Abstract
Rationale
Binge drinking during adolescence impairs learning and memory on the long term, and many studies suggest a role of neuroinflammation. However, whether neuroinflammation occurs after the very first exposures to alcohol remains unclear, while initial alcohol exposure impairs learning for several days in male rats.
Objectives
To investigate the role of neuroinflammation in the effects of only two binge-like episodes on learning and on neuronal plasticity in adolescent male rat hippocampus.
Methods
Animals received two ethanol i.p. injections (3 g/kg) 9 h apart. Forty-eight hours later, we recorded long-term depression (LTD) and potentiation (LTP) in CA1 area of hippocampus slices. In isolated CA1, we measured immunolabelings for microglial activation and Toll-like receptor 4 (TLR4) and mRNA levels for several cytokines.
Results
Forty-eight hours after the two binges, rats performed worse than control rats in novel object recognition, LTD was reduced, LTP was increased, and excitatory neurotransmission was more sensitive to an antagonist of the GluN2B subunit of the NMDA receptor. Exposure to ethanol with minocycline or indomethacin, two anti-inflammatory drugs, or with a TLR4 antagonist, prevented all effects of ethanol. Immunolabelings at 48 h showed a reduction of neuronal TLR4 that was prevented by minocycline pretreatment, while microglial reactivity was undetected and inflammatory cytokines mRNA levels were unchanged.
Conclusion
Two binge-like ethanol exposures during adolescence in rat involved neuroinflammation leading to changes in TLR4 expression and in GluN2B functioning inducing disturbances in synaptic plasticity and cognitive deficits. Anti-inflammatory drugs are good candidates to prevent brain function and memory deficits induced by few binge-drinking episodes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Binge drinking behavior consists in repeated cycles of alcohol intoxication episodes that brings blood alcohol level to 0.08 g/L in 2 h, and abstinence (Rolland and Naassila, 2017; Courtney and Polich 2009; Maurage et al. 2020). This pattern is common practice in adolescents and young adults, while the brain is not mature (Gogtay et al. 2004) and vulnerable to ethanol (Spear 2018). Both clinical and preclinical studies demonstrated memory impairments (Oliveira et al. 2015; Carbia et al. 2017; Smith et al. 2017; Gierski et al. 2020) in adolescent binge drinkers (Nagel et al. 2005), adult heavy drinkers (Beresford et al. 2006) and young adult rats exposed to long sequence of repeated binge drinking (Oliveira et al. 2015; Swartzwelder et al. 2014; Risher et al. 2015). Interestingly, such effects of ethanol have been associated with a smaller hippocampus in young binge drinker (Nagel et al. 2005). Despite the known memory impairments after alcohol exposure, the cellular mode of action of ethanol is not yet fully understood. Moreover, few information is available regarding the consequences of the very first binge drinking episodes, while these episodes might define the fundamental steps leading to long-lasting memory disturbances and/or alcohol addiction in adulthood after a history of binge drinking (Alaux-Cantin et al. 2013; Tavolacci et al. 2019). One of the current hypotheses on the mechanisms of action of ethanol is binge drinking-induced neuroinflammation (Pascual et al. 2018). More precisely, intermittent alcohol exposure for 30 days during adolescence in rat is associated with an increase of TLR4 expression during adulthood notably in the hippocampus and accompanied with cognitive dysfunction (Vetreno and Crews 2015). Post-mortem analysis of brain from alcoholic patients indicated the presence of chronic neuroinflammation through increased neuroimmune signaling protein expressions such as Toll-like receptors (TLR) 2, 3 and 4 in the orbitofrontal cortex (Crews et al. 2013). Interestingly, however, one binge drinking episode in humans is associated with a transient increase of TNF-α, a pro-inflammatory cytokine, in the blood 20 min after alcohol consumption (Afshar et al. 2015), suggesting an early and transient inflammation due to binging. Therefore, and in contrast to a chronic state of neuroinflammation measured after a history of binge drinking, it is possible that neuroinflammation is triggered during each intoxication, disappearing during recovery of the subject from alcohol intoxication. Thus, whether the first exposures to ethanol binge induce neuroinflammatory processes that may lead to cognitive deficits, as we previously reported (Silvestre de Ferron et al. 2015), is unclear.
The cellular mechanisms of learning and memory involve bidirectional plasticity in the hippocampus, that is long-term depression (LTD) and long-term potentiation (LTP). These signals can be measured either at the somatic level, revealing changes in cellular excitability, or at the dendritic level demonstrating the modulation of synaptic transmission. Importantly, both somatic and synaptic plasticity accompanied learning (Moser 1995) and modulation of some specific somatic transmembrane currents may affect synaptic function involved in learning and memory (Yang et al. 2014). Furthermore, GABA receptors density is higher at the soma and these receptors are one of the targets of ethanol. Therefore, measuring somatic and synaptic plasticity may inform on the mode of action of ethanol, i.e., whether ethanol preferentially changes cellular excitability or synaptic function as shown for isoproterenol in the CA1 area (Heginbotham and Dunwiddie 1991). Regarding the effect of ethanol, LTP is transiently depressed at both cellular sites after 2-week intermittent ethanol exposure during adolescence (Roberto et al. 2002), whereas nothing is known about LTD. In this context, we previously found that the two first episodes of binge drinking in adolescent rats evoke transient cognitive impairments after 48 h, accompanied with an abolition of somatic LTD in CA1 area of the hippocampus and an increase in LTP. These effects were further accompanied with an overexpression of the GluN2B subunit of the NMDA receptor (Silvestre de Ferron et al. 2015; Drissi et al. 2020). However, we still do not know if synaptic LTD is abolished and if neuroinflammation is involved in these effects. A role of inflammatory cytokines in ethanol-induced LTD abolition and overexpression of GluN2B is possible. Indeed, neuronal plasticity in the hippocampus is modulated by several chemokines and cytokines such as TNF-α (Maggio and Vlachos 2018), IL-1β (Ikegaya et al. 2003; Nisticò et al. 2013; Hoshino et al. 2017), TGF-β or IFN-ϒ produced by activated microglia (Muñoz et al. 2016; Flood et al. 2019). In addition, other model of neuroinflammation showed an increase in GluN2B subunit (Tang et al. 2020) and inhibiting IL-1β signaling restore NMDA-dependent transmission in some neurodegenerative disease (Bertani et al. 2017). Here, we hypothesize that two binge-like ethanol exposures in adolescent rat disturb the different forms of neuronal plasticity in CA1 area and learning at 48-h delay because of ethanol-induced inflammation. To check this hypothesis, we treated animals with ethanol and anti-inflammatory agents or an antagonist of TLR4 to prevent the effects of ethanol at behavioral and cellular levels in the hippocampus. In addition, we performed immunohistochemistry and biochemical analyses at 48 h to test whether ethanol-induced disturbances involved a long-lasting inflammation.
Materials and methods
Animals and groups
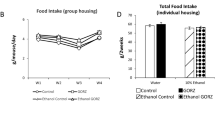
Late adolescent (45–55 days old; Schneider, 2013) male Sprague–Dawley rats received 2 ethanol (EtOH) injections 9 h apart (3 g/kg, i.p.) leading to blood ethanol content (BEC) of ca. 200 mg/dl at 30 min (Silvestre de Ferron et al. 2015; Drissi et al. 2020). We chose the dose of EtOH according to the mean level of BEC measured in French emergency hospital unit. The time between injections was determined considering the higher rate of ethanol metabolization in rodents and the necessity of a period without alcohol between binge episodes (Silvestre de Ferron et al. 2015). We studied only male rats because of the complexity of studying synaptic plasticity and alcohol interactions in female animals as we previously found (Rabiant et al. 2021). Pretreatment with anti-inflammatory-related agents (minocycline, MINO; indomethacin, INDO or TAK-242) was performed 30 min prior to each ethanol administration (Lu et al. 2017; Vetreno et al. 2018) ( Fig. 1). We tested control group (4 saline injections), MINO or INDO or TAK-242 group (2 drug + 2 saline injections), EtOH group (2 saline + 2 ethanol injections) and EtOH + MINO or EtOH + INDO, or EtOH + TAK-242 group (2 drug + 2 ethanol injections). Experiments were performed 48 h after the first injection following the European Community guiding principles for the care and use of animals (2010/63/UE, CE Off. J. October 20, 2010), the French Decree N° 2013‐118 and the local ethics committee rules (CREMEAP, project N° 3829 and 20,838).
