Abstract
The amygdala has been demonstrated to contribute to pain-related behavior and food preference. Here, the effect of pain on food preference and food-matched visual-cue memory, in the presence or absence of a basolateral amygdala (BLA) lesion, has been evaluated using a novel innovative apparatus and protocol. Forty adult male Wistar rats were randomly divided into five groups (n = 8) as follows: control, pain, ibuprofen + pain, BLA lesion, BLA lesion + pain groups. Bilateral lesions of the BLA were produced by passing a current of 1.5 mA for 7 s. Pain was induced on the right hind paw of the rats by sub-plantar injection of 50 μl of 2.5% formalin. The animals were encountered with four different meals including wholemeal, wholemeal + sugar, white flour, and biscuit. Each test session consisted of six trials with inter-trial intervals of 15 min. The number of visits to each meal zone and port, the amount of time spent in each food zone and port, traveled distance in each food zone, food consumption per each visit and the total food consumption were recorded. The control group showed a high biscuit preference and low white flour preference. Rats suffering BLA lesion and rats in the BLA lesion + pain group exhibited a shifted preference curve. They had a bias toward eating wholemeal + sugar rather than white flour and biscuit. This group also showed an impaired spatial memory. In conclusion, our findings suggest that the BLA may be involved in pain-induced food preference and food-matched visual-cue memory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are multiple factors including neurotransmitter levels, hormones, post-ingestion experiences, age and environmental factors that influence an animal's food preference. The brain manages food intake by means of a rich interplay of different internal and external state and trait-related signals (Smeets et al. 2012). The most important forebrain structures involved in food preference mechanisms are the nuclear groups of the amygdala, namely the basolateral (Wang et al. 2006) and central (Kemble and Schwartzbaum 1969) divisions. In rodents, many food preference-related signals such as gustatory and olfactory information directly or indirectly are received by the amygdala. The basolateral amygdala (BLA) receives gustatory information from the parabrachial nuclei, insular cortex and piriform cortex (Paré 2003). The neural circuits between the parabrachial nuclei and the amygdala mediate appetite suppression when animals are encountered with an unfavorable food. Actually, olfaction-related learning behavior requires a normal function of the BLA. In rats, electrolytic bilateral lesions in the central nucleus of the amygdala result in a significant decline in sweet preferences (Box and Mogenson 1975). However, Kemble et al. (1972) stated that the preference behavior of rats for a variety of saccharin and quinine solutions is not influenced by total amygdalectomy. It has also been indicated that rats suffering lesions in the basolateral amygdala show an increased preference for 25% sucrose solution (Rolls and Rolls 1973a). However, Siegel et al. (1987) reported that the chemical lesion of the BLA by ibotenic acid dramatically decreases sucrose solution consumption.
The amygdala is involved in pain-related emotional responses as well as food intake preferences. Through interactions with the cortical areas, it also contributes to cognitive aspects (Neugebauer 2015). Moreover, the amygdala has been found to have a dual effect (excitation/inhibition) on acute experimental pain responses (Ji and Neugebauer 2009). Pain seriously affects the daily activities, feeding behavior and quality of life in animals (Dueñas et al. 2016). There is a reciprocal interaction between pain and food reward and punishment behaviors (Becker et al. 2012). Interestingly, there is evidence that rewarding stimuli such as food, pleasurable music and odors and pain sensitivity influence each other. In the study by de la Puente et al., acute pain attenuated saccharin preference beyond the resolution of writhing behavior. The authors suggested that the changes in the expression of hedonic behavior, such as sweet taste preference, can be used as a more sensitive and translational model to evaluate analgesics (de la Puente et al. 2015). It has been shown that consumption of certain foods, especially high-calorie foods helps relieve pain (Anseloni et al. 2002; Kakeda et al. 2010) possibly by interaction with endogenous opioid system (Kracke et al. 2005) and the help of central pain processing pathways (Kakeda et al. 2010).
High levels of biochemical mediators including histamine (Tamaddonfard et al. 2008), prostaglandins (Kawabata 2011), opioids (Kapitzke et al. 2005), CGRP (Benemei et al. 2009) and neuropeptide Y (Hökfelt et al. 2007) released during inflammation and pain conditions have well-known effects on feeding behaviors. In both freely fed and food-deprived rabbits, histamine causes anorexia through the increased density of central H1 receptors (Kim 2012). H1 and H3 histamine receptors are crucial for the regulation of body weight and plasma triglycerides levels (Passani et al. 2011). Prostaglandins are also effective chemical compounds in feeding. The injection of prostaglandin E1, but not E2, in the medial and anterior hypothalamus in sheep led to a reduced spontaneous feeding. As a result, prostaglandins seem to be involved in the maintenance of energy balance (Baile et al. 1974).
Neuropeptide Y (NPY) is a highly conserved endogenous peptide, which has been implicated in both inflammatory and nociceptive effects (Solway et al. 2011). Moreover, NPY produces a pronounced stimulation of feeding in satiated rats (Gehlert 1999). The importance of endogenous opioids in feeding behavior has been shown in several studies (Reid 1985). Opioids are also involved in palatability and rewarding effects of foods (Gosnell and Levine 2009). Eating behavior is a complex response to different internal and external factors. Various stimuli including mechanical, metabolic and environmental ones may acutely influence energy intake. For example, in anorexia, changes of eating behavior during the disease may be related to the activation of a specific neuronal emergency circuit (Laviano et al. 2018).
The role of the BLA has already been investigated in food preference acquisition. Moreover, considering the interaction among brain regions, little is known about the effects of pain and a BLA lesion on pain-induced food preferences. The present study, however, did aim to provide information on the effect of pain and a BLA lesion on food preferences and food preference-related memory, using a novel protocol that may help acquire a new level of prominence in selection of the best medicine and improvement of treatments.
