Abstract
Objective
A considerable body of research links cognitive function to dopaminergic transmission in the prefrontal cortex, but less is known about cognition in relation to striatal dopamine D2/3 receptors in unmedicated patients with psychosis.
Methods
We investigated this association by obtaining PET recordings with the high-affinity D2/3 antagonist ligand [18F] fallypride in 15 medication-free patients with schizophrenia and 11 healthy controls. On the day of PET scanning, we undertook comprehensive neuropsychological testing and assessment of psychopathology using the Positive and Negative Syndrome Scale (PANSS).
Results
The patients’ performance in cognitive tests was significantly impaired in almost all domains. Irrespective of medication history, the mean [18F] fallypride binding potential (BPND) in the patient group tended to be globally 5–10% higher than that of the control group, but without reaching significance in any brain region. There were significant positive correlations between individual patient performance in the Trail Making Test (TMT(A) and TMT(B)) and Digit-Symbol-Substitution-Test with regional [18F] fallypride BPND, which remained significant after Bonferroni correction for the TMT(A) in caudate nucleus (CN) and for the TMT(B) in CN and putamen. No such correlations were evident in the control group.
Discussion
The association between better cognitive performance and greater BPND in schizophrenia patients may imply that relatively lower receptor occupancy by endogenous dopamine favors better sparing of cognitive function. Absence of comparable correlations in healthy controls could indicate a greater involvement of signaling at dopamine D2/3 receptors in certain cognitive functions in schizophrenia patients than in healthy controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Impairments in a wide range of cognitive domains are coming to be recognized to constitute a core feature of schizophrenia (Green et al. 2004; Keefe et al. 2007). Indeed, impairments of memory and executive function are present in nearly all patients with schizophrenia (Keefe and Harvey 2012). While antipsychotic medications can relieve the positive symptoms of schizophrenia, cognitive impairments are often refractory to available treatments (Gray and Roth 2007). This appears to be of particular clinical importance, since the severity of cognitive impairments in schizophrenia is a better predictor of poor functional outcome than are indices from any other psychopathology domain (Green and Harvey 2014). Ref. "Green et al. 2004" is cited in the body but its bibliographic information is missing. Kindly provide its bibliographic information in the list.Green MF, Nuechterlein KH, Gold JM, Barch DM, Cohen J, Essock S, Fenton WS, Frese F, Goldberg TE, Heaton RK, Keefe RS, Kern RS, Kraemer H, Stover E, Weinberger DR, Zalcman S, Marder SR (2004) Approaching a consensus cognitive battery for clinical trials in schizophrenia: the NIMH-MATRICS conference to select cognitive domains and test criteria. Biol Psychiatry 56(5):301-7
Investigations over the past decades link the cognitive impairments in schizophrenia to dysfunction of several neurotransmitter systems, including brain dopamine (Tamminga 2006). According to an influential model, cognitive impairments of schizophrenia arise in relation to a biphasic dysregulation of dopaminergic signaling, with overactivity of mesolimbic pathways and underactivity of mesocortical dopamine pathways (Buchanan et al. 2007). Recurrent loops connecting striatum with the prefrontal cortex are heavily modulated by dopaminergic neurotransmission (Carter et al. 2001; Helmich et al. 2010; Robinson et al. 2012). While there are well-established findings of a relationship between D1-mediated dopaminergic hypofunction in the prefrontal cortex with perturbation of certain cognitive domains (Goldman-Rakic et al. 2000; Minzenberg et al. 2009; Takahashi 2013), less is known about specific contributions of dopamine D2/3 receptor-mediated striatal neurotransmission in cognitive impairments in schizophrenia.
Results of several molecular imaging investigations by positron emission tomography (PET) in healthy volunteers show associations between cognition and dopaminergic neurotransmission in striatum. Thus, Volkow and colleagues showed a robust positive correlation between neurocognitive test performance and striatal D2/3 receptor availability (measured by [11C]raclopride-PET) in a group of 30 healthy volunteers, which remained significant after controlling for age effects (Volkow et al. 1998). In another PET study of 11 healthy participants, Backman et al. reported that higher D2/3 availability (measured as higher (in vivo) dopamine receptor binding potentials (BPND)) was a better predictor for cognitive performance than was age (Backman et al. 2000). Furthermore, higher D2/3 binding in the left caudate nucleus (CN) and putamen in a group of 30 healthy post-menopausal women predicted better executive function, indicated by performance of the Tower of London test of spatial planning (Reeves et al. 2005). Two other groups reported significant positive correlations between the performance in several cognitive tasks for executive functions and the striatal D2/3 receptor availability measured with [11C]raclopride-PET (Lawrence et al. 1998; Pavese et al. 2003). More recently, [11C]raclopride binding in CN proved to correlate with scores in a test of episodic memory of a large series of healthy elderly adults (Nyberg et al. 2016). Thus, there is a general relationship between striatal dopamine D2/3 receptor availability and executive function in healthy subjects across a wide range of ages.
In contrast to these findings in healthy volunteers, a consistent relationship between striatal dopaminergic markers and cognitive dysfunctions typically seen in schizophrenia is less clearly established. Meta-analysis of many molecular imaging studies reveals a hyperdopaminergic state in the striatum of patients with schizophrenia (Howes et al. 2012). Further, striatal dysfunction underlies particular aspects of perturbed cognition in schizophrenia (Simpson et al. 2010). One study showed a significant negative correlation between striatal dopamine transporter availability and cognitive symptoms, as measured by the PANSS cognitive component, in a group of ten schizophrenia patients (Yoder et al. 2004). In a single photon emission-computed tomography (SPECT) study of striatal dopamine D2/3 receptors, striatal binding in schizophrenia patients correlated with fine motor function and with performance in attentional tests (Yang et al. 2004a). However, these investigations were all performed in patients with uninterrupted antipsychotic medication. To avoid the confounding effects of recent use of antipsychotic medications, we undertook an [18F]fallypride PET study of dopamine D2/3 receptors in a group of healthy volunteers and in patients who had been either drug-naïve or medication-free for at least 6 months prior to scanning. We used [18F]fallypride as a tracer due to its high D2/3 receptor affinity, long physical half-life (109 min), and suitability for the quantification of striatal and extra-striatal D2/3 receptors during a single PET session (Mukherjee et al. 1995; Vernaleken et al. 2011). We then undertook an exploratory investigation of relationships between individual cognitive function and PET findings in the patient and control groups, testing the hypothesis that greater D2/3 receptor availability in striatum correlates with better performance in tests of executive function in healthy controls, and likewise in unmedicated patients with schizophrenia.
