Abstract
Rationale
Alcohol-use disorder (AUD) is associated with the propensity to choose smaller sooner options on the delay discounting task. It is unclear, however, how inherent risk underlies delay discounting behavior. As impulsive choice is a hallmark feature in AUD, it is important to understand the neural response to reward and delay while accounting for risk in impulsive decision-making.
Objective
This study examined activation associated with delay and reward magnitude, while controlling for risk in a probabilistic delay discounting task in AUD and examined if differences in activation were associated with treatment outcomes.
Methods
Thirty-nine recently abstinent alcohol-dependent volunteers and 46 controls completed a probabilistic delay discounting task paired with functional magnetic resonance imaging. Alcohol use was collected using a self-report journal for 3 months following baseline scan.
Results
During delay stimulus presentations, Controls exhibited greater activation compared to the Alcohol group notably in the anterior insula, middle/dorsal anterior cingulate cortex (ACC), dorsolateral prefrontal cortex (PFC), and inferior parietal lobule. For magnitude, the Alcohol group exhibited greater activation than Controls primarily in medial PFC, rostral ACC, left posterior parietal cortex, and right precuneus. Within the Alcohol group, alcohol craving severity negatively correlated with right lateral PFC activation during reward magnitude in individuals who completed the 3-month study without relapse, while non-completers showed the opposite relationship.
Conclusions
The results of this study extend previous findings that alcohol use disorder is associated with differences in activation during an immediate or delayed choice by delineating activation associated with the parameters of impulsive choice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the availability of pharmacological and psychosocial treatments for alcohol use disorder (AUD), it is still considered a chronically relapsing disorder. Impulsive choice is a significant risk factor for treatment failure (de Wit 2009; Stevens et al. 2015) and is a hallmark feature in AUD (Bjork et al. 2004; Petry 2001). Individuals with AUD (Bjork et al. 2004; Bobova et al. 2009; Mitchell et al. 2005; Petry 2001) and other substance-use disorders (MacKillop et al. 2011; Mitchell and Wilson 2012) consistently exhibit greater propensity for impulsive choices indexed by steeper discounting patterns (i.e., preference for smaller, immediate over larger, delayed rewards) compared to controls. From a clinical perspective, steeper devaluation of delayed rewards in AUD parallels the continued use of alcohol for its immediate rewarding properties, despite negative future consequences (e.g., poor health outcomes and financial hardships). These behavioral differences are accompanied by altered brain function during the performance of delay discounting tasks, where alcohol-dependent individuals show greater activation in limbic regions during impulsive choices (i.e., choosing smaller, sooner rewards) and greater cortical activation during delayed choices (Amlung et al. 2014; Boettiger et al. 2007) when compared to controls. These studies begin to detail differences in neural systems underlying delay discounting in AUD; however, most studies examine brain activation associated with an immediate or delayed choice and less is known about the mechanisms underlying the evaluation of reward magnitude and delay associated with impulsive decision-making. As decision outcome is influenced by the dynamic interaction of reward magnitude and delay (Ballard and Knutson 2009), it is critically important to identify activation that is differentially associated with each decision characteristic to better understand impulsive choice in AUD.
In addition, although evidence suggests that the delivery of any future reward is intrinsically paired with risk to some degree (Patak and Reynolds 2007), delay discounting tasks do not account for this inherent subjective risk. To model risk related to obtaining a reward, probability discounting tasks were developed, which present choices between smaller, certain rewards and larger, less certain rewards. Probability discounting tasks, however, do not test delay. To test the effect of risk on delay discounting behavior, probability discounting rates have been incorporated into delay discounting models (Lopez-Guzman et al. 2018). Compared to paradigms assuming risk neutrality, delay discounting models that account for subjective risk preferences have shown to improve model fit (Lopez-Guzman et al. 2018). Furthermore, as risk and delay discounting seem to be somewhat dependent, not including risk preferences may bias discounting rates, particularly in more risk-seeking individuals (Lopez-Guzman et al. 2018). This may result in the delay discounting differences consistently observed between substance users and controls to be inflated. Therefore, controlling for uncertainty is critical for better characterizing brain function associated with delay processing. Although independent risk preferences have shown to have significant impact on delay discounting rates, no studies have investigated delay and probability discounting simultaneously in AUD.
To account for inherent subjective risk during delay discounting, this study used a probabilistic delay discounting (PDD) task, which assigns an explicit probability of receiving a delayed reward. Reward magnitude and delay have shown to activate different brain regions during a delay discounting task in healthy controls; such that, increases in activation of nucleus accumbens, medial prefrontal cortex (mPFC), and posterior cingulate cortex correlate with increasing future reward magnitudes, while decreases in activation of lateral cortical regions (e.g., dorsolateral prefrontal cortex [DLPFC], posterior parietal cortex) correlated with increasing delays (Ballard and Knutson 2009). Expanding on the Ballard and Knutson (2009) results, we examined baseline differences in the neural response to delay and reward magnitude while controlling for risk between Alcohol and Control groups and between individuals with AUD who either remained abstinent or had only lapses through the duration of the 3-month follow-up study (“Completers”) and those who either relapsed or dropped out during the study (“Non-Completers”).
