Abstract
Rationale
The beneficial effects of nicotinic acetylcholine receptor (nAChR) agonists on cognitive performance have been widely shown. Paradoxically, recent preclinical studies employing extremely low doses of nAChR antagonists have also found cognitive enhancement, perhaps pointing to a novel treatment mechanism for cognitive deficits.
Objectives
The aim was to test whether low doses of the nAChR antagonist mecamylamine would benefit performance in human volunteers.
Methods
The study employed a double-blind within-subject design. Over four separate days, healthy adult non-smokers (n = 23) were tested with placebo and three trace doses of mecamylamine (0.25–1 mg, p.o.), adjusted for body weight. Participants performed three computerized tasks: a task of spatial selective attention and stimulus detection, the rapid visual information processing task (RVIPT) taxing sustained attention and working memory, and a change detection short-term memory task. Subjective state and vital signs were assessed repeatedly.
Results
Mecamylamine did not improve performance in any of the tasks. Any trends that were observed instead pointed toward performance impairment. Mecamylamine also had no effects on subjective state or vital signs.
Conclusions
The present results do not support the hypothesized cognitive-enhancing potential of low doses of mecamylamine. Contrary to preclinical reports, these findings speak against low-dose nAChR antagonism as a novel avenue for treating cognitive deficits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cognitive benefits of nicotinic acetylcholine receptor (nAChR) agonists are well established, with the majority of data derived from the prototypical nAChR agonist nicotine. These effects are not restricted to deprived smokers and are reported most consistently in tests of attention (Stolerman et al. 1995; Newhouse et al. 2004; Heishman et al. 2010). Several disease states marked by cognitive deficits, most prominently Alzheimer’s disease and schizophrenia, involve nAChR hypofunction (Perry et al. 2000; Pimlott et al. 2004; Martin et al. 2004; Adams and Stevens 2007; Petrovsky et al. 2010; Kendziorra et al. 2011; Wing et al. 2012) and may benefit from nAChR agonist treatment (Levin and Rezvani 2002; Singh et al. 2004). Over the last two decades, drug development efforts have invested into novel nAChR agonists, aiming for more pronounced benefits with reduced side effects. Effects have generally been in the expected direction, but most compounds failed clinical trials due to limited efficacy or side effects (Haydar and Dunlop 2010; Radek et al. 2010; Wallace et al. 2011; Hurst et al., 2013).
Antagonists of the nAChR generally produce effects opposite to agonists. In healthy volunteers, the nAChR antagonist mecamylamine at doses larger than 5 mg has been reported to impair learning and memory performance and slow performance on several tasks (Stolerman et al. 1973; Newhouse et al. 1992; Gitelman and Prohovnik 1992; Pickworth et al. 1997; Little et al. 1998; Hahn et al. 2014). However, in recent years, reports of paradoxical performance improvements emerged from the animal literature when mecamylamine was given at doses more than an order of magnitude lower than those typically causing impairment (Levin et al. 1987; Nagahara and Handa 1999; Grottick and Higgins 2000). At this low-dose range, mecamylamine improved working memory in rats and monkeys (Terry et al. 1999) and learning in rats with a U-shaped dose-response relationship (Levin and Caldwell 2006). Small doses of methyllycaconitine (MLA), an nAChR antagonist largely selective for the α7 subtype of nAChRs, improved accuracy in a rat paradigm of attention (Hahn et al. 2011), and the α4β2, α4β4, α3β2, and α2β2 nAChR antagonist dihydro-β-erythroidine (DHβE), although at larger doses, was reported to improve signal detection in another rat paradigm of attention (Levin et al. 2013).
The mechanism mediating such paradoxical improvements is unknown. A possible explanation is that the cognitive-enhancing effects of nAChR agonists may not be mediated by receptor activation per se, but by nAChR desensitization, i.e., the decline in response amplitude with prolonged agonist exposure until the receptor remains refractory to activation (Quick and Lester 2002). Indeed, nAChR desensitization has been suggested to mediate some behavioral effects of nAChR agonists (Picciotto et al. 2008; Buccafusco et al. 2009). Whichever the mechanism, if the cognitive benefits of low-dose nAChR antagonism were found to be a reliable phenomenon in humans, this may represent a novel nAChR-based treatment strategy with potentially fewer adverse effects.
