Abstract
The objective of this study is to examine the effect of milk powder supplementation with different calcium contents on bone mineral density (BMD) in postmenopausal Chinese women, and to determine a more appropriate dose of calcium supplementation. A 2-year, randomized controlled double-blind trial. Postmenopausal women (n = 210) aged 50–65 years were recruited and assigned randomly into three calcium supplementation groups. All participants received milk powder supplementation with different calcium contents (300, 600, and 900 mg per day for groups A, B, and C, respectively) and all groups received 800 IU of vitamin D per day. During the follow-up period, BMD of the left hip and lumbar spine (as the main indicator) was measured using dual-energy X-ray absorptiometry at the baseline, 1 and 2 years. Both three BMD measures and the changes of BMD over 2 years were used to analyze. Before adjusting for covariates, BMD in group A of the lumbar spine and groups A and B of greater trochanter decreased significantly from the baseline over time but increased significantly in the rest groups of the lumbar spine and greater trochanter and in three groups of Ward’s triangle. There were significant differences across the three groups for changes of BMD in the greater trochanter and Ward’s triangle. When adjusting for covariates, there were significant decreases with time in group A of the spine (P = 0.001), groups A and B of greater trochanter (P = 0.0002 and P = 0.04, respectively) and increases in groups B and C of Ward’s triangle (P = 0.03 and P = 0.004, respectively). BMD change in the greater trochanter was significantly different among three groups. For healthy postmenopausal women, high calcium milk powder supplementation was better in retarding bone loss than medium and low calcium in the greater trochanter. Considering the dietary calcium intake of postmenopausal women in north of China, a dose of 900 mg/day is considered as the most appropriate calcium supplementation for greater trochanter but not for other sites.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone mineral density (BMD) decreases at a rate of 0.7–1.0 % after middle age, and in postmenopausal women, this is three times greater compared with premenopausal women [1–3]. It has been shown that bone loss can be reduced by as much as 1.0 % each year through the use of calcium supplementation in postmenopausal women. Over many years, many randomized controlled trials have confirmed that both calcium supplementation alone and calcium with vitamin D supplementation can reduce bone loss and the incidence of osteoporosis and osteoporotic fracture in postmenopausal women [1, 4–12]. However, the most appropriate and significant dose of calcium supplementation is contentious in different countries. One study reported that 800 mg/day of calcium supplementation can retard bone loss in postmenopausal women with a low calcium diet in China [6]. However, with developments in our society and the improvement of living standards, the dietary calcium intake of people is increasing. Considering the side-effects of calcium supplementation, including kidney stones, constipation, and eventually increased risk of cardiovascular events [8, 13–18], identifying a more appropriate dose of calcium supplementation is necessary. In this study, a randomized controlled trial was designed to explore the effect of milk powder supplementation with different calcium contents on BMD in postmenopausal Chinese women.
Methods
Subjects
Hongqi Community Health Center (Harbin City, China) was randomly selected as the target community from all teaching community hospitals of Harbin Medical University. From this community, 276 volunteers were randomly recruited and those who met the inclusion criteria were entered into the study. Inclusion criteria comprised postmenopausal women aged between 50 and 65 years at the time of the study that had lived in Harbin for at least 5 years. Subjects were excluded if they: (i) had disorders of calcium metabolism or calcium absorption; (ii) had bone disorders; (iii) had gastrointestinal disease, coronary heart disease, stroke, diabetes, cancer, thyroid or parathyroid disease, chronic liver disease or chronic kidney disease; (iv) suffered from ovarian surgery, premenopausal hysterectomy, gastric resection, and thyroidectomy; (v) used estrogen at the time of the study or had taken drugs for a month or more; (vi) were milk powder intolerant; (vii) were likely to migrate. Based on these criteria, a total of 210 women were enrolled in the study.
Randomization and Treatments
In accordance with baseline BMD of the lumbar spine, participants were randomly assigned to three treatment groups (groups A, B and C) by block randomization. All participants were instructed to take 50 g of high calcium, low fat milk powder with boiled water every morning and evening, respectively. Each 50 g of milk powder contained 400 IU of vitamin D plus 150, 300 or 450 mg of calcium for groups A, B and C, respectively. Milk powder was produced by Nestle Corporation, Beijing, China. Based on the common ingredients of milk powder, according to the calcium content designed prior to the study, corresponding calcium carbonate was added to the milk powder to reach the intervention level.