Electrophysiology
We used 118 animals for electrophysiology. The brain of isoflurane anesthetized rats was immersed in a cutting solution (220 mM sucrose, 2 mM KCl, 1.3 mM NaH2PO4, 26 mM NaHCO3, 6 mM MgCl2, 0.2 mM CaCl2, 10 mM glucose; pH 7.2–7.4; 4 °C). 400-µm-thick dorsal hippocampus slices were prepared (vibratome Leica VT1200S, Rueil-Malmaison, France) and stored for 2 h at room temperature (RT) in a carbogen (95% O2, 5% CO2) gassed artificial cerebrospinal fluid (aCSF) composed of: 125 mM NaCl, 3 mM KCl, 1.25 mM NaH2PO4, 25 mM NaHCO3, 1.3 mM MgCl2, 2.3 mM CaCl2, 10 mM glucose; pH 7.2–7.4. The recording chamber was perfused with aCSF (28 ± 1 °C, flow rate: 6 mL/min). The Schaffer collaterals were stimulated using a bipolar tungsten electrode (PHYMEP, France), and signals were recorded with a 3 M NaCl (1–3 MΩ) filled glass microelectrodes placed in the CA1 stratum pyramidale or the stratum radiatum. For each slice, an input/output relationship determined the maximal response and the test stimulus intensity was set to 50–60% of this maximum. For field excitatory post-synaptic potentials recording (fEPSPs), maximal response was determined at stimulus intensity that evoked a population spike into the EPSP. We measured the amplitude of the population spikes instead of the slope of the initial positive signal (EPSP) because these parameters are not always changed in the same direction (Heginbotham and Dunwiddie 1991) and the slope of the dendritic fEPSPs. All signals were amplified (Grass amplifier, × 1000‐2000), filtered (1‐3 kHz) and recorded on computer with signal software (CED, Cambridge, UK). LTD was induced with 900 paired stimuli (200-ms interpulse interval) delivered at 1 Hz (pLFS), and LTP was induced with 3 × 1 s stimulation delivered at 33 Hz, or 2 × 1 s stimulation at 50 Hz, spaced by 10 s. LTP and LTD magnitude was expressed as the percentage of change of the response averaged during the last 10 min of recording and compared with the normalized baseline amplitude. NMDA-fEPSPs were recorded in a low-Mg2+ aCSF (0.1 mM MgCl2) containing CNQX (15 µM) and (-)-bicuculline methobromide (20 µM), and a GluN2B antagonist was applied (5 µM Ro25-6981). Result was expressed as the percentage of slope inhibition in the presence of Ro25-6981 and was calculated considering the effects of D-AP5 (50 µM), added at the end of recordings as 100% of fEPSP inhibition.
Immunohistochemistry and real-time PCR
Rats were anesthetized with pentobarbital (60 mg/kg i.p.), received heparin (2,500 IU, i.p.) and were transcardially perfused with heparinized 0.9% saline and iced 4% paraformaldehyde (PFA) in 0.1 M phosphate-buffered saline (PBS, pH 7.4). Brains were post-fixed in PFA and transferred in a 30% sucrose solution. Coronal Sects. (50 µm) were cut along the anterior–posterior axis of the CA1 at the Bregma and stored at -20 °C in cryoprotective solution (ethylene glycol 30%; sucrose 30%, NaCl 0.9%, in PBS 1X).
Iba1 immunofluorescence
Brain floating sections were washed 3 × 5 min with PBS 1x-T (PBS 0.1 M, 0.2% Triton X-100, pH 7.5) and then placed for 1 h at room temperature (RT) in 5% donkey blocking serum (PBS 0.1 M; 0.1% BSA; 0.1% Triton X-100). Sections were incubated at 4 °C for 72 h with primary antibody goat anti-Iba1 diluted 1/200 (ab5076, Abcam). Sections were washed 3 × 5 min with PBS 1x-0,1% Triton X-10 and were incubated for 1 h at RT in AlexaFluor 594 donkey anti-goat secondary antibody (Interchim 705 0.585.147, Interbiotech) diluted 1/250. Following 4 × 5 min washes with PBS 1x, sections were mounted as described previously. For each rat, we analyzed the body cell size and the circularity index of 10 CA1 stratum pyramidale microglia taken randomly (N = 8 in each groups).
TLR4 and NeuN immunofluorescence
Brain floating sections were washed 3 × 5 min with PBS 1x-T (PBS 0.1 M, 0.2% Triton X-100, pH 7.5), 30 min in methanol with 3% H2O2, washed 2 × 10 min in PBS 1x-T and placed in goat blocking serum (PBS 0.1 M; 0.1% BSA; 0.2% Triton X-100; 2% Goat serum, Bio West, Cat nº S2000-100) for 30 min at RT. Sections were incubated at 4 °C for 48 h with primary antibodies rabbit anti-TLR4 (NB56566 Novus bio, France) and mouse anti-NeuN (MAB 377 Merck Millipore), diluted 1: 50 and 1:100 in goat blocking serum, respectively. Afterward, sections were washed 3 × 5 min with PBS 1x-T and incubated for 1 h at RT in AlexaFluor 594 goat anti-rabbit IgG secondary antibody solution (111–585-003, Jackson ImmunoResearch Laboratories) and AlexaFluor 488 goat anti-mouse IgG secondary antibody (115–545-003, Jackson ImmunoResearch Laboratories), both diluted 1:250 in a solution of blocking serum of goat (Bio West, Cat nºS2000-100) and horse (Vectastain ABC Kit (Universal) PK-6200). Following 4 × 5 min washes with PBS 1x, sections were mounted on gelatinized microscope slides and lamellae with DAPI (4',6'-diamidino-2-phenylindole) containing mounting solution (Life Technologies Prolong Gold P36931). For each rats, we chose 15 neurons randomly, in the left and the right CA1 stratum pyramidale, and measured the immunofluorescence for NeuN and TLR4, and calculated the ratio of the labeling. NeuN immunofluorescence was used as normalization, and the ratio represents TLR4 changes. A z-stack of seven 2-µm adjacent layers with the highest fluorescence intensity was recorded for each field and pooled. Equal sized images were recorded from each tissue section with identical settings for excitation, detection, objective lens, aperture, laser power and photomultiplier gain/offset.
No immunoreactive cells were found when omitting the primary antibody; all photographs were taken with an AxioCam camera using confocal microscopy (Zeiss LSM170) and analyzed using ImageJ software (National Institute of Health, USA) by an experimenter blind to the experimental groups.
For RT-qPCR experiments, total RNA was extracted from isolated CA1 using ReliaPrep™ RNA Miniprep Systems (Promega, Charbonnières-les-bains, France). One microgram of total RNA was reverse transcribed into cDNA with multiscribe reverse transcriptase (Applied Biosystems). RT-qPCR was performed in triplicate for each sample using SYBR Green Supermix (Promega, Charbonnières-les-bains, France) for 35 cycles with a 3-step program (10 s of denaturation at 95 °C, 15 s of annealing at 60 °C and 20 s of elongation at 72°). Amplification specificity was assessed with a melting curve analysis, and mRNA levels were calculated using the 2−ΔΔCT method (Livak and Schmittgen 2001) relative to control values after normalization with GAPDH mRNA. The primers used are presented in Table 1.
Drugs
Ethanol (VWR, Strasbourg, France) was prepared in saline (0.9% NaCl) at a final concentration of 20% according to the Gay-Lussac Table. Minocycline hydrochloride (Hello Bio, UK) was prepared in saline with gentle warming and administered at 45 mg/kg, i.p. (Wang et al. 2015; Haber et al. 2018). Indomethacin (Hello Bio, UK) was prepared in saline containing 2% dimethylsulfoxid (DMSO) and administered at 4 mg/kg, i.p. (Pascual et al. 2007; Vetreno et al. 2018). TAK-242 (Sigma-Aldrich, France) was dissolved in DMSO and diluted in saline (final concentration of DMSO: 1%) and used at 3 mg/kg, i.p. (Pascual et al. 2007; Hwang et al. 2017; Vetreno et al. 2018). 6-Cyano-7-nitroquinoxaline-2,3-dione (CNQX; Sigma-Aldrich, France) was dissolved in DMSO and used at 15 µM final concentration (final concentration of DMSO: 0,15%); (-)-bicuculline methobromide, D-(-)-2-amino-5-phosphonopentanoic acid (D-AP5) and Ro 25–6981 maleate (Hello Bio, UK) were dissolved in distilled water and used at a final concentration of 20, 50 and 5 µM, respectively. IL-1β was prepared in distilled water and bath applied at 30 ng/mL in aCSF containing 1 µg/mL bovine serum albumin (BSA) 30 min before LTD induction (Nisticò et al. 2013).
