Abstract
Background
The objective of this study is to measure the levels of sestrin-2 (SESN2) and hypoxia-inducible factor-1 alpha (HIF-1α), which can be determinants in the relevant physiopathology and etiology, assessment of the clinical severity, and identification of new treatment targets in major depressive disorder (MDD) and its subtypes.
Methods
A total of 230 volunteers, including 153 patients diagnosed with MDD according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), and 77 healthy controls, were included in the study. Of the MDD patients included in the study, 40 had melancholic features, 40 had anxious distress features, 38 had atypical features, and the remaining 35 had psychotic features. All participants were administered the Beck’s Depression Inventory (BDI) and Clinical Global Impressions-Severity (CGI-S) scale. Serum SESN2 and HIF-1α levels of the participants were measured using the enzyme-linked immunosorbent assay (ELISA) method.
Results
The HIF-1α and SESN2 values of the patient group were found to be significantly lower than those of the control group (p < 0.05). The HIF-1α and SESN2 values were significantly lower in patients with melancholic, anxious distress, and atypical features compared to the control group (p < 0.05). The HIF-1α and SESN2 levels did not differ significantly between patients with psychotic features and the control group (p > 0.05).
Conclusion
The findings of the study suggested that knowledge of SESN2 and HIF-1α levels may contribute to the explanation of the etiology of MDD, objective assessment of the severity of the disease, and identification of new treatment targets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) is estimated to affect more than 300 million people worldwide, with a point prevalence of approximately 5% and a lifetime prevalence of 15% (Friedrich 2017). The neurobiology of MDD has not yet been fully elucidated. In recent years, it has been shown that oxidative stress plays a major role in its etiology (Lindqvist et al. 2017a; Maes et al. 2011). Oxidative stress occurs as a result of the disruption of the balance between the production and detoxification of free radicals in the form of reactive oxygen or nitrogen species in cells and tissues. Oxidative damage to the brain is a potential pathogenic factor of psychiatric and neurological diseases. In high concentrations, free radicals significantly reduce long-term synaptic reinforcement, signaling, and neuroplasticity of the brain (Salim 2017).
Sestrins are encoded by an evolutionarily conserved family of stress-inducible genes that are involved in the regulation of cell survival in response to various stress conditions, such as oxidative or genotoxic stress (Lee et al. 2013). Sestrin-2 (SESN2) is an antioxidant protein that plays a role in cellular functions such as the prevention of inflammation, energy production, homeostasis, and cell survival (Pasha et al. 2017). Hypoxia-inducible factor-1 (HIF-1), a nuclear transcription factor, is a master regulator of cellular oxygen homeostasis that can be expressed in human cells. HIF-1 has two protein subunits, HIF-1 alpha (HIF-1α) and HIF-1 beta (HIF-1β). HIF-1α is involved in cell proliferation, cell survival, glucose and iron metabolism, and angiogenesis. In parallel, it has been shown that HIF-1α plays a role in many diseases that create a hypoxic microenvironment, such as heart diseases, cancers, and cerebrovascular diseases (Semenza 2000).
In the light of the foregoing knowledge, this study was carried out in patients diagnosed with MDD according to the criteria set forth in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), and in MDD patients with melancholic, anxious distress, atypical, and psychotic features, in order to measure the SESN2 and HIF-1α levels as a potential (i) factor in the physiopathology and etiology of MDD and its subtypes, (ii) status determinant in the assessment of the clinical severity of MDD, and (iii) new treatment target in the therapy of MDD. The relationship between the MDD-related variables and the SESN2 and HIF-1α levels was investigated by comparing the patients with the healthy control subjects.
Material and method
Research design
The sample of the study consisted of 230 volunteers, 153 of whom were patients, who applied to Gaziantep University Faculty of Medicine, Department of Psychiatry, between October 2021 and May 2022 and met the inclusion criteria. Participants were examined by a psychiatrist, and the SCID-5-CV was used in their assessment. In 2013, the Diagnostic and Statistical Manual of Mental Disorders classified subtypes of mood disorders. Participants were grouped according to the diagnostic criteria of the DSM-5. Of the 153 MDD patients, 40 patients had melancholic, an additional 40 patients had anxious distress, 38 patients had atypical, and 35 patients had psychotic features. The investigation was conducted in accordance with the 2013 version of the Declaration of Helsinki. Informed consent was obtained after the nature of the procedures had been fully explained. Approval for the research was obtained from the ethics committee of Gaziantep University with decision number 2021/280.
Study ınclusion/exclusion criteria
The study inclusion criteria for the patient group were as follows: being aged between 18 and 65, having been diagnosed with MDD according to DSM-5 diagnostic criteria, and being included in one of the subtypes showing melancholy, anxious distress, atypical, psychotic features, absence of a history of comorbid medical disease, not having a history of alcohol and/or substance use, not being pregnant, and having agreed to participate in the study voluntarily.
