Abstract
Celiac disease (CD) is a chronic autoimmune disorder induced in genetically susceptible individuals by the ingestion of gluten from wheat, rye, barley, or certain varieties of oats. A careful diet follow-up is necessary to avoid health complications associated with long-term gluten intake by the celiac patients. Small peptides (GIP, gluten immunogenic peptides) derived from gluten digestion, which are excreted in the urine and feces, have emerged as promising biomarkers to monitor gluten intake. We have implemented a simple and sensitive label-free point-of-care (POC) device based on surface plasmon resonance for the direct detection of these biomarkers in urine. The assay employs specific monoclonal antibodies and has been optimized for the detection of the 33-mer α2-gliadin, known as the main immunogenic peptide of wheat gluten, and for the detection of GIP. Direct detection in undiluted urine has been accomplished by using biosensing chips containing a robust and stable biorecognition layer, obtained after carefully optimizing the biofunctionalization protocol. Excellent limits of detection have been reached (1.6–4.0 ng mL−1 using mAb G12 and A1, respectively), which ensures the detection of gluten peptides even when the gluten intake is around the maximum tolerable amount in the digestive tract (< 50 mg) for celiac individuals. No sample pretreatment, extraction, or dilution is required, and the analysis takes less than 15 min. The assays have excellent reproducibility‚ as demonstrated by measuring spiked urine samples containing the same target concentration using different biofunctionalized chips prepared and stored at different periods of time (i.e., CV% of 3.58% and 11.30%, for G12- and A1-based assays, respectively). The assay has been validated with real samples. These features pave the way towards an end-user easy-to-handle biosensor device for the rapid monitoring of gluten-free diet (GFD) and follow-up of the health status in celiac patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Celiac disease (CD) is an autoimmune enteropathy that leads to the destruction of the villi lining the small intestine. It is triggered by the ingestion of gluten-containing cereals in genetically predisposed individuals [1]. CD causes severe symptoms including chronic diarrhea, fatigue, abdominal distension, weight loss, and also anemia, osteoporosis, and neurological symptoms due to malabsorption of nutrients [2, 3]. The prevalence is approximately 1% worldwide but varies greatly in different geographical areas [4, 5]. It is estimated that the number of undiagnosed cases is even higher [6, 7]. Moreover, an increasing incidence of CD is observed, which can be partially attributed to the improvement in diagnostic techniques and disease awareness [8].
Gluten refers to a heterologous group of proteins composed of prolamin and glutelin fractions. The prolamin fraction known as gliadin contains the main toxic components [3]. Once consumed, gluten is partially digested into gliadin peptides (10 to 50 amino acids), which are resistant to degradation by intestinal proteases of the epithelial barrier of the intestinal mucosa [9]. These peptides are deaminated by enzyme tissue transglutaminase (tTG) converting them into more immunogenic molecules that activate the adaptive immune system [1]. This response involves antigen-presenting cells (APC) that express the haplotypes HLA-DQ2 and DQ8, the main genetic predisposition factor that triggers an immune response against digested gluten [10, 11]. The APC are highly reactive to gliadin-specific T cells, which produce a cascade of inflammatory mediators, resulting in a damage to the intestinal mucosa manifested as villous atrophy, characteristic of CD [1]. Currently there is no cure for CD and the only therapeutic treatment is a strict adherence to a gluten-free diet (GFD) in daily life [12, 13]. One of the main problems nowadays related to maintaining a GFD is the presence of hidden gluten in food [14]. Approximately, more than half of commercially available food contains gluten from wheat, barley, rye, or oats, including those products where it is used as thickener or binder [15]. According to the regulation Codex Alimentarius (CODEX STAN118-1979, revised in 2008) [16], the total level of gluten in gluten-free food does not exceed 20 mg kg−1. Therefore, constant vigilance is always required as the adhesion to a strict diet with zero gluten intakes is almost impossible given its ubiquity, cross-contamination, or the inadequate food labeling regulations [12, 17, 18]. As a result, persistent symptoms and enteropathy are common among celiac patients who are trying to follow a GFD. Specifically, research shows that 25–40% of adults with CD have persistent enteropathy after 2 years on a GFD. Children are thought to recover more quickly, and data suggest that 5–19% of celiac children on a GFD may have persistent enteropathy despite treatment with a GFD for at least 1 year. Moreover, the amount of gluten that celiac patients can tolerate has not yet been established due to the variability between individuals [18]. However, the effects of low gluten consumption in celiac patients have suggested that daily consumption of up to 50 mg can cause significant damage in the small intestine [19]. Hence, a daily intake of gluten less than 10 mg is recommended to be safe and unlikely to cause significant abnormalities or to trigger symptoms [6].
Currently, several companies have commercialized detection assays such as Quanta Flash® Celiac (Werfen Company, Spain), Alegria® (Orgentec Diagnostika, Germany), EliA™ Celikey (tTG)/EliA™ Gliadin (Thermo Scientific Phadia, USA), and Anti-Gliadin GAF-3X ELISA/Anti-tTG ELISA (Euroimmun, Germany) to diagnose celiac disease, and iVYLISA GIP™ (Biomedal, Spain) to monitor the adherence to the GFD. They are commonly based on solid-phase immunoassays (i.e., ELISA, chemiluminescence, and immunofluorescence) performed with bench-top, high-throughput instruments. They are sensitive and specific tools, although are also considerably expensive. Their handling requires specialized skills and commonly these analysis are done in central laboratories and research centers. However, their location in primary healthcare settings is more limited and definitely less accessible to the patient himself [18, 20,21,22].