One previous study tested low oral doses of mecamylamine (0.2, 0.5, 1 mg) in 15 adult human non-smokers with attention-deficit/hyperactivity disorder (ADHD; Potter et al. 2009). Mecamylamine slowed reaction time in the stop signal and stroop tasks and decreased delay tolerance, but it improved word recognition memory at the middle dose under some task conditions.
The aim of the present study was to systematically evaluate the cognitive-enhancing potential of low doses of mecamylamine in a larger sample of healthy human non-smokers. By choosing a within-subject repeated measures design and cognitive tasks with large trial numbers, pre-training participants extensively to minimize practice effects, and adjusting mecamylamine doses by body weight, we sought to increase signal to noise and enable the detection of potentially small performance effects. The cognitive tasks assessed visuospatial selective attention, rapid information processing and working memory, and short-term memory.
Methods
Participants
Twenty-four healthy non-smokers participated in the study. One participant was excluded because she had difficulty staying awake during cognitive testing. The remaining 23 participants (12 female; 7 African American, 13 Caucasian, 2 Hispanic, 1 Asian) were 24–53 years of age (mean ± stdev, 35.9 ± 10.1) with 12–22 years of education (16.0 ± 2.5). Participants were recruited from the local community through internet advertising, flyers, and referrals and gave written informed consent for a protocol approved by the University of Maryland Baltimore Institutional Review Board. All participants were non-smokers, with no more than 40 cigarettes in their lifetime and no nicotine exposure in the last year. Use of centrally active medications, pregnancy, history of neurological or psychiatric disorders including drug abuse, significant liver or kidney impairment, heart problems, hyper- and hypotension, and learning disability were exclusionary. Participants were paid for their time. Reimbursement did not depend on task performance.
Drugs
Mecamylamine is FDA-approved for treating hypertension; however, the FDA-approved product (Inversine®) is no longer commercially available. GMP-grade mecamylamine hydrochloride powder was obtained from Euticals SpA (Milan, Italy) and packaged into capsules by an in-house compounding pharmacist, who also produced matching placebo capsules. Microcrystalline cellulose was used as inactive filler.
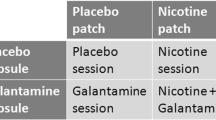
Study procedures
The study adopted a double-blind within-subject design. Each participant was tested with three low doses of mecamylamine and placebo over the course of four identical test sessions. The sequence of drug conditions was counterbalanced between participants. Doses of mecamylamine were chosen to be at least one order of magnitude lower than those observed to impair performance, and were adjusted for body weight:
<160 lb = 0.2, 0.4, and 0.8 mg
160–200 lb = 0.25, 0.5, and 1 mg
>200 lb = 0.3, 0.6, and 1.2 mg
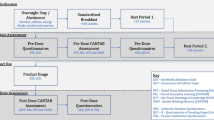
The study involved six total visits: one consent and screening visit, one training visit, and four test sessions scheduled with at least two intervening days. Screening included a medical history and physical exam, an EKG, blood and urine labs, a vision test and tests for drug use, smoking, and pregnancy. During the training visit, participants were given task instructions and performed a full-length version of each of the cognitive tasks described below, to minimize practice effects between test sessions.
The four test sessions each took approximately 5.5 h. Participants arrived in the morning, with efforts made to maintain consistent start times for each participant once chosen. Upon arrival, participants were tested for fever and recent alcohol use, and a urine sample was tested for pregnancy and drug use, all of which had to be negative for the session to proceed. A resting blood pressure and heart rate measurement was taken, and participants completed a side effects checklist, rating their current weakness/fatigue, dizziness, dry mouth, palpitations, and sleepiness as none (1), mild (2), moderate (3), or severe (4). They then completed the Profile of Mood States (POMS), an adjective rating questionnaire considered to be a standardized subjective mood state inventory (McNair et al. 1971). The study capsule was then administered. Vital signs were taken and the side effects checklist was completed hourly thereafter. During the drug-absorption period, participants were permitted to read, watch TV, or surf the internet. Three hours after capsule administration, at which time mecamylamine blood concentrations were expected to have reached a plateau (Young et al. 2001, Singh et al. 2006), the POMS was again completed and cognitive testing began. The order of the tasks always remained the same: first the spatial attentional resource allocation task, then the rapid visual information processing task, and lastly the change detection task. Testing took approximately 1.5 h in total. Vital signs were measured after the first task. Following cognitive testing, the POMS and side effects checklist were completed and vital signs were taken one last time.