All of the participants in the patient and control groups were evaluated by two psychiatrists. Melancholy, anxious distress, atypical, and psychotic subtypes were determined according to DSM-5 diagnostic criteria, but since the patients were evaluated by two psychiatrists, marked melancholic, marked atypical, and marked anxious subtypes were included in the study to avoid any heterogeneity.
The study inclusion criteria for the control group were as follows: absence of a history of psychiatric or comorbid medical disease, absence of a history of alcohol and/or substance use, and not being pregnant.
Participants in both the patient and control groups did not use any medication.
The study exclusion criteria for both patient and control groups, on the other hand, were as follows: being younger than 18 years old, being older than 65 years old, being pregnant, and having a history of alcohol and/or substance use.
Assessment tools
Sociodemographic data form
The sociodemographic data collected using a specific form included participants’ gender, age, occupation, history of additional medical diseases, smoking status, height, weight, marital status, educational level, lifestyle, and employment status. Additionally, clinical information that was collected by the administration of the same form referred to the participants’ past admissions, the number of past episodes, suicide history, active and/or passive suicidal ideation, familial mental illness history, and familial depression history.
Structured Clinical Interview for DSM-5-Clinician Version (SCID-5-CV)
SCID-5 is a semi-structured interview guide developed for making DSM-5 diagnoses. This guide can be applied by clinicians or trained mental health professionals who are familiar with the DSM-5 classification and diagnostic criteria (First et al. 2016). The Turkish validity and reliability studies of SCID-5 were completed by Müge et al. in 2018 (Elbir et al. 2019).
Beck’s Depression Inventory-1 (BDI-1)
BDI was developed by Beck et al. in 1961 to determine the severity of depressive symptoms (Beck et al. 1961). It consists of a total of 21 items. Each item is assigned a score between 0 and 3; thus, the total BDI score can range between 0 and 63. The cut-off score for the total BDI score is deemed to be 17. The Turkish validity and reliability studies of BDI were completed by Hisli et al. in 1988 (Hisli 1988).
Clinical Global Impressions-Severity (CGI-S) scale
CGI-S is a scale developed by Guy et al. to evaluate the severity of psychiatric disorders according to general clinical experience (Guy 1976). In CGI-S, the disease severity is graded from 0 to 7.
Laboratory measurements
After 12 h of fasting, 5 mL of blood was drawn from each patient and healthy control subject from the forearm antecubital region into a tube without anticoagulant. The blood samples were kept at room temperature for 20 min and centrifuged at 4000 gravity for 10 min to separate the sera. The separated sera were taken into Eppendorf tubes and stored at − 80 °C. At the time of the study, serum samples were brought to room temperature. The SESN2 and HIF-1α levels of the samples were measured using the enzyme-linked immunosorbent assay (ELISA) method with the help of commercial kits (FineTest, China, Cat. No: EH1556 and EH0551, respectively), which utilize the sandwich ELISA protocol.
Statistical analysis
The Shaphiro-Wilk test was used to determine whether the collected data conformed to the normal distribution. The Mann–Whitney U test was used to compare two groups with non-normally distributed variables. Kruskal–Wallis and Dunn’s multiple comparisons tests were used to compare more than two independent groups. Relationships between categorical variables were tested with chi-squared and Bonferroni correction for multiple comparison tests. Spearman’s rank correlation coefficient was used to test the relationships between numerical variables. Descriptive statistics were expressed as median [interquartile range (IQR): 25–75%] values in the case of numerical variables and as numbers (n) and percentage (%) values in the case of categorical variables. The effects of SESN2 and HIF-1α levels, age, and the number of past episodes on BDI and CGI-S scores were evaluated by multivariate linear regression analysis.
SPSS 24.0 (Statistical Package for Social Sciences for Windows, version 24.0, IBM Corp., Armonk, NY, USA, 2016) software package was used for statistical analyses. Probability (p) values of < 0.05 were deemed to indicate statistical significance.
Results
Sociodemographic results
There were no statistically significant differences between the patient and control groups in terms of sociodemographic characteristics (p > 0.05 for all). Sociodemographic data of the patient and control groups are given in Table 1.
Subgroup analysis also did not reveal any significant difference between the MDD patients with melancholic, anxious distress, atypical and psychotic features, and the healthy control subjects in terms of age, gender, marital status, lifestyle, educational level, and smoking status (p > 0.05 for all). Sociodemographic data of the subgroups of the patient group and the control group are given in Table 2.
The female/male ratios in the MDD group and in the MDD subgroups with melancholic, anxious distress, atypical, and psychotic features were found as 3.46/1, 3.44/1, 3/1, 2.8/1, and 1.19/1, respectively. The mean age was the highest in the MDD subgroup with psychotic features, followed by the control group and the MDD subgroups with atypical, melancholic, and anxious distress features in order.