Methods
Subjects
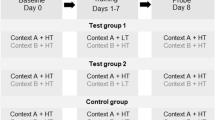
Forty adult male Wistar rats (200–250 g) were housed in a temperature-controlled room at 23 ± 1 °C, with a standard 12 h’ light/dark cycle. The animals were given free access to food (commercial standard rat chow) and water. The experimental procedures were approved by the Animal Research Ethics Committee of Shahid Bahonar University, Kerman, Iran (IR.UK.VETMED.REC.1398.018). The animals were randomly assigned into five experimental groups (n = 8), as follows: the control group, in which rats received no treatment. In pain group, the rats experienced formalin-induced inflammatory pain (Segawa et al. 2013). In ibuprofen + pain group, ibuprofen (10 mg/kg) was administered 30 min prior to formalin (Nesa et al. 2014). Rats in the BLA lesion group, received electrical stimulation to the BLA. Animals in BLA lesion + pain group received the formalin injection after the induction of a BLA lesion.
Surgery
Egg white (Raoul et al. 2007), as many other studies, was used to determine the size and shape of the lesions (Raoul et al. 2007). The white from a fresh hen’s egg was placed in a rectangular glass container and warmed in a water bath to 37 °C. The electrode set was attached to a sponge on the upper surface of the container and the cannula and electrode were inserted into the egg white. The transparency of the egg white and the glass container facilitates observation of changes in the size of the lesions over time.
The rats were anesthetized using a mixture of ketamine (100 mg/kg) and xylazine (2.5 mg/kg) and mounted onto the stereotaxic apparatus (Stoelting Co., USA). The skull was exposed and two small holes were drilled according to the Paxinos and Watson's rat brain atlas (AP = – 2.80, ML = ± 5, and DV = 8.6 mm from bregma). A bipolar electrode (Teflon-coated stainless steel, 0.125 mm diameter, Advent Co., UK) was inserted in the BLA and electric lesions were produced by passing a 1.5 mA current of 7 s duration (Korz and Frey 2005), finally, 1-week recovery period was considered and the animals were housed individually in clear plastic cages before the behavioral tests. At the end of the experiment, brain injury was estimated based on the results of Nissl staining. Lesion verification was done via a light microscopy and lesions were reconstructed based on rat brain atlas. Data were removed from analyses when the size or location of the lesion was not appropriate.
Pain induction
Pain was induced by subcutaneous injection of formalin (50 µl, 2.5%) to the right hind paw of rats using a microsyringe with a 27-gauge needle. Formalin was injected before the fifth trial. The behavioral responses consisted of two distinct periods, an early phase lasting the first 5 min; and a late phase lasting from 20 to 30 min following the injection of formalin (Kolesnikov et al. 2004).
Food type
In the present study, we used a novel innovative test apparatus and protocol that needed to be validated by help of a previous study. For this purpose, we applied the dietary pattern used in the study by Barnett and Spencer (1953). However, we divided the meals into two main classifications including sugary (whole meal + sugar and biscuit) and simple (whole meal and white flour) diets (Table 1). The foods were chopped into the small portions of the size nearest to 0.5 cm in maximum dimension. For preventing familiar effect, all of the above-mentioned diets were mixed with powdered ordinary laboratory rat food (50 percent).
Behavioral apparatus
A black plexiglass square apparatus (60 cm long × 60 cm wide × 30 cm high and a 60 cm × 60 cm floor), almost like an open field apparatus, was used. The floor was imaginary divided into nine identical squares. The device was also equipped with an electronic sensor underneath. Two types of load sensors from Avia Semiconductor’s patented technology (P. R. China) are being used: the first one (Model: YZC-133, rated load: 0.1 g/0.00022 lb–3 kg/6.61 lb, material: aluminum, weight: 32 g) has been used to indicate the changes in water and food consumption. The other one, with a rated load of 0.1–2 kg, has been applied to detect the location of the rats. There are three small ports in each interior surface of the box for access to solid material, liquid and odor. Moreover, there was a specific geometric visual-cue (50 cm × 10 cm) on each side. A food container, a water bottle with a load sensor underneath, and a small box for odorous compound were located on the external side of the apparatus. The external side was also equipped with a monitoring system (LCD) connected to a computer, and an SD card for data storage. Microcontroller atmega32/code vision and Visual studio/Vb. Net/for food and water measurement was used to capture and process the data.
The data of four middle squares that contain the ports (zones 2, 4, 6 and 8) presents the preference for the content of the nearest container. Four corner squares (1, 3, 7 and 9 squares) are considered for resting. The central square (squares 5) has been considered as animal release site (Fig. 1a). Specific visual cues were also incorporated. The number of visits to each meal zone and port, the amount of time spent in each food zone and port, traveled distance in each food zone, food consumption per each visit and the total food consumption were recorded.
a Overlook of rat preference meter apparatus. b Time line for experimental procedures: (A) The procedure included two sessions of habituation period lasting 15 min with a 4-h interval between. The ports were open while there was no food in the containers. (B) In each experimental session, the animals were exposed to four 12-h-acquisition phases and five 12-h-intertrial intervals and two 12-h-post acquisition phases
Procedure
After the recovery period (7 days), food-deprived rats (12 h) were tested by a habituation trial and another six trial protocols, as follows:
Habituation test (15 min/day): 2 days prior to the test, the rats were allowed to freely explore all areas of the apparatus that was free of food and water. If the animal spent more time in a specific area or did not show exploratory behavior, it would be excluded from the experiment.
The first trial: while the container in square 2 was provided by 10 g solid wholemeal, the rats were released in the central square (#5) and allowed to have access to the food within 12-h period.