Novel object recognition
Forty rats were handled every day the week preceding the experiment and were habituated to the experiment room and apparatus 3 times a week. The apparatus was a square box made of opaque Plexiglas (45 × 45 × 45 cm) with an open top under a 30‐lux illumination. Learning (phase 1) took place 48 h after treatments, and rats were transferred to the experiment room 30 min prior to the experiment and, then, placed into the arena for 10 min with two objects, A and B, placed at equal distance from the walls and different in form, material, color and too heavy to be moved. We checked for absence of spontaneous preference in phase 1. The apparatus and objects were cleaned between each animal to avoid bias. Recognition (phase 2) was performed 48 h later by replacing one familiar object (A or B) by a new one (object C) in a 5-min session. To counterbalance a possible effect of object A over B, the test was performed with object A as the familiar object in half of the cases, and in the other half, the object B was the familiar object. Digital video acquisition system (Pinnacle Studio HD v.15 software) was used. We measured the total exploration time spent on objects in both phase (sniffing, licking or touching the objects with forelimbs). Analysis was performed on all animals by two independent experimenters who were blind to the experimental conditions. An additional check of the video was done in case of divergence between the two experimenters. Exploration time for an object was normalized and expressed as a percentage of time spent by rats on an object compared with the total exploration time as follows: time spent on novel object (%) = novel object (s) / (novel object (s) + familiar object (s)) × 100. Total exploration time (s) was measured to reveal a potential effect of treatments on animal’s global exploratory activity. Animals that did explored both objects for at least 10 s were excluded.
Statistics
All data are expressed as mean ± SEM. For electrophysiology, “n” represents the number of slices and “N” the number of animals. Statistics were conducted using SigmaStat® (LogiLabo, Paris, France). A two‐way ANOVA with ethanol and minocycline or indomethacin or TAK-242 as factors was used for electrophysiology, behavior and immunochemistry. Post hoc multiple comparisons were made using a Tukey’s test. Learning phase of the NOR and IL-1β effect on LTD was tested with an unpaired Student’s t test. We applied a one-way ANOVA to RT-qPCR. We used the Shapiro–Wilk normality test in all case, and if it failed, we used an ANOVA on ranks Kruskal–Wallis test. Statistical significance was set at P < 0.05.
Results
Ethanol-induced memory impairments are prevented by minocycline pretreatment
In novel object recognition (NOR, Fig. 2), there was no spontaneous preference for the objects during the learning phase since no difference in the percentage of time spent on each object was found (object A: 48.5 ± 1.3%, N = 32 vs object B: 51.5 ± 1.3%, N = 32; P = 0.108). Furthermore, there was no effect of the treatments on locomotor activity since ANOVA of the total exploration time showed no significant effect of minocycline (F1,30 = 4.065, P = 0.053), of EtOH (F1,30 = 0.0177, P = 0.895) and no interaction (F1,28 = 0.186, P = 0.67; Fig. 2B). During recognition phase (Fig. 2C), a two-way ANOVA showed a significant effect of minocycline (F1,30 = 6.974, P = 0.013), no effect of EtOH (F1,30 = 1.227, P = 0.277) and an interaction between EtOH and minocycline (F1,28 = 6.247, P = 0.019). Post hoc analysis (Tukey’s test) revealed no significant difference in the time spent on the novel object between control and minocycline (NaCl: 59.9 ± 1.4%, N = 8 vs MINO: 60.2 ± 2.3%, N = 9; P = 0.918). However, animals treated with ethanol spent less time exploring the novel object compared with control (EtOH: 52.4 ± 2.63%, N = 6 vs NaCl: 59.9 ± 1.4%, N = 8; P = 0.024, Fig. 2C). Minocycline increased the percentage of time spent exploring the novel object (EtOH + MINO: 63.15 ± 1.95%, N = 9 vs EtOH 52.4 ± 2.63%, N = 6; P = 0.002) to a value similar to the MINO group (P = 0.299). Regarding the total exploration time for phase 2, a two-way ANOVA revealed a lack of effect of either minocycline (F1,30 = 3.984, P = 0.056), EtOH (F1,30 = 2.464, P = 0.128) or their interaction (F1,28 = 0.059, P = 0.81) (Fig. 2C). In summary, learning in NOR is impaired 48 h after two ethanol binge-like episodes and minocycline co-exposure prevented this effect.
The effects of ethanol and minocycline on learning capability in novel objet recognition (NOR) task. A) NOR protocol. B) Time spent on objects A and B during the learning phase (phase 1) reveals no spontaneous preference for the presented object (N = 32). Below is the total exploration time for each group showing no significant differences between groups. C) Top: time spent on the novel objet during recognition phase (phase 2). Ethanol (EtOH)-treated animals spent less time than control (NaCl) animals exploring the novel object. Minocycline (MINO) had no effect on novel object recognition compared to NaCl. Animals who received MINO before EtOH spent similar time on the novel object than NaCl animals. Bottom: total exploration time during phase 2 showing no effects of any treatments. Mean values are given ± standard error of the mean (SEM). N means numbers of animals. *P < 0.05; **P < 0.01
Anti-inflammatory agents prevent dendritic LTD abolition after ethanol
We recorded dendritic LTD in the stratum radiatum. A two-way ANOVA showed an effect of minocycline (F1,15 = 17.702, P = 0.001), of EtOH (F1,15 = 8.565, P = 0.012) and an interaction (F1,15 = 14.805, P = 0.002). Post hoc analysis (Tukey’s test) revealed an abolition of LTD after EtOH (EtOH:—4.3 ± 2.3%, n = 5, N = 4 vs NaCl:—27.2 ± 3.6%, n = 4, N = 3; P < 0.001, Fig. 3A1-A2). Minocycline alone had no effect on dendritic LTD (MINO:—28.4 ± 3.6%, n = 4, N = 3 vs NaCl:—27.2 ± 3.6%, n = 4, N = 3; P = 0.808, Fig. 3A1-A2). Minocycline applied before ethanol increased dendritic LTD compared with ethanol (EtOH + MINO:—31.5 ± 4.1%, n = 4, N = 2 vs EtOH:—4.3 ± 2.3%, n = 5, N = 4; P < 0.001, Fig. 3A1-A2) and resumed values to minocycline alone (MINO vs EtOH + MINO, P = 0.537). In summary, 48 h after two ethanol binge-like episodes, dendritic LTD is abolished and minocycline prevented this effect.
Minocycline is an antibiotic with anti-inflammatory properties. To demonstrate further the involvement of inflammation, we tested indomethacin, a non-steroidal anti-inflammatory (Fig. 3B). A two-way ANOVA revealed a significant effect of both indomethacin (F1,29 = 8.349, P = 0.008) and ethanol (F1,29 = 12.451, P = 0.002) and no significant interaction (F1,27 = 3.468, P = 0.073). Post hoc analysis (Tukey’s test) showed a significant reduction of synaptic LTD after ethanol (EtOH:—11.5 ± 4.2%, n = 7, N = 5 vs NaCl:—30.7 ± 4.0%, n = 8, N = 4; P = 0.003, Fig. 3B1-B2). Like minocycline, indomethacin alone had no effect on LTD compared with control (INDO:—37.4 ± 4.0%, n = 8, N = 3 vs NaCl,—30.7 ± 4.0%, n = 8, N = 4; P = 0.241, Fig. 3B1-B2). However, it prevented the abolition of synaptic LTD induced by ethanol (EtOH + INDO:—33.3 ± 4.0%, n = 8, N = 4 vs EtOH:—11.5 ± 4.2%, n = 7, N = 5; P < 0.001) and resumed values to indomethacin alone (INDO vs EtOH + INDO, P = 0.466) (Fig. 3B1-B2). In summary, the inhibitory effect of ethanol on dendritic LTD is also prevented by a pretreatment with indomethacin.
Ethanol-induced abolition of dendritic LTD is prevented by minocycline, indomethacin and TAK-242. A1) Top panel: NaCl and EtOH averaged raw signals during baseline (1, 3) and at the end of the recording (2, 4) (vertical calibration bar: 0.2 mV; horizontal calibration bar: 5 ms). Bottom panel: time course of dendritic long-term depression (LTD) for all slices tested revealing the preventive effect of MINO on EtOH-induced LTD abolition. A2) Top panel: MINO and EtOH + MINO averaged raw signals during baseline (5, 7) and at the end of the recording (6, 8) (vertical calibration bar: 0.2 mV; horizontal calibration bar: 5 ms). Bottom panel: bar graph illustrating the LTD magnitude for all groups. B1) Preventive effect of INDO on EtOH-induced LTD abolition. B2) Bar graph illustrating the LTD magnitude for all groups. C1) Prior administration of TAK-242 prevented the LTD disruption induced by EtOH. C2) Bar graph illustrating the LTD magnitude for each group. Mean values are given ± standard error of the mean (SEM). n means numbers of slices. Number of animals in A: NaCl, N = 3; MINO, N = 3; EtOH, N = 4; EtOH + MINO, N = 2. In B, NaCl, N = 4; INDO, N = 3; EtOH, N = 5; EtOH + INDO, N = 4. In C, NaCl, N = 3; TAK-242, N = 3; EtOH, N = 7; EtOH + TAK-242, N = 3. **P < 0.01; ***P < 0.001
In order to investigate further the role of neuroinflammation we administered TAK-242, an antagonist of TLR4 involved in the production of cytokines, 30 min before each ethanol injection. A two-way ANOVA of dendritic LTD (Fig. 3C) revealed a significant effect of both TAK-242 (F1,29 = 4.658, P = 0.04) and ethanol (F1,29 = 5.246, P = 0.03) and an interaction (F1,27 = 15.527, P < 0.001). Post hoc analysis (Tukey’s test) showed a reduction of LTD in EtOH slices compared with control (EtOH: -9.5 ± 3%, n = 9, N = 7 vs NaCl:—32.9 ± 4.5%, n = 7, N = 3; P < 0.001, Fig. 3C1-C2). TAK-242 alone had no effect on LTD compared with control (TAK-242: -26.2 ± 4.8%, n = 7, N = 3 vs NaCl,—32.9 ± 4.5%, n = 7, N = 3; P = 0.239, Fig. 3C1-C2). However, TAK-242 prevented the reduction of synaptic LTD after ethanol (EtOH + TAK-242: -32.4 ± 3%, n = 8, N = 3 vs EtOH: -9.5 ± 3%, n = 9, N = 7; P < 0.001) and resumed values to TAK-242 alone (TAK-242 vs EtOH + TAK-242, P = 0.26; Fig. 3C1-C2). Hence, pretreatment with TAK-242 prevents LTD abolition induced by ethanol.