Clinical features
The mean BDI scores of the patient and control groups were 31.41 ± 12.46 and 0.71 ± 0.74, respectively. Additionally, the mean CGI-S scores of the patient and control groups were 4.41 ± 1.29 and 1 ± 0, respectively. Accordingly, there was a significant difference between the BDI and CGI-S scores of the patient and control groups (p < 0.05 for all). There was also a significant difference in BDI and CGI-S scores between the subgroups of the patient group and the control group (p < 0.05 for all). The data on the BDI and CGI-S scores of the subgroups of the patient group and the control group are given in Table 3.
HIF-1α and SESN2 results
It was determined that HIF-1α and SESN2 values in the patient and control groups did not show normal distribution according to the groups. The median value was used to compare the values. A statistically significant difference was found between the HIF-1α and SESN2 values of the patient and control groups (p = 0.035 and p = 0.001, respectively). The median level of HIF-1α in the patient group was 1.18 ng/mL [25–75 percentile 0.82–1.71] in the control group, 1.27 [25–75 percentile 1.05–1.78]. The median level of SESN2 in the patient group was 2.03 ng/mL [25–75 percentile 1.76–2.57] in the control group, 2.37 ng/mL [25–75 percentile 2.03–2.91] (Table 4.).The differences in HIF-1α and SESN2 levels in the patient and control groups are shown in Figs. 1 and 2. ROC curve analysis was used to test the patient discrimination level of HIF-1α (AUC:0.585) and SESN2 (AUC:0.662) values (Figs. 3 and 4). No significant correlation was found between patients’ SESN2 and HIF-1α levels and their gender, smoking status, active suicidal ideation, familial mental illness history, and familial depression history.
Group comparisons
The mean HIF-1α level was the highest in the MDD subgroup with psychotic features, followed by the control group and the MDD subgroups with anxious distress, melancholic, and atypical features in order. On the other hand, the mean SESN2 level was the highest in the control group, followed by the MDD subgroups with psychotic, atypical, melancholic, and anxious distress features in order. A statistically significant difference was found between the HIF-1α and SESN2 values of the MDD subtypes and the control group (p = 0.001 for each). (The mean, standard deviation, and median data of the patient subgroups and the control group are given in Table 5.) The differences in HIF-1α and SESN2 levels in the subgroups of the patient group and the control group are shown in Figs. 1 and 2. (Comparison of the groups in terms of HIF-1α and SESN2 is given in Table 6.)
Correlation analyses
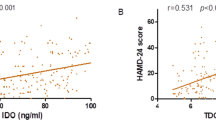
A weak positive correlation was found between SESN2 and HIF-1α levels of the patients (r = 0.361; p < 0.001). Accordingly, there was a moderate positive correlation between the HIF-1α and SESN2 levels in the MDD subgroups with atypical and psychotic features (r = 0.445 and p = 0.005, r = 0.495 and p = 0.002, respectively) (Table 7).
Regression analyses
In the multivariate linear regression analysis models, the HIF-1α levels, age, and the number of past episodes explained 26.4% of the variation in the BDI scores. Accordingly, a one-unit increase in the HIF-1α levels and the number of past episodes caused an increase of 5.48 and 2.83 points increase in the mean BDI scores, respectively (β = 5.48 ± 1.44, p < 0.001 and β = 2.83 ± 0.62, p < 0.001, respectively). Additionally, the HIF-1α levels, age, and the number of past episodes explained 24.7% of the variation in CGI-S scores. Accordingly, an increase in the one-unit HIF-1α level and the number of past episodes caused an increase in CGI-S mean scores of 0.46 and 0.28 points, respectively (β = 0.46 ± 0.15, p = 0.003 and β = 0, 28 ± 0.07, p < 0.001, respectively) (Table 8).
The SESN2 levels, age, and the number of past episodes explained 22.4% of the variation in the BDI scores. Accordingly, a one-unit increase in the SESN2 levels and the number of past episodes caused an increase of 3.77 and 2.97 points in the mean BDI scores, respectively (β = 3.77 ± 1.51, p = 0.014 and β = 2.97 ± 0.63, p = 0.001, respectively). Additionally, the SESN2 levels, age, and the number of past episodes explained 22.2% of the variation in the CGI-S scores. Accordingly, a one-unit increase in the SESN2 levels and the number of past episodes caused an increase of 0.32 and 0.29 points in the mean CGI-S scores, respectively (β = 0.32 ± 0.16, p = 0.042 and β = 0. 29 ± 0.07, p < 0.001, respectively) (Table 9).
Discussion
There are many studies in the literature on the etiology, physiopathology, clinical findings, and pathognomonic features of MDD (pessimistic mood, not enjoying life, changes in weight or appetite, sleep disturbances, fatigue, psychomotor retardation or agitation, impaired concentration, loss of self-confidence, suicidal thoughts, or attempts). Our study is the first to measure SESN2 and HIF-1α levels in MDD patients and their subtypes.
