Abstract
Impaired corticomotor function arising from altered intracortical and corticospinal pathways are theorized to impede muscle recovery following anterior cruciate ligament (ACL) surgery, yet functional implications of centrally driven adaptations remain unclear. We aimed to assess relationships between quadriceps corticomotor and neuromechanical function after ACL surgery, and to compare with contralateral and control limbs. 16 individuals after primary, unilateral ACL surgery and 16 sex- and age-matched controls participated. Corticomotor function was assessed using transcranial magnetic stimulation, and quantified via active motor thresholds (AMT), short-interval intracortical inhibition (SICI), and intracortical facilitation (ICF). Neuromechanical function was quantified via electromechanical delay, early and late-phase rate of torque development (RTD0–50, RTD100–200), coefficient of variation, maximal voluntary isometric contraction (MVIC) torque, and central activation ratio. We observed significant correlations in the ACL limbs between: AMT and RTD0–50 (r = − 0.513, p = 0.031), SICI and RTD100–200 (r = 0.501, p = 0.048), AMT and SICI (r = − 0.659, p = 0.010), AMT and ICF (r = 0.579, p = 0.031), RTD0–50 and MVIC (r = 0.504, p = 0.023), and RTD100–200 and MVIC (r = 0.680, p = 0.002). The ACL limbs demonstrated higher AMT compared to controls (44.9 ± 8.4 vs. 30.1 ± 8.2%, p < 0.001), and lesser MVIC torque (2.37 ± 0.52 vs. 2.80 ± 0.59 Nm/kg, p = 0.005) and RTD100–200 (6.79 ± 1.72 vs. 7.90 ± 1.98 Nm/kg/s, p = 0.006) compared to the contralateral limbs. Our findings indicate that lesser corticospinal excitability is associated with lesser early-phase RTD, and greater intracortical inhibition is associated with lesser late-phase RTD. These findings provide evidence of implications of altered intracortical and corticospinal pathways relative to the ability to rapidly generate quadriceps torque following ACL surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) injuries constitute a significant portion of major knee joint injuries sustained by young, active individuals, affecting upwards of 250,000 in the United States annually (Griffin et al. 2006). Alarmingly, the recommended solution to restore joint stability following injury, ACL reconstruction, does not prevent knee osteoarthritis (OA) (Luc et al. 2014a, b), presenting a specific challenge to health care professionals. Post-traumatic quadriceps weakness is a hallmark characteristic among individuals with a history of ACLR (Lisee et al. 2019), posing a significant threat to joint health by promoting an increased risk for reinjury (Grindem et al. 2016), and an accelerated onset (Oiestad et al. 2015) and progression (Culvenor et al. 2017) of symptomatic OA. Since articular cartilage degeneration is irreversible, the mainstay of prevention is early detection and intervention of modifiable sources of impairment. However, the underlying mechanisms of muscle dysfunction must be further explored to optimize the efficacy of evidence-based treatment models.
Neuromuscular adaptations, such as quadriceps weakness and central activation failure, are well documented among individuals with ACL surgery (Lisee et al. 2019). Over the past 15 years, a growing body of literature has implicated brain plasticity as a contributor to persistent quadriceps dysfunction (Baumeister et al. 2008; Grooms et al. 2017; Norte et al. 2018b; Diekfuss et al. 2019; Kuenze et al. 2015; Luc-Harkey et al. 2017; Pietrosimone et al. 2015a, b). Specifically, impaired corticomotor function arising from altered intracortical and corticospinal pathways are theorized to impede muscle recovery by creating less efficient brain-to-muscle communication during voluntary effort following ACL reconstruction. Transcranial magnetic stimulation (TMS) has been used to demonstrate higher active motor thresholds (AMT) (Kuenze et al. 2015; Lepley et al. 2015; Norte et al. 2018b; Pietrosimone et al. 2015a, b), suggesting the excitability of corticospinal projections to the quadriceps decreases after ACL reconstruction. Lesser corticospinal excitability (higher AMT) and greater intracortical inhibition [lower short-interval intracortical inhibition (SICI) amplitude] are associated with decreased quadriceps torque (Lepley et al. 2014; Bodkin et al. 2019) and central activation failure (Luc-Harkey et al. 2017), supporting the potential clinical relevance of these impairments. Importantly, characteristics of intracortical and corticospinal excitability are modifiable (Kuhn et al. 2017; Nitsche and Paulus 2000; Pietrosimone et al. 2015a, b; Weavil et al. 2015), and may offer novel targets in clinical rehabilitation. While strength and activation are important metrics of muscle capacity, they may fail to characterize the extent of muscle function.
In addition to muscle weakness, gross neuromuscular dysfunction can manifest as an impaired ability to initiate [electromechanical delay (EMD)] (Kaneko et al. 2002), rapidly produce [rate of torque development (RTD)] (Kline et al. 2015), and control (coefficient of variation [CV]) (Goetschius and Hart 2016) force production via altered motor neuron recruitment and firing. We have operationally defined these characteristics as neuromechanical function (Blackburn et al. 2009), which may provide a more complete description of dynamic muscle function. For example, non-contact ACL ruptures are reported to occur within the first 50 ms of initial contact during high-impact tasks when peak loading on the ACL is greatest (Weinhandl et al. 2013). Delaying the ability to initiate and rapidly generate force may place individuals at a greater risk for reinjury when performing dynamic tasks. Neuromuscular control of the knee has been identified as a predictor of second ACL injury (Paterno et al. 2010), suggesting that the diminished ability to smoothly control force production may further compound such risk. Therefore, neuromechanical function likely plays a pivotal role in the attenuation of everyday loading experienced at the knee.
