Abstract
Exercise training (ET) has several health benefits; however, our understanding of regional adaptations to ET is limited. We examined the functional and molecular adaptations to short- and long-term ET in elastic and muscular conduit arteries of db/db mice in relation to changes in cardiovascular risk factors. Diabetic mice and their controls were exercised at moderate intensity for 4 or 8 weeks. The vasodilatory and contractile responses of thoracic aortae and femoral arteries isolated from the same animals were examined. Blood and aortic samples were used to measure hyperglycemia, oxidative stress, inflammation, dyslipidemia, protein expression of SOD isoforms, COX, eNOS, and Akt. Short-term ET improved nitric oxide (NO) mediated vasorelaxation in the aortae and femoral arteries of db/db mice in parallel with increased SOD2 and SOD3 expression, reduced oxidative stress and triglycerides, and independent of weight loss, glycemia, or inflammation. Long-term ET reduced body weight in parallel with reduced systemic inflammation and improved insulin sensitivity along with increased SOD1, Akt, and eNOS expression and improved NO vasorelaxation. Exercise did not restore NOS- and COX-independent vasodilatation in femoral arteries, nor did it mitigate the hypercontractility in the aortae of db/db mice; rather ET transiently increased contractility in association with upregulated COX-2. Long-term ET differentially affected the aortae and femoral arteries contractile responses. ET improved NO-mediated vasodilation in both arteries likely due to collective systemic effects. ET did not mitigate all diabetes-induced vasculopathies. Optimization of the ET regimen can help develop comprehensive management of type 2 diabetes.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Exercise training (ET) is a cornerstone in the management of type 2 diabetes. ET is associated with reduced cardiovascular risk factors (Hejazi et al. 2023), diabetes complications (Rietz et al. 2022), and all-cause mortality (Liu et al. 2022b) Importantly, ET has no major adverse effects (Blond et al. 2020). Unfortunately, many patients have reduced exercise capacity (Joshi et al. 2010), which can be further exacerbated by aging or other comorbidities, depriving many diabetic patients from ET benefits. The molecular mechanisms underlying the beneficial effects of ET have yet to be fully discovered; elucidation of these mechanisms can direct us to novel drug targets with minimum adverse effects.
Endothelial dysfunction is the hallmark of diabetic vascular complications; a healthy endothelium improves blood flow and prevents atherosclerosis and thrombosis (Brunner et al. 2005). Endothelial dysfunction is an independent predictor of cardiovascular events and death in diabetic patients (Lerman and Zeiher 2005; Bertoluci et al. 2015). Many cardiometabolic risk factors typically co-exist in diabetic subjects including obesity, hyperglycemia, insulin resistance, oxidative stress, inflammation, and dyslipidemia. Body weight and inflammation are key determinants of endothelial dysfunction in the aortae of db/db mice (Sallam et al. 2011). It is unknown if the vascular benefits of ET are dependent on changes in body weight or inflammation in db/db mice.
Endothelial and vascular smooth muscles cells exhibit heterogenous properties in different vascular beds under physiological and diabetic conditions (Sallam and Laher 2020; Zelinskaya et al. 2021). Both endothelial and vascular smooth muscles cells show marked heterogeneity with respect to their phenotypes (Frid et al. 1997), receptors subtypes (Zheng et al. 2008), ion channels subtypes and density (Cheong et al. 2001), signaling pathways (D’Angelis et al. 1998), and subcellular organelles (Michelakis et al. 1997). Evolving evidence indicates differential adaptations of different arteries to aging (Tschudi et al. 1996), high fat diet (Bhattacharya et al. 2008), and diabetes (Sallam and Laher 2020).
The effects of ET vary as a function of duration, frequency, and intensity (Tschakert et al. 2022; Connolly et al. 2022), but the effects of ET on regionally different arteries are unclear. Both the aorta and femoral artery are conduit/large arteries. However, they differ significantly in their structure and function. The femoral artery is a muscular artery which contains more smooth muscle cells in the tunica media than is present in elastic arteries such as the aorta which contain much more elastic tissues in the tunica media (Leloup et al. 2015). Previous studies reported significant differences in vascular responses of the aorta and femoral arteries to physiological or pathological stimuli including diabetes (Leloup et al. 2015; Sallam and Laher 2020; Sato et al. 2023; Balis et al. 2023; Liskova et al. 2023). Importantly, as our study focused on the regional effects of ET on vascular function, it was imperative to include femoral arteries which are exposed to exercise-induced hyperemia, high sheer stress, and local oxidative stress in contrast with the aorta, which is a more proximal, elastic, and larger artery. Importantly, the aorta is the most intensively examined artery in the literature and served as a useful comparator for our results.
We examined the effects of ET on the vasodilatory and contractile profiles of femoral arteries and aortae from db/db mice in relation to changes in cardiovascular risk factors and expression of endothelial nitric oxide synthase (eNOS), Akt, cyclooxygenase (COX), and superoxide dismutase isoforms (SOD) after 4 or 8 weeks of moderate intensity exercise. We hypothesized that short-term ET could reverse diabetes-induced perturbations in both vasodilatory and contractile functions in femoral arteries independent of systemic changes in cardiovascular risk factors, whereas ET benefits in the aortae would be dependent on systemic changes in body weight and inflammation and would require longer duration of ET.
Methods
Animals
Five weeks old male db/db mice (BKS.Cg-m +/+ Leprdb/J) and their age-matched normoglycemic heterozygous littermate controls (BKS.Cg-m+/+ Leprdb/+/J) were purchased from Jackson Laboratory (Bar Harbor, Maine, USA). The mice were housed under standardized conditions of temperature and light and had free access to standard rodent chow and water. Body weight and fasting blood glucose were recorded weekly. We selected db/db mice for this study as they show insulin resistance and hyperinsulinemia before hyperglycemia. Later, their pancreatic beta cells mass and insulin production drop mimicking the development of type 2 diabetes in humans (Dalbøge et al. 2013). The animal care protocol was approved by the University of British Columbia Animal Care Committee (A06-0308).
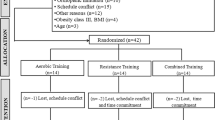
Exercise training protocol
Six- to nine-week-old db/db and control mice were randomly assigned to sedentary (sed) or exercise (ex) groups to yield four groups: db/db sed, db/db ex, control sed, and control ex. Mice assigned to the exercise groups underwent moderate intensity exercise on a motorized wheel system (Lafayette Instrument Co, Lafayette, IN, USA) for an hour a day, 5 days a week. The exercise regimen continued for either 4 or 8 weeks including an initial 2 weeks of acclimatization during which the wheel speed was gradually increased from 2.5 to 5.2 m/min less than 60% of the maximum speed (25 m/min) attained by C57Bl/6 J mice (Massett and Berk 2005). We used these two durations of ET to coincide with different stages of diabetes progression in db/db mice as plasma insulin levels peak at about 8–10 weeks of age then decline (Dalbøge et al. 2013; Sallam and Laher 2020). The effectiveness of the ET program was validated by examining the heart/body weight ratio and skeletal muscle citrate synthase activity.
Intraperitoneal glucose tolerance test
To minimize the acute effects of ET, mice were not exercised 24 h before undergoing glucose tolerance tests. Mice (10 or 14 weeks old) were fasted overnight and given a 40% glucose solution (2.0 g/kg, i.p.) in the morning. Blood samples were collected from the tail vein at zero, 15-, 30-, 60-, and 120-min post-glucose administration. Plasma was separated by centrifugation and stored at − 76 °C for later analyses of glucose (catalog # MAK263, Sigma-Aldrich, USA), and insulin (catalog # 80-INSMS-E01, ALPCO Diagnostic, USA) according to the manufacturers’ instructions. The area under the curve for plasma glucose or insulin levels was calculated using Prism version 5.0 (GraphPad software, USA). Insulin sensitivity index was calculated according to the formula of Matsuda and DeFronzo (Matsuda and DeFronzo 1999) with a minor modification; we used 100 instead of 10,000 as a numerator to yield more convenient numbers.