The second trial: after removing the wholemeal and cleaning the apparatus, the animal was released in the central square while wholemeal + sugar was put in the container in square 4 and the feeding behavior was evaluated for 12 h.
The third and fourth trials: similar to the previous procedures, the third and fourth trials were conducted with white flour (the container in the square 6) and biscuit (the container in the square 8), respectively.
The fifth trial: all different diets were simultaneously accessible in their previous mentioned containers.
The sixth trial: during the sixth trial, there was no food in the containers. This trial was design based on our hypothesis that animal food preference-related behavior is influenced by his previous post-ingestion experience and memory (Fig. 1b).
Histology
At the end of the experiment, the animals with the BLA lesion were euthanized under a deep anesthesia. Thereafter, the brains were removed and fixed in 10% formalin. Paraffin-embedded sections of 20 μm thickness were then stained with Nissl to confirm the lesion locations by microscopic inspection (Li et al. 2013) (Fig. 2).
Statistical analysis
All data are expressed as mean ± standard error of mean (SEM). The behavioral data were compared between the groups using independent sample t tests and ANOVA (one way and two way) followed by post hoc tests for multiple comparisons. p value less than 0.05 was considered to be statistically significant.
Results
Time-course and the number of paw licks after formalin-induced pain
The time course and the number of licks are shown in Fig. 3a, b, respectively. The BLA lesion + pain and ibuprofen + pain groups showed significant decreases in the number of licks and licking time in comparison with the pain group in both phases of the test (p < 0.001).
Food consumption
Figure 4a shows the amount of food consumption in rats. The order of food consumption in the control group was biscuit, wholemeal + sugar, wholemeal and white flour, respectively. However, the pain group has indicated the following order of preferences: wholemeal + sugar, biscuit, wholemeal and white flour, respectively.
a The differences in food consumptions (in grams) and the order of food preferences among the groups. *p < 0.05, **p < 0.01 and ***p < 0.001 versus control groups, #p < 0.05 and ###p < 0.001 as compared with pain group. b The differences between the consumption of sugary (wholemeal + sugar + biscuit meal) and simple (wholemeal + white flour) diets in different study groups *p < 0.05 and ***p < 0.001 versus simple diet (n = 8)
The preference order for the BLA lesion group was wholemeal + sugar, white flour, wholemeal, biscuit, respectively, while the order in BLA-lesion + pain group was wholemeal + sugar, wholemeal, biscuit, white flour, respectively. The pain group showed significant increased preferences for wholemeal + sugar and wholemeal (p < 0.001) than the other meals as compared with the control group. The BLA-lesion group had the largest amount of white flour consumption (p < 0.001), while the BLA lesion + pain rats consumed the least amount of biscuit as compared with the control group (p < 0.001). The BLA lesion + pain group had different amount of wholemeal, wholemeal + sugar and biscuit consumptions as compared with the pain group (Fig. 4a). As shown in Fig. 4b, the rats in control, pain, ibuprofen + pain and BLA lesion + pain groups showed more preference to sugary diet (wholemeal + sugar + biscuit meal) rather than the simple one (wholemeal + white flour) (p < 0.001).
Table 2 shows that in the pain, BLA lesion and BLA lesion + pain groups, the order of food preferences in the fifth trial is different from that of the first four trials. By comparing the first four trial data versus that of the fifth trial, it can be noticed that high-calorie foods exhibit more changes. The comparison of food preferences orders and food consumptions between the two phases of the study, the first four day- and the 5th-day trials, indicated that the pain group consumed more food than the BLA lesion + pain and control groups. While white flour was the least preferred meal in pain group, BLA lesion + pain rats ate almost equal amounts of white flour and biscuit as the least preferred meals, indicating the changes in food preferences. Moreover, throughout both phases of the trial, the animals in the pain group, but not in the BLA lesion and BLA lesion + pain groups, consumed a significantly greater amount of food. Mean total food intake in the fifth trial for animals suffering pain is 27.7 ± 3. However, it is 17.1 ± 2 for animals in BLA lesion + pain group. Regarding the mean comparisons of the total food intake between the two phases of the study, the BLA lesion group is the only exception. The rats in this group consumed less food in the first-4 days (18.8 ± 1) compared to that of the 5th day (22.2 ± 1) (Table 2).
According to the data from the first four trials (when the meals were accessible one after the other), the rats with BLA lesions showed markedly reduced total food intake compared to the control animals. They also consumed smaller amounts of wholemeal and white flour. Moreover, in the fifth trial (when all the different meals were accessible simultaneously), the BLA lesion led to a growing consumption of total food intake compared to the control animals. In the fifth trial, the lesioned rats ate more wholemeal and white flour in comparison with that of the same animals in the first four trials. Interestingly, in the fifth trial, the BLA lesion caused rats to significantly consume more wholemeal, wholemeal + sugar and white flour, but less biscuit, in comparison with the control animals. This confirms that the food preference order in the fifth trial is different from that of the sixth trial. Taken together, BLA lesion seems to cause impairment in food-matched visual-cue memory.
In the first four trials, BLA lesion accompanied by pain led to decreases in total food intake and in the amount of wholemeal, wholemeal + sugar, and biscuit consumptions compared to that of the control group. In the fifth trial, this group showed increased consumption of wholemeal, wholemeal + sugar and white flour, but not biscuit, compared to the control group. The significant differences between the data obtained from the fifth sixth trials suggest memory impairment in this group.
In both phases of the trials, pain group demonstrated an increased food intake compared to that of the control group. However, in the fifth trial, they consumed significantly smaller amounts of food than in the first four trials. In comparison with the control animals, the pain group consumed significantly more amounts of wholemeal, wholemeal + sugar and white flour in both phases of the study. Moreover, they showed significant decreases in the consumption of wholemeal, white flour, and biscuit in the fifth trial in comparison with the first four trials. Surprisingly, there were no differences between the two phases of the trial regarding the time spent and the number of visits for the preferred food. Taken together, these data indicate that unlike the other types of memory, there are no significant changes in food-matched visual-cue due to pain stimulus.