The relationship between centrally driven neurological adaptations and unique characteristics of muscle quality is not well understood. Previous authors have investigated relationships between corticomotor function and traditional strength measures (torque and central activation), yet none have assessed measures of neuromechanical function (EMD, RTD, CV) in this regard. In an effort to better understand the functional implications of altered corticomotor pathways, the relationships between measures of corticomotor and neuromechanical function must be established. Therefore, our purpose was to assess these relationships among individuals with a history of ACL surgery. To better understand the factors that could potentially influence existing relationships between corticomotor and neuromechanical outcomes, we aimed to further explore relationships between outcomes within each category. Our secondary purpose was to compare outcomes to the contralateral and control limbs. We hypothesized that reduced corticomotor function (less corticospinal excitability and greater intracortical inhibition) would be associated with poor neuromechanical function, and that outcomes would be worse in the ACL injured limb compared to the contralateral and control limbs.
Methods
Study design
We used a cross-sectional design to assess the quadriceps corticomotor and neuromechanical function of individuals with a history of ACL surgery and controls. For aim 1, measures of corticomotor function (AMT, SICI, and intracortical facilitation [ICF]) were treated as explanatory variables for individual measures of neuromechanical function (maximal voluntary isometric contraction [MVIC] torque, EMD, RTD, CV, and central activation ratio [CAR]). Relationships were assessed for the ACL limb and matched control limb in each group. For aim 2, all measures of corticomotor and neuromechanical function were compared between groups, and neuromechanical function was compared between limbs in the ACL group.
Participants
16 individuals with a history of primary, unilateral ACL surgery and 16 sex- and age-matched controls volunteered to participate in this study. ACL participants were recruited from our University medical center, student-body, and local community. To be eligible, ACL participants must have been 18–35 years old and more than 6 months from surgical reconstruction (n = 15) or repair (n = 1). Those with a history of failed reconstruction or repair, treated multi-ligament knee injury, treated articular lesion, surgical procedure other than the index knee surgery, or concussion were excluded. Graft type and meniscal procedure were reported descriptively. Individuals without ACL injury who were free of lower extremity surgery or injury within 12 months were enrolled, and matched with ACL participants by sex and age (± 2 years). Participants were instructed to refrain from caffeine and alcohol use during the 12 h prior to testing, and those who were taking prescribed stimulants or depressants were excluded. All participants were screened according to the safety and ethical guidelines for use of TMS in clinical practice and research (Rossi et al. 2011). Our Institutional Review Board for Biomedical Research approved this study, and all participants provided verbal and written informed consent prior to beginning the procedures below.
Procedures
Testing procedures were conducted during one session in the order described below. The order of testing was counterbalanced in the ACL group based on the injured limb. Since control participants were matched at a 1:1 ratio, the control limb was determined based on which limb (dominant or non-dominant) was injured. To allow ample time for recovery between neuromechanical and corticomotor testing, each participant was given approximately 10 min to rest in a seated position as previously described (Norte et al. 2018a). All participants self-reported their knee function using the International Knee Documentation Committee (IKDC) Subjective Knee Evaluation prior to neuromechanical and corticomotor testing.
Participant set-up
Participants sat on a treatment plinth with the knees flexed to approximately 90 degrees, while the skin over the muscle belly of the vastus medialis obliquus (VMO) was shaved, cleansed with alcohol and debrided to minimize skin impedance as previously described (Lepley et al. 2015; Luc-Harkey et al. 2017; Norte et al. 2018b). Two circular Ag–AgCl disposable surface electromyography (EMG) electrodes (EL503, Biopac Systems Inc., Goleta, CA, USA) were placed over the muscle belly with an inter-electrode distance of 20 mm in accordance with established guidelines (Hermens et al. 2000). A ground electrode was placed over the contralateral medial malleolus. The EMG signal fidelity was verified by assessing cross-talk and ensuring a minimal standard deviation of ≤ 0.002 volts.
Neuromechanical
Participants were seated upright in a stationary dynamometer (System 4 Pro, Biodex Inc., Shirley, NY), with the knee flexed to 90 degrees. Participants were instructed to keep their head and shoulders against the chair and to only use their thigh during strength testing. Padded straps were secured over the chest and lap to further reduce aberrant motion. In preparation for CAR assessment, two 3″ × 5″ self-adhesive electrodes (ValuTrode, Axelgaard Manufacturing Co., Ltd) were placed over the quadriceps in a rectus femoris configuration as previously described (Pietrosimone et al. 2011) to avoid the EMG electrodes. Next, participants completed a series of 4–5 familiarization trials at increasingly greater intensities (25%, 50%, 75%, and 100% MVIC). Instructions were given to kick out as hard and as fast as possible for 3 s. Visual feedback was provided via TV monitor and verbal encouragement/goal setting was delivered by the investigator to promote maximum effort. Three MVIC trials were then performed and assessed for MVIC torque, EMD, RTD, and CV. Two additional MVIC trials were performed in which a supramaximal percutaneous electrical stimulus was manually delivered to the quadriceps based on a visual plateau of the torque output using the superimposed burst technique as previously described (Norte et al. 2018b). The transient increase in torque was used to calculate the CAR from the final two trials only. A minimum of 60 s rest between test trials was ensured. Testing was performed bilaterally in a counterbalanced fashion.