Plasma and tissues samples collection and analyses
Mice were anesthetized with pentobarbital (50 mg/kg, i.p.) combined with heparin (50 U/kg). Blood samples were withdrawn slowly from the inferior vena cava and centrifuged (10 min at 4 °C, 1000 g) to separate the plasma, which was aliquoted and snap frozen for later measurements of plasma glucose (catalog # MAK263, Sigma-Aldrich, USA), insulin (catalog # 80-INSMS-E01, ALPCO Diagnostics, USA), 8-isoprostane (catalog # 516,351, Cayman Chemical, USA), CRP (catalog # 41-CRPM-90E, ALPCO Diagnostics, USA); lipids were measured by Dade RXL analyzer system. To inhibit in vitro formation of 8-isoprostane, butylated hydroxy toluene (0.005%) was added to plasma aliquots destined for 8-isoprostane measurements. Mice hearts were removed after blood collection, blotted with filter papers, and weighed. The thoracic aortae and main femoral arteries were harvested and placed in ice-cold physiologic salt solution (PSS). Arteries were cleared of the adherent connective tissues and either snap-frozen and stored at − 76 °C for western blot analysis or suspended in wire myograph chambers for isometric force measurements. A part of the thigh adductor muscle was snap frozen for citrate synthase analysis. Frozen adductor muscles were homogenized in ice cold lysis buffer CelLytic™ MT (catalog # C 3228, Sigma-Aldrich, USA) then centrifuged at 4 °C for 30 min at 16,000 g. The supernatant was assayed for protein content using a Coomassie Plus Protein Assay (catalog # 23,236; Pierce-Thermo Fisher Scientific, USA). Ten microgram protein of each sample was analyzed for oxidative capacity using a citrate synthase assay kit (catalog # CS0720, Sigma-Aldrich, USA) according to the manufacturer’s instructions.
Assessment of vascular function
We used the thoracic aortae (internal diameter 0.68 + 0.02 mm) and the main femoral artery (internal diameter 0.24 + 0.01 mm). There were no significant differences in the internal diameters of the aortae, or femoral arteries between db/db and control mice. The arteries were cut into 2 mm long rings and mounted in a wire myograph system (Danish Myotechnology, Denmark) for isometric force measurement as described previously (Sallam et al. 2011). The optimum resting tension was 5.5 mN and 3 mN for the aortae and femoral arteries, respectively, as determined in preliminary experiments. PSS was prepared according to the following composition (mM): NaCl (119), KCl (4.7), KH2PO4 (1.18), MgSO4 (1.17), NaHCO3 (24.9), EDTA (0.023), CaCl2 (1.6), and dextrose (11.1). High concentrations of KCl (30 or 80 mM) solution were prepared by equimolar substitution of NaCl by KCl in PSS. The functional experiments were conducted on the aortae and femoral arteries isolated from the same animals and compared simultaneously under identical conditions.
Endothelium-dependent and -independent vasorelaxation
The aortic or femoral rings were constricted with a submaximal dose of the ɑ1-adrenoceptor agonist phenylephrine (PE) or the thromboxane A2 analogue U-46619, respectively, because PE did not yield stable contractions in femoral arteries. After a stable contraction was obtained, acetylcholine (ACh) (10−9 to 10−5 M) was added cumulatively at half-log increments to examine endothelium-dependent relaxation. After a 30-min washout period, the arterial rings were constricted again, and sodium nitroprusside (SNP), a direct nitric oxide (NO) donor, was added (10−10 to 10−5 M) to examine endothelium-independent relaxation. Responses to ACh or SNP were calculated as percent decrease in force with respect to the initial PE- or U-46619-induced contraction (% relaxation).
Contribution of NOS, COX, or NOS & COX independent pathways to ACh-induced vasorelaxation
Arterial rings were incubated with a NOS inhibitor (Nω-Nitro-L-arginine methyl ester [L-NAME]; 10−4 M), a COX inhibitor (indomethacin; 10−5 M), the combination of L-NAME and indomethacin, or for 30 min before the construction of ACh concentration response relationship.
Contractile responses
Responses to KCl (30 and 80 mM) and PE (10−9 M to 10−4 M) were examined in aortic and femoral rings. Responses to PE were examined in the presence or absence of COX inhibitor (indomethacin; 10−5 M). The contractile responses were presented as the net force generated (mN).
Western blotting
Aortic segments from 3 to 5 mice from the same treatment group were pooled to yield enough protein for western blot analysis. Frozen arteries were homogenized in ice-cold RIPA buffer (catalog# sc-24948, Santa Cruz Biotechnology, USA). The homogenates were centrifuged at 10,000 g for 30 min at 4 °C. The protein contents of the supernatants were determined by Coomassie Plus Protein Assay (catalog # 23,236, Pierce-Thermo Fisher Scientific, USA). Protein samples (30–40 μg total protein) were prepared in Laemmli sample buffer, separated by 12% or (8–10) % SDS-PAGE, then transferred overnight (at 4 °C, 40 V) to a nitrocellulose membrane. Next, the membranes were blocked for 1 h in 5% skim milk in Tris-buffered saline containing 0.05% Tween 20, then washed (3 × 15 min). The membranes were horizontally cut to probe target proteins with different molecular weights. The cut membranes were incubated overnight at 4 °C with primary antibodies against SOD1, SOD2, SOD3, Akt, COX-1, COX-2 (catalog# sc-17767, sc-133134, sc-271170, sc-5298, sc-1754, sc-1747; Santa Cruz Biotechnology, USA), eNOS (catalog# 32027S, Cell Signaling, USA), or β-actin (catalog# 612,656, BD, Canada). Membranes were washed (3 × 15 min) and incubated with their corresponding secondary antibodies for 2 h. After washing (3 × 15 min), the membranes were visualized using an enhanced chemiluminescent detection kit (catalog # 32,109; Pierce-Thermo Fisher Scientific, USA) using a ChemiDoc XRS imager (BioRad Laboratories, Canada). Volume analyses of the protein bands were performed using Quantity One software (BioRad Laboratories, USA). To control for variations in protein loading, band intensity of a specified protein was related to the band intensity of β-actin (a housekeeping protein).
Statistical analysis
Data are displayed as mean ± standard error (S.E.). Biochemical parameters and proteins expression were compared using two-way ANOVA followed by Bonferroni post hoc test. Changes in vascular function were analyzed using two-way repeated measures ANOVA followed by Bonferroni post hoc test. The correlation between vascular responses and biochemical parameters were examined using Pearson correlation coefficient. The citrate synthase activity of exercised groups vs sedentary groups was analyzed using unpaired t-test. The sample size of each group is specified as (n) in the footnote for each table or figure. Non-linear regression, maximum response (Emax), and statistical analyses were carried out using Prism version 5.0 (GraphPad software, USA). Statistically significant differences were set at p < 0.05.
Results
Efficacy of the ET program
The effectiveness of ET was confirmed by increases in skeletal muscle oxidative capacity, as indicated by increased citrate synthase activity after short-term ET in control mice (ex10–13wk old = 5.0 ± 0.06 μmole.min−1..ml−1 vs sed10–13wk old = 4.7 ± 0.05 μmole.min−1.ml−1, p < 0.05) and in db/db mice (ex10–13wk old = 3.9 ± 0.04 μmole.min−1.ml−1 vs sed10–13wk old = 3.6 ± 0.06 μmole.min−1.ml−1, p < 0.05). Similarly, there were increases in citrate synthase activity after long term ET in control mice (ex14–20 wk old = 6.61 ± 0.54 μmole.min−1.ml−1 vs sed14–20 wk old = 4.21 + 0.32 μmole.min−1.ml−1, p < 0.05) and db/db mice (ex14–20 wk old = 2.47 ± 0.24 μmole.min−1.ml−1 vs sed14–20 wk old = 1.6 ± 0.18 μmole.min−1.ml−1, p < 0.05). In addition, the heart/body weight ratios of control exercise group were higher than in control sedentary mice (0.43 ± 0.01% vs 0.39 ± 0.01%, p < 0.05). Similarly, exercised db/db (0.26 ± 0.01%) had higher heart/body weight ratios than sedentary db/db mice (0.23 ± 0.01%, p < 0.05).