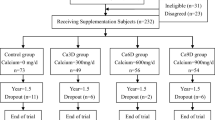
During the experiment, the investigators were fully blinded to the group allocation until the end of the study. The study flow is summarized in Fig. 1.
Follow-Up and Compliance
Participants were followed-up for 2 years with data collection at baseline, 1 and 2 years, including food intake frequency, BMD, blood specimens of morning fast and 24 h urine sample. At baseline, subjects were interviewed about their demographic and socioeconomic background, food intake frequency, past medical history, reproductive and menstrual history, past physical activity level, calcium tablets and vitamin D supplementation, and mentality and reply. Data on food intake frequency were collected using the Food Frequency Questionnaire (FFQ), which was designed in case report form [7]. The validity and reliability of this questionnaire were tested.
In the first and second year, identical data were collected, except for past medical history and reproductive and menstrual history. Participants were face-to-face interviewed by trained investigators using a structured and validated questionnaire. Each subject recalled their diet over the past year with the help of estimating portion size through detailed pictorial information. Dietary nutrient intake was estimated using 3-day food records, including details on energy, protein, calcium, vitamin, and other microelements.
Throughout the study, subjects were instructed to record their milk powder intake every day. Records and empty pouches were returned every two and half months, and then the next batch of milk powder was provided. According to the records and returned pouches, the compliance of each subject was determined.
Outcome Measurements
BMD measurements were carried out by dual-energy X-ray absorptiometry (DXA; Norland Corp, USA) in the Harbin Orthopedics Hospital at the baseline, 1 and 2 years. Measurements were taken at the following sites: the left hip (femoral neck, greater trochanter, and Ward’s triangle) and the lumbar spine (L2–L4). The primary outcomes included T score, Z score, BMD, and bone mineral content (BMC).
Serum ions, such as calcium, phosphate and magnesium, biochemical indices, such as trioxypurine, albumin, total cholesterol, triglyceride, alkaline phosphatase and creatinine, and urinary ions, such as calcium, magnesium, sodium, potassium, and chlorine, were measured by standard laboratory methods in the second hospital affiliated to Harbin Medical University.
Statistical Analysis
A power analysis was undertaken before the study so that a change of 5 % in BMD over 2 years could be detected with 85 % power, provided that 50 subjects were included in each study group. Data were reported as mean ± standard deviation (SD) for continuous variables and frequency (%) for categorical variables. Differences in baseline characteristics between the three groups were compared using analysis of variance (ANOVA) for continuous normal and equal variance variables, the χ 2 test for categorical variables and the Kruskal–Wallis test for non-normal variables or ordinal variables. Fisher’s exact test was used when numbers were too small for the χ 2 test. Repeated measures analysis of variance was employed to compare the differences between the baseline and the first and second year in BMD. Differences in BMD changes between the three groups were compared by analysis of co-variance (ANCOVA) with the baseline BMD, years since menopause and calcium tablet use as the covariates. Bonferroni was used where multiple comparisons were made. All tests were two-tailed. A 5 % level was used as the level of significance. All analyses were conducted using SAS v9.2 software (SAS Institute, Cary, NC).
Results
Dropout Rate
During the first year, 36 of 210 participants dropped out of the study, therefore 174 subjects (59, 63, and 52 for groups A, B and C, respectively) yielded a total dropout rate of 17.1 %. Of the women dropping out, subjects withdrew due to disease (5), death (2), relocation (6), and personal reasons (23). During the second year, 47 subjects dropped out with a dropout rate of 22.4 %. Dropout was attributable to illness in (8), death (2), relocation (7), and personal reasons (30).
Baseline Characteristics
The baseline characteristics of the study subjects are shown in Table 1. Mean age of the subjects was 56.4 ± 3.8 years, body mass index (BMI) was 24.7 ± 2.8 kg/m2, dietary calcium intake was 573.8 ± 227.8 mg/day (from 3-day food records), and years since menopause was 6.9 ± 4.2 years. Dietary calcium intake was only from daily food, not including calcium supplementation from milk powder and calcium tablet use. Participants in the three randomization groups were well-matched with respect to age, anthropometric measurements, physical activity level, and daily dietary calcium intake. With respect to the other characteristics, there were no significant differences between the three groups, except for calcium tablet use and years since menopause.
BMD of the lumbar spine and hip at baseline, 1 and 2 years are shown in Table 2. Baseline BMD for all sites was well-balanced across the groups.