Corticomotor
Single- and paired-pulse TMS paradigms were used to assess corticospinal (AMT) and intracortical (SICI, ICF) pathways. Participants remained seated in the dynamometer chair, and wore a Lycra swim cap with a 1 cm x 1 cm grid to aid in determining the optimal stimulus location. Two lines were drawn on the swim cap, with one aligned from nasion to inion (longitudinal), and the other connecting the tragi of each ear (horizontal). The vertex was determined by measuring 50% of the distance along the longitudinal and horizontal lines, and ear plugs were worn.
Participants were instructed to gently extend the knee to reach a threshold line equal to 5% of the previously determined MVIC torque displayed on a TV monitor. Further instructions were given to limit movement other than the test knee, and to completely relax, while remaining focused on the task. During testing, a 100 mm double-cone coil was positioned over the primary motor cortex contralateral to the test limb. Magnetic stimuli equal to 50% of the maximum stimulator output (BiStim2, Magstim Company Ltd., Wales, UK) were then delivered during the plateaued region of the contraction in a systematic fashion until the largest motor evoked potential (MEP) was observed. A minimum of 2 stimuli were delivered at each grid location, and in the case of visually inconsistent MEP amplitudes, the location that produced the largest and most consistent signals was used for testing. Once the optimal location was determined, the stimulus intensity was reduced in 5% decrements until the MEP was no longer observable (Norte et al. 2018b). The intensity was then increased in 1% increments until the MEP reappeared (≥ 100 µV) in 4 of 8 trials (Luc et al. 2014a, b). The lowest intensity capable of producing an MEP was recorded as the AMT. Lastly, MEP (120% AMT), SICI (80% AMT, 3 ms inter-pulse internal, 120% AMT), and ICF (80% AMT, 15 ms inter-pulse internal, 120% AMT) amplitudes were calculated from 3 additional blocks of 8 stimuli performed in a random sequence (Chen 2000; Thomas et al. 2016). Testing was only performed on the ACL injured limb and matched control limbs. Previous research has reported no between-limb differences in AMT following ACL reconstruction and in heathy controls (Norte et al. 2018b). Therefore, we chose to omit testing from the contralateral limb to minimize risk exposure and time requirements.
Data reduction
Neuromechanical
EMG and force data were sampled at 1000 Hz, and collected simultaneously using a 16-bit data acquisition system (MP160, Biopac Systems Inc., Goleta, CA, USA) and AcqKnowledge software (v. 5.0, Biopac Systems Inc.). We assessed the frequency content of force and EMG data prior to digital filtering (finite impulse response, Blackman window), and visually assessed the onset of signals before and after filtering to confirm the absence of a phase shift. We applied a 15 Hz low-pass filter to all force data (Andersen et al. 2010). EMG data were band-pass filtered from 10 to 500 Hz, band-stop filtered from 59.5 to 60.5 Hz, and amplified with a gain of 1000. The root mean square of filtered EMG signals was then taken using a 20 ms sample (Pamukoff et al. 2017). The scaling of the software display window was then adjusted to aid in the visualization of EMG and force onsets (horizontal time scale: 0.5 s, vertical EMG scale: 0.025 volts, vertical force scale: 0.5 volts). The mean and standard deviation (SD) of the baseline signals were calculated during the 200 ms prior to visual onset. The onset of EMG and force were considered when the signals reached 3 SDs above the baseline mean (de Ruiter et al. 2004). Signals must have remained above 3 SDs for at least 50 ms to be considered “ON.” EMD was calculated as the time from EMG onset to force onset (ms). RTD was calculated as the change in torque divided by a specified time during early (0–50 ms) and late (100–200 ms) phases, and normalized to body mass (Nm/kg/s). The horizontal time scale was then changed to 3 s, and CV was calculated during a 500 ms epoch by dividing the SD of the highest plateaued torque region by its mean, expressed as a percentage (%). MVIC torque was quantified by taking the average of the peak values recorded from each trial, and normalized to body mass (Nm/kg) (Goetschius and Hart 2016). CAR was calculated by dividing the mean torque from a 100 ms epoch prior to the electrical stimulus by the superimposed burst torque, expressed as a percentage (%).
Corticomotor
MEP signals were sampled at 2000 Hz and band-pass filtered from 1–5000 Hz. The peak-to-peak MEP amplitudes were measured and averaged over 8 trials for MEP 120%, SICI, and ICF. SICI and ICF amplitudes were normalized to the MEP 120% amplitude, and expressed an unit-less ratios (Thomas et al. 2016).
Statistical analysis
A previous study reported that lesser AMT is associated with greater quadriceps MVIC torque (r = − 0.62) (Lepley et al. 2014). Based on the previously reported direction of this relationship, we chose to use one-tailed tests in our analyses. Using a moderate correlation of 0.6 (α = 0.05, 1–β = 0.80), we estimated that 15 participants would be needed for each group to identify relationships between AMT and neuromechanical outcome measures if they existed (G*Power v. 3.1.9.4). Since AMT was considered the primary outcome measure, this was the only variable used in our sample size estimate.
