Abstract
In this study, we report the epidemiology and risk factors for humeral fractures (proximal humerus and shaft) among men and women residing in south-eastern Australia. Incident fractures during 2006 and 2007 were identified using X-ray reports (Geelong Osteoporosis Study Fracture Grid). Risk factors were identified using data from case–control studies conducted as part of the Geelong Osteoporosis Study. Median age of fracture was lower in males than females for proximal humerus (33.0 vs 71.2 years), but not for humeral shaft (8.9 vs 8.5 years). For females, proximal humerus fractures occurred mainly in the 70–79 and 80+ years age groups, whereas humeral shaft fractures followed a U-shaped pattern. Males showed a U-shaped pattern for both proximal humerus and humeral shaft fractures. Overall age-standardised incidence rates for proximal humerus fractures in males and females were 40.6 (95 % CI 32.7, 48.5) and 73.2 (95 % CI 62.2, 84.1) per 100,000 person years, respectively. For humeral shaft fractures, the age-standardised rate was 69.3 (95 % CI 59.0, 79.6) for males and 61.5 (95 % CI 51.9, 71.0) for females. There was an increase in risk of proximal humerus fractures in men with a lower femoral neck BMD, younger age, prior fracture and higher milk consumption. In pre-menopausal women, increased height and falls were both risk factors for proximal humerus fractures. For post-menopausal women, risk factors associated with proximal humerus fractures included a lower non-milk dairy consumption and sustaining a prior fracture. Humeral shaft fractures in both sexes were sustained mainly in childhood, while proximal humerus fractures were sustained in older adulthood. The overall age-standardised rates of proximal humerus fractures were nearly twice as high in females compared to males, whereas the incidence rates of humeral shaft fractures were similar.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humerus fractures are the third most common type of fracture in the elderly (over 65 years), after the femoral neck and radius [1–4]. In contrast, fractures of the distal humerus are rare, making up 1–2 % of all adult fractures and approximately 5–10 % of all osteoporotic fractures in those aged over 60 years [5–8]. Both of these types of fractures can be osteoporotic in nature, and since populations in many countries are ageing, these fractures are occurring with increasing frequency in some areas [1, 5, 9]. However, there are some studies which show that proximal humerus fracture incidence is not increasing and has in fact, stabilised [10, 11]. The estimated lifetime risk for an osteoporotic humeral fracture is 12.9 % for women and 4.1 % for men [11]. The cost of these fractures is high; the total cost of osteoporosis and osteopenia (moderate bone loss) in Australians over 50 years of age during 2012 was $2.75 billion [12].
Fractures of the proximal or distal humerus are associated with considerable morbidity, particularly in the elderly [5, 11]. Daily activities are affected which can have a large impact on quality of life for up to 18 months post-fracture [13]. In addition, the loss of quality of life after humerus fracture is close to that for hip fracture [13]. Most proximal humerus fractures are managed conservatively (immobilisation), with good outcomes for approximately 80 % of patients with non-displaced fractures [2, 3, 9]. However, in more recent years, the number of proximal humerus fractures treated using internal fixation has increased [14]. Displaced fractures, however, can require hospitalisation, with a lengthy stay that can lead to long-term functional deficits [2, 3]. The average length of hospital stay for displaced proximal humerus fractures is 24 days, second only to hip fracture [2]. Distal humerus fractures, however, have more significant challenges including expensive treatment, since surgery is almost always required, long follow-up time and rehabilitation [5, 6]. After the fracture event, both proximal and distal humerus fractures are followed by increased risks of falling, sustaining a hip fracture and mortality [3, 6].
Some risk factors for proximal humeral fractures have been reported, including low bone mass, height loss since age 25 years, personal history of fractures, maternal history of hip fracture, low level of physical activity, low BMI, history of falls, poor vision, insulin-dependent diabetes, alcohol consumption, poor health, poor neuromuscular function and low physical activity level, but not all have been confirmed by multiple studies.
Both proximal and humeral shaft fractures have not been extensively studied because they were considered uncommon [2, 11]. Due to considerable morbidity and increased risks of mortality, it is important to determine which individuals may be likely to sustain a humerus fracture and to prioritise fracture prevention or post-fracture treatment [3]. Therefore, in this study, we investigated, the incidence of humeral fractures at both the proximal humerus and the humeral shaft, of which the latter have not been extensively studied. We also reported the cause of these fractures as well as identifying independent risk factors, to ultimately help prevent fractures of the humerus and prevent the associated morbidity and mortality.
