Abstract
Low bone volume and changes in bone quality or microarchitecture may predispose individuals to fragility fractures. As the dominant component of the human skeleton, cortical bone plays a key role in protecting bones from fracture. However, histological investigations of the underlying structural changes, which might predispose to fracture, have been largely limited to the cancellous bone. The aim of this study was to investigate the age-association and regional differences of histomorphometric properties in the femoral neck cortical bone. Undecalcified histological sections of the femoral neck (n = 20, aged 18–82 years, males) were cut (15 μm) and stained using modified Masson-Goldner stain. Complete femoral neck images were scanned, and cortical bone boundaries were defined using our previously established method. Cortical bone histomorphometry was performed with low (×50) and high magnification (×100). Most parameters related to cortical width (Mean Ct.Wi, Inferior Ct.Wi, Superior Ct.Wi) were negatively associated with age both before and after adjustment for height. The inferior cortex was the thickest (P < 0.001) and the superior cortex was the thinnest (P < 0.008) of all cortical regions. Both osteonal size and pores area were negatively associated with age. Osteonal area and number were higher in the antero-inferior area (P < 0.002) and infero-posterior area (P = 0.002) compared to the postero-superior area. The Haversian canal area was higher in the infero-posterior area compared to the postero-superior area (P = 0.002). Moreover, porosity was higher in the antero-superior area (P < 0.002), supero-anterior area (P < 0.002) and supero-posterior area (P < 0.002) compared to the infero-anterior area. Eroded endocortical perimeter (E.Pm/Ec.Pm) correlated positively with superior cortical width. This study describes the changes in cortical bone during ageing in healthy males. Further studies are needed to investigate whether these changes explain the increased susceptibility to femoral neck fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone loss occurs throughout the skeleton with ageing, and consequently, the risk of fractures increases [1, 2]. In particular, hip fractures not only result in a high level of morbidity and mortality, but also cause a heavy burden to the healthcare system [3, 4]. Skeletal failure occurs when the forces applied to the bone exceed its load-bearing capacity, and the age-dependent bone loss is usually accelerated under the influence of osteoporosis [5, 6].
Histomorphometric analysis has commonly been used to study the changes in bone remodelling and bone structure. It is essential to understand the age-dependent variation in histological properties at the femoral neck since cortical thinning and loss of cancellous bone are both causes of age-related femoral neck fractures [7, 8]. The pioneering work by Jonathan Reeve and colleagues has authenticated the necessity of investigating changes in cortical bone histology in healthy subjects at the femoral neck [9, 10].
Although the cancellous bone is critical for stress transfer and femoral neck stiffness, the cortical bone has been regarded as the major load-bearing compartment by many previous studies [8, 11, 12]. However, it is also likely that the contribution of cortical and cancellous bone can vary greatly with age and even between individuals owing to different bone volume fractions [13–16]. In general, various features of the cortical bone in human femoral neck were assessed in previous studies to either detect structural changes explaining increased hip fracture risk [17, 18] or to investigate the mechanical properties (strength, elasticity, geometry, etc.) by applying visual or acoustic microscopy [19–22].
Histological analysis of the structural bone characteristics attributable to age-related bone loss has mostly been conducted at the iliac crest [23–25], and previous histomorphometric studies in healthy subjects have focused almost exclusively on cancellous bone [26, 27]. The understanding of cortical bone across adulthood and the studies of the underlying morphometric changes that might predispose a person to a fragility fracture of the femoral neck are limited. Furthermore, females with potential postmenopausal osteoporosis have been the subjects of most histomorphometric studies [18, 28–30]. No systematic investigation has been conducted for the histomorphometric properties of the cortical bone at the femoral neck of male subjects with respect to ageing and between femoral neck regions. This study aims to resolve this issue. We hypothesise that the structural changes in cortical bone occur with age. Since the ability of cortical bone to resist fracture deteriorates with ageing, the age-associated changes of the cortical structure may explain the susceptibility for fractures. In the present work, we studied the complete cross section of the male femoral neck using quantitative cortical bone histomorphometry. The variation of histological values with age as well as between anatomical regions was then investigated.
Materials and Methods
Subjects
Femoral neck samples were obtained from 20 cadavers (mean age, 47 ± 18.2 years, range 18–82 years, males) at Kuopio University Hospital, Kuopio, Finland. The subjects were divided into two sub-groups based on age (≤50 years, N = 12 and >50 years, N = 8). There was no previous history of medical conditions or use of drugs known to affect bone metabolism (Table 1).