Methods
This study was approved by all responsible authorities: The Federal Institute for Pharmaceuticals and Medical Products (Bundesamt für Arzneimittel (BfArM), Bonn), the local ethics committee of the Medical Faculty of the RWTH Aachen University (Aachen, Germany), and the German national radiation safety authorities (Bundesamt für Strahlenschutz (BfS)). The examination procedure was explained in detail to all subjects, who afterwards signed a written informed consent. All investigations were performed in the Department of Psychiatry, Psychotherapy and Psychosomatics and the Department of Nuclear Medicine of the RWTH Aachen University, Germany.
Subjects
The patient group consisted of 15 patients with schizophrenia (ten males and five females of mean age 30.2 years (SD 10.9; range 18–52 years), being medication-free for at least 6 months prior to PET scanning (N = 9) or drug-naïve (N = 6). The mean duration of illness was 2 years (SD 5; range 0.5 to 7 years). The six drug-naïve patients were diagnosed with a first episode of schizophrenia (mean duration of symptoms: 6 to 9 months). A group of 11 healthy volunteers (seven males and four females) of mean age 30.6 years (SD 9.6; range 19–48 years) matched for level of education served as a control group.
Inclusion criteria consisted of normal findings in standard laboratory parameters (small blood count, coagulation factors, electrolytes, liver values, creatine kinase and TSH), electrocardiogram and electroencephalogram, as well as negative urine screening for illegal drugs (amphetamines, barbiturates, cocaine, marijuana, opiates, and methadone using a standard pharmacy test) at interview and on the day of PET scanning. For females, a negative pregnancy test and reliable contraception was required, along with a confirmatory negative pregnancy test on the day of PET scanning. A further prerequisite for inclusion was provision of freely given, signed informed consent. In the case of patients, physicians not involved in the study had vetted the participants’ capacity to give informed consent. Prior to inclusion, all subjects were carefully examined for presence of any exclusion criterion (any relevant DSM-IV axis I disease other than schizophrenia or schizoaffective disorder, current use of psychotropic drugs of abuse, or any other relevant past or present serious medical or neurological diseases).
All subjects received a small compensation for their participation in the form of vouchers to a value of 100 Euros. This research was conducted in strict accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its most recent revision. Detailed demographic and psychopathological data of the included subjects are given in Table 1.
Study design
The neurocognitive assessment and the clinical examination took place on the same day as the [18F]fallypride PET scan. In order to evaluate some cognitive domains known to be impaired in schizophrenia (Nuechterlein et al. 2008), the following four tests were administered to all subject:
-
(1)
Trail-Making Test (TMT(A/B)) (Reitan 1958), a widely used test of high sensitivity, but somewhat low specificity (Kortte et al. 2002), which consists of two parts. In part A, the participant is instructed to draw a line connecting 25 numbers consecutively as quickly as possible. In part B, the participant alternates between consecutive numbers and letters. Performance of A and B is scored as the time taken to complete each trial without error. The TMT(A/B) reflects a combination of several cognitive functions, measuring complex visual scanning with a motor component, motor speed, and agility. Part B, which entails a greater cognitive burden, is particularly sensitive to deficits in cognitive flexibility and executive function (Kortte et al. 2002).
-
(2)
Digit-Symbol-Substitution Task (DSST) a subtest of the Wechsler Intelligence Scale (Wechsler 1997) primarily quantifies the speed of mental processing. Participants are instructed to pair symbols to numbers and write them into blank squares as quickly as possible, while referring to a digit-symbol key presented at the top of the examination sheet. The DSST score is the number of correct substitutions made in 90 s.
-
(3)
Verbal Fluency Task (“Regensburger Wortfluessigkeitstest”; RWT) (Harth et al. 2004) is a verbal fluency test standardized for German language. The test consists of four parts, designed to assess phonemic and semantic fluency and the ability for category change. The observation time for each part is 1 min.
-
(4)
Letter-Number Span (Gold et al. 1997) a test of working memory performance in which the examiner presents a series of increasingly longer sequences of intermixed numbers and letters (2 to 7 stimuli) at a rate of 1/s. After each sequence presentation, the participant is asked to first repeat the numbers in ascending order and then the letters in alphabetical order. Four trials are presented for each sequence length; the test is concluded when the subject fails four consecutive trials of the same length. One point is scored for each correctly repeated sequence, to a maximum of 24 points.
Radiochemistry and data acquisition
The radiosynthesis of [18F]fallypride, as described in detail earlier (Vernaleken et al. 2013), is obtained by a high-yield modification of the synthesis method for [18F]desmethoxyfallypride (Gründer et al. 2003). A high-resolution Siemens ECAT EXACT 922/47 whole-body PET scanner (Siemens AG, Germany) was used to acquire dynamic emission images in 3D-mode (field-of-view 16.2 cm; 47 planes; full width a half maximum (FWHM) axial 4.6 mm, in-plane: 6.0 mm). The standard procedure for the dynamic data acquisition comprised 39 sequential time frames (3 × 20 s, 3 × 1 min, 3 × 2 min, 3 × 3 min, 21 × 5 min, 2 × 8 min, 4 × 10 min) to a total of 180 min. A 15-min transmission scan using a 68Ge source performed prior to tracer administration enabled the subsequent attenuation correction of the emission sequence. A vacuum mask was used for comfortable immobilization of the subject’s head during the scanning procedure. We applied fiducial felt-tip marks to the head to monitor for excessive head displacement between the transmission scan and the tracer administration. A mean of 213 ± 30 MBq [18F]fallypride was injected as a slow bolus to the cubital vein in the non-dominant arm (patients 214 ± 31 MBq, controls: 213 ± 30 MBq; p = 0.967 paired t test). The specific activity was 1483 ± 1350 (range 131–5022) GBq/μmol (patients 1471 ± 1574 GBq/μmol; controls 1495 ± 1420 GBq/μmol; p = 0.89; paired t test), corresponding in each case to < 1 nmol mass injected. The injected mass did not significantly correlate with the measured BPND in any region, neither in patients nor in healthy volunteers.