Minocycline also prevents the effects of the two binge on hippocampus somatic plasticity
We further wished to check whether ethanol exposure altered similarly dendritic and somatic LTD since the latter reflects excitatory level of pyramidal neurons mainly determined by a balance between glutamatergic excitations and GABAergic inhibitions, the two major targets of ethanol. Regarding LTD (Fig. 4), a two-way ANOVA revealed a lack of effect of minocycline (F1,36 = 2.711, P = 0.109), an effect of EtOH (F1,36 = 9.021, P = 0.005) and an interaction (F1,34 = 5.13, P = 0.03). Post hoc analysis (Tukey’s test) showed a smaller LTD after ethanol (EtOH: -17.2 ± 4.2%, n = 12, N = 6 vs NaCl: -44.2 ± 4.8%, n = 9, N = 6; P < 0.001, Fig. 4A). Minocycline alone had no effect on LTD compared with control (MINO: -41 ± 6.4%, n = 8, N = 5 vs NaCl: -44.2 ± 4.8%, n = 9, N = 6; P = 0.679, Fig. 4B). When minocycline was administered before ethanol (EtOH + MINO group), LTD reached -37.3 ± 5.3% (n = 9, N = 5, Fig. 4C-D), a value similar to LTD in the MINO group (P = 0.621) and greater to the EtOH group (P = 0.006). In summary, minocycline prevents the inhibitory effect of two ethanol binge-like episodes on somatic LTD at 48-h delay.
Minocycline prevents somatic LTD depression after ethanol. Top panel: averaged raw signals during baseline (1,3) and at the end of the recording (2, 4) (vertical calibration bar: 0.2 mV; horizontal calibration bar: 10 ms). Middle panel: single slice recording corresponding to the above averaged signals. A) LTD was significantly decreased in ethanol (EtOH) slices (N = 6, n = 12) compared with control (NaCl, N = 6, n = 9). B) Minocycline (MINO, N = 5, n = 8) had no effect on somatic LTD. C) Prior administration of MINO (EtOH + MINO, N = 5, n = 9), prevented LTD abolition by EtOH. D) Bar graph for LTD magnitude in each condition. Mean values are given ± standard error of the mean (SEM). n means numbers of slices. **P < 0.01; ***P < 0.001
Regarding somatic LTP, we previously found that the two-ethanol binge-like exposures altered the threshold to induce LTP (Silvestre de Ferron et al. 2015). Here, we checked whether minocycline also prevented this effect. For this purpose, we tested two different high-frequency stimulation (HFS) in order to elaborate a BCM-like curve (Bienenstock-Cooper-Munro; Fig. 5). When LTP was triggered with HFS 3 × 33 Hz (Fig. 5A), a two-way ANOVA revealed no effect of minocycline (F1,18 = 2.774, P = 0.115), an effect of EtOH (F 1,18 = 8.193, P = 0.011) and no interaction (F 1,16 = 2.729, P = 0.118). Post hoc analysis (Tukey’s test) indicated similar LTP magnitude between control and minocycline alone (NaCl: 17.4 ± 5.5%, n = 5, N = 4 vs MINO: 17.4 ± 3.4%, n = 5, N = 4; P = 0.993). In contrast, 48 h after the two binge, LTP magnitude was increased compared with control (EtOH: 34.8 ± 1.6%, n = 5, N = 3 vs NaCl: 17.4 ± 5.5%, n = 5, N = 4; P = 0.006). Interestingly, administration of minocycline before ethanol decreased LTP as compared to ethanol (EtOH + MINO: 22 ± 3.9%, n = 5, N = 3 vs EtOH: 34.8 ± 1.6%, n = 5, N = 3; P = 0.032) and resumed values to minocycline alone (MINO vs EtOH + MINO, P = 0.405). When we tested HFS 2 × 50 Hz (Fig. 5B), a two-way ANOVA revealed no significant effect of minocycline (F1,15 = 2.96, P = 0.109), a significant effect of EtOH (F1,15 = 11.393, P = 0.005) and an interaction (F1,13 = 7.959, P = 0.014). Post hoc analysis (Tukey’s test) showed no difference in LTP magnitude between control and minocycline (NaCl: 27.4 ± 3.7%, n = 5, N = 4 vs MINO: 30.8 ± 3.9%, n = 4, N = 3; P = 0.438). Here again, EtOH induced an increase of LTP compared to control (EtOH: 46.9 ± 2.3%, n = 4, N = 3 vs NaCl: 27.4 ± 3.7%, n = 5, N = 4; P < 0.001). In this condition too, administration of minocycline before ethanol reduced LTP compared with ethanol alone (EtOH + MINO: 32.6 ± 1.5%, n = 4, N = 2 vs EtOH: 46.9 ± 2.3%, n = 4, N = 3; P = 0.008) and with no difference with minocycline alone (EtOH + MINO vs MINO, P = 0.709). After ethanol, the BCM-like curve is shifted to the left (Fig. 5C) revealing a change in the threshold for LTP versus LTD. In the presence of minocycline, the curve in the presence of ethanol resumes to the control curve. In summary, somatic LTP is increased 48 h after two ethanol binge-like episodes and LTD is decreased. Minocycline alone had no effect but prevented the effects of ethanol on LTP, LTD and on the left shift of the threshold for bidirectional plasticity.
Minocycline prevents the effects of ethanol on LTP and on the threshold for bidirectional plasticity. A) Left: time course of LTP induced by HFS 3 × 33 Hz for each treatment. Right: bar graph showing LTP magnitude in the different conditions. Minocycline (MINO, N = 4, n = 5) alone had no effect on LTP compared with control (NaCl, N = 4, n = 5). Ethanol (EtOH, N = 3, n = 4) significantly increased LTP and prior administration of MINO (N = 3, n = 5) prevented this effect. B) Similar representation for LTP induced with HFS 2 × 50 Hz. MINO (N = 3, n = 4) alone had no effect on LTP. EtOH (N = 3, n = 4) increased LTP and prior administration of MINO (N = 2, n = 4) prevented this effect of EtOH. C) Bernstein–Cooper–Munro (BCM) curve indicating the ability of neurons to trigger LTP or LTD according to the frequency of stimulation (Hz). The curve for EtOH was shifted to the left compared with NaCl while that for MINO was similar to NaCl group. Thus, MINO pretreatment brought back the curve to control. Mean values are given ± standard error of the mean (SEM). n means numbers of slices. *P < 0.05; **P < 0.01; ***P < 0.001
Anti-GluN2B agent is more effective 48 h after the initial binge
In previous studies, the two ethanol binges increased the sensitivity of NMDA-fEPSPs to an antagonist of the GluN2B subunit of the NMDA receptor at 48-h delay. We thus tested whether an anti-inflammatory was able to prevent this effect. NMDA-fEPSPs were pharmacologically isolated in CA1, and its sensitivity to a GluN2B antagonist was assessed with bath application of 5 µM Ro25-6981 (Fig. 6). A two-way ANOVA showed no significant effect of both minocycline (F1,29 = 0.788, P = 0.383) and ethanol (F1,29 = 2.324, P = 0.139) but a significant interaction between minocycline and ethanol (F1,27 = 5.004, P = 0.034). Post hoc analysis (Tukey’s test) showed that NMDA-fEPSPs sensitivity to Ro25-6981 was higher in EtOH slices compared with control (EtOH: 31.4 ± 3%, n = 8, N = 6 vs NaCl: 19.2 ± 3.7%, n = 8, N = 7; P = 0.012, Fig. 6A-B). Minocycline alone had no effect on NMDA-fEPSPs sensitivity to Ro25-6981 compared with control (MINO: 23.6 ± 3.2%, n = 7, N = 4 vs NaCl: 19.2 ± 3.7%, n = 8, N = 7; P = 0.357). However, when minocycline was administered before ethanol (EtOH + MINO), NMDA-fEPSPs sensitivity to Ro25-6981 was decreased compared with EtOH (EtOH + MINO: 21.2 ± 3%, n = 8, N = 5 vs EtOH: 31.4 ± 3%, n = 8, N = 6; P = 0.033, Fig. 6B). These latter values resumed to MINO alone (EtOH + MINO: 21.2 ± 3%, n = 8, N = 5 vs MINO: 23.6 ± 3.2%, n = 7, N = 4; P = 0.624). Thus, 48 h after two ethanol binge-like episodes, NMDA-fEPSPs sensitivity to a GluN2B antagonist was increased and minocycline prevented this effect.