Sample Preparation
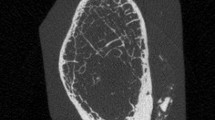
Transverse cross sections were cut from the femoral neck with a band saw. A minor cut was marked on the inferior bone edge to enable the correct orientation of the sample during the measurements. Samples were dehydrated in ethanol for at least 48 h before embedding in polymethylmethacrylate according to standard protocols [31]. After embedding, 15-μm-thick sections were cut using a microtome (Reichert-Jung; Cambridge Instruments, Heidelberg, Germany) and stained with modified Masson-Goldner trichrome stain. The entire cross section of the femoral neck was scanned using an auto-image scanner (Particle Analyzer; Carl Zeiss, Jena, Germany) to acquire a complete histological image (×50) for histomorphometric analysis. An image programme (GNU Image Manipulation Program, version 2.0) was utilised for delineation of different histological boundaries in the images [32].
Bone Histomorphometry
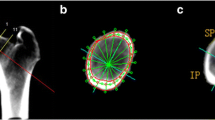
Each histological image (×50) was separated into three independent zones (the absolute cortex area, the endocortical bone area and the cancellous bone area), based on our previous criteria of histological boundary definition (Fig. 1) [32].
The histomorphometric analyses of cortical bone were conducted using Bioquant Osteo II (Bioquant Image Analysis, Nashville, TN, USA). The nomenclature, abbreviations and parameters follow the recommendations by the American Society for Bone and Mineral Research (ASBMR) [33]. First, the samples were analysed with bright light microscopy using a magnification of ×50 in images covering the complete femoral neck (low-magnification measurements). Then, the absolute cortex area was evaluated under bright light and polarisation microscopy using a magnification of ×100 (high-magnification measurements). For this analysis, the absolute cortex area was divided into eight anatomical locations. In each location, at least five fields (1.51 mm2 for each) of view were randomly imaged and measured (Fig. 2).
Cross section of the femoral neck at the cut face showing eight anatomical locations: area 1 infero-anterior; area 2 antero-inferior; area 3 antero-superior; area 4 supero-anterior; area 5 supero-posterior; area 6 postero-superior; area 7 postero-inferior; area 8 infero-posterior. In each location, at least five fields (1.51 mm2 for each) of view were randomly imaged and measured
Based on low-magnification (×50) imaging, the area and width parameters were determined. Cortical bone area [Ct.B.Ar. (mm2)] was measured as the tissue area between the absolute cortex boundary and the periosteum. Endocortical area [Ec.Ar. (mm2)] was measured as the tissue area between the absolute cortex boundary and the endocortical boundary. Cancellous bone area [Cn.B.Ar. (mm2)] was measured as the inner tissue area outside the endocortical boundary. The parameters of cortical bone area per tissue area [Ct.B.Ar./T.Ar. (%)], endocortical area per tissue area [Ec.Ar./T.Ar. (%)] and cancellous bone area per tissue area [Cn.B.Ar./T.Ar. (%)] were also determined. Mean cortical width [mean Ct.Wi. (mm)] was calculated as the average value of all (average 315 measurements/sample) perpendicular widths between the absolute cortex boundary and the periosteum. Similarly, the regional cortical widths at four different anatomic regions were measured, i.e. anterior cortical width [anterior Ct.Wi. (mm)], posterior cortical width [posterior Ct.Wi. (mm)], inferior cortical width [inferior Ct.Wi. (mm)] and superior cortical width [superior Ct.Wi. (mm)]. Besides, the periosteal perimeter [Ps.Pm. (mm)] and endocortical perimeter [Ec.Pm. (mm)] were further measured.
Based on high-magnification (×100) imaging, the bone tissue area was quantified per octant. The percentage of osteonal area per sampled cortical area was calculated: [On.Ar./Sa.Ct.Ar. (%)]. The mean osteonal perimeter [On.Pm. (μm)] was determined as an average of all (average 30 osteons/octant) measured osteons. Similarly, the Haversian canal perimeter [H.Pm. (μm)] was determined as the average value of all (average 30 Haversian canals/octant) measured Haversian canals. The Haversian canal area [H.Ar. (mm2)] was determined as the sum of all (average 30 Haversian canals/octant) measured Haversian canals. The osteon number [N.On (#)], the minimum osteonal diameter [min.On.Dm. (μm)] and the maximum osteonal diameter [max.On.Dm. (μm)] were also determined. The mean wall width [W.Wi. (μm)] of osteons was calculated using all (average 12 measurements/osteon) perpendicular distances between the Haversian canal boundary and the outer edge of the circular osteon. Moreover, pore area [Po.Ar. (mm2)] was determined as the sum of all (average 15 pores/octant) measured pores, and the porosity was calculated as follows: [Po.Ar/Sa.Ct.Ar. (%)]. The pore number [N.Po (#)] was also determined. Osteoid surfaces were recognised as unmineralised seams along the absolute cortex boundary, and the bone turnover of the endocortical surface was identified by calculating osteoid perimeter per endocortical perimeter [O.Pm./Ec.Pm. (%)]. Likewise, erosion surfaces were recognised (with or without osteoclasts) along the absolute cortex boundary by calculating erosion perimeter per endocortical perimeter [E.Pm./Ec.Pm. (%)].