Image and data analysis
We applied a Hanning filter (4 mm FWHM) and filtered back-projection for the reconstruction of emission frames. We then applied a nonlinear spatial normalization of the summed dynamic baseline scan to a template in the MNI space using the MEDx software (v3.43; Medical Numerics, USA) with six parameters after a frame-by-frame motion-correction. Next, we applied anatomic templates as polygonal volumes of interest (VOIs) for extraction of time-activity curves (TACs) from cerebellum, and bilateral putamen (PUT), caudate nucleus (CN), thalamus (THAL), and inferior temporal gyrus (ITG). These VOIs are representative of the main brain regions with reliably quantifiable [18F]fallypride binding and have been used in several of our previous investigations (e.g., (Gründer et al. 2008; Vernaleken et al. 2010, 2013)). The [18F]fallypride binding potentials (BPND) of the VOIs were calculated using the simplified reference tissue model (SRTM), with cerebellum serving as the reference region (Lammertsma and Hume 1996). While there are traces of D2/3 receptor binding in cerebellum (0.13% of putamen binding; (Hall et al. 1996)), its use as a reference region for calculating [18F]fallypride BPND in our VOIs is a widely established approach (Siessmeier et al. 2005; Vernaleken et al. 2011; Ishibashi et al. 2013; Cumming et al. 2013). We cannot completely exclude the possibility that our BPND values were slightly underestimated because of traces of specific binding in the cerebellum. However, the low magnitude of this binding (Langer et al. 2017) predicts low bias in striatum, albeit with relatively higher bias in the cerebral cortex, where specific binding is also low. Further, the strong correlation (correlation coefficient greater than 0.99 with a slope of 1.0) between regional BPNDs obtained with the STRM and BPNDs obtained with metabolite-corrected plasma input function (Kessler et al. 2005) also suggests that the bias should be consistently less than 5% for our reference tissue method (Olsson et al. 2004; Gründer et al. 2008). All participants were under medical supervision during the PET recording and afterwards for at least an additional 2 h. None of the included subjects dropped out or experienced any noteworthy adverse events during the PET examination.
Statistical analysis
We used the SPSS statistical analysis software package (SPSS Version 20 for Windows; IBM, New York, NY, USA) for all analyses. The BPND-values calculated in the VOIs and scores from the neuropsychological tests were compared between the groups using a non-parametric Mann-Whitney test, in keeping with the small sample size. Effect sizes (ES) were calculated for each comparison using the open source software G*Power (Faul et al. 2007). In the next step, we carried out an exploratory regression analysis testing for group-wise relationships between regional [18F]fallypride BPND and cognitive test scores. Due to heteroscedasticity of most of the measured parameters, we used the Spearman rank-order correlation. The significance level was set to 0.05. Bonferroni correction was applied to accommodate problems due to multiple testing.
Results
D2/3 receptor availability
Mean BPND-values measured in the VOIs for the patient and control groups are presented in Table 2; coefficients of variation were less than 27% in all four brain regions considered. Receptor availability was 5–10% higher in the patient group for all VOIs examined, but without reaching statistical significance. In Table 2, we separately depict mean BPND-values measured in the two patient subgroups according to disease stage (six de novo, drug-naïve patients and nine previously medicated patients, drug-free for at least 6 months at the time of scanning). The mean BPND-values did not differ between subgroups in any of the four regions (p < 0.05 for all regions; no Bonferroni correction).
There were no significant correlations between regional BPND and age (patients: ITG r = − 0.27, p = 0.33; THAL r = 0.36, p = 0.19; CN r = − 0.43, p = 0.11; PUT r = − 0.46, p = 0.1; controls: ITG r = 0.14, p = 0.68; THAL r = 0.27, p = 0.42; CN r = − 0.29; p = 0.4; PUT r = − 0.09, p = 0.79), nor were there any associations with illness duration in the patient group (ITG r = − 0.21, p = 0.46; THAL r = 0.05, p = 0.87; CN r = − 0.19, p = 0.50; PUT r = 0.02, p = 0.94).
Cognitive performance
Patients performed worse than controls in almost all neuropsychological tests (Table 3). Even after Bonferroni correction (for a total of eight subtests of four tests), the results in the patient group were significantly worse for the following tests: (1) TMT–TMT(A); 38.3 ± 12.6 s (patients) versus 25.1 ± 7.7 s (controls; p = 0.003); (2) TMT(B); 87.1 ± 27.3 s (patients) versus 56.5 ± 19.3 s (controls; p = 0.005); (3) DSST; 42.7 ± 10.9 (patients) versus 60.6 ± 14.7 (controls; p = 0.003); and (4) the verbal-fluency task for phonemic fluency; 8.1 ± 3.8 (patients) versus 13.2 ± 3.8 (controls; p = 0.003), semantic fluency; 16.3 ± 6.3 (patients) versus 23.7 ± 4.8 (controls; p = 0.002) and semantic category change; 11.5 ± 3.8 (patients) versus 16.7 ± 3.7 (controls; p = 0.002). We saw no evidence for differences in cognitive performance between the medication-naïve and previously medicated subgroups (Table 3).
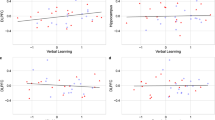
Further, we observed in the patient group significant negative correlations between the times needed to perform the TMT(A) and TMT(B) tasks and the regional [18F]fallypride BPND, irrespective of medication history (Table 4). These correlations were particularly strong in the bilateral CN (for TMT(A): left CN r = − 0.83, p < 0.001; right NC r = − 0.86, p < 0.001; for TMT(B): left CN r = − 0.81, p < 0.001; right CN r = − 0.85, p < 0.001) and in bilateral putamen (for TMT(A): left putamen: r = − 0.84, p < 0.001, right putamen: r = − 0.81, p < 0.001; for TMT(B): left putamen: r = − 0.85, p < 0.001; right putamen r = − 0.83, p < 0.001), remaining significant also after Bonferroni correction. Conversely, the DSST scores correlated positively with the [18F]fallypride BPND in bilateral CN (left CN r = 0.62, p = 0.014; right CN r = 0.57; p = 0.028) and at trend-level in bilateral putamen (left putamen r = 0.51, p = 0.056; right putamen r = 0.47; p = 0.079), but these associations were not strong enough to survive Bonferroni correction. TMT(B) scores in the patients correlated significant with [18F]fallypride BPND in the ITG (r = − 0.75; p = 0.001), but not in THAL (r = − 0.44, p = 0.1). There were no significant correlations between cognitive test scores and regional [18F]fallypride BPND in the control group.
Discussion
This exploratory PET study aimed to contribute to a better understanding of the role of striatal dopaminergic neurotransmission in the cognitive impairments in schizophrenia. In previous molecular imaging studies, such relationships have emerged in healthy volunteers, but corresponding findings in schizophrenia patients are equivocal, and likely to have been confounded by medication. Thus, we tested for associations between cognitive performance and the D2/3 receptor availability in striatum and in selected extrastriatal regions using the highly affine radioligand [18F]fallypride, in groups of 15 schizophrenia patients (of whom six were medication naïve and nine had been medication free for at least 6 months) and in 11 demographically matched healthy volunteers.
Our study revealed two main findings: First, we observed a very strong association between performance in a test of executive function (TMT) and the D2/3 receptor availability in striatum (CN and putamen), and the ITG cortex (but not THAL), irrespective of medication history in the schizophrenia patients. Second, we did not find corresponding relationships in the healthy control group, in whom D2/3 receptor availability globally (but not statistically significantly) tended to be 5–10% lower.