The development of portable, compact, and easy-to-handle tools entails significant advantages for its self-use by patients, as it allows direct detection or personalized monitoring of therapies usually with a small amount of a biological sample. Such is the case of the qualitative tests based on lateral flow immunochromatography (LFT) Sintomax® (Augurix SA, Switzerland), Xeliac® Test (Eurospital, Italy), and Biocard™ celiac test (AniBiotech®, Vantaa, Finland) [22,23,24,25]. These companies have developed qualitative, direct, rapid, and easy tests that support the monitoring or the diagnosis of the disease by the end-user. However, the limitation of these tests is mainly related to the lack of quantification of the analyte concentration to know the evolution of the immune response to treatment. In other instances (i.e., GlutenDetect®, Biomedal, Spain), the sensitivity might not be enough to detect small intakes of gluten, and the use of additional cocktails for dilution and pretreatment of samples complicates the steps done by the user and restricts its continuous use at home.
We have designed, fabricated, and implemented a compact, portable, and easy-to-use device based on surface plasmon resonance (SPR) biosensing that overcomes the limitations mentioned above, to specifically and quantitatively monitor gluten intake levels from a simple urine analysis. The device is based on immunoassays similar to the ones used in the iVYCHECK GIP Urine™ test (Biomedal, Spain), where gluten immunogenic peptides (GIP), originated after gliadin degradation, are detected in urine and feces samples using highly specific monoclonal antibodies (mAb). These antibodies (G12 and A1) have a high affinity for GIP, especially for the α2-gliadin 33-mer peptide (MW ~ 3.9 kDa), a small-sized and digestion-resistant peptide, which is the most immunodominant toxic peptide to the celiac patients [18, 22]. This test relies in a sandwich lateral flow immunoassay (LFIA) using both A1 and G12 antibodies (thus being necessary the presence of two different epitopes per molecule to detect the GIP); it requires a sample preconditioning and provides a qualitative response. A quantitative reading can only be obtained by digital reading with a specific scanner (iVYCHECK Reader), available in research laboratory settings after introduction of the LFIA cartridge. This SPR-based approach removes this two-step reading and removes the need of having two different epitopes in the GIP, as it relies on an indirect competitive immunoassay (using only one type of antibody). A customized gold-chip biofunctionalization strategy has been precisely established, successfully providing the direct, quantitative analysis of whole urine. No previous extraction, pretreatment, or even dilution step is needed. The assays are implemented in a compact biosensor prototype, showing excellent levels of detection with both specific antibodies and wide working ranges that allow detecting minimum concentrations of GIP for a strict GFD or low gluten intake.
Materials and methods
Urine sample collection
Two different types of urine samples were received from internal studies and collected according to the donor’s gluten-containing diet. Group 1 samples are obtained from celiac disease patients and healthy volunteers on strict gluten-free diet (GFD) and were used during the optimization and assessment of immunoassays. Group 2 samples are collected from healthy individuals following an unrestricted normal gluten-containing diet. The α2-gliadin 33-mer peptide concentrations were analyzed with the iVYCHECK GIP Urine™ lateral flow device and quantified with the iVYCHECK GIP Reader™ from Biomedal S.L. (Seville, Spain) [17]. All volunteers were provided with sterile falcons (50 mL). Urine samples were collected and stored at − 20 °C. Written consent was obtained from all volunteers that provided samples.
POC device and detection assay format
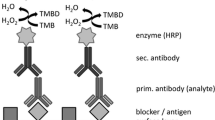
The plasmonic biosensor device involves a miniaturized platform (20 × 20 cm2) (see Fig. 1 and Electronic Supplementary Material (ESM) Fig. S1) which incorporates the optical setup, the biosensor chip, and the flow cell to bring samples over the sensing area [26]. The sensor chips consist of a gold thin layer (1 nm Ti/49 nm Au) evaporated on glass substrates. Additional external components, which can be further integrated such as input light source and spectrometer, are also incorporated (for a detailed description of the biosensor device and working principle, please refer to the ESM). Briefly, the device tracks in real time the shift of the resonance peak (ΔλSPR) of the gold sensor chip that arises when refractive index changes occur on its surface, which are originated after binding or desorbing events occur (see ESM Figs. S1 and S2). Thus, the sensing is direct and label-free. The selected detection assay is based on an indirect competitive immunoassay, where a similar compound of the target analyte (i.e., competitor) is immobilized on the sensor surface and competes with the analyte for the binding of a fixed concentration of the specific antibody (see Fig. 2 for a representative scheme of the assay). In this way, the concentration of analyte is inversely proportional to the signal observed, being maximum at zero analyte concentration. The competitor in this case was the prolamin working group (PWG) gliadin, which contains the epitopes the antibody is specific for. A covalent attachment of the PWG gliadin was selected.