Number of visits
Statistical analysis of the data showed significant differences among control, pain and BLA lesion + pain groups regarding the number of visits to the food ports and zones. As compared with the control rats, the pain and BLA lesion + pain groups showed an increase in the number of visits to the wholemeal + sugar port (p < 0.001). The rats in the pain group also showed significantly increased visits to the wholemeal and wholemeal + sugar zones as compared to the control animals (p < 0.001). As compared with the control rats, the BLA-lesion rats showed increases in the number of visits to wholemeal, wholemeal + sugar and white flour zones. Moreover, there were significant differences in the number of visits to wholemeal, wholemeal + sugar and biscuit ports and zones between BLA lesion + pain and pain groups (Fig. 5a, b).
Time spent
As shown in Fig. 6, while the BLA lesion + pain group spent significantly (p < 0.001) more time in the wholemeal + sugar port and zone, the BLA lesion group spent significantly (p < 0.001) more time in white flour port and zone compared with the control animals. In addition, as compared with the control rats, the pain group spent less time in white flour and biscuit ports (p < 0.001).
Furthermore, compared to the animals in the pain group, the BLA-lesion + pain affected rats spent significantly more time in the wholemeal + sugar port and zone (p < 0.001). Moreover, the BLA-lesion group and ibuprofen-treated animals spent significantly more time (p < 0.001) in the white flour port and biscuit zone in comparison to the animals with pain (Fig. 6a, b).
Mean distance traveled scores
The distance traveled in wholemeal, wholemeal + sugar, white flour and biscuit meal-related zones in either of the studied groups is significantly different from the control group.
The BLA-lesion group exhibited a significantly increased distance traveled in the wholemeal + sugar and white flour zones compared to the control group (p < 0.001). In addition, the animals in the BLA-lesion group traveled significantly longer distances in all the meal zones compared to the rats in the pain group (p < 0.001) (Fig. 7).
The sixth trial or food-matched visual-cue memory
Comparing the ordering results of the fifth and sixth trials indicated that biscuit was the most preferred choice of the rats in the control and ibuprofen + pain groups in both trials, while the preference order was different between them. Regarding the number of visits to and time spent in each zone, there were no significant differences with empty and filled containers in the control and pain groups. The BLA-lesion group exhibited higher preference for wholemeal + sugar and white flour in the fifth trial, but not in the sixth trial. Wholemeal + sugar was the highest preference among the animals in the BLA lesion + pain group in both trials. The order of food preferences in the fifth trial in the BLA-lesion and BLA lesion + pain groups is significantly different from that of the sixth trial (*p < 0.05, **p < 0.01 and***p < 0.001) (Fig. 8a, b).
Discussion
Here, we evaluated the effects of pain on food preferences in rats with or without BLA lesions by using an innovative test apparatus and protocol. In the present study, biscuit was the most preferred and white flour was the least preferred food by animals in the control and ibuprofen groups. This finding is similar to that of a previous study by Barnett and Spencer who used a traditional simple method (Barnett and Spencer 1953). However, by help of a new methodology, the amount of food eaten by the rat, the number of visits to and time spent in different ports and zones, the distance traveled in the zones; and food-matched visual-cue related learning and memory could all be simultaneously assessed in the present study.
Biscuit contains the highest levels of total fat, calories and protein out of all four choices. Regarding the carbohydrate content, biscuit is also in the second ranking. Its selection as the first preference can be at least partially attributed to the foraging theory that predicts that the decisions that maximize energy per unit time and thus deliver the highest payoff will be selected for and persist (Inglis et al. 1996). However, wholemeal + sugar was the highly preferred diet in rats with pain. The rats received BLA lesions preferred wholemeal + sugar over biscuit, while the BLA lesion + pain group showed a significantly preference for wholemeal + sugar. Comparing the data from the fifth and sixth trials shows that pain group has larger amount of food consumption as compared with the BLA lesion + pain and control groups in both phases and this may be duo to more activity and less rest time in animals with reduced pain (Jung et al. 2010). While white flour was the least preferred meal in pain group, BLA lesion + pain rats ate almost equal amounts of white flour and biscuit as the least preferred meals, indicating the changes in food preferences. In order to evaluate the effects of pain reduction on animal’s behavior, ibuprofen was administrated. Compared to the pain group, the use of ibuprofen led to the outcomes similar to that of the control group. Using different food items including chow, cauliflower, sultanas, potato, greens and orange peel, previous studies have suggested that the BLA plays a significant role in food selection in rats (Rolls and Rolls 1973b). Furthermore, the amygdala, including the BLA, is well known to be relevant to pain processes as well as pain-related memory (Li et al. 2013; Neugebauer 2015). The amygdala lesions dramatically prevent development and maintenance of pain (Li et al. 2013). Actually, the effects of amygdala on pain and pain-induced behaviors are dependent on how the stimulus influences the functional activity of the amygdala (Ji and Neugebauer 2009; Lee et al. 2013). The BLA consists of the neurons that respond preferentially to noxious stimuli (Ji et al. 2010). The amygdala also contributes to pain-related decision-making through prefrontal cortical deactivation (Ji et al. 2010). In this study, pain reduction in rats with a BLA lesion may be associated with the amygdala connectivity of pain relevant regions (Li et al. 2013).