NMDA-fEPSP response to Ro25-6981, a GluN2B antagonist. A) Averaged raw signal during baseline, after 5 µM Ro25-6981 (Ro-25) and in the presence of 50 µM D-AP5 for each group (vertical calibration bar: 0.02 mV; horizontal calibration bar: 10 ms). B) Bar graph illustrating the percentage of fEPSPs slope inhibition. Minocycline (MINO) alone had no effect. After EtOH, the inhibition was increased, and a prior administration of MINO prevented this effect. Mean values are given ± standard error of the mean (SEM). n means numbers of slices. *P < 0.05. The number of animal for each group is: NaCl, N = 7; MINO, N = 4; EtOH N = 6; EtOH + MINO N = 5
Bath application of IL-1β block synaptic LTD
The fact that anti-inflammatory agents prevent the effects of ethanol on learning and on hippocampus plasticity measured at 48-h delay suggests that circulating cytokine at this time point may be responsible for the blockade of synaptic LTD. In order to check this assumption, we measured whether bath applied IL-1β (or BSA; bovine serum albumin, the solvent) blocked synaptic LTD on hippocampus slices from naïve animals. In the presence of BSA (n = 8, N = 4), LTD reached -35.8 ± 6.1% (Fig. 7A). When IL-1β was bath applied (n = 6, N = 4), LTD was abolished to—4.25 ± 9.1% (Student’s t test, P = 0.011 compared to BSA alone; Fig. 7A-B). In additional experiments, we checked whether the blocking effect of IL-1β on LTD was permanent or transient. Here, we first blocked LTD with IL-1β, washed out the drug and tested again LTD. The result shows that IL-1β blocked LTD only when present in the bath and not on the long-term, after washout of the drug (Fig. 7C). These experiments demonstrate that IL-1β, a pro-inflammatory cytokine, disturbs synaptic LTD.
IL-1β abolished LTD. (A) Bath application of BSA alone (N = 4, n = 8) had no effect on LTD magnitude, whereas Il-1β (in BSA) at 30 ng/ml abolished LTD (N = 4, n = 6). (B) Bar graph summarizing the effects in A. (C) In independent experiments, we check that IL-1β was responsible for LTD blockade by inducing LTD after washout of the drug
mRNA levels for neuroinflammatory markers are unaltered following the two alcohol exposure
Considering that IL-1β abolishes LTD when bath applied on slices, we documented other molecular actors related to neuroinflammation that may also modulate synaptic plasticity. We thus quantified the mRNA levels for neuroinflammatory markers such as TNF-α, IL-1β, IFN-γ and TGF-β. Interestingly, 48 h after ethanol, none of the mRNA levels were altered (Fig. 8), and neither minocycline nor indomethacin pretreatment had an effect (one-way ANOVA, F3,28 = 0.899, P = 0.454; F3,28 = 0.062, P = 0.979; H3,28 = 2.122, P = 0.547; H3,28 = 0.071, P = 0.995, respectively).
Cellular markers for neuroinflammation
Our results suggest that ethanol triggers neuroinflammation to abolish LTD 48 h later, but without any changes in the mRNA levels of inflammatory cytokines. These results suggest that microglial cells, which release cytokines, were possibly not activated at this time point. Using immunohistochemistry, we studied Iba1 labeling of morphological changes in microglia and the expression of TLR4 in NeuN-positive neurons 48 h after ethanol treatment in CA1 area to see whether LTD abolition was accompanied with microglia activation or not.
No microglial activation 48 h after ethanol exposure
A two-way ANOVA of cell body circularity showed no significant effect of both minocycline (F1,30 = 3.161, P = 0.086) and ethanol (F1,30 = 0.007, P = 0.934) and no significant interaction (F1,28 = 0.651, P = 0.426, Fig. 9A-C). Regarding the cell body size, a two-way ANOVA showed no effect of both minocycline (F1,30 = 0.166, P = 0.687) and ethanol (F1,30 = 0.648, P = 0.428) and no significant interaction (F1,28 = 0.594, P = 0.447, Fig. 9B-C). Thus, neither ethanol exposure nor minocycline had an effect on the circularity and cell body size of microglia in the CA1 area at a 48-h delay.
Effects of minocycline on Iba1 immunofluorescence labeling in CA1 area 48 h after the two ethanol binge episodes. (A) Histogram of circularity index of microglia body cells. (B) Histogram of microglia body cells size. There was no effect of ethanol (EtOH) or minocycline (MINO) or the combination on these parameters. (C) Photographs of iba1 immunolabeling in the four groups tested
TLR4 expression in the CA1 pyramidal cell layer 48 h after ethanol
TLR4 receptors were localized in the membrane of the CA1 pyramidal neurons labeled with NeuN (Fig. 10). A two-way ANOVA of TLR4 immunofluorescence showed no significant effect of both minocycline (F1,25 = 1063, P = 0.314) and ethanol (F1,25 = 1.211, P = 0.283) and a significant interaction between minocycline and ethanol (F1,22 = 5.209, P = 0.033). Post hoc analysis (Tukey’s test) revealed that ethanol decreased TLR4 immunofluorescence in CA1 pyramidal neurons by 66% compared to control (P = 0.031, Fig. 10A-C) and that minocycline pretreatment prevented this effect (EtOH vs MINO + EtOH, P = 0.029, Fig. 8A-C). To normalize the labeling, we calculated the ratio between TLR4 and NeuN intensity (Fig. 10B). A two-way ANOVA showed an effect of minocycline (F1,25 = 9.4, P = 0.006), no effect of ethanol (F1,25 = 1.57, P = 0.223) and no interaction (F1,22 = 3.604, P = 0.071). Post hoc analysis (Tukey’s test) showed that ethanol decreased TLR4/NeuN ratio in CA1 by 65% compared to control (P = 0.043) and that minocycline pretreatment prevented this effect (EtOH vs MINO + EtOH, P = 0.002). Altogether, the results show that 48 h after two alcohol exposure, TLR4 is modulated only in pyramidal neurons.
TLR4 immunolabeling in NeuN labeled neurons in hippocampus CA1 area of adolescent rats 48 h after ethanol with or without minocycline. (A) Ethanol decreased the intensity of TLR4 labeling by 64% (P = 0.031), and minocycline pretreatment prevented this effect (EtOH versus EtOH + MINO, P = 0.029). (B) Ethanol decreased the ratio of TLR4 and NeuN labeling by -62% (P = 0.043). Minocycline pretreatment prevented this effect (EtOH versus EtOH + MINO, P = 0.002). (C) Photographs of NeuN, TLR4 and of the co-labeling showed at two different magnifications (scale bar at the top is 50 µm and is 10 µm at the bottom). *: P < 0.05; **: P < 0.01
Discussion
This study demonstrates that in adolescent rats, two ethanol binge-like exposures induce cognitive deficits at 48-h delay together with an increased role for GluN2B, a selective blockade of synaptic LTD and an increase in LTP in the hippocampus but without signs of neuroinflammation at cellular level and at the level of cytokines mRNA. However, the effects of ethanol at behavioral and cellular levels were prevented by pretreatment with different anti-inflammatory agents, suggesting that ethanol exposure induced a rapid, short-lasting neuroinflammation that leads to the changes observed after 48 h.