Direct correlations between executive functions and the dopamine D2/3 receptor availability in CN and putamen have been reported previously in healthy controls (Volkow et al. 1998; Backman et al. 2000; Reeves et al. 2005), but have not hitherto been investigated in medication-free schizophrenia patients. In our study, higher D2/3 receptor availability in striatum of the patient group was associated with better performance (shorter performance times) in TMT(A) and TMT(B). Thus, relatively high dopamine D2/3 receptor availability especially in striatum mitigates against aspects of cognitive dysfunction in these patients with schizophrenia. In general, observations of dopamine D2/3 receptor availability for benzamide radioligands such as [18F]fallypride are formally ambiguous, as the measured BPND is reduced to some unknown extent by competition from endogenous dopamine (Morris et al. 2010). Insofar as higher D2/3 availability favors cognitive performance in our patient group, this may imply that it is the dynamic range of dopamine signaling that determines cognitive flexibility. In this conjectural scenario, those patients with lower basal occupancy by endogenous dopamine in striatum, as indicated by relatively higher BPND, can accommodate a more robust dopaminergic response to a cognitive challenge. In support of this model, Rajji and colleagues reported a strong association between improving cognitive performance and increasing D2/3 receptor availability in the whole striatum to [11C]-raclopride PET in a geriatric sample followed after a dose reduction of antipsychotic medication (Rajji et al. 2017).
Further, in our patient group, the dopamine D2/3 receptor availability in the cortical region ITG correlated with performance of the TMT(B) test. Due to its more complex design, the TMT(B) measures not only just visuomotor abilities, but also cognitive flexibility, set-shifting, and inhibition (Arbuthnott and Frank 2000; Kortte et al. 2002). Results of most functional neuroimaging studies emphasize the decisive role of the prefrontal cortex for the performance in TMT(B) (Allen et al. 2011), although some findings link TMT(B) scores directly with activation (Jacobson et al. 2011), perfusion (Horacek et al. 2006), and cortical thickness in the ITG (MacPherson et al. 2017). Furthermore, the ITG is implicated in several complex cognitive processes (Cabeza and Nyberg 2000), including visual perception (Ishai et al. 1999; Herath et al. 2001), which is a factor in TMT performance. However, it remains unclear whether our isolated finding speaks to the function of the ITG or rather sui generis for dopamine D2/3 receptors in other cortical regions. In this regard, other molecular imaging results point to an association between D2/3 availability in frontal regions and set shifting in antipsychotic-naïve, first episode schizophrenia patients (Fagerlund et al. 2013).
Surprisingly, we failed to detect correlations between cognitive performance and [18F]fallypride BPND in our healthy control group. This could imply a certain robustness of cognition to individual differences in D2/3 availability in healthy controls. Indeed, a moderate reduction of available D2/3 receptors by a pharmacological blockade with sulpiride (17% occupancy to [11C]raclopride-PET) was without effect on cognition of healthy volunteers, whereas a further receptor blockade (28% occupancy) induced some cognitive impairments (Mehta et al. 2008). Similar to our findings, another group reported a significant linear correlation between D2/3 availability in frontal cortex and some cognitive domains in schizophrenia patients, but not in healthy controls (Fagerlund et al. 2013). One possible interpretation of such discrepancies could be that D2/3 receptor availability has a greater impact on certain cognitive functions in schizophrenia patients than in healthy controls. Indeed, some previous investigations postulated that behavioral flexibility is supported by cooperative actions of D1- and D2-like receptors (Floresco and Magyar 2006), whereby D2/3 receptor activation may mediate behavioral adjustment in novel situations, while concomitant D1 receptor activation limits the cognitive focus and stabilizes the existing strategy (Seamans and Yang 2004; Floresco and Magyar 2006). Thus, the rigid association between some cognitive functions and D2/3 receptor availability seen in our patients may translate to reduced behavioral and cognitive flexibility, which are among the most prevalent cognitive deficits associated with schizophrenia (Floresco et al. 2009).
In this study, we recapitulate our earlier findings of cognitive function deficits in un-medicated patients with schizophrenia (Veselinović et al. 2015). The generally poor cognitive performance in the patient group, particularly in the TMT, may be a marker for more general cognitive disorganization (Mahurin et al. 2006) or more specifically of impaired executive functions and cognitive flexibility (Kortte et al. 2002). Further, acute symptoms in our unmedicated sample may also have contributed to their worse cognitive performance in the TMT(B). In this task, positive symptoms could confound performance since visual scanning is involved, even as negative symptoms could impair the motor component. Indeed, numerous previous investigations speak on behalf of a moderate association between negative symptoms and neurocognition (Heydebrand et al. 2004; Ventura et al. 2009; Lindsberg et al. 2009; Leeson et al. 2010; Meyer et al. 2014) and a lesser association between positive symptoms and cognition (Addington et al. 2005; Ventura et al. 2009, 2010) in chronic and first-episode schizophrenia.
We found a trend towards globally 5–10% higher D2/3 receptor availability in medication-free patients suffering from schizophrenia compared to age matched healthy volunteers. Previous studies report elevated D2/3 receptor availability in comparable patients groups (Wong et al. 1986; Tune et al. 1993; Laruelle 1998; Kestler et al. 2001), or no significant difference (Hietala et al. 1994; Nordstrom et al. 1995; Yang et al. 2004b; Glenthoj et al. 2006; Suridjan et al. 2013). Howes and colleagues (Howes et al. 2012) confirmed in their comprehensive meta-analysis an increased D2/3 receptor availability of small effect size in previously medicated patients with schizophrenia (Cohen d = 0.26, p = 0.049), as corroborated by two other meta-analyses of various SPECT and PET studies (Weinberger and Laruelle 2002; Brunelin et al. 2013). Mukherjee and colleagues reported a test–retest error for [18F]fallypride BPND of up to 10% in a sample of six healthy normal subjects (Mukherjee et al. 2002), whereas other report rather good test-retest variability ranging from 4% in striatum to 6–8% in cortical regions (Cropley et al. 2008; Dunn et al. 2013). In any case, the present sample size is clearly inadequate to detect group differences in BPND, especially in consideration of the mixed treatment history; a simple power calculation suggests that a sample size of at least 64 per group would be required to detect a significant BPND difference assuming an effect size such as reported in the meta-analyses. The citation “Weinberger et al. 2002” has been changed to “Weinberger and Laruelle, 2002” to match the author name/date in the reference list. Please check if the change is fine in this occurrence and modify the subsequent occurrences, if necessary.I agree with the changed citation.
Sample size and test-retest stability are key issues in relation to the detection of small group differences in [18F]fallypride BPND. Further limitations of our study are the relatively large age range of patients and controls, and the mixed patient group in relation to stage of illness/medication history. The wide age range arises from the logistics of recruitment of medication-free patients with schizophrenia. Nonetheless, we were unable to detect any age-dependence of BPND, either in the patient or control groups over an age range of three decades, despite earlier reports of a > 10% decline in striatum with each decade of healthy aging (Bäckman et al. 2006; Cumming et al. 2013). This is likely due to inadequate power of the present study, which also failed to replicate a report of greater rate decline in D2/3 receptor availability with increasing illness duration (Kestler et al. 2001). However, the present investigation was an exploratory and correlational study designed to search for associations between D2/3 receptor availability and cognitive performance. As such, present findings should motivate further investigations in more narrowly defined groups.