In this study, the mean HIF-1α level of the patient group was found to be significantly lower than that of the control group. In comparison, in a study conducted with 20 pregnant women with and without preeclampsia, the HIF-1α levels of the patients with preeclampsia were found to be significantly higher than those of the patients without preeclampsia (Akhilesh et al. 2013). In another study, it was found that maternal serum HIF-1α levels did not differ significantly between normatensive and preeclamptic pregnant patients and that the HIF-1α levels were significantly higher in the late-onset preeclampsia group. The authors of the study attributed the previously mentioned increase in the HIF-1α levels to the inflammation and oxygen-independent mechanisms in late-onset preeclampsia (Alici Davutoğlu et al. 2018). In a study conducted with 60 obstructive sleep apnea (OSA) patients and 24 healthy control subjects, the HIF-1α levels were found to be significantly higher in the patient group than in the control group (Gabryelska et al. 2020). Additionally, in another study, serum HIF-1α levels were found to be significantly higher in patients with ischemic stroke compared to the healthy control subjects. The authors of the study attributed the said increase in the HIF-1α levels to the deactivation of the Von Hippel Lindau Protein (pVHL), which controls the HIF-lα level in the first stages of ischemic stroke, where oxygen levels drop to critical levels (Rahmati et al. 2021).
It has been emphasized that chronic hypoxia is involved in the pathogenesis and exacerbation of MDD (Kanekar et al. 2015; Kious et al. 2018; Yamagata et al. 2017) and that long-term mild hypoxia also plays a role in depression (Kushwah et al. 2016). HIF-1α has been shown to play a central role in hypoxia under physiological and pathological conditions (Greer et al. 2012). It has been argued that genes associated with depression may be affected by HIF-1, that creatinine metabolism, which is emphasized in the treatment of depression, can be modulated by HIF-1, and that hypoxic or hyperoxic exposure that raises HIF-1 levels may have antidepressant effects. Accordingly, it has been hypothesized that raising the HIF levels may be a new potential treatment target in the treatment of depression (Kang et al. 2021).
It has also been demonstrated that HIF-1α levels can be regulated independently of hypoxia (Kuschel et al. 2012) and that HIF-1α has a protective role in oxidative stress (Li et al. 2019). All this information suggests that HIF-1α may be involved in the etiopathogenesis of MDD. The inadequacy of defense mechanisms against oxidative stress in the context of brain-related diseases including depression (Smaga et al. 2015) supports the low HIF-1α levels detected in the patient group investigated in this study. Low HIF-1α may cause MDD by disrupting the organism’s response to hypoxia.
Despite advances in psychopharmacology and the use of new and effective antidepressants, the fact that the efficacy of pharmacological agents in the treatment of depression is still unsatisfactory has led to the search for new treatment methods, including biological and non-pharmacological methods. An example is hyperbaric oxygen therapy (HBOT), which involves the use of 100% pure oxygen at a pressure above atmospheric pressure (Sutherland et al. 2016). HBOT is widely used in the treatment of many diseases such as diabetic foot ulcers, carbon monoxide poisoning, vascular dementia, and traumatic brain injury (Elraiyah et al. 2016; Juurlink et al. 2005; You et al. 2019). The efficacy of HBOT in the treatment of mental disorders such as depression and anxiety in patients with spinal cord injury was found to be comparable to psychotherapy (Feng and Li 2017). It has been suggested that in addition to reducing inflammation in nerve tissue, HBOT also inhibits serotonin reuptake, which may be useful in the treatment of depression (Lim et al. 2017). A study conducted in 2014 in diabetic animals demonstrated that HBOT activates HIF-1α through stabilization, thus contributing to increased cellular proliferation. Additionally, it has been shown that HBOT modulates HIF-1α, which plays a central role in diabetic wound healing, over a complex set of mechanisms (Sunkari et al. 2015). The mechanism of action which renders HBOT successful in the treatment of patients with depression is not yet clear. Therefore, further studies designed to evaluate the efficacy of HBOT in MDD patients are needed. The fact that the HIF-1α levels were found to be significantly lower in the patient group compared to the control group in this study suggests that HBOT may be effective in patients with depression through HIF-1α levels.
The HIF-1α levels significantly differed also between the subgroups of the patient group, except for the group of MDD patients with psychotic features and the control group. As a matter of fact, the literature data suggest that depression with psychotic features significantly differs from depression without psychotic features (Østergaard et al. 2012b) in potential trigger factors (Domschke et al. 2011; Østergaard et al. 2013b, 2013c), underlying biological factors (Cubells et al. 2002; Meyers et al. 1999; Nelson and Davis 1997; Posener et al. 2000), symptomatology except for the psychotic symptoms (Maj et al. 2007; Østergaard et al. 2012a), long-term prognosis (Coryell et al. 1996; Johnson et al. 1991; Østergaard et al. 2013a; Park et al. 2010; Rotschild et al. 1993; Vythilingam et al. 2003), and responses to psychopharmacological and electroconvulsive therapies (Brown et al. 1982; Petrides et al. 2001). The fact that the study findings related to MDD patients with melancholic, anxious distress, and atypical features significantly differed from the findings related to MDD patients with psychotic features suggests that psychotic depression may differ from other subtypes in pathophysiology. Therefore, it would be careful to approach MDD patients with psychotic features differently in terms of both diagnosis and treatment.
