Abstract
Rationale
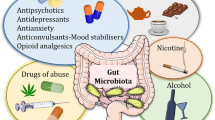
Growing evidence supports a role for the microbiota in regulating gut-brain interactions and, thus, psychiatric disorders. Despite substantial scientific efforts to delineate the mechanism of action of psychotropic medications at a central nervous system (CNS) level, there remains a critical lack of understanding on how these drugs might affect the microbiota and gut physiology.
Objectives
We investigated the antimicrobial activity of psychotropics against two bacterial strain residents in the human gut, Lactobacillus rhamnosus and Escherichia coli. In addition, we examined the impact of chronic treatment with these drugs on microbiota and intestinal parameters in the rat.
Results
In vitro fluoxetine and escitalopram showed differential antimicrobial effects. Lithium, valproate and aripiprazole administration significantly increased microbial species richness and diversity, while the other treatments were not significantly different from controls. At the genus level, several species belonging to Clostridium, Peptoclostridium, Intestinibacter and Christenellaceae were increased following treatment with lithium, valproate and aripiprazole when compared to the control group. Animals treated with escitalopram, venlafaxine, fluoxetine and aripiprazole exhibited an increased permeability in the ileum.
Conclusions
These data show that psychotropic medications differentially influence the composition of gut microbiota in vivo and that fluoxetine and escitalopram have specific antimicrobial activity in vitro. Interestingly, drugs that significantly altered gut microbial composition did not increase intestinal permeability, suggesting that the two factors are not causally linked. Overall, unravelling the impact of psychotropics on gastrointestinal and microbiota measures offers the potential to provide critical insight into the mechanism of action and side effects of these medications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The burden of psychiatric disorders on society continues to grow, with estimates from the World Health Organization (WHO) suggesting that worldwide, 322 million and 60 million people are affected by depression and bipolar disorder, respectively (World Health Organization 2017). Treatment options used in the management of psychiatric disorders are often associated with metabolic side effects (Beyazyüz et al. 2013; Correll et al. 2015; Olguner Eker et al. 2017; Reynolds and Kirk 2010; Tschoner et al. 2007) and high non-response rates (Ackenheil and Weber 2004; Al-Harbi 2012; Hatta and Ito 2014; Nelson 1998). Over the last decade, a growing body of evidence has highlighted a significant role for the gut microbiota in interactions between the gut and the brain (Bercik et al. 2012; Collins et al. 2012; Cryan and Dinan 2012b; Dinan et al. 2013; Mayer et al. 2014; Mayer et al. 2015). Moreover, alterations in this microbiota-gut-brain axis are associated with several behavioural and psychiatric conditions (Cryan and Dinan 2012a; Foster and McVey Neufeld 2013; Luna and Foster 2015). Strikingly, individuals with depression (Jiang et al. 2015; Kelly et al. 2016; Naseribafrouei et al. 2014; Zheng et al. 2016), bipolar disorder (Evans et al. 2017) and schizophrenia (Dinan et al. 2014; Schwarz et al. 2017) exhibit alterations in microbiota composition compared to controls. Moreover, recent data has shown that the transfer of microbiota from humans with depression into microbiota-depleted rats or mice induces a depressive-like phenotype, indicating that the gut microbiota may play a key role in the onset of depressive behaviour (Kelly et al. 2016; Zheng et al. 2016).
Despite substantial scientific efforts to unravel the effects of psychotropic medications in the central nervous system, the impact that these drugs have on gut physiology and microbiota composition is rarely considered. Some isolated studies have shown that antidepressants and antipsychotics possess a microbiota-targeted action. Indeed sertraline, fluoxetine and paroxetine are bactericidal against gram-positive bacteria such as Staphylococcus and Enterococcus (Ayaz et al. 2015b; Coban et al. 2009); however, these data are mostly reliant on in vitro microbiological studies and are not exhaustive. Regarding antipsychotics, it has been shown that chronic administration of the antipsychotics olanzapine and risperidone affects the gut microbiota composition in animals and humans (Bahr et al. 2015b; Davey et al. 2013; Davey et al. 2012; Kao et al. 2018; Morgan et al. 2014). A recent study has demonstrated that intake of atypical antipsychotics is associated with significant changes in microbiota composition (Flowers et al. 2017a), while larger cohort studies have suggested that the use of medications can alter the gut microbiota more generally (Falony et al. 2016; Maier et al. 2018). Behavioural responses to cocaine, another compound belonging to the class of psychotropics, have recently been shown to be affected by gut microbiota shifts in mice (Kiraly et al. 2016).
Importantly, psychotropic medications are often administered orally, thus the gut microbiota represents a plausible target for distal action of these drugs. To this end, we sought to examine the effects that commonly used psychotropics have on microbiota composition and intestinal permeability, which is closely regulated by the gut microbiota (Karl et al. 2017; Ott et al. 2017; Ulluwishewa et al. 2011). Furthermore, we assess the antimicrobial activity of these medications against isolated strains resident in the human gut, Lactobacillus rhamnosus and Escherichia coli. Unravelling the comparative microbiome and gastrointestinal actions of different psychotropics in vivo will provide new insight into the mechanism of these drugs and their side effects and may have a critical impact on future clinical practice and drug discovery efforts.
Materials and methods
Bacterial growth-inhibition assay
Lactobacillus rhamnosus 6118 was grown in anaerobiosis at 37 °C overnight in MRS broth (BD Difco Lactobacilli MRS Broth). Escherichia coli APC105 was grown shaking overnight at 37 °C in BHI broth (Oxoid™ Brain Heart Infusion Broth). Overnight cultures were resuspended in broth to an OD reading (optical density at 600-nm wavelength) of 0.1, which corresponded to their lag phase. Resuspended cultures were incubated with a range of drugs dissolved in sterile deionised water at different concentrations (100, 400 and 600 μg/mL). The OD of the bacteria was measured every hour for up to 7 h. The vehicle consisted of the dissolution medium only, and each curve was produced in triplicates.
Animals
Adult male Sprague Dawley rats (n = 8/group; 200–250 g on arrival) were obtained from Envigo, UK. They were housed two per cage and maintained under a 12-h light/dark cycle, provided with chow and water ad libitum. Rats in the same cage underwent the same treatment to avoid confounding factors such as coprophagy. Animals were acclimated to housing conditions for 1 week prior to experimental treatment. Experiments were conducted in accordance with the European Directive 2010/63/EU. Approval by the Animal Experimentation Ethics Committee of University College Cork was obtained before commencement of all animal-related experiments.
Drug administration
Each drug was administered for 28 days in drinking water or in the chow, and the administration continued throughout the behavioural assessment until the animals were culled (Fig. 1, Table 1).
The control group received a standard diet (Ssniff, SM Teklad Global 18% Protein Rodent diet, item no. S9912-S710) and drinking water. A second group received 6.38 mg/kg/day of escitalopram oxalate (5 mg/kg/day of free base) in drinking water and standard diet. A third group received 20 mg/kg/day of venlafaxine HCl in drinking water and standard diet. A fourth group received 10 mg/kg/day of fluoxetine HCl in drinking water and standard diet. A fifth group received 0.2% lithium-supplemented diet, corresponding to approx. 150 mg/kg/day, and hypertonic saline water (1.5% NaCl, in order to prevent lithium-induced ionic imbalance). A sixth group received 2% valproate-supplemented diet, corresponding to approx. 1.5 g/kg/day, and drinking water. A seventh group received 0.027% aripiprazole-supplemented diet, corresponding to approx. 20 mg/kg/day, and drinking water. The concentration of each drug in drinking water and in the chow was determined from the average daily water/food consumption and the average body weight per rat. These dosing regimens have been previously used in chronic behavioural and neurochemical studies in rats (Ariel et al. 2017; Kaminska and Rogoz 2016; Lyons et al. 2012; Monti et al. 2010; O’Leary et al. 2012; Segnitz et al. 2009; Sogaard et al. 2005; Vidal et al. 2010; Watase et al. 2007). The drinking bottles were protected from light and changed every second day, and the chow was stored at 4 °C during the experiment.