There are several prominent and conflicting theories of addiction. Although the reward deficiency syndrome model postulates that chronic alcohol and substance use diminishes the response for natural, or non-drug (i.e., monetary), rewards (Blum et al. 2000), we still hypothesized that the Alcohol compared to the Control group would exhibit greater activation in reward salience regions during reward magnitude stimulus presentations and less activation in cognitive control regions during delay stimulus presentations. Our expectations are based on the impulsivity theory of addiction, which argues that individuals with an addiction show a strong response to rewards (Bjork et al. 2012). In addition, the response to rewards in addiction is context dependent, where striatal reactivity to reward is heightened for reward outcome and attenuated for reward anticipation (Luijten et al. 2017). A meta-analysis of reward reactivity, however, shows that individuals with addictive disorders exhibit greater prefrontal cortical regions of activation compared to controls during both reward outcome and reward anticipation, while the control group exhibits greater activation in parietal, temporal, and cingulate cortices (Luijten et al. 2017).
In early abstinence, the presence of negative emotional states, including depression and impulsivity, contributes to relapse due to a desire to alleviate these negative emotional states (i.e., negative reinforcement) (Koob and Le Moal 2001); therefore, it was expected that Non-Completers would exhibit greater impulsivity compared to Completers. In addition, because higher treatment drop-out rate is highly correlated with craving severity during alcohol withdrawal (O’Connor et al. 1991), this study also aimed to identify how craving interacts with brain function during probabilistic delay discounting to influence treatment outcome during the early stages of recovery. Previous neuroimaging studies have largely examined craving in the context of cue-induced craving (Braus et al. 2001; Grusser et al. 2004) and found that both cognitive and affective processes are activated during these tasks (Kober et al. 2010); however, it is unclear how craving may interact with neural responses to reward and delay during decision-making to promote abstinence. As cognitive control is required to overcome craving and maintain sobriety, we hypothesized that greater activation in brain regions responsible for cognitive control (i.e., DLPFC) during reward magnitude and delay stimulus presentations would correlate with decreased alcohol craving intensity in study Completers compared to Non-Completers.
Materials and methods
Participants and procedure
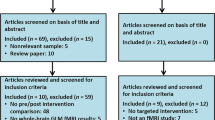
Thirty-nine volunteers meeting DSM-IV criteria for alcohol dependence were recruited from the Veterans Affairs Portland Heath Care System (VAPORHCS) and community substance abuse treatment programs, and 46 control subjects were recruited from the VAPORHCS and online advertisements. All participants in the Alcohol group were enrolled in a substance abuse treatment program at the time of consent. All participants gave written informed consent, as approved by the VAPORHCS and Oregon Health & Science University (OHSU) Institutional Review Boards. Participants were excluded based on medical history and laboratory blood tests indicating any current or past medical illness that might affect cognition (e.g., stroke, head injury, HIV, hepatitis B or C, anemia), use of antipsychotics, benzodiazepines, antiparkinsonian medications, or anticholinergics, head trauma with loss of consciousness, and magnetic resonance imaging (MRI) contraindications. In addition, past or current Axis I diagnoses, other than depression, post-traumatic stress disorder, nicotine dependence, and alcohol dependence (for the Alcohol group only) were exclusionary. Participants were between 21 and 55 years old and alcohol and drug free (except for nicotine or caffeine), verified with a negative urine drug screen. The Alcohol group self-reported abstinence for 1 to 4 weeks at the time of consent (visit 1).
Participants received a $50 gift card to a local retail chain after completing visit 1 (consent and screening) and another for completing visit 2 (scan). Following the scan, only subjects in the Alcohol group returned for three monthly follow-up visits and were compensated with $20 gift cards for each visit. Subjects in the Alcohol group were asked to report any alcohol or drug use between visits, including frequency and amount, in a weekly drinking diary that was reviewed at each monthly follow-up visit, along with medical records and information from the subject’s treatment provider. Within the Alcohol group, Completers (n = 16) included participants who completed the 3-month follow-up study without relapse (n = 13) or with only lapses (n = 3), and Non-Completers (n = 23) were those who either dropped out of the study (n = 16) or relapsed (n = 7). An episode of relapse was defined as one or more days of heavy drinking [more than five drinks per day] or three or more consecutive days of any drinking following at least 4 days of sobriety (Maisto et al. 2003). Alcohol use that did not meet these criteria was deemed a lapse.
Probabilistic delay discounting task
The PDD is an economic choice task, where subjects choose between a guaranteed immediate reward and an alternative reward that varies in magnitude, risk, and delay to receipt. The subjective value of the alternative (delayed and probabilistic) reward is given by
where Vp is the subjective value of a discounted reward of magnitude, M, d is the delay in days until the reward is received, θ is the odds against ratio, θ = (1 − p)/p, where p is the probability of receiving the reward, and k and h are fitting parameters that characterize the degree of delay and probability discounting, respectively (Ho et al. 1999; Vanderveldt et al. 2015). Larger values of k indicate greater delay discounting, and larger values of h indicate greater aversion to risky choices. Specifically, subjects were asked to choose between $20 available immediately with 100% certainty (not shown on the screen) or an option with varying levels of reward magnitude ($20, $60, $100, or $140), delay of receiving the reward (0, 4, 8, or 12 months), and probability of receiving the reward (25%, 33%, 50%, or 100%) (Fig. 1). For each choice trial, the presentation of magnitude, probability, and delay stimuli were presented every 2.5 s in random order. Once a stimulus appeared on the screen, it remained on the screen until all three stimuli were visible. The three stimuli remained on the screen for 2.5 s before being replaced with a “+” symbol. Subjects had 4 s to push either the left button ($20 now) or the right button (alternative reward) immediately following the presentation of the third stimulus followed by a 1–4 s jitter during which the “+” symbol remained on the screen until the next choice pair was presented (Fig. 1). In addition to the inter-trial jitter, magnitude, probability, and delay stimuli were presented in random order to avoid possible confounds of presentation order. For example, within a choice trial, magnitude may be presented first, second, or third in relation to probability and delay. Each subject performed the same practice PDD task in the laboratory before performing it in the scanner.
