Abstract
Purpose
Transcranial direct current stimulation (tDCS) can alter cortical excitability, making it a useful tool for promoting neuroplasticity in dysphagia rehabilitation. Clinical trials show functional improvements in swallowing following anodal tDCS despite varying dosing parameters and outcomes. The aim of the current study was to determine the most effective amplitude criterion (e.g., 0 mA [sham/control], 1 mA, 2 mA) of anodal tDCS for upregulating the swallowing sensorimotor cortex.
Method
As a novel paradigm, tDCS, functional near-infrared spectroscopy (fNIRS), and surface electromyography (sEMG) were simultaneously administered while participants completed a swallowing task. This allowed for measurement of the cortical hemodynamic response and submental muscle contraction before, during, and after tDCS. At the conclusion of the study, participants were asked to rate their level of discomfort associated with tDCS using a visual analog scale.
Results
There was no significant difference in the hemodynamic response by time or amplitude. However, post-hoc analyses indicated that in the post-stimulation period, changes to the hemodynamic response in the left (stimulated) hemisphere were significantly different for the groups receiving 1 mA and 2 mA of tDCS compared to baseline. Participants receiving 1 mA of tDCS demonstrated reduced hemodynamic response. There was no significant difference in submental muscle contraction during or after tDCS regardless of amplitude. Anodal tDCS was well tolerated in healthy adults with no difference among participant discomfort scores across tDCS amplitude.
Conclusions
During a swallowing task, healthy volunteers receiving 1 mA of anodal tDCS demonstrated a suppressed hemodynamic response during and after stimulation whereas those receiving 2 mA of anodal tDCS had an increase in the hemodynamic response. tDCS remains a promising tool in dysphagia rehabilitation, but dosing parameters require further clarification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In an effort to improve treatment for dysphagia (difficulty swallowing) following stroke, researchers are exploring a type of non-invasive brain stimulation known as transcranial direct current stimulation (tDCS). tDCS is administered using a neuromodulation device that can be applied to consenting patients of all cognitive levels. During tDCS, a positively-charged anode and a negatively-charged cathode are placed on the scalp to deliver low-intensity electrical current to the underlying cortical regions of interest. Dosing paradigms for dysphagia rehabilitation vary based on electrode placement, amplitude administered, length of stimulation, and task dependency. Understanding dosing paradigms remains in its infancy given that the exact mechanisms underlying tDCS as a rehabilitative tool are not completely understood. However, studies in humans have demonstrated increased cortical activation following anodal tDCS and reduced cortical activation with cathodal tDCS (Ammann et al. 2017; Nitsche et al. 2003; Zheng et al. 2011). It is believed that cortical stimulation either upregulates or downregulates the action potential of the underlying neurons depending upon the electrode montage. If this is the case, application of anodal tDCS following brain injury, such as a stroke, may assist with modulation of neuronal firing and cortical reorganization of damaged areas. This type of passive neuromodulation could be especially beneficial to patients with dysphagia following a stroke who may have concomitant cognitive issues and limited ability to actively participate in rehabilitation, especially given that tDCS is documented to be well-tolerated with primary complaints of itching, tingling, or burning beneath the electrode during stimulation (Bikson et al. 2016; Turski et al. 2017).
Anodal tDCS is believed to modulate depolarization by affecting the sodium and calcium receptors of the neuron (Pisegna et al. 2016; Stagg et al. 2009), as well as having an immediate effect on GABA. Long-term effects of tDCS are believed to be related to the release of activity-dependent brain-derived neurotrophic factor (BDNF) as well as changes to N-methyl-D-aspartate (NMDA) receptors (Batsikadze et al. 2013; Fritsch et al. 2010; Nitsche and Paulus 2001). GABAergic changes have also been observed in tDCS after-effects (Nitsche et al. 2003; Roche et al. 2015).
It seems logical then that tDCS could be an effective rehabilitative tool to modulate neuronal firing in patients diagnosed with neurological disease by harnessing principles of neuroplasticity. However, optimal dosing parameters are elusive; this is especially true in dysphagia research as cortical lateralization of swallowing remains a controversial issue. In an effort to define which cerebral hemisphere should receive anodal stimulation, some researchers have used transcranial magnetic stimulation to measure motor evoked potentials (MEPs) of the submental muscles before and after tDCS in healthy volunteers (Jefferson et al. 2009; Zhao et al. 2015). Some studies have found that anodal tDCS to the dominant hemisphere resulted in greater pharyngeal motor evoked potentials (MEPs) on the stimulated side only (Jefferson et al. 2009; Zhao et al. 2015) while others have found that anodal tDCS to the contralesional or non-dominant hemisphere resulted in increased MEPs bilaterally (Vasant et al. 2014). Although these studies made evident a neurophysiological connection between tDCS to the pharyngeal motor cortex and pharyngeal MEPs, they were limited in establishing the clinical significance of tDCS.