Open field (OF) test
To assess possible sedative effects of treatments, the animals were placed in an open arena brightly lit from above and the test was carried out as previously described (O’Mahony et al. 2014). Briefly, 30 min before behavioural testing, the animals were habituated to the room. The apparatus consisted of a white round arena with a diameter of 90 cm, brightly lit to 1000 lx. At the beginning of the test, animals were placed into the centre of the arena and allowed to explore for 10 min. After testing, the animals were returned to their home cage. The arena was cleaned with 70% ethanol between trials to ensure that no cue smell remained from the previous trail. Faecal output was manually scored. Total distance travelled was analysed using a tracking software system (Ethovision XT 11.5, Noldus). None of the treatments at the doses tested affected the locomotor activity or the faecal output of the animals (Fig. S1).
Intestinal permeability
Freshly isolated ileal and colonic tissues were placed in Krebs solution and cut along the mesenteric border. Tissues were then mounted into the Ussing chamber apparatus (Harvard Apparatus, Kent, UK, exposed area of 0.12 cm2) as previously described (Golubeva et al. 2017). Four kilodaltons of FITC-dextran was added to the mucosal chamber at a final concentration of 2.5 mg/mL; 200-μL samples were collected from the serosal chamber after 1 h and every 30 min for the following 3 h. FITC was measured at 485-nm excitation/535-nm emission wavelengths.
Microbiota composition and short-chain fatty acids analysis in the caecal content
Caecum was harvested and immediately snap-frozen and stored at − 80 °C prior to the analysis. DNA was extracted using the Qiagen QIAmp Fast DNA Stool Mini Kit coupled with an initial bead-beating step. The V3-V4 hypervariable region of the 16S rRNA gene was amplified and prepared for sequencing as outlined in the Illumina 16S Metagenomic Sequencing Library protocol. Samples were sequenced at Teagasc Sequencing Facility (TFRC, Moorepark) on the Illumina MiSeq platform using a 2 × 250-bp kit. Reads were assembled, processed and analysed following the pipeline, described in Supplemental Methods. Short-chain fatty acids (SCFAs) were measured by gas chromatography, using a Varian 3500 GC flame-ionization system fitted with a ZB-FFAP column. For construction of the heatmap, log2 ratios were calculated from group medians of highly abundant bacteria at the genus level using R (version 3.3.2) and R Studio (version 1.0.136).
Statistical analysis
Data are presented as mean + SEM. Intestinal permeability and in vitro data were analysed using mixed between-within subjects ANOVA followed by unpaired two-tailed t test. Body weight and organ weights were analysed using one-way ANOVA followed by Dunnett’s test. 16S rRNA sequencing data was analysed using Kruskal-Wallis non-parametric test followed by Mann-Whitney U test and corrected for multiple comparisons using the Benjamin-Hochberg false discovery rate (FDR) method. Grubbs method was employed to test for any specific outliers (Grubbs 1950). Threshold for statistical significance was set at p < 0.05.
Results
Fluoxetine and escitalopram exert specific antimicrobial activity against two bacterial strain residents in the human gut
We tested the effects of psychotropic medications on growth of Lactobacillus rhamnosus 6118 and E. coli APC105 in vitro. These bacterial strains belong to two of the four dominant phyla of the mammalian gut (Firmicutes and Proteobacteria, respectively). Each drug was assessed at three different concentrations (100, 400 and 600 μg/mL). Growth curves were performed measuring the optical density (OD) at different time points. Growth of L. rhamnosus was completely inhibited by 400 and 600 μg/mL fluoxetine, while growth of E. coli was inhibited by 600 μg/mL escitalopram and by all three doses of fluoxetine (Fig. 2). Venlafaxine, lithium and valproate did not exhibit antimicrobial activity in vitro. Aripiprazole’s antimicrobial activity was not assessed due to its tendency to precipitate with components of the broth, resulting in high risk of false positive data from OD measurements.
Effect of psychotropic drugs on the growth of Lactobacillus rhamnosus6118 andEscherichia coliAPC105 in vitro. Escitalopram and fluoxetine have differential antimicrobial effects. In bold are bactericidal doses. Statistics: Data are expressed as mean + SEM. *p < 0.05, **p < 0.01 and ***p < 0.001 (n = 3/group). Escitalopram effect on E.coli: F(7;56) = 491.682, p < 0.001 for the effect of time, F(3;8) = 82.898, p < 0.001 for the effect of treatment, F(21;56) = 59.87, p < 0.001 for the time × treatment interaction. Fluoxetine effect on L. rhamnosus: F(7;56) = 42.467, p < 0.001 for the effect of time, F(3;8) = 28.574, p < 0.001 for the effect of treatment, F(21;56) = 15.439, p < 0.001 for the time × treatment interaction. Fluoxetine effect on E.coli: F(7;56) = 188.805, p < 0.001 for the effect of time, F(3;8) = 712.570, p < 0.001 for the effect of treatment, F(21;56) = 176.477, p < 0.001 for the time × treatment interaction. Data were analysed with a mixed between-within subjects ANOVA. F F statistic. Mean values in each time point were further compared to the vehicle with unpaired t test. Statistical outcomes for the t test are described in Supplemental Material
Administration of fluoxetine, lithium, valproate and aripiprazole significantly alters gut microbiota composition
Our in vitro results demonstrated that certain psychotropic drugs differentially modulate the growth of resident gut bacteria. To confirm this in an in vivo setting and to assess if any of the treatments induced changes in intestinal microbiota composition, we performed 16S sequencing of bacterial rRNA of the caecum content following chronic administration in rats. The sequencing revealed a significant increase in the bacterial richness and diversity of rats treated with lithium, valproate and aripiprazole as compared to the vehicle-treated group (Fig. 3a). Moreover, separation according to group was further illustrated through principal coordinate analysis (PCoA), with statistical support of the significant separation between escitalopram, venlafaxine, lithium, valproate, aripiprazole and the vehicle (p < 0.05, Fig. 3b).