The fully crossed factorial design included 4 × 4 × 4 = 64 distinct permutations for each run of the PDD. Subjects performed two 20-min runs during their MRI session. Across the two runs, each permutation was presented twice, for a total of 128 trials. All subjects were offered the same set of questions, presented in random order. After each choice, the subject received visual notification of the outcome on the screen, such that an immediate choice produced “You will receive $20 now” and missed trials produced “You missed the last question.” Choice of the delayed reward produced one of two outcomes depending on the probability of receiving the reward. For example, if a subject chose a 25% chance of receiving $140 in 12 months, they would either see “You will receive $140 in 12 months” or “You receive nothing.” Subjects were paid the amount of one choice selected at random (between $0 and 140) at the time specified during that trial (day of scan up to 1 year following the scan). Prior to task performance, subjects were informed that in the case of a deferred payment, an appointment would be made to come back to the lab and it was their responsibility to follow-through with the appointment. Values of k and h were determined by a softmax procedure, which uses an optimized maximum-likelihood estimation procedure (fminsearch, MATLAB and Statistics Toolbox Release 2013b, The MathWorks, Inc., Natick, Massachusetts) that identifies the surface that best separates choices of the immediate reward ($20) from the alternative reward (Fig. 1) (Miedl et al. 2012). Normalized values of k and h, calculated by taking the natural log, were used to index delay and probability discounting, respectively.
Craving severity measurement
Craving intensity was assessed on a scale of 0–100 with a visual analog scale (VAS) in the Alcohol group. Participants were asked “How intense are your alcohol cravings today?” and instructed to indicate the intensity of their cravings by placing a vertical mark and a corresponding number on a line between 0 (“no cravings”) and 100 (“the most intense cravings imaginable”).
Magnetic resonance imaging acquisition and analysis
Imaging data was acquired on a 3 Tesla (T) Siemens TIM Trio MRI scanner. A localizer scan was acquired in order to guide slice alignment during anatomical and functional scans. Two T2*-weighted echo-planar imaging (EPI) functional runs were acquired (24 slices, 4 mm thick, gap width = 1 mm, TR/TE/α = 2000 ms/38 ms/80°, matrix = 128 × 128, FOV = 240 mm2, 615 volumes per run, in-plane pixel size of 1.875 mm2), while subjects performed the PDD. One high-resolution T1-weighted anatomical magnetically prepared rapid acquisition gradient echo (MPRAGE; 144 slices, 1 mm thick, TR/TE/TI/α = 2300 ms/3.4 ms/1200 ms/12°, FOV = 224 mm × 256 mm) was acquired for co-registration with functional images and statistical overlay.
Functional MRI (fMRI) data processing was carried out using FEAT (FMRI Expert Analysis Tool) version 6.00, part of FSL (FMRIB’s Software Library, www.fmrib.ox.ac.uk/fsl). The following pre-processing steps were applied to each EPI: motion correction using MCFLIRT; slice-timing correction using Fourier-space time-series phase-shifting; skull-stripped using BET; spatial smoothing using a Gaussian kernel of FWHM 5-mm; grand-mean intensity normalization of the entire 4D dataset by a single multiplicative factor; and high-pass temporal filtering (Gaussian-weighted least-squares straight line fitting, with sigma = 50.0 s). EPI images were registered to the MPRAGE using FLIRT (FMRIB’s Linear Image Registration Tool) then to the standard Montreal Neurological Institute (MNI) space using 12-parameter affine transformation.
The analysis examined activation during the presentation of magnitude and delay stimuli, while controlling for risk, irrelevant of choice. The general linear model (GLM) included seven regressors; three regressors for magnitude, delay, and probability events during choice trials; three regressors for magnitude, delay, and probability events during control trials; and one regressor to account for data for missed trials. Control trials were defined as trials where a magnitude of $20 was presented as the first stimulus since regardless of the subsequent risk and delay, the immediate option will always be more certain and/or sooner, as it offers $20 now with no risk. Onset times of magnitude, delay, and probability cues within choice and control trials were modeled separately and were used as contrasts. Contrasts of interest included magnitude and delay conditions contrasted with their cue-specific control condition. Regressors were created by convolving a set of delta functions, representing onset times of each event, with a canonical (double-gamma) hemodynamic response function. The first temporal derivatives were included in the model to capture variance associated with the temporal lag of the hemodynamic response along with six motion parameters estimated during motion correction.
Group-level analyses were carried out using FLAME (FMRIB’s Local Analysis of Mixed Effects) with automatic outlier detection. Z statistic images were thresholded non-parametrically using clusters determined by Z > 3.1 and a (corrected) cluster significance threshold of p = 0.05. Preprocessed EPIs were combined across runs using FEAT. Completers and Non-Completers were combined to form the Alcohol group and were compared to Controls in whole-brain voxel-wise analyses. Similarly, within the Alcohol group, separate analyses were conducted to compare Completers to Non-Completers. As there were significant differences in age, years of education, and cigarettes per day, between the Alcohol and Control groups, these variables were modeled as nuisance covariates in the between-group analyses.