Bone Mineral Density Changes
Before adjusting for covariates, for the lumbar spine, BMD of groups B and C increased significantly at the first year and decreased thereafter. There was no significant difference between the baseline and the second year and no bone loss was observed. BMD in group A kept unchanged in the first year and then decreased significantly in the second year. For the femoral neck, BMD of the three groups remained stable. For the greater trochanter, BMD in groups A and B kept unchanged in the first year and decreased significantly in the second year, but group C increased significantly in the first year, although it was tiny, and then decreased to the level of the baseline. For the Ward’s triangle, BMD in the three groups increased significantly with time both in the first and second years (Table 2). When adjusting for the baseline BMD, years since menopause and calcium tablet use, there were significant decreases with time in group A of the spine (P = 0.001), groups A and B of greater trochanter (P = 0.0002 and P = 0.04, respectively) and increases in groups B and C of Ward’s triangle (P = 0.03 and P = 0.004, respectively).
Table 3 shows the results of analysis of covariance for the changes of BMD, where baseline BMD, years since menopause and calcium tablet use were covariates. Before adjusting for covariates, there were significant differences between the three groups for changes of BMD in the greater trochanter and Ward’s triangle. However, when adjusting for covariates, only the change of BMD in the greater trochanter was significant.
Discussion
Because of the difference from western countries in dietary patterns, the traditional Asian diet is very low in calcium content [6]. This study was designed to examine whether milk powder supplementation with different calcium contents over 2 years was effective in retarding bone loss in healthy postmenopausal women in China. This study confirmed high calcium milk powder supplementation to be beneficial for the prevention of bone loss in older women, which is consistent with a number of previous reports [5–7, 19]. In this study, significant differences from the baseline over time were found for BMD at all sites, except femoral neck. Although there were no significant differences between the baseline and the first and second year in femoral neck, no bone loss was observed. BMD in group A of the lumbar spine retained constant in the first year and then decreased significantly in the second year as well as BMD in groups A and B of greater trochanter. The bone loss observed in the second year might be relative with the low-dose calcium supplementation.
However, when adjusting for baseline BMD, years since menopause and calcium tablet use, the significant difference for change of BMD in the Ward’s triangle was eliminated. This could be related to the short-term follow-up time, small differences in calcium supplementation dose between the three groups, or poor compliance with the regimen. A previous study [20] showed that adherence to treatment affected the results of calcium supplementation, especially when adherence was bad. In this study, years since menopause and calcium tablet use were significantly different between the three groups, which could confound the effect of calcium supplementation. Although they have been adjusted for, the confounding effect might be not completely eliminated.
To explore the optimal dose of calcium supplementation, only three doses of calcium supplementation were designed. Although significant differences were found in the greater trochanter and Ward’s triangle between the three groups, currently, 900 mg/day was temporarily considered as the more appropriate dose. In the future, more doses groups should be designed to find the more specific and appropriate dose of calcium supplementation.
In conclusion, supplementing 300 mg/day of calcium cannot reduce bone loss in the lumbar spine and greater trochanter, but 600 and 900 mg/day can do. For the greater trochanter, supplementing 900 mg/day of calcium was better than 600 and 300 mg/day in reducing bone loss. Considering the dietary calcium intake of postmenopausal women in the north of China, a calcium supplementation dose 900 mg/day is currently considered as the most appropriate for greater trochanter but not for other sites. If women are able to remain compliant with the regimen and continue to supplement calcium for a long time, a more specific optimal dose of calcium supplementation could be identified.
Author’s Contribution
Meina Liu and Qiuju Zhang designed the study and prepared the first draft of the paper. They are guarantor. Yongjie Chen, Qiao Zhang, Xianfu Ma, and Ning Li contributed to the experimental work. Yaming Xiao and Biao Xie were responsible for statistical analysis of the data. All authors agree to be accountable for the work and to ensure that any questions relating to the accuracy and integrity of the paper are investigated and properly resolved.