Six randomized controlled trials (RCT) have been published to date evaluating the effectiveness of anodal tDCS as a clinical treatment paradigm in patients with dysphagia following stroke (Ahn et al. 2017; Kumar et al. 2011; Pingue et al. 2018; Shigematsu et al. 2013; Suntrup-Krueger et al. 2018; Yang et al. 2012) with a seventh RCT currently under review (Kumar et al., under review). Dosing parameters have varied for each study, making a direct comparison between studies difficult (Table 1). Amplitude of stimulation has ranged from 1 to 2 mA with a length of stimulation ranging from 20 to 30 min. Number of sessions and electrode placement have varied as well. In some instances, improvement in swallowing was observed immediately following tDCS (Kumar et al. 2011; Shigematsu et al. 2013; Suntrup-Krueger et al. 2018) whereas other studies indicated delayed (Yang et al. 2012) or no improvements (Ahn et al. 2017; Pingue et al. 2018). Two recent meta-analyses including the RCTs listed above have indicated that tDCS is effective at improving post-stroke dysphagia compared to sham (Chiang et al. 2019; Marchina et al. 2021). However, given the various dosing parameters examined thus far, it is clear that the use of tDCS in dysphagia rehabilitation warrants further investigation. Specifically, improved guidance on the most effective amplitude(s) of tDCS is needed.
Purpose and hypotheses
The aim of the current study was to determine the most effective amplitude criterion (e.g., 0 mA [sham/control], 1 mA, 2 mA) of anodal tDCS for upregulating the swallowing sensorimotor cortex. These tDCS doses were chosen as they are consistent with most other studies which seek to evaluate the efficacy of tDCS (Table 1). As a novel paradigm, tDCS, functional near-infrared spectroscopy (fNIRS), and surface electromyography (sEMG) were simultaneously administered while participants completed a swallowing task. This allowed for measurement of the cortical hemodynamic response and submental muscle contraction before, during, and after varying doses of tDCS. At the conclusion of the study, participants were asked to rate their level of discomfort associated with tDCS using a visual analogue scale as the effect of tDCS amplitude on comfort is not well-established in the literature. The research question was: Does amplitude of tDCS (e.g., 0 mA [sham/control], 1 mA, 2 mA) affect the cortical hemodynamic, submental muscle contraction, or perception of discomfort during cued swallow task? It was hypothesized that the highest amplitude of tDCS (e.g., 2 mA) would result in the greatest change to the cortical hemodynamic response, greatest submental muscle contraction, and the highest rating of discomfort in comparison to the low-dose (e.g., 1 mA) or sham conditions.
Methods
Participants
This study was approved by the James Madison University Internal Review Board. Participants thirty years and older were recruited by bulk email advertisement; interested parties completed a Qualtrics survey to determine eligibility. Exclusion criteria included: presence of a pacemaker or deep brain stimulator, history of swallowing problems or direct dysphagia treatment, history of uncontrolled reflux symptoms as evidenced by a score of 13 or greater on the Reflux Symptom Index (Belafsky et al. 2002), history of brain injury or neurological disorder including stroke, previous neck injury requiring treatment by a physician, history of psychiatric disorder other than medically-managed depression, presence of speech motor control abnormalities, history of epileptic seizures, or diagnosis of progressive neurodegenerative disorder. Healthy participants were chosen for this study to minimize the possibility of pathological differences influencing the outcomes. Eligible participants were scheduled for a single session.
Pilot data indicated an effect size of f = 0.52 (G*Power; Faul et al. 2007, 2009), and a requisite sample size of 21 total participants, 7 per group to achieve a power of 0.95. Twenty-seven healthy adults consented to this study. Fifteen were female. Age range for all subjects was 30–66 years (mean 45.1 years, SD 10.88). All participants were right-handed.
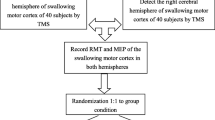
Design
In this prospective, between and within-subjects design, participants were randomly assigned to receive one of three doses of anodal tDCS to the left pericentral cortex: 0 mA (sham/control), 1 mA, or 2 mA. Both the researcher facilitating the session (author L.G.) and the participant were blinded to condition. Although evidence suggests there is bilateral cortical activation during swallowing, the anode was placed over the left hemisphere in the current study as prior imaging studies have found greater and/or earlier activation in the left hemisphere during swallowing tasks in healthies (Kamarunas et al. 2018; Martin et al. 2004; Toogood et al. 2017).
Procedures
Setup
Participants were seated upright in a stationary chair for equipment setup. Initial setup included locating the cortical regions of interest (ROIs) for placement of the functional near-infrared spectroscopy (fNIRS), which included the bilateral ventral precentral and postcentral gyri. Grounded in the Beer-Lambert Law, fNIRS uses the absorption of near-infrared light to detect changes to the oxyhemoglobin (HbO) and deoxyhemoglobin (HbR) of the cerebral cortex (Strangman et al. 2002). ROIs corresponded with the Montreal Neurological Institute (MNI) coordinates shown to be activated during swallowing (Table 2; Kamarunas et al. 2018; Soros et al. 2009). Each participant’s head was normalized into MNI brain space using Brainsight v2.0 (Rogue Research, Montreal, Quebec) and a standard sex-matched MRI. Eyeglasses with optical position sensors (NDI, Waterloo, Ontario, Polaris Model 8,800,072) registered the MRI image to the participant’s head using specific anatomical locations of the head and face as references.
Once the ROIs were identified, the fNIRS probes were fitted through the tDCS electrodes; see below for details on tDCS setup. The fNIRS probes were then placed bilaterally with each side consisting of a three emitter and five detector array. Each emitter and detector pair were spaced 3 cm apart from each other. Light at wavelengths 690 and 830 nm was released from the emitters, absorbed and reflected by the cortex, and identified by the detectors to measure changes in blood oxygenation. The changes in concentrations of oxygenated hemoglobin (e.g., the hemodynamic response; HDR) were recorded by a continuous wave fNIRS system (TechEn, Milford, MA, Model CW6;). Signals were monitored, and each channel was individually gained at the beginning of each recording session. The sampling rate was 25 Hz.