Altered microbiota richness and diversity in psychotropic-treated animals as compared to vehicle-treated animals.a Alpha diversity. Statistics: Kruskal-Wallis test for Chao1 (p = 0.000) and Shannon (p = 0.000). Mann-Whitney U test for: Chao1 index: lithium U(16) = 6, p = 0.006; valproate U(16) = 10, p = 0.021; aripiprazole U(16) = 12, p = 0.036. Shannon index: lithium U(16) = 0, p = 0.001; valproate U(16) = 2, p = 0.002; aripiprazole U(16) = 0, p = 0.001. Data are expressed as median and min-to-max values. *p < 0.05, **p < 0.01 and ***p < 0.001 (n = 8/group). b Principal coordinate analysis of Bray-Curtis compiled distance matrix of all microbial relative abundances compared with the vehicle group (light grey ellipse). Escitalopram, venlafaxine, lithium, valproate and aripiprazole show significant variation from the vehicle (Adonis PERMANOVA p < 0.05). c Heatmap of log2 fold change ratio of medians at the genus level. Red indicates an increase and blue a decrease of taxa in the different treatment groups as compared to vehicle-treated rats. Microbial genera that were significantly different in at least one of the experimental groups compared to the vehicle were selected for the heatmap. E escitalopram, Ve venlafaxine, F fluoxetine, L lithium, Va valproate, A aripiprazole
At the phylum level, lithium induced a significant increase in Actinobacteria and a decrease in Bacteroidetes; valproate induced an increase in Actinobacteria, Firmicutes and a decrease in Bacteroidetes; fluoxetine induced a decrease in Deferribacteres and aripiprazole induced an increase in Firmicutes (Fig. S2, Table S1). At the family level, lithium, valproate and aripiprazole increased significantly the levels of Peptostreptococcaceae, Clostridiaceae and Ruminococcaceae (Fig. S3, Table S2). Other families were increased by the different treatments, while some of the less abundant families were decreased (refer to Supplemental Material for details). At the genus level of the most abundant taxa, lithium increased the relative abundance of Ruminococcaceae uncultured and decreased the relative abundance of Bacteroides and Ruminococcus 1; valproate decreased the relative abundance of S24-7 uncultbact and increased the relative abundance of Ruminococcaceae uncultured, while aripiprazole decreased the relative abundance of Ruminococcus 1 (Fig. 4). None of the treatments significantly affected the genera Lachnospiraceae uncultured, Akkermansia, S24-7 uncultbact and Oscillibacter.
Psychotropic drugs differentially affect bacterial composition at genus level of the most abundant taxa. Lithium increased the relative abundance of Ruminococcaceae uncultured and decreased the relative abundance of Bacteroides and Ruminococcus 1. Valproate decreased the relative abundance of S24-7 uncultbact and increased the relative abundance of Ruminococcaceae uncultured. Aripiprazole decreased the relative abundance of Ruminococcus 1. Data are expressed as median and min-to-max values. *p < 0.05 (n = 8/group). Data was analysed using Kruskal-Wallis non-parametric test followed by Mann-Whitney U test and corrected for multiple comparisons using the Benjamin-Hochberg false discovery rate (pFDR) method (refer to Supplemental Material for details on statistics)
Interestingly, the relative abundance of minor genera including Clostridium sensu stricto 1, Ruminiclostridium 5, Intestinibacter, Eubacterium coprostanoligens, Peptoclostridium, Eubacterium oxidoreducens, Christensenellaceae uncultured and Clostridia Family XIII was increased by lithium, valproate and aripiprazole administration (Fig. 5), while antidepressant administration did not influence significantly the abundance of these taxa. Among the antidepressants assessed, fluoxetine induced a marked depletion of the genera Prevotella 7, Prevotella 9 and Succinivibrio (Fig. 6).
Psychotropic drugs differentially affect bacterial composition at genus level of the less abundant taxa. Lithium, valproate and aripiprazole induced an increase in the relative abundance of Clostridium sensu stricto 1, Ruminoclostridium 5, Intestinibacter, Eubacterium coprostanoligens, Peptoclostridium, Eubacterium oxidoreducens, Christensenellaceae and Clostridia Family XIII. Data are expressed as median and min-to-max values. *p < 0.05 (n = 8/group). Data was analysed using Kruskal-Wallis non-parametric test followed by Mann-Whitney U test and corrected for multiple comparisons using the Benjamin-Hochberg false discovery rate (pFDR) method (refer to Supplemental Material for details on statistics)
Fluoxetine-sensitive genera in vivo. The genera Prevotella 7, Prevotella 9 and Succinivibrio were all depleted in the caecum of animals treated with fluoxetine. Data are expressed as median and min-to-max values. *p < 0.05 (n = 8/group). Data was analysed using Kruskal-Wallis non-parametric test followed by Mann-Whitney U test and corrected for multiple comparisons using the Benjamin-Hochberg false discovery rate (pFDR) method (refer to Supplemental Material for details on statistics)
Valproate and aripiprazole alter the levels of caecal short-chain fatty acids
A key function of gut bacteria is the catabolism of non-digestible dietary fibres resulting in the production of SCFAs, which in turn modulate a number of physiological processes (den Besten et al. 2013; Koh et al. 2016; Morrison and Preston 2016). We decided to examine the abundance of short-chain fatty acids (SCFAs) in the caecal content in response to psychotropic drugs. Valproate administration induced a significant decrease in the levels of propionate and butyrate while augmenting the levels of isovalerate. Aripiprazole administration induced a significant increase in the levels of acetate and isovalerate (Fig. 7). Two other SCFAs, valerate and isobutyrate, were also quantified and were not affected by any psychotropic treatment (see Fig. S4).
Short-chain fatty acid (SCFA) caecal levels.Statistics: all SCFAs had p < 0.05 in one-way ANOVA. Acetate: Dunnett’s t test p = 0.035 for aripiprazole vs vehicle. Propionate: Dunnett’s t test p = 0.029 for valproate vs vehicle. Butyrate: Dunnett’s t test p = 0.042 for valproate vs vehicle. Isovalerate: Dunnett’s t test p = 0.002 for valproate vs vehicle; p = 0.001 for aripiprazole vs vehicle. Data are expressed as mean + SEM. *p < 0.05 and **p < 0.01 (n = 8/group)
Escitalopram, venlafaxine, fluoxetine and aripiprazole administration increases ileal but not colonic permeability
We assessed paracellular intestinal permeability of treated animals in both ileum and colon tissues ex vivo. Among the drugs tested, escitalopram, venlafaxine, fluoxetine and aripiprazole administration significantly increased epithelial permeability in the distal ileum as compared to vehicle-treated animals (Fig. 8). None of the drugs at the doses tested affected permeability in the distal colon.
Effect of drug treatments on epithelial permeability in small and large intestine. In the different panels, each treatment is compared to the vehicle. a In the distal ileum, escitalopram-, venlafaxine-, fluoxetine- and aripiprazole-treated rats showed a significant increase in FITC paracellular pemerability. b In the colon, none of the drugs induced significant changes in intestinal permeability. Data were analysed with a mixed between-within subjects ANOVA. Statistics: Distal ileum F(5;235) = 385.037, p < 0.001 for the effect of time, F(6;47) = 4.181, p < 0.01 for the effect of treatment, F(30;235) = 3.490, p < 0.01 for the time × treatment interaction. Distal colon F(5;235) = 298.307, p < 0.001 for the effect of time, but no effects for treatment or time × treatment interaction. F F statistic. Mean values in each time point were further compared to the vehicle with unpaired t test. Statistical outcomes for the t test are described in Supplemental Material. Data are expressed as mean + SEM. *p < 0.05, **p < 0.01 and ***p < 0.001 (n = 7–8/group)
Discussion
There is an increasing emphasis on the interactions between gut microbiota and drug action across different therapeutic areas including oncology, cardiovascular medicine and even psychiatry. Here, we assessed whether orally administered psychotropics can affect microbial and intestinal function in healthy adult rats. Escitalopram and fluoxetine showed differential antimicrobial activity in vitro, whereas lithium, valproate and aripiprazole induced significant changes in gut microbiota composition and SCFA levels in vivo. Fluoxetine also induced minor but significant changes in bacterial genera in vivo. Escitalopram, venlafaxine, fluoxetine and aripiprazole increased the intestinal permeability in the ileum but not colon.