Howes et al. attributed a slightly higher striatal D2/3 availability in schizophrenia patients to persisting effects of recent exposure to antipsychotic medication (Howes et al. 2012). Six of our 15 patients had never been treated with an antipsychotic medication previously and had diagnosis of a first episode of schizophrenia, with symptom duration of 6 to 9 months, whereas the remaining nine patients had a longer duration of illness, and previous antipsychotic treatment. Although our sub-group sizes are too small to support comparisons, we suppose that this clinical heterogeneity may have contributed to dispersion of our molecular imaging results. In particular, previous history of antipsychotic medication may have altered dopamine receptor availability, as suggested by basic research showing that prolonged pharmacological blockade of D2/3 dopamine receptors leads to a compensatory increase of their densities (Oda et al. 2015) or increased affinity state for dopamine agonists, i.e. sensitization (Seeman 2013).
In summary, we report a positive relationship between dopamine D2,3 receptor availability in striatum and ITG with some aspects of cognition in a group of 15 schizophrenia patients, but no such relationships in healthy age-matched controls. This could indicate a greater involvement of signaling at dopamine D2/3 receptors in certain cognitive functions in schizophrenia patients than in healthy controls. In this scenario, lower basal occupancy by endogenous dopamine in those patients with higher D2,3 receptor availability may favor better cognitive performance and flexibility. Present results give heuristic support to the mechanism by which pharmacological blockade of dopamine D2/3 receptors, intended to ameliorate positive symptoms of schizophrenia, may contribute to worsening of cognitive function and furthermore implicate neocortical as well as striatal receptors in these effects.
References
Addington J, Saeedi H, Addington D (2005) The course of cognitive functioning in first episode psychosis: changes over time and impact on outcome. Schizophr Res 78:35–43. https://doi.org/10.1016/j.schres.2005.05.008
Allen MD, Owens TE, Fong AK, Richards DR (2011) A functional neuroimaging analysis of the trail making test-B: implications for clinical application. Behav Neurol 24:159–171. https://doi.org/10.3233/BEN-2011-0278
Arbuthnott K, Frank J (2000) Trail making test, part B as a measure of executive control: validation using a set-switching paradigm. J Clin Exp Neuropsychol 22:518–528. https://doi.org/10.1076/1380-3395(200008)22:4;1-0;FT518
Backman L, Ginovart N, Dixon RA et al (2000) Age-related cognitive deficits mediated by changes in the striatal dopamine system. Am J Psychiatry 157:635–637. https://doi.org/10.1176/ajp.157.4.635
Bäckman L, Nyberg L, Lindenberger U, Li SC, Farde L (2006) The correlative triad among aging, dopamine, and cognition: current status and future prospects. Neurosci Biobehav Rev 30:791–807. https://doi.org/10.1016/j.neubiorev.2006.06.005
Brunelin J, Fecteau S, Suaud-Chagny M-F (2013) Abnormal striatal dopamine transmission in schizophrenia. Curr Med Chem 20:397–404. https://doi.org/10.2174/0929867311320030011
Buchanan RW, Freedman R, Javitt DC, Abi-Dargham A, Lieberman JA (2007) Recent advances in the development of novel pharmacological agents for the treatment of cognitive impairments in schizophrenia. Schizophr Bull 33:1120–1130. https://doi.org/10.1093/schbul/sbm083
Cabeza R, Nyberg L (2000) Imaging cognition II: an empirical review of 275 PET and fMRI studies. J Cogn Neurosci 12:1–47
Carter CS, MacDonald AW, Ross LL, Stenger VA (2001) Anterior cingulate cortex activity and impaired self-monitoring of performance in patients with schizophrenia: an event-related fMRI study. Am J Psychiatry 158:1423–1428. https://doi.org/10.1176/appi.ajp.158.9.1423
Cropley VL, Innis RB, Nathan PJ, Brown AK, Sangare JL, Lerner A, Ryu YH, Sprague KE, Pike VW, Fujita M (2008) Small effect of dopamine release and no effect of dopamine depletion on [18F]fallypride binding in healthy humans. Synapse 62:399–408. https://doi.org/10.1002/syn.20506
Cumming P, Xiong G, la Fougere C et al (2013) Surrogate markers for cerebral blood flow correlate with [(1)(8)F]-fallypride binding potential at dopamine D(2/3) receptors in human striatum. Synapse 67:199–203. https://doi.org/10.1002/syn.21630
Dunn JT, Clark-Papasavas C, Marsden P, Baker S, Cleij M, Kapur S, Kessler R, Howard R, Reeves SJ (2013) Establishing test-retest reliability of an adapted [(18)F]fallypride imaging protocol in older people. J Cereb Blood Flow Metab 33:1098–1103. https://doi.org/10.1038/jcbfm.2013.55
Fagerlund B, Pinborg LH, Mortensen EL, Friberg L, Baaré WFC, Gade A, Svarer C, Glenthøj BY (2013) Relationship of frontal D(2/3) binding potentials to cognition: a study of antipsychotic-naive schizophrenia patients. Int J Neuropsychopharmacol 16:23–36. https://doi.org/10.1017/S146114571200003X
Faul F, Erdfelder E, Lang A-G, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Floresco SB, Magyar O (2006) Mesocortical dopamine modulation of executive functions: beyond working memory. Psychopharmacology 188:567–585. https://doi.org/10.1007/s00213-006-0404-5
Floresco SB, Zhang Y, Enomoto T (2009) Neural circuits subserving behavioral flexibility and their relevance to schizophrenia. Behav Brain Res 204:396–409. https://doi.org/10.1016/j.bbr.2008.12.001
Glenthoj BY, Mackeprang T, Svarer C, Rasmussen H, Pinborg LH, Friberg L, Baaré W, Hemmingsen R, Videbaek C (2006) Frontal dopamine D(2/3) receptor binding in drug-naive first-episode schizophrenic patients correlates with positive psychotic symptoms and gender. Biol Psychiatry 60:621–629. https://doi.org/10.1016/j.biopsych.2006.01.010