Methods
Participants 1: GOSFracGrid
The first dataset used in this analysis was the Geelong Osteoporosis Study Fracture Grid (GOSFracGrid), which documents all fractures occurring in the Barwon Statistical Division (BSD, located in south-eastern Australia) through examination of radiology reports from the imaging centres in the region [15]. For this sample, the population at risk was the entire population of the BSD, of all ages. This area is appropriate for epidemiological studies because it has a large population (~260,000) and is representative of the Australian population [16]. The GOSFracGrid was used to investigate age, left- and right-side proportions and incidence rates in males and females with humerus fractures during the years 2006 and 2007.
Fracture Ascertainment 1: GOSFracGrid
All fractures with the International Statistical Classification of Diseases and Related Health Problems, 9th version (ICD-9) Code of 812 (humerus) [17] were included. Fractures of the proximal humerus or humeral shaft were identified separately by closer examination of the X-ray reports. Fractures that occurred at the distal end of the humerus were not included in this study. Individuals with fractures who lived outside of the BSD region were excluded. This method of fracture ascertainment has been previously validated [15].
For fractures identified between 2006 and 2007, X-ray reports with the wording “suspicious of” or “possible” fracture were excluded unless a subsequent X-ray report was available confirming the fracture. The median age and inter-quartile range (IQR) of individuals with humerus (proximal humerus and humeral shaft) fractures were determined.
Incidence Rate Calculations
Fracture incidence rates (using data from the GOSFracGrid) were age standardised to the Australian population using data from the Australian Bureau of Statistics 2006 Census Community Profile Series (catalogue number 2001.0) [18]. “Fracture incidence rates” were expressed as fractures per 100,000 persons per year. The 95 % CIs were calculated using population data from the Barwon Statistical Division [18].
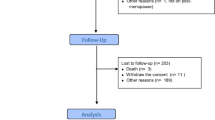
Participants 2: GOS Case–Control Study
A second dataset, the Geelong Osteoporosis Study Fracture Cohort [19], was used for a separate analysis of fracture details and risk factors for fracture. Controls for this analysis were collected from the participants at baseline from the Geelong Osteoporosis Study [16], which was run in parallel to the Fracture Cohort data collection. Male participants were recruited between 2005 and 2008. There were no risk factor data collected for females during this time; however, we have data for females recruited between 1994 and 1996. The female cohort includes only participants aged 35 years or over but the male cohort covers the entire adult age range (≥20 years). Both controls and individuals with fractures during this time period were invited to participate in a series of questionnaires and clinical assessments. The questionnaires included information about details of the fracture event, treatments and lifestyle factors. In this cohort, there were 33 humerus fractures in men with 23 occurring at the proximal humerus, nine at the humeral shaft and one involving both the proximal humerus and shaft. There were 48 humerus fractures in women with 37 occurring at the proximal humerus, nine occurring at the humeral shaft and two occurring at both the proximal humerus and shaft. There were 1537 controls for men and 1172 controls for women.
Questionnaire Data 2: GOS Case–Control Study
Participants from the Fracture Cohort provided details of the fracture event including information about whether the fracture was a result of a fall, the height from which the fall occurred, whether the participant was stationary, walking, running or skiing/riding/skating at the time of fall, whether the fall occurred inside or outside, the cause of the fall and how the participant landed when they fell. Some patients reported multiple different treatments given for their humerus fracture.
In addition to information about the fracture event and treatment, lifestyle and individual factors were collected from participants of the Fracture Cohort, as well as the controls. This included age, weight (kg), height (cm) and BMD at the femoral neck, ultradistal forearm, midforearm and lateral spine (lateral view of the lumbar and mid-to-lower thoracic vertebrae). Ultradistal forearm BMD was also used for women because it was found to be a more sensitive measure of bone fragility. The BMD measurements were performed using dual-energy X-ray absorptiometry (DXA; Lunar DPX-L; Lunar, Madison, WI). Quality assurance tests are carried out every day, and phantom scans are also completed three times per week. Education level was divided into three groups: did not finish high school, finished high school and post-secondary qualification. Prior fracture for women was classified as those which occurred age 45 years or over (fragility fracture). For men, prior fracture was counted at all ages (any prior fracture). Fractures resulting from motor vehicle accidents were excluded. Smoking was classified as “yes” or “no” where “yes” indicated that the person either currently smoked, or smoked in the past. A response of “no” indicated that a person had never smoked. Alcohol consumption was divided into “low” and “high” where high consumption was “several times per week” or more. Milk consumption was divided into “low” and “high”, where “high” was 250 mL (1 cup) or more per day. Non-milk dairy consumption included all cheese and/or yoghurt consumption. Consumption was considered “higher” if the individual consumed at least one serve of either cheese or yoghurt per day. Mobility was defined as “low” or “high”, where “high” included an active lifestyle including light exercise or more several times per week. Falls were classified differently for men and women due to differences in fall frequency between the sexes [20]. In women, falls were classified as “low” or “high”, where “high” included “a few times” or more over a period of 12 months. For men, one or more falls over 12 months was considered “high” falls risk. The current use of a walking aid, oral glucocorticoid use, diabetes status and decreased vision were all classified as “yes” or “no”.
