Abstract
Rationale
The Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) classifies attention deficit hyperactivity disorder (ADHD) as a neurodevelopmental disorder that interferes with human functioning and development. As the clinical presentation of ADHD involves a deficiency in executive function, neurocognitive deficits involving distinctive neuropathological changes must be present for clinical diagnosis.
Objectives
The vesicular monoamine transporter (VMAT), specifically VMAT-2, plays a role in ADHD pathogenesis. In addition, experimental data show that the stimulants (amphetamines and methylphenidate) are first-line treatments for the condition because of their extensive interaction with VMAT-2. The interactions of peptides, bupropion, and nutritional supplements with VMAT-2 receptors have been researched, but more evidence is needed to elucidate their pharmacodynamic properties. Therefore, this literature review evaluated the current pharmacological treatment modalities, peptides, and nutritional supplements for ADHD that target the VMAT-2 system.
Methods, results, and conclusions
We obtained relevant studies from several platforms, including the National Center for Biotechnology, Clinical Key, Access Medicine, and PubMed. From the results of these studies, we observed that stimulants interact highly with the VMAT-2 transporter, with omega-3 fatty acids, peptides, and bupropion exerting some modulatory activity on VMAT-2. These agents should be considered for the future treatment of ADHD, although clinical-level research involving human participants is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The psychopathology of attention deficit hyperactivity disorder (ADHD) involves dysfunctions across several domains, including working memory, executive function, response inhibition, emotional control, and planning/organization (Stahl 2014). The affected brain regions include but are not limited to, the prefrontal cortex, mesolimbic system, basal ganglia, reticular activating system, hippocampus, amygdala, and ventral tegmental area (VTA) (Stahl 2014). The epidemiology and occurrence of ADHD in the United States are relatively high, with an incidence rate of 10.47% between 2021 and 2022 (Li et al. 2023), even though statistical research has shown that it can be overly diagnosed (Kazda et al. 2021). Therefore, effective treatment methodologies, diagnostic tools, and screening criteria must be diligently utilized in clinical practice and research.
ADHD is a developmental disorder that is four times more likely to be diagnosed in males than in females (Blum et al. 2008). In this manuscript, the general neurobiology of ADHD is emphasized; however, the text is focused on the critical first step of understanding monoamines and their interaction with the VMAT-2 protein. However, it is essential to understand that childhood development, age, and gender play a role in its pathological processes, even though these topics are beyond the scope of this manuscript.
In addition to diagnosis, at a molecular level, both norepinephrine (NE) and dopamine (DA) are neurotransmitters essential for adequate prefrontal cortex function. Imbalances in these neurotransmitters have been associated with learning disabilities, including ADHD (Blum et al. 2008). Changes in the prefrontal cortex white matter have also been associated with ADHD due to disorganized tracts projecting from this area (Blum et al. 2008), which attenuate circuitry between dopaminergic and adrenergic neurons. In addition, a dysfunctional vesicular monoamine transporter-2 (VMAT-2) system plays a role in ADHD pathogenesis and dopamine dysregulation. Therefore, the objective and purpose of this literature review is to investigate the VMAT-2 system in ADHD to understand the relationship between VMAT-2 and ADHD and its current pharmacotherapy.
Methods
A systematic search of relevant literature was conducted across several platforms, including the National Center for Biotechnology (NCBI), Clinical Key, Access Medicine, and PubMed. References were compiled to match journal specifications. This study did not involve experiments on human subjects, and articles obtained were done so through open-access rights and Creative Commons permissions.
VMAT-2 protein and ADHD: the linkage
VMAT-2 protein: discovery and function
The VMAT protein was discovered in 1992; it comprises VMAT-1 and VMAT-2 and is widely expressed in the mammalian central nervous system (CNS) (Alwindi and Bizanti 2023). VMAT-1 is predominantly expressed in the endocrine system, whereas VMAT-2 is primarily found in nervous tissue and neuroendocrine cells (Eiden and Weihe 2011; Wimalasena 2011). In the CNS, VMAT-2 translocates monoamines, specifically dopamine (Nickell et al. 2014), from axoplasm to the vesicular lumen. VMAT-2 has also been hypothesized to synthesize and store trace amines, including tyramine and phenylethylamine (Eiden and Weihe 2011), in trace amine receptors (particularly TAAR-1), a receptor distinctive from VMAT-2. As tyramine and phenylethylamine are trace amines with structures akin to the sympathomimetic structure of dopamine, norepinephrine, and serotonin, they may be promising agents for ADHD treatment. However, further research is needed (Burns and Kidron 2022). In addition, protein mapping has revealed VMAT-1 and VMAT-2 to be acidic glycoproteins derived from two distinct genes (Eiden and Weihe 2011). Sequence structuring has revealed transmembrane domains akin to plasma membrane monoamine transporter proteins (Wimalasena 2011). Secondary protein structures reveal high N- and C-terminal variability (Wimalasena 2011) in these two glycoprotein transporters.
VMAT-2 binding sites: an ADHD linkage
Recently, the VMAT-2 transporter has been shown to consist of two distinct sites that bind reserpine and tetrabenazine, with tetrabenazine implicated in the treatment of chorea in Huntington’s disease (Nickell et al. 2014). Reserpine and tetrabenazine reduce a cells’ capacity to store monoamines within the brain, with reserpine acting at peripheral sites, inhibiting involuntary movements. Extensive research is needed to clarify this finding, which may contribute to the involuntary and impulsive nature of ADHD.
The tetrabenazine-binding site on VMAT-2 is not pH-dependent, and high levels of catecholamines suppress its binding (Nickell et al. 2014), thereby prohibiting the depressive effect of reserpine. Nickell et al. (2014) also described the impact of lobeline and other agents, such as tetrabenazine, on the VMAT-2 transporter, which is discussed later, along with other naturalistic substances.
Studies elucidate the role of VMAT-2 in ADHD. Toren et al. (2005) showed that the platelet vesicular monoamine density (VMAT-2 specifically) was decreased in children with ADHD, suggesting that this specific transporter is responsible for the neurochemical changes observed in patients with ADHD. Furthermore, VMAT-2 can be replicated peripherally by the platelet vesicular monoamine transporter, which has been quantified to study monoamine metabolism. In addition, Lu and Wolf (1997) showed that the VMAT-2 mRNA was significantly increased in the ventral tegmental area (VTA) rostral and transitional zones in killed rat models after 3 days. However, 14 days after amphetamine cessation, no changes were observed in VMAT-2 mRNA expression; however, the reason for this result is unclear.
The amphetamines and VMAT-2: classical ADHD treatment
Amphetamine mechanism of action at VMAT-2 protein
Current psychopharmacology research shows that at high doses (non-therapeutic ranges), VMAT-2 can be “inhibited” by amphetamines, causing VMAT-2 vesicles to release the classical monoamines DA and NE into the axoplasm; however, this model is no longer broadly accepted (Eiden and Weihe 2011; Stahl 2014). Various models are depicted in Table 1.
For instance, Stahl (2014) reported that VMAT-2 is not affected by amphetamines at therapeutic doses but is affected at higher doses (Stahl 2014). However, research data from fly and rodent models have shown that in pharmacologically relevant quantities (therapeutic doses), amphetamines activate VMAT-2 like their effect at higher doses (Wimalasena 2011; Freyberg et al. 2016), lending clues to the role of VMAT-2 in the therapeutic response of patients with ADHD to amphetamines, contradicting the previous model.