Statistical Analysis
Shapiro–Wilkinson tests were used to determine whether the data were normally distributed. An independent T test was used to compare low-magnification parameters between the age groups. In addition, analysis of covariance (general linear model) was used to adjust for height. The Mann–Whitney U test was used to compare different age groups of high-magnification parameters since the data of two groups were not normally distributed. In other cases of the non-normally distributed variables, the Kruskal–Wallis test followed by multiple comparison analysis using the Mann–Whitney U test was performed to evaluate the differences of cortical width in four anatomical regions of the femoral neck and examine the areal differences of high-magnification parameters between octants. The Bonferroni correction was applied in both cases.
Spearman’s correlation was conducted to investigate the possible relationships between endocortical parameters (O.Pm/Ec.Pm, E.Pm/Ec.Pm) and low-magnification parameters. All analyses were performed using SPSS Statistical software (version 20.0; SPSS, Chicago, IL, USA). P values <0.05 were considered to be statistically significant.
Results
Low-Magnification Cortical Bone Parameters
Most cortical width-related parameters (mean cortical width, inferior cortical width and superior cortical width) were negatively associated with age (P < 0.05) (Table 2). Similarly, the values of cortical bone area per tissue area were found to be negatively associated with age (P < 0.01) (Fig. 3). In contrast, the parameters of cancellous bone area and periosteal perimeter exhibited an age-related increase (P < 0.05). No age-association was found on either the cortical width of the anterior (anterior cortical width, P = 0.907) and posterior region (posterior cortical width, P = 0.056), or other bone area-related parameters (cortical bone area, P = 0.096; endocortical area, P = 0.306; endocortical area/tissue area, P = 0.81; cancellous bone area/tissue area, P = 0.093) (Table 2).
Scatter plots for associations between the values of low-magnification parameters with age. The inferior, superior cortical width and values of cortical bone area were negatively associated with age (P < 0.05). Although the anterior and posterior cortical width also exhibited decrescent tendency, the variations were not statistically significant. In contrast, the periosteal perimeter was found to increase with ageing (P < 0.05). Ant. Ct.Wi anterior cortical width, Post. Ct.Wi posterior cortical width, Inf. Ct.Wi inferior cortical width, Sup. Ct.Wi superior cortical width, Ct.B.Ar/T.Ar cortical bone area/tissue area, Ps.Pm periosteal perimeter
After adjustment for height, the statistically significant age-association in cortical width-related parameters (mean cortical width, inferior cortical width and superior cortical width) still remained. Similarly, the values of cortical bone area (P = 0.018) and cortical bone area per tissue area (P = 0.003) were found to be significantly associated with age.
There was a significant variation in cortical width in four different anatomical regions (P < 0.001). The inferior cortex was the thickest (P < 0.001) and the superior cortex was the thinnest of all cortical regions (P < 0.008). There was no significant difference between the width of the anterior and posterior cortex (P = 0.29) (Fig. 4).
Mean cortical width (SD) in four regions of the femoral neck (n = 20). The inferior cortex was the thickest (P < 0.001) and the superior cortex was the thinnest of all cortical regions (P < 0.008). There was no significant difference between the width of the anterior and posterior cortex (P = 0.29). * P ≤ 0.008
High-Magnification Cortical Bone Parameters
The osteonal structure-related parameters (osteonal area and Haversian canal area) were negatively associated with age (P < 0.05) (Fig. 5). There was also a negative association between pore-related parameters (pore area and porosity) and age (P < 0.01). There were no significant differences in other high-magnification cortical bone parameters (Table 3).
The age-associated loss in osteonal system is exemplified by two cross-sectional samples A (29 years) and B (82 years) (×5). The magnified images show the osteonal structures under polarised light (×100). Osteons undergoing normal remodelling (1) were more frequent in young sample (a), than in older sample (b). Osteons with excessive deep resorption and adjacent merging (2) were found more in older sample (b) than in younger sample (a)
When comparing the eight anatomical areas, there was significant variation in the parameters of osteonal area (P < 0.01), osteonal number (P < 0.01), Haversian canal area (P < 0.05) and porosity (P < 0.01). For other high-magnification parameters, no significant areal differences were found (Table 4).