Sensor chip biofunctionalization and assay development
Details on the chemical and immunochemical reagents and buffers are summarized in the ESM. The formation of a self-assembled monolayer (SAM) onto the sensor chip surface was carried out using HS-C11-(EG)6-O-CH2-COOH in absolute ethanol (1 mM) after overnight incubation at room temperature. Then, sensor chips were rinsed with ethanol and dried with a N2 stream. Biofunctionalization procedure was performed in situ in order to optimize the immobilization conditions. Carboxylic groups of thiols were activated with a solution of 3(3-dimethylaminopropyl) carbodiimide hydrochloride (EDC), N-hydroxysulfosuccinimide (NHS) (EDC/NHS, 0.2 M /0.05 M) in MES buffer at a flow rate of 20 μL min−1 for 20 min. A solution of PWG gliadin (50 μg mL−1) in acetate buffer (pH 5.0) was injected after activation at a flow rate of 10 μL min−1 for 35 min. Then, the remaining unreacted carboxylic groups were deactivated with a solution of 1 M ethanolamine pH 8.5 at a flow rate of 30 μL min−1 for 2 min (see Fig. 2). An ex situ immobilization was also used to generate the sensor chips for routine-based analysis following the optimized conditions. In this case, for the activation step, 200 μL of the EDC/NHS solution was dropped over the SAM-functionalized sensor chips (20 min), followed by the overnight incubation at 4 °C with PWG gliadin (50 μg mL−1 in acetate buffer, pH 5.0) and the ethanolamine deactivation step (2 min). In between each step, sensor chips were rinsed with Milli-Q water and dried with a stream of N2. Chips were mounted on the optical device and kept in a continuous flow of PBST buffer at 25 μL min−1 before measurements.
A fixed concentration of each monoclonal antibody was chosen after performing non-competitive assays (i.e., in the absence of analyte) over PWG gliadin–biofunctionalized sensor chips: G12 mAb (2 μg mL−1) and A1 mAb (5 μg mL−1). The antibody concentration was selected so that (i) it enabled the analysis under non-saturation conditions in PBST buffer and (2) the signal was high enough to allow monitoring a broad range of analyte concentrations (data not shown). A stock solution of target α2-gliadin 33-mer peptide (1 mg mL−1 in PBS) was used to prepare the standards to obtain the calibration curve (from 0.1 ng mL−1 to 4.0 μg mL−1 in PBST buffer) using both antibodies. The incubation time between the antibody and the analyte was set to 15 min at room temperature. Sample containing the antibody-analyte mixture was then flowed through the sensor chip at a flow rate of 25 μL min−1. Free antibodies not bound to the 33-mer peptide in solution can then interact with the immobilized PWG gliadin. Total dissociation of the antibody-PWG gliadin interaction was efficiently accomplished by injecting a 5 mM NaOH solution during 120 s. Calibration curves for the 33-mer peptide detection were obtained by representing the signal (obtained after signal stabilization t ~ 800 s) vs concentration. The average (ΔλSPR) and standard deviation (SD) of triplicate analysis were graphed, and the data were adjusted to a dose-response inhibition equation, as described elsewhere [26, 27]. The analytical parameters such as limit of detection (LOD), the half inhibitory concentration (IC50), and the working range (the interval between IC80 and IC20, which defines the linear range of the assay) were calculated. Intra-assay (two calibration curves obtained with the same biofunctionalized sensor chip) and inter-assay (three calibration curves obtained with three different biofunctionalized sensor chips) variability was assessed.
Analysis of urine samples
The effect of urine on the assay performance (i.e., non-specific adsorption) was removed by adding a blocking layer consisting of BSA 10 mg mL−1 diluted in PBST. This solution was injected over the sensor chip for 2 min right before the injection of each urine sample. The conditions to achieve full removal of non-specific adsorptions from urine are summarized in the ESM. Control experiments related to the effect of urine were done with urine collected from group 1 donors (i.e., adhered to a GFD and therefore, with no 33-mer peptide present). The effect of urine in the assay was evaluated with calibration curves generated using α2-gliadin 33-mer peptide standards prepared in urine from group 1 donors. Additional calibration curves were obtained for GIP instead of only 33-mer peptide by using real urine sample containing digested GIP. The GIP concentration of this urine sample was previously quantified with the lateral flow test iVYCHECK GIP Urine™ and the iVYCHECK GIP Reader™. The sample was subjected to a preconcentration step using centrifugal filters Amicon Ultra 10 kDa to obtain a stock GIP solution of known concentration. Then, a set of serial dilutions at different concentrations of GIP were prepared with group 1 urine as solvent and analyzed with each monoclonal antibody. Finally, 21 patient samples from group 2 donors were directly analyzed with the biosensor and the concentration of GIP calculated from the calibration curves. The results were compared with those values determined with the commercial detection assay (iVYCHECK GIP Urine™, Biomedal) and expressed as percentage recovery:
Those urine samples whose concentration fell below the LOD were preconcentrated before analysis using the centrifugal filters Amicon Ultra 10 kDa. Samples whose concentration was above the working range required additional dilution using group 1 urine. All samples were analyzed in triplicate.
Results and discussion
Bringing diagnostics close to the primary care or to the patient itself requires simple, yet sensitive, fast, and direct analysis of a readily extracted sample. Urine sample is ideal; however, its direct detection is not always possible depending on the detection assay. Manipulation of the sample to obtain a reliable signal commonly involves sample pretreatment or dilution at best, eventually affecting the sensitivity required and moving away from the concept of point-of-care. Our detection assay is based on an indirect competitive assay performed on a label-free optical device, and we have newly customized the sensing chip biofunctionalization to facilitate the direct addition in urine and to extend the half-life of the biosensing chips.