Equipment
All tasks were performed on a 19-in. 5:4 IPS LCD monitor with a screen resolution of 1280 × 1024 and a refresh rate of 60 Hz. Responses were recorded using a Logitech F310 gamepad controller. Only the left and right bumper buttons were used. All tasks were created and run in E-Prime version 2.0.
Task paradigms
Spatial attentional resource allocation task
The spatial attentional resource allocation task (SARAT) is a visuospatial stimulus detection paradigm (Hahn et al. 2006), shown to be sensitive to the performance-enhancing effects of nicotine (Hahn et al. 2007, 2013, 2014). Participants fixated on a quartered circle in the center of the screen (diameter approximately 2.6° of visual angle), black against a light gray (10 % contrast; 130 cd/m2) background. They were instructed to respond as quickly as possible when detecting a 500-ms target stimulus appearing in one of four locations in the corners of the screen, marked by circular place holders (diameter 1.3° of visual angle), positioned at 10° of visual angle (Fig. 1a).
A cue in the central circle preceded the target signal by 400, 700, 1000, or 1300 ms, chosen randomly to make target onset temporally unpredictable and discourage anticipatory responding to the cue. Either one quarter turned black to indicate the location of the upcoming target (predictive cue) or all four quarters turned black (nonpredictive cue). Predictive cue trials allowed for a narrow attentional focus, while nonpredictive cue trials required attention to be spread widely to encompass the entire display. Participants were asked to press a button with their dominant index finger upon detecting a target. Targets were presented in the continued presence of the cue. Targets consisted of peripheral placeholders filling with a gray (40 % contrast) and white checkerboard pattern of 3 × 3 pixels each. The cue persisted for 500 ms after target offset. Only task background was then displayed for an intertrial interval (ITI) of 400, 700, 1000, or 1300 ms.
The task was presented in eight 5-min blocks of 60 trials each: 30 predictive cue trials, of which six had no target to discourage anticipatory responding to the cue, and 30 nonpredictive cue trials, of which six had no target. To increase the temporal jitter of the task and augment stimulus detection demands, 30 additional 2.7-s periods during which only task background was presented were interspersed between trials. The entire task took approximately 45 min to complete.
Rapid visual information processing task
The rapid visual information processing task (RVIPT) requires the maintenance of intense rapid information processing and working memory demands over time. Performance therefore reflects processing speed, sustained attention, and working memory.
The RVIPT has been used extensively to evaluate the cognitive effects of cholinergic agents and is sensitive to the performance-enhancing effects of nicotine (e.g., Wesnes and Warburton 1984; Foulds et al. 1996; Warburton and Mancuso 1998). The task consists of a string of digits (1 through 9), presented one at a time at a rate of 100/min. Each digit was presented for 600 ms, with no ITI. Participants were instructed to respond by button press when they identified three consecutive odd or three consecutive even digits. Responses within an 1800-ms time window following the onset of the last digit of a target sequence were considered hits, all other responses were considered false alarms. On average, 8 target sequences were presented per minute. The number of digits separating targets ranged from 4 to 29. The task was performed in two blocks of 15 min each, with a break between to ensure feasibility.