Specifically, osteonal area was higher in the antero-inferior area compared to the postero-superior area (P < 0.001), as well as higher in the infero-posterior area compared to the postero-superior area (P < 0.002). Similarly, osteonal number was also higher in the antero-inferior area (P < 0.002) and the infero-posterior area (P = 0.002) compared to the postero-superior area. Haversian canal area was higher in the infero-posterior area compared to the postero-superior area (P = 0.002). Moreover, porosity was higher in the antero-superior area (P < 0.002), supero-anterior area (P < 0.002) and supero-posterior area (P < 0.002) compared to the infero-anterior area (Fig. 6).
Significant variation of high-magnification parameters between eight anatomical areas. Osteonal area and osteonal number were higher in the antero-inferior area and infero-posterior area compared to the postero-superior area. The Haversian canal area was higher in the infero-posterior area compared to the postero-superior area. Porosity was higher in the antero-superior area, supero-anterior area and supero-posterior area compared to the infero-anterior area. *P ≤ 0.002. N. On osteon number, On.Ar/Sa.Ct.Ar osteonal area/cortical area, H.Ar Haversian canal area
Correlations
The erosion perimeter per endocortical perimeter was positively associated with superior cortical width (P < 0.01). The osteoid perimeter per endocortical perimeter did not correlate with any of the low-magnification cortical parameters.
Discussion
This study provides histological analyses of cortical bone structure at the femoral neck from previously healthy male cadavers. We demonstrated that the changes in cortical bone structure are both age- and anatomical region-associated.
In the study subjects, the height correlated with age (P = 0.01) while the weight did not (P = 0.213). Therefore, low-magnification parameters were adjusted for height when these parameters were compared between the age groups.
The cortical thickness was negatively associated with age both before and after height adjustment. It has been suggested that the age-related bone loss at the hip occurs through a series of structural changes in bone. These changes tend to preserve bone structure in mechanically loaded regions (e.g. the postero-superior and antero-inferior regions of the femoral neck cortex [34]), whereas less mechanically loaded regions (e.g. the superior cortex of the femoral neck) are attenuated with age [35]. According to this theory, we found no significant age-associated loss of cortical thickness in the anterior and posterior cortex either before or after adjustment for height. However, recent studies indicate that hip fractures involve a complicated set of structural deficits. Besides rarely loaded structures, regions that are relatively protected from age-related bone loss (e.g. the inferior cortex of the femoral neck [36]) may also be somehow involved [37]. Therefore, thinning of the inferior cortex of the femoral neck with age in our study was expected. The negative age-associated decreases in mean cortical width observed in this study are consistent with the data reported by others, both at the femoral neck and at other skeletal sites [23, 25].
Based on our histological criteria [32], we divided the cross section of the femoral neck into three zones to separate cortical bone, endocortical bone area and cancellous bone [38]. The absolute cortical bone area was negatively associated with age within the whole tissue area of the cross section, whereas cancellous bone showed positive age-association. This finding is consistent with previous histological studies [39–41]. Interestingly, no age-associated change was detected in the endocortical bone area, either before or after adjustment for height. Although cortical thinning with age might be associated with the conversion of compact to cancellous bone arising from disordered Haversian remodelling [42, 43], losses of cortical and cancellous bones on different time axes have been found [34, 44]. Furthermore, both endocortical perimeter and periosteal perimeters were positively associated with age, although the significances of these trends were lost after adjustment for height. It has been suggested that the generalised bone loss (e.g. endocortical resorption) could be compensated for by the periosteal apposition to some extent. Thus, the hip strength and its resistance to fracture could be maintained [45, 46]. Some studies have suggested that the periosteum of the femoral neck is disrupted by the attachment of the capsule of the hip joint, and that periosteal bone apposition does not occur at the femoral neck [47, 48]. Other studies, however, have shown that bone formation occurs on the outer periosteal surface of the femoral neck [49, 50]. We still cannot draw the conclusion that the femoral neck expands with ageing.
In this cohort, the inferior cortex was the thickest and the superior cortex was the thinnest. Similar findings have been shown before [51, 52]. The superior cortex has been shown to get thinner three times faster with age than the inferior cortex [53]. The structural changes of cortical bone at the femoral neck are both age-associated and anatomical region-dependent.
Femoral osteonal morphology depends on the remodelling balance achieved within individual remodelling units. Structural changes of osteonal and Haversian canal area may thus result from different resorption depths as well as osteonal combination [54, 55]. We observed negative age-associated changes in osteonal and Haversian canal area. In contrast, the osteonal diameter showed no significant age-association. Although one study found similar changes at the iliac crest [24], some other studies have suggested that osteonal dimensions could never be systematically affected by age and sex [56]. The lack of agreement in osteonal changes with ageing may reflect the differences in methodology, sample size as well as various definitions of parameters and cortical boundaries. In our study, the osteons with excessively enlarged Haversian canals (>82 μm) due to the adjacent merging were excluded, because previous studies have suggested that the enlargement and clustering of the osteonal system may predict the formation of cortical pores [57, 58]. As a result, the age-associated loss in osteonal system suggested by the present study was reasonably explained. Moreover, we also showed that the changes of osteons undergoing normal remodelling (without excessive deep resorption [59] ) were negatively associated with age. In addition, the excessive resorption is more likely to lead to osteon merging and the formation of “giant” canals [60], the prevalence of which has a negative influence on the ability of the cortical shell to withstand stresses associated with a fall [61]. Therefore, the age-associated loss in normal osteons may potentially increase the age-associated fragility at the femoral neck.