Immunoassay development
Two monoclonal antibodies (G12 and A1) with a high affinity for 33-mer peptide have been considered for the assay development. They show reactivity to different prolamin epitopes from wheat, barley, rye, and some oat varieties. The G12 mAb recognizes QPQ-(L/Q)-P-(Y/F) and A1 mAb reacts against the epitopes Q-(Q/L)-P(Y/F)-PQP. Both antibodies are currently used in research, food analysis, and clinical monitoring of CD and implemented in commercial assays such as ELISA and LFT for the detection of GIP excreted in human feces and urine [22, 28,29,30]. For the indirect competitive assay, PWG gliadin (MW ~ 33 to 45 kDa), which contains the epitopes the antibody is specific for, is immobilized on the sensor chip surface at a fixed concentration and competes with the free 33-mer peptide (or the family of GIP in a real sample) for the binding of the monoclonal antibodies (G12 or A1) (see Fig. 2). To facilitate the attachment of PWG gliadin, a self-assembled monolayer (SAM) with reactive groups (-COOH group) was added to the gold sensor chip.
Contrary to the use of conventional aliphatic thiolated compounds (i.e., mercaptoundecanoic acid or mercaptohexadecanoic acid), in this case, we have selected thiol groups containing ethylene glycol units in their structure in order to prevent non-specific adsorptions from the urine matrix [31, 32]. A reactive compound (HS-C11-(EG)6-O-CH2-COOH) and an inert one (HS-C11-(EG)4-OH) used as lateral spacer to spread the PWG gliadin on the sensor chip surface were initially selected. Parameters such as SAM composition at different COOH:OH molar ratios (3:7, 1:1, 7:3, and 1:0) and suitable buffer to attach the PWG gliadin (50 μg mL−1) were tested (see ESM Fig. S3A). Those conditions resulting in higher PWG gliadin immobilization signal (ΔλSPR 12.7 ± 1.5 nm) were selected (SAM ratio COOH:OH 1:0 -no spacers- and acetate buffer pH 5.0 for PWG gliadin immobilization). According to the results obtained, acid pH (between pH 4.0 and 5.5) can improve considerably the immobilization signal due to the electrostatic interactions between the SAM layer and the PWG gliadin (i.e., it increases the local concentration of PWG gliadin on the surface, resulting in a more efficient coupling yield). ESM Fig. S3B shows a real-time sensorgram of an in situ immobilization for the selected conditions. Then, the in situ immobilization was adapted to an ex situ strategy, with the aim of generating enough sensor chips to perform routine analysis and to study their stability over time. The same signal for the antibody detection was virtually obtained over gliadin-coated sensor chips functionalized via either the in situ or the ex situ protocol (i.e., ΔλSPR 1.2 ± 0.1 for G12 mAb and 1.0 ± 0.1 for A1 mAb; see ESM Fig. S3C), confirming that both procedures were equally effective and that the biofunctionalization is stable and reproducible. The optimal concentration of antibodies was determined by non-competitive assays. Moreover, the total dissociation of the PWG gliadin-antibody interaction was guaranteed using NaOH 5 mM without damaging gliadin integrity, allowing the repeated use of the sensor chip. The recognition layer was viable for at least 20 cycles of interactions with G12 mAb and 32 cycles with A1 mAb (see ESM Fig. S4A and B, respectively). Under these conditions, calibration curves using both antibodies were obtained by measuring different 33-mer peptide concentrations.
ESM Fig. S5 shows two representative calibration curves using both mAbs and different 33-mer peptide concentrations in PBST buffer. ESM Table S1 shows the analytical parameters of the curves. The LOD using G12 mAb is around one order of magnitude lower than A1 mAb (i.e., ~ 2 ng mL−1 and ~ 20 ng mL−1, respectively). Also, the sensitivity reflected in the IC50 values is more than one order of magnitude better for G12 mAb assay. Nevertheless, the working range for the assay with A1 mAb is wider compared with the one obtained with G12 mAb, as a direct consequence of its lower slope (i.e., ~ − 1.4 for G12 mAb assay and ~ − 1 for A1 mAb assay), which extends the measurement range. This eventually can be an advantage as a higher number of real samples may fall within this range and, therefore, this increases the assay capabilities. The intra- and inter-assay evaluation confirms the high reproducibility and stability of the immunoassays in the same sensor chip or in different sensor chips, especially in the case of the G12 assay. ESM Fig. S6A and B show representative sensorgrams obtained for different 33-mer peptide concentrations for both G12 and A1 assays which exemplify the low level of noise of the signals for each measurement.