Disturbances of bidirectional plasticity after only two binge-like episodes
Synaptic plasticity in the hippocampus is considered the mechanism underlying learning and memory. Indeed, LTD is necessary for novelty acquisition (Ge et al. 2010), consolidation of fear memory (Liu et al. 2014) and for working and episodic memories (Zeng et al. 2001). Here, LTD was decreased 48 h after only two ethanol-binge like exposures and this was accompanied with cognitive deficits in a learning task related to LTD (Ge et al. 2010). The present work confirms our previous studies (Silvestre de Ferron et al. 2015; Drissi et al. 2020) and extends them by showing that LTD is reduced at both the soma and the dendritic tree. These latter observations also extend the results from Roberto et al. (2002) who recorded dendritic and somatic LTP after chronic intermittent ethanol exposure along late adolescence in rats. However, it is acknowledged that changes in population spike are unlikely to reflect changes in synaptic strength related to memory. Nonetheless, any facilitation or reduction of synaptic transmission taking place in an ensemble of neurons during learning can be measured through monitoring the population spike magnitude. Indeed, learning is accompanied by parallel changes at both somatic and synaptic level in the hippocampus (Moser 1995). Moreover, GABA receptors are one of the many targets of ethanol and perisomatic inhibitory synapses alterations may be the origin of pathophysiological conditions (Wittner and Maglóczky 2017). Furthermore, both synaptic and somatic regulation of specific transmembrane currents (such as the IA potassium current) may be required to complete synaptic modification involved in memory (Yang et al. 2014). At last, it may happen that there is no concomitance of changes between population spike plasticity and fEPSPs, indicating predominant changes in cell excitability rather than modification in synaptic strength (Heginbotham and Dunwiddie 1991). Hence, the concomitance of LTD reduction at the two recording sites reveals that ethanol disturbs different cellular mechanisms at the same time and the difference related to the location of recordings probably reflects differences in the cellular mechanisms underlying somatic versus dendritic plasticity. Indeed, changes at somatic level may refer more to changes in excitability of the soma, while alteration of synaptic plasticity reflects changes in synaptic strength (Heginbotham and Dunwiddie 1991). Our results combined with those of Roberto et al. (2002) help to demonstrate that ethanol acts on both types of network properties at once: intrinsic excitability properties and synaptic strength. The present results are also consistent with those demonstrating an abolition of hippocampus LTD following two ethanol binge-like injections performed during neonatal period (Izumi et al. 2005) or in adult rats after chronic ethanol exposure (Thinschmidt et al. 2003). Surprisingly, the present decrease in LTD goes along with an increase of LTP 48 h after ethanol. This is the second time only that such result is reported after ethanol (Silvestre de Ferron et al. 2015). Interestingly, such phenotype of bidirectional plasticity has been also reported in an animal model of multiple sclerosis in which it was associated with neuroinflammation (Nisticò et al. 2013). In addition, we found that the sensitivity of NMDA-fEPSPs to Ro25-6981, a GluN2B antagonist, is increased 48 h after ethanol, an effect we correlated with an increased expression of the subunit (Drissi et al. 2020). We also confirm the shift of the BCM-like curve to the left after ethanol, indicating a greater ability for the network to trigger LTP, while LTD induction becomes more difficult. This is consistent with the idea that a low GluN2A-to-GluN2B ratio decreases the probability to induce LTD (Paoletti et al. 2013; Silvestre de Ferron et al. 2015). Importantly, minocycline pre-treatment restored the BCM-like curve to control, demonstrating that ethanol-induced neuroinflammation participates to the left shift of the curve and that ethanol exposure even as short as two binges induced metaplasticity, which, in turn, is responsible for cognitive deficits.
Neuroinflammation and the effects of two binges
Minocycline pretreatment prevented the two binge induced memory impairment, the alterations in hippocampus plasticity and the higher NMDA-fEPSPs sensitivity to a GluN2B antagonist as well as the BCM-like curve shift. Importantly, prior administration of indomethacin, a non-steroidal anti-inflammatory and of the TLR4 receptor antagonist TAK-242 also prevented the ethanol-induced abolition of LTD. Altogether, three structurally unrelated compounds with distinct pharmacological targets, all with anti-inflammatory properties, prevented the effects of ethanol. Thus, ethanol-induced inflammation and TLR4 activation are very likely to be responsible for cellular and behavioral effects of only two binges although we did not reveal the presence of an early inflammatory state that is during the intoxicating effects of ethanol. Nonetheless, these results have to be considered in the light of those showing that during ethanol intoxication, peripheral inflammation is present in humans 20 min after a single binge drinking session with a blood ethanol level of about 130 mg/dl (Afshar et al. 2015). The herein reported results regarding minocycline are in accordance with those revealing the effectiveness of minocycline in preventing the effects related to ethanol-induced neuroinflammation after a longer exposure (Pascual et al. 2011; Qin and Crews, 2012), ethanol’s rewarding properties (Gajbhiye et al. 2017) or ethanol intake (Agrawal et al. 2011). However, in our study microglial cells did not show morphological changes at the time of LTD blockade, suggesting an absence of microglial reactivity at this time point. TLR4 receptor is expressed on microglia, astrocytes and neurons (Tang et al. 2007; Okun et al. 2011; Li et al. 2015b), and we measured a decrease in CA1 pyramidal neurons TLR4 immunofluorescence that was interestingly, prevented by minocycline. Lack of microglial reactivity and decreased in TLR4 labeling are in contradiction with other studies. TLR4-related signaling pathways (MAPK, NF-ƘB), proinflammatory mediators (COX-2, i-NOS, HMGB1) and mnesic dysfunctions have been revealed at the end of a two-week intermittent ethanol exposure in adolescent mice, and these responses were TLR4-dependent (Montesinos et al. 2016). The discrepancies with these studies may come from higher doses of ethanol tested and a longer exposure inducing an increased TLR4 expression at 24 h that remains until adulthood (Qin and Crews 2012; Vetreno and Crews 2012). Because of the short exposure duration we used and the lower dose of ethanol tested, it is conceivable that ethanol-induced neuroinflammation occurred during the presence of ethanol in the body and did not last for 48 h. In this context, the lack of microglia reactivity 48 h later and the preventing effects of different anti-inflammatory are not surprising. Regarding neuronal TLR4 labeling, we found a decrease 48 h after ethanol which was absent after minocycline pretreatment. This result suggests that ethanol modulates TLR4 as suggested after a longer binge-like ethanol exposure during adolescence (Montesinos et al. 2018). In fact, there is a lack of data regarding the time course of microglia activity after ethanol exposure although a recent study brought new insight on this matter (Peng and Nixon 2021). In other models of induced neuroinflammation, like after mechanical brain damage in the hippocampus, an increased expression of neuronal TLR4 was detected after 4 h, with a peak at 24 h, a visible recovery after 3 days and total recovery at 7 days (Li et al. 2015a). Finally, we hypothesize that our measurements were taken at a time when the immune response was terminated, that is the peak of TLR4 expression occurred early after binge-like intoxication followed by a negative regulation. This hypothesis is supported by the mRNA levels of the different cytokines measured at 48 h. Although we were limited by the use of mRNA analysis only, we did not detect any increase of cytokines that could potentially blocked LTD as we found for IL-1β, suggesting that at 48 h the blockade of LTD is not due to a residual neuroinflammation accompanied with a high level of cytokines. Nonetheless, complementary experiments are necessary to define the kinetic of inflammation in this model of two binges.
Could we suggest a sequence of events after ethanol binge drinking?
Our results refute the hypothesis that the blockade of LTD 48 h after two binges is due to the presence of neuroinflammation with a high level of cytokine at that time point. Thus, it is necessary to find another way to explain the blockade of LTD after only few binge-like exposures. Another key effect of repeated ethanol exposure is the alteration of the epigenome as many studies demonstrated before (Legastelois et al. 2017; Pandey et al. 2017). Indeed, the inhibitory effects of only two binges on memory and LTD were prevented with an HDAC inhibitor (Drissi et al. 2020) and Pascual et al. (2011) showed that chronic ethanol exposure led to cognitive impairments associated with a decrease of histone acetylation in the hippocampus of mice, which were not present in mice lacking the TLR4 receptors. Thereby, a hypothesis is that early and short-lasting neuroinflammation induced by ethanol binge-like episodes triggers TLR4 receptor activation, which in turn leads to epigenetic changes, a blockage of synaptic LTD, inducing learning and memory deficits. However, the functional relationship between ethanol-induced epigenetic modifications and plasticity disturbances in our model needs to be further investigated to determine whether all effects of ethanol are related to the unique modulation of GluN2B subunit expression as we previously suggested (Drissi et al. 2020).
To conclude, there is a therapeutic potential of anti-inflammatory to prevent the long-term consequences of drug abuse in adolescence (Guerri and Pascual 2019), notably on ethanol intake (Agrawal et al. 2011), withdrawal-induced anxiety and relapse (Gajbhiye et al. 2018). In a similar vein, early TLR4 inhibition reduces hippocampal injury at puberty in a rat model of neonatal hypoxic-ischemic brain damage (Tang et al. 2019), demonstrating a major role of TLR4 in the downstream neuroinflammatory events related to brain injury. Here, we showed that anti-inflammatory drugs administered at the same time that ethanol binge-like episodes prevent the effects of ethanol on learning and memory. Therefore, anti-inflammatory treatment appears to be good candidate for preventing most of the short- and long-term effects of alcohol on the brain during adolescence.