Statistical Analysis: Risk Factors for Humerus Fractures
Descriptive statistics were calculated for the potential risk factors as described above, except BMD, which was converted into a T score for these analyses. Values were reported as median (IQR) or N (%). The Mann–Whitney test was used to determine differences for continuous data between the control and fracture groups. A Chi-Square test or Fisher’s test was used for categorical variables. Binary logistic regression was performed to determine which factors were independent predictors for humerus fracture in men and women separately. Predictors were considered significant if the p value was <0.05. In women, an interaction between age and falls/education was identified. Therefore, the analysis was conducted with two separate datasets: pre-menopausal and post-menopausal women.
Results
During 2006 and 2007, there were 283 humerus fractures in males and of these, 105 were fractures of the proximal humerus and 178 of the humeral shaft (Table 1). Of the 385 females who sustained humerus fractures, 218 were proximal humerus fractures. Four females sustained multiple humeral fractures at different events. No pathological or spontaneous fractures were observed. Males and females differed in the proportion of proximal humerus fractures: 37.1 and 56.6 %, respectively, of all humeral fractures (p < 0.001).
All Humerus Fractures
The median age for humerus fractures (proximal humerus and shaft combined) was lower in males compared to females, 14.5 (IQR 6.8–43.2) years versus 61.8 (IQR 9.7–79.5) years, (p < 0.001). For males, 59 % of humerus fractures occurred on the left side and 40.6 % on the right. One male sustained a bilateral fracture (0.4 %). For females, 53.3 % occurred on the left side and 46.2 % on the right. Two females sustained bilateral fractures (0.5 %). There was no difference in left- and right-side proportions between males and females (p = 0.14).
Proximal Humerus Fractures
The median age differed between the sexes: for males, it was 33.0 (IQR 17.3–63.1) years, and for females, 71.2 (IQR 58.4–82.0) years (p < 0.001). For males, 56.2 % of fractures occurred on the left and 42.9 % on the right side; one male had bilateral fractures in the same event. In females, 52.3 % occurred on the left side, and 47.2 % occurred on the right. The left and right proportions for proximal humerus fractures did not differ between males and females (p < 0.51).
Humeral Shaft Fractures
Median age for humeral shaft fractures between males and females was not different: 8.9 (IQR 5.6–16.4) years versus 8.5 (IQR 5.9–59.6) years (p = 0.09). When comparing the median age for humeral shaft with proximal humerus fractures, the differences were significant for both sexes (p < 0.001). For males, 60.7 % occurred on the left and 39.3 % on the right. In females, 55.2 % occurred on the left side and 44.8 % on the right. The left and right proportions of humeral shaft fractures were not different between males and females (p = 0.30).
Incidence Rates
All Humerus Fractures
Incidence rates derived from the GOSFracGrid for proximal humerus, humeral shaft and total humeral fractures by decade for males are shown in Fig. 1, and, for females, in Fig. 2. The pattern of humerus fracture incidence for males followed a U-shaped pattern. The largest peak was in children, with an incidence rate of 317.5 (95 % CI 257.6, 377.4). Another peak occurred in the 80+ year age group, with an incidence rate of 194.7 (95 % CI 102.1, 287.2). Females had a peak of incidence in childhood (311.4, 95 % CI 250.0, 372.7) and another large peak in the 80+ year age group (621.7, 95 % CI 493.9, 749.4). Across all age groups, humerus fracture incidence per 100,000 person years (standardised to the Australian population) was similar in males (109.9, 95 % CI 96.9, 122.9) and females (135.3, 95 % CI 120.7, 149.8), and for both sexes, it was 123.1 (95 % CI 113.3, 132.8).
Proximal Humerus Fractures
For proximal humerus fractures, there was a small peak in incidence during adolescence for males (age 10–19 years), with an incidence rate of 58.5 per 100,000 persons per year (95 % CI 34.1, 83.0). The incidence rates for all other age groups were below 50 per 100,000 persons per year, except for the oldest age groups, 70–79 and 80+ years, with incidence rates of 71.5 (95 % CI 31.1, 112.0) and 114.5 (95 % CI 43.5, 185.5), respectively. Females showed an increase in proximal humerus fracture incidence across the age groups and the highest incidence occurred in the oldest age group (80 + years), with an incidence rate of 464.5 (95 % CI 354.1, 575.0). Overall incidence rates (standardised to the Australian population) for proximal humerus fractures in males and females were 40.6 (95 % CI 32.7, 48.5) and 73.2 (95 % CI 62.2, 84.1) per 100,000 person years, respectively. The total incidence (standardised to the Australian population) for both sexes was 57.4 (95 % CI 50.1, 64.2).