Amphetamines interact with VMAT-2 in vitro (human studies are somewhat lacking), are non-substrate inhibitors of VMAT-2, and block DA accumulation in synaptic vesicles, allowing higher levels of DA to efflux into the axoplasm (Freyberg et al. 2016). Although pH changes during amphetamine administration have been explored, further research is required to better understand the mechanism of action of VMAT-2 at the molecular level (Stahl 2014). As the exact mechanism of action of amphetamines in VMAT-2 has not been elucidated, several different hypotheses (Wimalasena 2011; Freyberg et al. 2016) have been developed to explain the MOA of amphetamines in the VMAT-2 transporter.
VMAT-2 mechanism of action: the models
pH gradient model
A synaptic vesicle containing monoamines comprises two distinctive transporters in its plasma membrane (Fig. 1): the VMAT-2 transmembrane protein and a V-type ATPase pump (Fig. 2), ATP pumps that use ATP to pump hydrogen ions into vesicles. The VMAT-2 protein is a proton antiporter that relies on low luminal pH (acidic environment) for DA transport into vesicles (Wimalasena 2011). Because monoamine vesicles are relatively acidic (Wimalasena 2011) and have H+-ATPase pumps (V-ATPases) in addition to VMAT-2 monoamine antiporters (Freyberg et al. 2016), any disruption in the pH gradient can induce neurotransmitter release into the axoplasm.
The VMAT-2 transporter functions as a stoichiometric antiporter (moves one substance against its gradient and the other down its gradient) protein by removing two hydrogen ions from the vesicle in exchange for a monoamine transported into the vesicle against its concentration gradient. Because hydrogen ions are pumped out of the vesicle, monoamine accumulation increases protonation, which is the precise basis for the pH gradient model. Furthermore, the V-type ATPase transporter uses ATP to transport hydrogen ions into vesicles, which is the basis for its relative acidity compared to the more alkaline pH of the axoplasm (Guillot and Miller 2009).
Freyberg et al. (2016) discussed the importance of protonation of monoamines and amphetamines. As V-ATPase is ultimately responsible for loading monoamines through VMAT-2 into the vesicular lumen, monoamines are protonated. Furthermore, because amphetamines are basic, with pKA values between 8.8 and 9.9, they help decrease the vesicular pH gradient via a buffering mechanism that can release DA and block substrate import (Freyberg et al. 2016). Ultimately, this mechanism reduces the pH gradient and spills the vesicular contents into the axoplasm for subsequent exocytosis into the synaptic cleft for postsynaptic D1 or D2 binding. However, further research is needed, as few in vivo studies have been performed.
Freyberg et al. (2016) indicated that in Drosophila melanogaster fly models, amphetamines enter the VMAT-2 transporter in exchange for H + efflux out of the vesicle, increasing the vesicular pH and favoring DA release from the vesicle into the dopaminergic axoplasm, like another experiment (Sulzer and Rayport 1990). In this experiment, chromaffin granules were used, and three psychostimulants, including fenfluramine, imipramine, and tyramine, were found to reduce the pH gradient, causing a reduced uptake and increased release of neurotransmitters, along with inhibition of acidification of the vesicle.
Therefore, both experiments supported the pH gradient model, although further research using human models is required to confirm the in vivo effects of amphetamines. Furthermore, Freyberg et al. (2016) used whole-brain models with a dVMAT pHluorin sensor and showed that amphetamines required both VMAT-2 and a dopamine-associated transporter (DAT) to alkalinize the vesicular lumen. Chloroquine and amphetamine at 1 mM were used to alkalinize the VMAT lumen, and they were shown to cause deacidification of vesicular lumen contents relative to the starting acidic pH. Their findings indicated that when the total efflux of hydrogen ions exceeded the net influx of hydrogen ions by a VMAT-mediated mechanism, the pH gradient was disrupted, causing the release of neurotransmitters into axoplasm (Freyberg et al. 2016).
Sulzer and Rayport (1990) used chromaffin granules in animal models to determine the effect of psychostimulants on the pH gradient. At relevant doses, the alkalinizing effects of amphetamines, cocaine, and phencyclidine disrupted the delicate acidic gradient found in VMAT-2 transporters and their vesicles in cultured midbrain dopaminergic neurons. Because the pH gradient is reduced, neurotransmitter reuptake is reduced, causing subsequent monoamine release into the axoplasm (Sulzer and Rayport 1990). The pH gradient model is shown in Fig. 1.
Dopamine reuptake inhibition model
Even though experimental data favor the pH gradient model, scientists have shown that amphetamines function through a carrier-mediated exchange pathway. Partilla et al. (2006) used crude vesicular fractions from rat caudate assays. Their research showed that amphetamines tended to deplete monoamines in VMAT-2 transporters through a carrier-mediated exchange mechanism rather than through an alkaline agent, as was mentioned previously. Although they point to another potential mode by which amphetamines affect VMAT-2, the data remains inconclusive. Schwartz et al. (2006) showed that psychostimulants inhibit vesicular DA uptake in rat striatal synaptic vesicles through competitive inhibition in a concentration-dependent manner, exclusively depending on dosage. Higher concentrations of amphetamines enhanced the efflux of DA from VMAT-2 vesicles into the axoplasm, preparing DA for release into the synaptic cleft.
Redistribution model
Riddle et al. (2007) performed an immunoreactivity experiment in rodent models and showed that amphetamine and methylphenidate altered VMAT-2 immunoreactivity in rat neurons, redistributing VMAT-2 transporters within the synaptic nerve terminals. However, cytoplasmic transporters of vesicular glutamate, acetylcholine, and GABA were largely unaffected and were not translocated following amphetamine and methylphenidate treatment. High-dose amphetamine (2 mg/kg), but not methylphenidate, is involved in VMAT-2 trafficking, causing hyperlocomotive behavior, which is a novel finding (Riddle et al. 2007). Therefore, in ADHD treatment, dopaminergic and noradrenergic targeting is essential based on the interactions of VMAT-2 with stimulant medications, as discussed in the succeeding section.
Front-line ADHD treatment pharmacotherapeutic agents: the VMAT-2 linkage
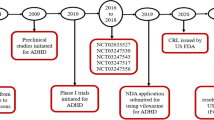
Lisdexamfetamine dimesylate
Lisdexamfetamine dimesylate (LDX) is a stimulant of the amphetamine class used to treat ADHD (Najib et al. 2017). LDX is an amphetamine prodrug consisting of a dextroamphetamine core structure covalently bound to a L-lysine amino acid group, which is hydrolyzed by the body to produce pure D-amphetamine (Blick and Keating 2007) following oral ingestion. LDX was designed to be as effective as alternative extended-release stimulant preparations, such as amphetamine salt combined with ER. Owing to its prodrug design, it has a diminished likelihood of adverse reactions and toxicity and a reduced potential for misuse or abuse (Nguyen et al. 2012).
Mechanism of action
Similar to traditional amphetamine products, this medication functions at the neuronal level through a specific mechanism. Several studies have shown the effectiveness of LDX compared to placebo in adults with moderate-to-severe ADHD. Substantial improvements in ADHD rating scales, Clinical Global Improvement scores, and executive function assessments across all doses of LDX (30–70 mg daily) have been reported (Biederman et al. 2012; DuPaul et al. 2012; Adler et al. 2013; Najib et al. 2017). The D-amphetamine produced by LDX can penetrate the blood–brain barrier and bind to specific sites within the CNS. This direct interaction leads to therapeutic benefits by enhancing the transmission of noradrenaline and DA neurotransmitters similar to amphetamine salts.