Statistical analysis of behavioral and demographic data
Independent samples t tests with equal variance assumed and chi-square tests were used to analyze behavioral data with SPSS version 24 (SPSS Inc., Chicago, IL).
Analysis of the relationship between activation and craving
Craving was added to the GLM as an independent variable in a separate whole-brain voxel-wise analysis conducted within the Alcohol group to examine the interaction between craving and treatment outcome on activation during reward magnitude and delay presentations. Whole-brain fMRI statistics were corrected for multiple comparisons by using cluster-correction with voxel height threshold of Z > 3.1 and cluster significance of p < 0.05.
Results
Demographics and behavioral measures (Table 1)
The Control group included 46 subjects, none of whom reported any heavy or daily use of alcohol or any other drug use. The Alcohol group included 39 alcohol-dependent subjects who were abstinent from alcohol at the time of the scan (range 6–55 days abstinent before scan). There were no significant differences between Completers and Non-Completers in age (t(37) = − 0.413, p = 0.682), sex (χ2 = 2.457), years of education (t(37) = − 0.407, p = 0.687), years of alcohol-use (t(37) = − 0.308, p = 0.760), standard drinks per day (t(37) = 0.509, p = 0.613), days abstinent on scan day (t(36) = 0.875, p = 0.387), delay discounting (t(37) = − 0.346, p = 0.731), probability discounting (t(37) = − 0.813, p = 0.421), craving intensity (t(37) = − 0.723, p = 0.474), or in the frequency of cigarette use (t(37) = − 1.219, p = 0.230), but significant differences between the Control group and the Alcohol group (Completers and Non-Completers combined) were seen in age (t(83) = − 2.820, p = 0.006), years of education (t(83) = 2.142, p = 0.035), cigarettes per day (t(83) = − 2.686, p = 0.009), and delay discounting (t(83) = − 2.026, p = 0.046) (Table 1). The groups differed on rates of both major depressive disorder (MDD) (χ2 = 0.002) and post-traumatic stress disorder (PTSD) (χ2 = 0.005). The Alcohol group included eight subjects with current MDD, two subjects with PTSD, and four subjects with comorbid MDD/PTSD diagnoses, while the Control group included only one subject with MDD.
Controls vs alcohol group
Group differences during magnitude presentation show that the Alcohol group exhibited greater activation in the calcarine, lingual, fusiform, and occipital gyri, cuneus, precuneus, superior medial gyrus (SMG), rostral anterior cingulate cortex (rACC), right superior temporal, angular, and supramarginal gyri, and right pre and postcentral gyrus, while the Control group showed no significant regions of greater activation (Table 2). Within group analyses show that the Alcohol and Control groups both exhibited significant activation in the occipital, fusiform, and lingual gyri, ACC, middle cingulate cortex (MCC), supplementary motor area (SMA), superior parietal lobule (SPL), precentral gyrus, left postcentral gyrus, middle frontal gyrus (MFG), SMG, insula, thalamus, and the right inferior frontal gyrus (IFG; Fig. 2a, Tables 3 and 4). In addition, the Control group exhibited significant activation in the left IFG, caudate, inferior parietal lobule (IPL), precuneus, posterior cingulate cortex, and right superior frontal gyrus (SFG; Table 4).
Group differences in activation elicited by magnitude and delay during the PDD. a Magnitude-elicited activation was similar across Control and Alcohol groups; however, the Control group showed additional and more prominent regions of activation. Group comparisons showed that the Alcohol group exhibited greater activation than Controls in the calcarine, lingual, fusiform, and occipital gyri, cuneus, precuneus, superior medial gyrus, rostral ACC (rACC), right superior temporal, angular, and supramarginal gyri, and right pre and postcentral gyrus, while the Control Group showed no significant regions of greater activation. b Delay-elicited activation was significant in multiple regions in the Control group, while the Alcohol group showed no regions of significant activation. Group comparisons showed that the Control group exhibited greater activation than the Alcohol group in the occipital lobe, insula, putamen, left thalamus, inferior frontal gyrus, superior medial gyrus, supplementary motor area, right middle frontal gyrus, anterior and middle cingulate cortices, right superior and inferior parietal lobule, right supramarginal gyrus, and pre- and postcentral gyri, while the Alcohol group showed no significant regions of greater activation
During delay presentation, significant group differences show that the Control compared to the Alcohol group exhibited greater activation in the calcerine, lingual, fusiform and occipital gyri, anterior insula, putamen, SMA, SMG, MCC, dorsal ACC (dACC), right MFG, right SPL and IPL, IFG, left thalamus, right supramarginal gyrus, and pre- and postcentral gyri. The Alcohol group showed no significant regions of greater activation (Table 5). Within groups, the Control group exhibited significant activation in the calcerine, lingual, and occipital gyri, insula, putamen, caudate, thalamus, IFG, right pallidum, left rolandic operculum, SFG, SMG, SMA, MFG, ACC, MCC, and pre- and postcentral gyri, while the Alcohol group showed no regions of significant activation (Figs. 2b and 3, Table 6).