Humeral Shaft Fractures
The pattern of humeral shaft fracture incidence for males was different to that observed for proximal humerus fractures. There was a peak in childhood, which had an incidence rate of 294.0 (95 % CI 236.3, 351.6). Incidence was lower in an older age group (40–49 years): 2.7 (95 % CI, 0.0, 8.1); however, it was greater again in the oldest age group (80+ years): 80.2 (95 % CI, 20.8, 139.6). The pattern of incidence in females had a peak in childhood (0–9 years), with an incidence rate 298.8 (95 % CI, 238.7, 358.9), which is similar to that observed for males in this age group. There was another peak in the oldest age group (80+ years) with an incidence rate of 150.3 (95 % CI 87.5, 213.1). The rate (standardised to the Australian population) in males and females was similar: 69.3 (95 % CI 59.0, 79.6) for males and 61.5 (95 % CI 51.9, 71.0) for females. The total incidence for both sexes was 65.4 (95 % CI 58.4, 72.4) for humeral shaft fractures.
Cause and Treatment of Fracture
All Humerus Fractures
Additional information about cause of fracture for both men and women was obtained from the Fracture Cohort dataset (Table 2). For all humeral fractures, 84.8 % of men and 89.6 % of women stated that their fracture was the result of a fall. Most fractures in women occurred after a fall from standing height while walking (61.9 %). There was no difference in the location of the fall between sexes; both reported falling outside the home (78.6 % in men and 60.6 % in women) more than inside the home. The cause of fall was similar in men and women, with the most common causes being uneven surface (15.8 % men, 20.0 % women), slippery surface (15.8 % men, 12.7 % women) and loss of balance (13.2 % men, 10.9 % women). Men and women landed from their fall in different ways; men mainly fell onto their face/stomach (20.4 %) or shoulder (30.6 %) whereas women fell onto either an outstretched hand/arm or on a shoulder (25.6 and 33.3 %, respectively). Overall, men were hospitalised for humerus fracture more than women (69.7 vs 22.9 %, p < 0.001). Men appeared to spend a shorter time in the hospital before discharge [median 4 days (IQR 2–13) versus 9 days (IQR 3–21)], but this difference did not reach significance. There was no age-sex influence on hospitalisations or surgical duration of hospital stay.
Proximal Humerus Fractures
For proximal humerus fractures, a large majority of both sexes (87.5 % of men and 92.3 % of women) stated that their fracture was the result of a fall. A large proportion of women (68.6 %) stated that they fell from a standing height while walking. There was also a difference in the location of the fall; most men reported falling outside the home (76.2 %) while women reported falling inside and outside in relatively even proportions (56.6 % outside). The cause of fall was similar in men and women, with the most common causes being uneven surface (13.3 % men, 20.8 % women), slippery surface (16.7 % men, 10.4 % women) and loss of balance (13.3 % men, 12.5 % women). Men and women landed from their fall in similar ways: either on an outstretched hand/arm (12.9 % in men, 25.0 % in women) or on a shoulder (45.2 % in men, 34.4 % in women). Men with proximal humerus fractures were hospitalised more often than women (65.2 vs 21.6 %, p < 0.001).
Humeral Shaft Fractures
For humeral shaft fractures, 80.0 % of men and 77.8 % of women stated that their fracture was the result of a fall. There was no difference in the location of the fall between sexes: both reported falling outside the home (75.0 %) more than inside the home (25.0 %). The cause of fall was similar between the sexes, with the most common cause in men being an uneven surface (22.2 %), followed by a slippery surface, loss of balance and momentary distraction (all 11.1 %). In women, the most common cause was a slippery surface (28.6 %), followed by uneven surface and an obstacle (both 14.3 %). Men and women landed from their fall in different ways; men mainly fell onto their face/stomach (52.6 %) while women fell onto either an outstretched hand/arm or on a shoulder (both 28.6 %). Men were hospitalised more often than women (77.8 vs 33.3 %, p = 0.034), but numbers for this analysis were small, so this result should be interpreted with caution.
Risk Factors for Humeral Fracture
All Humerus Fractures
Descriptive risk factors were determined from Fracture Cohort data and are shown in Table 3 for men and Table 4 for women. Overall, men with any humerus fracture (compared to controls) had lower femoral neck BMD (p = 0.041), more prior fractures (p < 0.001) and higher milk consumption (p = 0.002). Women had a lower ultradistal forearm BMD (p = 0.004), higher age (p = 0.044), more prior fractures (p < 0.001), more falls (p = 0.014) and fewer individuals reporting decreased vision (p = 0.039).