Gold JM, Carpenter C, Randolph C, Goldberg TE, Weinberger DR (1997) Auditory working memory and Wisconsin Card Sorting Test performance in schizophrenia. Arch Gen Psychiatry 54:159–165. https://doi.org/10.1001/archpsyc.1997.01830140071013
Goldman-Rakic PS, Muly EC, Williams GV (2000) D1 receptors in prefrontal cells and circuits. Brain Res Rev 31:295–301. https://doi.org/10.1016/S0165-0173(99)00045-4
Gray JA, Roth BL (2007) Molecular targets for treating cognitive dysfunction in schizophrenia. Schizophr Bull 33:1100–1119
Green MF, Harvey PD (2014) Cognition in schizophrenia: past, present, and future. Schizophr Res Cogn 1:e1–e9. https://doi.org/10.1016/j.scog.2014.02.001
Green MF, Nuechterlein KH, Gold JM, Barch DM, Cohen J, Essock S, Fenton WS, Frese F, Goldberg TE, Heaton RK, Keefe RS, Kern RS, Kraemer H, Stover E, Weinberger DR, Zalcman S, Marder SR (2004) Approaching a consensus cognitive battery for clinical trials in schizophrenia: the NIMH-MATRICS conference to select cognitive domains and test criteria. Biol Psychiatry 56(5):301–307
Gründer G, Fellows C, Janouschek H et al (2008) Brain and plasma pharmacokinetics of aripiprazole in patients with schizophrenia: an [18F]fallypride PET study. Am J Psychiatry 165:988–995. https://doi.org/10.1176/appi.ajp.2008.07101574
Gründer G, Siessmeier T, Piel M, Vernaleken I, Buchholz HG, Zhou Y, Hiemke C, Wong DF, Rösch F, Bartenstein P (2003) Quantification of D2-like dopamine receptors in the human brain with 18F-desmethoxyfallypride. J Nucl Med 44:109–116
Hall H, Farde L, Halldin C et al (1996) Autoradiographic localization of extrastriatal D2-dopamine receptors in the human brain using [125I]epidepride. Synapse 23:115–123. https://doi.org/10.1002/(SICI)1098-2396(199606)23:2<115::AID-SYN7>3.0.CO;2-C
Harth S, Müller SV, Aschenbrenner S et al (2004) Regensburger Wortflüssigkeits-Test (RWT). Z Neuropsychol 15:315–321. https://doi.org/10.1024/1016-264x.15.4.315
Helmich RC, Derikx LC, Bakker M, Scheeringa R, Bloem BR, Toni I (2010) Spatial remapping of cortico-striatal connectivity in Parkinson’s disease. Cereb Cortex 20:1175–1186
Herath P, Kinomura S, Roland PE (2001) Visual recognition: evidence for two distinctive mechanisms from a PET study. Hum Brain Mapp 12:110–119
Heydebrand G, Weiser M, Rabinowitz J, Hoff AL, DeLisi L, Csernansky JG (2004) Correlates of cognitive deficits in first episode schizophrenia. Schizophr Res 68:1–9. https://doi.org/10.1016/S0920-9964(03)00097-5
Hietala J, Syvalahti E, Vuorio K et al (1994) Striatal D2 dopamine receptor characteristics in neuroleptic-naive schizophrenic patients studied with positron emission tomography. Arch Gen Psychiatry 51:116–123
Horacek J, Dockery C, Kopecek M, Spaniel F, Novak T, Tislerova B, Klirova M, Palenicek T, Höschl C (2006) Regional brain metabolism as the predictor of performance on the trail making test in schizophrenia. A 18FDG PET covariation study. Neuro Endocrinol Lett 27:587–594
Howes OD, Kambeitz J, Kim E, Stahl D, Slifstein M, Abi-Dargham A, Kapur S (2012) The nature of dopamine dysfunction in schizophrenia and what this means for treatment. Arch Gen Psychiatry 69:776–786. https://doi.org/10.1001/archgenpsychiatry.2012.169
Ishai A, Ungerleider LG, Martin A, Schouten JL, Haxby JV (1999) Distributed representation of objects in the human ventral visual pathway. Proc Natl Acad Sci U S A 96:9379–9384
Ishibashi K, Robertson CL, Mandelkern MA, et al (2013) The simplified reference tissue model with 18F-fallypride positron emission tomography: choice of reference region
Jacobson SC, Blanchard M, Connolly CC, Cannon M, Garavan H (2011) An fMRI investigation of a novel analogue to the Trail-Making Test. Brain Cogn 77:60–70. https://doi.org/10.1016/j.bandc.2011.06.001
Keefe RSE, Bilder RM, Davis SM, Harvey PD, Palmer BW, Gold JM, Meltzer HY, Green MF, Capuano G, Stroup TS, McEvoy J, Swartz MS, Rosenheck RA, Perkins DO, Davis CE, Hsiao JK, Lieberman JA, CATIE Investigators, Neurocognitive Working Group (2007) Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE trial. Arch Gen Psychiatry 64:633–647. https://doi.org/10.1001/archpsyc.64.6.633
Keefe RSE, Harvey PD (2012) Cognitive impairment in schizophrenia BT—novel antischizophrenia treatments. In: Geyer MA, Gross G (eds) Springer. Berlin Heidelberg, Berlin, Heidelberg, pp 11–37
Kessler RM, Ansari MS, Riccardi P, Li R, Jayathilake K, Dawant B, Meltzer HY (2005) Occupancy of striatal and extrastriatal dopamine D2/D3 receptors by olanzapine and haloperidol. Neuropsychopharmacology 30:2283–2289. https://doi.org/10.1038/sj.npp.1300836
Kestler LP, Walker E, Vega EM (2001) Dopamine receptors in the brains of schizophrenia patients: a meta-analysis of the findings. Behav Pharmacol 12:355–371
Kortte KB, Horner MD, Windham WK (2002) The trail making test, part B: cognitive flexibility or ability to maintain set? Appl Neuropsychol 9:106–109. https://doi.org/10.1207/S15324826AN0902_5
Lammertsma AA, Hume SP (1996) Simplified reference tissue model for PET receptor studies. NeuroImage 4:153–158. https://doi.org/10.1006/nimg.1996.0066
Langer O, Halldin C, Dollé F, Swahn CG, Olsson H, Karlsson P, Hall H, Sandell J, Lundkvist C, Vaufrey F, Loc'h C, Crouzel C, Mazière B, Farde L (2017) Carbon-11 epidepride: a suitable radioligand for PET investigation of striatal and extrastriatal dopamine D2 receptors. Nucl Med Biol 26:509–518. https://doi.org/10.1016/S0969-8051(99)00005-0
Laruelle M (1998) Imaging dopamine transmission in schizophrenia. A review and meta-analysis. Q J Nucl Med 42:211–221
Lawrence AD, Weeks RA, Brooks DJ, et al (1998) The relationship between striatal dopamine receptor binding and cognitive performance in Huntington’s disease. Brain : a journal of neurology 121 (Pt 7). England: 1343–1355.