The animals in the pain group showed higher sweet preference rather than the BLA lesion rats which exhibited the most consumption of white flour, maybe due to the BLA-lesion induced pain inhibition. Actually, a reciprocal interaction seems to be between nociception and brain regions involved in the control of food intake. A relationship between consumption of palatable diet and pain endogenous central pain control mechanisms has already been indicated (Garzón et al. 1983; Smeets et al. 2012; Nuseir et al. 2017). Multiple investigations have revealed that endogens opioids play a regulatory role in the control of feeding behavior (Bodnar 2004). During the fifth trial, the order of food consumption in the pain group was wholemeal + sugar, biscuit, wholemeal and white flour, respectively. Sugary compounds may exert modulatory effects on nociceptive signals (Drewnowski et al. 2012). However, the BLA lesion + pain group has indicated the following order of preferences: wholemeal + sugar, wholemeal, biscuit meal and white flour, respectively. The difference in the orders can be due to the lower pain score in BLA lesion + pain group rather than the pain group.
Nociceptive conditions lead to restlessness and subsequent increased activity, energy expenditure and calorie consumption (Choi et al. 2014). Biscuit has more calories, total fat and protein content than the other meals. It has been shown that animals have a great tendency to eat high-calorie (biscuit meal and wholemeal + sugar), high-fat (biscuit meal, wholemeal and wholemeal + sugar) and high-protein (biscuit meal, wholemeal and wholemeal + sugar) foods. Pain is also involved in behavioral and neural characteristics of conditioned taste aversion and preference (Yamamoto and Ueji 2011).
The BLA is a major area for odor–taste association and preference learning (Yamamoto and Ueji 2011). It is also involved in behavioral and neural characteristics of conditioned taste aversion and preference (Yamamoto and Ueji 2011). The BLA is also involved in eating/drinking-related experiences (Rolls and Rolls 1973a) and food preferences (Borsini and Rolls 1984).
Due to extremely strong olfactory sensitivity, odor–taste association and preference learning have a crucial role in food selection in rats (Desgranges et al. 2010). So, in the present study, despite adding and mixing of the ordinary laboratory rat food to the studied meals, odor–taste association and preference learning may have relative effects on food consumption and order of preferences.
The direct projection of nociceptive neurons to various brain areas including the limbic system and the hypothalamus (Thompson and Neugebauer 2017) leads to the expectation that pain may affect food preferences. It has been indicated that neuropathic pain diminishes some forms of reward and changes sweet taste preferences or food rewards (Cooper and Turkish 1989). However, studies have led to controversial results (Amorim et al. 2014). In the study by Small and Apkarian, there were no significant differences in mean pleasantness/unpleasantness ratings for each of the sweet, sour, salty and bitter stimuli between the chronic back pain and control groups (Small and Apkarian 2006). Both humans and animals normally prefer sweet and salty tasting over sour and bitter substances (Inui-Yamamoto et al. 2017).
Food composition and post-ingestive effects are factors influencing food preferences. Chemical compounds in the food can affect food behaviors and food preferences through the gut–brain axis (Lyte 2018). Here, we used various meal compositions with different degrees of sweetness. It seems that sweetness is a major factor in the development of food preferences. In the present study, biscuit and wholemeal + sugar were the sweetest. Food preferences may also be affected by the amount of calories consumed. Here, the order of calorie content was biscuit, wholemeal + sugar, wholemeal and white flour, respectively.
Applying a different study protocol, Rolls and Rolls (1973b) concluded that the amygdala plays an important role in preferences for a novel versus a familiar food and in learning that the ingestion of a food is associated with sickness (Rolls and Rolls 1973b). In the current study protocol, the animals were familiarized with the different study meals within the first four trials. Moreover, enough time was considered for the rats to experience the post-ingestion effects of the studied foods.
It has been indicated that access to different types of food results in an increase in overall food and calorie intake in comparison with the situation that only one type of food is accessible to animals (Martire et al. 2013). However, regarding the mean comparisons of the total food intake between the two phases of the present study, the BLA lesion group is the only exception. The rats in this group consumed less food in the first-4 days (when the meals were accessible one after the other) compared to that of the 5th day (when all the different meals were accessible simultaneously). Compared to the first four trials, the BLA lesion rats in the fifth trial consumed more of all the study foods except biscuit. However, pain seems to have an inhibitory effect on this result.
The basolateral amygdala has a fundamental role in emotion processing and induction of neuropsychiatric aspects of pain (Maren 1999). However, there have been no reports of rats suffering BLA lesion plus pain regarding food preferences. Here, the food preference order in the fifth trial in rats suffering a BLA lesion was different from that of the sixth trial. Taken together, a BLA lesion seems to cause an impairment in food-matched visual-cue memory. Moreover, the other related data including the number of visits, the time spent, the distance traveled, and the results associated with the food-matched visual-cue memory were also statistically significantly different between the pain and BLA lesion + pain groups.
Food selection is influenced by the post-ingestion consequences (Benoit et al. 2010). The hippocampus, amygdala and prefrontal cortex are the main areas that help animals effectively learn and memorize the post-ingestion effects of foods (Benoit et al. 2010). Our data suggest that the animals in the pain group have a high tendency to consume wholemeal + sugar. They also showed more food intake than all other groups. These effects may be due to the well-known analgesic efficacy of sweet-tasting substances (Harrison et al. 2010) and pain-induced restlessness and hyperactivity (Smeester et al. 2017). Surprisingly, lesions of the ventromedial hypothalamus that help control eating behavior negatively affect sweet-taste-induced analgesic effects (Solway et al. 2011).
In pain conditions, some brain systems that control eating are affected by the substances that are released by central and peripheral tissues such as endogenous opioids, neuropeptide Y, substance P, histamine, prostaglandins, CGRP (Schou et al. 2017). Opioid circuitry in the nucleus accumbens and ventral pallidum has been reported to mediate taste-reactivity responses to palatable events, and regarding reward. These two areas have a significant connection with the basolateral amygdala (Wassum et al. 2009) Involvement of enkephalins and endorphins in the hedonics of feeding has already been indicated (Skoubis et al. 2005). Administration of naltrexone, an opioid antagonist, significantly deviated the rat’s preference for the chocolate-coated cookies to standard chow pellets (Cooper and Turkish 1989). So, pain-induced deviation in food preferences may occur secondary to pain-induced endogenous opioid release. It is necessary to carry out supplementary studies to further clarify this issue.