Phoresor II Auto tDCS was setup next (Iomed, Salt Lake City, UT, Model No. PM850). Prior to securing the fNIRS probes, tDCS electrodes were placed with the 6.5 × 6.5 cm saline-soaked anodal electrode positioned over the left primary motor cortex and the 6.5 × 6.5 cm saline-soaked cathode positioned over the right supraorbital region. Six 6 mm holes in the anodal electrode allowed for the placement of the fNIRS probes through the electrode for simultaneous tDCS and fNIRS. Since the tDCS electrode distributes electrical current beneath the entire surface area of the electrode (Pisegna et al. 2016; Wagner et al. 2007), the punched holes should not make a significant difference in the overall current density received by the participant, and this process has been replicated in other studies (Knotkova et al. 2019; Yan et al. 2015). Once all fNIRS probes and tDCS electrodes were in place, 3 M™ Coban self-adhering wrap was placed around the patient’s head to secure the instrumentation.
A piezoelectric accelerometer (Kistler Instrument Corporation, Amherst, NY) was secured over the thyroid notch using medical tape and signaled laryngeal elevation during swallowing. Next, the skin was abraded with an alcohol swab and surface electromyography (sEMG) electrodes were placed on the skin to measure bilateral submental muscle activity. Norotrode 20 disposable electrodes were placed along with the posterior one-third of the submental muscles at midline and were 22 mm ± 1 mm apart from one another. The submental muscles, consisting of the anterior belly of the digastric, mylohyoid, and geniohyoid, were chosen as they are documented to be associated with movement of the hyoid bone during swallowing (Vaiman et al. 2004; Wheeler et al. 2007). A single Positrace ECG electrode was placed along the right clavicle and served as the grounding electrode. Digital signals were recorded using PowerLab 16/35 and LabChart8 software (AD Instruments, Inc., Sydney, Australia). A trained observer also documented online visualization of hyolaryngeal elevation that represented swallowing directly into the LabChart8 software. Each session was video recorded and synced in LabChart8. Figure 1 displays the equipment setup.
A 3/16 in. diameter silicon tube was connected to a Masterflex motorized infusion pump (Cole-Parmer Instrument Co., Chicago, IL) to allow for automatic water bolus delivery. To minimize jaw and head movements during bolus delivery, participants held the tubing in the left corner of their mouth throughout the study. Water was dispensed at the rate of 1 mL/minute and acted as a cue for the participant to swallow. A 1 mL water bolus was selected given its resemblance to the volume of a saliva swallow (Lagerlof and Dawes 1984; Rudney et al. 1995).
Session task
Following equipment setup, each participant completed three 30-min blocks (i.e., pre-tDCS, tDCS, post-tDCS). During each block, the participant was instructed to sit as still as possible and to swallow every time they received a 1 mL water bolus from the tube placed in their mouth. Simultaneous fNIRS and swallowing task was utilized as this is considered best clinical practice when working with patients to encourage cortical reorganization. Further, this replicates the majority of studies done with tDCS in swallowing. During the first five minutes of each 30-min block, the participant received 1 mL of water each minute followed by a three-minute rest period where no water was administered. During the rest period, the participant was free to swallow their saliva as needed. Following the three-minute rest period, water was again administered at a rate of 1 mL/minute for five minutes. This alternating pattern was continued throughout the 30 min so that there was a total of four five-minute periods of swallowing and three three-minute rest periods, yielding 20 total swallows per 30-min block (Fig. 2). All signals were recorded continuously for each block.
During the second 30-min block only, participants were randomly assigned to receive either 0 mA (sham/control), 1 mA, or 2 mA of tDCS for the duration of the 30 min while continuing to receive water boluses and swallow as detailed above. A trained assistant started the tDCS as both the researcher completing the session (author L.G.) and the participant were blinded to the condition. In the case of sham/control, the tDCS unit ramped up to 2 mA over the course of 15 s and then was turned off by the trained assistant. During the ramp-up period, the participant received the same sensation of tingling as the participants who received active tDCS for 30 min, yet the control participants were unaware that the device was then turned off. At the conclusion of the second 30-min block (i.e., following tDCS administration), all participants were asked to rate their level of discomfort while receiving tDCS using a 100 mm anchored visual analogue scale (VAS). The left side was labeled as “no discomfort” and the right side was labeled as “discomfort that was difficult to tolerate for 30 min”. Participants were asked to put a single line (i.e. tic mark) on the VAS to represent their level of discomfort during the tDCS condition.
The third 30-min block (post-tDCS) was then completed as described above with five water infusions over the course of 5 min (one per minute) then 3 min of rest alternately repeated for a total of 20 swallows. Once all three experimental blocks were completed, equipment was removed, and the participant was excused. No adverse events occurred.