Leeson VC, Barnes TRE, Harrison M, Matheson E, Harrison I, Mutsatsa SH, Ron MA, Joyce EM (2010) The relationship between IQ, memory, executive function, and processing speed in recent-onset psychosis: 1-year stability and clinical outcome. Schizophr Bull 36:400–409. https://doi.org/10.1093/schbul/sbn100
Lindsberg J, Poutiainen E, Kalska H (2009) Clarifying the diversity of first-episode psychosis: neuropsychological correlates of clinical symptoms. Nord J Psychiatry 63:493–500. https://doi.org/10.3109/08039480903118182
MacPherson SE, Cox SR, Dickie DA et al (2017) Processing speed and the relationship between Trail Making Test-B performance, cortical thinning and white matter microstructure in older adults. Cortex 95:92–103. https://doi.org/10.1016/j.cortex.2017.07.021
Mahurin RK, Velligan DI, Hazleton B, Mark Davis J, Eckert S, Miller AL (2006) Trail making test errors and executive function in schizophrenia and depression. Clin Neuropsychol 20:271–288. https://doi.org/10.1080/13854040590947498
Mehta MA, Montgomery AJ, Kitamura Y, et al. (2008) Dopamine D2 receptor occupancy levels of acute sulpiride challenges that produce working memory and learning impairments in healthy volunteers. Psychopharmacology 196(1). Germany: 157–165. https://doi.org/10.1007/s00213-007-0947-0
Meyer EC, Carrion RE, Cornblatt BA, Addington J, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, Tsuang MT, Walker EF, Woods SW, Heinssen R, Seidman LJ, the NAPLS group (2014) The relationship of neurocognition and negative symptoms to social and role functioning over time in individuals at clinical high risk in the first phase of the North American Prodrome Longitudinal Study. Schizophr Bull 40:1452–1461. https://doi.org/10.1093/schbul/sbt235
Minzenberg MJ, Laird AR, Thelen S, Carter CS, Glahn DC (2009) Meta-analysis of 41 functional neuroimaging studies of executive function in schizophrenia. Arch Gen Psychiatry 66:811–822. https://doi.org/10.1001/archgenpsychiatry.2009.91
Morris ED, Constantinescu CC, Sullivan JM, Normandin MD, Christopher LA (2010) Noninvasive visualization of human dopamine dynamics from PET images. NeuroImage 51:135–144. https://doi.org/10.1016/j.neuroimage.2009.12.082
Mukherjee J, Christian BT, Dunigan KA, Shi B, Narayanan TK, Satter M, Mantil J (2002) Brain imaging of 18F-fallypride in normal volunteers: blood analysis, distribution, test-retest studies, and preliminary assessment of sensitivity to aging effects on dopamine D-2/D-3 receptors. Synapse 46:170–188. https://doi.org/10.1002/syn.10128
Mukherjee J, Yang ZY, Das MK, Brown T (1995) Fluorinated benzamide neuroleptics--III. Development of (S)-N-[(1-allyl-2-pyrrolidinyl)methyl]-5-(3-[18F]fluoropropyl)-2, 3-dimethoxybenzamide as an improved dopamine D-2 receptor tracer. Nucl Med Biol 22:283–296
Nordstrom AL, Farde L, Eriksson L, Halldin C (1995) No elevated D2 dopamine receptors in neuroleptic-naive schizophrenic patients revealed by positron emission tomography and [11C]N-methylspiperone. Psychiatry Res 61:67–83
Nuechterlein KH, Green MF, Kern RS et al (2008) The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. Am J Psychiatry 165:203–213. https://doi.org/10.1176/appi.ajp.2007.07010042
Nyberg L, Karalija N, Salami A, et al. (2016) Dopamine D2 receptor availability is linked to hippocampal-caudate functional connectivity and episodic memory. Proceedings of the National Academy of Sciences of the United States of America 113(28). United States: 7918–7923. https://doi.org/10.1073/pnas.1606309113
Oda Y, Kanahara N, Iyo M (2015) Alterations of dopamine D2 receptors and related receptor-interacting proteins in schizophrenia: the pivotal position of dopamine supersensitivity psychosis in treatment-resistant schizophrenia. Int J Mol Sci 16:30144–30163. https://doi.org/10.3390/ijms161226228
Olsson H, Halldin C, Farde L (2004) Differentiation of extrastriatal dopamine D2 receptor density and affinity in the human brain using PET. NeuroImage 22:794–803. https://doi.org/10.1016/j.neuroimage.2004.02.002
Pavese N, Andrews TC, Brooks DJ, et al. (2003) Progressive striatal and cortical dopamine receptor dysfunction in Huntington’s disease: a PET study. Brain : a journal of neurology 126(Pt 5). England: 1127–1135.
Rajji TK, Mulsant BH, Nakajima S, Caravaggio F, Suzuki T, Uchida H, Gerretsen P, Mar W, Pollock BG, Mamo DC, Graff-Guerrero A (2017) Cognition and dopamine D2 receptor availability in the striatum in older patients with schizophrenia. Am J Geriatr Psychiatry 25:1–10. https://doi.org/10.1016/j.jagp.2016.08.001
Reeves SJ, Grasby PM, Howard RJ, Bantick RA, Asselin MC, Mehta MA (2005) A positron emission tomography (PET) investigation of the role of striatal dopamine (D2) receptor availability in spatial cognition. NeuroImage 28:216–226. https://doi.org/10.1016/j.neuroimage.2005.05.034
Reitan RM (1958) Validity of the trail making test as an indicator of organic brain damage. Percept Mot Skills 8:271–276. https://doi.org/10.2466/PMS.8.7.271-276
Robinson JL, Laird AR, Glahn DC, Blangero J, Sanghera MK, Pessoa L, Fox PM, Uecker A, Friehs G, Young KA, Griffin JL, Lovallo WR, Fox PT (2012) The functional connectivity of the human caudate: an application of meta-analytic connectivity modeling with behavioral filtering. NeuroImage 60:117–129. https://doi.org/10.1016/j.neuroimage.2011.12.010
Seamans JK, Yang CR (2004) The principal features and mechanisms of dopamine modulation in the prefrontal cortex. Prog Neurobiol 74:1–58. https://doi.org/10.1016/j.pneurobio.2004.05.006
Seeman P (2013) Are dopamine D2 receptors out of control in psychosis? Prog Neuro-Psychopharmacol Biol Psychiatry 46:146–152. https://doi.org/10.1016/j.pnpbp.2013.07.006
Siessmeier T, Zhou Y, Buchholz H-G, Landvogt C, Vernaleken I, Piel M, Schirrmacher R, Rösch F, Schreckenberger M, Wong DF, Cumming P, Gründer G, Bartenstein P (2005) Parametric mapping of binding in human brain of D2 receptor ligands of different affinities. J Nucl Med 46:964–972