Effect of the urine in the assay performance
Urine, as any other human fluids, can affect the immunoassays, as it is commonly reported [26, 33], hindering either by the interaction between the receptor and the target or by the non-specific adsorption of some of its components on the sensor surface. This eventually results in worst assay performance, being necessary the implementation of sample pretreatment or dilution steps. To minimize or avoid any of these undesired effects, we have employed thiols containing ethylene glycol units in their structure (EG-thiols) [31]. The generation of this ethylene glycol layer did not however completely remove non-desired adsorptions when analyzing pure urine (see red sensorgram in the Fig. 3a, λSPR ~ 0.5 nm) or even after diluting urine 50% (blue sensorgram in Fig. 3a, λSPR ~ 0.25 nm). Nevertheless, introducing an extra blocking step consisting of BSA (10 mg mL−1 in PBST) for 2 min before each urine sample analysis, resulted in the formation of an extra layer (as evidenced by the resultant positive signal of ΔλSPR around 0.12 ± 0.02 nm; see ESM Fig. S7A) with antifouling properties which completely suppressed any kind of adsorptions derived from urine (see Fig. 3a, green and orange sensorgrams for 50% and urine 100%, respectively, where ΔλSPR ~ 0). The experimental conditions of this extra step were precisely optimized to achieve maximum efficiency (see the ESM for detailed description and Fig. S7 therein). Moreover, under these conditions, the addition of BSA did not seem to affect the interaction of the antibody with the PWG gliadin layer, as signals for both G12 and A1 antibodies remained the same as can be checked in Fig. 3b. The regeneration and reusability of such sensor surfaces were similarly assessed, and a slightly higher deterioration was observed compared with PBST measurements (see ESM and Fig. S7C, D). Nevertheless, it was still possible to have active sensor surfaces for around 15–17 cycles, for both G12 and A1 antibodies. The inter-assay variability was also very low, as observed when evaluating the signal obtained within different sensor chips prepared with the same conditions (see ESM Fig. S7E).
a Blocking effect of BSA (10 mg mL−1) to minimize non-specific adsorptions of urine. b Comparison of antibody signals in PBST, urine-PBST 1:1, and undiluted urine. G12 mAb = 2 μg mL−1 and A1 mAb = 5 μg mL−1 over surfaces blocked with BSA (10 mg mL−1). c Calibration curve for 33-mer peptide in PBST, urine-PBST 1:1, and urine 100% using G12 mAb = 2 μg mL−1 and d using A1 mAb = 5 μg mL−1. Each point represents the mean ± SD of three replicates
Complete calibration curves prepared directly in urine 100% indeed demonstrate that the developed strategy does not affect at any level the assay performance compared with 50% urine or in PBST (see Fig. 3c, d for calibration curves with G12 and A1 antibodies, respectively, and Table 1 for a summary of the assay analytical features). As can be observed, the differences are minimal and the curves look analogous. The LOD and IC50 are very similar for both 100 and 50% urine, which confirm the excellent effect that the extra blocking with BSA causes regarding the removal of any interference. A slight variation in the LOD and in the slope of the assay is observed, compared with PBST buffer (i.e., it decreases as the amount of urine increases) which translates in broader working range when whole urine is analyzed although these differences are minimal, thus not hindering the attempt of directly analyzing real samples. Real-time sensorgrams for different 33-mer peptide concentrations incubated with both G12 and A1 antibodies are shown in ESM Fig. S8A, B.
Selectivity of G12 and A1 mAb for GIP in real urine samples
Previous studies have demonstrated the capability of G12 and A1 mAbs of recognizing other toxic immunogenic peptides generated from gluten (GIP) present in wheat, barley, rye, and oats. The affinity however varies significantly depending on the epitope. From those studies, A1 showed a broader specificity than G12 [18, 34]. After consumption of gluten from different origins, several GIP will be present in the patient’s urine and their quantification might therefore be affected due to the recognition pattern of the antibody employed. Therefore, in order to mimic a real sample analysis, calibration curves with both antibodies were done using a mixture of GIP obtained from a real urine sample instead of single 33-mer peptide, applying the optimal conditions described above. Figure 4 shows the calibration curves obtained in urine 100% using GIP with G12 mAb (purple) and A1 mAb (orange), which are compared with those obtained with 33-mer peptide for G12 mAb (blue) and A1 mAb (green). Calibration curves of 33-mer peptide and digested GIP obtained with G12 mAb (blue and purple lines) were very similar in terms of analytical parameters, such as the LOD and the linear range (see data summarized in Table 1). These results highlight the high specificity of the G12 mAb to directly measure the 33-mer peptide in urine in a set of gliadin-derived peptides without affecting the resulting average sensitivity. On the contrary, for the case of A1 antibody assays (green and orange calibration curves), although the LODs were similar, the IC50 was twice smaller when using GIP mixture, which reflects that the recognition pattern of this antibody indeed includes other peptides, maybe with even higher affinity than for 33-mer peptide [35]. Also, using GIP as target analyte resulted in a more restricted working range (i.e., the calibration curve has a higher slope than for 33-mer (0.864 vs 0.623)), but still broader than the one obtained with G12 mAb. These characteristics may eventually benefit the real sample analysis, by avoiding previous dilution in highly concentrated samples, for example. Nevertheless, in a more real scenario where the target analyte is a mixture of peptides, the assay using G12 mAb offers a better sensitivity for GIP than using A1 mAb. Besides, the coefficients of variability (CV) of key parameters of 33-mer and GIP immunoassays with G12 mAb, which are significantly improved (see ESM Table S2) compared with the one obtained in PBST (shown in ESM Table S1), proved the excellent reproducibility and great robustness of our plasmonic biosensor. Moreover, for the case of G12 mAb–based assay, our biosensor device offers a better performance than the semi-quantitative lateral flow test (iVYCHECK GIP Urine™), which relies on the use of A1 and G12 antibodies. The SPR-based assay needs only one epitope per molecule, so it could detect shorter GIP than iVYCHECK GIP Urine™, which in this case requires the presence of two epitopes in the peptide to be detected via sandwich assay. Moreover, A1 antibody has very low affinity for deamidated peptides. Considering that one of the main processes of gluten to become more immunogenic is the deamidation by tissue transglutaminase, it may be possible that deamidated peptides are underestimated by the lateral flow immunoassay. Additionally, the iVYCHECK GIP Urine™ test is capable of detecting GIP in urine in the range of 6.48–100 ng mL−1 although it requires a sample extraction or dilution pretreatment in order to isolate the peptides and/or to remove interferences [22, 36]. Conversely, our biosensor can directly analyze the urine collected from the individuals and no additional treatment (besides adding the antibody to the sample) is needed, with an even lower LOD, set at 1.6 ng mL−1. This biosensor assay also outperforms previous results [26], which required urine dilution to remove urine undesired effect and properly quantify GIP levels, without sacrificing the detectability levels.