Effect of ET on cardiovascular risk factors
Sedentary db/db mice aged 10–13 weeks had heavier body weights (45.87 ± 0.7 g vs 27.96 ± 0.3, p < 0.05) and were hyperglycemic (fasting glucose: 31.54 ± 1.3 mmol/L vs 5.03 ± 0.2 mmol/L, p < 0.05), glucose intolerant (GTT AUC: 5892 ± 161.5 vs 1234 ± 57.3, p < 0.05), with lower insulin sensitivity (1.13 ± 0.1 vs 23.66 ± 2.9, p < 0.05) than age-matched normoglycemic controls. They also showed hypertriglyceridemia, hypercholesterolemia, higher systemic oxidative stress (8-isoprostane: 210.9 ± 27.1 pg/mL vs 36.92 ± 6.2 pg/mL, p < 0.05), and inflammation (CRP: 4.05 ± 0.2 ng/mL vs 2.57 ± 0.3 ng/mL, p < 0.05) than age-matched normoglycemic controls (Table 1).
Four weeks of ET reduced plasma 8-isoprostane and triglycerides levels in db/db mice relative to their sedentary diabetic controls. Four weeks of ET` increased insulin sensitivity and elevated plasma CRP levels in normoglycemic mice compared with their sedentary controls (Table 1).
At 14–20 weeks of age, sedentary db/db mice showed more severe signs of diabetes. They were more obese (48.86 ± 1.2 g vs 45.87 ± 0.7 g, p < 0.05), more hyperglycemic (54.66 ± 1.5 mM vs 31.54 ± 1.3 mM, p < 0.05), more glucose intolerant (GTTglucose AUC: 10,059 ± 270.9 vs 5892 ± 161.5, p < 0.05), less able to secrete insulin (GTTinsulin AUC: 263.1 ± 21 vs 394.8 ± 43.5, p < 0.05), with higher levels of plasma CRP (5.12 ± 0.3 ng/mL vs 4.05 ± 0.2 ng/mL, p < 0.05), but lower cholesterol levels (2.71 ± 0.1 mM vs 3.77 ± 0.16 mM, p < 0.05) compared with 10–13-week-old sedentary db/db mice.
Long-term ET reduced the body weights of db/db mice and improved glycemic control as reflected by lower fasting plasma glucose levels and improved glucose tolerance. Additionally, long-term ET reduced plasma CRP level in db/db mice. Both short-term and long-term ET reduced plasma 8-isoprostane and triglycerides levels of db/db mice compared with sedentary db/db mice.
Long-term ET reduced body weight, and increased insulin sensitivity and plasma CRP levels in normoglycemic control mice (Table 1).
Exercise and vascular reactivity
Effect of short-term ET on vascular reactivity of the aortae and femoral arteries
Vasodilatory responses
Endothelium-dependent, ACh-induced vasodilation was impaired in the aortae and femoral arteries of db/db mice compared to their age matched normoglycemic controls. Endothelium-independent, SNP-induced vasorelaxation was impaired in the aortae, but not the femoral arteries of db/db mice. Short-term ET restored endothelium-dependent, ACh-induced relaxation in the aortae (Emax: db/db exaorta = 76.25 ± 1.32% vs db/db sedaorta = 57.58 ± 2.04%, p < 0.05) and femoral arteries of db/db mice (Emax: db/db exfemoral = 71.54 ± 1.41% vs db/db sedfemoral = 60.79 ± 1.74%, p < 0.05). Preincubation with L-NAME (10−4 M) abolished ACh vasorelaxation in the aortae of both sedentary and exercise groups, but did not abolish vasorelaxation in the femoral arteries, indicating that a significant proportion of femoral arteries relaxation was NO-independent. Pre-incubation with L-NAME and indomethacin nullified ET-induced improvement in ACh-induced vasodilatation in the femoral arteries of db/db mice, indicating that exercise improved NO and PGI2 mediated component in the vasorelaxation. Also, short-term ET improved endothelium-independent, SNP-induced relaxation in the aortae of db/db mice (Emax: db/db exaorta = 88.05 ± 1.36% vs db/db sedaorta = 74.98 ± 1.47%, p < 0.05) as shown in Fig. 1.
Cumulative concentration response curves of acetylcholine and sodium nitroprusside in the aortae and femoral of sedentary and exercise db/db and control mice at 10–13 weeks of age. Values are displayed as mean ± S.E. and represent n = 6–10 mice. Statistical analysis was done using two-way repeated measures ANOVA followed by Bonferroni post hoc test. * denotes p < 0.05 compared with sedentary normoglycemic group (10–13 weeks old); # denotes p < 0.05 compared with exercised normoglycemic group (10–13 weeks old); @ denotes p < 0.05 compared with exercised db/db group (10–13 weeks old)
Contractile responses
The aortae of db/db mice showed enhanced responses to both PE and KCl compared with their normoglycemic controls. Short-term ET further augmented the enhanced contractions in the aortae of db/db mice in response to 80 mM KCl (db/db exaorta = 7.83 ± 0.34 mN vs db/db sedaorta = 6.62 ± 0.48 mN, p < 0.05) and PE (Emax: db/db exaorta = 14.28 ± 0.21 mN vs db/db sedaorta = 12.71 ± 0.22 mN, p < 0.05). Preincubation with indomethacin (10−5 M) reduced PE contractions in the aortae of both exercised and sedentary db/db mice and abolished the difference between the two groups, suggesting a role for COX in ET-induced hypercontractility in the aortae of db/db mice. In contrast to responses in the aorta, the femoral artery of db/db mice showed reduced contractile responses to PE and KCl compared with normoglycemic mice. Similar to its effects on the aortae, ET augmented KCl induced contraction (Emax: db/db exfemoral = 4.14 ± 0.25 mN vs db/db sedfemoral = 3.02 ± 0.22 mN, p < 0.05) and PE triggered contraction (Emax: db/db exfemoral = 3.13 ± 0.16 mN vs db/db sedfemoral = 1.94 ± 0.1 mN, p < 0.05) in femoral arteries of db/db mice. Exercise also enhanced KCl contractions in normoglycemic control mice (Emax: control exfemoral = 5.7 ± 0.78 mN vs control sedfemoral = 4.53 ± 0.78 mN, p < 0.05) (Fig. 2).
Contractile responses to KCl and phenylephrine in the aortae and femoral arteries of sedentary and exercise db/db and normoglycemic mice at 10–13 weeks of age. Values are displayed as mean ± S.E. and represent n = 6–10 mice. Statistical analysis was done using two-way repeated measures ANOVA followed by Bonferroni post hoc test. * denotes p < 0.05 compared with sedentary normoglycemic group (10–13 weeks old), # denotes p < 0.05 compared with exercised normoglycemic group (10–13 weeks old), $ denotes p < 0.05 compared with sedentary db/db group (10–13 weeks old), @ denotes p < 0.05 compared with exercised db/db (10–13 weeks old)
Effect of long-term ET on vascular reactivity of the aortae and femoral arteries
Vasodilatory responses
Similar to effects of short-term ET, long-term ET continued to improve ACh-induced, NO-mediated vasorelaxation in the aortae and femoral arteries of db/db mice, but did not restore L-NAME- and indomethacin-resistant component of vasodilation in femoral arteries. Long-term ET also enhanced SNP-induced vasorelaxation in the aortae of db/db mice (Fig. 3).
Cumulative concentration response curves of acetylcholine and sodium nitroprusside in the aortae and femoral of sedentary and exercise db/db and normoglycemic mice at 14–20 weeks of age. Values are displayed as mean ± S.E. and represent n = 6–10 mice. Statistical analysis was done using two-way repeated measures ANOVA followed by Bonferroni post hoc test. * denotes p < 0.05 compared with sedentary normoglycemic group (14–20 weeks old); # denotes p < 0.05 compared with exercised normoglycemic group (14–20 weeks old); @ denotes p < 0.05 compared with exercised db/db group (14–20 weeks old)
Contractile responses
Unlike the effects of short-term ET, long-term ET (8 weeks) did not augment the contraction in response to KCl (80 mM) or PE in the aortae of db/db mice. However, long-term ET did not restore the aortic contractions in db/db mice to the magnitude observed in normoglycemic mice. Long-term ET augmented KCl-induced contractions in the femoral arteries of db/db mice (Emax: db/db exfemoral = 5.1 ± 0.32 mN vs db/db sedfemoral = 3.78 ± 0.28 mN, p < 0.05) without altering PE-induced contractions, whereas it reduced PE-induced contractions in normoglycemic control mice (Fig. 4).