Change detection task
The change detection task (CDT) is a visual short-term memory task and was included as a probe for potential mnemonic effects of mecamylamine. The task was chosen because it enables the presentation of a large number of trials with different set sizes in a short period of time, thus yielding reliable measurements of varying memory load conditions. It is relatively unconducive to verbal rehearsal, thus narrowing down possible interpretations of potential drug effects. A 220-ms encoding array of either one or five colored squares was presented (Fig. 1b). Possible colors were red, magenta, purple, yellow, white, blue, cyan, green, olive, and teal. Half of the trials showed five colored squares and the other half showed one colored square. After a 1100-ms retention interval, one square reappeared for 2000 ms and participants determined whether this square was of the same or a different color than the square previously displayed at this location. On half the trials, the color was the same, on the other half, the color changed. Participants responded “same” with a right button press and “different” with a left button press. Trials were separated by a 1000-ms intertrial interval. The task consisted of 180 total trials, presented over 5 blocks of 36 trials separated by short breaks, and took approximately 13 min to complete.
Data analysis
SARAT
Reaction time (RT) was expressed as the average over trials, and omission errors were expressed as the percentage of trials in which no response was recorded. Each variable was analyzed by two-factor ANOVA with cue condition (predictive vs. nonpredictive cue) and mecamylamine dose (placebo, low, medium, high) as within-subject factors.
RVIPT
RT was expressed as the average over responses reflecting correctly identified target sequences (hits). Hits and false alarms were expressed as a percentage and combined into the sensitivity index A' according to the following formula (Grier 1971):
A ' = 0.5 + ((%hits ‐ % false alarms) + ((%hits ‐ % false alarms) ^ 2))/(4 * % hits * (1 − % false alarms))
This non-parametric signal detection index was chosen because the assumption of normal distribution and equal variances of signal and non-signal events are often violated in vigilance situations (Loeb and Alluisi 1984). RT and A' were analyzed by one-factor ANOVAs with mecamylamine dose as within-subject factor.
CDT
Response accuracy was expressed as the percentage of correct responses across trials in which the color of the probed item had or had not changed. Reaction time was expressed as the average over all correct and incorrect response trials. Each variable was analyzed by two-factor ANOVA with set size (1 vs. 5) and mecamylamine dose as within-subject factors.
Note that SEMs plotted in all graphs were adjusted to remove between-subject variability in the average performance across dose levels (Cousineau 2007; Morey 2008). This method essentially yields a variability index reflective specifically of interindividual differences in drug effect, the focus of this study. Supplementary Table 1 lists data for all conditions, independent of significance, with unadjusted SEM.
Results
SARAT
RT (Fig. 2a) was significantly slower in nonpredictive than in predictive cue trials (main effect of cue condition: F(1,22) = 49.3, P < 0.001), consistent with previous findings (Hahn et al. 2006, 2011). Mecamylamine had no effect on RT under either cue condition (main effect of dose: F(3,66) = 0.545, P > 0.6; cue × dose interaction: F(3,66) = 0.236, P > 0.8).
Effects of mecamylamine on reaction time (a) and omission errors (b) in the spatial attentional resource allocation task. Bars reflect the mean performance in each dose condition. Error bars reflect SEMs, adjusted to remove between-subject variability in the average performance across dose levels (Cousineau 2007; Morey 2008) to yield variability related to interindividual differences in drug effect. Doses Small, Medium (Med), and Large refer to 0.2, 0.4, and 0.8 mg of mecamylamine for participants weighing <160 lb; to 0.25, 0.5, and 1 mg for 160–200 lb; and to 0.3, 0.6, and 1.2 mg for >200 lb. Pla Placebo. *P < 0.05 in paired t test comparing performance after mecamylamine to performance after vehicle
Omission errors (Fig. 2b) did not differ between cue conditions (P > 0.4). Mecamylamine appeared to subtly increase omission errors. However, the main effect of dose in ANOVA was not significant (P = 0.18), and neither was the cue × dose interaction (P = 0.15).
RVIPT
Stimulus detection sensitivity A' appeared to be reduced by mecamylamine (Fig. 3a), but the main effect of dose in ANOVA was only a trend (F(3,66) = 2.16, P = 0.10).