Data analysis
Swallows were readily identifiable in LabChart8 since they were marked in real time by the trained observer who documented hyolaryngeal elevation at the time of bolus delivery. If further verification of a swallowing occurrence was needed, a review of the video recording as well as the signal from the accelerometer facilitated the decision-making process. Swallow onsets were marked from the sEMG signal in LabChart8. Swallow onset was defined as 10% of the maximum amplitude at the beginning of the signal. Similarly, swallow offset was defined as when the signal returned to 10% of maximum amplitude at the end of the signal as described by Ludlow et al. (2019). Once all of the swallow onsets were marked, the times were exported to Excel.
fNIRS
fNIRS data were preprocessed with HOMER2 software (Boas et al. 2012) in Matlab 2013 (The MathWorks Inc., Natick, MA). Onset of cued swallows in LabChart8 and HOMER2 were time synchronized with shared auxiliary signals. Swallow onset times from the sEMG signal were input into HOMER2. Raw wavelengths were converted to optical density values. Physiological signals were removed with a bandpass filter at 0.01–0.5 Hz then optical density was converted to hemoglobin concentrations with the application of the modified Beer-Lambert law. Motion correction was completed using a correlation-based signal improvement filter (Cui et al. 2010) then adaptive short separation filtering. The event-related averages of oxygenated hemoglobin (OxyHb) from − 5 to 35 s from swallow onset from each channel were exported from HOMER2 into Excel. Figure 3 displays the aggregated oxygenated and deoxygenated hemodynamic response for each amplitude across time by hemisphere.
Baseline hemodynamic activity was controlled by subtracting the mean baseline activity from each channel individually. Baseline was defined as − 5 to 0 s prior to swallow onset. The median value across 5–30 s from swallow onset from each channel was computed (Herold et al. 2018) and then averaged across all the channels for each hemisphere separately. Therefore, each participant had one median OxyHb value for each hemisphere per condition (pre-tDCS, tDCS, post-tDCS). For analysis, these OxyHb values were normalized to baseline (pre-tDCS) to reflect changes during and after tDCS.
sEMG
Raw sEMG data were collected with a 2 mV range using a 10 kHz sampling rate. Consistent with other sEMG research protocols, a band-pass filter was applied (75–500 Hz) to the signal (Zhu et al. 2017). The signal was then rectified and smoothed with a low pass filter (10 Hz). The smoothed signal was normalized to the largest muscle contraction during a swallow across the entirety of the session (e.g., pre-tDCS, tDCS, post-tDCS); this was normalized as 100%. The mean sEMG signal during rest was averaged across trials and normalized as 0% for each block of the session (e.g., pre-tDCS, tDCS, post-tDCS).
Once the sEMG swallowing signal was normalized, swallow onset was defined as 10% of the maximum amplitude at the beginning of the signal. Swallow offset was defined as when the signal returned to 10% of maximum amplitude at the end of the signal (Ludlow et al. 2019). The root mean square (RMS) was calculated from onset to offset for each trial of each condition and averaged. Submental muscle contraction was normalized to the pre-tDCS block to reflect changes in submental sEMG activation level from baseline during the tDCS and post-tDCS conditions.
Discomfort score
The location of the tic mark along the 100 mm line was measured and a score out of 100 was determined where 0 indicated no discomfort and 100 indicated discomfort that was difficult to tolerate for 30 min.
Statistical analysis
Data from three of the 27 participants were excluded due to poor fNIRS signals; therefore, the final analysis came from 24 healthy participants, 8 in each group. To compare changes in cortical activation as measured by OxyHb before, during, and after tDCS, one 2-way mixed ANOVA was completed for each hemisphere examining the interaction between the groups (0 mA, 1 mA, 2 mA) and condition (pre-tDCS, tDCS, post-tDCS). Post-hocs were completed when indicated using independent and paired samples t tests. A two-way mixed ANOVA was completed to examine the effects of group and condition on submental contraction as measured by sEMG. A one-way between-subjects ANOVA was used to assess for differences in the level of discomfort based on the amplitude of tDCS administered. Alpha level was set to 0.05.
Results
Group comparisons
There was no significant difference between groups based on age (F(2,21) = 1.29, p = 0.30, ηp2 = 0.11). However, there was a significant difference between groups based on sex, as assessed by a Fisher’s exact test, p = 0.03. Post hoc analysis involved pairwise comparisons using multiple Fisher’s exact tests (2 × 2) with a Bonferroni correction. Statistical significance was accepted at p < 0.016667. The proportion of males and females within each group was not statistically significant when compared at the group level (sham vs. 1 mA: p = 0.026, sham vs. 2 mA: p = 0.077, 1 mA vs. 2 mA: p = 1.0). See Table 3 for demographic information.
Hemodynamic response
For the right (unstimulated) hemisphere, there were no significant interactions between group and condition (F(4,42) = 1.23, p = 0.31, ηp2 = 0.11) and no effect of condition (F(2,42) = 0.30, p = 0.75, ηp2 = 0.014; Fig. 4). For the left (stimulated) hemisphere, there were no significant interactions between group and condition (F(4,42) = 2.55, p = 0.053, ηp2 = 0.20), and there was no effect of condition (F(2,42) = 0.67, p = 0.52, ηp2 = 0.03; Fig. 5).
However, given the interactional trend and large effect size for the left hemisphere, post-hoc comparisons were made for the left hemisphere to examine between-group differences. There was a significant finding for between-group differences between the 1 mA and 2 mA groups during the post-tDCS condition (t = -2.25, p = 0.041, d = 0.95), with the 2 mA group having a significantly more positive OxyHb change (x̄ = 4.8 μM) compared to the 1 mA group, which had a decrease in OxyHb (x̄ = -5.9 μM). All other comparisons were not significant (p > 0.05).
Post-hoc examination of within-group differences for the left hemisphere indicated a significant difference between the pre-tDCS and post-tDCS conditions for the 1 mA group only, (t(7) = 2.9, p = 0.023, d = 0.57), with a significant decrease in OxyHb during the post-tDCS period compared to baseline values. All other comparisons were not significant (p > 0.05).