Contractile responses to KCl and phenylephrine in the aortae and femoral arteries of sedentary and exercise db/db and normoglycemic mice at 14–20 weeks of age. Values are displayed as mean ± S.E. and represent n = 6–10 mice. Statistical analysis was done using two-way repeated measures ANOVA followed by Bonferroni post hoc test. * denotes p < 0.05 compared with sedentary normoglycemic group (14–20 weeks old); # denotes p < 0.05 compared with exercised normoglycemic group (14–20 weeks old); $ denotes p < 0.05 compared with sedentary db/db group (14–20 weeks old)
Correlation analysis of the cardiovascular risk factors and vascular responses
ET restored ACh-induced vasodilatation in the aortae and femoral arteries of db/db mice in parallel with reduced levels of plasma glucose, markers of systemic oxidative stress and inflammation, and triglycerides. However, the relative contributions of these effects to altered vasodilatation or vasoconstriction are unknown. Correlation analysis revealed that ACh maximum responses in the aortae were negatively associated with body weight, plasma glucose, 8-isoprostane, and triglycerides. In the femoral artery, ACh maximum responses were negatively associated with body weight, plasma glucose, and cholesterol. The maximum contractile responses to PE were positively correlated with body weight, plasma glucose, 8-isoprostane, CRP, and cholesterol in the aortae, whereas in the femoral arteries, PE maximum responses were negatively correlated with plasma glucose, 8-isoprostane, and triglycerides, suggesting substantial heterogeneity of vascular responses between regionally different arteries. These results suggest that the beneficial effects of exercise are likely mediated by a collective (and not a single action) of ET (Table 2).
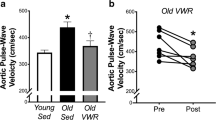
ET and expression of aortic proteins
Short-term ET increased protein expression of SOD2 and SOD3 in the aortae of db/db mice compared with sedentary db/db mice. Short-term ET also increased the protein contents of eNOS and Akt in the aortae of normoglycemic control mice compared with their sedentary controls. Long-term ET increased the expression of SOD1, eNOS, and Akt expression in the aortae of db/db mice compared with sedentary db/db. Exercise did not alter the aortic protein content of COX-1; however, levels of COX-2 were increased by short (4 weeks) but not long-term (8 weeks) ET in the aortae of db/db and control mice compared with sedentary mice (Fig. 5).
Representative blots and bar graph of the protein expression of SOD1, SOD2, SOD3, eNOS, Akt, and COX-2 in the aortae of sedentary and exercise db/db and normoglycemic mice. Values are displayed as mean ± S.E. and represent n = 4–6 independent experiments. Statistical analysis was done using two-way ANOVA followed by Bonferroni post hoc test. $ denotes p < 0.05 compared with sedentary db/db group; @ denotes p < 0.05 compared with exercised db/db group; ɑ denotes p < 0.05 compared with sedentary normoglycemic group
Discussion
We investigated the effects of two durations of ET on various aspects of vasodilatory and contractile responses in two regionally different arteries (aortae and femoral arteries) of db/db mice and their normoglycemic controls. We examined both endothelium-dependent (NO-mediated and NO-independent) and endothelium independent vasodilatation as well as receptor-dependent and -independent contractile responses in parallel with alterations in cardiovascular risk factors and proteins which play key roles in the vasculature. The functional experiments were conducted on the aortae and femoral arteries isolated from the same animals and compared simultaneously under identical conditions.
Short-term ET and NO-mediated vasodilatation
Short-term ET restored ACh-induced relaxation in the aortae and femoral arteries of db/db mice (Fig. 1) in association with reduced plasma 8-isoprostane and triglyceride levels (Table 1) and increased aortic expression of SOD2 and extracellular SOD3 (Fig. 5) without concurrent changes in body weights (Table 1). Our findings are in agreement with previous reports that ET improved vasodilatation independent of weight loss in diabetic (Green et al. 2003) and obese subjects (Mestek et al. 2010). An acute bout of exercise promotes blood flow to actively contracting skeletal muscles to meet their increased energy needs during exercise (exercise-induced hyperemia). The increased blood flow mechanically stimulates endothelial cells in skeletal muscles feed arteries via increased intraluminal shear stress and pressure leading to upregulation of eNOS expression and NO synthesis (Woodman et al. 2018). In agreement with our results are findings that treatment with rosiglitazone and metformin ameliorated vascular dysfunction in diabetic subjects without changing body weight or glycemic control (Bagi et al. 2004; Matsumoto et al. 2008). The benefit of exercise in improving cardiovascular health in obese individuals independent of weight loss is well established (Gaesser et al. 2011) and could be secondary to suppressing the downstream effects of obesity, mainly oxidative stress and dyslipidemia rather than reducing obesity directly.
Exercise increases oxygen demand and cellular respiration of skeletal muscles resulting in generation of reactive oxygen species (ROS) (Ji et al. 2006). It is known that just 1 h of endurance exercise results in increased oxidant production (Dillard et al. 1978). However, regular/repeated bouts of exercise results in adaptive changes that leads to upregulation of cellular antioxidant systems (Powers et al. 2016). Similar responses also occur in tissues other than skeletal muscles; ET increased protein expression of SOD isoforms in arteries (Lee et al. 2011), the heart (Moien-Afshari et al. 2008), and the liver (Chang et al. 2004). We observed a reduction in plasma 8-isoprostane, a marker of systemic oxidative stress (Table 1) that occurred in parallel with increased aortic SOD2 and SOD3 expression in db/db mice following 4 weeks of ET (Fig. 5), suggesting that the effects of ET were generalized and not limited to the skeletal muscles or the aortae. Reducing oxidative stress could explain, at least in part, how short-term ET improved vasodilatation in the aortae of db/db mice since ROS interfere with NO signaling at multiple steps: eNOS activation, NO degradation, soluble guanylyl cyclase activation, and/or contractile apparatus functioning (De Vriese et al. 2000; Félétou and Vanhoutte 2006). However, antioxidants have not shown significant therapeutic benefits in diabetic patients (Heart Protection Study Collaborative Group 2002; Kataja-Tuomola et al. 2010), suggesting that reducing oxidative stress may not be the sole mechanism by which ET improves vasodilatation. Indeed, short-term ET also reduced plasma triglycerides in db/db mice (Table 1). Earlier studies have showed that triglycerides levels can predict cardiovascular events and death (Hanefeld et al. 1996; Bansal et al. 2007) and that dyslipidemia plays a key role in the endothelial dysfunction in diabetic patients (Watts et al. 1996). The Steno-2 trial applied a multiple risk factor reduction strategy and concluded that lipid-lowering rather than glycemic control accounted for the major reduction of cardiovascular events in type 2 diabetic patients (Gæde and Pedersen 2004).
Long-term ET and NO-mediated vasodilatation
Long-term ET improved NO-mediated vasodilatation in aortae and femoral arteries of db/db mice (Fig. 3) in parallel with reductions in oxidative stress and triglycerides levels similar to short-term ET. Additionally, long-term ET decreased body weight, improved glycemic control, and suppressed systemic inflammation (Table 1) likely due to the decrease in the fat mass as many of proinflammatory cytokines are released directly from adipocytes and adipose tissue-derived macrophages (Berg and Scherer 2005). Regarding vascular homeostasis, long-term ET increased the aortic expression of SOD1, eNOS, and Akt in db/db mice (Fig. 5), suggesting that long-term ET improved vasodilatation by increasing NO bioavailability by upregulating NO synthesis and decreasing its breakdown. The multifaceted effects of ET could explain the greater efficacy of exercise over other interventions such as food restriction (Sakamoto et al. 1998), insulin treatment (Aas et al. 2006), or antioxidant supplements (MRC/BHF Heart Protection Study 2002; Kataja-Tuomola et al. 2010). Our correlation analysis (Table 2) suggests that ACh maximum responses in the aortae and femoral arteries were negatively associated with body weight, plasma glucose, 8-isoprostane, and triglycerides in the aortae and with body weight, plasma glucose and cholesterol in the femoral arteries. Therefore, a corresponding multifactorial pharmacological intervention like ET is probably the optimal therapeutic strategy for diabetic patients who can’t exercise regularly.