Limited studies have investigated the effect of psychotropic medications on growth of microbial strains. We found that both SSRI escitalopram and fluoxetine have diverse antimicrobial activity in vitro against E. coli and L. rhamnosus, two bacteria residing in the human gut (Thursby and Juge 2017; Walter 2008). These results are in line with previous work showing that SSRIs possess antimicrobial action in vitro especially against gram-positive bacteria such as Staphylococcus and Enterococcus (Ayaz et al. 2015a; Coban et al. 2009). Moreover, the antimicrobial activity of some antidepressants has been previously confirmed by the synergistic effects of some SSRIs in combination with antibiotics, as well as their effects against some antibiotic-resistant bacteria (Bohnert et al. 2011a; Munoz-Bellido et al. 1996, 2000). Interestingly, the two drugs, despite both belonging to the same class of antidepressants, showed different effects, with fluoxetine having strong antimicrobial activity and escitalopram being a weak antimicrobial. A possible mechanism through which fluoxetine and escitalopram might inhibit bacterial growth is through their action as efflux pump inhibitors, which interferes with the normal functioning of the bacteria (Bohnert et al. 2011b). Intriguingly, among the drugs assessed in vitro, only fluoxetine induced overt shifts in gut microbiota composition in vivo. Moreover, differences in drug doses might occur in the two experimental settings, making it challenging to directly compare the experiments. These data highlight that some caution is required in extrapolating the results of in vitro assays to predict the effects of drugs on complex gut microbial ecology.
The composition of the gut microbiota was substantially changed in vivo in lithium-, valproate- and aripiprazole- treated animals. Interestingly, the microbial shifts were often consistent across groups, with a significant increase in the relative abundance of minor genera (Fig. 6), while high abundant genera were generally not affected and were decreased in few instances (Fig. 5; i.e. Lachnospiraceae NK4A136, Ruminococcus 1, Bacteroides). Consistent with changes in bacterial genera, the alpha diversity was also augmented in animals treated with lithium, valproate and aripiprazole, suggesting an increase in microbial richness and diversity. Administration of the SSRI fluoxetine also induced changes in microbiota composition, specifically decreasing the genera Prevotella 7, Prevotella 9 and Succinivibrio (Fig. 6).
Some previous studies have shown that, among psychotropic medications, antipsychotics in particular exert an effect on the gut microbiota. Both atypical antipsychotics olanzapine (Davey et al. 2013; Morgan et al. 2014) and risperidone (Bahr et al. 2015a)-induced changes in gut microbiota composition in rodents and children, respectively. Chronic treatment with risperidone was associated with significantly lower ratio of Bacteroidetes:Firmicutes in healthy young males and with an increase in gut microbiota diversity when compared to control participants. Interestingly, we found the same trend in our animals treated with aripiprazole (a compound that belongs to the same therapeutic class of risperidone): at the genus level, 21 of the 26 genera belonging to Firmicutes were significantly increased and two genera belonging to Bacteroidetes were decreased. In addition, the microbial alpha-diversity of aripiprazole-treated rats was significantly increased, in line with data on risperidone-treated children. The results, however, are not always consistent. In a bipolar disease cohort, for example, treatment with atypical antipsychotics induced a decrease in microbial diversity, with the effect being present in females but not in males (Flowers et al. 2017b). In the same study, the bipolar cohort treated with atypical antipsychotics showed, at the microbiota genus level, a significant increase in Lachnospiraceae abundance and a significant decrease in Akkermansia (Flowers et al. 2017b). Also, a recent large-scale study in vitro looking at the effect of several non-antibiotic drugs on human gut bacteria in vitro found that Akkermansia was significantly more sensitive than all other strains to atypical antipsychotics (Maier et al. 2018). In contrast with these findings, treatment with the atypical antipsychotic aripiprazole did not affect the two aforementioned genera in our rats. The fact that antipsychotics cluster together on microbiome despite different chemical structures and CNS effects, implicates that direct bacterial activity may be part of their mechanism of action or at least their side effects.
An important aspect of this study would be to understand the biological and physiological relevance of the bacteria that were altered in response to psychotropic administration. Even though some of the affected genera have not been fully characterised, others have been previously associated to diverse conditions and are described in Table 2.
It is important to note that further work is required to measure the level of these drugs in the caecum, in order to clarify whether these medications reach the caecum at adequate concentrations and are not completely absorbed in the upper gastrointestinal tract. This investigation will further elucidate if the drugs are having a direct microbial effect or are affecting the gut microbiome through indirect mechanisms (such as the gut-brain signalling). Moreover, future studies might want to assess the microbiome-targeted effects of these medications at lower doses, such as those translational to a human setting.
While some knowledge existed of the impact exerted by antipsychotics on the gut microbiota, other classes of psychotropics (see Table 1) have not previously been investigated in vivo. Here, we show that chronic administration of the mood stabiliser lithium and the anticonvulsant valproate significantly affected the microbial composition and richness in rats. The increase in richness might be directly due to the effect of the drugs on the microbial stability and the presence of different bacteria competing for the same niche. This effect on richness might also be time- and dose-dependent. Principal coordinate analysis of Bray-Curtis (beta-diversity) showed that lithium, valproate and aripiprazole had a significant separation from the vehicle group. On the contrary, psychotropics belonging to the class of antidepressants (specifically escitalopram, venlafaxine and fluoxetine) did not markedly affect this aspect of microbial richness and diversity. Only fluoxetine clustered far from the vehicle group in the principal coordinate analysis of Bray-Curtis (Fig. 3b).
Short-chain fatty acids (SCFAs) are produced in the caecum by microbial fermentation (den Besten et al. 2013; Morrison and Preston 2016) and are key regulators of several host processes such as metabolism (De Vadder et al. 2014), behaviour (Schroeder et al. 2007) and CNS function (Erny et al. 2015; Huuskonen et al. 2004). With marked alterations present at the microbiota level, it was perhaps not surprising that changes in SCFAs occurred. Valproate and aripiprazole influenced SCFA abundance in the caecum, with acetate and isovalerate being increased by aripiprazole treatment and propionate, butyrate and isovalerate being differentially altered by valproate (Fig. 7). We next investigated whether changes in SCFA levels were associated with specific microbial taxa that are known producers of SCFAs. Clostridium spp., a known producer of the SCFA acetate (Koh et al. 2016), was found to be increased in aripiprazole-treated animals, while valproate-treated rats showed a decrease in Bacteroidetes, which might explain the reduction in propionate in this experimental group. However, in our study, the correlations between bacterial taxa and SCFAs were limited and sometimes discordant, for example, Prevotella, which is a producer of acetate (Koh et al. 2016), was decreased by aripiprazole administration. Therefore, the medications might have a different and direct influence on SCFA levels that are not mediated by the intestinal bacteria and still need to be teased apart.
The impact of psychotropic drugs on gut functionality is poorly understood. Thus, we assessed epithelial permeability in the small and large intestines and found that the three antidepressants escitalopram, venlafaxine and fluoxetine, together with the atypical antipsychotic aripiprazole, increased epithelial permeability in the ileum. Escitalopram, venlafaxine and fluoxetine share a common mechanism of action that is the blockade of the serotonin (5-HT) transporter (SERT) leading to increases in intrasynaptic 5-HT levels. SERT is not only present in the brain, it is also widely expressed on epithelial cells of the intestinal mucosa where it removes 5-HT from the interstitial space following release by enterochromaffin cells (Chen et al. 2001; Chen et al. 1998; Coates et al. 2004; Wade et al. 1996). 5-HT is involved in the control of intestinal permeability (Bischoff et al. 2009; Haub et al. 2010; Yamada et al. 2003); thus, it is plausible to speculate that the changes observed in ileal permeability might be dependent on direct effects of the three antidepressants on SERT. In addition to the antidepressants, also the atypical antipsychotic aripiprazole increased permeability in the ileum; however, this effect is not SERT-mediated and may be due to its effects on other 5-HT receptors. On the other hand, aripiprazole induced a concomitant shift in gut microbiota and future studies are needed to determine if there is a causal link between microbiota and permeability in this specific treatment group. Interestingly, the action of psychotropics on intestinal permeability was region-specific, with the colon being largely unaffected.