Data were assessed for normality using the Shapiro–Wilk test, and visually inspected for outliers. Outliers were operationally defined as any value exceeding 3 × the interquartile range, and were removed from statistical analysis. Simple bivariate correlation coefficients (Pearson’s r) were used to assess the relationships between measures of corticomotor and neuromechanical function in the ACL group. To further describe any existing relationships, correlation coefficients were also used to assess the relationships within each category of variables. Correlations were interpreted as negligible (0.0–0.29), low (0.30–0.49), moderate (0.50–0.69), high (0.70–0.89), or very high (0.90–1.0) (Mukaka 2012). We used the Benjamin–Hochberg method to control for a false discovery rate of 5% among significantly correlated variables. A one-way multiple analysis of variance was used to assess the effect of ACL surgery history on all normally distributed outcome measures for the injured limb. Paired-samples t-tests were used with a Benjamin–Hochberg correction to compare outcomes between limbs in the ACL group. The Mann–Whitney U test (between groups) and Wilcoxon Signed-Rank test (between limbs) were used to compare non-normally distributed outcomes. Cohen’s d effect sizes with 95% confidence intervals were calculated to demonstrate the magnitude of between-limb and between-group differences. All data were evaluated at an alpha level of 0.05, and statistical analyses were performed using the Statistical Package for the Social Sciences (v. 25, IBM Corporation, Armonk, NY, USA).
Results
Group demographics are presented in Table 1. Individuals with a history of ACL surgery reported lower IKDC scores compared to controls. CV was non-normally distributed in the control (Shapiro–Wilk, p = 0.020) and contralateral (Shapiro–Wilk, p = 0.034) limbs, and all other variables were normally distributed. SICI and ICF data were not obtained in 4 participants in the ACL group and 1 participant in the control group due to the inability to elicit a measurable MEP during this portion of testing. Representative EMG tracings of these data are presented in Fig. 1. CAR data were not obtained in 2 control participants due to discomfort with the electrical stimulus. A total of 2 data points were identified as outliers and removed prior to analysis: ICF (ACL) and CV (control). Final analysis including the following: AMT (ACL injured n = 16, control n = 16), SICI (ACL injured n = 12, control n = 15), ICF (ACL injured n = 11, control n = 15), EMD (ACL injured n = 16, ACL contralateral n = 16, control n = 16), RTD0–50 (ACL injured n = 16, ACL contralateral n = 16, control n = 16), RTD100–200 (ACL injured n = 16, ACL contralateral n = 16, control n = 16), MVIC torque (ACL injured n = 16, ACL contralateral n = 16, control n = 16), CV (ACL injured n = 16, ACL contralateral n = 16, control n = 15), and CAR (ACL injured n = 16, ACL contralateral n = 16, control n = 14).
Between-category relationships
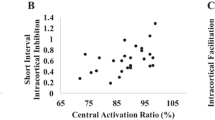
Correlations between categories of corticomotor and neuromechanical function are presented in Table 2 and Fig. 2 for individuals with a history of ACL surgery. We observed a moderate negative association between AMT and RTD0–50, and a moderate positive association between SICI and RTD100–200.
Scatterplot depictions of statistically significant correlation coefficients among individuals with a history of ACL surgery between a AMT and RTD0–50, b SICI and RTD100–200, c SICI and AMT, d ICF and AMT, e MVIC and RTD0–50, and f MVIC and RTD100–200. The dotted lines represent the line of best fit
Within-category relationships
Correlations within categories of corticomotor and neuromechanical function are presented in Table 2 and Fig. 2 for individuals with a history of ACL surgery. AMT demonstrated a moderate negative association with SICI and a moderate positive association with ICF. RTD0–50 and RTD100–200 demonstrated moderate positive associations with MVIC torque.
Between-limb and between-group comparisons
Group means for corticomotor and neuromechanical outcomes are presented in Table 3. There was a statistically significant difference in corticomotor function between groups (F(8,14) = 5.45, p = 0.003, Wilk’s Λ = 0.243, observed power = 0.974). In particular, individuals with a history of ACL surgery demonstrated higher AMT values compared to controls (corrected model p < 0.001, d = − 1,78 95% CI [− 2.60, − 0.96]). Additionally, MVIC torque (p = 0.005, d = − 0.77 95% CI [− 1.51, − 0.04]) and RTD100–200 (p = 0.006, d = − 0.91 95% CI [− 1.64, 0.18]) were lower in the ACL injured limb compared to the contralateral limb.