Odds ratios from the logistic regression analysis are shown in Table 5. In men, those with humerus fracture had lower femoral neck BMD T score (OR 0.65; 95 % CI 0.43, 0.98), more prior fractures (OR 6.60; 95 % CI 2.66, 16.34) and higher milk consumption (OR 2.84, 95 % CI 1.38, 5.83) compared to controls. Only 13.1 % of all participants had both a prior fracture and high milk consumption. In pre-menopausal women, two risk factors were identified: height (in cm) (1.13; 95 % CI 1.01, 1.28) and falls (OR 6.89; 95 % CI 1.50, 31.52). In post-menopausal women, those with humerus fracture were more likely to have “finished high school” (OR 2.97; 95 % CI 1.33, 6.66), had lower ultradistal forearm BMD 0.67 (95 % CI 0.46, 0.97), higher weight (OR 1.03; 95 % CI 1.00, 1.05), more prior fractures (>45 years) (OR 9.37; 95 % CI 3.20, 27.46), a higher consumption of non-milk dairy products (OR 0.37; 95 %CI 0.16, 0.86) and reported decreased vision more frequently (OR 0.36; 95 % CI 0.18, 0.75).
Proximal Humerus Fractures
Men with a fracture of the proximal humerus (compared to controls) had lower femoral neck BMD (p = 0.016), more prior fractures (p < 0.001) and higher milk consumption (p = 0.003). Women with proximal humerus fracture had more prior fractures (p < 0.001) and more falls (0.018).
An analysis of risk factors for proximal humerus fracture showed similar results to risk factors identified for all humerus fractures in both sexes. In men, lower femoral neck BMD, prior fracture and higher milk consumption were risk factors. In addition, proximal humerus fractures in men occurred less frequently with increasing age (OR 0.97, 95 % CI 0.95, 1.00). For pre-menopausal women, both increased height and falls were risk factors for proximal humerus fractures. In post-menopausal women, prior fracture (>45 years), a lower consumption of non-milk dairy products and those who finished high school had an increased risk of humerus fracture.
Humeral Shaft Fractures
Men with humeral shaft fractures (compared to controls) had more prior fractures (p = 0.039) and consumed more alcohol (p = 0.044). Women only showed a lower ultradistal forearm BMD (p = 0.025). There were insufficient humeral shaft fractures for both sexes to perform logistic regressions (N = 9 for men and women each).
Discussion
This study reports on the epidemiology and risk factors associated with humerus fractures over a two-year-time period in males and females living in south-eastern Australia. For all humerus fractures, the median age for males was lower than in females. This was true for proximal humerus fractures but not for humeral shaft fractures. The pattern of incidence for both proximal humerus and humeral shaft fractures was similar in males and females. We also reported on the cause of fracture which was mainly the result of a fall (>75 %) in both males and females. Men were hospitalised more often than women for humeral fractures. Finally, we reported risk factors for adult humeral fractures (total humerus and proximal humerus), showing that risk factors were varied and different between men and women.
The previously published literature reports that proximal humerus fractures are mainly sustained by women, generally with low BMD [1, 3, 5, 8, 9]. We observed a similar pattern in our study. By far, the most common cause of humerus fracture is a fall, generally from standing height [1, 8, 9]. Our data are in agreement with this; we also report that the most common mechanism of fracture is a fall from standing height, onto an outstretched hand/arm or shoulder. Additionally, men tended to sustain proximal humerus fractures outside the home, whereas women sustained fractures both inside and outside the home. Humeral shaft fractures, however, were more similar; both men and women reported fracturing mainly outside the home.
A study by Roux et al. [4] examined proximal humerus fractures in males and females (aged 16–97 years) admitted to a hospital in Nice, France from November 2009 to November 2010. There were 325 patients during this time period, and 69 % were female. The left- and right-side proportions of proximal humerus fractures were approximately equal. A simple fall was the cause of fracture in 82 % of females and 55 % of males. These results are similar to the values we have reported.
Several studies have reported humeral fracture incidence, usually in elderly individuals, or for the proximal humerus separately. In France [3], the incidences for men and women aged 40 years and over were 477 and 163 per 1,000,000, respectively for proximal fractures treated in hospital during 2009. These lower incidences may be attributable to only ascertaining hospital admission/separation reports, which can miss some fractures. An Austrian study used hospital discharge records to determine 2008 incidence of proximal humerus fractures in men and women aged 50 years and over, of 141 and 383 per 100,000 men and women, respectively [11]. Equivalent rates from our study were 43.9 for men and 190.4 for women. The rates are considerably higher than our Australian rates despite our ascertainment not being restricted to only those patients admitted to hospital.