The findings of this study indicated that the SESN2 levels of the patient group were significantly lower than those of the control group. There are also many studies in the literature that addressed the serum SESN2 levels in the context of several diseases. In one of these studies, in which the SESN2 levels of 194 diabetics and 46 controls were compared, SESN2 levels were found to be significantly higher in individuals with metabolic syndrome. In the said study, the paradoxical increase in serum SESN2 levels was attributed to the metabolic stress or compensatory mechanisms to resistance to SESN2 (Chung et al. 2018). In another study, serum SESN2 levels were found to be significantly low in patients with type 2 diabetes mellitus (Mohany and Al Rugaie 2020). In a study comparing patients with coronary artery disease with healthy individuals, plasma SESN2 levels were increased in patients with coronary artery disease accompanied by old age and obesity, while both plasma SESN2 and SESN3 levels were increased in patients with coronary artery disease accompanied by diabetes. These results were interpreted that different members of the Sestrin family exert antioxidant effects in a specific oxidative stress environment (Ye et al. 2017). In another study, the SESN2 levels of 44 asthmatic patients were found to be higher compared to those of 32 healthy control subjects. The said increase in the SESN2 levels of asthma patients was attributed to the oxidative stress caused by the increased hypoxia due to restricted airflow in asthma (Kang et al. 2019). It was suggested that SESN2 may play a role in aortic dissection (AD) by regulating oxidative stress in AD patients who have higher SESN2 levels (Xiao et al. 2019). In a study investigating the relationship between SESN2 levels and preeclampsia (PE), SESN2 levels were found to be significantly higher in the severe PE group, but there was no significant difference between the PE and control groups. This finding was attributed to lower oxidative stress and systemic inflammatory response in PE (Tayyar et al. 2019).
SESN2 suppresses the production of reactive oxygen species and provides cytoprotection against a variety of harmful stimuli, including hypoxia, oxidative stress, endoplasmic reticulum (ER) stress, and DNA damage (Lee et al. 2013). Hypoxia enhances peroxide defense by HIF-1α-dependent regulation of SESN2 (Essler et al. 2009). All these findings and the fact that SESN2 was found to be involved in the pathways which are possibly involved in the pathogenesis of depression led to the hypothesis that SESN2 may play a role in the pathogenesis of MDD. Information such as the demonstration of SESN2 as a new therapeutic target for the prevention of hypoxia-related diseases and metabolic disorders, and HIF-1α-dependent regulation of SESN2, suggest that low SESN2 may be the main reason for the deterioration of oxidative stress homeostasis in the pathogenesis of MDD. The designation of SESN2 as a new therapeutic target in the prevention of hypoxia-related diseases and metabolic disorders in some studies (Pan et al. 2021) and the findings that indicate the HIF-1α-dependent regulation of SESN2 (Essler et al. 2009) suggest that the main reason for the deterioration of homeostasis in oxidative stress in the pathogenesis of MDD may be low SESN2 levels. The view that treatments regulating HIF-1α levels can increase SESN2 levels and the low levels of HIF-1α and SESN2 detected in the patient group included in this study suggest that HBOT, which regulates HIF-1α, may be used in the treatment of MDD, and that SESN2 monitoring in the clinic may be a status marker for MDD. However, long-term prospective follow-up studies covering the disease and remission periods are needed to reach a more definitive conclusion on the subject. The differences detected between the subgroups of the patient group in SESN2 levels support the suggestions made about the relationship between the HIF-1α levels and psychotic depression and prompt approaching psychotic depression as a different disorder in terms of both diagnosis and treatment.
The fact that correlation analysis revealed a relationship between HIF-1α and SESN2 levels in MDD patients supports the regulation between HIF-1α and SESN2. Impairment in the HIF-1α-dependent regulation of SESN2 in the pathogenesis of MDD may explain the lower HIF-1α and SESN2 levels in the patient group compared to the control group. In previous studies, depression subtypes were compared in terms of inflammatory processes and poorer immune inflammatory and metabolic health was seen in atypical depression (Lamers et al. 2020). Similarly, the correlation between HIF-1 alpha and SESN2 in the psychotic depression subtype may indicate the need for further immune inflammatory studies for this subtype.
The association found between HIF-1α and SESN2 levels and the scores obtained from BDI and CGI-S in the linear regression analysis may provide more objective data in the assessment of the severity of the disease in MDD, eliminate the biases in the assessment process, and make it easier to evaluate patients with defensive attitudes.
The results we have obtained should be evaluated by considering some limitations. The study is cross-sectional. In order to use SESN2 and HIF-1α as state markers in the clinical evaluation of patients, studies with larger populations of different races are needed.