Discussion
Our primary finding was that greater AMT associated with lesser RTD0-50 in those with a history of ACL surgery, suggesting that individuals with less excitable corticospinal projections to quadriceps motor neurons generate early-phase torque slower, or to a lesser degree. Early rate of torque development is governed by neural factors, such as motor unit recruitment and discharge rate (Maffiuletti et al. 2016), which may explain its relationship with corticospinal excitability. From a functional perspective, early-phase rate of torque development is reported to be associated with sport-specific tasks (e.g., sprint performance) (Tillin et al. 2013), and a more sensitive indicator of change in neuromuscular function after ACL reconstruction (Angelozzi et al. 2012) as compared to traditional estimates of maximum torque. Moreover, this finding appears to be problematic for knee joint health considering that the ability to rapidly generate quadriceps torque is needed to resist perturbation, produce dynamic stability, and attenuate joint forces during early loading when ACL strain is greatest (Kernozek and Ragan 2008; Weinhandl et al. 2013). In fact, data from previous authors (Blackburn et al. 2016) suggest that lesser early-phase rate of torque development associates with greater peak vertical ground reaction force loading rates and heel strike transient magnitude in ACL reconstructed individuals during walking gait. These findings suggest that a diminished ability to rapidly generate torque early may contribute to the already increased risk for post-traumatic osteoarthritis in this population (Barenius et al. 2014) by altering knee joint loading characteristics during simple activities of daily living.
Lesser quadriceps corticospinal excitability has been demonstrated among individuals with ACL reconstruction compared to controls (Kuenze et al. 2015; Norte et al. 2018b; Pietrosimone, Lepley et al. 2015; Lepley et al. 2015), with one study reporting a decrease in AMT from pre-surgery to 6 months post-surgery (Lepley et al. 2015). The ACL group in our study demonstrated higher AMT compared to controls, supporting previous findings. We observed a large magnitude difference (mean difference = 14.8%), which exceeded an estimated minimal detectable change range of 2.9–7.5% [standard deviation = 8.3; ICC3,1 = 0.792–0.970 (Luc et al. 2014a, b)], suggesting its clinical relevance. Despite the current evidence base, our lack of understanding the functional relevance of cortically driven impairments has presented a major challenge to the development of therapeutic interventions that address these concerns. To elucidate this knowledge gap, previous studies have reported on the relationships between measures of corticomotor outcomes and quadriceps strength (Lepley et al. 2014; Bodkin et al. 2019), central activation (Luc-Harkey et al. 2017; Lepley et al. 2014), and patient-reported knee function (Pietrosimone et al. 2013) in this population. For example, greater AMT (lesser corticomotor excitability) is reported to be associated with lesser quadriceps torque (r = − 0.50 to − 0.62) and central activation (r = − 0.39 to − 0.64) (Bodkin et al. 2019; Lepley et al. 2014; Luc-Harkey et al. 2017), yet we did not observe these relationships. As these findings have not been consistently replicated (Norte et al. 2018a; Lepley et al. 2014), further investigation is warranted.
A second important finding was that lesser SICI amplitude associated with lesser RTD100–200 in those with a history of ACL surgery, suggesting that individuals with greater intracortical inhibition generate late-phase torque slower, or to a lesser degree. This was an interesting and unexpected finding, given that the capacity of muscle to produce maximal strength is believed to predominantly govern late rate of torque development, rather than neural mechanisms (Maffiuletti et al. 2016; Andersen and Aagaard 2006). Regardless, neural drive remains a lesser contributor during the late phase, which may explain its relationship with intracortical inhibition. Previous authors (Luc-Harkey et al. 2017) have reported an association between lesser SICI amplitude (greater intracortical inhibition) and quadriceps central activation in ACL reconstructed individuals. Additionally, a weak relationship has been reported between higher late-phase RTD and subjective knee function, suggesting that intracortical inhibition may indirectly affect patient perception. Collectively, these data provide evidence for the functional relevance of intracortical pathways.
In addition to investigating the relationships between corticomotor and neuromechanical outcomes, we also wanted to explore relationships within each category to better understand our findings. It is well established that corticospinal excitability, and subsequent motor control, is influenced by inhibitory and excitatory processes within the motor cortex (Chen 2004). Our findings support this notion in that greater AMT was associated with lesser SICI and greater ICF amplitudes. This suggests that greater intracortical inhibition and facilitation associate with lesser corticospinal excitability. Previous authors (Orth et al. 2003) have reported a strong association between the thresholds for SICI and ICF with AMT, more so than resting motor threshold, highlighting the importance of measuring these variables at a fixed percentage of an active contraction. In regard to the neuromechanical outcomes, early and late-phase RTD were each associated with MVIC torque. This appears to suggest that factors which diminish the ability to rapidly generate force have the potential to negatively affect the total force generating capacity.
Despite observing a relationship between several measures of corticomotor and neuromechanical function, AMT was the only variable that differed between groups. From a neuromechanical perspective, this conflicts with previous findings reporting longer EMD, slower RTD, lesser MVIC torque, higher CV (greater torque variability), and lesser CAR in individuals with a history of ACL reconstruction compared to controls (Goetschius and Hart 2016; Norte et al. 2018b; Kaneko et al. 2002; Johnson et al. 2018). In contrast to others, our sample appeared to be highly active, with the ACL group reporting mean pre-injury and current Tegner scores of 9.3 and 7.5, respectively. Although subjective knee function was lower in the patient group, it is possible that participation in high-level physical activities could have accounted for a lack of differences from controls. Additionally, our control group demonstrated central activation failure to a greater extent than previous findings, suggesting the presence of gross inhibition. However, our control group was comparable to a previous report (Goetschius and Hart 2016) of 50 controls based on IKDC (98.1 vs. 98.9%), MVIC torque (2.58 vs. 2.57 Nm/kg), and CV (0.84 vs. 0.88%). Given that the only difference between our findings and this previous report was a discrepancy in CAR (81.4 vs. 91.0%), it is also possible that our participants were more apprehensive in response to the electrical stimulus, which could have lowered our values. Regardless, it is possible that additional between-group differences could have been masked by this finding. When assessing between-group effect sizes, we did observe a large magnitude deficit in CV from the ACL injured limb compared to the control limb, despite being statistically non-significant. This was the only variable in addition to AMT that demonstrated a homogenous confidence interval, suggesting we were underpowered to detect this difference. When comparing outcomes between limbs, the ACL injured limb was significantly weaker (moderate effect size) and generated less late-phase torque (large effect size) than the contralateral limb, demonstrating the presence of neuromechanical impairment. Based on our observed associations, these findings appear to lend further credence to the idea that corticomotor function should be considered in the treatment plan of these individuals.