Group differences in anterior cingulate cortex activation. a Controls showed greater activation than the Alcohol group in the dorsal anterior cingulate/middle cingulate cortices during delay. b Alcohol group showed greater activation than controls in the rostral anterior cingulate cortex during magnitude
As groups significantly differ in MDD and PTSD diagnoses, a secondary analysis was conducted excluding 10 subjects in the alcohol group with either diagnosis. The differences in activation between Control and Alcohol groups, absent of any mental health diagnoses, remained significant.
Completers vs non-completers
There were no significant whole-brain differences in activation between Completers and Non-Completers during the magnitude or delay events. Exploratory analyses using functional regions of interest from the Alcohol and Control group comparisons during magnitude (ACC) and delay (insula) events also show no significant differences between Completers and Non-Completers. Using a lower voxel height threshold of Z > 2.3 (default in FSL), we found a group by craving interaction, where the relationship between craving and activation for magnitude differed between Completers and Non-Completers. Non-Completers exhibited a positive relationship between craving and activation in right IFG/MFG, while the relationship was negative in Completers (Fig. 4). This relationship was only significant for magnitude.
Group differences in the relationship between activation and craving. Alcohol craving was assessed using a visual analog scale (VAS) ranging from 0 (no craving) to 100 (most intense craving imaginable). Scatterplot illustrates the group interaction and shows differences between study Completers and Non-Completers on the relationship between craving and beta values for right lateral prefrontal cortex (LPFC) from the whole-brain regression during magnitude (group × activation interaction)
Discussion
This study used a probabilistic delay discounting task during fMRI to measure brain function associated with decision-making based on independently variable delays to receipt and monetary reward magnitudes while accounting for risk. The Alcohol group demonstrated greater delay discounting than the Control group, consistent with the idea that impulsive choice is a potential behavioral phenotype in substance-use disorders (Bickel et al. 2014; Lim et al. 2017; MacKillop 2013). In addition, in line with previous studies of impulsive choice in substance-use disorders (Bobova et al. 2009; MacKillop et al. 2011; Mitchell et al. 2005), the Alcohol group exhibited pronounced differences in regions critical for integrating, assessing, and updating information used by reward evaluation processes that determine choice preferences (Ernst and Paulus 2005; McClure et al. 2004). Here, we show that impulsive choice, as measured using the PDD, is a promising construct for differentiating between AUD and healthy controls. Furthermore, within the Alcohol group, study Completers and Non-Completers showed differential relationships between activation of the right lateral PFC and craving while evaluating reward magnitude, suggesting that lateral PFC activation may interact with relapse risk factors to influence goal-directed behavior in the early stages of recovery.
Limbic regions play an important role in executive function, where the anterior insula is thought to mediate recruitment of executive control regions by activating cognitive control signal transmission to the ACC, thereby enhancing cognitive and inhibitory control (Menon and Uddin 2010). The Alcohol group exhibited less activation than Controls in MCC/dACC and anterior insula during delay, which may suggest that the Alcohol group is allocating less attentional resources to delay. This imbalance may be attributed to greater activation of the rACC in response to reward magnitude leading to an overvaluation of monetary reward. This interpretation is consistent with the functional parcellation of the ACC where the subgenual/rACC is responsible for processing emotional and motivational information (Zilverstand et al. 2018), while the MCC/dACC is implicated in attentional control (Anderson 2016) and conflict monitoring (Botvinick et al. 2004; Carter and van Veen 2007).
Within the cognitive control regions, the Alcohol group exhibited greater activation in the ventral medial PFC (VMPFC) during magnitude and diminished activation of the DLPFC during delay, which may indicate a lack of cognitive control and response inhibition during delay. This is in line with computational models of neurobiological processes of self-control where VMPFC activation is associated with assessing and assigning value to basic attributes of an option (i.e., magnitude, immediate availability), while abstract attributes, such as delay, require DLPFC recruitment (Hare et al. 2014). These models postulate that the DLPFC modulates the activity of the VMPFC to maximize subjective benefits of the overall option (i.e., maximize monetary payout). Our results are consistent with this idea and suggest that less recruitment of the DLPFC during delay may enhance VMPFC reactivity to reward in the Alcohol group.
In summary, the anterior insula, ACC/MCC, and PFC are regions that are sensitive to highly relevant stimuli and responsible for salience detection and attentional control (Zilverstand et al. 2018). Our results showing that the Alcohol group exhibited greater activation in rACC and medial PFC in response to reward magnitude and less activation in MCC/dACC, anterior insula, and lateral PFC during delay may provide a mechanism by which greater salience attribution to reward and less attentional control for delay contributes to steeper discounting in AUD. This is in line with previous reports of greater salience attribution to reward (Bjork et al. 2012) and deficits in cognitive control (see Le Berre et al. 2017) affecting higher-order functioning and decision-making in substance-dependent individuals. We also show that increased craving is associated with greater activation of the lateral PFC in Non-Completers, while the opposite is true in Completers. This negative relationship between the PFC and craving in study Completers is similar to findings of a negative relationship between functional connectivity of the executive control network and craving in AUD patients maintaining sobriety (Kohno et al. 2017), suggesting that greater PFC activation may attenuate craving and increase the likelihood of successful treatment completion. As dysregulation of executive control regions interrupts goal-directed behavior (Zilverstand et al. 2018), these results may indicate a vulnerability, particularly in reward- and goal-driven behavior in treatment non-completers, given that the interaction was observed during reward magnitude response. Furthermore, as repeated drug and alcohol intake promotes excessive attention towards drug-related or reward cues mediated by the PFC (Goldstein and Volkow 2011), frontal cortical regulation seems to be critical for overcoming relapse risk factors, such as craving, which may lead to higher instances of treatment completion and abstinence. Finally, as these results were no longer significant using more stringent p values, these interpretations linking brain function to cognitive function should be taken with caution and future studies are required to simultaneously test the role of the PFC in reward-driven behavior to better understand the role of the PFC in treatment outcome.