Drug interactions and contraindications
LDX lacks inhibitory activity toward cytochrome (CYP) CYP450 isoenzymes (FDA 2017). Notably, the active component of the medication, D-amphetamine, exerts a limited inhibitory effect on the activity of CYP2D6 (FDA 2017). The CYP2D6 cytochrome system plays a vital role in the metabolic breakdown of multiple anti-depressants and second-generation antipsychotic medications. Importantly, the administration of lisdexamfetamine dimesylate is contraindicated concurrent with or within two weeks of the use of monoamine oxidase inhibitors (MAOIs) (Najib 2009; Hutson et al. 2014; Najib et al. 2017). Patients with severe kidney impairment or end-stage renal disease are advised to lower the dosage of LDX and D-amphetamine because these medications are cleared from the body through the kidneys and cannot be eliminated via dialysis (Comiran et al. 2016; Najib et al. 2017).
Furthermore, acidifying and alkalinizing agents change the acidity or alkalinity, respectively, of substances that affect urinary pH as seen through psychopharmacology measures. Acidifying and alkalinizing agents decrease and increase, respectively, the levels of amphetamine in the blood (FDA 2017).
TAAR-1 modulation and neuroinflammation
LDX may indirectly affect Mitogen- activated protein kinase phosphate 3 (MAKP3) signaling and TAAR1 activation. The robust control of these receptors through the influence of LDX has been demonstrated in a previous study (Quintero et al. 2022). MAPK3 activation plays a crucial role in the downstream modulation of neuroinflammation by inducing specific anti-inflammatory cytokines (such as IL-2 and IL-10). Consequently, TAAR1 regulation is linked to MAPK3 activation (Quintero et al. 2022).
Notably, ADHD is associated with neuroinflammation and impaired immune regulation, highlighting potential connections between these factors. Although the inflammatory effects of LDX with respect to ADHD have not been assessed, recent studies have not found evidence of a relationship between LDX and the regulation of IL-10 (an anti-inflammatory cytokine responsible for managing the duration and intensity of the inflammatory response), TNFα, or IL-1β (proinflammatory cytokines) (Bristot et al. 2019; Quintero et al. 2022).
Amphetamine-dextroamphetamine
Amphetamine-dextroamphetamine is a CNS stimulant medication of the amphetamine class, with equal parts racemic amphetamine and dextroamphetamine, used to treat ADHD. This medication combines four salts: dextroamphetamine sulfate, dextroamphetamine saccharate, amphetamine sulfate, and amphetamine aspartate monohydrate. The alkalizing effects of combining the four salts increase drug efficacy.
Mechanism of action
Amphetamine-dextroamphetamine is a formulated medication that consists of three mixed amphetamine salt (MAS) beads, each designed for the immediate, pulsed-delayed, and extended release of amphetamine salts, presenting a unique pharmacokinetic pattern (FDA 2017). Similar to other MAS compounds, it impedes the reuptake of NE and DA, thereby increasing the levels of these monoamine neurotransmitters in synaptic spaces. Additionally, amphetamine salts may potentially hinder the activity of monoamine oxidase, further amplifying synaptic monoamine concentrations (Strawn and Picard 2017). This augmentation of noradrenergic and dopaminergic neurotransmission, particularly in the prefrontal cortex, contributes to improved attention, working memory, and processing speed in individuals with ADHD. Similar to conventional amphetamine products, Amphetamine-dextroamphetamine functions at the neuronal level by restricting the reuptake of NE and DA, causing an increased release of neurotransmitters into the extra-neuronal space (Strawn and Picard 2017). Currently, the interactions of Mydayis with TAAR-1 and its potential implications for neuroinflammation are being studied, furthering our understanding of its multifaceted mechanism of action (Garey et al. 2020).
Drug interactions and contraindications
Patients are at an increased risk of developing serotonin syndrome when they are administered a combination of MAOIs, selective serotonin reuptake inhibitors, and serotonin norepinephrine reuptake inhibitors for ADHD (FDA 2017). When co-administered with Cytochrome P450 2D6 inhibitors, patients may experience increased exposure to amphetamine products. Serotonin syndrome is a life-threatening disease with symptoms that include mental status changes, autonomic instability, and neuromuscular and GI symptoms (FDA 2017). Additionally, therapeutic doses of this medication were associated with peripheral vasculopathy and Raynaud’s phenomenon in all age groups. A decreased dosage or discontinuation of treatment remediates symptoms (FDA 2017).
Amphetamine-dextroamphetamine and VMAT-2 interactions
VMAT is a crucial protein found in presynaptic neurons and that plays a fundamental role in the packaging, storage, and release of neurotransmitters, specifically monoamines such as DA, NE, and serotonin. VMAT actively transports monoamine neurotransmitters from the cytoplasm to synaptic vesicles, which are small intracellular compartments within nerve terminals. These vesicles act as storage units for neurotransmitters before their release into synapses. VMAT uses the energy generated from proton movement across the vesicular membrane to transport monoamines into vesicles, maintaining their concentration, and protecting them from degradation by enzymes in the cytoplasm (Kameg and Fradkin 2021).
Amphetamine-dextroamphetamine is an indirect sympathomimetic agent that interacts with VMAT. It enters presynaptic neurons through the DA and NE transporters (DAT and NET, respectively). Once inside, these compounds cause reverse transport of DA and NE by VMAT from the vesicles into the cytoplasm (Majarwitz and Perumareddi 2023). This process, known as reverse transport or efflux, disrupts the normal storage of neurotransmitters within the vesicles, leading to increased cytoplasmic concentrations of DA and NE.
Increased cytosolic levels of neurotransmitters lead to their release into the synaptic cleft through DAT and NET, which are located on the presynaptic membrane (Majarwitz and Perumareddi 2023). This elevated release of DA and NE into the synapse enhances neurotransmission, affects signaling pathways, and influences various brain circuits involved in cognitive function, attention, motivation, and executive control (Kameg and Fradkin 2021).
The interaction of amphetamine-dextroamphetamine mixed compound with VMAT alters the normal neurotransmitter storage and release processes, contributing to the therapeutic effects of medications in conditions such as ADHD and narcolepsy (Kameg and Fradkin 2021).
Methylphenidate
Ritalin, the brand name for methylphenidate, is a prominent CNS stimulant used therapeutically for ADHD and narcolepsy (FDA 2009). Its inception in the 1950s marked considerable advancements in the pharmacological management of ADHD-related symptoms, primarily targeting deficits in attention, focus, and impulse control. Ritalin is a psychostimulant that acts by inhibiting DA and NE reuptake via DAT and NET, respectively. This mechanism enhances the synaptic concentrations of these neurotransmitters, thereby modulating neuronal communication in brain regions implicated in executive function and attention (FDA 2009). Over the years, Ritalin has garnered considerable clinical attention and has undergone refinements in formulation and dosing to optimize its therapeutic efficacy while minimizing adverse effects. Its widespread use in the pediatric and adult populations underscores its importance in the management of ADHD symptomatology (Huss et al. 2017).
