and bone loss over time [8]. Lifestyle factors, such as physical inactivity, smoking, inadequate dietary intakes and excessive alcohol consumption frequently seen in the presence of depression may play a role, although these factors did not explain the current observations. Increases in cortisol, inflammation and oxidative stress are further mechanisms hypothesised to be implicated. The observed relationship differed for younger and older men. As normal ageing is associated with changes in bone turnover markers, it is possible that any SSRI-related changes among those aged > 60 years may have been masked [24].
Both strengths and weaknesses need to be taken into consideration when interpreting this study. The cross-sectional study design precludes a determination of causality due to no assessment of change in markers of bone turnover over time. Residual, unrecognised and/or confounding by indication is possible and power limitations prevented investigation into duration and dose effects and likely explains the loss of significance in regard to concurrent BMD at the hip once the sample was stratified. Furthermore, although the number of SSRI users reflected the expected prevalence of use in men [25], given the sample size, the current study included a small number of SSRI users, with the number of users further reduced when the group was dichotomized by age. Inflammatory cytokines or other biochemical markers, such as vitamin D and cortisol levels were not assessed at the time of analyses; therefore we are unable to comment whether or not they are contributing to underlying biological mechanisms. Strengths of this study include the use of a gold standard tool in the measurement of depressive disorders, data covering the full adult age range and our ability to take into consideration a host of potential confounders.
In conclusion, our population-based data suggest that SSRI use is associated with dysregulations in bone turnover markers among younger men independent of lifestyle, depression and other recognised confounders. The observed decreases in both CTx and PINP are likely to contribute to a low bone turnover state and increased skeletal fragility with a mismatch between bone formation and resorption resulting in bone loss. This supports previous observations suggesting that SSRI use is associated with low BMD and increased fracture risk. This is yet another piece of evidence to support the need for monitoring bone health in users of SSRIs.
References
Pratt LA, Brody DJ, Gu Q (2011) Antidepressant use in persons aged 12 and over: United States, 2005–2008. NCHS Data Brief 76:1–8
Hendrickx G, Boudin E, Van Hul W (2015) A look behind the scenes: the risk and pathogenesis of primary osteoporosis. Nat Rev Rheumatol 11:462–74
Henry M, Pasco J, Nicholson G, Kotowicz M (2011) Prevalence of osteoporosis in Australian men and women: Geelong Osteoporosis Study. Med J Aust 195:321–322
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Watts JJ, Abimanyi-Ochom J, Sanders KM (2012) Osteoporosis costing all Australians a new burden of disease analysis—2012 to 2022 report. Osteoprosis Australia, Glebe, NSW
Rabenda V, Nicolet D, Beaudart C, Bruyere O, Reginster JY (2013) Relationship between use of antidepressants and risk of fractures: a meta-analysis. Osteoporos Int 24:121–137
Wu Q, Bencaz AF, Hentz JG, Crowell MD (2012) Selective serotonin reuptake inhibitor treatment and risk of fractures: a meta-analysis of cohort and case-control studies. Osteoporos Int 23:365–375
Fernandes BS, Hodge JM, Pasco JA, Berk M, Williams LJ (2016) Effects of depression and serotonergic antidepressants on bone: mechanisms and implications for the treatment of depression. Drugs Aging 33:21–25
Williams LJ, Pasco JA, Jacka FN, Henry MJ, Dodd S, Berk M (2009) Depression and bone metabolism. Rev Psychother Psychosom 78:16–25
Williams LJ, Pasco JA, Stuart AL, Jacka FN, Brennan SL, Dobbins AG, Honkanen RJ, Koivumaa-Honkanen H, Rauma PH, Berk M (2015) Psychiatric disorders, psychotropic medication use and falls among women: an observational study. BMC Psychiatry 15:75
Stuart AL, Pasco JA, Jacka FN, Berk M, Williams LJ (2018) Falls and depression in men: a population-based study. Am J Mens Health 12:14–18
World Health Organisation (2007) Prevention and management of osteoporosis: report of a WHO scientific group. In: World Health Organisation Scientific Group on the prevention and management of osteoporosis, Geneva
Pasco JA, Nicholson GC, Kotowicz MA (2012) Cohort profile: Geelong Osteoporosis Study. Int J Epidemiol 41:1565–1575
First M, Spitzer R, Gibbon M, Williams J (2002) Structured clinical interview for DSM-IV-TR axis I disorders, research version, non-patient edition. (SCID-I/NP). Biometrics Research, New York State Psychiatric Institute, New York