Surface electromyography
There was no interaction between group and condition for submental muscle contraction (F(4,40) = 0.99, p = 0.42, ηp2 = 0.09) and no effect of condition (F(2,40) = 2.70, p = 0.08, ηp2 = 0.12). Post-hoc comparison indicated a difference between pre-tDCS and post-tDCS contraction (p = 0.027) across groups, with greater contraction observed in the post condition (Fig. 6).
Discomfort scale
Descriptively, the mean discomfort score for both the 1 mA and 2 mA groups was at least double that of the discomfort score for the sham group. However, there was no effect on participant discomfort scores as a function of tDCS amplitude, F(2,21) = 1.57, p = 0.23, η2 = 0.13. This may be related to the large standard deviation for both the 1 mA and 2 mA groups. Descriptive statistics are listed in Table 4.
Discussion
To address the effect of tDCS dosing parameters during a swallowing task, we used a novel paradigm and simultaneously combined tDCS, fNIRS, and sEMG. Potentially related to insufficient statistical power, results were not statistically significant, however, trends suggest anodal tDCS to the pericentral cortex increased the hemodynamic response in both cerebral hemispheres during 30 min of 2 mA tDCS but suppressed it for the 1 mA group. Within the left (stimulated) hemisphere, there were trends for significance between groups, with the hemodynamic response being significantly higher in the 2 mA group compared to the 1 mA group during the final 30 min after tDCS was applied. Interestingly, submental muscle contraction mirrored the changes to the hemodynamic response; there was a nonsignificant reduction of submental muscle contraction during 1 mA of anodal tDCS as measured by surface electromyography (sEMG) and a nonsignificant increase in submental muscle contraction during 2 mA of anodal tDCS. Increased submental muscle contraction continued into the post-stimulation period for the 2 mA group, while the 1 mA group returned to baseline levels.
There was no significant effect of tDCS amplitude on participant discomfort. That is to say, participants did not demonstrate increased discomfort with the increased amplitude of tDCS. This is consistent with other reports that tDCS is safe for use with humans and generally well tolerated (Bikson et al. 2016; Turski et al. 2017). This finding adds to the argument that tDCS may be a beneficial augmentation to dysphagia rehabilitation for patients of all types, including those with limited communication related to advanced neurological disease.
Cortical modulation effects
To our knowledge, this is the first study that used simultaneous pairing of fNIRS and tDCS to evaluate changes to the hemodynamic response based on tDCS amplitude during a swallowing task. Although the cause for contradictory changes to the hemodynamic response for both groups receiving anodal tDCS (1 mA and 2 mA) cannot be fully answered by the data, our results are congruent with previous literature. A recent systematic review of tDCS and fNIRS studies found reduced cortical activation during tDCS stimulation (amplitudes ranging from 0.5-2 mA) and inconsistent post-stimulation effects on the hemodynamic response (Patel et al. 2020). The studies included in this systematic review included but were not specific to, swallowing.
Our results are not in agreement with a recent systematic review and meta-analysis of clinical studies evaluating the effects of tDCS on post-stroke dysphagia specifically. Although Marchina et al. (2021) found tDCS to be effective at improving post-stroke dysphagia, subgroup analyses revealed a significant moderate effect size for the low-intensity stimulation group (i.e., 1 mA for 20 min/day) compared to high-intensity stimulation group (i.e., 2 mA for at least 30 min/day). There was no significant difference between ipsilesional vs. contralesional stimulation or acute vs. chronic dysphagia (Marchina et al. 2021). However, this review focused on treatment studies with patients with dysphagia and outcome measures consisting of clinical assessments (i.e., Penetration-Aspiration Scale score [PAS], Dysphagia Outcome and Severity Scale [DOSS]) while our participants were healthy and our outcome measures included changes to the hemodynamic response and submental muscle contraction. This incongruence may also be attributed to individual variability in the dose–response relationship (Esmaeilpour et al. 2018; Marchina et al. 2021).
Still, the exact reason for the suppression of the hemodynamic response during 1 mA of anodal tDCS while 2 mA of stimulation enhances it remains unclear. There is evidence to suggest that the genetic make-up of an individual plays a role in one’s response to tDCS. Specifically, individuals with val66met polymorphism secrete different amounts of activity-dependent BDNF and therefore may respond differently to tDCS (Fritsch et al. 2010; Wiegand et al. 2016). Results may be related to genetic factors that could not be accounted for given the limitations and small sample size of the current study.
Role of sham stimulation
One of the most consistent findings was an increase in both the hemodynamic response and submental muscle contraction for participants receiving sham tDCS. Although our sham procedures were similar to several other placebo-controlled tDCS studies (Pingue et al. 2018; Suntrup-Krueger et al. 2018), some researchers are beginning to question if even sham stimulation is enough to modulate neural activity (Boonstra et al. 2016; Fonteneau et al. 2019; Nikolin et al. 2018). Typical tDCS sham protocols include ramping up the stimulation to 1 mA or 2 mA over a 15 to 30 s period before ramping down or turning the device off (Dyke et al. 2016; Pena-Gomez et al. 2012; Stagg et al. 2013), but Boonstra et al. (2016) found significant changes in the 15-min resting-state EEG signal of healthy participants after receiving sham stimulation (30 s ramp up to 2 mA, 30 s ramp down).