Pain has also been shown to elevate the levels of cyclooxygenase-2 (COX-2) and prostaglandin E2 (PGE2) in the central nervous system (CNS). Moreover, the amygdala is known to play a role in nociception, particularly in inflammation-evoked pain that is associated with increased levels of COX-2 and PGE2. These effects may be mediated by an opiate-induced decrease in the amygdala signaling.
The amygdalar histaminergic system is modulated by oral somatic sensation and palatability of foods (Ishizuka et al. 2010). Various types of histamine receptors in the BLA have been described and it has been suggested that they may play a role in the consolidation of different type of tasks. Also, histamine depletion in the hippocampus or basolateral amygdala impairs long-term memory and the both brain structures receive important glutamatergic and histaminergic innervation, suggesting that these neurotransmitters might be involved as coding signals to modulate memory and learning mechanisms (Álvarez and Ruarte 2004). CGRP, alone or through interacting with corticotropin-releasing factor in the amygdala, contributes to pain control and pain-related behaviors (Neugebauer et al. 2009; Han et al. 2010). Morover, intra-BLA administration of CGRP in rats led to the anti-nociceptive effects (Li et al. 2008).
The results of the sixth trial indicated that the rats with pain mostly visited the non-preferred ports and zones. This might be due to pain-related memory impairment (Kooshki et al. 2017) and pain-induced anxiety (Parent et al. 2012). We might, therefore, reasonably doubt that such pain-related psychological issues induce changes in food preference patterns.
Research has shown that pain impairs working memory (Bushnell et al. 2015) and, as a result, rats’ ability to find the location of preferred food containers may be damaged. Yet little understood question is what are the reasons for such food preferences order in rats with pain? Is it related to learning and memory impairments or food preferences changes or both of them? Here, despite the first four trials and the sixth trial, the rats had access to all kinds of meals within the fifth trial, which they had the opportunity to perceive the odors and the locations of all foods. So, changes in food preferences have occurred regardless of whether the subjects had pain-induced memory impairments. For illustration, a comparison of the fifth with the sixth trial shows what wholemeal + sugar was the most preferred meal for ibuprofen-treated rats in the fifth trial, while it was the least preferred one in the sixth trial.
This study has some limitations that could be addressed in future. First, we needed to validate our innovative test apparatus and protocol by help of a previous study. Therefore, we were not free to choose the foods. For this purpose, we applied the dietary pattern used in the study by Barnett and Spencer (1953). The second limitation concerns the lack of a distinct odor difference among the meals.
Conclusions
Using an innovative multi-purpose protocol, we found that chemically induced pain may change the food preferences and impairs food-matched visual-cue-dependent memory in rats. Moreover, the BLA appears to play an important role in such processes, possibly by involvement of neuromodulators such as endogenous opioids or the reciprocal relationships between brain regions involved in pain regulation and the BLA. Additional investigations are needed to clarify the exact underlying mechanisms.
Availability of data and material
The data and materials for all experiments are available upon request from the corresponding author and will be made available in a data repository prior to the publication.
References
Álvarez EO, Ruarte MB (2004) Glutamic acid and histamine-sensitive neurons in the ventral hippocampus and the basolateral amygdala of the rat: functional interaction on memory and learning processes. Behav Brain Res 152:209–219
Amorim D, David-Pereira A, Pertovaara A, Almeida A, Pinto-Ribeiro F (2014) Amitriptyline reverses hyperalgesia and improves associated mood-like disorders in a model of experimental monoarthritis. Behav Brain Res 265:12–21
Anseloni VC, Weng H-R, Terayama R et al (2002) Age-dependency of analgesia elicited by intraoral sucrose in acute and persistent pain models. Pain 97:93–103
Baile C, Martin F, Forbes J, Webb R, Kingsbury W (1974) Intrahypothalamic injections of prostaglandins and prostaglandin antogonists and feeding in sheep. J Dairy Sci 57:81–88
Barnett S, Spencer MM (1953) Experiments on the food preferences of wild rats (Rattus norvegicus Berkenhout). Epidemiol Infect 51:16–34
Becker S, Gandhi W, Schweinhardt P (2012) Cerebral interactions of pain and reward and their relevance for chronic pain. Neurosci Lett 520:182–187
Benemei S, Nicoletti P, Capone JG, Geppetti P (2009) CGRP receptors in the control of pain and inflammation. Curr Opin Pharmacol 9:9–14
Benoit SC, Davis JF, Davidson T (2010) Learned and cognitive controls of food intake. Brain Res 1350:71–76
Bodnar RJ (2004) Endogenous opioids and feeding behavior: a 30-year historical perspective. Peptides 25:697–725
Borsini F, Rolls E (1984) Role of noradrenaline and serotonin in the basolateral region of the amygdala in food preferences and learned taste aversions in the rat. Physiol Behav 33:37–43