Previous work describing humerus fractures in the same region (BSD) during 1994/1996 reported that the incidence rate standardised to the Australian population (adults aged 35 years and over) for humerus fractures in women was 10 per 10,000 per year (95 % CI 9, 12), and for men, it was 3 per 10,000 per year (95 % CI 2, 4) [19]. In this study, we determined incidence rates for all ages, but for adults aged 30 years and over, the humerus fracture incidence in 2006/2007 was 13.9 per 10,000 per year (95 % CI 12.1, 15.8) in women and 5.9 per 10,000 per year in men (95 % CI 4.6, 7.1). The increase in humerus fracture incidence for women follows the projected rise as estimated in Sanders et al. (1999) of approximately 25 % from 1994/1996 to 2006/2007 [21]. This work also calculated that in men, the projected incidence rate was lower than in women; reaching only ~3.8 per 10,000 by 2006. This study showed that the incidence for men almost doubled between 1994/1996 and 2006/2007, which is a greater increase than projected. This may be because research has focussed on post-menopausal women with osteoporosis for the prevention of fractures, and thus, there are not as many effective therapies and guidelines for men.
A study by Palvanen et al. [22] examined the mechanisms of injury in Finnish patients aged 50 years or over with fractures resulting from low energy trauma of the upper extremity (proximal humerus, elbow and wrist). They showed that there were distinct mechanisms of fracture for each of the different sites and that the injuries occurred mainly as a result of a fall with impact at the site of fracture. The study also showed that 97 % of proximal humerus fractures were the result of a fall, which is similar to the values we report (87.5 % in men and 92.3 % in women). Our study reports that a large proportion (62.5 % of men and 71.8 % of women) sustained a fracture as the result of a fall from standing height or less, which is lower than the Finnish result of 90 %. We also report that 29.2 % of men and 66.7 % of women were walking when they fell, the latter of which is similar to the Finnish value of 61 %. Approximately half of the patients (54 %) in the Finnish study reported sustaining their fractures outdoors, which was similar to our results for women (56.6 %) but not for men (76.2 %). There were differences in reporting of the “reason for falling” between the Finnish study and our study. Tripping/slipping was the reason for 72 % of proximal humerus fractures in the Finnish study, whereas we reported that the main reasons for falling were uneven or slippery surface and loss of balance. The Finnish study also reported that individuals with proximal humerus fractures did not break their fall (with an outstretched arm or hand) as often as the control group (OR 0.33 95 % CI 0.14, 0.80). In this study, we found that many (45.2 % of men and 34.4 % of women) individuals sustained a fracture of the humerus from landing on their shoulder, which is consistent with not breaking their fall with an outstretched hand or arm. We also found that some individuals (12.9 % of men and 25.0 % of women) landed on their hand or arm after falling. The reason for many of the differences between our results and the Finnish study may be due to the age range investigated; the latter study included only patients aged 50 years and over, while we included all adult men (≥20 years) and women aged 35 years or over.
In our study, we reported a range of factors that influenced humerus fracture in men and women. Other studies have also reported risk factors, such as the work by Olsen et al. [23], which showed that prior osteoporotic fractures increased the risk of proximal humerus fractures. We have also previously reported on the increased risk of subsequent fracture after a prior fracture [24]. In our study, both men and post-menopausal women had a significant increase in risk of humerus fracture if they had sustained a prior fracture (ORs 6.60 and 9.37, respectively). Other studies have reported that low BMD and a high falls risk are predictors of proximal humerus fracture [2, 4, 8], which we also observed in our study. We report that a high femoral neck BMD in men and ultradistal forearm BMD in women were associated with a reduced risk of humerus fracture. Additionally, falls were found to be an important predictor of fracture in pre-menopausal women (OR 6.89). Falls were also an independent predictor of humerus fractures in post-menopausal women, but when adjusted for age, became non-significant. Older age was protective in men, which may suggest that humerus fractures occur more often in younger men [7].