The available data in the literatüre and the findings of this study reveal the importance of SESN2 and HIF-1α in understanding the etiology and pathophysiology of MDD, objectively assessing the severity of MDD, and developing new treatment modalities for MDD. The relationship between HIF-1α and SESN2 and the fact that an increase in the HIF-1α levels will also increase the SESN2 levels may benefit further strengthening the defense mechanisms against oxidative stress, preventing MDD, and shortening the treatment period(Bhatt et al. 2020; Lindqvist et al. 2017b).
Data Availability
Data can be provided by correspond if requested.
References
Akhilesh M, Mahalingam V, Nalliah S, Ali RM, Ganesalingam M, Haleagrahara N (2013) Hypoxia-inducible factor-1α as a predictive marker in pre-eclampsia. Biomed Rep 1:257–258
Alici Davutoğlu E, Akkaya Firat A, Ozel A, Yılmaz N, Uzun I, Temel Yuksel I, Madazlı R (2018) Evaluation of maternal serum hypoxia inducible factor-1α, progranulin and syndecan-1 levels in pregnancies with early-and late-onset preeclampsia. J Matern Fetal Neonatal Med 31:1976–1982
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Bhatt S, Nagappa AN, Patil CR (2020) Role of oxidative stress in depression. Drug Discov Today 25:1270–1276
Brown RP, Frances A, Kocsis JH, Mann JJ (1982) Psychotic vs. nonpsychotic depression: comparison of treatment response. J Nerv Ment Dis 170:635–637
Chung HS, Hwang H-J, Hwang SY, Kim NH, Seo JA, Kim SG, Kim NH, Baik SH, Choi KM, Yoo HJ (2018) Association of serum sestrin2 level with metabolic risk factors in newly diagnosed drug-naïve type 2 diabetes. Diabetes Res Clin Pract 144:34–41
Coryell W, Leon A, Winokur G, Endicott J, Keller M, Akiskal H, Solomon D (1996) Importance of psychotic features to long-term course in major depressive disorder. Am J Psychiatry 153(4):483–489
Cubells JF, Price LH, Meyers BS, Anderson GM, Zabetian CP, Alexopoulos GS, Nelson JC, Sanacora G, Kirwin P, Carpenter L (2002) Genotype-controlled analysis of plasma dopamine β-hydroxylase activity in psychotic unipolar major depression. Biol Psychiat 51:358–364
Domschke K, Lawford B, Young R, Voisey J, Morris CP, Roehrs T, Hohoff C, Birosova E, Arolt V, Baune BT (2011) Dysbindin (DTNBP1)–a role in psychotic depression? J Psychiatr Res 45:588–595
Elbir M, Alp Topbaş O, Bayad S, Kocabaş T, Topak Z, Çetin Ş, Özdel O, Ateşçi FÇ, Aydemir Ö (2019) Adaptation and reliability of the structured clinical interview for DSM-5-disorders-clinician version (SCID-5/CV) to the Turkish language. Turk J Psychiatry 30(1):51–56
Elraiyah T, Tsapas A, Prutsky G, Domecq JP, Hasan R, Firwana B, Nabhan M, Prokop L, Hingorani A, Claus PL (2016) A systematic review and meta-analysis of adjunctive therapies in diabetic foot ulcers. J Vasc Surg 63:46S-58S. e2
Essler S, Dehne N, Brüne B (2009) Role of sestrin2 in peroxide signaling in macrophages. FEBS Lett 583:3531–3535
Feng J-J, Li Y-H (2017) Effects of hyperbaric oxygen therapy on depression and anxiety in the patients with incomplete spinal cord injury (a STROBE-compliant article). Medicine 96(29):e7334
First MB, Williams JB, Karg RS, Spitzer RL (2016) SCID-5-CV: structured clinical interview for DSM-5 disorders: clinician version. American Psychiatric Association Publishing Arlington, VA
Friedrich MJ (2017) Depression is the leading cause of disability around the world. JAMA 317:1517–1517
Gabryelska A, Szmyd B, Panek M, Szemraj J, Kuna P, Białasiewicz P (2020) Serum hypoxia-inducible factor-1α protein level as a diagnostic marker of obstructive sleep apnea. Pol Arch Intern Med 130:158–160
Greer SN, Metcalf JL, Wang Y, Ohh M (2012) The updated biology of hypoxia-inducible factor. EMBO J 31:2448–2460
Guy W (1976) Clinical global impression. In: ECDEU Assessment manual for Psychopharmacology-Revised, Volume DHEW Publ. No. ADM 76-338, pp 217–222
Hisli N (1988) Beck Depresyon Envanterinin gecerliligi uzerine bit calisma (a study on the validity of Beck Depression Inventory.). Psikoloji Dergisi 6:118–122
Johnson J, Horwath E, Weissman MM (1991) The validity of major depression with psychotic features based on a community study. Arch Gen Psychiatry 48:1075–1081
Juurlink DN, Buckley N, Stanbrook MB, Isbister G, Bennett MH, McGuigan M (2005) Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev (1):CD002041