The pore area and porosity were negatively associated with age. This seems contradictory to the previous studies but the definitions of the cortical bone boundaries have varied [62–64]. Based on our histological criteria, the “absolute cortex” consisted of pure cortical bone tissue only, and was defined mainly based on the size of composite canals and their distance to an additional “guide” boundary [ 32]. As a result, many endocortical canals were excluded, while some previous studies might have included them. On the other hand, age-associated cortical expansion may lead to super-osteon formation, which is supported by the fact that the periosteal region has the highest density of clustered osteons [10]. Therefore, the formation of cortical pores predicted by the enlargement and clustering of the osteonal system [57, 58] may primarily occur in the periosteal cortex. These periosteal pores would predominantly compose the cortical porosity according to our criteria. This was confirmed by our finding that number of pores tends to be positively associated with age, although the differences were not significant. However, this positive age-associated change is restricted to the periosteal cortex, which is not enough to be responsible for the increase in porosity, because the pore area in the endocortical bone has been found to be much greater than in the periosteal cortex [63].
Therefore, the exclusion of partially trabecularised cortical bone with larger pores would lead to the decreased porosity in present study. Based on our criteria, the trabecularised cortical bone with larger pores had been predominantly included into the endocortical bone area. The transitional zone between cortical and cancellous bone has been very rarely defined as the endocortical bone area by previous studies, which may be explained by the fact that increased trabecularisation of the cortical bone complicates the identification of endocortical features [65, 66]. Thus, in our study, the positive age-associated changes in porosity and pore area might be the key characteristics of the endocortical bone. This was also consistent with our other finding that the endocortical bone area tends to be positively associated with age, although the changes were not significant.
The regional comparisons of the femoral neck cross section revealed some differences. Osteonal area and osteonal number were higher in the antero-inferior area and infero-posterior area compared to the postero-superior area. The Haversian canal area was higher in the infero-posterior area compared to the postero-superior area. As described previously, the inferior cortex was much thicker than the superior cortex. Therefore, the regional differences of osteonal structure could be explained with cortical thinning. Since the thinner cortex offers less volume in which remodelling may occur, the probability of including relatively intact osteons is correspondingly reduced as well. As a result, the values of osteonal structure-related parameters were higher in the inferior-adjacent regions. On the other hand, our result also suggested that the porosity was higher in the antero-superior area, supero-anterior area and supero-posterior area compared to the infero-anterior area. This is consistent with previous findings that, at the femoral neck, the superior cortex is more porous than the inferior cortex [64, 67]. In accordance with the results of Yeni and Norman [68], we did not find any differences in porosity between the inferior and posterior cortex at the femoral neck. However, our results showed a porosity increase in the anterior cortex projecting to the superior region at the normal femoral neck, which may help to explain the specific porosity difference between the anterior and inferior cortex in the findings by Malo et al. [31]. Moreover, the cortical loss was found primarily along the infero-anterior to supero-posterior axis in cases with femoral neck fracture [61, 69]. Our results suggested a significant cortical porosity difference along exactly the same axis; therefore, this may reveal the underlying morphometric changes that might predispose to fragility fracture of the femoral neck.
The positive association between the superior cortical width and erosion surface could be explained by the loss of cortical bone through the trabecularisation of the endocortical region [44]. As mentioned previously, cortical thinning shortens the volume in which remodelling may occur, which may reduce the probability of detecting a resorption space as well.
Our study has some limitations. The number of samples is relatively small, especially for studying age-related changes. Thus, the statistical power to show significant changes may have been inadequate for some parameters. The secular changes in cortical dimensions and architecture cannot be excluded, as this was a cross-sectional study. Moreover, this study only takes male subjects into account. Since many previous studies have examined the effect of ageing on cortical bone in the hip with a cross-sectional study design in women [35, 41, 44], and women have cortical thinning with ageing that is two times faster than in men [53], we do not know whether similar changes of histological property will be observed in female subjects.