Interestingly, some studies have demonstrated that the gut microbiota of depressed (Kelly et al. 2016; Naseribafrouei et al. 2014) and bipolar (Evans et al. 2017) patients has an abnormal composition. This suggests that the gut-targeted effects of psychotropics might be part of the mechanism of action of these medications; however, this needs to be further investigated and confirmed. In this vein, future studies examining the impact of these drugs on microbiota composition in animal models of mental disorders and subsequently on human cohorts are warranted.
The functional consequences of drug-induced microbiome changes maybe at multiple levels including drug efficacy, kinetics, side effects and safety. Regarding side effects, weight gain has been the most studied in the context of the microbiome due to the relationship between microbiota composition and obesity (Torres-Fuentes et al. 2017) and appetite regulation (Cani et al. 2009; van de Wouw et al. 2017). Indeed, weight gain induced by antipsychotics (including olanzapine and risperidone) can be modulated by targeting the microbiome with antibiotics and prebiotics (Bahr et al. 2015a; Bahr et al. 2015b; Kao et al. 2018; Morgan et al. 2014). In a recent meta-analysis, all of the antidepressants tested here increased weight gain in a population cohort (Gafoor et al. 2018), suggesting a dissociation between their effects on microbiome and bodyweight per se.
In conclusion, the present study demonstrates that psychotropic medications differentially affect gut microbiota composition and intestinal permeability in healthy adult rats. Interestingly, such changes do not parallel with the impact of these drugs on in vitro isolated bacterial strains or on intestinal permeability per se. Together, these data highlight the importance of investigating the impact of drugs used for the treatment of psychiatric disorders on microbiota-gut-brain axis function.
References
Ackenheil M, Weber K (2004) Differing response to antipsychotic therapy in schizophrenia: pharmacogenomic aspects. Dialogues Clin Neurosci 6:71–77
Al-Harbi KS (2012) Treatment-resistant depression: therapeutic trends, challenges, and future directions. Patient Preference Adherence 6:369–388
Ariel L, Inbar S, Edut S, Richter-Levin G (2017) Fluoxetine treatment is effective in a rat model of childhood-induced post-traumatic stress disorder. Transl Psychiatry 7:1260
Ayaz M, Subhan F, Ahmed J, Khan A-u, Ullah F, Ullah I, Ali G, Syed N-i-H, Hussain S (2015a) Sertraline enhances the activity of antimicrobial agents against pathogens of clinical relevance. J Biol Res 22:4
Ayaz M, Subhan F, Ahmed J, Khan AU, Ullah F, Ullah I, Ali G, Syed NI, Hussain S (2015b) Sertraline enhances the activity of antimicrobial agents against pathogens of clinical relevance. J Biol Res (Thessalon) 22:4
Bahr SM, Tyler BC, Wooldridge N, Butcher BD, Burns TL, Teesch LM, Oltman CL, Azcarate-Peril MA, Kirby JR, Calarge CA (2015a) Use of the second-generation antipsychotic, risperidone, and secondary weight gain are associated with an altered gut microbiota in children. Transl Psychiatry 5:e652
Bahr SM, Weidemann BJ, Castro AN, Walsh JW, deLeon O, Burnett CML, Pearson NA, Murry DJ, Grobe JL, Kirby JR (2015b) Risperidone-induced weight gain is mediated through shifts in the gut microbiome and suppression of energy expenditure. EBioMedicine 2:1725–1734
Bercik P, Collins SM, Verdu EF (2012) Microbes and the gut-brain axis. Neurogastroenterology Motility 24:405–413
Beyazyüz M, Albayrak Y, Eğilmez OB, Albayrak N, Beyazyüz E (2013) Relationship between SSRIs and metabolic syndrome abnormalities in patients with generalized anxiety disorder: a prospective study. Psychiatry Investigation 10:148–154
Bischoff SC, Mailer R, Pabst O, Weier G, Sedlik W, Li Z, Chen JJ, Murphy DL, Gershon MD (2009) Role of serotonin in intestinal inflammation: knockout of serotonin reuptake transporter exacerbates 2,4,6-trinitrobenzene sulfonic acid colitis in mice. Am J Physiol Gastrointest Liver Physiol 296:G685–G695
Bohnert JA, Szymaniak-Vits M, Schuster S, Kern WV (2011a) Efflux inhibition by selective serotonin reuptake inhibitors in Escherichia coli. J Antimicrob Chemother 66:2057–2060
Bohnert JA, Szymaniak-Vits M, Schuster S, Kern WV (2011b) Efflux inhibition by selective serotonin reuptake inhibitors in Escherichia coli. J Antimicrob Chemother 66:2057–2060
Cani PD, Lecourt E, Dewulf EM, Sohet FM, Pachikian BD, Naslain D, De Backer F, Neyrinck AM, Delzenne NM (2009) Gut microbiota fermentation of prebiotics increases satietogenic and incretin gut peptide production with consequences for appetite sensation and glucose response after a meal. Am J Clin Nutr 90:1236–1243
Caparrós-Martín JA, Lareu RR, Ramsay JP, Peplies J, Reen FJ, Headlam HA, Ward NC, Croft KD, Newsholme P, Hughes JD, O’Gara F (2017) Statin therapy causes gut dysbiosis in mice through a PXR-dependent mechanism. Microbiome 5:95
Chen JX, Pan H, Rothman TP, Wade PR, Gershon MD (1998) Guinea pig 5-HT transporter: cloning, expression, distribution, and function in intestinal sensory reception. Am J Phys 275:G433–G448
Chen JJ, Li Z, Pan H, Murphy DL, Tamir H, Koepsell H, Gershon MD (2001) Maintenance of serotonin in the intestinal mucosa and ganglia of mice that lack the high-affinity serotonin transporter: abnormal intestinal motility and the expression of cation transporters. J Neurosci 21:6348–6361
Chen L, Wilson JE, Koenigsknecht MJ, Chou WC, Montgomery SA, Truax AD, Brickey WJ, Packey CD, Maharshak N, Matsushima GK, Plevy SE, Young VB, Sartor RB, Ting JP (2017) NLRP12 attenuates colon inflammation by maintaining colonic microbial diversity and promoting protective commensal bacterial growth. Nat Immunol 18:541–551
Coates MD, Mahoney CR, Linden DR, Sampson JE, Chen J, Blaszyk H, Crowell MD, Sharkey KA, Gershon MD, Mawe GM, Moses PL (2004) Molecular defects in mucosal serotonin content and decreased serotonin reuptake transporter in ulcerative colitis and irritable bowel syndrome. Gastroenterology 126:1657–1664
Coban AY, Tanriverdi Cayci Y, Keles Uludag S, Durupinar B (2009) Investigation of antibacterial activity of sertralin. Mikrobiyol Bul 43:651–656
Collins SM, Surette M, Bercik P (2012) The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol 10:735–742