References
Afshar M, Richards S, Mann D et al (2015) Acute immunomodulatory effects of binge alcohol ingestion. Alcohol 49:57–64. https://doi.org/10.1016/j.alcohol.2014.10.002
Agrawal RG, Hewetson A, George CM et al (2011) Minocycline reduces ethanol drinking. Brain Behav Immun 25:S165–S169. https://doi.org/10.1016/j.bbi.2011.03.002
Alaux-Cantin S, Warnault V, Legastelois R et al (2013) Alcohol intoxications during adolescence increase motivation for alcohol in adult rats and induce neuroadaptations in the nucleus accumbens. Neuropharmacology 67:521–531. https://doi.org/10.1016/j.neuropharm.2012.12.007
Beresford TP, Arciniegas DB, Alfers J et al (2006) Hippocampus Volume Loss Due to Chronic Heavy Drinking. Alcohol: Clin Exp Res 30:1866–1870. https://doi.org/10.1111/j.1530-0277.2006.00223.x
Bertani I, Iori V, Trusel M et al (2017) Inhibition of IL-1β Signaling Normalizes NMDA-Dependent Neurotransmission and Reduces Seizure Susceptibility in a Mouse Model of Creutzfeldt-Jakob Disease. J Neurosci 37:10278–10289. https://doi.org/10.1523/JNEUROSCI.1301-17.2017
Carbia C, Cadaveira F, Caamaño-Isorna F et al (2017) Binge drinking during adolescence and young adulthood is associated with deficits in verbal episodic memory. PLoS ONE 12:e0171393. https://doi.org/10.1371/journal.pone.0171393
Courtney KE, Polich J (2009) Binge drinking in young adults: Data, definitions, and determinants. Psychol Bull 135:142–156. https://doi.org/10.1037/a0014414
Crews FT, Qin L, Sheedy D et al (2013) High mobility group box 1/Toll-like receptor danger signaling increases brain neuroimmune activation in alcohol dependence. Biol Psychiatry 73:602–612. https://doi.org/10.1016/j.biopsych.2012.09.030
Drissi I, Deschamps C, Fouquet G et al (2020) Memory and plasticity impairment after binge drinking in adolescent rat hippocampus: GluN2A/GluN2B NMDA receptor subunits imbalance through HDAC2. Addict Biol 25:e12760. https://doi.org/10.1111/adb.12760
Flood L, Korol SV, Ekselius L et al (2019) Interferon-γ potentiates GABAA receptor-mediated inhibitory currents in rat hippocampal CA1 pyramidal neurons. J Neuroimmunol 337:577050. https://doi.org/10.1016/j.jneuroim.2019.577050
Gajbhiye SV, Tripathi RK, Salve B et al (2017) Evaluation of effect of minocycline on rewarding potential and alcohol relapse in place preference model in mice. Neurosci Lett 649:28–33. https://doi.org/10.1016/j.neulet.2017.04.007
Gajbhiye SV, Tripathi RK, Petare A et al (2018) Minocycline in Alcohol Withdrawal Induced Anxiety and Alcohol Relapse in Rats. Curr Clin Pharmacol 13:65–72. https://doi.org/10.2174/1574884713666180228110310
Ge Y, Dong Z, Bagot RC et al (2010) Hippocampal long-term depression is required for the consolidation of spatial memory. Proc Natl Acad Sci USA 107:16697–16702. https://doi.org/10.1073/pnas.1008200107
Gierski F, Stefaniak N, Benzerouk F et al (2020) Component process analysis of verbal memory in a sample of students with a binge drinking pattern. Addict Behav Rep 12:100323. https://doi.org/10.1016/j.abrep.2020.100323
Gogtay N, Giedd JN, Lusk L et al (2004) Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci U S A 101:8174–8179. https://doi.org/10.1073/pnas.0402680101
Guerri C, Pascual M (2019) Impact of neuroimmune activation induced by alcohol or drug abuse on adolescent brain development. Int J Dev Neurosci 77:89–98. https://doi.org/10.1016/j.ijdevneu.2018.11.006
Haber M, James J, Kim J et al (2018) Minocycline plus N-acteylcysteine induces remyelination, synergistically protects oligodendrocytes and modifies neuroinflammation in a rat model of mild traumatic brain injury. J Cereb Blood Flow Metab 38:1312–1326. https://doi.org/10.1177/0271678X17718106
Heginbotham LR, Dunwiddie TV (1991) Long-term increases in the evoked population spike in the CA1 region of rat hippocampus induced by beta-adrenergic receptor activation. J Neurosci 11:2519–2527
Hoshino K, Hasegawa K, Kamiya H, Morimoto Y (2017) Synapse-specific effects of IL-1β on long-term potentiation in the mouse hippocampus. Biomed Res 38:183–188. https://doi.org/10.2220/biomedres.38.183
Hwang J-W, Jeon Y-T, Lim Y-J, Park H-P (2017) Sevoflurane postconditioning-induced anti-inflammation via inhibition of the toll-like receptor-4/nuclear factor kappa B pathway contributes to neuroprotection against transient global cerebral ischemia in rats. Int J Mol Sci 18. https://doi.org/10.3390/ijms18112347
Ikegaya Y, Delcroix I, Iwakura Y et al (2003) Interleukin-1beta abrogates long-term depression of hippocampal CA1 synaptic transmission. Synapse 47:54–57. https://doi.org/10.1002/syn.10154
Izumi Y, Kitabayashi R, Funatsu M et al (2005) A single day of ethanol exposure during development has persistent effects on bi-directional plasticity, N-methyl-D-aspartate receptor function and ethanol sensitivity. Neuroscience 136:269–279. https://doi.org/10.1016/j.neuroscience.2005.07.015
Legastelois R, Jeanblanc J, Vilpoux C et al (2017) Epigenetic mechanisms and alcohol use disorders: a potential therapeutic target. Biol Aujourdhui 211:83–91. https://doi.org/10.1051/jbio/2017014
Li Y, Korgaonkar A, Swietek B et al (2015) Toll-like receptor 4 enhancement of non-NMDA synaptic currents increases dentate excitability after brain injury Ying. Neurobiol Dis 74:240–253. https://doi.org/10.1038/jid.2014.371
Li Y, Korgaonkar AA, Swietek B et al (2015) Toll-like receptor 4 enhancement of non-NMDA synaptic currents increases dentate excitability after brain injury. Neurobiol Dis 74:240–253. https://doi.org/10.1016/j.nbd.2014.11.021
Liu X, Gu Q-H, Duan K, Li Z (2014) NMDA receptor-dependent LTD is required for consolidation but not acquisition of fear memory. J Neurosci 34:8741–8748. https://doi.org/10.1523/JNEUROSCI.2752-13.2014
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25(4):402–408. https://doi.org/10.1006/meth.2001.1262
Lu Y, Giri PK, Lei S et al (2017) Pretreatment with minocycline restores neurogenesis in the subventricular zone and subgranular zone of the hippocampus after ketamine exposure in neonatal rats. Neuroscience 352:144–154. https://doi.org/10.1016/j.neuroscience.2017.03.057
Maggio N, Vlachos A (2018) Tumor necrosis factor (TNF) modulates synaptic plasticity in a concentration-dependent manner through intracellular calcium stores. J Mol Med (berl) 96:1039–1047. https://doi.org/10.1007/s00109-018-1674-1
Maurage P, Lannoy S, Mange J et al (2020) What We Talk About When We Talk About Binge Drinking: Towards an Integrated Conceptualization and Evaluation. Alcohol Alcohol 55:468–479. https://doi.org/10.1093/alcalc/agaa041
Montesinos J, Pascual M, Rodríguez-Arias M, Miñarro J, Guerri C (2016) Involvement of TLR4 in the long-term epigenetic changes, rewarding and anxiety effects induced by intermittent ethanol treatment in adolescence. Brain Behav Immun 53:159–171. https://doi.org/10.1016/j.bbi.2015.12.006
Montesinos J, Pascual M, Millán-Esteban D, Guerri C (2018) Binge-like ethanol treatment in adolescence impairs autophagy and hinders synaptic maturation: Role of TLR4. Neurosci Lett 682:85–91. https://doi.org/10.1016/j.neulet.2018.05.049
Moser EI (1995) Learning-related changes in hippocampal field potentials. Behav Brain Res 71:11–18. https://doi.org/10.1016/0166-4328(95)00051-8
Muñoz MD, Antolín-Vallespín M, Tapia-González S, Sánchez-Capelo A (2016) Smad3 deficiency inhibits dentate gyrus LTP by enhancing GABAA neurotransmission. J Neurochem 137:190–199. https://doi.org/10.1111/jnc.13558
Nagel BJ, Schweinsburg AD, Phan V, Tapert SF (2005) Reduced hippocampal volume among adolescents with alcohol use disorders without psychiatric comorbidity. Psychiatry Res 139:181–190. https://doi.org/10.1016/j.pscychresns.2005.05.008