In conclusion, we found thinning of the superior cortex of the femoral neck with age in healthy males. Investigations of the underlying structural changes that might predispose to fracture have been largely limited to computed tomography-based approaches, as well as to the skeletal sites that do not fracture, such as the iliac crest. Studies on femoral neck biopsies from healthy subjects are rare. Therefore, our study provides useful insight into the histological changes at femoral neck with age. These changes may explain the underlying mechanisms that give rise to an osteoporotic femoral fracture. Further studies to confirm these findings are needed. Moreover, since most previous studies have applied various definitions both for parameters and bone boundaries, our method could be used to obtain data that are more comparable between studies.
References
Zebaze RM, Ghasem-Zadeh A, Bohte A et al (2010) Intracortical remodelling and porosity in the distal radius and postmortem femurs of women: a cross-sectional study. Lancet 375:1729–1736
Rantalainen T, Nikander R, Heinonen A, Daly RM, Sievanen H (2011) An open source approach for regional cortical bone mineral density analysis. J Musculoskelet Neuronal Interact 11:243–248
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence an economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22(3):465–475
Barrett-Connor E (1995) The economic and human costs of osteoporotic fracture. Am J Med 98(Suppl 2A):3S–8S
Burghardt AJ, Kazakia GJ, Ramachandran S, Link TM, Majumdar S (2010) Age- and gender-related differences in the geometric properties and biomechanical significance of intracortical porosity in the distal radius and tibia. J Bone Miner Res 25:983–993
Kaptoge S, Beck TJ, Reeve J et al (2008) Prediction of Incident hip fracture risk by femur geometry variables measured by hip structural analysis in the study of osteoporotic fractures. J Bone Miner Res 23:1892–1904
Chen H, Zhou X, Fujita H, Onozuka M, Kubo KY (2013) Age-related changes in trabecular and cortical bone microstructure. Int J Endocrinol 2013:213–234
Manske SL, Liu-Ambrose T, Cooper DM et al (2009) Cortical and trabecular bone in the femoral neck both contribute to proximal femur failure load prediction. Osteoporos Int 20:445–453
Jordan GR, Loveridge N, Bell KL, Power J, Rushton N, Reeve J (2000) Spatial clustering of remodeling osteons in the femoral neck cortex: a cause of weakness in hip fracture? Bone 26:305–313
Bell KL, Loveridge N, Reeve J et al (2001) Super-osteons (remodeling clusters) in the cortex of the femoral shaft: influence of age and gender. Anat Rec 264:378–386
Koivumäki JE, Thevenot J, Pulkkinen P et al (2012) Cortical bone finite element models in the estimation of experimentally measured failure loads in the proximal femur. Bone 51:737–740
Jee WSS (2001) Integrated bone tissue physiology: anatomy and physiology. Cowin SC, editor. CRC Press, New York
Bousson V, Le Bras A, Roqueplan F et al (2006) Volumetric quantitative computed tomography of the proximal femur: relationships linking geometric and densitometric variables to bone strength. Role for compact bone. Osteoporos Int. 17:855–864
Turner CH (2005) The biomechanics of hip fracture. Lancet 366:98
Bouxsein ML, Fajardo RJ (2005) Cortical stability of the femoral neck and hip fracture risk. Lancet 366:1523–1524
Lotz JC, Cheal EJ, Hayes WC (1995) Stress distributions within the proximal femur during gait and falls: implications for osteoporotic fracture. Osteoporos Int 5:252–261
Bousson V, Peyrin F, Bergot C et al (2004) Cortical bone in the human femoral neck: three-dimensional appearance and porosity using synchrotron radiation. J Bone Miner Res 19:794–801
Blain H, Chavassieux P, Portero-Muzy N et al (2008) Cortical and trabecular bone distribution in the femoral neck in osteoporosis and osteoarthritis. Bone 43:862–868
Rho JY, Kuhn-Spearing L, Zioupos P (1998) Mechanical properties and the hierarchical structure of bone. Med Eng Phys 20:92–102
Koivumäki JE, Thevenot J, Pulkkinen P et al (2012) Ct-based finite element models can be used to estimate experimentally measured failure loads in the proximal femur. Bone 50:824–829
Raum K (2011) Bone quantitative ultrasound. Springer Dordrecht Heidelberg, London
Rho JY, Zioupos P, Currey JD, Pharr GM (2002) Microstructural elasticity and regional heterogeneity in human femoral bone of various ages examined by nanoindentation. J Biomech 35:189–198
Melsen F, Melsen B, Mosekilde L et al (1978) Histomorphometric analysis of normal bone from the iliac crest. Acta Pathol Microbiol Scand. 86:70–81