Other researchers have argued that the presence of a medical device like tDCS could induce enough expectation from the participant to result in a placebo effect (Burke et al. 2019; Fonteneau et al. 2019; Kaptchuk et al. 2000; Kaptchuk and Miller 2015).
Limitations and future directions
Although there is not a clear explanation for the differences seen between 1 and 2 mA of anodal tDCS, current findings suggest that further research on the effectiveness of tDCS is needed. Its exact role in neuromodulation remains undefined. In addition, varying dosing parameters, such as the timing of stimulation, electrode montage, and length and amplitude of stimulation make it difficult to draw distinct conclusions between studies published to date.
The current study is not without limitations. First, participants did not receive individual MRI scans for this study so the fNIRS probes were placed on the scalp based on a normalized and sex-matched MRI within Brainsight. This could have resulted in the imprecise placement of the fNIRS probes but is likely no more imprecise than using the 10–20 system. In addition, participants were healthy and relatively young. It is possible that greater neuromodulation effects from the same doses of tDCS would be seen in geriatric or neurologically-impaired populations whose baseline cortical activation may be divergent from the participants in this study. Future studies should explore the differences in tDCS effects on neurologically intact versus neurologically-impaired populations. Next, participants received only one 30-min session of tDCS; some evidence suggests that only 20–60% of participants demonstrate cortical excitability following a single session of anodal tDCS, potentially related to individual variability (Bashir et al. 2019). Therefore, further studies should continue to explore the effect of consecutive sessions on the hemodynamic response. In relation to the sEMG data, EMG frequency spectrum data was not analyzed, although this may give information regarding muscular fatigue. Future studies should consider this as well. Finally, participants were simply asked to swallow when receiving a water bolus. Although this swallowing should have induced cortical activation on its own, a more deliberate task, such as completing an effortful swallow with biofeedback, may elicit more significant activation. Although we considered implementing this in the current study, we decided against it due to the potential confounder of participant fatigue by the end of the study. Future studies should continue to evaluate task selection, with consideration for fatigue, as a factor of tDCS effectiveness.
Conclusions
During the simultaneous pairing of fNIRS, tDCS, and sEMG, 30 min of anodal tDCS to the left pericentral cortex of healthy adults was well tolerated with no significant difference among participant discomfort scores across tDCS amplitudes. During the post-tDCS period, there was a significant difference in the hemodynamic response between groups receiving 1 mA or 2 mA of anodal tDCS. Within the 1 mA group, there was a suppression of the hemodynamic response in the left (stimulated) hemisphere after receiving tDCS compared to baseline, potentially indicating that 2 mA of anodal tDCS is more likely to upregulate the swallowing sensorimotor cortex compared to sham or 1 mA of anodal tDCS. Although not statistically significant, there was also a reduction in submental muscle contraction following 1 mA of anodal tDCS and an increase in submental muscle contraction following 2 mA of anodal tDCS. tDCS remains a promising tool in dysphagia rehabilitation, but dosing parameters require further clarification.
Data availability
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
Code availability
NA.
References
Ahn YH, Sohn HJ, Park JS, Ahn TG, Shin YB, Park M, Ko SH, Shin YI (2017) Effect of bihemispheric anodal transcranial direct current stimulation for dysphagia in chronic stroke patients: a randomized clinical trial. J Rehabilitative Med 49:30–35
Ammann C, Lindquist MA, Celnik PA (2017) Response variability of different anodal transcranial direct current stimulation intensities across multiple sessions. Brain Stimul 10(4):757–763
Bashir S, Ahmad S, Alatefi M, Hamza A, Sharaf M, Fecteau S, Yoo WK (2019) Effects of anodal transcranial direct current stimulation on motor evoked potentials variability in humans. Physiol Rep 7(13):e14087
Batsikadze G, Moliadze V, Paulus W, Kuo MF, Nitsche MA (2013) Partially non-linear stimulation intensity-dependent effects of direct current stimulation on motor cortex excitability in humans. J Physiol 591(7):1987–2000
Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the reflux symptom index (RSI). J Voice 16(2):274–277
Bikson, M., Grossman, P., Thomas, C., Zannou, A.L., Jiang, J., Adnan, T., Mourdoukoutas, A., Kronberg, G., Truong, D., Boggio, P., Brunoni, A., Charvet, L., Fregni, F., Fritsch, B., Gillick, B., Hamilton, R.H., Hampstead, B.M., Jankord, R., Kirston, A.,… Woods, A.J. (2016). Safety of transcranial direct current stimulation: Evidence based update 2016. Brain Stimulation, 9, 641-661
Boas, D., Dubb, J., & Huppert, T. (2012). Hemodynamic evoked response (HOMER2) [Software]. Available from https://www.nitrc.org/projects/homer2.
Boonstra TW, Nikolin S, Meisener AC, Martin DM, Loo CK (2016) Change in mean frequency of resting-state electroencephalography after transcranial direct current stimulation. Front Hum Neurosci 10(270):1–13
Burke MJ, Kaptchuk TJ, Pascual-Leone A (2019) Challenges of differential placebo effects in contemporary medicine: the example of brain stimulation. Ann Neurol 85(1):12–20
Chiang CF, Lin MT, Hsiao MY, Yeh YC, Liang YC, Wang TG (2019) Comparative efficacy of noninvasive neurostimulation therapies for acute and subacute poststroke dysphagia: a systematic review and network meta-analysis. Arch Phys Med Rehabil 100(4):P739-750
Cui X, Bray S, Reiss A (2010) Functional near infrared spectroscopy (NIRS) signal improvement based on negative correlation between oxygenated and deoxygenated hemoglobin dynamics. Neuroimage 49(4):3039
Dyke K, Kim S, Jackson GM, Jackson SR (2016) Intra-subject consistency and reliability of response following 2mA transcranial direct current stimulation. Brain Stimul 9:819–825
Esmaeilpour Z, Marangolo P, Hampstead BM, Bestmann S, Galletta E, Knotkova H, Bikson M (2018) Incomplete evidence that increasing current intensity of tDCS boosts outcomes. Brain Stimul 11(2):310–321
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavioral Res Methods 39(2):175–191
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Res Methods, 41(4): 1149–1160.