References
Ho SC, Chen YM, Woo JL, Lam SS (2004) High habitual calcium intake attenuates bone loss in early postmenopausal Chinese women: an 18-month follow-up study. J Clin Endocrinol Metab 89(5):2166–2170. doi:10.1210/jc.2003-031338
Nordin BE (2009) The effect of calcium supplementation on bone loss in 32 controlled trials in postmenopausal women. Osteoporos Int 20(12):2135–2143. doi:10.1007/s00198-009-0926-x
Shea B, Wells G, Cranney A, Zytaruk N, Robinson V et al (2006) WITHDRAWN: calcium supplementation on bone loss in postmenopausal women. Cochrane Database Syst Rev 1:CD004526. doi:10.1002/14651858.CD004526.pub3
Cooper L, Clifton-Bligh PB, Nery ML, Figtree G, Twigg S et al (2003) Vitamin D supplementation and bone mineral density in early postmenopausal women. Am J Clin Nutr 77(5):1324–1329
Storm D, Eslin R, Porter ES, Musgrave K, Vereault D et al (1998) Calcium supplementation prevents seasonal bone loss and changes in biochemical markers of bone turnover in elderly New England women: a randomized placebo-controlled trial. J Clin Endocrinol Metab 83(11):3817–3825. doi:10.1210/jcem.83.11.5289
Lau E, Woo J, Lam V, Hong A (2001) Milk supplementation of the diet of postmenopausal Chinese women on a low calcium intake retards bone loss. J Bone Miner Res 16(9):1704–1709
Chee W, Suriah A, Chan S, Zaitun Y, Chan Y (2003) The effect of milk supplementation on bone mineral density in postmenopausal Chinese women in Malaysia. Osteoporos Int 14(10):828–834
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J et al (2006) Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 354(7):669–683. doi:10.1056/NEJMoa055218
Spangler M, Phillips BB, Ross MB, Moores KG (2011) Calcium supplementation in postmenopausal women to reduce the risk of osteoporotic fractures. Am J Health Syst Pharm 68(4):309–318
Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A (2007) Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet 370(9588):657–666. doi:10.1016/S0140-6736(07)61342-7
Prince RL, Devine A, Dhaliwal SS, Dick IM (2006) Effects of calcium supplementation on clinical fracture and bone structure: results of a 5-year, double-blind, placebo-controlled trial in elderly women. Arch Intern Med 166(8):869–875. doi:10.1001/archinte.166.8.869
Spangler M, Phillips BB, Ross MB, Moores KG (2011) Calcium supplementation in postmenopausal women to reduce the risk of osteoporotic fractures. Am J Health Syst Pharm 68(4):309–318. doi:10.2146/ajhp070175
Li S, Na L, Li Y, Gong L, Yuan F et al (2013) Long-term calcium supplementation may have adverse effects on serum cholesterol and carotid intima-media thickness in postmenopausal women: a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr 98(5):1353–1359. doi:10.3945/ajcn.113.062844
Zittermann A, Pilz S, Borgermann J, Gummert JF (2011) Calcium supplementation and vitamin D: a trigger for adverse cardiovascular events? Future Cardiol 7(6):725–727. doi:10.2217/fca.11.65
Bolland MJ, Barber PA, Doughty RN, Mason B, Horne A et al (2008) Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial. BMJ 336(7638):262–266. doi:10.1136/bmj.39440.525752.BE
Pentti K, Tuppurainen MT, Honkanen R, Sandini L, Kroger H et al (2009) Use of calcium supplements and the risk of coronary heart disease in 52-62-year-old women: the Kuopio Osteoporosis Risk Factor and Prevention Study. Maturitas 63(1):73–78. doi:10.1016/j.maturitas.2009.03.006
Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR (2011) Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ 342:d2040. doi:10.1136/bmj.d2040
Bolland MJ, Avenell A, Baron JA, Grey A, MacLennan GS et al (2010) Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ 341:c3691. doi:10.1136/bmj.c3691
Prince R, Devine A, Dick I, Criddle A, Kerr D et al (1995) The effects of calcium supplementation (milk powder or tablets) and exercise on bone density in postmenopausal women. J Bone Miner Res 10(7):1068–1075. doi:10.1002/jbmr.5650100711
Reid IR, Mason B, Horne A, Ames R, Reid HE et al (2006) Randomized controlled trial of calcium in healthy older women. Am J Med 119(9):777–785. doi:10.1016/j.amjmed.2006.02.038
Acknowledgments
This work was supported by the National Natural Science Foundation of China [81273183].
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
Yongjie Chen, Yaming Xiao, Biao Xie, Qiao Zhang, Xianfu Ma, Ning Li, Meina Liu, and Qiuju Zhang declare that they have no conflict of interest.
Ethical approval
All procedures performed in study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Meina Liu and Qiuju Zhang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Chen, Y., Xiao, Y., Xie, B. et al. Effect of Milk Powder Supplementation with Different Calcium Contents on Bone Mineral Density of Postmenopausal Women in Northern China: A Randomized Controlled Double-Blind Trial. Calcif Tissue Int 98, 60–66 (2016). https://doi.org/10.1007/s00223-015-0065-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-015-0065-7