Box BM, Mogenson G (1975) Alterations in ingestive behaviors after bilateral lesions of the amygdala in the rat. Physiol Behav 15:679–688
Bushnell M, Case L, Ceko M et al (2015) Effect of environment on the long-term consequences of chronic pain. Pain 156:S42
Choi KW, Somers TJ, Babyak MA, Sikkema KJ, Blumenthal JA, Keefe FJ (2014) The relationship between pain and eating among overweight and obese individuals with osteoarthritis: an ecological momentary study. Pain Res Manag 19:e159–e163
Cooper SJ, Turkish S (1989) Effects of naltrexone on food preference and concurrent behavioral responses in food-deprived rats. Pharmacol Biochem Behav 33:17–20
de la Puente B, Romero-Alejo E, Vela JM, Merlos M, Zamanillo D, Portillo-Salido E (2015) Changes in saccharin preference behavior as a primary outcome to evaluate pain and analgesia in acetic acid-induced visceral pain in mice. J Pain Res 8:663
Desgranges B, Ramirez-Amaya V, Ricaño-Cornejo I, Lévy F, Ferreira G (2010) Flavor preference learning increases olfactory and gustatory convergence onto single neurons in the basolateral amygdala but not in the insular cortex in rats. PLoS ONE 5:e10097
Drewnowski A, Mennella JA, Johnson SL, Bellisle F (2012) Sweetness and food preference. J Nutr 142:1142S-1148S
Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I (2016) A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res 9:457
Garzón J, Sánchez-Blázquez P, Höllt V, Lee N, Loh H (1983) Endogenous opioid peptides: comparative evaluation of their receptor affinities in the mouse brain. Life Sci 33:291–294
Gehlert D (1999) Role of hypothalamic neuropeptide Y in feeding and obesity. Neuropeptides 33:329–338
Gosnell B, Levine A (2009) Reward systems and food intake: role of opioids. Int J obes 33:54–58
Han JS, Adwanikar H, Li Z, Ji G, Neugebauer V (2010) Facilitation of synaptic transmission and pain responses by CGRP in the amygdala of normal rats. Mol Pain. https://doi.org/10.1186/1744-8069-6-10
Harrison D, Bueno M, Yamada J, Adams-Webber T, Stevens B (2010) Analgesic effects of sweet-tasting solutions for infants: current state of equipoise. Pediatrics 126:894–902
Hökfelt T, Brumovsky P, Shi T, Pedrazzini T, Villar M (2007) NPY and pain as seen from the histochemical side. Peptides 28:365–372
Inglis I, Shepherd D, Smith P, Haynes P, Bull D, Cowan D, Whitehead D (1996) Foraging behaviour of wild rats (Rattus norvegicus) towards new foods and bait containers. Appl Anim Behav Sci 47:175–190
Inui-Yamamoto C, Yamamoto T, Ueda K, Nakatsuka M, Kumabe S, Inui T, Iwai Y (2017) Taste preference changes throughout different life stages in male rats. PLoS ONE 12:e0181650
Ishizuka T, Sako N, Murotani T, Morimoto A, Yamatodani A, Ohura K (2010) The effect of hardness of food on amygdalar histamine release in rats. Brain Res 1313:97–102
Ji G, Neugebauer V (2009) Hemispheric lateralization of pain processing by amygdala neurons. J Neurophysiol 102:2253–2264
Ji G, Sun H, Fu Y, Li Z, Pais-Vieira M, Galhardo V, Neugebauer V (2010) Cognitive impairment in pain through amygdala-driven prefrontal cortical deactivation. J Neurosci 30:5451–5464
Jung AP, Curtis TS, Turner MJ, Lightfoot JT (2010) Physical activity and food consumption in high-and low-active inbred mouse strains. Med Sci Sports Exerc 42:1826
Kakeda T, Ogino Y, Moriya F, Saito S (2010) Sweet taste-induced analgesia: an fMRI study. NeuroReport 21:427–431
Kapitzke D, Vetter I, Cabot PJ (2005) Endogenous opioid analgesia in peripheral tissues and the clinical implications for pain control. Ther clin risk manage 1:279
Kawabata A (2011) Prostaglandin E2 and pain—an update. Biol Pharm Bull 34:1170–1173
Kemble ED, Levine MS, Gregoire K, Koepp K, Thomas TT (1972) Reactivity to saccharin and quinine solutions following amygdaloid or septal lesions in rats. Behav Biol 7:503–512
Kemble ED, Schwartzbaum J (1969) Reactivity to taste properties of solutions following amygdaloid lesions. Physiol Behav 4:981–985
Kim SF (2012) Animal models of eating disorders. Neuroscience 211:2–12
Kolesnikov Y, Cristea M, Oksman G, Torosjan A, Wilson R (2004) Evaluation of the tail formalin test in mice as a new model to assess local analgesic effects. Brain Res 1029:217–223
Kooshki R, Abbasnejad M, Esmaeili-Mahani S, Raoof M (2017) The modulatory role of orexin 1 receptor in CA1 on orofacial pain-induced learning and memory deficits in rats. Basic Clin Neurosci 8:213
Korz V, Frey JU (2005) Bidirectional modulation of hippocampal long-term potentiation under stress and no-stress conditions in basolateral amygdala-lesioned and intact rats. J Neurosci 25:7393–7400
Kracke GR, Uthoff KA, Tobias JD (2005) Sugar solution analgesia: the effects of glucose on expressed mu opioid receptors. Anesth Analg 101:64–68
Laviano A, Di Lazzaro L, Koverech A (2018) Changes in eating behavior, taste and food preferences and the effects of gastrointestinal hormones. Clin Nutr Exp 20:65–70
Lee MC, Ploner M, Wiech K et al (2013) Amygdala activity contributes to the dissociative effect of cannabis on pain perception. PAIN® 154:124–134
Li N, Liang J, Fang C-Y, Han H-R, Ma M-S, Zhang G-X (2008) Involvement of CGRP and CGRPl receptor in nociception in the basolateral nucleus of amygdala of rats. Neurosci Lett 443:184–187
Li Z, Wang J, Chen L, Zhang M, Wan Y (2013) Basolateral amygdala lesion inhibits the development of pain chronicity in neuropathic pain rats. PLoS ONE 8:e70921