ET and NO-independent vasodilation
Pretreatment of femoral arteries with L-NAME and indomethacin did not abolish ACh-induced vasodilatation, indicating a significant contribution of a NOS- and COX-independent component, generally identified as endothelium dependent hyperpolarizing factor (EDHF). Neither the short- nor long-term ET regimen used in this study improved EDHF effects in the femoral arteries of db/db mice (Figs. 1 and 3). Other studies reported that ET improved NO-mediated vasorelaxation, but not EDHF-mediated pathway in rats with heart failure (Kemi et al. 2013) and that passive leg movement induced NO but not EDHF-mediated hyperemia in healthy males (Trinity et al. 2021). In contrast, some studies reported that ET improved EDHF mediated vasodilatation in the aortae and arteries from the gastrocnemius muscles of aged rats (Huang et al. 2019), suggesting that the nature of EDHF could vary in different animal models and in different blood vessels.
Short-term ET and vasoconstriction
Vascular dysfunction in diabetes also involves altered contractile responses. Our results show augmented contractile responses in the aortae of db/db mice, whereas femoral arteries showed attenuated contractility compared to the normoglycemic control group (Figs. 2 and 4). Previous studies reported heterogenous results regarding PE-mediated vascular contractile responses in diabetic subjects (Yang et al. 2020; Sallam and Laher 2020); some reported augmented responses (Abebe et al. 1990; Nobe et al. 2002), while other reported attenuated contractility (Ma et al. 2008; Nobe et al. 2012). Nevertheless, there is an agreement that there is a dysregulation of Ca2+ handling in vascular tissues in diabetic subjects. Apparently, the outcome depends on the anatomical site of the artery examined, stage of diabetes, and the intracellular signaling system involved (Yang et al. 2020; Sallam and Laher 2020), including type and concentration of ROS generated locally and their cellular target(s) (Lounsbury et al. 2000). For example, PE-induced vasoconstriction mediated by L-type calcium (Cav1.2) channels was attenuated, while contractions mediated by store-operated calcium channels and sarcoplasmic reticulum calcium release were enhanced in the aortae of diabetic rats (Yang et al. 2020). In agreement with our results, augmented contractile responses were reported in the aortae of db/db mice and were attributed to increased protein expression of the activated form of CPI-17 and RhoA (Xie et al. 2006) and increased activity of Rho kinase (Nuno et al. 2009) possibly leading to increased calcium sensitization. The role of oxidative stress in vascular hypercontractility observed in diabetes is confirmed in numerous studies (Kanie and Kamata 2000; Félétou and Vanhoutte 2006; Shi et al. 2007). For example, Kanie and Kamata (2000) reported that the enhanced norepinephrine contractions in the aortae of db/db were reduced by SOD, whereas norepinephrine contractile responses in control mice were enhanced by an inhibitor of SOD1. ROS can directly depolarize cell membranes (Kourie 1998), inhibit potassium channels (Gutterman et al. 2005), facilitate the release of calcium from intracellular stores (Lounsbury et al. 2000; Forman et al. 2002), and/or enhance the formation of vasoconstrictor isoprostanes from plasma membrane lipids (Cracowski et al. 2002). On the other hand, attenuated vasoconstrictions in diabetic models were frequently attributed to upregulation of iNOS (Cheng and Pang 2004; Lee et al. 2008), dysregulation of COX (Marrachelli et al. 2006; Shi and Vanhoutte 2008), impairment in L-type calcium channels, and/or transformation of vascular smooth muscles from contractile phenotypes to proliferative phenotypes (Yang et al. 2020).
Although short-term ET restored vasodilatation in the aortae of db/db mice (Fig. 1), it did not mitigate augmented contractile responses but rather exacerbated them (Fig. 2). Short-term ET also restored the attenuated contractile responses to KCl and PE in the femoral arteries of db/db mice (Fig. 2). Several studies reported that ET enhanced vasoconstriction under physiological (McAllister and Laughlin 1997; Sugawara et al. 2007; Just and DeLorey 2016) and diabetic (Setty et al. 2004) conditions. It has been proposed that ET modulates sympathetic receptor responsiveness to balance the pronounced exercise-induced vasodilatation to prevent a significant drop in peripheral resistance (Just et al. 2016). However, our results show that ET training augmented both receptor-dependent and -independent vasoconstriction and that pretreatment with indomethacin suppressed the augmented aortic vasoconstriction in exercised db/db mice (Fig. 2), suggesting that COX mediated ET-induced vascular hypercontractility in the aortae, as supported by an increase in the aortic protein expression of COX-2 (Fig. 5). Increased COX expression and/or activity are associated with enhanced vasoconstriction in different disease models (de Oliveira et al. 2021; Dourado et al. 2023).
In the femoral arteries, short-term ET mitigated the attenuated contractile responses likely via modulating the sympathetic system to balance concurrently induced vasodilatation to prevent a significant drop in peripheral resistance (Just et al. 2016; Orssatto et al. 2018). It is also possible that ET upregulation of antioxidant systems in skeletal muscle vasculature leads to reduced local oxidative stress (Powers et al. 2016) and consequently mitigates the detrimental effects of ROS on calcium handling machinery in femoral arteries (Liu et al. 2019). There is evidence that ET-induced hypercontractility is exaggerated in diabetes, in part, due to an exaggerated exercise pressor reflex through unknown mechanisms. This exaggerated exercise pressor reflex could increase the risk of adverse cardiovascular events during and after exercise (Grotle et al. 2020).
Long-term ET and vasoconstriction
Some effects of exercise are duration dependent (Liu et al. 2022a). Our study shows that ET-induced aortic hypercontractility (Fig. 2) was transient and was absent after 8 weeks of exercise (Fig. 4) in parallel with short-term upregulation of aortic COX-2 expression (Fig. 5). However, long-term ET could not normalize the enhanced contractile responses in the aortae of db/db mice. Long-term ET enhanced contractile responses to KCl, but not PE in the femoral arteries of db/db, and reduced PE contractile responses in normoglycemic mice, suggesting local vascular sympathetic downregulation that could result from alterations in postsynaptic adrenergic receptors after repeated bouts of exercise (Delorey 2021).
ET and regional vascular heterogeneity
One of the strengths of this study is that the aortae and femoral arteries examined were isolated from the same animals and were assessed simultaneously under similar experimental conditions to minimize methodological variability. Our study shows that ET improvement of endothelium-dependent, NO-mediated, vasodilatation is likely a systemic adaptation, as it affected both the aortae and femoral arteries similarly. Also, the maximum vasodilatory responses in both arteries were negatively correlated with body weight and blood glucose levels. However, local differences exist, as the ACh maximum vasodilatory response in the aortae was negatively correlated with plasma 8-isoprostane and triglycerides, whereas in the femoral arteries, it was negatively correlated with plasma cholesterol (Table 2). Regarding vascular contractility, short-term ET caused transient increases in the contractile responses in both the aortae and femoral arteries. Long-term ET affected the aortae and femoral arteries contractile responses differently. Therefore, the effects of ET on vasomotor function of the aortae and the femoral arteries were mostly consistent and were probably triggered by systemic changes in glycemic control, oxidative stress, and inflammation.
Limitation
Due to funding constrains and large number of animals required for this study, we were unable to examine both male and female mice.
Conclusion
Our study examined both vasodilatory and contractile functions of two different arteries, coupled with measurements of molecular and biochemical changes produced by short-and long-term ET. The ET protocols used in our study enhanced NO-mediated vasodilatation but did not reverse all the detrimental effects of diabetic milieu on other vascular functions. Further research is needed for optimizing the structure of the ET program for comprehensive management of type 2 diabetes and for elucidating the upstream trigger of the multifaceted actions of ET.