Limitations
This study demonstrates differences in neural processing during decision-making between individuals in early recovery from AUD and healthy control subjects; however, potential limitations should be mentioned. In this study, we aimed to collect alcohol use data for 3 months following baseline measures in the Alcohol group, which is considered the minimum time enrolled in a treatment program to see positive outcomes (e.g., abstinence, less criminal involvement, stronger mental health) (Deane et al. 2012). Similar to other studies reporting attrition rates of approximately 50–80% in the first 3 months after entering drug and alcohol treatment programs (Deane et al. 2012; Stark 1992), we observed an attrition rate of roughly 51%, and despite attempts to follow AUD individuals for 3 months, our study Non-Completer group consisted mostly of individuals who dropped out of the study and three individuals who self-reported relapsing. Although treatment drop-out does not necessarily indicate relapse, a linear relationship exists between length of stay and positive treatment outcomes (Zhang et al. 2003), and relapse rates remain high for those who do receive treatment (Moos and Moos 2006). Furthermore, as this study used differences in baseline measures to infer treatment completion outcome 3 months later, longitudinal studies are needed to determine if differences in brain function are sustained during the first 3 to 6 months of recovery and if they track with alcohol use and craving. We were unable to examine sex differences in this study due to the low number of female participants. Future studies examining the interactive effects of sex differences with relapse risk factors in promoting abstinence are important, as alcohol-related outcomes including rates of AUD (Keyes et al. 2008) and treatment enrollment (Agabio et al. 2017) vary between men and women.
Although we found an interaction between craving and DLPFC when assessing monetary reward magnitude between Non-Completers and Completers, it is important to note that self-report craving measures, such as the VAS, do not reliably correlate with alcohol-use behavior (Drobes and Thomas 1999). Although it is possible that this simple measure of craving contributed to the loss of significance of the interaction we found when using a more stringent p value, these results should be considered with caution. Future studies should examine the validity of this interaction by using a more robust measure of craving, such as the Penn Alcohol Craving Scale, which includes questions about the frequency, intensity, and duration of craving as well as the ability to resist drinking and an overall rating of craving for alcohol during the previous week (Flannery et al. 1999).
Potential PDD task design limitations were considered. The PDD tested differences in brain activation between groups when choosing between a constant immediate reward and an alternative reward, which varied in time, magnitude, and probability of receiving the reward. With this design, we were unable to examine brain activation when choosing between two future delays. Evidence shows that during delay discounting, lateral prefrontal and posterior parietal activation was present irrespective of delay, even when two future delays were presented (McClure et al. 2004). As we found significant differences in lateral PFC and posterior parietal regions between the Alcohol and Control groups, future tasks would benefit from incorporating choice pairs with two future delays to distinguish the versatile roles of these regions during different decision-making paradigms. In addition, although this study examined brain function controlling for each parameter inherent in delay discounting (magnitude, delay, and probability), future studies should consider examining differences in brain reactivity to reward as a function of delay and uncertainty.
In this study, participants received additional compensation equal to one choice trial randomly selected from all trials (i.e., potentially real rewards). Discounting of real versus hypothetical monetary rewards has been extensively studied in delay and probability discounting, generally finding no statistical behavioral differences in responses between the two types of rewards (Matusiewicz et al. 2013). Furthermore, real and hypothetical rewards during delay discounting have been shown to activate similar brain regions during fMRI (Bickel et al. 2009). Although real compensation randomly chosen from all trials incentivizes participants to answer each question as though it will be the one chosen, we did not collect information regarding concerns over future whereabouts and/or current financial states, which may potentially bias discounting behavior. Future studies should address this issue by implementing a debriefing at the end of the visit to control for any potential bias.
Conclusion
Together, these results extend the neuroimaging literature of choice selection during delay discounting in AUD. Here, we provide evidence that attentional control and salience attribution are disrupted in AUD, such that dysfunctional ACC recruitment may diminish cognitive control signals to regions in the dorsal and ventral lateral PFC (Johnston et al. 2007; Menon and Uddin 2010) further disrupting DLPFC function of processing abstract attributes and modulating VMPFC activation. Results from this study further support the importance of the PFC in executive and inhibitory control over reward-driven behavior, which is critical in regulating craving and maintaining sobriety. We postulate that alcohol-induced neuroadaptations may manifest in steeper discounting behavior and may mediate craving and vulnerability to relapse.
Change history
21 December 2019
After publication of this paper, the authors determined an error in the funding information section CX17008-CDA2 should be CX001790 (MK).