Fonteneau C, Mondino M, Arns M, Baeken C, Bikson M, Brunoni AR, Burke MJ, Neuvoen T, Padberg F, Pascual-Leone A, Poulet E, Ruffini G, Santarnecchi E, Sauvaget A, Schellhorn K, Suaud-Chagny MF, Palm U, Brunelin J (2019) Sham tDCS: A hidden source of variability? Reflections for further blinded, controlled trials. Brain Stimul 12(3):668–673
Fritsch B, Reis J, Martinowich K, Schambra HM, Ji Y, Cohen LG, Lu B (2010) Direct current stimulation promotes BDNF-dependent synaptic plasticity: potential implications for motor learning. Neuron 66:198–204
Herold F, Wiegel P, Scholkmann F, Muller NG (2018) Applications of functional near-infrared spectroscopy (fNIRS) neuroimaging in exercise-cognition science: a systematic, methodology-focused review. J Clin Med 7(12):466
Jefferson S, Mistry S, Singh S, Rothwell J, Hamdy S (2009) Characterizing the application of transcranial direct current stimulation in human pharyngeal motor cortex. Am J Physiol-Gastrointestinal Liv Physiol 297(6): G1035-G1040.
Kamarunas E, Mulheren R, Palmore K, Ludlow C (2018) Timing of cortical activation during spontaneous swallowing. Exp Brain Res 236:475–484
Kaptchuk TJ, Miller FG (2015) Placebo effects in medicine. N Engl J Med 373:8–9
Kaptchuk TJ, Goldman P, Stone DA, Stason WB (2000) Do medical devices have enhanced placebo effects? J Clin Epidemiol 53(8):786–792
Knotkova H, Riggs A, Berisha D, Borges H, Bernstein H, Patel V, Truong DQ, Unal G, Arce D, Datta A, Bikson M (2019) Automatic M1-SO montage headgear for transcranial direct current stimulation (tDCS) suitable for home and high-throughput in-clinic applications. Neuromodulation 22(8):904–910
Kumar S, Wagner CW, Frayne C, Zhu L, Selim M, Feng W, Schlaug G (2011) Noninvasive brain stimulation may improve stroke-related dysphagia: a pilot study. Stroke 42(4):1035–1040
Kumar S, Langmore S, Massaro J, Palmisano J, Wang N, Searls D, Lioutas V, Pisegna J, Wagner C, Schlaug G (under review) Fostering eating after stroke with transcranial direct current stimulation (FEASt): a randomized controlled trial of non-invasive brain stimulation for dysphagia recovery.
Lagerlof F, Dawes C (1984) The volume of saliva in the mouth before and after swallowing. J Dent Res 63(5):618–621
Ludlow CL, Kent RD, Gray LC (2019) Measuring voice, speech, and swallowing in the clinic and laboratory. Plural Publishing Inc, San Diego, CA
Marchina S, Pisegna JM, Massaro JM, Langmore SE, McVey C, Wang J, Kumar S (2021) Transcranial direct current stimulation for post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. J Neurol 268(1):293–304
Martin RE, MacIntosh BJ, Smith RC, Barr AM, Stevens TK, Gati JS, Menon RS (2004) Cerebral areas processing swallowing and tongue movement are overlapping but distinct: a functional magnetic resonance imaging study. J Neurophysiol 92:2428–2443
Nikolin S, Martin D, Loo CK, Boonstra, & T.W. (2018) Effects of tDCS dosage on working memory in healthy participants. Brain Stimul 11(3):518–527
Nitsche MA, Paulus W (2001) Sustained excitability elevations induced by transcranial DC motor cortex stimulation in humans. Neurology 57(10):1899–1901
Nitsche MA, Schauenburg A, Lang N, Liebetanz D, Exner C, Paulus W, Tergau F (2003) Facilitation of implicit motor learning by weak transcranial direct current stimulation of the primary motor cortex in the human. J Cogn Neurosci 15(5):619–626
Patel R, Dawidziuk A, Darzi A, Singh H, Leff DR (2020) Systematic review of combined functional near-infrared spectroscopy and transcranial direct-current stimulation studies. Neurophotonics 7(2): 020901–1–020901–30.