Vedi S, Kaptoge S, Compston JE (2011) Age-related changes in iliac crest cortical width and porosity: a histomorphometric study. J Anat 218:510–516
Brockstedt H, Kassem M, Eriksen EF et al (1993) Age- and sex-related changes in iliac cortical bone mass and remodeling. Bone 14:681–691
Cohen-Solal M, Shih M-S, Lundy M, Parfitt A (1991) A new method for measuring cancellous bone erosion depth: application to the cellular mechanisms of bone loss in postmenopausal osteoporosis. J Bone Miner Res 6:1331–1338
Tsangari H, Findlay DM, Fazzalari NL (2007) Structural and remodeling indices in the cancellous bone of the proximal femur across adulthood. Bone 40:211–217
Ma YL, Zeng QQ, Chiang AY et al (2014) Effects of teriparatide on cortical histomorphometric variables in postmenopausal women with or without prior alendronate treatment. Bone 59:139–147
Ottewell PD, Wang N, Brown HK et al (2014) Zoledronic acid has differential antitumor activity in the pre- and postmenopausal bone microenvironment in vivo. Clin Cancer Res 20:2922–2932
Bobinac D, Marinovic M, Bazdulj E et al (2013) Microstructural alterations of femoral head articular cartilage and subchondral bone in osteoarthritis and osteoporosis. Osteoarthr Cartil 21:1724–1730
Malo MK, Rohrbach D, Isaksson H et al (2013) Longitudinal elastic properties and porosity of cortical bone tissue vary with age in human proximal femur. Bone 53(2):451–458
Tong XY, Malo M, Tamminen IS et al (2015) Development of new criteria for cortical bone histomorphometry in femoral neck: intra- and inter-observer reproducibility. J Bone Miner Metab 33(1):109–118
Dempster DW, Compston JE, Drezner MK et al (2013) Standardized nomenclature, symbols, and units for bone histomorphometry: a 2012 update of the report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res 28(1):2–17
Thomas CD, Mayhew PM, Power J et al (2009) Femoral neck trabecular bone: loss with aging and role in preventing fracture. J Bone Miner Res 24:1808–1818
Poole KE, Mayhew PM, Rose CM et al (2010) Changing structure of the femoral neck across the adult female lifespan. J Bone Miner Res 25:482–491
Mayhew PM, Thomas CD, Clement JG et al (2005) Relation between age, femoral neck cortical stability, and hip fracture risk. Lancet 366:129–135
Johannesdottir F, Poole KE, Reeve J et al (2011) Distribution of Cortical bone in the femoral neck and hip fracture: a prospective case-control analysis of 143 incident hip fractures; the Ages-Reykjavik study. Bone 48:1268–1276
Zebaze R, Ghasem-Zadeh A, Mbala A, Seeman E (2013) A new method of segmentation of compact-appearing, transitional and trabecular compartments and quantification of cortical porosity from high resolution peripheral quantitative computed tomographic images. Bone 54:8–20
Evans FG (1976) Mechanical properties and histology of cortical bone from younger and older men. Anat Rec 185:1–12
Zagba-Mongalma G, Goret-Nicaise M, Diana A (1988) Age changes in human bone: a microradiographic and histological study of subperiosteal and periosteal calcifications. Gerontology 34:265–276
Riggs BL, Melton LJ, Robb RA et al (2004) Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res 19:1945–1954
Power J, Loveridge N, Lyon A et al (2003) Bone remodeling at the endocortical surface of the human femoral neck: a mechanism for regional cortical thinning in cases of hip fracture. J Bone Miner Res 18:1775–1780
Power J, Doube M, van Bezooijen RL, Loveridge N, Reeve J (2012) Osteocyte recruitment declines as the osteon fills in: interacting effects of osteocytic sclerostin and previous hip fracture on the size of cortical canals in the femoral neck. Bone 50:1107–1114
Nicks KM, Amin S, Melton LJ 3rd et al (2013) Three-dimensional structural analysis of the proximal femur in an age stratified sample of women. Bone 55:179–188
Szulc P, Seeman E, Duboeuf F, Sornay-Rendu E, Delmas PD (2006) Bone fragility: failure of periosteal apposition to compensate for increased endocortical resorption in postmenopausal women. J Bone Miner Res 21:1856–1863
Szulc P, Delmas PD (2007) Bone loss in elderly men: increased endosteal bone loss and stable periosteal apposition. The prospective minos study. Osteoporos Int. 18:495–503
Cullinane DM, Einhorn TA (2002) Principles of bone biology. In: Bilezikian JP, Raisz LG, Rodan GA (eds) Biomechanics of bone. Academic Press, San Diego
Holzer G, von Skrbensky G, Holzer LA, Pichl W (2009) Hip fractures and the contribution of cortical versus trabecular bone to femoral neck strength. J Bone Miner Res 24:468–474
Kaptoge S, Dalzell N, Loveridge N et al (2003) Effects of gender, anthropometric variables, and aging on the evolution of hip strength in men and women aged over 65. Bone 32:561–570