Mechanism of action
Methylphenidate operates as a psychostimulant, primarily through its interaction with DA and NE neurotransmitters in the CNS. It is a potent inhibitor of DAT and NET, impeding their reuptake. In contrast, amphetamine operates by promoting the release of DA and NE from presynaptic neurons into the synaptic cleft via a process that involves the displacement of neurotransmitter-containing vesicles. Inhibition by methylphenidate leads to elevated concentrations of DA and NE in the synaptic cleft of neurons. By impeding the reuptake process, methylphenidate prolongs the availability and enhances the action of these neurotransmitters at postsynaptic receptors. This prolonged presence of neurotransmitters, particularly in areas implicated in attention, behavioral regulation, and executive function, disrupts “seeking” type behaviors and helps alleviate symptoms associated with ADHD. Increased dopaminergic and noradrenergic signaling contributes to improved concentration, focus, and impulse control, which are notable symptoms in individuals diagnosed with ADHD (FDA 2009). Therefore, the core mechanism of methylphenidate involves modulating the levels of neurotransmitters, particularly DA and NE, to foster enhanced neuronal communication and mitigate symptoms characteristic of ADHD.
Drug interactions and contraindications
Methylphenidate should not be administered to individuals who are currently using or have previously used MAOIs because of the potential adverse reactions, including a high risk of hypertensive crises in all populations above six years old. Caution is advised when combining Ritalin with pressor agents because of possible blood pressure effects. Its primary metabolism into ritalinic acid through de-esterification, rather than oxidative pathways, might decrease the efficacy of hypertensive medications (FDA 2009). Furthermore, racemic methylphenidate may interfere with the metabolism of certain drugs, such as coumarin anticoagulants, anticonvulsants, and tricyclic drugs, requiring possible dosage adjustments and monitoring when co-administered in all age groups (FDA 2009). Contraindications for Ritalin include heightened anxiety, tension, and agitation, which may be exacerbated by the co-administration. Additionally, it is contraindicated in patients with hypersensitivity to drugs, glaucoma, motor tics, family history, or diagnosis of Tourette’s syndrome (FDA 2009).
Methylphenidate and VMAT-2 interactions
Unlike other stimulants such as amphetamines that directly interact with VMAT, the mechanism of action of methylphenidate does not involve VMAT interactions. VMATs package neurotransmitters into synaptic vesicles for storage and subsequent release into the synaptic cleft upon neuronal stimulation, whereas methylphenidate impedes the reuptake of DA and NE, which promotes increased concentrations of these neurotransmitters in the synaptic clefts. The impact of methylphenidate on VMAT receptors or the storage and release of neurotransmitters from synaptic vesicles is not central to its mechanism (Di Miceli et al. 2022).
However, one study found that methylphenidate administration prompted a substantial increase in vesicular DA uptake and binding of dihydrotetrabenazine, a ligand for VMAT-2, within purified striatal vesicles obtained from treated rats (Sandoval et al. 2002). Notably, this effect was observed solely in the purified vesicle preparations and was not attributed to lingering methylphenidate from the initial treatment.
Moreover, methylphenidate treatment displayed differing impacts on VMAT-2 protein levels within distinct cellular fractions. An increase in the striatal vesicle subcellular fraction and a decrease in the plasmalemma membrane fraction could suggest that methylphenidate treatment initiates redistribution of the VMAT-2 protein, which potentially influences the trafficking of synaptic vesicles within dopaminergic neurons. Additionally, the involvement of dopamine D1 and D2 receptors in modulating the effects on VMAT-2 dynamics in the vesicular subcellular fraction suggests a complex interplay among methylphenidate, neurotransmitter receptors, and VMAT-2 function, necessitating further exploration for a comprehensive understanding of their interactions (Sandoval et al. 2002).
Alternative agents and VMAT-2: adjunctive ADHD treatment modalities
Polyunsaturated fatty acids
Omega-3, a polyunsaturated fatty acid (n-3 PUFA) derived from the diet, is a major component of the neuronal membrane and plays a crucial role in the development and function of the brain (Healy-Stoffel and Levant 2018). In a study involving spontaneously hypertensive rats, which were used as an established animal model of ADHD, deficiency in omega-3 fatty acids was linked to significantly higher locomotor activity than that in the control group, illustrating its effect on hyperactivity (Hauser et al. 2014). In addition to improved motor activity, an omega-3 enriched diet was observed to lead to alterations in novelty-seeking and anxiety behaviors, which are characteristic of ADHD. Combined supplementation of omega-3 and − 6 fatty acids have been shown to be an effective therapy for ADHD in children with or without methylphenidate (MPH) (Barragán et al. 2017) as and in children with ADHD refractory to MPH treatment (Perera et al. 2012). The supplementation of MPH with n-3 PUFA led to increased tolerability, which could contribute to medication compliance.
Mechanism of action and effect on VMAT-2
Although certain studies have found a correlation between n-3 PUFA deficiency and reduced DA neurotransmission (Healy-Stoffel and Levant 2018), its effect on VMAT-2 has yet to be elucidated. In rats conditioned with amphetamine, fish oil enriched in omega-3 fatty acids modulates the brain DA system by decreasing amphetamine-induced D1R and D2R release and increasing VMAT-2 density in the prefrontal cortex (Metz et al. 2019). In healthy humans, n-3 PUFA supplementation fails to significantly increase striatal VMAT-2 availability. Over the course of the 6-month study, subjects between 18 and 25 years old who were taking the FDA-approved formulation of n-3 PUFA showed a mean increase in docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) levels of 75% and 450%, respectively, as well as improved working memory performance but not through striatal VMAT-2 regulation (Narendran et al. 2012). In addition to the formation of cell membrane phospholipid bilayer, DHA and EPA act as precursors for synthesis of specialized pro-resolving mediators, such as resolvins, protectins, and maresins with anti-inflammatory properties (Duvall and Levy 2016).
Bupropion hydrochloride
Background
Bupropion hydrochloride (Bupropion), commonly sold under the brand name Wellbutrin, is used as a non-stimulant treatment for ADHD (Verbeeck et al. 2017). Bupropion functions as a non-competitive antagonist of nicotinic acetylcholine receptors and is a member of the aminoketone class of anti-depressants, designated as (±)-1-(3-chlorophenyl)-2-[(1,1-dimethylethyl)amino]-1-propanone hydrochloride. Serving as a DA and NE reuptake inhibitor, bupropion is associated with the redistribution of VMAT-2, similar to its stimulant counterpart methylphenidate (Rau et al. 2005). Although the database is currently limited, prevailing evidence suggests increased efficacy and tolerance of bupropion in children and adolescents with ADHD (Ng 2017).
Mechanism of action
Animal studies and human clinical trials have demonstrated that bupropion inhibits DA and NE reuptake (Stahl et al. 2004; Dhillon et al. 2008), with greater functional potency at the DA transporter. Commonly used as an anti-depressant, its actions on serotonergic transmission differ from those of other anti-depressants, as it does not pre- or post-synaptically alter serotonin neurotransmission. Consequently, the side effect profiles of dry mouth, nausea, and insomnia of the medication differ from the stereotypical side effects of anti-depressants (Stahl et al. 2004; Dhillon et al. 2008).