Clinical implications
Target values of corticospinal excitability have been recently identified to discriminate levels of functioning among individuals with ACL reconstruction, which may provide useful clinical targets. For example, achieving an AMT ≤ 50.5% in the injured limb is reported to be an excellent discriminator of quadriceps strength indicative of satisfactory knee function (Bodkin et al. 2019), which could serve as an initial goal for neurophysiological recovery. As the individual progresses, achieving an AMT ≤ 39.5% is reported to be an acceptable discriminator of healthy status (Norte et al. 2019). Applying these methods to determine optimal values of intracortical function may provide an additional clinical target for intervention.
Corticospinal excitability (AMT) and intracortical inhibition (SICI) were associated with aspects of rate of torque development, providing evidence for their clinical relevance. Previous studies have reported an increase in measures of corticospinal excitability (AMT, MEP amplitude) using EMG biofeedback (Pietrosimone et al. 2015a, b), anodal transcranial direct current stimulation to the primary motor cortex (Nitsche and Paulus 2000), and isometric muscle contractions (Weavil et al. 2015), likely as a result of increased motor unit recruitment and firing rates. However, lengthening muscle contractions are reported to preferentially enhance cortical excitability to compensate for reduced spinal excitability in comparison to isometric contractions (Gruber et al. 2009). Therefore, eccentric exercise appears to be an appropriate neurophysiological adjunct in this population. Interestingly, resistance training can be modified to preferentially enhance early (fast-velocity concentric and eccentric) (de Oliveira et al. 2013; Oliveira et al. 2016) and late-phase (high-intensity) (Andersen et al. 2010) rate of torque development, suggesting this may be advantageous from a neuromuscular perspective. However, due to differences in the population, intervention, and outcome measures studied, the most appropriate treatments and clinical targets remain unclear at this time.
Limitations
Our findings are limited in several ways. First, we analyzed a small sample, and may have been underpowered to detect several relationships between measures of corticomotor and neuromechanical function. For example, we observed evidence of a negative association between SICI and ICF, yet this failed to reach statistical significance (p = 0.055). We powered our study based on the relationship between AMT and MVIC torque given that these measures are most frequently cited, and were underpowered to observe group differences among all outcome measures assessed. Additionally, we used a liberal statistical approach to control for a false discovery rate, rather than the more conservative Bonferroni approach to correct for multiple comparisons among our selected outcomes. Therefore, it is possible that several findings occurred due to chance alone, and caution should be taken when interpreting. Second, we did not compare corticomotor function between limbs in the ACL group. Although previous research has reported no between-limb differences in AMT after ACL reconstruction, we cannot be certain that our sample did not differ in this regard. Third, we chose to assess corticomotor function from the VMO to remain consistent with much of the current literature, yet, this approach may not characterize the function of the entire quadriceps musculature. Last, our cohort varied by sex, time from surgery, and surgical procedure. Although the generalizability of our findings is supported by our diverse cohort, these factors have been previously reported to influence quadriceps strength-related impairments (Kuenze et al. 2019). Furthermore, it is unclear how such factors (among others) may confound the observed relationships. As we were not powered to account for confounding variables in our correlational analyses, our findings should be considered as preliminary, and interpreted with caution.
Conclusions
The primary findings of our study were that lesser corticospinal excitability associated with lesser early phase rate of torque development, and that greater intracortical inhibition associated with lesser late-phase rate of torque development in individuals with a history of ACL surgery. The ACL injured limbs also demonstrated less corticospinal excitability compared to controls, and lesser peak torque and late-phase rate of torque development compared to the contralateral limbs. These findings provide new evidence for the implications of altered intracortical and corticospinal pathways relative to the ability to rapidly generate quadriceps torque among individuals with a history of ACL surgery.