Effects of mecamylamine on signal detection sensitivity (a) and reaction time (b) in the rapid visual information processing task. Bars reflect the mean performance in each dose condition. Error bars reflect SEMs, adjusted to remove between-subject variability in the average performance across dose levels (Cousineau 2007; Morey 2008). Doses Small, Medium (Med), and Large refer to 0.2, 0.4, and 0.8 mg for participants weighing <160 lb; to 0.25, 0.5, and 1 mg for 160–200 lb; and to 0.3, 0.6, and 1.2 mg for >200 lb. *P < 0.05, (*) P = 0.057 in paired t tests comparing performance after mecamylamine to performance after vehicle
RT appeared to be slowed by mecamylamine (Fig. 3b). Again, the main effect of dose in ANOVA was not significant (P = 0.15).
CDT
Response accuracy was significantly lower with set size 5 as compared with set size 1 (F(1,22) = 155, P < 0.001), but there was no effect of mecamylamine dose (P = 0.4) and no set size × dose interaction (P > 0.4). RT was slower with set size 5 than with set size 1 (P < 0.001), but was not affected by mecamylamine dose (main effect: P > 0.3; set size × dose: P > 0.5). Data are presented in Supplementary Table 1.
Vital signs
When including all six time points (pre-drug and hourly thereafter) into two-factor ANOVA, there were no significant main effects of mecamylamine dose on systolic or diastolic blood pressure, or on heart rate, and no dose × time interactions. When averaging ratings over the measurements before, during, and after cognitive testing (3, 3:45, and 4:30 h after capsule administration), the time points at which mecamylamine blood concentrations can be assumed to be highest, there were still no significant effects of dose in one-factor ANOVA, an expectable result given that the doses tested were over ten times lower than those used to treat hypertension.
Subjective state measures
Side effects checklist
Weakness/fatigue, dizziness, dry mouth, palpitations, and sleepiness were analyzed separately. In two-factor ANOVA (dose × time), there were no main effects of mecamylamine dose and no interactions of dose with time (six measurement time points).
The POMS ratings were combined into subscale vigor, fatigue, depression, tension, confusion, anger, and total mood disturbance (McNair et al. 1971). Two-factor ANOVA (dose × time) yielded no main effects of mecamylamine dose and no interactions of dose with time point (pre-drug, pre-testing, post-testing) on any subscale.
Discussion
The aim of the present study was to test the cognitive-enhancing potential of very low doses of mecamylamine. Preclinical studies reported improvements in attention and learning and memory with low doses of mecamylamine and other nAChR antagonists (Terry et al. 1999; Levin and Caldwell 2006; Hahn et al. 2011; Levin et al. 2013). The only study previously conducted in human volunteers, specifically in adults diagnosed with ADHD, yielded mixed results, with slowed RT on some measures and improved recognition memory at one dose under specific task conditions (Potter et al. 2009).
The present study did not confirm the hypothesized performance benefits. Trends were observed on three out of six performance measures analyzed (omission errors in the SARAT and signal detection sensitivity and RT in the RVIPT), which were in part dose related. However, all trends reflected impaired, not improved performance. Thus, while the cognitive probes appeared sensitive to effects of mecamylamine even at the low-dose range tested (past studies reported impairments at doses larger than 5 mg), the results clearly do not support the hypothesized cognitive-enhancing potential of low doses of mecamylamine.
The doses of mecamylamine tested in the present study were chosen to be at least one order of magnitude lower than those previously reported to induce impaired cognitive performance (Stolerman et al. 1973; Newhouse et al. 1992; Gitelman and Prohovnik 1992; Pickworth et al. 1997; Little et al. 1998; Hahn et al. 2014), in line with preclinical findings. The doses were identical to those used by Potter et al. (2009), with the exception that we administered slightly lower doses to participants under 160 lb and slightly larger doses to those over 200 lb, in an effort to reduce interindividual variation in mecamylamine blood concentration. The present trends align with Potter et al.’s results with regard to slowed RT. Potter et al. (2009) additionally identified decreased delay tolerance, and our results were also suggestive of additional impairment. Considering that the improvement in word recognition memory reported by Potter et al. (2009) was not dose related (seen at only the middle dose) and was observed only under specific task conditions, we conclude that the cognitive effect profile of low doses of mecamylamine is overall negative.