Studies have also shown that low dietary calcium intake, poor vision, high alcohol consumption, diabetes and low physical activity are associated with an increased risk of humerus fracture [2, 8]. We did not observe any differences between controls and individuals with humerus fractures in terms of diabetes, alcohol or physical activity, but we did observe differences in terms of milk and other dairy consumption as well as poor vision. We observed that post-menopausal women who reported decreased vision had a lower risk of humerus fracture. This may be explained by considering that the women who were aware they had poor eyesight may be more careful to avoid tripping or stumbling. Our study also reported that in men, milk consumption was a risk factor for humerus fracture and in post-menopausal women, non-milk dairy consumption was protective. Milk consumption may not have been a risk factor for post-menopausal women because many had a high consumption, and it was difficult to determine any differences between the control and fracture groups. Equally, men tended to consume small amounts of non-milk dairy products overall. These results are supported by those recently published by Michaëlsson et al. [25], which investigated the impact of milk and non-milk (fermented) dairy products on mortality and fracture risk in two large Swedish cohorts of men and women. This Swedish study reported that there was an increased fracture risk in women with high milk consumption, but the effect was not observed for men. The study also reported that high consumption of fermented dairy products resulted in a reduction of fracture risk. This is an important finding, as high milk consumption is often recommended to avoid osteoporosis. Finally, our study reported weight and height as risk factors in pre- and post-menopausal women, respectively, which may be due to differences in the mechanism of fracture. Those who are heavier or taller may have an increased risk of a fall that leads to a humerus fracture.
One strength of this study is the methodology, which involved the use of radiological reports rather than hospital discharge data, thus avoiding the ascertainment of the same fracture multiple times [15]. Due to the small number of medical imaging centres in the region, we were able to ascertain fractures for most residents of the BSD. However, for one radiological clinic that opened in 2005, we were unable to obtain radiological reports. We may also have missed a small number of fractures from residents of the BSD who sustained their fractures and were managed outside the region. We also had a small number of participants from the Fracture Cohort to investigate risk factors, but our results are similar to those reported in the literature. The Fracture Cohorts for men and women were of different ages; women were 35 years or over, and men were 20 years and over. However, we observed that women did not sustain many humerus fractures in the 20–29 year age group (Fig. 2), suggesting that even if the Fracture Cohort for women contained all adult individuals, the results would not differ from what we have reported. Finally, incidence rate data were collected for men and women during the years 2006 and 2007, whereas risk factors were collected for women at a different time (1994–1996), which we acknowledge as a limitation in the results for risk factors in this study. In addition, the numbers of participants in the Fracture Cohorts for both men and women were low and as such, the results of the risk factor analysis should be interpreted with caution.
Conclusions
This study reports on humerus fractures for males and females during 2006 and 2007 in south-eastern Australia. For all humerus fractures, males had a lower median age than females. The median age of humeral shaft fracture was lower than for proximal humerus fractures, in both sexes. Men were hospitalised more often than women. Males and females both had high incidence of humeral shaft fractures in childhood, with increasing proximal humerus fractures in mid-adulthood (>50 years). Many fractures were the result of a fall onto an outstretched hand or shoulder. In men, age, femoral neck BMD, prior fracture and milk consumption were identified as independent predictors of humerus fracture. In pre-menopausal women, only height and falls were independent predictors. However, in post-menopausal women, ultradistal forearm BMD, weight, education, prior fracture, dairy consumption and decreased vision were all independent predictors. These risk factors may help to predict and prevent proximal humerus and shaft fractures in men and women.
References
Hirzinger C, Tauber M, Resch PDH (2011) Die Fraktur des proximalen humerus [Fractures of the proximal humerus]. Der Unfallchirurg [The Trauma Surgeon] 114:1051–1058
Lee SH, Dargent-Molina P, Bréart G (2002) Risk factors for fractures of the proximal humerus: results from the EPIDOS prospective study. J Bone Miner Res 17:817–825
Maravic M, Briot K, Roux C (2014) Burden of proximal humerus fractures in the French National Hospital Database. Orthop Traumatol 100:931–934