References
Andersen LL, Aagaard P (2006) Influence of maximal muscle strength and intrinsic muscle contractile properties on contractile rate of force development. Eur J Appl Physiol 96:46–52
Andersen LL, Andersen JL, Zebis MK, Aagaard P (2010) Early and late rate of force development: differential adaptive responses to resistance training? Scand J Med Sci Sports 20:e162–e169
Angelozzi M, Madama M, Corsica C, Calvisi V, Properzi G, McCaw ST, Cacchio A (2012) Rate of force development as an adjunctive outcome measure for return-to-sport decisions after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 42:772–780
Barenius B, Ponzer S, Shalabi A, Bujak R, Norlen L, Eriksson K (2014) Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med 42:1049–1057
Baumeister J, Reinecke K, Weiss M (2008) Changed cortical activity after anterior cruciate ligament reconstruction in a joint position paradigm: an EEG study. Scand J Med Sci Sports 18:473–484
Blackburn JT, Bell DR, Norcross MF, Hudson JD, Engstrom LA (2009) Comparison of hamstring neuromechanical properties between healthy males and females and the influence of musculotendinous stiffness. J Electromyogr Kinesiol 19:e362–e369
Blackburn JT, Pietrosimone B, Harkey MS, Luc BA, Pamukoff DN (2016) Quadriceps Function and Gait Kinetics after Anterior Cruciate Ligament Reconstruction. Med Sci Sports Exerc 48:1664–1670
Bodkin SG, Norte GE, Hart JM (2019) Corticospinal excitability can discriminate quadriceps strength indicative of knee function after ACL-reconstruction. Scand J Med Sci Sports. 29(5):716–724
Chen R (2000) Studies of human motor physiology with transcranial magnetic stimulation. Muscle Nerve Suppl 9:S26–S32
Chen R (2004) Interactions between inhibitory and excitatory circuits in the human motor cortex. Exp Brain Res 154:1–10
Culvenor AG, Ruhdorfer A, Juhl C, Eckstein F, Oiestad BE (2017) Knee extensor strength and risk of structural, symptomatic, and functional decline in knee osteoarthritis: a systematic review and meta-analysis. Arthritis Care Res (Hoboken) 69:649–658
de Oliveira FB, Rizatto GF, Denadai BS (2013) Are early and late rate of force development differently influenced by fast-velocity resistance training? Clin Physiol Funct Imaging 33:282–287
de Ruiter CJ, Kooistra RD, Paalman MI, de Haan A (2004) Initial phase of maximal voluntary and electrically stimulated knee extension torque development at different knee angles. J Appl Physiol 1985(97):1693–1701
Diekfuss JA, Grooms DR, Yuan W, Dudley J, Barber Foss KD, Thomas S, Ellis JD, Schneider DK, Leach J, Bonnette S, Myer GD (2019) ‘Does brain functional connectivity contribute to musculoskeletal injury? A preliminary prospective analysis of a neural biomarker of ACL injury risk. J Sci Med Sport 22:169–174
Goetschius J, Hart JM (2016) Knee-extension torque variability and subjective knee function in patients with a history of anterior cruciate ligament reconstruction. J Athl Train 51:22–27
Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, Demaio M, Dick RW, Engebretsen L, Garrett WE Jr, Hannafin JA, Hewett TE, Huston LJ, Ireland ML, Johnson RJ, Lephart S, Mandelbaum BR, Mann BJ, Marks PH, Marshall SW, Myklebust G, Noyes FR, Powers C, Shields C Jr, Shultz SJ, Silvers H, Slauterbeck J, Taylor DC, Teitz CC, Wojtys EM, Yu B (2006) Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med 34:1512–1532
Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA (2016) Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med 50:804–808
Grooms DR, Page SJ, Nichols-Larsen DS, Chaudhari AM, White SE, Onate JA (2017) Neuroplasticity associated with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 47(3):180–189
Gruber M, Linnamo V, Strojnik V, Rantalainen T, Avela J (2009) Excitability at the motoneuron pool and motor cortex is specifically modulated in lengthening compared to isometric contractions. J Neurophysiol 101:2030–2040
Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G (2000) Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol 10:361–374
Johnson AK, Palmieri-Smith RM, Lepley LK (2018) Contribution of neuromuscular factors to quadriceps asymmetry after anterior cruciate ligament reconstruction. J Athl Train 53:347–354
Kaneko F, Onari K, Kawaguchi K, Tsukisaka K, Roy SH (2002) Electromechanical delay after ACL reconstruction: an innovative method for investigating central and peripheral contributions. J Orthop Sports Phys Ther 32:158–165
Kernozek TW, Ragan RJ (2008) Estimation of anterior cruciate ligament tension from inverse dynamics data and electromyography in females during drop landing. Clin Biomech (Bristol, Avon) 23:1279–1286
Kline PW, Morgan KD, Johnson DL, Ireland ML, Noehren B (2015) Impaired quadriceps rate of torque development and knee mechanics after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 43:2553–2558
Kuenze CM, Hertel J, Weltman A, Diduch D, Saliba SA, Hart JM (2015) Persistent neuromuscular and corticomotor quadriceps asymmetry after anterior cruciate ligament reconstruction. J Athl Train 50:303–312
Kuenze C, Pietrosimone B, Lisee C, Rutherford M, Birchmeier T, Lepley A, Hart J (2019) Demographic and surgical factors affect quadriceps strength after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 27:921–930
Kuhn YA, Keller M, Ruffieux J, Taube W (2017) Adopting an external focus of attention alters intracortical inhibition within the primary motor cortex. Acta Physiol (Oxf) 220:289–299