A limitation to the above conclusion is that cognitive domains not covered by the present study may have shown improvement with low doses of mecamylamine. We chose paradigms testing different attentional functions, rapid information processing, working and short-term memory. Rather than increasing the number of paradigms, we opted for a larger number of trials per task to ensure conclusive findings for the domains tested. The possibility remains that long-term memory processes may be positively affected by low-dose nAChR antagonism, and Potter et al.’s word recognition paradigm may have tapped such processes. However, overall, impairments suggested by our and Potter et al.’s study would appear to outweigh any but very substantial benefits in circumscribed cognitive domains. Another limitation is that the present study only tested healthy volunteers, and beneficial effects may still be seen in specific clinical populations.
The question remains whether antagonists selective for specific nAChR subtypes may have cognitive-enhancing potential. Mecamylamine is an antagonist at all nAChR subtypes, but given its relatively weak potency at the α7 subtype (Meyer et al. 1997), it may have spared α7 nAChRs at the very low-dose range tested here. Low doses of the α7 nAChR antagonist MLA have been reported to improve stimulus detection in a rat model of attention with an inversely U-shaped dose-response function (maximum effect at 0.4 mg/kg; Hahn et al. 2011). Thus, the possibility that low doses of α7 nAChR antagonists have cognitive benefits deserves additional study.
The finding that both RVIPT performance indices showed trends suggesting mecamylamine-induced impairment may be reflective of the fact that the RVIPT is the most challenging task. Beyond rapidly processing the digits, the task requires an odd/even decision and working memory update every 600 ms, without pause, for 15 min at a time. The average hit rate was below 50 % for this task, and no participant approached ceiling. This may suggest that cognitive task performance is most sensitive to impairment by nAChR antagonism when processing capacity is taxed to the limit. Previous results with a larger dose of mecamylamine (7.5 mg), reported in abstract form (Hahn et al. 2014), were consistent with larger effects under more taxing task conditions. In that study, mecamylamine slowed N-back RT particularly in the hardest (2-back) condition, and slowed SARAT RT in nonpredictive cue trials only in a task block that was twice as long as other blocks, presumably challenging sustained attention processes.
In summary, the present study did not support the hypothesized cognitive-enhancing potential of low doses of mecamylamine. Contrary to preclinical reports, the present findings speak against low-dose nAChR antagonism as a novel avenue for treating cognitive deficits.
References
Adams CE, Stevens KE (2007) Evidence for a role of nicotinic acetylcholine receptors in schizophrenia. Front Biosci 12:4755–4772
Buccafusco JJ, Beach JW, Terry AV (2009) Desensitization of nicotinic acetylcholine receptors as a strategy for drug development. J Pharmacol Exp Ther 328:364–370
Cousineau D (2007) Confidence intervals in within-subject designs: a simpler solution to Loftus and Masson’s method. Tutor Quant Methods Psychol 1:42–45
Foulds J, Stapleton J, Swettenham J, Bell N, McSorley K, Russell MAH (1996) Cognitive performance effects of subcutaneous nicotine in smokers and never-smokers. Psychopharmacology 127:31–38
Gitelman DR, Prohovnik I (1992) Muscarinic and nicotinic contributions to cognitive function and cortical blood flow. Neurobiol Aging 13:313–318
Grier JB (1971) Nonparametric indexes for sensitivity and bias—computing formulas. Psychol Bull 75:424–429
Grottick AJ, Higgins GA (2000) Effect of subtype selective nicotinic compounds on attention as assessed by the five-choice serial reaction time task. Behav Brain Res 117:197–208