Pena-Gomez C, Sala-Lonch R, Junque C, Clemente IC, Vidal D, Bargallo N, Falcon C, Valls-Sole J, Pascual-Leone A, Bartres-Faz D (2012) Modulation of large-scale brain networks by transcranial direct current stimulation evidenced by resting-state functional MRI. Brain Stimul 5(3):252–263
Pingue V, Priori A, Malovini A, Pistarini C (2018) Dual transcranial direct current stimulation for poststroke dysphagia: a randomized controlled trial. Neurorehabil Neural Repair 32(6–7):635–644
Pisegna JM, Kaneoka A, Pearson WG, Kumar S, Langmore SE (2016) Effects of non-invasive brain stimulation on post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. Clin Neurophysiol 127:956–968
Roche N, Geiger M, Bussel B (2015) Mechanisms underlying transcranial direct current stimulation in rehabilitation. Ann Phys Rehabil Med 58:214–219
Rudney JD, Ji Z, Larson CJ (1995) The prediction of saliva swallowing frequency in humans from estimates of salivary flow rate and the volume of saliva swallowed. Arch Oral Biol 40(6):507–512
Shigematsu T, Fujishima I, Ohno K (2013) Transcranial direct current stimulation improves swallowing function in stroke patients. Neurorehabil Neural Repair 27(4):363–369
Soros P, Inamoto Y, Martin RE (2009) Functional brain imaging of swallowing: An activation likelihood estimation meta-analysis. Hum Brain Mapp 30:2426–2439
Stagg CJ, Best JG, Stephenson MC, O’Shea J, Wylezinska M, Kincses ZT, Morris PG, Matthews PM, Johansen-Berg H (2009) Polarity-sensitive modulation of cortical neurotransmitters by transcranial stimulation. J Neurosci 29(16):5202–5206
Stagg CJ, Lin RL, Mezue M, Segerdahl A, Kong Y, Xie J, Tracey I (2013) Widespread modulation of cerebral perfusion induced during and after transcranial direct current stimulation applied to the left dorsolateral prefrontal cortex. J Neurosci 33(28):11425–11431
Strangman G, Boas DA, Sutton JP (2002) Review: Non-invasive neuroimaging using near-infrared light. Biol Psychiat 52:679–693
Suntrup-Krueger S, Ringmaier C, Muhle P, Wollbrink A, Kemmling A, Hanning U, Claus I, Warnecke T, Teismann I, Pantev C, Dziewas R (2018) Randomized trial of transcranial direct current stimulation for poststroke dysphagia. Ann Neurol 83:328–340
Toogood JA, Smith RC, Stevens TK, Gati JS, Menon RS, Theurer J, Weisz S, Affoo RH, Martin RE (2017) Swallowing preparation and execution: Insights from a delayed-response functional magnetic resonance imaging (fMRI) study. Dysphagia 32:526–541
Turski CA, Kessler-Jones A, Chow C, Hermann B, Hsu D, Jones J, Seeger SK, Chappell R, Boly M, Ikonomidou C (2017) Extended multiple-field high-definition transcranial direct current stimulation (HD-tDCS) is well tolerated and safe in healthy adults. Restor Neurol Neurosci 35(6):631–642
Vaiman M, Eviatar E, Segal S (2004) Surface electromyographic studies of swallowing in normal subjects: a review of 440 adults. Otolaryngol-Head Neck Surg 131(6):977–985
Vasant DH, Mistry S, Michou E, Jefferson S, Rothwell JC, Hamdy S (2014) Transcranial direct current stimulation reverses neurophysiological and behavioral effects of focal inhibition of human pharyngeal motor cortex on swallowing. J Physiol 592(4):695–709
Wheeler KM, Chiara T, Sapienza CM (2007) Surface electromyographic activity of the submental muscles during swallow and expiratory pressure threshold training tasks. Dysphagia 22:108–116
Wiegand A, Nieratschker V, Plewnia C (2016) Genetic modulation of transcranial direct current stimulation effects on cognition. Front Hum Neurosci 10:651
Yan J, Wei Y, Wang Y, Xu G, Li Z, Li X (2015) Use of functional near-infrared spectroscopy to evaluate the effects of anodal transcranial direct current stimulation on brain connectivity in motor-related cortex. J Biomed Opt 20(4):046007
Yang EJ, Baek SR, Shin J, Lim JY, Jang HJ, Kim YK, Paik NJ (2012) Effects of transcranial direct current stimulation (tDCS) on post-stroke dysphagia. Restor Neurol Neurosci 30:303–311
Zhao S, Dou Z, Wei X, Li J, Dai M, Wang Y, Yang Q, He H (2015) Task-concurrent anodal tDCS modulates bilateral plasticity in the human suprahyoid motor cortex. Front Hum Neurosci 9:1–9
Zheng X, Alsop DC, Schlaug G (2011) Effects of transcranial direct current stimulation (tDCS) on human regional cerebral blood flow. Neuroimage 50:26–33
Zhu M, Yu B, Yang W, Jiang Y, Lu L, Huang Z, Chen S, Li G (2017) Evaluation of normal swallowing functions by using dynamic high-density surface electromyography maps. Biomed Eng Online 16(133):1–18
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. James Madison University supported participant incentives in the form of gift cards through internal funding mechanisms.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation and data collection were performed by LG and EK. Data analysis was completed by LG and EK. The first draft of the manuscript was written by LG and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Lindsay Griffin: None known. Erin Kamarunas: None known. Christina Kuo: None known. Cynthia O’Donoghue: None known.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Internal Review Board of James Madison University (March 2018, No. 18–0423).
Consent to participate
The authors affirm that all study participants provided informed written consent prior to study enrollment.
Consent for publication
The authors affirm that all study participants provided informed consent for publication.
Additional information
Communicated by Melvyn A. Goodale.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Griffin, L., Kamarunas, E., Kuo, C. et al. Comparing amplitudes of transcranial direct current stimulation (tDCS) to the sensorimotor cortex during swallowing. Exp Brain Res 240, 1811–1822 (2022). https://doi.org/10.1007/s00221-022-06381-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-022-06381-z