Simpson EH, Kellendonk C, Kandel E (2010) A possible role for the striatum in the pathogenesis of the cognitive symptoms of schizophrenia. Neuron 65:585–596. https://doi.org/10.1016/j.neuron.2010.02.014
Suridjan I, Rusjan P, Addington J, Wilson A, Houle S, Mizrahi R (2013) Dopamine D2 and D3 binding in people at clinical high risk for schizophrenia, antipsychotic-naive patients and healthy controls while performing a cognitive task. J Psychiatry Neurosci 38:98–106. https://doi.org/10.1503/jpn.110181
Takahashi H (2013) PET neuroimaging of extrastriatal dopamine receptors and prefrontal cortex functions. J Physiol 107:503–509. https://doi.org/10.1016/j.jphysparis.2013.07.001
Tamminga CA (2006) The neurobiology of cognition in schizophrenia. J Clin Psychiatry 67(Suppl 9):9–42
Tune LE, Wong DF, Pearlson G, Strauss M, Young T, Shaya EK, Dannals RF, Wilson AA, Ravert HT, Sapp J, Cooper T, Chase GA, Wagner HN Jr (1993) Dopamine D2 receptor density estimates in schizophrenia: a positron emission tomography study with 11C-N-methylspiperone. Psychiatry Res 49:219–237
Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH (2009) Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res 113:189–199. https://doi.org/10.1016/j.schres.2009.03.035
Ventura J, Thames AD, Wood RC, Guzik LH, Hellemann GS (2010) Disorganization and reality distortion in schizophrenia: a meta-analysis of the relationship between positive symptoms and neurocognitive deficits. Schizophr Res 121:1–14. https://doi.org/10.1016/j.schres.2010.05.033
Vernaleken I, Janouschek H, Raptis M, Hellmann S, Veselinovic T, Bröcheler A, Boy C, Cumming P, Hiemke C, Rösch F, Schäfer WM, Gründer G (2010) Dopamine D2/3 receptor occupancy by quetiapine in striatal and extrastriatal areas. Int J Neuropsychopharmacol 13:951–960
Vernaleken I, Klomp M, Moeller O, Raptis M, Nagels A, Rösch F, Schaefer WM, Cumming P, Gründer G (2013) Vulnerability to psychotogenic effects of ketamine is associated with elevated D2/3-receptor availability. Int J Neuropsychopharmacol 16:745–754. https://doi.org/10.1017/S1461145712000764
Vernaleken I, Peters L, Raptis M, Lin R, Buchholz HG, Zhou Y, Winz O, Rösch F, Bartenstein P, Wong DF, Scháfer WM, Gründer G (2011) The applicability of SRTM in [(18)F]fallypride PET investigations: impact of scan durations. J Cereb Blood Flow Metab 31:1958–1966. https://doi.org/10.1038/jcbfm.2011.73
Veselinović T, Vernaleken I, Janouschek H, Kellermann T, Paulzen M, Cumming P, Gründer G (2015) Effects of anticholinergic challenge on psychopathology and cognition in drug-free patients with schizophrenia and healthy volunteers. Psychopharmacology 232:1607–1617. https://doi.org/10.1007/s00213-014-3794-9
Volkow ND, Gur RC, Wang G-J, Fowler JS, Moberg PJ, Ding YS, Hitzemann R, Smith G, Logan J (1998) Association between declines in brain dopamine activity with age and cognitive and motor impairment in healthy individuals. Am J Psychiatry 155:344–349. https://doi.org/10.1176/ajp.155.3.344
Wechsler D (1997) WAIS-III administration and scoring manual
Weinberger DR, Laruelle M (2002) Neuropharmacological imaging in schizophrenia. In: Davis KL, Charney D, Coyle JTCN (eds) Neuropsychopharmacology: the fifth generation of progress. Lippincott, Williams, & Wilkins. Pennsylvania, Philadelphia
Wong DF, Wagner HNJ, Tune LE et al (1986) Positron emission tomography reveals elevated D2 dopamine receptors in drug-naive schizophrenics. Science 234:1558–1563
Yang YK, Yeh TL, Chiu NT, Lee IH, Chen PS, Lee LC, Jeffries KJ (2004a) Association between cognitive performance and striatal dopamine binding is higher in timing and motor tasks in patients with schizophrenia. Psychiatry Res 131:209–216. https://doi.org/10.1016/j.pscychresns.2003.07.002
Yang YK, Yu L, Yeh TL, Chiu NT, Chen PS, Lee IH, SPECT study (2004b) Associated alterations of striatal dopamine D2/D3 receptor and transporter binding in drug-naive patients with schizophrenia: a dual-isotope SPECT study. Am J Psychiatry 161:1496–1498. https://doi.org/10.1176/appi.ajp.161.8.1496
Yoder KK, Hutchins GD, Morris ED, Brashear A, Wang C, Shekhar A (2004) Dopamine transporter density in schizophrenic subjects with and without tardive dyskinesia. Schizophr Res 71:371–375. https://doi.org/10.1016/j.schres.2004.03.015
Funding
This study was supported by the German Research Association (Deutsche Forschungsgemeinschaft, DFG; KFO-112/2-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Vernaleken has served on the speakers’ bureau of Bristol-Myers Squibb (New York, NY), Eli Lilly (Indianapolis, Ind), and GlaxoSmithKline (London, UK). Dr. Gründer has served as a consultant for Allergan (Dublin, Ireland), Boehringer Ingelheim (Ingelheim, Germany), Eli Lilly (Indianapolis, Ind, USA), Janssen-Cilag (Neuss, Germany), Lundbeck (Copenhagen, Denmark), Ono Pharmaceuticals (Osaka, Japan), Otsuka (Chiyoda, Japan), Recordati (Milan, Italy), Roche (Basel, Switzerland), Servier (Paris, France), and Takeda (Osaka, Japan). He has served on the speakers’ bureau of Eli Lilly, Janssen Cilag, Neuraxpharm (Langenfeld, Germany), Roche, Servier, and Trommsdorf (Aachen, Germany). He has received grant support from Boehringer Ingelheim and Roche. He is co-founder of Mind and Brain Institute GmbH (Zornheim, Germany) and Brainfoods GmbH (Zornheim, Germany). Dr. Veselinović, Dr. Janouschek, Prof. Cumming, Dr. Paulzen, and Dr. Mottaghy declare no conflicts of interest.
Electronic supplementary material
Figure 1
Scatter plots showing the distributions of the D2/3 receptor availability ([18F]fallypride BPND) in the patients and the controls. Depicted are values for two striatal regions (caudate nucleus, putamen) and two extrastriatal regions (inferior temporal gyrus, thalamus). (PDF 49 kb)
Rights and permissions
About this article
Cite this article
Veselinović, T., Vernaleken, I., Janouschek, H. et al. The role of striatal dopamine D2/3 receptors in cognitive performance in drug-free patients with schizophrenia. Psychopharmacology 235, 2221–2232 (2018). https://doi.org/10.1007/s00213-018-4916-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-018-4916-6