Calibration curves in urine 100% obtained using as follows: 33-mer peptide and G12 mAb (blue); 33-mer peptide and A1 mAb (green); GIP extracted from urine and G12 mAb (purple); GIP and A1 mAb (orange). Each point represents the mean ± SD of three replicates obtained with three different sensor chips
Sensor chip storage and stability
The stability over time of the sensor chips was studied following a systematic optimization of several sensitive parameters (data not disclosed due to confidentiality). Under the optimal conditions of preparation, biofunctionalization, and storage, we observed that the biofunctionalized sensor chips were stable for up to 6 months without affecting their integrity and functionality, as can be seen in ESM Fig. S9, where urine samples spiked with 33-mer peptide (at the corresponding IC50 concentration) were analyzed after different span times. As can be observed, very similar signals were obtained for the two assays using either G12 or A1 antibodies (CV of 3.58% and 11.30% respectively), which is indicative of the excellent robustness and stability of our protocol for at least the evaluated period of time.
Validation with real urine samples
In order to evaluate the accuracy and reliability of the biosensor device, 21 urine samples collected from group 2 donors (healthy volunteers who had previously ingested a certain amount of gluten) were analyzed with our plasmonic biosensor and the data compared with the results obtained with the iVYCHECK GIP Urine™ test [22]. The signals were interpolated in both G12 and A1 mAb calibration curves of digested GIP. Each sample was measured three times obtaining the average, standard deviation, and the recovery. Results are summarized in Table 2. The accuracy offered by our approach is excellent, with recovery values of 96–101% and 91–111% for both G12 and A1 antibody assays, respectively. The excellent correlation of our biosensor device with the iVYCHECK GIP Urine™ test can be seen also in Fig. 5 with an almost perfect correlation (i.e., slope close to 1 in both cases, 0.96 for G12-based assay and 1.03 for A1-based assay). As can be seen in the correlation plot, for higher concentrations (> 80 ng mL−1), a slight drift appears, with a tendency to increase the slope (i.e., overestimate) for the A1-based assay and with a trend to decrease the slope (i.e., underestimate) for the G12-based assay. These trends, however, are not that significant for the range of concentration evaluated. Moreover, the level of precision and reproducibility is also evident from the SD values observed for each of the samples. Overall, the performed validation corroborates the excellent features achieved with our biosensor approach, in terms of reproducibility, accuracy, and precision for the quantification of GIP.
Evaluation of the biosensor device for low gluten intake diet follow-up
We have performed a quantitative test to monitor the consumption of gluten in diet. The G12-based assay was selected because of its lower limit of quantification (LOQ = IC80 of 3.4 ng mL−1) compared with the A1-based assay (9.1 ng mL−1). Urine samples were collected from two healthy volunteers from group 2, who had an uncontrolled gluten diet (UGD). Later, they started a supervised gluten-free diet for at least 36 h. Between days 1 (24 h) and 2 (48 h), urine samples were collected to corroborate that the volunteers had adhered to a GFD for a sufficient time. In the next days, volunteers ingested a certain amount of gluten every day (50, 150, and 250 mg at night at the same time each day). Urine samples were collected in the morning each day. The G12 antibody was directly added to the urine samples and incubated for 15 min before analyzing them with the biosensor as described above. Figure 6 shows the evolution of GIP concentration in urine during the controlled gluten diet. As expected, maximum levels of GIP were observed during regular diet (first day) which significantly decreased after the 36-h period of non-gluten consumption (which fell around the LOQ of the assay (around 4 ng mL−1)). Then, the gradual increase in the gluten intake nicely correlates with an increase in the concentration of peptides excreted in urine. This representative study exemplifies the great potential our biosensor device has as a convenient tool for diet monitoring or for disease therapy follow-up.