Data availability
Data of the study are available from the corresponding author upon request.
Abbreviations
- COX:
-
Cyclooxygenase
- CRP:
-
C-reactive protein
- EDHF:
-
Endothelium-dependent hyperpolarizing factor
- ET:
-
Exercise training
- eNOS:
-
Endothelial nitric oxide synthase
- GTT:
-
Glucose tolerance test
- PE:
-
Phenylephrine
- mN:
-
Millinewton
- L-NAME:
-
Nω-Nitro-L-arginine methyl ester
- PSS:
-
Physiologic salt solution
- R:
-
Pearson correlation coefficient
- Sed:
-
Sedentary
- SOD:
-
Superoxide dismutase
References
Aas A-M, Seljeflot I, Torjesen PA et al (2006) Blood glucose lowering by means of lifestyle intervention has different effects on adipokines as compared with insulin treatment in subjects with type 2 diabetes. Diabetologia 49:872–880. https://doi.org/10.1007/S00125-006-0205-8
Abebe W, Harris KH, MacLeod KM (1990) Enhanced contractile responses of arteries from diabetic rats to α1-adrenoceptor stimulation in the absence and presence of extracellular calcium. J Cardiovasc Pharmacol 16:239–248. https://doi.org/10.1097/00005344-199008000-00010
Bagi Z, Koller A, Kaley G (2004) PPARγ activation, by reducing oxidative stress, increases NO bioavailability in coronary arterioles of mice with type 2 diabetes. American Journal of Physiology-Heart and Circulatory Physiology 286:H742–H748. https://doi.org/10.1152/AJPHEART.00718.2003
Balis P, Berenyiova A, Misak A et al (2023) The phthalic selenoanhydride decreases rat blood pressure and tension of isolated mesenteric, femoral and renal arteries. Molecules 28:4826. https://doi.org/10.3390/molecules28124826
Bansal S, Buring JE, Rifai N et al (2007) Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA 298:309. https://doi.org/10.1001/JAMA.298.3.309
Berg AH, Scherer PE (2005) Adipose tissue, inflammation, and cardiovascular disease. Circ Res 96:939–949. https://doi.org/10.1161/01.RES.0000163635.62927.34
Bertoluci MC, Cé GV, da Silva AM et al (2015) Endothelial dysfunction as a predictor of cardiovascular disease in type 1 diabetes. World J Diabetes 6:679–692. https://doi.org/10.4239/wjd.v6.i5.679
Bhattacharya I, Mundy AL, Widmer CC et al (2008) Regional heterogeneity of functional changes in conduit arteries after high-fat diet. Obesity (silver Spring) 16:743–748. https://doi.org/10.1038/oby.2007.111
Blond K, Brinkløv CF, Ried-Larsen M et al (2020) Association of high amounts of physical activity with mortality risk: a systematic review and meta-analysis. Br J Sports Med 54:1195–1201. https://doi.org/10.1136/bjsports-2018-100393
Brunner H, Cockcroft JR, Deanfield J et al (2005) Endothelial function and dysfunction. Part II: Association with cardiovascular risk factors and diseases. A statement by the Working Group on Endothelins and Endothelial Factors of the European Society of Hypertension. J Hypertens 23:233–246. https://doi.org/10.1097/00004872-200502000-00001
Chang S-P, Chen Y-H, Chang W-C et al (2004) Increase of anti-oxidation by exercise in the liver of obese Zucker rats. Clin Exp Pharmacol Physiol 31:506–511. https://doi.org/10.1111/j.1440-1681.2004.04035.x
Cheng X, Pang CCY (2004) Increased vasoconstriction to noradrenaline by 1400W, inhibitor of iNOS, in rats with streptozotocin-induced diabetes. Eur J Pharmacol 484:263–268. https://doi.org/10.1016/j.ejphar.2003.11.002
Cheong A, Dedman AM, Xu SZ, Beech DJ (2001) K V α1 channels in murine arterioles: differential cellular expression and regulation of diameter. American Journal of Physiology-Heart and Circulatory Physiology 281:H1057–H1065. https://doi.org/10.1152/AJPHEART.2001.281.3.H1057
Connolly MG, Bruce SR, Kohman RA (2022) Exercise duration differentially effects age-related neuroinflammation and hippocampal neurogenesis. Neuroscience 490:275–286. https://doi.org/10.1016/j.neuroscience.2022.03.022
Cracowski JL, Durand T, Bessard G (2002) Isoprostanes as a biomarker of lipid peroxidation in humans: physiology, pharmacology and clinical implications. Trends Pharmacol Sci 23:360–366. https://doi.org/10.1016/S0165-6147(02)02053-9
D’Angelis CA, Nickerson PA, Steinhorn RH, Morin FC (1998) Heterogeneous distribution of soluble guanylate cyclase in the pulmonary vasculature of the fetal lamb. Anat Rec 250:62–69. https://doi.org/10.1002/(SICI)1097-0185(199801)250:1%3c62::AID-AR6%3e3.0.CO;2-G
da Orssatto LBR, Wiest MJ, Diefenthaeler F (2018) Neural and musculotendinous mechanisms underpinning age-related force reductions. Mech Ageing Dev 175:17–23. https://doi.org/10.1016/j.mad.2018.06.005
Dalbøge LS, Almholt DL, Neerup TS, Vassiliadis E, Vrang N, Pedersen L, Fosgerau K, Jelsing J (2013) Characterisation of age-dependent beta cell dynamics in the male db/db mice. PLoS One 8(12):e82813. https://doi.org/10.1371/journal.pone.0082813
de Oliveira HT, Couto GK, Davel AP, Xavier FE, Rossoni LV (2021) Chronic cyclooxygenase-2 inhibition prevents the worsening of hypertension and endothelial dysfunction induced by ouabain in resistance arteries of spontaneously hypertensive rats. Vascul Pharmacol 139:106880. https://doi.org/10.1016/j.vph.2021.106880
De Vriese AS, Verbeuren TJ, Van de Voorde J et al (2000) Endothelial dysfunction in diabetes. Br J Pharmacol 130:963–974. https://doi.org/10.1038/sj.bjp.0703393
Delorey DS (2021) Sympathetic vasoconstriction in skeletal muscle: modulatory effects of aging, exercise training, and sex. Appl Physiol Nutr Metab 46:1437–1447. https://doi.org/10.1139/apnm-2021-0399
Dillard CJ, Litov RE, Savin WM et al (1978) Effects of exercise, vitamin E, and ozone on pulmonary function and lipid peroxidation. J Appl Physiol Respir Environ Exerc Physiol 45:927–932. https://doi.org/10.1152/jappl.1978.45.6.927
Dourado TMH, Assis VO, Awata WMC et al (2023) Mineralocorticoid receptors contribute to ethanol-induced vascular hypercontractility through reactive oxygen species generation and up-regulation of cyclooxygenase 2. Eur J Pharmacol 949:175723. https://doi.org/10.1016/j.ejphar.2023.175723
Félétou M, Vanhoutte PM (2006) Endothelial dysfunction: a multifaceted disorder (The Wiggers Award Lecture). Am J Physiol Heart Circ Physiol 291:H985-1002. https://doi.org/10.1152/ajpheart.00292.2006
Forman HJ, Torres M, Fukuto J (2002) Redox signaling. Mol Cell Biochem 234–235:49–62. https://doi.org/10.1023/A:1015913229650
Frid MG, Dempsey EC, Durmowicz AG, Stenmark KR (1997) Smooth muscle cell heterogeneity in pulmonary and systemic vessels. Importance in vascular disease. Arterioscler Thromb Vasc Biol 17:1203–1209. https://doi.org/10.1161/01.atv.17.7.1203
Gæde P, Pedersen O (2004) Intensive integrated therapy of type 2 diabetes. Diabetes 53:S39–S47. https://doi.org/10.2337/DIABETES.53.SUPPL_3.S39
Gaesser GA, Angadi SS, Sawyer BJ (2011) Exercise and diet, independent of weight loss, improve cardiometabolic risk profile in overweight and obese individuals. Phys Sportsmed 39:87–97. https://doi.org/10.3810/psm.2011.05.1898
Green DJ, Walsh JH, Maiorana A et al (2003) Exercise-induced improvement in endothelial dysfunction is not mediated by changes in CV risk factors: pooled analysis of diverse patient populations. Am J Physiol Heart Circ Physiol 285:H2679–H2687. https://doi.org/10.1152/ajpheart.00519.2003