Roux A, Decroocq L, Batti SE, Bonnevialle N, Moineau G, Trojani C, Boileau P, Peretti Fd (2012) Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol 98:715–719
Charissoux J-L, Vergnenegre G, Pelissier M, Fabre T, Mansat P (2013) Epidemiology of distal humerus fractures in the elderly. Orthop Traumatol 99:765–769
Palvanen M, Kannus P, Niemi S, Parkkari J (2010) Secular trends in distal humeral fractures of elderly women: Nationwide statistics in Finland between 1970 and 2007. Bone 46:1355–1358
Min W, Anwar A, Ding BC, Tejwani NC (2010) Open distal Humérus fractures: review of the literature. Bull Hosp Jt Dis 68:257-261
Chu SP, Kelsey JL, Keegan THM, Sternfeld B, Prill M, Quesenberry CP, Sidney S (2004) Risk factors for proximal humerus fracture. Am J Epidemiol 160:360–367
Clement ND, Duckworth AD, McQueen MM, Court-Brown CM (2014) The outcome of proximal humeral fractures in the elderly: predictors of mortality and function. Bone Jt J 96-B:970-977
Kannus P, Palvanen M, Niemi S, Sievänen H, Parkkari J (2009) Rate of proximal humeral fractures in older Finnish women between 1970 and 2007. Bone 44:656–659
Dimai HP, Svedbom A, Fahrleitner-Pammer A, Pieber T, Resch H, Zwettler E, Thaler H, Szivak M, Amrein K, Borgström F (2013) Epidemiology of proximal humeral fractures in Austria between 1989 and 2008. Osteoporos Int 24:2413–2421
Watts JJ, Abimanyi-Ochom J, Sanders KM (2013) Osteoporosis costing all Australians A new burden of disease analysis—2012 to 2022. Osteoporosis Australia. http://apo.org.au/node/37062
Abimanyi-Ochom J, Watts JJ, Borgström F, Nicholson GC, Shore-Lorenti C, Stuart AL, Zhang Y, Iuliano S, Seeman E, Prince R, March L, Cross M, Winzenberg T, Laslett LL, Duque G, Ebeling PR, Sanders KM (2015) Changes in quality of life associated with fragility fractures: Australian arm of the International Cost and Utility Related to Osteoporotic Fractures Study (AusICUROS). Osteoporos Int 26:1781–1790
Huttunen TT, Launonen AP, Pihlajamäki H, Kannus P, Mattila VM (2012) Trends in the surgical treatment of proximal humeral fractures: a nationwide 23-year study in Finland. BMC Musculoskeletal Disorders 13:261
Pasco JA, Nicholson GC, Henry MJ, Kotowicz MA, Gaudry TM (1999) Identification of incident fractures: the Geelong osteoporosis study. Aust N Z J Med 29:203–206
Pasco JA, Nicholson GC, Kotowicz MA (2012) Cohort profile: Geelong osteoporosis study. Int J Epidemiol 41:1565–1575
Centers for Disease Control and Prevention (2013) International Classification of Diseases, Ninth Revision (ICD-9)
Australian Bureau of Statistics (2006) Census Community Profile Series (catalogue number 2001.0)
Sanders KM, Seeman E, Ugoni AM, Pasco JA, Martin TJ, Skoric B, Nicholson GC, Kotowicz MA (1999) Age- and gender-specific rate of fractures in Australia: a population-based study. Osteoporos Int 10:240–247
Hill K, Schwarz J (2004) Assessment and management of falls in older people. Intern Med J 34:557–564
Sanders KM, Nicholson GC, Ugoni AM, Pasco JA, Seeman E, Kotowicz MA (1999) Health burden of hip and other fractures in Australia beyond 2000. Med J Aust 170:467–470
Palvanen M, Kannus P, Parkkari J, Pitkäjärvi T, Pasanen M, Vuori I, Järvinen M (2000) The injury mechanisms of osteoporotic upper extremity fractures among older adults: a controlled study of 287 consecutive patients and their 108 controls. Osteoporos Int 11:822–831
Olsson C, Nordqvist A, Petersson CJ (2004) Increased fragility in patients with fracture of the proximal humerus: a case control study. Bone 34:1072–1077
Holloway KL, Brennan SL, Kotowicz MA, Bucki-Smith G, Timney EN, Dobbins AG, Williams LJ, Pasco JA (2015) Prior fracture as a risk factor for future fracture in an Australian cohort. Osteoporos Int 26:629–635
Michaëlsson K, Wolk A, Langenskiöld S, Basu S, Lemming EW, Melhus H, Byberg L (2014) Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ 349:g6015
Acknowledgments
The study was supported by the National Health and Medical Research Council (NHMRC) Australia (Project 628582), the Geelong Regional Medical Foundation, Arthritis Foundation of Australia, Perpetual Trustees, and Amgen Europe (GmBH); however, the funding bodies played no part in the design or conduct of the study, the collection, management, analysis and interpretation of the data, nor in the preparation or review of the manuscript. Sharon L. Brennan-Olsen is supported by an Alfred Deakin Postdoctoral Fellowship (2015–2016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kara L. Holloway, Gosia Bucki-Smith, Amelia G. Morse, Sharon L Brennan-Olsen, Mark A. Kotowicz, David J. Moloney, Kerrie M. Sanders, Sam Korn, Elizabeth N. Timney, Amelia G. Dobbins and Julie A. Pasco these authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This study was approved by the Barwon Health Human Research Ethics Committee. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Holloway, K.L., Bucki-Smith, G., Morse, A.G. et al. Humeral Fractures in South-Eastern Australia: Epidemiology and Risk Factors. Calcif Tissue Int 97, 453–465 (2015). https://doi.org/10.1007/s00223-015-0039-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-015-0039-9