Levels of GIP in urine collected from two individuals determined with the G12 mAb biosensor during a controlled low gluten intake. The monitoring was done during a regular diet, followed by 2 days of GFD, and by a controlled gluten intake of 50, 150, and 250 mg in the following days. Each point represents the mean ± SD of triplicate measurements (sample corresponding to a gluten intake of 250 mg for patient 2 was not collected)
Conclusions
We have developed a plasmonic device that allows rapid, highly reproducible, accurate, and non-invasive gluten intake control using a small amount of patient’s urine (200 μL). We demonstrate that with the explicitly designed biofunctionalization protocol, the plasmonic biosensor directly quantifies GIP generated after digestion of gluten and excreted in the urine. No extraction or any other type of sample pretreatment or purification is needed, which greatly simplifies the analysis and speeds up its implementation as an autonomous POC device that could be easily used by celiac patients to monitor their own adherence to GFD. Excellent levels of sensitivity and specificity are reached using two different monoclonal antibodies (G12 and A1) that show a different recognition pattern of GIP. In both cases, the LODs achieved (around 1.6 and 4.0 ng mL−1 respectively) guarantee the detection of minimal quantities of GIP even after low gluten intake. This device shows exceptional reproducibility and reliability, exemplified in the intra- and inter-assays’ low variability and the low CV% obtained when measuring replicates of urine spiked samples over time with different chips, and very good accuracy, demonstrated in the correlation analysis with a significant number of real samples, reaching recoveries close to 100%. All of this corroborates the feasibility and robustness of the developed biosensing method. So far, the biosensor chips show a promising storage stability of 6 months although further studies will cover a broader time span to ensure a storage capability in compliance with commercialized tests standards. Moreover, further integration of the biosensor chip in a disposable microfluidics cartridge will enable their integration and potential manufacturing. This biosensing strategy implemented in the plasmonic biosensor is highly attractive to monitor the treatment of celiac disease and to assess any potential infringement of a gluten-free diet, as it has been illustrated with the tracking of the GIP levels in two individuals subjected to a controlled gluten diet. Overall, the developed biosensor device holds great potential as a convenient sensing tool for the label-free non-invasive celiac disease follow-up, for promoting self-monitoring of celiac patients in the daily life, and it reduces the need for additional invasive investigations on follow-up.
References
Green PHR, Lebwohl B, Greywoode R. Celiac disease. Allergy Clin Immunol. 2015;134:1099–106.
Comino I, Real A, De Lorenzo L, Cornell H, López-Casado MA, Barro F, et al. Diversity in oat potential immunogenicity: basis for the selection of oat varieties with no toxicity in coeliac disease. Gut. 2011;60:915–22.
Sharma GM, Pereira M, Williams KM. Gluten detection in foods available in the United States - a market survey. Food Chem. 2015;169:120–6.
Bernardo D, Peña AS. Developing strategies to improve the quality of life of patients with gluten intolerance in patients with and without coeliac disease. Eur J Intern Med. 2012;23:6–8.
Valenti S, Corica D, Ricciardi L, Romano C. Gluten-related disorders: certainties, questions and doubts. Ann Med. 2017;49:569–81.
Castillo NE, Theethira TG, Leffler DA. The present and the future in the diagnosis and management of celiac disease. Gastroenterol Rep. 2015;3:3–11.
Esteve M, Rosinach M, Llordés M, Calpe J, Montserrat G, Pujals M, et al. Case-finding in primary care for coeliac disease: accuracy and cost-effectiveness of a rapid point-of-care test. United Eur Gastroenterol J. 2018;6:855–65.
Polanco I, Koester Weber T, Martínez-Ojinaga E, Molina M, Sarria J. Efficacy of a point-of-care test based on deamidated gliadin peptides for the detection of celiac disease in pediatric patients. Rev Esp Enferm Dig. 2017;109:743–8.
Garnier-Lengliné H, Cerf-Bensussan N, Ruemmele FM. Celiac disease in children. Clin Res Hepatol Gastroenterol. 2015;39:544–51.
Harris LA, Park JY, Voltaggio L, Lam-Himlin D. Celiac disease: clinical, endoscopic, and histopathologic review. Gastrointest Endosc. 2012;76:625–40.
Meresse B, Malamut G, Cerf-Bensussan N. Celiac disease: an immunological jigsaw. Immunity. 2012;36:907–19.
Jnawali P, Kumar V, Tanwar B. Celiac disease: overview and considerations for development of gluten-free foods. Food Sci Hum Wellness. 2016;5:169–76.
Jabri B, Sollid LM. T cells in celiac disease. J Immunol. 2017;198:3005–14.
Stamnaes J, Sollid LM. Celiac disease: autoimmunity in response to food antigen. Semin Immunol. 2015;27:343–52.
Moreno ML, Rodríguez-Herrera A, Sousa C, Comino I. Biomarkers to monitor gluten-free diet compliance in celiac patients. Nutrients. 2017;9:1–14.
I.F.S. Codex Alimentarius. Standard for foods for special dietary use for persons intolerant to gluten CODEX STAN118-1979., http://www.codexalimentarius.net. (2019). http://www.codexalimentarius.net. Accessed 13 Feb 2019.
Moreno ML, Cebolla A, Munõz-Suano A, Carrillo-Carrion C, Comino I, Pizarro A, et al. Detection of gluten immunogenic peptides in the urine of patients with coeliac disease reveals transgressions in the gluten-free diet and incomplete mucosal healing. Gut. 2017;66:250–7.
Comino I, Real A, Moreno ML, Montes R, Cebolla A, Sousa C. Immunological determination of gliadin 33-mer equivalent peptides in beers as a specific and practical analytical method to assess safety for celiac patients. J Sci Food Agric. 2013;93:933–43.