Drug interactions and contraindications
Human CYPs are involved in transforming bupropion into its active metabolite, hydroxybupropion. CYP2B6 almost exclusively mediates bupropion hydroxylation, implying a risk of toxicity when used concurrently with other pharmacological agents that interact with CYP2B6 (Hesse et al. 2000). Additionally, although competitive inhibition of CYP2D6 is minimal, using bupropion with the CYP2D6-metabolized drug desipramine resulted in a five-fold increase in desipramine levels, indicating a drug–drug interaction between the two (Reese et al. 2008). In addition to being contraindicated in individuals allergic or hypersensitive to bupropion, the administration of this medication is contraindicated by the concurrent use of monoamine oxidase inhibitors (Foley et al. 2006). Other contraindications for bupropion include seizure disorders and worsening mood and behavioral disorders.
Effects on VMAT-2
The role of VMAT-2 in DA distribution has been outlined extensively. VMAT-2 regulates cytoplasmic DA levels by sequestering free DA in synaptic vesicles. Amphetamines disrupt the proton gradient, which is crucial for DA uptake and is facilitated by VMAT-2 (Rau et al. 2005). Current research indicates that through the role of bupropion in inhibiting the DAT, the medication allows for the sequestration of free DA into synaptic vesicles. By inhibiting the access of methamphetamine to DAT, bupropion indirectly increases VMAT-2 activity (Heinzerling et al. 2014). This mechanism mimics the effects of MPD, a stimulant ADHD pharmacological agent, on the redistribution of VMAT-2 proteins, leading to increased vesicular DA uptake (Rau et al. 2005). Owing to its low potential for abuse, Wellbutrin is more suitable for ADHD treatment compared to its counterparts (Stahl et al. 2004). However, although MPD provides neuroprotection against oxidative damage caused by amphetamines, such as methamphetamine, bupropion could be toxic over prolonged use (Rau et al. 2005).
Effects on ADHD
Clinical evidence points to limited tolerance of mainstay stimulant medications for ADHD, highlighting the advantages of alternative non-stimulant treatment options, such as Wellbutrin (Ng 2017; Verbeeck et al. 2017). In pediatric populations, bupropion is better tolerated than MPD and has a comparable efficacy toward ADHD treatment (Ng 2017). In adult populations, low-quality evidence shows that bupropion decreases the severity of ADHD symptoms and has a tolerability similar to that of a placebo (Verbeeck et al. 2017). Current research on adult and pediatric populations highlights the potential benefits of using Bupropion as ADHD treatment but emphasizes the need for further research. Additionally, further studies on bupropion use in patients with ADHD with comorbidities of nicotine dependence or depression are needed (Maneeton et al. 2011).
Pituitary adenylate cyclase-activating polypeptide (PACAP)
Background
Pituitary adenylate cyclase-activating polypeptide (PACAP), encoded by ADCYAP1, is found in humans with diverse physiological functions. PACAP is structurally related to vasoactive intestinal peptide and acts by binding to both vasoactive intestinal peptide and PACAP receptors (Teng et al. 1998). Functionally, PACAP acts as a hypophysiotropic hormone that stimulates adenylate cyclase and elevates cAMP levels in target cells. In addition to its role as a hypophysiotropic hormone, PACAP serves as a neurotransmitter and neuromodulator, participating in the paracrine and autocrine regulation of various cell types (Velasco et al. 2022). Notably, PACAP has been implicated in posttraumatic stress disorder, with a specific genetic variant predominant in females, highlighting its potential role in neurobiological mechanisms underlying maladaptive responses to traumatic events (Velasco et al. 2022).
ADHD pathogenesis
The mechanism of action of PACAP and its role in ADHD involves intricate neurobiological pathways. PACAP is crucial in neurophysiological systems, including the stress response and fear memory, and acts through its receptors, particularly PAC1. Studies on PACAP-deficient mice revealed neurodevelopmental disorder-like (NDD)-like behaviors, such as hyperactivity and deficient pre-pulse inhibition, akin to ADHD symptoms. Notably, PACAP−/− mice exhibit abnormalities in the axon initial segment (AIS) length in layer 2/3 pyramidal neurons, a region associated with ADHD and autism spectrum disorder (Iwahashi et al. 2023). AIS, which is essential for proper neuronal function, was elongated in PACAP−/− mice, suggesting a link between AIS abnormalities and NDDs (Iwahashi et al. 2023). Interestingly, treatment with the ADHD drug atomoxetine not only ameliorated hyperactivity in PACAP−/− mice but also improved AIS abnormalities, indicating a potential therapeutic avenue for NDDs (Iwahashi et al. 2023). This study highlighted the intricate interplay between PACAP-, AIS-, and ADHD-related behaviors and provides insights into novel drug therapies for NDDs.
VMAT-2 Interaction
PACAP38, an isotype of PACAP, binds most effectively to the PAC1 receptor which is present in the nigrostriatal pathways specialized for dopaminergic transmission (Vaudry et al. 2000). One experiment investigated whether exposure to PACAP38 affected brain inflammation in mice that were administered methamphetamine (Guillot et al. 2008). PACAP38 was prepared as a lyophilized powder and administered subcutaneously. Mice exposed to methamphetamine that received PACAP38 showed decreased inflammation in the striatum and increased immunohistochemical tracing of VMAT2 compared to those that did not receive PACAP38 (Guillot et al. 2008). The increase in VMAT2 tracings in the PACAP38 group occurred in the absence of changes in the binding affinity (Km) of the stained VMAT2 proteins, suggesting that PACAP38 affected the production of VMAT2 rather than VMAT2 functioning. Therefore, PACAP38 may decrease methamphetamine-associated brain inflammation by increasing VMAT2 production (Guillot et al. 2008). In another study, an isotype of PACAP (PACAP27) was provided to a mouse model of Parkinson’s disease, and the concentration of thyroid-hormone-positive neurons was measured as a proxy for therapeutic benefit, given that TH-positive neurons are biomarkers for the decreased function of the dopaminergic neural system (Wang et al. 2008). The thyroid protein TH is required for intracellular DA transport (Korchynska et al. 2022). In a mouse model of Parkinson’s disease, PACAP27 modulated the expression of VMAT2 in a dose-dependent manner (Wang et al. 2008). Specifically, a 2 µg/day dose of PACAP27 resulted in increased production of VMAT2, and a 0.2 µg/day dose of PACAP27 resulted in decreased production of VMAT2 (Wang et al. 2008). Collectively, these findings suggest that for specific PACAP isotypes, PACAP has a threshold concentration, above which it may not directly affect VMAT2 activity and, therefore, DA signaling in the brain.
Lobeline
Lobelia inflata, also known as lobeline, is found in Indian tobacco products. It was extracted from an alkaloid mixture in 1838 and has been extensively used in alternative medicine for anti-spasmodic, diuretic, emetic, myorelaxant, and stimulant effects, in addition to its ability to reverse narcotic overdose. This alkaloid interacts with both VMAT2 and nicotinic acetylcholine receptors, and various other neurotransmitter transporter systems (Crooks et al. 2011). Interestingly, lobelines reduce the behavioral effects of psychostimulants, making them an excellent adjunctive therapy for reducing the risk of stimulant addiction.
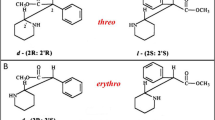
Pharmacodynamics, VMAT-2, and ADHD
Importantly, lobeline has a high affinity for nicotinic acetylcholine receptors and is a nicotinic agonist even though it is structurally similar to nicotine (Barlow and Johnson 1989). This is important for producing some of its anti-spasmodic effects and even tobacco cessation. Further exploration of these effects are beyond the scope of the present review.