Kanekar S, Bogdanova OV, Olson PR, Sung Y-H, D’Anci KE, Renshaw PF (2015) Hypobaric hypoxia induces depression-like behavior in female Sprague-Dawley rats, but not in males. High Alt Med Biol 16:52–60
Kang Y, Chen C, Hu X, Du X, Zhai H, Fang Y, Ye X, Yang W, Sun S (2019) Sestrin2 is involved in asthma: a case–control study. Allergy Asthma Clin Immunol 15:1–6
Kang I, Kondo D, Kim J, Lyoo IK, Yurgelun-Todd D, Hwang J, Renshaw PF (2021) Elevating the level of hypoxia inducible factor may be a new potential target for the treatment of depression. Med Hypotheses 146:110398
Kious BM, Kondo DG, Renshaw PF (2018) Living high and feeling low: altitude, suicide, and depression. Harv Rev Psychiatry 26:43–56
Kuschel A, Simon P, Tug S (2012) Functional regulation of HIF-1α under normoxia—is there more than post-translational regulation? J Cell Physiol 227:514–524
Kushwah N, Jain V, Deep S, Prasad D, Singh SB, Khan N (2016) Neuroprotective role of intermittent hypobaric hypoxia in unpredictable chronic mild stress induced depression in rats. PLoS One 11:e0149309
Lamers F, Milaneschi Y, Vinkers CH, Schoevers RA, Giltay EJ, Penninx BWJH (2020) Depression profilers and immuno-metabolic dysregulation: longitudinal results from the NESDA study. Brain Behav Immun 88:174–183
Lee JH, Budanov Andrei V, Karin M (2013) Sestrins orchestrate cellular metabolism to attenuate aging. Cell Metab 18:792–801
Li F, Nasir M, Olten B, Bloch MH (2019) Meta-analysis of placebo response in adult antidepressant trials. CNS Drugs 33:971–980
Lim S-W, Sung K-C, Shiue Y-L, Wang C-C, Chio C-C, Kuo J-R (2017) Hyperbaric oxygen effects on depression-like behavior and neuroinflammation in traumatic brain injury rats. World Neurosurg 100:128–137
Lindqvist D, Dhabhar FS, James SJ, Hough CM, Jain FA, Bersani FS, Reus VI, Verhoeven JE, Epel ES, Mahan L (2017) Oxidative stress, inflammation and treatment response in major depression. Psychoneuroendocrinology 76:197–205
Lindqvist D, Dhabhar FS, James SJ, Hough CM, Jain FA, Bersani FS, Reus VI, Verhoeven JE, Epel ES, Mahan L, Rosser R, Wolkowitz OM, Mellon SH (2017) Oxidative stress, inflammation and treatment response in major depression. Psychoneuroendocrinology 76:197–205
Maes M, Galecki P, Chang YS, Berk M (2011) A review on the oxidative and nitrosative stress (O&NS) pathways in major depression and their possible contribution to the (neuro) degenerative processes in that illness. Prog Neuropsychopharmacol Biol Psychiatry 35:676–692
Maj M, Pirozzi R, Magliano L, Fiorillo A, Bartoli L (2007) Phenomenology and prognostic significance of delusions in major depressive disorder: a 10-year prospective follow-up study. J Clin Psychiatry 68:14450
Meyers BS, Alexopoulos GS, Kakuma T, Tirumalasetti F, Gabriele M, Alpert S, Bowden C, Meltzer HY (1999) Decreased dopamine beta-hydroxylase activity in unipolar geriatric delusional depression. Biol Psychiat 45:448–452
Mohany KM, Al Rugaie O (2020) Association of serum sestrin 2 and betatrophin with serum neutrophil gelatinase associated lipocalin levels in type 2 diabetic patients with diabetic nephropathy. J Diabetes Metab Disord 19:249–256
Nelson JC, Davis JM (1997) DST studies in psychotic depression: a meta-analysis. Am J Psychiatry 154:1497–1503
Østergaard SD, Bille J, Søltoft-Jensen H, Lauge N, Bech P (2012) The validity of the severity–psychosis hypothesis in depression. J Affect Disord 140:48–56
Østergaard SD, Rothschild AJ, Uggerby P, Munk-Jørgensen P, Bech P, Mors O (2012b) Considerations on the ICD-11 classification of psychotic depression. Psychother Psychosom 81:135–144
Østergaard SD, Bertelsen A, Nielsen J, Mors O, Petrides G (2013) The association between psychotic mania, psychotic depression and mixed affective episodes among 14,529 patients with bipolar disorder. J Affect Disord 147:44–50
Østergaard SD, Petrides G, Dinesen PT, Skadhede S, Bech P, Munk-Jørgensen P, Nielsen J (2013) The association between physical morbidity and subtypes of severe depression. Psychother Psychosom 82:45–52
Østergaard SD, Waltoft BL, Mortensen PB, Mors O (2013) Environmental and familial risk factors for psychotic and non-psychotic severe depression. J Affect Disord 147:232–240