Lyte JM (2018) Eating for 3.8 × 1013: examining the impact of diet and nutrition on the microbiota-gut-brain axis through the lens of microbial endocrinology. Front Endocrinol. https://doi.org/10.3389/fendo.2018.00796
Maren S (1999) Neurotoxic basolateral amygdala lesions impair learning and memory but not the performance of conditional fear in rats. J Neurosci 19:8696–8703
Martire SI, Holmes N, Westbrook RF, Morris MJ (2013) Altered feeding patterns in rats exposed to a palatable cafeteria diet: increased snacking and its implications for development of obesity. PLoS ONE 8:e60407
Nesa L, Munira S, Mollika S, Islam M (2014) Evaluation of analgesic, anti-inflammatory and CNS depressant activities of methanolic extract of Lawsonia inermis barks in mice. Avicenna J Phytomed 4:287
Neugebauer V (2015) Amygdala pain mechanisms. Pain control. Springer, Berlin, pp 261–284
Neugebauer V, Galhardo V, Maione S, Mackey SC (2009) Forebrain pain mechanisms. Brain Res Rev 60:226–242
Nuseir KQ, Alzoubi KH, Alhusban A, Bawaane A, Al-Azzani M, Khabour OF (2017) Sucrose and naltrexone prevent increased pain sensitivity and impaired long-term memory induced by repetitive neonatal noxious stimulation: role of BDNF and β-endorphin. Physiol Behav 179:213–219
Paré D (2003) Role of the basolateral amygdala in memory consolidation. Prog Neurobiol 70:409–420
Parent AJ, Beaudet N, Beaudry H et al (2012) Increased anxiety-like behaviors in rats experiencing chronic inflammatory pain. Behav Brain Res 229:160–167
Passani MB, Blandina P, Torrealba F (2011) The histamine H3 receptor and eating behavior. J Pharmacol Exp Ther 336:24–29
Raoul S, Leduc D, Vegas T et al (2007) Deep brain stimulation electrodes used for staged lesion within the basal ganglia: experimental studies for parameter validation. J Neurosurg 107:1027–1035
Reid LD (1985) Endogenous opioid peptides and regulation of drinking and feeding. Am J Clin Nutr 42:1099–1132
Rolls BJ, Rolls ET (1973a) Effects of lesions in the basolateral amygdala on fluid intake in the rat. J Comp Physiol Psychol 83:240
Rolls ET, Rolls BJ (1973b) Altered food preferences after lesions in the basolateral region of the amygdala in the rat. J Comp Physiol Psychol 83:248
Schou WS, Ashina S, Amin FM, Goadsby PJ, Ashina M (2017) Calcitonin gene-related peptide and pain: a systematic review. J Headache Pain 18:34
Segawa T, Miyakoshi N, Kasukawa Y, Aonuma H, Tsuchie H, Shimada Y (2013) Analgesic effects of minodronate on formalin-induced acute inflammatory pain in rats. Biomed Res 34:137–141
Siegel A, Joyner K, Smith G (1987) Amygdaloid-lesion decrease sham feeding of sucrose. International journal of obesity, vol 11. Stockton Press Houndmills, Basingstoke, pp 22–22
Skoubis P, Lam H, Shoblock J, Narayanan S, Maidment N (2005) Endogenous enkephalins, not endorphins, modulate basal hedonic state in mice. Eur J Neurosci 21:1379–1384
Small DM, Apkarian AV (2006) Increased taste intensity perception exhibited by patients with chronic back pain. Pain 120:124–130
Smeester BA, Lee J-H, Beitz AJ (2017) Influence of social interaction on nociceptive-induced changes in locomotor activity in a mouse model of acute inflammatory pain: use of novel thermal assays. Brain Res Bull 134:47–54
Smeets PA, Charbonnier L, van Meer F, van der Laan LN, Spetter MS (2012) Food-induced brain responses and eating behaviour. Proc Nutr Soc 71:511–520
Solway B, Bose SC, Corder G, Donahue RR, Taylor BK (2011) Tonic inhibition of chronic pain by neuropeptide Y. Proc Natl Acad Sci 108:7224–7229
Tamaddonfard E, Khalilzadeh E, Hamzeh-Gooshchi N, Seiednejhad-Yamchi S (2008) Central effect of histamine in a rat model of acute trigeminal pain. Pharmacol Rep 60:219
Thompson JM, Neugebauer V (2017) Amygdala plasticity and pain. Pain research & management 2017
Wang Y, Fontanini A, Katz DB (2006) Temporary basolateral amygdala lesions disrupt acquisition of socially transmitted food preferences in rats. Learn Mem 13:794–800
Wassum K, Ostlund S, Maidment N, Balleine B (2009) Distinct opioid circuits determine the palatability and the desirability of rewarding events. Proc Natl Acad Sci 106:12512–12517
Yamamoto T, Ueji K (2011) Brain mechanisms of flavor learning. Front Syst Neurosci 5:76
Acknowledgements
This work was supported by funds from Shahid Bahonar University of Kerman.
Funding
This study was financially supported by Shahid Bahonar University of Kerman, Kerman, Iran (Grant number: 98.6).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study. MA designed the study protocol. MZ collected the data. SEM carried out the statistical analyses. MA and VS and MR drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest to declare.
Ethical approval
All experiments were executed in accordance with the guidelines on ethical standards for investigation in animals in Shahid Bahonar University of Kerman, Kerman, Iran (IR.UK.VETMED.REC.1398.018).
Additional information
Communicated by Sreedharan Sajikumar.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zamyad, M., Abbasnejad, M., Esmaeili-Mahani, S. et al. Pain influences food preference and food-related memory by activating the basolateral amygdala in rats. Exp Brain Res 239, 79–93 (2021). https://doi.org/10.1007/s00221-020-05961-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-020-05961-1