Regarding VMAT-2, lobeline is an inhibitor of the [3H] dihydrotetrabenazine-binding site on VMAT-2 and inhibits DA uptake into rat striatal vesicles (Teng et al. 1997). Its affinity for VMAT2 is approximately 100× higher than that of DAT. Furthermore, instead of increasing the effects of amphetamines, lobeline inhibits amphetamine-induced DA release in a concentration range that inhibits VMAT-2, but not DAT. This could be an excellent treatment choice for individuals who are dependent on amphetamines and those with ADHD to reduce the side effects caused by stimulants at the presynaptic terminal by interacting with the tetrabenazine binding site on VMAT-2.
Few experiments have used lobeline to treat ADHD. However, Martin et al. (2018) employed 42 human participants, with nine completing the seven-day protocol of lobeline and methylphenidate administration. The participants received a methylphenidate capsule followed by a lobeline tablet after 1 h. Next, the participants were given a 15-min assessment of cognition to determine whether lobeline had a favorable effect on ADHD symptoms. The results showed that in adults with ADHD, lobeline had improved their working memory, but did not affect their attention and produced nausea as an adverse effect. This lends clues to the pharmacodynamic properties of lobelines in promoting DA release and inhibiting VMAT-2. Further studies are required to elucidate this phenomenon.
Conclusion
ADHD and VMAT-2 have pathophysiological associations; therefore, medications targeting the VMAT-2 system could effectively treat ADHD. These medications are predominantly stimulants, including lisdexamfetamine, mixed amphetamine salts, and methylphenidate. For the purpose of this review, we used the pH gradient model, in which amphetamines disrupt the pH gradient; it explained the plethoric effects of amphetamines. In addition, bupropion, an off-label agent for ADHD, has a moderate VMAT-2 interaction and could be investigated further in psychiatric medicine. Other agents, including lobeline, PACAP, and omega-3 fatty acids, have also been implicated in the VMAT-2 system, which may explain some of their efficacy. However, they are more likely to be adjunct treatments for ADHD than standalone modalities. VMAT-2 inhibitors and ligands can be developed for ADHD but must first be tested in animal models before being tested on humans to ensure quality, safety, and efficacy. This review focused on the critical first step of understanding the monoamines, specifically DA, and their complex interaction with VMAT-2 protein complex. However, future research should clarify how other physical elements, such as development and sex, contribute to childhood ADHD progression and pathophysiology.
References
Adler LA, Dirks B, Deas PF, Raychaudhuri A, Dauphin MR, Lasser RA, Weisler RH (2013) Lisdexamfetamine dimesylate in adults with attention-deficit/ hyperactivity disorder who report clinically significant impairment in executive function: results from a randomized, double-blind, placebo-controlled study. J Clin Psychiatry 74:694–702. https://doi.org/10.4088/JCP.12m08144
Alwindi M, Bizanti A (2023) Vesicular monoamine transporter (VMAT) regional expression and roles in pathological conditions. Heliyon 9:e22413. https://doi.org/10.1016/j.heliyon.2023.e22413
Barlow RB, Johnson O (1989) Relations between structure and nicotine-like activity: X-ray crystal structure analysis of (-)-cytisine and (-)-lobeline hydrochloride and a comparison with (-)-nicotine and other nicotine-like compounds. Br J Pharmacol 98:799–808. https://doi.org/10.1111/j.1476-5381.1989.tb14608.x
Barragán E, Breuer D, Döpfner M (2017) Efficacy and safety of Omega-3/6 fatty acids, methylphenidate, and a combined treatment in children with ADHD. J Atten Disord 21:433–441. https://doi.org/10.1177/1087054713518239
Biederman J, Fried R, Hammerness P, Surman C, Mehler B, Petty CR, Faraone SV, Miller C, Bourgeois M, Meller B, Godfrey KM, Reimer B (2012) The effects of lisdexamfetamine dimesylate on the driving performance of young adults with ADHD: a randomized, double-blind, placebo-controlled study using a validated driving simulator paradigm. J Psychiatr Res 46:484–491. https://doi.org/10.1016/j.jpsychires.2012.01.007
Blick SKA, Keating GM (2007) Lisdexamfetamine. Paediatr Drugs 9:129–135 discussion 136. https://doi.org/10.2165/00148581-200709020-00007
Blum K, Chen ALC, Braverman ER, Comings DE, Chen TJH, Arcuri V, Blum SH, Downs BW, Waite RL, Notaro A, Lubar J, Williams L, Prihoda TJ, Palomo T, Oscar-Berman M (2008) Attention-deficit-hyperactivity disorder and reward deficiency syndrome. Neuropsychiatr Dis Treat 4:893–918. https://doi.org/10.2147/ndt.s2627
Bristot G, Ascoli BM, Scotton E, Géa LP, Pfaffenseller B, Kauer-Sant’Anna M (2019) Effects of lithium on inflammatory and neurotrophic factors after an immune challenge in a lisdexamfetamine animal model of mania. Braz J Psychiatry 41:419–427. https://doi.org/10.1590/1516-4446-2017-0001
Burns C, Kidron A (eds) (2022) Biochemistry, tyramine. StatPearls. Internet. In: StatPearls Publishing, Treasure Island (FL), p 2024 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK563197/
Comiran E, Kessler FH, Fröehlich PE, Limberger RP (2016) Lisdexamfetamine: a pharmacokinetic review. Eur J Pharm Sci 89:172–179. https://doi.org/10.1016/j.ejps.2016.04.026
Crooks PA, Zheng G, Vartak AP, Culver JP, Zheng F, Horton DB, Dwoskin LP (2011) Design, synthesis and interaction at the vesicular monoamine transporter-2 of lobeline analogs: potential pharmacotherapies for the treatment of psychostimulant abuse. Curr Top Med Chem 11:1103–1127. https://doi.org/10.2174/156802611795371332
Dhillon S, Yang LPH, Curran MP (2008) Bupropion: a review of its use in the management of major depressive disorder. Drugs 68:653–689. https://doi.org/10.2165/00003495-200868050-00011
Di Miceli M, Derf A, Gronier B (2022) Consequences of acute or chronic methylphenidate exposure using ex vivo neurochemistry and in vivo electrophysiology in the prefrontal cortex and striatum of rats. Int J Mol Sci 23:8588. https://doi.org/10.3390/ijms23158588
DuPaul GJ, Weyandt LL, Rossi JS, Vilardo BA, O’Dell SM, Carson KM, Verdi G, Swentosky A (2012) Double-blind, placebo-controlled, crossover study of the efficacy and safety of lisdexamfetamine dimesylate in college students with ADHD. J Atten Disord 16:202–220. https://doi.org/10.1177/1087054711427299