Grotle AK, Macefield VG, Farquhar WB, O'Leary DS, Stone AJ (2020) Recent advances in exercise pressor reflex function in health and disease. Auton Neurosci 228:102698. https://doi.org/10.1016/j.autneu.2020.102698
Gutterman DD, Miura H, Liu Y (2005) Redox modulation of vascular tone: focus of potassium channel mechanisms of dilation. Arterioscler Thromb Vasc Biol 25:671–678. https://doi.org/10.1161/01.ATV.0000158497.09626.3B
Hanefeld M, Fischer S, Julius U et al (1996) Risk factors for myocardial infarction and death in newly detected NIDDM: the diabetes intervention study, 11-year follow-up. Diabetologia 39:1577–1583. https://doi.org/10.1007/S001250050617
Heart Protection Study Collaborative Group (2002) MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20 536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360(9326):23–33. https://doi.org/10.1016/S0140-6736(02)09328-5
Hejazi K, Mohammad Rahimi GR, Rosenkranz SK (2023) Effects of exercise training on inflammatory and cardiometabolic risk biomarkers in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled Trials. Biol Res Nurs 25:250–266. https://doi.org/10.1177/10998004221132841
Huang J, Zhang H, Tan X et al (2019) Exercise restores impaired endothelium-derived hyperpolarizing factor-mediated vasodilation in aged rat aortic arteries via the TRPV4-KCa2.3 signaling complex. Clin Interv Aging 14:1579–1587. https://doi.org/10.2147/CIA.S220283
Ji LL, Gomez-Cabrera M-C, Vina J (2006) Exercise and hormesis: activation of cellular antioxidant signaling pathway. Ann N Y Acad Sci 1067:425–435. https://doi.org/10.1196/annals.1354.061
Joshi D, Shiwalkar A, Cross MR et al (2010) Continuous, non-invasive measurement of the haemodynamic response to submaximal exercise in patients with diabetes mellitus: Evidence of impaired cardiac reserve and peripheral vascular response. Heart 96:36–41. https://doi.org/10.1136/hrt.2009.177113
Just TP, Cooper IR, DeLorey DS (2016) Sympathetic vasoconstriction in skeletal muscle: adaptations to exercise training. Exerc Sport Sci Rev 44:137–143. https://doi.org/10.1249/JES.0000000000000085
Just TP, DeLorey DS (2016) Exercise training and α1-adrenoreceptor-mediated sympathetic vasoconstriction in resting and contracting skeletal muscle. Physiol Rep 4(3):e12707. https://doi.org/10.14814/phy2.12707
Kanie N, Kamata K (2000) Contractile responses in spontaneously diabetic mice: I. Involvement of superoxide anion in enhanced contractile response of aorta to norepinephrine in C57BL/KsJ(db/db) mice. General Pharmacology: Vascular System 35:311–318. https://doi.org/10.1016/S0306-3623(02)00115-5
Kataja-Tuomola MK, Kontto JP, Männistö S et al (2010) Effect of alpha-tocopherol and beta-carotene supplementation on macrovascular complications and total mortality from diabetes: Results of the ATBC Study. Ann Med 42:178–186. https://doi.org/10.3109/07853890903508887
Kemi OJ, Haram PM, Høydal MA et al (2013) Exercise training and losartan improve endothelial function in heart failure rats by different mechanisms. Scandinavian Cardiovascular Journal 47:160–167. https://doi.org/10.3109/14017431.2012.754935
Kourie JI (1998) Interaction of reactive oxygen species with ion transport mechanisms. Am J Physiol 275(1):C1-24. https://doi.org/10.1152/ajpcell.1998.275.1.C1
Lee S, Park Y, Dellsperger KC, Zhang C (2011) Exercise training improves endothelial function via adiponectin-dependent and independent pathways in type 2 diabetic mice. Am J Physiol Heart Circ Physiol 301:H306–H314. https://doi.org/10.1152/ajpheart.01306.2010
Lee JH, Xia S, Ragolia L (2008) Upregulation of AT2 receptor and iNOS impairs angiotensin II-induced contraction without endothelium influence in young normotensive diabetic rats. Am J Physiol Regul Integr Comp Physiol 295(1):R144–54. https://doi.org/10.1152/ajpregu.00191.2008
Leloup AJA, Van Hove CE, Heykers A et al (2015) Elastic and muscular arteries differ in structure, basal NO production and voltage-gated Ca(2+)-channels. Front Physiol 6:375. https://doi.org/10.3389/fphys.2015.00375
Lerman A, Zeiher AM (2005) Endothelial function: cardiac events. Circulation 111:363–368. https://doi.org/10.1161/01.CIR.0000153339.27064.14
Liskova S, Cacanyiova S, Cebova M, Berenyiova A, Kluknavsky M, Micurova A, Valachova K, Soltes L, Bernatova I (2023) Taxifolin reduces blood pressure via improvement of vascular function and mitigating the vascular inflammatory response in spontaneously hypertensive rats. Int J Mol Sci 24(16):12616. https://doi.org/10.3390/ijms241612616
Liu W, Kuang H, Xia Y et al (2019) Regular aerobic exercise-ameliorated troponin I carbonylation to mitigate aged rat soleus muscle functional recession. Exp Physiol 104:715–728. https://doi.org/10.1113/EP087564
Liu H, Liu S, Wang K, Zhang T, Yin L, Liang J, Yang Y, Luo J (2022a) Time-dependent effects of physical activity on cardiovascular risk factors in adults: a systematic review. Int J Environ Res Public Health 19(21):14194. https://doi.org/10.3390/ijerph192114194
Liu X, Wu Z, Li N (2022b) Association between physical exercise and all-cause and CVD mortality in patients with diabetes: an updated systematic review and meta-analysis. Afr Health Sci 22:250–266. https://doi.org/10.4314/ahs.v22i3.27
Lounsbury KM, Hu Q, Ziegelstein RC (2000) Calcium signaling and oxidant stress in the vasculature. Free Radic Biol Med 28:1362–1369. https://doi.org/10.1016/S0891-5849(00)00222-7
Ma L, Zhu B, Chen X et al (2008) Abnormalities of sarcoplasmic reticulum CA2+ mobilization in aortic smooth muscle cells from streptozotocin-induced diabetic rats. Clin Exp Pharmacol Physiol 35:568–573. https://doi.org/10.1111/j.1440-1681.2007.04832.x
Marrachelli VG, Miranda FJ, Alabadí JA et al (2006) Contribution of endothelin receptors and cyclooxygenase-derivatives to the altered response of the rabbit renal artery to endothelin-1 in diabetes. Eur J Pharmacol 534:178–186. https://doi.org/10.1016/j.ejphar.2006.01.043
Massett MP, Berk BC (2005) Strain-dependent differences in responses to exercise training in inbred and hybrid mice. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology 288:R1006–R1013. https://doi.org/10.1152/AJPREGU.00476.2004
Matsuda M, DeFronzo RA (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22:1462–1470. https://doi.org/10.2337/DIACARE.22.9.1462
Matsumoto T, Noguchi E, Ishida K et al (2008) Metformin normalizes endothelial function by suppressing vasoconstrictor prostanoids in mesenteric arteries from OLETF rats, a model of type 2 diabetes. American Journal of Physiology-Heart and Circulatory Physiology 295:H1165–H1176. https://doi.org/10.1152/AJPHEART.00486.2008
McAllister RM, Laughlin MH (1997) Short-term exercise training alters responses of porcine femoral and brachial arteries. J Appl Physiol 82:1438–1444. https://doi.org/10.1152/jappl.1997.82.5.1438
Mestek ML, Westby CM, Van Guilder GP et al (2010) Regular aerobic exercise, without weight loss, improves endothelium-dependent vasodilation in overweight and obese adults. Obesity 18:1667–1669. https://doi.org/10.1038/oby.2009.467