Lepley AS, Ericksen HM, Sohn DH, Pietrosimone BG (2014) Contributions of neural excitability and voluntary activation to quadriceps muscle strength following anterior cruciate ligament reconstruction. Knee 21:736–742
Lepley AS, Gribble PA, Thomas AC, Tevald MA, Sohn DH, Pietrosimone BG (2015) Quadriceps neural alterations in anterior cruciate ligament reconstructed patients: a 6-month longitudinal investigation. Scand J Med Sci Sports 25:828–839
Lisee C, Lepley AS, Birchmeier T, O’Hagan K, Kuenze C (2019) Quadriceps strength and volitional activation after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Sports Health 11:163–179
Luc BA, Lepley AS, Tevald MA, Gribble PA, White DB, Pietrosimone BG (2014a) Reliability of corticomotor excitability in leg and thigh musculature at 14 and 28 days. J Sport Rehabil 23:330–338
Luc B, Gribble PA, Pietrosimone BG (2014b) Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train 49:806–819
Luc-Harkey BA, Harkey MS, Pamukoff DN, Kim RH, Royal TK, Blackburn JT, Spang JT, Pietrosimone B (2017) Greater intracortical inhibition associates with lower quadriceps voluntary activation in individuals with ACL reconstruction. Exp Brain Res 235:1129–1137
Maffiuletti NA, Aagaard P, Blazevich AJ, Folland J, Tillin N, Duchateau J (2016) Rate of force development: physiological and methodological considerations. Eur J Appl Physiol 116:1091–1116
Mukaka MM (2012) Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J 24:69–71
Nitsche MA, Paulus W (2000) Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol 527(Pt 3):633–639
Norte GE, Hertel J, Saliba SA, Diduch DR, Hart JM (2018a) Quadriceps function and patient-reported outcomes after anterior cruciate ligament reconstruction in patients with or without knee osteoarthritis. J Athl Train 53:965–975
Norte GE, Hertel J, Saliba SA, Diduch DR, Hart JM (2018b) Quadriceps neuromuscular function in patients with anterior cruciate ligament reconstruction with or without knee osteoarthritis: a cross-sectional study. J Athl Train 53:475–485
Norte GE, Hertel JN, Saliba SA, Diduch DR, Hart JM (2019) Quadriceps and patient-reported function in ACL-reconstructed patients: a principal component analysis. J Sport Rehabil. 28(1):8–16
Oiestad BE, Juhl CB, Eitzen I, Thorlund JB (2015) ‘Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthr Cartil 23:171–177
Oliveira AS, Corvino RB, Caputo F, Aagaard P, Denadai BS (2016) Effects of fast-velocity eccentric resistance training on early and late rate of force development. Eur J Sport Sci 16:199–205
Orth M, Snijders AH, Rothwell JC (2003) The variability of intracortical inhibition and facilitation. Clin Neurophysiol 114:2362–2369
Pamukoff DN, Pietrosimone B, Ryan ED, Lee DR, Brown LE, Blackburn JT (2017) Whole-body vibration improves early rate of torque development in individuals with anterior cruciate ligament reconstruction. J Strength Condition Res. 31(11):2992–3000
Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, Hewett TE (2010) Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 38:1968–1978
Pietrosimone BG, Selkow NM, Ingersoll CD, Hart JM, Saliba SA (2011) Electrode type and placement configuration for quadriceps activation evaluation. J Athl Train 46:621–628
Pietrosimone BG, Lepley AS, Ericksen HM, Gribble PA, Levine J (2013) Quadriceps strength and corticospinal excitability as predictors of disability after anterior cruciate ligament reconstruction. J Sport Rehabil 22:1–6
Pietrosimone BG, Lepley AS, Ericksen HM, Clements A, Sohn DH, Gribble PA (2015a) Neural excitability alterations after anterior cruciate ligament reconstruction. J Athl Train 50:665–674
Pietrosimone B, McLeod MM, Florea D, Gribble PA, Tevald MA (2015b) Immediate increases in quadriceps corticomotor excitability during an electromyography biofeedback intervention. J Electromyogr Kinesiol 25:316–322
Rossi S, Hallett M, Rossini PM, Pascual-Leone A (2011) Screening questionnaire before TMS: an update. Clin Neurophysiol 122:1686
Thomas AC, Pietrosimone BG, Bayer CJ (2016) Agreement between investigators using paired-pulse transcranial magnetic stimulation to assess quadriceps intracortical excitability. J Sport Rehabil 1–13
Tillin NA, Pain MT, Folland J (2013) Explosive force production during isometric squats correlates with athletic performance in rugby union players. J Sports Sci 31:66–76
Weavil JC, Sidhu SK, Mangum TS, Richardson RS, Amann M (2015) Intensity-dependent alterations in the excitability of cortical and spinal projections to the knee extensors during isometric and locomotor exercise. Am J Physiol Regul Integr Comp Physiol 308:R998–R1007
Weinhandl JT, Earl-Boehm JE, Ebersole KT, Huddleston WE, Armstrong BS, O’Connor KM (2013) Anticipatory effects on anterior cruciate ligament loading during sidestep cutting. Clin Biomech (Bristol, Avon) 28:655–663
Acknowledgments
The authors would like to thank the Great Lakes Athletic Trainers’ Association for funding this work.
Funding
This study was funded by the Great Lakes Athletic Trainers’ Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Communicated by Winston D Byblow.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Scheurer, S.A., Sherman, D.A., Glaviano, N.R. et al. Corticomotor function is associated with quadriceps rate of torque development in individuals with ACL surgery. Exp Brain Res 238, 283–294 (2020). https://doi.org/10.1007/s00221-019-05713-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-019-05713-w