Tommasini A, Not T, Ventura A. Ages of celiac disease: from changing environment to improved diagnostics. World J Gastroenterol. 2011;17:3665–71.
Leja M, Kojalo U, Frickauss G, Bandere B, Gavars D, Viesturs B. Changing patterns of serological testing for celiac disease in Latvia. J Gastrointest Liver Dis. 2011;20:121–6.
Mubarak A, Wolters VM, Gmelig-Meyling FHJ, ten Kate FJW, Houwen RHJ. Tissue transglutaminase levels above 100 U/mL and celiac disease: a prospective study. World J Gastroenterol. 2012;18:4399–403.
Moreno ML, Sousa C, Rodriguez A, Cebolla A. Detecting gluten peptides in human fluids (2016). WO/2016/005643, Filed July 9, 2015, Published January 14, 2016.
Bienvenu F, Anghel SI, Besson Duvanel C, Guillemaud J, Garnier L, Renosi F, et al. Early diagnosis of celiac disease in IgA deficient children: contribution of a point-of-care test. BMC Gastroenterol. 2014;14:186.
Benkebil F, Combescure C, Anghel SI, Besson Duvanel C, Schäppi MG. Diagnostic accuracy of a new point-of-care screening assay for celiac disease. World J Gastroenterol. 2013;19:5111–7.
Wu H, Wallach M, Shimoni O. Challenges with point-of-care tests (POCT) for celiac disease. In Rodrigo L, Hernandez-Lahoz C, editors. Celiac disease - from the bench to the clinic. IntechOpen; 2019. p. 1–12.
Soler M, Estevez MC, Moreno ML, Cebolla A, Lechuga LM. Label-free SPR detection of gluten peptides in urine for non-invasive celiac disease follow-up. Biosens Bioelectron. 2016;79:158–64.
Peláez EC, Estevez MC, Portela A, Salvador JP, Marco MP, Lechuga LM. Nanoplasmonic biosensor device for the monitoring of acenocoumarol therapeutic drug in plasma. Biosens Bioelectron. 2018;119:149–55.
Morón B, Bethune MT, Comino I, Manyani H, Ferragud M, López MC, et al. Toward the assessment of food toxicity for celiac patients: characterization of monoclonal antibodies to a main immunogenic gluten peptide. PLoS One. 2008;3:1–13.
Comino I, Real A, Vivas S, Siglez M, Caminero A, Nistal E, et al. Monitoring of gluten-free diet compliance in celiac patients by assessment of gliadin 33-mer equivalent epitopes in feces. Am J Clin Nutr. 2012;95:670–7.
Real A, Comino I, Moreno ML, López-Casado MA, Lorite P, Torres MI, et al. Identification and in vitro reactivity of celiac immunoactive peptides in an apparent gluten-free beer. PLoS One. 2014;9:12–4.
De Vos K, Girones J, Popelka S, Schacht E, Baets R, Bienstman P. SOI optical microring resonator with poly(ethylene glycol) polymer brush for label-free biosensor applications. Biosens Bioelectron. 2009;24:2528–33.
Schilp S, Rosenhahn A, Pettitt ME, Bowen J, Callow ME, Callow J, et al. Physicochemical properties of (ethylene glycol)-containing self-assembled monolayers relevant for protein and algal cell resistance. Langmuir. 2009;25:10077–82.
Vega B, Calle A, Sánchez A, Lechuga LM, Ortiz AM, Armelles G, et al. Real-time detection of the chemokine CXCL12 in urine samples by surface plasmon resonance. Talanta. 2013;109:209–15.
Comino I, Real A, Gil-Humanes J, Pistón F, de Lorenzo L, Moreno ML, et al. Significant differences in coeliac immunotoxicity of barley varieties. Mol Nutr Food Res. 2012;56:1697–707.
Cebolla A, Moreno ML, Coto L, Sousa C. Gluten immunogenic peptides as standard for the evaluation of potential harmful prolamin content in food and human specimen. Nutrients. 2018;10:1–16.
Sousa C, Comino I, Real A, Vivas S, Cebolla A. Determination of levels of immunogenic gluten peptides in human samples (2013). WO/2012/089868, Filed December 28, 2011, Published July, 5, 2012.
Funding
We received financial support from URINETEST Project (Retos Colaboración URINETEST RTC-2016-5452-1). ICN2 is supported by the Severo Ochoa program from Spanish MINECO (Grant No. SEV-2017-0706).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Angel Cebolla is the CEO and shareholder of Biomedal SL, the company which owns the patent for the detection of GIP in urine and stools to check gluten consumption. Biomedal SL is the exclusive licensor of the products for determination of GIP in urine/stools by using A1 and G12 antibodies. Carolina Sousa is co-inventor of the patent for the detection of GIP in urine and stools.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Published in the topical collection featuring Female Role Models in Analytical Chemistry.
Electronic supplementary material
ESM 1
(PDF 1.12 mb)
Rights and permissions
About this article
Cite this article
Peláez, E.C., Estevez, MC., Domínguez, R. et al. A compact SPR biosensor device for the rapid and efficient monitoring of gluten-free diet directly in human urine. Anal Bioanal Chem 412, 6407–6417 (2020). https://doi.org/10.1007/s00216-020-02616-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-020-02616-6