Michelakis ED, Reeve HL, Huang JM et al (1997) Potassium channel diversity in vascular smooth muscle cells. Can J Physiol Pharmacol 75:889–897
Moien-Afshari F, Ghosh S, Elmi S et al (2008) Exercise restores coronary vascular function independent of myogenic tone or hyperglycemic status in db/db mice. American Journal of Physiology-Heart and Circulatory Physiology 295:H1470–H1480. https://doi.org/10.1152/AJPHEART.00016.2008
Nobe K, Sakai Y, Maruyama Y, Momose K (2002) Hyper-reactivity of diacylglycerol kinase is involved in the dysfunction of aortic smooth muscle contractility in streptozotocin-induced diabetic rats. Br J Pharmacol 136:441–451. https://doi.org/10.1038/sj.bjp.0704722
Nobe K, Hashimoto T, Honda K (2012) Two distinct dysfunctions in diabetic mouse mesenteric artery contraction are caused by changes in the Rho A-Rho kinase signaling pathway. Eur J Pharmacol 683:217–225. https://doi.org/10.1016/j.ejphar.2012.03.022
Nuno DW, Harrod JS, Lamping KG (2009) Sex-dependent differences in rho activation contribute to contractile dysfunction in type 2 diabetic mice. Am J Physiol Heart Circ Physiol 297(4):H1469–77. https://doi.org/10.1152/ajpheart.00407.2009
Powers SK, Radak Z, Ji LL (2016) Exercise-induced oxidative stress: past, present and future. J Physiol 594:5081–5092. https://doi.org/10.1113/JP270646
Rietz M, Lehr A, Mino E et al (2022) Physical activity and risk of major diabetes-related complications in individuals with diabetes: a systematic review and meta-analysis of observational studies. Diabetes Care 45:3101–3111. https://doi.org/10.2337/dc22-0886
Sakamoto S, Minami K, Niwa Y et al (1998) Effect of exercise training and food restriction on endothelium-dependent relaxation in the Otsuka Long-Evans Tokushima fatty rat, a model of spontaneous NIDDM. Diabetes 47:82–86. https://doi.org/10.2337/diab.47.1.82
Sallam NA, Laher I (2020) Redox signaling and regional heterogeneity of endothelial dysfunction in db/db mice. Int J Mol Sci 21:1–20. https://doi.org/10.3390/ijms21176147
Sallam N, Fisher A, Golbidi S, Laher I (2011) Weight and inflammation are the major determinants of vascular dysfunction in the aortae of db/db mice. Naunyn Schmiedebergs Arch Pharmacol 383:483–492. https://doi.org/10.1007/s00210-011-0614-1
Sato A, Nagasawa Y, Suzuki H et al (2023) Differential effects of Ca2+ channel blockers nifedipine and cilnidipine on arterial elasticity in the aortic and femoral arterial segments of anesthetized rabbits. Biol Pharm Bull 46:1324–1331. https://doi.org/10.1248/bpb.b23-00391
Setty S, Sun W, Martinez R et al (2004) α-Adrenoceptor-mediated coronary vasoconstriction is augmented during exercise in experimental diabetes mellitus. J Appl Physiol 97:431–438. https://doi.org/10.1152/JAPPLPHYSIOL.01122.2003
Shi Y, Vanhoutte PM (2008) Oxidative stress and COX cause hyper-responsiveness in vascular smooth muscle of the femoral artery from diabetic rats. Br J Pharmacol 154:639–651. https://doi.org/10.1038/bjp.2008.110
Shi Y, So KF, Man RYK, Vanhoutte PM (2007) Oxygen-derived free radicals mediate endothelium-dependent contractions in femoral arteries of rats with streptozotocin-induced diabetes. Br J Pharmacol 152:1033–1041. https://doi.org/10.1038/sj.bjp.0707439
Sugawara J, Komine H, Hayashi K, Yoshizawa M, Otsuki T, Shimojo N, Miyauchi T, Yokoi T, Maeda S, Tanaka H (2007) Systemic α-adrenergic and nitric oxide inhibition on basal limb blood flow: effects of endurance training in middle-aged and older adults. Am J Physiol Heart Circ Physiol 293(3):H1466–72. https://doi.org/10.1152/ajpheart.00273.2007
Trinity JD, Kwon OS, Broxterman RM et al (2021) The role of the endothelium in the hyperemic response to passive leg movement: looking beyond nitric oxide. Am J Physiol Heart Circ Physiol 320:H668–H678. https://doi.org/10.1152/AJPHEART.00784.2020
Tschakert G, Handl T, Weiner L, Birnbaumer P, Mueller A, Groeschl W, Hofmann P (2022) Exercise duration: independent effects on acute physiologic responses and the need for an individualized prescription. Physiol Rep 10(3):e15168. https://doi.org/10.14814/phy2.15168
Tschudi MR, Barton M, Bersinger NA et al (1996) Effect of age on kinetics of nitric oxide release in rat aorta and pulmonary artery. J Clin Invest 98:899–905. https://doi.org/10.1172/JCI118872
Watts GF, O’Brien SF, Silvester W, Millar JA (1996) Impaired endothelium-dependent and independent dilatation of forearm resistance arteries in men with diet-treated non-insulin-dependent diabetes: role of dyslipidaemia. Clin Sci (lond) 91:567–573. https://doi.org/10.1042/cs0910567
Woodman CR, Seawright JW, Luttrell MJ et al (2018) Importance of mechanical signals in promoting exercise-induced improvements in vasomotor function of aged skeletal muscle resistance arteries. Am J Physiol Heart Circ Physiol 315:H602–H609. https://doi.org/10.1152/ajpheart.00732.2017
Xie Z, Su W, Guo Z et al (2006) Up-regulation of CPI-17 phosphorylation in diabetic vasculature and high glucose cultured vascular smooth muscle cells. Cardiovasc Res 69:491–501. https://doi.org/10.1016/j.cardiores.2005.11.002
Yang H, Chen XY, Kuang SJ et al (2020) Abnormal Ca2+ handling contributes to the impairment of aortic smooth muscle contractility in Zucker diabetic fatty rats. J Mol Cell Cardiol 141:82–92. https://doi.org/10.1016/j.yjmcc.2020.03.009
Zelinskaya I, Kornushin O, Savochkina E, Dyachuk V, Vasyutina M, Galagudza M, Toropova Y (2021) Vascular region-specific changes in arterial tone in rats with type 2 diabetes mellitus: opposite responses of mesenteric and femoral arteries to (2002) acetylcholine and 5-hydroxytryptamine. Life Sci 286:120011. https://doi.org/10.1016/j.lfs.2021.120011
Zheng Y-M, Wang Q-S, Liu Q-H et al (2008) Heterogeneous gene expression and functional activity of ryanodine receptors in resistance and conduit pulmonary as well as mesenteric artery smooth muscle cells. J Vasc Res 45:469–479. https://doi.org/10.1159/000127438
Funding
Nada Sallam received a scholarship from the Ministry of Higher Education, Egypt.
Author information
Authors and Affiliations
Contributions
Nada Sallam: Conceptualization; Investigation; Methodology; Data curation; Formal analysis; Writing & editing- original draft. Baohua Wang: Methodology. Ismail Laher: Supervision; Funding acquisition; Editing. The authors declare that all data were generated in-house and that no paper mill was used.
Corresponding author
Ethics declarations
Ethical approval
This study was carried out following the principles of the Declaration of Helsinki. The experimental animal protocols were approved by University of British Columbia Animal Care Committee (A06-0308).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sallam, N.A., Wang, B. & Laher, I. Exercise training and vascular heterogeneity in db/db mice: evidence for regional- and duration-dependent effects. Naunyn-Schmiedeberg's Arch Pharmacol 397, 2421–2436 (2024). https://doi.org/10.1007/s00210-023-02775-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-023-02775-0