Correll CU, Detraux J, De Lepeleire J, De Hert M (2015) Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiatry 14:119–136
Cryan JF, Dinan TG (2012a) Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci 13:701–712
Cryan JF, Dinan TG (2012b) Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci 13:701–712
Davey KJ, O’Mahony SM, Schellekens H, O’Sullivan O, Bienenstock J, Cotter PD, Dinan TG, Cryan JF (2012) Gender-dependent consequences of chronic olanzapine in the rat: effects on body weight, inflammatory, metabolic and microbiota parameters. Psychopharmacology 221:155–169
Davey KJ, Cotter PD, O'Sullivan O, Crispie F, Dinan TG, Cryan JF, O'Mahony SM (2013) Antipsychotics and the gut microbiome: olanzapine-induced metabolic dysfunction is attenuated by antibiotic administration in the rat. Transl Psychiatry 3:e309
De Vadder F, Kovatcheva-Datchary P, Goncalves D, Vinera J, Zitoun C, Duchampt A, Backhed F, Mithieux G (2014) Microbiota-generated metabolites promote metabolic benefits via gut-brain neural circuits. Cell 156:84–96
van de Wouw M, Schellekens H, Dinan TG, Cryan JF (2017) Microbiota-gut-brain axis: modulator of host metabolism and appetite. J Nutr 147:727–745
Dinan TG, Stanton C, Cryan JF (2013) Psychobiotics: a novel class of psychotropic. Biol Psychiatry 74:720–726
Dinan TG, Borre YE, Cryan JF (2014) Genomics of schizophrenia: time to consider the gut microbiome? Mol Psychiatry 19:1252–1257
Erny D, Hrabe de Angelis AL, Jaitin D, Wieghofer P, Staszewski O, David E, Keren-Shaul H, Mahlakoiv T, Jakobshagen K, Buch T, Schwierzeck V, Utermohlen O, Chun E, Garrett WS, McCoy KD, Diefenbach A, Staeheli P, Stecher B, Amit I, Prinz M (2015) Host microbiota constantly control maturation and function of microglia in the CNS. Nat Neurosci 18:965–977
Evans SJ, Bassis CM, Hein R, Assari S, Flowers SA, Kelly MB, Young VB, Ellingrod VE, McInnis MG (2017) The gut microbiome composition associates with bipolar disorder and illness severity. J Psychiatr Res 87:23–29
Falony G, Joossens M, Vieira-Silva S, Wang J, Darzi Y, Faust K, Kurilshikov A, Bonder MJ, Valles-Colomer M, Vandeputte D, Tito RY, Chaffron S, Rymenans L, Verspecht C, De Sutter L, Lima-Mendez G, D'Hoe K, Jonckheere K, Homola D, Garcia R, Tigchelaar EF, Eeckhaudt L, Fu J, Henckaerts L, Zhernakova A, Wijmenga C, Raes J (2016) Population-level analysis of gut microbiome variation. Science 352:560–564
Flowers SA, Evans SJ, Ward KM, McInnis MG, Ellingrod VL (2017a) Interaction between atypical antipsychotics and the gut microbiome in a bipolar disease cohort. Pharmacotherapy 37:261–267
Flowers SA, Evans SJ, Ward KM, McInnis MG, Ellingrod VL (2017b) Interaction between atypical antipsychotics and the gut microbiome in a bipolar disease cohort. Pharmacotherapy: J Human Pharmacology Drug Therapy 37:261–267
Forslund K, Hildebrand F, Nielsen T, Falony G, Le Chatelier E, Sunagawa S, Prifti E, Vieira-Silva S, Gudmundsdottir V, Krogh Pedersen H, Arumugam M, Kristiansen K, Yvonne Voigt A, Vestergaard H, Hercog R, Igor Costea P, Roat Kultima J, Li J, Jørgensen T, Levenez F, Dore J, Meta HIT c, Bjørn Nielsen H, Brunak S, Raes J, Hansen T, Wang J, Dusko Ehrlich S, Bork P, Pedersen O (2015) Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 528:262–266
Foster JA, McVey Neufeld K-A (2013) Gut–brain axis: how the microbiome influences anxiety and depression. Trends Neurosci 36:305–312
Freier TA, Beitz DC, Li L, Hartman PA (1994) Characterization of Eubacterium coprostanoligenes sp. nov., a cholesterol-reducing anaerobe. Int J Syst Bacteriol 44:137–142
Gafoor R, Booth HP, Gulliford MC (2018) Antidepressant utilisation and incidence of weight gain during 10 years’ follow-up: population based cohort study. BMJ 361:k1951
Golubeva AV, Joyce SA, Moloney G, Burokas A, Sherwin E, Arboleya S, Flynn I, Khochanskiy D, Moya-Pérez A, Peterson V, Rea K, Murphy K, Makarova O, Buravkov S, Hyland NP, Stanton C, Clarke G, Gahan CGM, Dinan TG, Cryan JF (2017) Microbiota-related changes in bile acid and tryptophan metabolism are associated with gastrointestinal dysfunction in a mouse model of autism. EBioMedicine 24:166–178
Goodrich JK, Davenport ER, Waters JL, Clark AG, Ley RE (2016) Cross-species comparisons of host genetic associations with the microbiome. Science 352:532–535
Grubbs FE (1950) Sample criteria for testing outlying observations. Ann Math Stat 21:27–58
Hatta K, Ito H (2014) Strategies for early non-response to antipsychotic drugs in the treatment of acute-phase schizophrenia. Clinical Psychopharmacology Neuroscience 12:1–7
Haub S, Ritze Y, Bergheim I, Pabst O, Gershon MD, Bischoff SC (2010) Enhancement of intestinal inflammation in mice lacking interleukin 10 by deletion of the serotonin reuptake transporter. Neurogastroenterol Motil 22(826–834):e229
Huuskonen J, Suuronen T, Nuutinen T, Kyrylenko S, Salminen A (2004) Regulation of microglial inflammatory response by sodium butyrate and short-chain fatty acids. Br J Pharmacol 141:874–880
Jiang H, Ling Z, Zhang Y, Mao H, Ma Z, Yin Y, Wang W, Tang W, Tan Z, Shi J, Li L, Ruan B (2015) Altered fecal microbiota composition in patients with major depressive disorder. Brain Behav Immun 48:186–194
Kaminska K, Rogoz Z (2016) The antidepressant- and anxiolytic-like effects following co-treatment with escitalopram and risperidone in rats. J Physiol Pharmacol 67:471–480
Kao AC-C, Spitzer S, Anthony DC, Lennox B, Burnet PWJ (2018) Prebiotic attenuation of olanzapine-induced weight gain in rats: analysis of central and peripheral biomarkers and gut microbiota. Transl Psychiatry 8:66
Karl JP, Margolis LM, Madslien EH, Murphy NE, Castellani JW, Gundersen Y, Hoke AV, Levangie MW, Kumar R, Chakraborty N, Gautam A, Hammamieh R, Martini S, Montain SJ, Pasiakos SM (2017) Changes in intestinal microbiota composition and metabolism coincide with increased intestinal permeability in young adults under prolonged physiological stress. Am J Physiol Gastrointest Liver Physiol 312:G559–g571
Kelly JR, Borre Y, O’ Brien C, Patterson E, El Aidy S, Deane J, Kennedy PJ, Beers S, Scott K, Moloney G, Hoban AE, Scott L, Fitzgerald P, Ross P, Stanton C, Clarke G, Cryan JF, Dinan TG (2016) Transferring the blues: depression-associated gut microbiota induces neurobehavioural changes in the rat. J Psychiatr Res 82:109–118