References
Agabio R, Pisanu C, Gessa GL, Franconi F (2017) Sex differences in alcohol use disorder. Curr Med Chem 24:2661–2670
Amlung M, Sweet LH, Acker J, Brown CL, MacKillop J (2014) Dissociable brain signatures of choice conflict and immediate reward preferences in alcohol use disorders. Addict Biol 19:743–753
Anderson BA (2016) What is abnormal about addiction-related attentional biases? Drug Alcohol Depend 167:8–14
Ballard K, Knutson B (2009) Dissociable neural representations of future reward magnitude and delay during temporal discounting. Neuroimage 45:143–150
Bickel WK, Pitcock JA, Yi R, Angtuaco EJ (2009) Congruence of BOLD response across intertemporal choice conditions: fictive and real money gains and losses. J Neurosci 29:8839–8846
Bickel WK, Koffarnus MN, Moody L, Wilson AG (2014) The behavioral- and neuro-economic process of temporal discounting: a candidate behavioral marker of addiction. Neuropharmacology 76 Pt B:518–527
Bjork JM, Hommer DW, Grant SJ, Danube C (2004) Impulsivity in abstinent alcohol-dependent patients: relation to control subjects and type 1-/type 2-like traits. Alcohol 34:133–150
Bjork JM, Smith AR, Chen G, Hommer DW (2012) Mesolimbic recruitment by nondrug rewards in detoxified alcoholics: effort anticipation, reward anticipation, and reward delivery. Hum Brain Mapp 33:2174–2188
Blum K, Braverman ER, Holder JM, Lubar JF, Monastra VJ, Miller D, Lubar JO, Chen TJ, Comings DE (2000) Reward deficiency syndrome: a biogenetic model for the diagnosis and treatment of impulsive, addictive, and compulsive behaviors. J Psychoactive Drugs i-iv(32 Suppl):1–112
Bobova L, Finn PR, Rickert ME, Lucas J (2009) Disinhibitory psychopathology and delay discounting in alcohol dependence: personality and cognitive correlates. Exp Clin Psychopharmacol 17:51–61
Boettiger CA, Mitchell JM, Tavares VC, Robertson M, Joslyn G, D'Esposito M, Fields HL (2007) Immediate reward bias in humans: fronto-parietal networks and a role for the catechol-O-methyltransferase 158(Val/Val) genotype. J Neurosci 27:14383–14391
Botvinick MM, Cohen JD, Carter CS (2004) Conflict monitoring and anterior cingulate cortex: an update. Trends Cogn Sci 8:539–546
Braus DF, Wrase J, Grusser S, Hermann D, Ruf M, Flor H, Mann K, Heinz A (2001) Alcohol-associated stimuli activate the ventral striatum in abstinent alcoholics. J Neural Transm (Vienna) 108:887–894
Carter CS, van Veen V (2007) Anterior cingulate cortex and conflict detection: an update of theory and data. Cogn Affect Behav Neurosci 7:367–379
de Wit H (2009) Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addict Biol 14:22–31
Deane FP, Wootton DJ, Hsu CI, Kelly PJ (2012) Predicting dropout in the first 3 months of 12-step residential drug and alcohol treatment in an Australian sample. J Stud Alcohol Drugs 73:216–225
Drobes DJ, Thomas SE (1999) Assessing craving for alcohol. Alcohol Res Health 23:179–186
Ernst M, Paulus MP (2005) Neurobiology of decision making: a selective review from a neurocognitive and clinical perspective. Biol Psychiatry 58:597–604
Flannery BA, Volpicelli JR, Pettinati HM (1999) Psychometric properties of the Penn alcohol craving scale. Alcohol Clin Exp Res 23:1289–1295
Goldstein RZ, Volkow ND (2011) Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci 12:652–669
Grusser SM, Wrase J, Klein S, Hermann D, Smolka MN, Ruf M, Weber-Fahr W, Flor H, Mann K, Braus DF, Heinz A (2004) Cue-induced activation of the striatum and medial prefrontal cortex is associated with subsequent relapse in abstinent alcoholics. Psychopharmacology 175:296–302
Hare TA, Hakimi S, Rangel A (2014) Activity in dlPFC and its effective connectivity to vmPFC are associated with temporal discounting. Front Neurosci 8:50
Ho MY, Mobini S, Chiang TJ, Bradshaw CM, Szabadi E (1999) Theory and method in the quantitative analysis of “impulsive choice” behaviour: implications for psychopharmacology. Psychopharmacology 146:362–372
Johnston K, Levin HM, Koval MJ, Everling S (2007) Top-down control-signal dynamics in anterior cingulate and prefrontal cortex neurons following task switching. Neuron 53:453–462
Keyes KM, Grant BF, Hasin DS (2008) Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug Alcohol Depend 93:21–29
Kober H, Mende-Siedlecki P, Kross EF, Weber J, Mischel W, Hart CL, Ochsner KN (2010) Prefrontal-striatal pathway underlies cognitive regulation of craving. Proc Natl Acad Sci USA 107:14811–14816
Kohno M, Dennis LE, McCready H, Hoffman WF (2017) Executive control and striatal resting-state network interact with risk factors to influence treatment outcomes in alcohol-use disorder. Front Psychiatry 8:182
Koob GF, Le Moal M (2001) Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology 24:97–129
Le Berre AP, Fama R, Sullivan EV (2017) Executive functions, memory, and social cognitive deficits and recovery in chronic alcoholism: a critical review to inform future research. Alcohol Clin Exp Res 41:1432–1443
Lim AC, Cservenka A, Ray LA (2017) Effects of alcohol dependence severity on neural correlates of delay discounting. Alcohol Alcohol 52:506–515
Lopez-Guzman S, Konova AB, Louie K, Glimcher PW (2018) Risk preferences impose a hidden distortion on measures of choice impulsivity. PLoS One 13:e0191357
Luijten M, Schellekens AF, Kuhn S, Machielse MW, Sescousse G (2017) Disruption of reward processing in addiction : an image-based meta-analysis of functional magnetic resonance imaging studies. JAMA Psychiatry 74:387–398