Nisticò R, Mango D, Mandolesi G et al (2013) Inflammation subverts hippocampal synaptic plasticity in experimental multiple sclerosis. PLoS ONE 8:e54666. https://doi.org/10.1371/journal.pone.0054666
Okun E, Griffioen KJ, Mattson MP (2011) Toll-like receptor signaling in neural plasticity and disease. Trends Neurosci 34:269–281. https://doi.org/10.1016/j.tins.2011.02.005
Oliveira AC, Pereira MC, da Santana LN, S, et al (2015) Chronic ethanol exposure during adolescence through early adulthood in female rats induces emotional and memory deficits associated with morphological and molecular alterations in hippocampus. J Psychopharmacol 29:712–724. https://doi.org/10.1177/0269881115581960
Pandey SC, Kyzar EJ, Zhang H (2017) Epigenetic Basis of the Dark Side of Alcohol Addiction. Neuropharmacology 122:74–84. https://doi.org/10.1016/j.neuropharm.2017.02.002
Paoletti P, Bellone C, Zhou Q (2013) NMDA receptor subunit diversity: impact on receptor properties, synaptic plasticity and disease. Nat Rev Neurosci 14:383–400. https://doi.org/10.1038/nrn3504
Pascual M, Blanco AM, Cauli O et al (2007) Intermittent ethanol exposure induces inflammatory brain damage and causes long-term behavioural alterations in adolescent rats. Eur J Neurosci 25:541–550. https://doi.org/10.1111/j.1460-9568.2006.05298.x
Pascual M, Baliño P, Alfonso-Loeches S et al (2011) Impact of TLR4 on behavioral and cognitive dysfunctions associated with alcohol-induced neuroinflammatory damage. Brain Behav Immun 25(Suppl 1):S80-91. https://doi.org/10.1016/j.bbi.2011.02.012
Pascual M, Montesinos J, Guerri C (2018) Role of the innate immune system in the neuropathological consequences induced by adolescent binge drinking. J Neurosci Res 96:765–780. https://doi.org/10.1002/jnr.24203
Peng H, Nixon K (2021) Microglia Phenotypes Following the Induction of Alcohol Dependence in Adolescent Rats. Alcohol Clin Exp Res 45:105–116. https://doi.org/10.1111/acer.14504
Qin L, Crews FT (2012) Chronic ethanol increases systemic TLR3 agonist-induced neuroinflammation and neurodegeneration. J Neuroinflammation 9:130. https://doi.org/10.1186/1742-2094-9-130
Rabiant K, Antol J, Naassila M, Pierrefiche O (2021) Sex difference in the vulnerability to hippocampus plasticity impairment after binge-like ethanol exposure in adolescent rat: Is estrogen the key? Addict Biol 26:e13002. https://doi.org/10.1111/adb.13002
Risher M-L, Fleming RL, Risher C et al (2015) Adolescent Intermittent Alcohol Exposure: Persistence of Structural and Functional Hippocampal Abnormalities into Adulthood. Alcohol Clin Exp Res 39:989–997. https://doi.org/10.1111/acer.12725
Roberto M, Nelson TE, Ur CL, Gruol DL (2002) Long-term potentiation in the rat hippocampus is reversibly depressed by chronic intermittent ethanol exposure. J Neurophysiol 87:2385–2397. https://doi.org/10.1152/jn.2002.87.5.2385
Rolland B, Naassila M (2017) Binge Drinking: Current Diagnostic and Therapeutic Issues. CNS Drugs 31:181–186. https://doi.org/10.1007/s40263-017-0413-4
Schneider M (2013) Adolescence as a vulnerable period to alter rodent behavior. Cell Tissue Res 354:99–106. https://doi.org/10.1007/s00441-013-1581-2
Silvestre de Ferron B, Bennouar KE, Kervern M, Alaux-Cantin S, Robert A, Rabiant K, Antol J, Naassila M, Pierrefiche O (2015) Two binges of ethanol a day keep the memory away in adolescent rats: key role for GLUN2B subunit. Int J Neuropsychopharmacol 19(1):pyv087. https://doi.org/10.1093/ijnp/pyv087
Smith KW, Gierski F, Andre J et al (2017) Altered white matter integrity in whole brain and segments of corpus callosum, in young social drinkers with binge drinking pattern. Addict Biol 22:490–501. https://doi.org/10.1111/adb.12332
Spear LP (2018) Effects of adolescent alcohol consumption on the brain and behaviour. Nat Rev Neurosci 19:197–214. https://doi.org/10.1038/nrn.2018.10
Swartzwelder HS, Hogan A, Risher M-L et al (2014) Effect of sub-chronic intermittent ethanol exposure on spatial learning and ethanol sensitivity in adolescent and adult rats. Alcohol 48:353–360. https://doi.org/10.1016/j.alcohol.2014.02.003
Tang S-C, Arumugam TV, Xu X et al (2007) Pivotal role for neuronal Toll-like receptors in ischemic brain injury and functional deficits. Proc Natl Acad Sci U S A 104:13798–13803. https://doi.org/10.1073/pnas.0702553104
Tang Z, Cheng S, Sun Y et al (2019) Early TLR4 inhibition reduces hippocampal injury at puberty in a rat model of neonatal hypoxic-ischemic brain damage via regulation of neuroimmunity and synaptic plasticity. Exp Neurol 321:113039. https://doi.org/10.1016/j.expneurol.2019.113039
Tang X-H, Zhang G-F, Xu N et al (2020) Extrasynaptic CaMKIIα is involved in the antidepressant effects of ketamine by downregulating GluN2B receptors in an LPS-induced depression model. J Neuroinflammation 17:181. https://doi.org/10.1186/s12974-020-01843-z
Tavolacci M-P, Berthon Q, Cerasuolo D et al (2019) Does binge drinking between the age of 18 and 25 years predict alcohol dependence in adulthood? A retrospective case-control study in France. BMJ Open 9:e026375. https://doi.org/10.1136/bmjopen-2018-026375
Thinschmidt JS, Walker DW, King MA (2003) Chronic ethanol treatment reduces the magnitude of hippocampal LTD in the adult rat. Synapse 48:189–197. https://doi.org/10.1002/syn.10203
Vetreno RP, Crews FT (2012) Adolescent binge drinking increases expression of the danger signal receptor agonist HMGB1 and Toll-like receptors in the adult prefrontal cortex. Neuroscience 226:475–488. https://doi.org/10.1016/j.neuroscience.2012.08.046
Vetreno RP, Crews FT (2015) Binge ethanol exposure during adolescence leads to a persistent loss of neurogenesis in the dorsal and ventral hippocampus that is associated with impaired adult cognitive functioning. Front Neurosci 9:35. https://doi.org/10.3389/fnins.2015.00035
Vetreno RP, Lawrimore CJ, Rowsey PJ, Crews FT (2018) Persistent Adult Neuroimmune Activation and Loss of Hippocampal Neurogenesis Following Adolescent Ethanol Exposure: Blockade by Exercise and the Anti-inflammatory Drug Indomethacin. Front Neurosci 12:200. https://doi.org/10.3389/fnins.2018.00200
Wang N, Mi X, Gao B et al (2015) Minocycline inhibits brain inflammation and attenuates spontaneous recurrent seizures following pilocarpine-induced status epilepticus. Neuroscience 287:144–156. https://doi.org/10.1016/j.neuroscience.2014.12.021
Wittner L, Maglóczky Z (2017) Synaptic Reorganization of the Perisomatic Inhibitory Network in Hippocampi of Temporal Lobe Epileptic Patients. Biomed Res Int 2017:7154295. https://doi.org/10.1155/2017/7154295
Yang Y-S, Kim K-D, Eun S-Y, Jung S-C (2014) Roles of somatic A-type K(+) channels in the synaptic plasticity of hippocampal neurons. Neurosci Bull 30:505–514. https://doi.org/10.1007/s12264-013-1399-7
Zeng H, Chattarji S, Barbarosie M et al (2001) Forebrain-specific calcineurin knockout selectively impairs bidirectional synaptic plasticity and working/episodic-like memory. Cell 107:617–629. https://doi.org/10.1016/s0092-8674(01)00585-2
Acknowledgements
CD and CM are PhD students supported by the Région Hauts-de-France, University of Picardy Jules Verne and the Ministry of French Research and Education. GF is supported by ERA-NET program: Psi-Alc (FKZ: 01EW1908)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
“The authors declare no conflict of interest”.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Deschamps, C., Uyttersprot, F., Debris, M. et al. Anti-inflammatory drugs prevent memory and hippocampal plasticity deficits following initial binge-like alcohol exposure in adolescent male rats. Psychopharmacology 239, 2245–2262 (2022). https://doi.org/10.1007/s00213-022-06112-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-022-06112-w