Kim KA, Gu W, Lee IA, Joh EH, Kim DH (2012) High fat diet-induced gut microbiota exacerbates inflammation and obesity in mice via the TLR4 signaling pathway. PLoS One 7:e47713
Kiraly DD, Walker DM, Calipari ES, Labonte B, Issler O, Pena CJ, Ribeiro EA, Russo SJ, Nestler EJ (2016) Alterations of the host microbiome affect behavioral responses to cocaine. Sci Rep 6:35455
Koh A, De Vadder F, Kovatcheva-Datchary P, Bäckhed F (2016) From dietary Fiber to host physiology: short-chain fatty acids as key bacterial metabolites. Cell 165:1332–1345
Kong F, Hua Y, Zeng B, Ning R, Li Y, Zhao J (2016) Gut microbiota signatures of longevity. Curr Biol 26:R832–R833
Kovatcheva-Datchary P, Nilsson A, Akrami R, Lee YS, De Vadder F, Arora T, Hallen A, Martens E, Björck I, Bäckhed F (2015) Dietary fiber-induced improvement in glucose metabolism is associated with increased abundance of Prevotella. Cell Metab 22:971–982
Li L, Buhman KK, Hartman PA, Beitz DC (1995) Hypocholesterolemic effect of Eubacterium coprostanoligenes ATCC 51222 in rabbits. Lett Appl Microbiol 20:137–140
Li L, Batt SM, Wannemuehler M, Dispirito A, Beitz DC (1998) Effect of feeding of a cholesterol-reducing bacterium, Eubacterium coprostanoligenes, to germ-free mice. Lab Anim Sci 48:253–255
Li M, Wang B, Sun X, Tang Y, Wei X, Ge B, Tang Y, Deng Y, He C, Yuan J, Li X (2017) Upregulation of intestinal barrier function in mice with DSS-induced colitis by a defined bacterial consortium is associated with expansion of IL-17A producing gamma delta T cells. Front Immunol 8:824
Ling Z, Li Z, Liu X, Cheng Y, Luo Y, Tong X, Yuan L, Wang Y, Sun J, Li L, Xiang C (2014) Altered fecal microbiota composition associated with food allergy in infants. Appl Environ Microbiol 80:2546–2554
López-Contreras BE, Morán-Ramos S, Villarruel-Vázquez R, Macías-Kauffer L, Villamil-Ramírez H, León-Mimila P, Vega-Badillo J, Sánchez-Muñoz F, Llanos-Moreno LE, Canizalez-Román A, Río-Navarro B, Ibarra-González I, Vela-Amieva M, Villarreal-Molina T, Ochoa-Leyva A, Aguilar-Salinas CA, Canizales-Quinteros S (2018) Composition of gut microbiota in obese and normal-weight Mexican school-age children and its association with metabolic traits. Pediatric Obesity 13:381–388
Luna RA, Foster JA (2015) Gut brain axis: diet microbiota interactions and implications for modulation of anxiety and depression. Curr Opin Biotechnol 32:35–41
Lyons L, ElBeltagy M, Bennett G, Wigmore P (2012) Fluoxetine counteracts the cognitive and cellular effects of 5-fluorouracil in the rat hippocampus by a mechanism of prevention rather than recovery. PLoS One 7:e30010
Maier L, Pruteanu M, Kuhn M, Zeller G, Telzerow A, Anderson EE, Brochado AR, Fernandez KC, Dose H, Mori H, Patil KR, Bork P, Typas A (2018) Extensive impact of non-antibiotic drugs on human gut bacteria. Nature 555:623–628
Mayer EA, Knight R, Mazmanian SK, Cryan JF, Tillisch K (2014) Gut microbes and the brain: paradigm shift in neuroscience. J Neurosci 34:15490–15496
Mayer EA, Tillisch K, Gupta A (2015) Gut/brain axis and the microbiota. J Clin Invest 125:926–938
Monti B, Gatta V, Piretti F, Raffaelli SS, Virgili M, Contestabile A (2010) Valproic acid is neuroprotective in the rotenone rat model of Parkinson’s disease: involvement of alpha-synuclein. Neurotox Res 17:130–141
Morgan AP, Crowley JJ, Nonneman RJ, Quackenbush CR, Miller CN, Ryan AK, Bogue MA, Paredes SH, Yourstone S, Carroll IM, Kawula TH, Bower MA, Sartor RB, Sullivan PF (2014) The antipsychotic olanzapine interacts with the gut microbiome to cause weight gain in mouse. PLoS One 9:e115225
Morrison DJ, Preston T (2016) Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microbes 7:189–200
Munoz-Bellido JL, Munoz-Criado S, Garcia-Rodriguez JA (1996) In-vitro activity of psychiatric drugs against Corynebacterium urealyticum (Corynebacterium group D2). J Antimicrob Chemother 37:1005–1009
Munoz-Bellido JL, Munoz-Criado S, Garcia-Rodriguez JA (2000) Antimicrobial activity of psychotropic drugs: selective serotonin reuptake inhibitors. Int J Antimicrob Agents 14:177–180
den Besten G, van Eunen K, Groen AK, Venema K, Reijngoud DJ, Bakker BM (2013) The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res 54:2325–2340
Naseribafrouei A, Hestad K, Avershina E, Sekelja M, Linløkken A, Wilson R, Rudi K (2014) Correlation between the human fecal microbiota and depression. Neurogastroenterology Motility 26:1155–1162
Nelson JC (1998) Treatment of antidepressant nonresponders: augmentation or switch? J Clin Psychiatry 59(Suppl 15):35–41
O’Leary OF, O’Connor RM, Cryan JF (2012) Lithium-induced effects on adult hippocampal neurogenesis are topographically segregated along the dorso-ventral axis of stressed mice. Neuropharmacology 62:247–255
O’Mahony SM, Felice VD, Nally K, Savignac HM, Claesson MJ, Scully P, Woznicki J, Hyland NP, Shanahan F, Quigley EM, Marchesi JR, O’Toole PW, Dinan TG, Cryan JF (2014) Disturbance of the gut microbiota in early-life selectively affects visceral pain in adulthood without impacting cognitive or anxiety-related behaviors in male rats. Neuroscience 277:885–901
Olguner Eker Ö, ÖZsoy S, Eker B, DoĞAn H (2017) Metabolic effects of antidepressant treatment. Archives Neuropsychiatry 54:49–56
Olivares, M., Neef, A., Castillejo, G., Palma, G. D., Varea, V., Capilla, A., Palau, F., Nova, E., Marcos, A., Polanco, I., Ribes-Koninckx, C., Ortigosa, L., Izquierdo, L., Sanz, Y., 2014. The HLA-DQ2 genotype selects for early intestinal microbiota composition in infants at high risk of developing coeliac disease. Gut
Ott B, Skurk T, Hastreiter L, Lagkouvardos I, Fischer S, Büttner J, Kellerer T, Clavel T, Rychlik M, Haller D, Hauner H (2017) Effect of caloric restriction on gut permeability, inflammation markers, and fecal microbiota in obese women. Sci Rep 7:11955
Paquin-Proulx D, Ching C, Vujkovic-Cvijin I, Fadrosh D, Loh L, Huang Y, Somsouk M, Lynch SV, Hunt PW, Nixon DF, SenGupta D (2016) Bacteroides are associated with GALT iNKT cell function and reduction of microbial translocation in HIV-1 infection. Mucosal Immunol 10:69
Raman M, Ahmed I, Gillevet PM, Probert CS, Ratcliffe NM, Smith S, Greenwood R, Sikaroodi M, Lam V, Crotty P, Bailey J, Myers RP, Rioux KP (2013) Fecal microbiome and volatile organic compound metabolome in obese humans with nonalcoholic fatty liver disease. Clinical Gastroenterology Hepatology 11 e863:868–875