Carpenter RD, Sigurdsson S, Zhao S et al (2011) Effects of age and sex on the strength and cortical thickness of the femoral neck. Bone 48:741–747
Backman S (1957) The proximal end of the femur: investigations with special reference to the etiology of femoral neck fractures; anatomical studies; roentgen projections; theoretical stress calculations; experimental production of fractures. Acta Radiol 146(Suppl):1–166
Hammer A (2010) The structure of the femoral neck: a physical dissection with emphasis on the internal trabecular system. Ann Anat. 192:168–177
Johannesdottir F, Aspelund T, Reeve J et al (2013) Similarities and differences between sexes in regional loss of cortical and trabecular bone in the mid-femoral neck: the AGES-Reykjavik longitudinal study. J Bone Miner Res 28:2165–2176
Dong XN, Guo XE (2000) Is the cement line a weak interface? Proceedings of the 46th Annual Meeting of the Orthopaedic Research Society, Orlando, FL
Dong XN, Guo XE (2001) Extracting intrinsic debonding strength of cement lines from osteon pushout experiments. In: Proceedings of the 47th Annual Meeting of the Orthopaedic Research Society, San Francisco
Pfeiffer S, Crowder C, Harrington L, Brown M (2006) Secondary osteon and haversian canal dimensions as behavioral indicators. Am J Phys Anthropol 131:460–468
Busse B, Hahn M, Schinke T et al (2010) Reorganization of the femoral cortex due to age-, sex-, and endoprosthetic-related effects emphasized by osteonal dimensions and remodeling. J Biomed Mater Res A. 92:1440–1451
Bell KL, Loveridge N, Jordan GR et al (2000) A novel mechanism for induction of increased cortical porosity in cases of intracapsular hip fracture. Bone 27:297–304
Mori S, Burr DB (1993) Increased intracortical remodeling after fatigue damage. Bone 14:103–109
Jordan G, Loveridge N, Power J, Bell KL, Reeve J (1998) Clustering of cortical remodelling: a mechanism for generating focal weakness in hip fracture. American Society for Bone and Mineral Research and International Bone and Mineral Society (ASBMR-IBMS) second joint meeting
Bell KL, Loveridge N, Power J et al (1999) Regional differences in cortical porosity in the fractured femoral neck. Bone 24:57–64
Cooper DM, Thomas CD, Clement JG et al (2007) Age-dependent change in the 3D structure of cortical porosity at the human femoral midshaft. Bone 40:957–965
Schnitzler CM, Mesquita JM (2013) Cortical porosity in children is determined by age-dependent osteonal morphology. Bone 55:476–486
Chappard C, Bensalah S, Olivier C et al (2013) 3D characterization of pores in the cortical bone of human femur in the elderly at different locations as determined by synchrotron micro-computed tomography images. Osteoporos Int 24:1023–1033
Martin RB, Pickett JC, Zinaich S (1980) Studies of skeletal remodeling in aging men. Clin Orthop 149:268–282
Thomas CD, Feik SA, Clement JG (2006) Increase in pore area, and not pore density, is the main determinant in the development of porosity in human cortical bone. J Anat 209:219–230
Rohde K, Rohrbach D, Gluer CC et al (2014) Influence of porosity, pore size, and cortical thickness on the propagation of ultrasonic waves guided through the femoral neck cortex: a simulation study. IEEE Trans Ultrason Ferroelectr Freq Control 61:302–313
Yeni YN, Norman TL (2000) Fracture toughness of human femoral neck: effect of microstructure, composition, and age. Bone 26:499–504
Bell KL, Loveridge N, Power J et al (1999) Structure of the femoral neck in hip fracture: cortical bone loss in the inferoanterior to superoposterior axis. J Bone Miner Res 14:111–119
Acknowledgments
The authors would like to acknowledge Ms. Ritva Sormunen and Mr. Arto Koistinen for their assistance in sample preparation. We would also like to acknowledge the financial support from the China Scholarship Council (CSC), Sigrid Juselius Foundation and the Strategic Funding of the University of Eastern Finland.
Conflict of interest
Dr. Tong Xiaoyu, Dr. Inari Burton, Dr. Hanna Isaksson, Dr. Jukka Jurvelin and Dr. Heikki Kröger have no conflict of interest.
Human and Animal Rights and Informed Consent
Our research was performed with prior informed consent from each participant or their near relatives. Ethical approval for collection of samples was granted by the National Authority for Medicolegal Affairs (Permission Number: 5783/04/044/07).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tong, X., Burton, I.S., Isaksson, H. et al. Cortical Bone Histomorphometry in Male Femoral Neck: The Investigation of Age-Association and Regional Differences. Calcif Tissue Int 96, 295–306 (2015). https://doi.org/10.1007/s00223-015-9957-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-015-9957-9