Giles C, Ireland P (1996) Dietary questionnaire for epidemiological studies (version 2). The Cancer Council Victoria, Melbourne
Brennan SL, Henry MJ, Nicholson GC, Kotowicz MA, Pasco JA (2009) Socioeconomic status and risk factors for obesity and metabolic disorders in a population-based sample of adult females. Prev Med 49:165–171
Brennan SL, Henry MJ, Nicholson GC, Kotowicz MA, Pasco JA (2010) Socioeconomic status, obesity and lifestyle in men: the Geelong Osteoporosis Study. J Mens Health 7:31–41
Aydin H, Mutlu N, Akbas NB (2011) Treatment of a major depression episode suppresses markers of bone turnover in premenopausal women. J Psychiatr Res 45:1316–1320
Shea ML, Garfield LD, Teitelbaum S, Civitelli R, Mulsant BH, Reynolds CF 3rd, Dixon D, Dore P, Lenze EJ (2013) Serotonin-norepinephrine reuptake inhibitor therapy in late-life depression is associated with increased marker of bone resorption. Osteoporos Int 24: 1741–1749
Diem SJ, Joffe H, Larson JC, Tsai JN, Guthrie KA, LaCroix AZ, Ensrud KE, Freeman EW, Leder BZ (2014) Effects of escitalopram on markers of bone turnover: a randomized clinical trial. J Clin Endocrinol Metab 99:E1732-7
Ortuno MJ, Robinson ST, Subramanyam P, Paone R, Huang YY, Guo XE, Colecraft HM, Mann JJ, Ducy P (2016) Serotonin-reuptake inhibitors act centrally to cause bone loss in mice by counteracting a local anti-resorptive effect. Nat Med 22:1170–1179
Hodge JM, Wang Y, Berk M, Collier FM, Fernandes TJ, Constable MJ, Pasco JA, Dodd S, Nicholson GC, Kennedy RL, Williams LJ (2013) Selective serotonin reuptake inhibitors inhibit human osteoclast and osteoblast formation and function. Biol Psychiatry 74:32–39
Fratzl-Zelman N, Roschger P, Misof BM, Nawrot-Wawrzyniak K, Potter-Lang S, Muschitz C, Resch H, Klaushofer K, Zwettler E (2011) Fragility fractures in men with idiopathic osteoporosis are associated with undermineralization of the bone matrix without evidence of increased bone turnover. Calcif Tissue Int 88:378–387
Nguyen TV, Meier C, Center JR, Eisman JA, Seibel MJ (2007) Bone turnover in elderly men: relationships to change in bone mineral density. BMC Musculoskelet Disord 8:13
Lockhart P, Guthrie B (2011) Trends in primary care antidepressant prescribing 1995–2007: a longitudinal population database analysis. Br J Gen Pract 61:e565–e572
Acknowledgements
This work was supported by the National Health and Medical Research Council (NHMRC), Australia (Projects 299831, 628582, 1009367, 1026265, 1021345, 1104438). LJW is supported by a NHMRC Career Development Fellowship (1064272). MB is supported by a NHMRC Senior Principal Research Fellowship (1059660). VC and JC are supported by Postgraduate Scholarships from Deakin University. The funding providers played no role in the design or conduct of the study; collection, management, analysis and interpretation of the data; or in preparation, review or approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LJW has received grant/research support from Eli Lilly, Pfizer, The University of Melbourne, Deakin University. MB has received Grant/Research Support from the NIH, Cooperative Research Centre, Simons Autism Foundation, Cancer Council of Victoria, Stanley Medical Research Foundation, MBF, NHMRC, Beyond Blue, Rotary Health, Geelong Medical Research Foundation, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Meat and Livestock Board, Organon, Novartis, Mayne Pharma, Servier and Woolworths, has been a speaker for Astra Zeneca, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Janssen Cilag, Lundbeck, Merck, Pfizer, Sanofi Synthelabo, Servier, Solvay and Wyeth, and served as a consultant to Allergan, Astra Zeneca, Bioadvantex, Bionomics, Collaborative Medicinal Development, Eli Lilly, Glaxo SmithKline, Janssen Cilag, Lundbeck Merck, Pfizer and Servier. JAP has recently received grant/research support from the National Health and Medical Research Council (NHMRC), BUPA Foundation, Amgen/GlaxoSmithKline/Osteoporosis Australia/Australian and New Zealand Bone and Mineral Society, Western Alliance, Barwon Health, Deakin University and the Geelong Community Foundation. JH, MAK, ALS, VC and JC have no disclosures.
Ethical Approval
The Human Research Ethics Committee at Barwon Health approved the study.
Human and Animal Rights and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Williams, L.J., Berk, M., Hodge, J.M. et al. Selective Serotonin Reuptake Inhibitors (SSRIs) and Markers of Bone Turnover in Men. Calcif Tissue Int 103, 125–130 (2018). https://doi.org/10.1007/s00223-018-0398-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-018-0398-0