MacKillop J (2013) Integrating behavioral economics and behavioral genetics: delayed reward discounting as an endophenotype for addictive disorders. J Exp Anal Behav 99:14–31
MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, Munafo MR (2011) Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology 216:305–321
Maisto SA, Pollock NK, Cornelius JR, Lynch KG, Martin CS (2003) Alcohol relapse as a function of relapse definition in a clinical sample of adolescents. Addict Behav 28:449–459
MATLAB and Statistics Toolbox Release 2013b, Copyright 1984-2012, The MathWorks, Inc., Natick, Massachusetts, United States
Matusiewicz AK, Carter AE, Landes RD, Yi R (2013) Statistical equivalence and test-retest reliability of delay and probability discounting using real and hypothetical rewards. Behav Process 100:116–122
McClure SM, Laibson DI, Loewenstein G, Cohen JD (2004) Separate neural systems value immediate and delayed monetary rewards. Science 306:503–507
Menon V, Uddin LQ (2010) Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct 214:655–667
Miedl SF, Peters J, Buchel C (2012) Altered neural reward representations in pathological gamblers revealed by delay and probability discounting. Arch Gen Psychiatry 69:177–186
Mitchell SH, Wilson VB (2012) Differences in delay discounting between smokers and nonsmokers remain when both rewards are delayed. Psychopharmacology 219:549–562
Mitchell JM, Fields HL, D'Esposito M, Boettiger CA (2005) Impulsive responding in alcoholics. Alcohol Clin Exp Res 29:2158–2169
Moos RH, Moos BS (2006) Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction 101:212–222
O'Connor PG, Gottlieb LD, Kraus ML, Segal SR, Horwitz RI (1991) Social and clinical features as predictors of outcome in outpatient alcohol withdrawal. J Gen Intern Med 6:312–316
Patak M, Reynolds B (2007) Question-based assessments of delay discounting: do respondents spontaneously incorporate uncertainty into their valuations for delayed rewards? Addict Behav 32:351–357
Petry NM (2001) Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology 154:243–250
Stark M (1992) Dropping out of substance abuse treatment: a clinically oriented review. Clin Psychol Rev 12:93–116
Stevens L, Verdejo-Garcia A, Roeyers H, Goudriaan AE, Vanderplasschen W (2015) Delay discounting, treatment motivation and treatment retention among substance-dependent individuals attending an in inpatient detoxification program. J Subst Abus Treat 49:58–64
Vanderveldt A, Green L, Myerson J (2015) Discounting of monetary rewards that are both delayed and probabilistic: delay and probability combine multiplicatively, not additively. J Exp Psychol Learn Mem Cogn 41:148–162
Zhang Z, Friedmann PD, Gerstein DR (2003) Does retention matter? Treatment duration and improvement in drug use. Addiction 98:673–684
Zilverstand A, Huang AS, Alia-Klein N, Goldstein RZ (2018) Neuroimaging impaired response inhibition and salience attribution in human drug addiction: a systematic review. Neuron 98:886–903
Acknowledgments
We thank the staff of the Veterans Affairs Portland Health Care System Substance Abuse Treatment Program, CODA Treatment Recovery, Hooper Detox Stabilization Center, Central City Concern, and Volunteers of America Residential Treatment Centers, Portland, OR, for their help and recruitment efforts and also Ethan Sawyer for his help with the manuscript.
Funding
This work was supported in part by the National Institute on Alcohol Abuse and Alcoholism R21AA020039 (WFH); Department of Veterans Affairs Clinical Sciences Research and Development Merit Review Program, I01 CX001558-01A1 (WFH); Department of Justice 2010-DD-BX-0517 (WFH); National Institute on Drug Abuse P50DA018165 (WFH); and Oregon Clinical and Translational Research Institute, 1 UL1 RR024140 01 from the National Center for Research Resources, a component of the National Institutes of Health and National Institute of Health Roadmap for Medical Research. Dr. Kohno was supported by National Institute on Drug Abuse T32 DA007262, National Institute on Alcohol Abuse and Alcoholism T32 AA007468, Department of Veterans Affairs Clinical Sciences Research and Development Career Development Award CX17008-CDA2, Oregon Health & Science University Collins Medical Trust Award APSYC0249, and Medical Research Foundation of Oregon APSYC0250.
Author information
Authors and Affiliations
Contributions
MK conceptualized this approach, made significant contributions to the analysis and writing of this manuscript, and mentored LD in the interpretation of results and writing of this manuscript. LD, HM, BT, DS, and DL collected these data. DS, DL, WH, and SM each contributed significantly to designing the PDD task. BN was a Co-I on the grant and advised on imaging and design. LD performed initial data analyses with the neuroimages. WH was the PI on the project, supervised the collection and analysis of data, and contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Laura E. Dennis and Milky Kohno share co-first authorship.
The contents of this paper do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Rights and permissions
About this article
Cite this article
Dennis, L.E., Kohno, M., McCready, H.D. et al. Neural correlates of reward magnitude and delay during a probabilistic delay discounting task in alcohol use disorder. Psychopharmacology 237, 263–278 (2020). https://doi.org/10.1007/s00213-019-05364-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-019-05364-3