Hahn B, Ross TJ, Stein EA (2006) Neuroanatomical dissociation between bottom-up and top-down processes of visuospatial selective attention. NeuroImage 32:842–853
Hahn B, Ross TJ, Yang Y, Kim I, Huestis MA, Stein EA (2007) Nicotine enhances visuospatial attention by deactivating areas of the resting brain default network. J Neurosci 27:3477–3489
Hahn B, Shoaib M, Stolerman IP (2011) Selective nicotinic receptor antagonists: effects on attention and nicotine-induced attentional enhancement. Psychopharmacology 217:75–82
Hahn B, Harvey AN, Concheiro-Guisan M, Huestis MA, Holcomb HH, Gold JM (2013) A test of the cognitive self-medication hypothesis of tobacco smoking in schizophrenia. Biol Psychiatry 74:436–443
Hahn B, Harvey AN, Fischer B, Keller W, Ross TJ, Stein EA (2014) Nicotinic modulation of the default network of resting brain function in non-smokers. American College of Neuropsychopharmacology 53rd Annual Meeting, Poster Number M216
Haydar SN, Dunlop J (2010) Neuronal nicotinic acetylcholine receptors—targets for the development of drugs to treat cognitive impairment associated with schizophrenia and Alzheimer’s disease. Curr Top Med Chem 10:144–152
Heishman SJ, Kleykamp BA, Singleton EG (2010) Meta-analysis of the acute effects of nicotine and smoking on human performance. Psychopharmacology 210:453–469
Hurst R, Rollema H, Bertrand D (2013) Nicotinic acetylcholine receptors: from basic science to therapeutics. Pharmacol Ther 137:22–54
Kendziorra K, Wolf H, Meyer PM, Barthel H, Hesse S, Becker GA, Luthardt J, Schildan A, Patt M, Sorger D, Seese A, Gertz H-J, Sabri O (2011) Decreased cerebral a4ß2* nicotinic acetylcholine receptor availability in patients with mild cognitive impairment and Alzheimer’s disease assessed with positron emission tomography. Eur J Nucl Med Mol Imaging 38:515–525
Levin ED, Caldwell DP (2006) Low-dose mecamylamine improves learning of rats in the radial-arm maze repeated acquisition procedure. Neurobiol Learn Mem 86:117–122
Levin ED, Rezvani AH (2002) Nicotinic treatment for cognitive dysfunction. Curr Drug Targets CNS Neurol Disord 1:423–431
Levin ED, Castonguay M, Ellison GD (1987) Effects of the nicotinic receptor blocker mecamylamine on radial-arm maze performance in rats. Behav Neural Biol 48:206–212
Levin ED, Cauley M, Rezvani AH (2013) Improvement of attentional function with antagonism of nicotinic receptors in female rats. Eur J Pharmacol 702:269–274
Little JT, Johnson DN, Minichiello M, Weingartner H, Sunderland T (1998) Combined nicotinic and muscarinic blockade in elderly normal volunteers: cognitive, behavioral, and physiologic responses. Neuropsychopharmacology 19:60–69
Loeb M, Alluisi EA (1984) Theories of vigilance. In: Warm JS (ed) Sustained attention in human performance. Wiley, London, pp. 179–205
Martin LF, Kem WR, Freedman R (2004) Alpha-7 nicotinic receptor agonists: potential new candidates for the treatment of schizophrenia. Psychopharmacology 174:54–64
McNair DM, Lorr M, Droppleman LF (1971) Profile of mood states manual. Educational and Industrial Testing Service, San Diego, CA
Meyer EM, Tay ET, Papke RL, Meyers C, Huang GL, deFiebre CM (1997) 3-[2,4-Dimethoxybenzylidene]anabaseine (DMXB) selectively activates rat alpha 7 receptors and improves memory-related behaviors in a mecamylamine-sensitive manner. Brain Res 768:49–56
Morey RD (2008) Confidence intervals from normalized data: a correction of Cousineau (2005). Tutor Quant Methods Psychol 4:61–64
Nagahara AH, Handa RJ (1999) Fetal alcohol-exposed fats exhibit differential response to cholinergic drugs on a delay-dependent memory task. Neurobiol Learn Mem 72:230–243
Newhouse PA, Potter A, Corwin J, Lenox R (1992) Acute nicotinic blockade produces cognitive impairment in normal humans. Psychopharmacology 108:480–484
Newhouse PA, Potter A, Singh A (2004) Effects of nicotinic stimulation on cognitive performance. Curr Opin Pharmacol 4:36–46
Perry E, Martin-Ruiz C, Lee M, Griffiths M, Johnson M, Piggott M et al (2000) Nicotinic receptor subtypes in human brain ageing, Alzheimer and Lewy body diseases. Eur J Pharmacol 393:215–222