Pan C, Chen Z, Li C, Han T, Liu H, Wang X (2021) Sestrin2 as a gatekeeper of cellular homeostasis: physiological effects for the regulation of hypoxia-related diseases. J Cell Mol Med 25:5341–5350
Park M-H, Kim T-S, Yim H-W, Jeong SH, Lee C, Lee C-U, Kim J-M, Jung S-W, Lee M-S, Jun T-Y (2010) Clinical characteristics of depressed patients with a history of suicide attempts: results from the CRESCEND study in South Korea. J Nerv Ment Dis 198:748–754
Pasha M, Eid AH, Eid AA, Gorin Y, Munusamy S (2017) Sestrin2 as a novel biomarker and therapeutic target for various diseases. Oxidative Med Cell Longev 2017:3296294
Petrides G, Fink M, Husain MM, Knapp RG, Rush AJ, Mueller M, Rummans TA, O’Connor KM, Rasmussen KG Jr, Bernstein HJ (2001) ECT remission rates in psychotic versus nonpsychotic depressed patients: a report from CORE. J ECT 17:244–253
Posener JA, DeBattista C, Williams GH, Kraemer HC, Kalehzan BM, Schatzberg AF (2000) 24-hour monitoring of cortisol and corticotropin secretion in psychotic and nonpsychotic major depression. Arch Gen Psychiatry 57:755–760
Rahmati M, Ferns GA, Mobarra N (2021) The lower expression of circulating miR-210 and elevated serum levels of HIF-1α in ischemic stroke; possible markers for diagnosis and disease prediction. J Clin Lab Anal 35:e24073
Rotschild AJ, Samson JA, Bond TC, Luciana MM, Schildkraut JJ, Schatzberg AF (1993) Hypothalamic-pituitary-adrenal axis activity and 1-year outcome in depression. Biol Psychiat 34:392–400
Salim S (2017) Oxidative stress and the central nervous system. J Pharmacol Exp Ther 360:201–205
Semenza GL (2000) HIF-1: mediator of physiological and pathophysiological responses to hypoxia. J Appl Physiol 88:1474–1480
Smaga I, Niedzielska E, Gawlik M, Moniczewski A, Krzek J, Przegaliński E, Pera J, Filip M (2015) Oxidative stress as an etiological factor and a potential treatment target of psychiatric disorders. Part 2. Depression, anxiety, schizophrenia and autism. Pharmacol Rep 67:569–580
Sunkari VG, Lind F, Botusan IR, Kashif A, Liu ZJ, Ylä-Herttuala S, Brismar K, Velazquez O, Catrina SB (2015) Hyperbaric oxygen therapy activates hypoxia-inducible factor 1 (HIF-1), which contributes to improved wound healing in diabetic mice. Wound Repair Regen 23:98–103
Sutherland AM, Clarke HA, Katz J, Katznelson R (2016) Hyperbaric oxygen therapy: a new treatment for chronic pain? Pain Pract 16:620–628
Tayyar AT, Tayyar A, Kozali S, Karakus R, Eser A, Abide Yayla C, Yalcin ET, Dag I, Eroglu M (2019) Maternal serum sestrin 2 levels in preeclampsia and their relationship with the severity of the disease. Hypertens Pregnancy 38:13–19
Vythilingam M, Chen J, Bremner JD, Mazure CM, Maciejewski PK, Nelson JC (2003) Psychotic depression and mortality. Am J Psychiatry 160:574–576
Xiao T, Zhang L, Huang Y, Shi Y, Wang J, Ji Q, Ye J, Lin Y, Liu H (2019) Sestrin2 increases in aortas and plasma from aortic dissection patients and alleviates angiotensin II-induced smooth muscle cell apoptosis via the Nrf2 pathway. Life Sci 218:132–138
Yamagata H, Uchida S, Matsuo K, Harada K, Kobayashi A, Nakashima M, Nakano M, Otsuki K, Abe-Higuchi N, Higuchi F (2017) Identification of commonly altered genes between in major depressive disorder and a mouse model of depression. Sci Rep 7:1–10
Ye J, Wang M, Xu Y, Liu J, Jiang H, Wang Z, Lin Y, Wan J (2017) Sestrins increase in patients with coronary artery disease and associate with the severity of coronary stenosis. Clin Chim Acta 472:51–57
You Q, Li L, Xiong S-q, Yan Y-f, Li D, Yan N-n, Chen H-p, Liu Y-p (2019) Meta-analysis on the efficacy and safety of hyperbaric oxygen as adjunctive therapy for vascular dementia. Front Aging Neurosci 11:86
Funding
This study was supported by the Gaziantep University Scientific Research Projects Management Unit (Project number: TF.UT.21.45).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the ethical commission of Gaziantep University with decision number 2021/280. All participants gave written informed consent in accordance with the Declaration of Helsinki.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aslan, E., Demir, B., Ulusal, H. et al. Sestrin-2 and hypoxia-ınducible factor-1 alpha levels in major depressive disorder and its subtypes. Psychopharmacology 240, 1691–1704 (2023). https://doi.org/10.1007/s00213-023-06402-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-023-06402-x