Duvall MG, Levy BD (2016) DHA- and EPA-derived resolvins, protectins, and maresins in airway inflammation. Eur J Pharmacol 785:144–155. https://doi.org/10.1016/j.ejphar.2015.11.001
Eiden LE, Weihe E (2011) VMAT2: a dynamic regulator of brain monoaminergic neuronal function interacting with drugs of abuse. Ann N Y Acad Sci 1216:86–98. https://doi.org/10.1111/j.1749-6632.2010.05906.x
FDA (2017) Mydayis. https://pi.shirecontent.com/PI/PDFs/Mydayis_USA_ENG.pdf
FDA (2009) Ritalin. https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/010187s077lbl.pdf
Foley KF, DeSanty KP, Kast RE (2006) Bupropion: Pharmacology and therapeutic applications. Expert Rev Neurother 6:1249–1265. https://doi.org/10.1586/14737175.6.9.1249
Freyberg Z, Sonders MS, Aguilar JI, Hiranita T, Karam CS, Flores J, Pizzo AB, Zhang Y, Farino ZJ, Chen A, Martin CA, Kopajtic TA, Fei H, Hu G, Lin YY, Mosharov EV, McCabe BD, Freyberg R, Wimalasena K, Hsin LW, Sames D, Krantz DE, Katz JL, Sulzer D, Javitch JA (2016) Mechanisms of amphetamine action illuminated through optical monitoring of dopamine synaptic vesicles in Drosophila brain. Nat Commun 7:10652. https://doi.org/10.1038/ncomms10652
Garey JD, Lusskin SI, Scialli AR (2020) Teratogen update: amphetamines. Birth Defects Res 112:1171–1182. https://doi.org/10.1002/bdr2.1774
Guillot TS, Miller GW (2009) Protective actions of the vesicular monoamine transporter 2 (VMAT2) in monoaminergic neurons. Mol Neurobiol 39:149–170. https://doi.org/10.1007/s12035-009-8059-y
Guillot TS, Richardson JR, Wang MZ, Li YJ, Taylor TN, Ciliax BJ, Zachrisson O, Mercer A, Miller GW (2008) PACAP38 increases vesicular monoamine transporter 2 (VMAT2) expression and attenuates methamphetamine toxicity. Neuropeptides 42:423–434. https://doi.org/10.1016/j.npep.2008.04.003
Hauser J, Makulska-Gertruda E, Reissmann A, Sontag TA, Tucha O, Lange KW (2014) The effects of nutritional polyunsaturated fatty acids on locomotor activity in spontaneously hypertensive rats. Atten Defic Hyperact Disord 6:61–65. https://doi.org/10.1007/s12402-013-0125-7
Healy-Stoffel M, Levant B (2018) N-3 (Omega-3) fatty acids: effects on brain dopamine systems and potential role in the etiology and treatment of neuropsychiatric disorders. CNS Neurol Disord Drug Targets 17:216–232. https://doi.org/10.2174/1871527317666180412153612
Heinzerling KG, Swanson AN, Hall TM, Yi Y, Wu Y, Shoptaw SJ (2014) Randomized, placebo-controlled trial of bupropion in methamphetamine-dependent participants with less than daily methamphetamine use. Addiction 109:1878–1886. https://doi.org/10.1111/add.12636
Hesse LM, Venkatakrishnan K, Court MH, von Moltke LL, Duan SX, Shader RI, Greenblatt DJ (2000) CYP2B6 mediates the in vitro hydroxylation of bupropion: potential drug interactions with other antidepressants. Drug Metab Dispos 28:1176–1183
Huss M, Duhan P, Gandhi P, Chen CW, Spannhuth C, Kumar V (2017) Methylphenidate dose optimization for ADHD treatment: review of safety, efficacy, and clinical necessity. Neuropsychiatr Dis Treat 13:1741–1751. https://doi.org/10.2147/NDT.S130444
Hutson PH, Pennick M, Secker R (2014) Preclinical pharmacokinetics, pharmacology and toxicology of lisdexamfetamine: a novel d-amphetamine pro-drug. Neuropharmacology 87:41–50. https://doi.org/10.1016/j.neuropharm.2014.02.014
Iwahashi M, Yoshimura T, Harigai W, Takuma K, Hashimoto H, Katayama T, Hayata-Takano A (2023) Pituitary adenylate cyclase-activating polypeptide deficient mice show length abnormalities of the axon initial segment. J Pharmacol Sci 153:175–182. https://doi.org/10.1016/j.jphs.2023.08.006
Kameg B, Fradkin D (2021) Management of attention-deficit/hyperactivity disorder in adults. J Nurse Pract 17:432–436. https://doi.org/10.1016/j.nurpra.2020.11.005
Kazda L, Bell K, Thomas R, McGeechan K, Sims R, Barratt A (2021) Overdiagnosis of attention-deficit/hyperactivity disorder in children and adolescents: a systematic scoping review. JAMA Netw Open 4:e215335. https://doi.org/10.1001/jamanetworkopen.2021.5335
Korchynska S, Rebernik P, Pende M, Boi L, Alpár A, Tasan R, Becker K, Balueva K, Saghafi S, Wulff P, Horvath TL, Fisone G, Dodt HU, Hökfelt T, Harkany T, Romanov RA (2022) A hypothalamic dopamine locus for psychostimulant-induced hyperlocomotion in mice. Nat Commun 13:5944. https://doi.org/10.1038/s41467-022-33584-3
Li Y, Yan X, Li Q, Li Q, Xu G, Lu J, Yang W (2023) Prevalence and trends in diagnosed ADHD among US children and adolescents, 2017–2022. JAMA Netw Open 6:e2336872. https://doi.org/10.1001/jamanetworkopen.2023.36872
Lu W, Wolf ME (1997) Expression of dopamine transporter and vesicular monoamine transporter 2 mRNAs in rat midbrain after repeated amphetamine administration. Brain Res Mol Brain Res 49:137–148. https://doi.org/10.1016/s0169-328x(97)00136-8
Majarwitz DJ, Perumareddi P (2023) Attention-deficit/hyperactivity disorder across the spectrum: from childhood to Adulthood. Prim Care 50:21–36. https://doi.org/10.1016/j.pop.2022.10.004
Maneeton N, Maneeton B, Srisurapanont M, Martin SD (2011) Bupropion for adults with attention-deficit hyperactivity disorder: Meta-analysis of Randomized, placebo‐controlled trials. Psychiatry Clin Neurosci 65:611–617. https://doi.org/10.1111/j.1440-1819.2011.02264.x
Martin CA, Nuzzo PA, Ranseen JD, Kleven MS, Guenthner G, Williams Y, Walsh SL, Dwoskin LP (2018) Lobeline effects on cognitive performance in adult ADHD. J Atten Disord 22:1361–1366. https://doi.org/10.1177/1087054713497791
Metz VG, Segat HJ, Dias VT, Barcelos RCS, Maurer LH, Stiebe J, Emanuelli T, Burger ME, Pase CS (2019) Omega-3 decreases D1 and D2 receptors expression in the prefrontal cortex and prevents amphetamine-induced conditioned place preference in rats. J Nutr Biochem 67:182–189. https://doi.org/10.1016/j.jnutbio.2019.02.007
Najib J (2009) The efficacy and safety profile of lisdexamfetamine dimesylate, a prodrug of d-amphetamine, for the treatment of attention-deficit/hyperactivity disorder in children and adults. Clin Ther 31:142–176. https://doi.org/10.1016/j.clinthera.2009.01.015
Najib J, Wimer D, Zeng J, Lam KW, Romanyak N, Paige Morgan E, Thadavila A (2017) Review of lisdexamfetamine dimesylate in adults with attention-deficit/hyperactivity disorder. J Cent Nerv Syst Dis 9:1179573517728090. https://doi.org/10.1177/1179573517728090