Rath HC, Herfarth HH, Ikeda JS, Grenther WB, Hamm TE Jr, Balish E, Taurog JD, Hammer RE, Wilson KH, Sartor RB (1996) Normal luminal bacteria, especially Bacteroides species, mediate chronic colitis, gastritis, and arthritis in HLA-B27/human beta2 microglobulin transgenic rats. J Clin Invest 98:945–953
Ren D, Li L, Schwabacher AW, Young JW, Beitz DC (1996) Mechanism of cholesterol reduction to coprostanol by Eubacterium coprostanoligenes ATCC 51222. Steroids 61:33–40
Reynolds GP, Kirk SL (2010) Metabolic side effects of antipsychotic drug treatment – pharmacological mechanisms. Pharmacol Ther 125:169–179
Schroeder FA, Lin CL, Crusio WE, Akbarian S (2007) Antidepressant-like effects of the histone deacetylase inhibitor, sodium butyrate, in the mouse. Biol Psychiatry 62:55–64
Schubert AM, Rogers MA, Ring C, Mogle J, Petrosino JP, Young VB, Aronoff DM, Schloss PD (2014) Microbiome data distinguish patients with Clostridium difficile infection and non-C. difficile-associated diarrhea from healthy controls. MBio 5:e01021–e01014
Schwarz E, Maukonen J, Hyytiäinen T, Kieseppä T, Orešič M, Sabunciyan S, Mantere O, Saarela M, Yolken R, Suvisaari J (2017) Analysis of microbiota in first episode psychosis identifies preliminary associations with symptom severity and treatment response. Schizophr Res 192:398–403
Scott KA, Ida M, Peterson VL, Prenderville JA, Moloney GM, Izumo T, Murphy K, Murphy A, Ross RP, Stanton C, Dinan TG, Cryan JF (2017) Revisiting Metchnikoff: age-related alterations in microbiota-gut-brain axis in the mouse. Brain Behav Immun 65:20–32
Segnitz N, Schmitt A, Gebicke-Harter PJ, Zink M (2009) Differential expression of glutamate transporter genes after chronic oral treatment with aripiprazole in rats. Neurochem Int 55:619–628
Sogaard B, Mengel H, Rao N, Larsen F (2005) The pharmacokinetics of escitalopram after oral and intravenous administration of single and multiple doses to healthy subjects. J Clin Pharmacol 45:1400–1406
Thursby E, Juge N (2017) Introduction to the human gut microbiota. Biochem J 474:1823–1836
Torres-Fuentes C, Schellekens H, Dinan TG, Cryan JF (2017) The microbiota–gut–brain axis in obesity. Lancet Gastroenterology Hepatology 2:747–756
Tschoner A, Engl J, Laimer M, Kaser S, Rettenbacher M, Fleischhacker WW, Patsch JR, Ebenbichler CF (2007) Metabolic side effects of antipsychotic medication. Int J Clin Pract 61:1356–1370
Ulluwishewa D, Anderson RC, McNabb WC, Moughan PJ, Wells JM, Roy NC (2011) Regulation of tight junction permeability by intestinal bacteria and dietary components. J Nutr 141:769–776
Vidal R, Valdizan E, Vilaró M, Pazos A, Castro E (2010) Reduced signal transduction by 5-HT4 receptors after long-term venlafaxine treatment in rats. Br J Pharmacol 161:695–706
Wade PR, Chen J, Jaffe B, Kassem IS, Blakely RD, Gershon MD (1996) Localization and function of a 5-HT transporter in crypt epithelia of the gastrointestinal tract. J Neurosci 16:2352–2364
Walter J (2008) Ecological role of lactobacilli in the gastrointestinal tract: implications for fundamental and biomedical research. Appl Environ Microbiol 74:4985–4996
Watase K, Gatchel JR, Sun Y, Emamian E, Atkinson R, Richman R, Mizusawa H, Orr HT, Shaw C, Zoghbi HY (2007) Lithium therapy improves neurological function and hippocampal dendritic arborization in a spinocerebellar ataxia type 1 mouse model. PLoS Med 4:e182
World Health Organization, 2017. Depression and other common mental disorders: global health estimates. Geneva
Wu H, Esteve E, Tremaroli V, Khan MT, Caesar R, Mannerås-Holm L, Ståhlman M, Olsson LM, Serino M, Planas-Fèlix M, Xifra G, Mercader JM, Torrents D, Burcelin R, Ricart W, Perkins R, Fernàndez-Real JM, Bäckhed F (2017) Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nat Med 23:850–858
Xie, Y., Zhou, G., Wang, C., Xu, X., Li, C., 2018. Temporal changes in gut microbiota and signaling molecules of the gut-brain axis in mice fed meat protein diets. bioRxiv
Yamada T, Inui A, Hayashi N, Fujimura M, Fujimiya M (2003) Serotonin stimulates endotoxin translocation via 5-HT3 receptors in the rat ileum. Am J Physiol Gastrointest Liver Physiol 284:G782–G788
Zhan G, Yang N, Li S, Huang N, Fang X, Zhang J, Zhu B, Yang L, Yang C, Luo A (2018) Abnormal gut microbiota composition contributes to cognitive dysfunction in SAMP8 mice. Aging (Albany NY) 10:1257–1267
Zheng P, Zeng B, Zhou C, Liu M, Fang Z, Xu X, Zeng L, Chen J, Fan S, Du X, Zhang X, Yang D, Yang Y, Meng H, Li W, Melgiri ND, Licinio J, Wei H, Xie P (2016) Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host's metabolism. Mol Psychiatry 21:786–796
Acknowledgments
The authors gratefully acknowledge Pat Fitzgerald, Gonzalo Rabasa, Karen Scott, Gilliard Lach, Gerry Moloney, Anna Golubeva and Kieran Rea for their invaluable support. We would also like to acknowledge Wiley Barton for his assistance in R scripts and the Teagasc Sequencing Facility, Dr. Paul Cotter, Dr. Fiona Crispie and Ms. Laura Finnegan.
Funding
APC Microbiome Ireland is a research centre funded by Science Foundation Ireland (SFI), through the Irish Government’s National Development Plan (grant no. 12/RC/2273). JFC, TGD and CS have research funding from Dupont Nutrition Biosciences APS, Cremo SA, Alkermes Inc., 4D Pharma PLC, Mead Johnson Nutrition, Nutricia Danone, Suntory Wellness. JFC, TGD, CS and GC have spoken at meetings sponsored by food and pharmaceutical companies.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Experiments were conducted in accordance with the European Directive 2010/63/EU. Approval by the Animal Experimentation Ethics Committee of University College Cork was obtained before commencement of all animal-related experiments.
Conflict of interest
All other authors declare that they have no conflict of interest.
Additional information
This article belongs to a Special Issue on Microbiome in Psychiatry & Psychopharmacology.
Rights and permissions
About this article
Cite this article
Cussotto, S., Strain, C.R., Fouhy, F. et al. Differential effects of psychotropic drugs on microbiome composition and gastrointestinal function. Psychopharmacology 236, 1671–1685 (2019). https://doi.org/10.1007/s00213-018-5006-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-018-5006-5