Petrovsky N, Quednow BB, Ettinger U, Schmechtig A, Mossner R, Collier DA, Kuhn KU, Maier W, Wagner M, Kumari V (2010) Sensorimotor gating is associated with CHRNA3 polymorphisms in schizophrenia and healthy volunteers. Neuropsychopharmacology 35:1429–1439
Picciotto MR, Addy NA, Mineur YS, Brunzell DH (2008) It is not “either/or”: activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Prog Neurobiol 84:329–342
Pickworth WB, Fant RV, Butschky MF, Henningfield JE (1997) Effects of mecamylamine on spontaneous EEG and performance in smokers and non-smokers. Pharmacol Biochem Behav 56:181–187
Pimlott SL, Piggott M, Owens J, Greally E, Court JA, Jaros E et al (2004) Nicotinic acetylcholine receptor distribution in Alzheimer’s disease, dementia with Lewy bodies, Parkinson’s disease, and vascular dementia: in vitro binding study using 5-[(125)I]-A-85380. Neuropsychopharmacology 29:108–116
Potter AS, Ryan KK, Newhouse PA (2009) Effects of acute ultra-low dose mecamylamine on cognition in adult attention-deficit/hyperactivity disorder (ADHD). Hum Psychopharmacol 24:309–317
Quick MW, Lester RAJ (2002) Desensitization of neuronal nicotinic receptors. J Neurobiol 53:457–478
Radek RJ, Kohlhaas KL, Rueter LE, Mohler EG (2010) Treating the cognitive deficits of schizophrenia with alpha4beta2 neuronal nicotinic receptor agonists. Curr Pharm Des 16:309–322
Singh A, Potter A, Newhouse P (2004) Nicotinic acetylcholine receptor system and neuropsychiatric disorders. IDrugs. 7:1096–1103
Singh A, Das DK, Kelley ME (2006) Mecamylamine (Targacept). IDrugs 9:205–217
Stolerman IP, Goldfarb T, Fink R, Jarvik ME (1973) Influencing cigarette smoking with nicotine antagonists. Psychopharmacologia 28:247–259
Stolerman IP, Mirza NR, Shoaib M (1995) Nicotine psychopharmacology: addiction, cognition and neuroadaptation. Med Res Rev 15:47–72
Terry AV, Buccafusco JJ, Prendergast MA (1999) Dose-specific improvements in memory-related task performance by rats and aged monkeys administered the nicotinic-cholinergic antagonist mecamylamine. Drug Dev Res 47:127–136
Wallace TL, Ballard TM, Pouzet B, Riedel WJ, Wettstein JG (2011) Drug targets for cognitive enhancement in neuropsychiatric disorders. Pharmacol Biochem Behav 99:130–145
Warburton DM, Mancuso G (1998) Evaluation of the information processing and mood effects of a transdermal nicotine patch. Psychopharmacology 135:305–310
Wesnes K, Warburton DM (1984) Effects of scopolamine and nicotine on human rapid information-processing performance. Psychopharmacology 82:147–150
Wing VC, Wass CE, Soh DW, George TP (2012) A review of neurobiological vulnerability factors and treatment implications for comorbid tobacco dependence in schizophrenia. Addiction Reviews 1248:89–106
Young JM, Shytle RD, Sanberg PR, George TP (2001) Mecamylamine: new therapeutic uses and toxicity/risk profile. Clin Ther 23:532–565
Acknowledgments
We would like to thank Franklin Blatt (Pharm. D.) for generating the study capsules and preparing blinded treatments for study days. We would like to thank Dr. Ian Stolerman for insightful comments on this manuscript and Drs. Mariel Herbert and Joshua Chiapelli for their help with screening participants. This work was supported by a grant from the National Institute on Drug Abuse (grant number R01 DA035813 to B.H.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Participants were recruited from the local community through internet advertising, flyers, and referrals and gave written informed consent for a protocol approved by the University of Maryland Baltimore Institutional Review Board.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Yuille, M.B., Olmstead, C.K., Wells, A.K. et al. A test of the cognitive-enhancing potential of low-dose mecamylamine in healthy non-smokers. Psychopharmacology 234, 109–116 (2017). https://doi.org/10.1007/s00213-016-4443-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-016-4443-2