Narendran R, Frankle WG, Mason NS, Muldoon MF, Moghaddam B (2012) Improved working memory but no effect on striatal vesicular monoamine transporter type 2 after omega-3 polyunsaturated fatty acid supplementation. PLoS ONE 7:e46832. https://doi.org/10.1371/journal.pone.0046832
Ng QX (2017) A systematic review of the use of bupropion for attention-deficit/hyperactivity disorder in children and adolescents. J Child Adolesc Psychopharmacol 27:112–116. https://doi.org/10.1089/cap.2016.0124
Nguyen M, Shapiro MA, Tharani S (2012) Clinical utility of lisdexamfetamine for the management of attention-deficit hyperactivity disorder. Clin Med Insights Ther 4. https://doi.org/10.4137/CMT.S8706
Nickell JR, Siripurapu KB, Vartak A, Crooks PA, Dwoskin LP (2014) The vesicular monoamine transporter-2: an important pharmacological target for the discovery of novel therapeutics to treat methamphetamine abuse. Adv Pharmacol 69:71–106. https://doi.org/10.1016/B978-0-12-420118-7.00002-0
Partilla JS, Dempsey AG, Nagpal AS, Blough BE, Baumann MH, Rothman RB (2006) Interaction of amphetamines and related compounds at the vesicular monoamine transporter. J Pharmacol Exp Ther 319:237–246. https://doi.org/10.1124/jpet.106.103622
Perera H, Jeewandara KC, Seneviratne S, Guruge C (2012) Combined ω3 and ω6 supplementation in children with attention-deficit hyperactivity disorder (ADHD) refractory to methylphenidate treatment: a double-blind, placebo-controlled study. J Child Neurol 27:747–753. https://doi.org/10.1177/0883073811435243
Quintero J, Gutiérrez-Casares JR, Álamo C (2022) Molecular characterisation of the mechanism of action of stimulant drugs lisdexamfetamine and methylphenidate on ADHD neurobiology: a review. Neurol Ther 11:1489–1517. https://doi.org/10.1007/s40120-022-00392-2
Rau KS, Birdsall E, Hanson JE, Johnson-Davis KL, Carroll FI, Wilkins DG, Gibb JW, Hanson GR, Fleckenstein AE (2005) Bupropion increases striatal vesicular monoamine transport. Neuropharmacology 49:820–830. https://doi.org/10.1016/j.neuropharm.2005.05.004
Reese MJ, Wurm RM, Muir KT, Generaux GT, St John-Williams L, McConn DJ (2008) An in vitro mechanistic study to elucidate the desipramine/bupropion clinical drug–drug interaction. Drug Metab Dispos 36:1198–1201. https://doi.org/10.1124/dmd.107.020198
Riddle EL, Hanson GR, Fleckenstein AE (2007) Therapeutic doses of amphetamine and methylphenidate selectively redistribute the vesicular monoamine transporter-2. Eur J Pharmacol 571:25–28. https://doi.org/10.1016/j.ejphar.2007.05.044
Sandoval V, Riddle EL, Hanson GR, Fleckenstein AE (2002) Methylphenidate redistributes vesicular monoamine transporter-2: role of dopamine receptors. J Neurosci 22:8705–8710. https://doi.org/10.1523/JNEUROSCI.22-19-08705.2002
Schwartz K, Weizman A, Rehavi M (2006) The effect of psychostimulants on [3H]dopamine uptake and release in rat brain synaptic vesicles. J Neural Transm (Vienna) 113:1347–1352. https://doi.org/10.1007/s00702-005-0383-4
Stahl SM (2014) Stahl’s essential psychopharmacology. Cambridge
Stahl SM, Pradko JF, Haight BR, Modell JG, Rockett CB, Learned-Coughlin S (2004) A review of the neuropharmacology of bupropion, a dual norepinephrine and dopamine reuptake inhibitor. Prim Care Companion J Clin Psychiatry 6:159–166. https://doi.org/10.4088/pcc.v06n0403
Støier JF, Konomi-Pilkati A, Apuschkin M, Herborg F, Gether U (2023) Amphetamine-induced reverse transport of dopamine does not require cytosolic Ca2+. J Biol Chem 299:105063. https://doi.org/10.1016/j.jbc.2023.105063
Strawn JR, Picard LS (2017) Triple-bead mixed amphetamine salt for ADHD. Curr Psychiatry 16:33–37
Sulzer D, Rayport S (1990) Amphetamine and other psychostimulants reduce pH gradients in midbrain dopaminergic neurons and chromaffin granules: a mechanism of action. Neuron 5:797–808. https://doi.org/10.1016/0896-6273(90)90339-h
Teng LH, Crooks PA, Sonsalla PK, Dwoskin LP (1997) Lobeline and nicotine evoke [3H]overflow from rat striatal slices preloaded with [3H]dopamine: Differential inhibition of synaptosomal and vesicular [3H]dopamine uptake. J Pharmacol Exp Ther 280:1432–1444
Teng B, Murthy KS, Kuemmerle JF, Grider JR, Makhlouf GM (1998) Selective expression of vasoactive intestinal peptide (VIP)2/pituitary adenylate cyclase-activating polypeptide (PACAP)3 receptors in rabbit and guinea pig gastric and tenia coli smooth muscle cells. Regul Pept 77:127–134. https://doi.org/10.1016/s0167-0115(98)00112-8
Toren P, Rehavi M, Luski A, Roz N, Laor N, Lask M, Weizman A (2005) Decreased platelet vesicular monoamine transporter density in children and adolescents with attention deficit/hyperactivity disorder. Eur Neuropsychopharmacol 15:159–162. https://doi.org/10.1016/j.euroneuro.2004.07.002
Vaudry D, Gonzalez BJ, Basille M, Yon L, Fournier A, Vaudry H (2000) Pituitary adenylate cyclase-activating polypeptide and its receptors: from structure to functions. Pharmacol Rev 52:269–324
Velasco ER, Florido A, Flores Á, Senabre E, Gomez-Gomez A, Torres A, Roca A, Norrholm S, Newman EL, Das P, Ross RA, Lori A, Pozo OJ, Ressler KJ, Garcia-Esteve LL, Jovanovic T, Andero R (2022) PACAP-PAC1R modulates fear extinction via the ventromedial hypothalamus. Nat Commun 13:4374. https://doi.org/10.1038/s41467-022-31442-w
Verbeeck W, Bekkering GE, Van den Noortgate W, Kramers C (2017) Bupropion for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev 10:CD009504. https://doi.org/10.1002/14651858.CD009504.pub2
Wang G, Pan J, Tan YY, Sun XK, Zhang YF, Zhou HY, Ren RJ, Wang XJ, Chen SD (2008) Neuroprotective effects of PACAP27 in mice model of Parkinson’s disease involved in the modulation of K(ATP) subunits and D2 receptors in the striatum. Neuropeptides 42:267–276. https://doi.org/10.1016/j.npep.2008.03.002
Wimalasena K (2011) Vesicular monoamine transporters: Structure-function, pharmacology, and medicinal chemistry. Med Res Rev 31:483–519. https://doi.org/10.1002/med.20187
Acknowledgements
We thank Editage (www.editage.com) for English language editing.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Warlick IV, H., Tocci, D., Prashar, S. et al. Role of vesicular monoamine transporter-2 for treating attention deficit hyperactivity disorder: a review. Psychopharmacology (2024). https://doi.org/10.1007/s00213-024-06686-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00213-024-06686-7