Abstract
We determined the pharmacologic profile of ASP7657, trans-4-[({[1-(quinolin-2-ylmethyl)-5-(trifluoromethyl)-1H-indol-7 yl] carbonyl} amino) methyl] cyclohexanecarboxylic acid methanesulfonate (1:1), a newly synthesized selective E-type prostaglandin (EP)4 receptor antagonist using several in vitro and in vivo experiments. ASP7657 exhibited high affinity for rat and human EP4 receptors, with Ki values of 6.02 nM and 2.21 nM, respectively. In addition, ASP7657 potently inhibited the PGE2-induced cyclic adenosine monophosphate (cAMP) increase in Chinese hamster ovary (CHO) cells expressing rat EP4 receptors and human lymphoblastoid T (Jurkat) cells, with IC50 values of 0.86 nM and 0.29 nM, respectively. In contrast, ASP7657 did not inhibit the PGE2-induced intracellular calcium increase in HEK293 cells expressing rat EP1 and EP3 receptors, or cAMP increase in CHO cells expressing rat EP2 receptors. ASP7657 showed good pharmacokinetic properties following oral dosing and dose-dependently antagonized the prostaglandin (PG)E2-mediated inhibition of lipopolysaccharide-induced tumor necrosis factor-α release from rat whole blood culture. In addition, 4 weeks repeated oral administration of ASP7657 dose-dependently attenuated albuminuria in type 2 diabetic mice; these effects were significant at doses of 0.01 mg/kg or higher. These results demonstrate that ASP7657 is a potent and selective EP4 receptor antagonist that may be useful in future studies to help clarify the physiological and pathophysiological roles of PG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of diabetes is rapidly rising, with current projections estimating that the number of diabetic individuals will rise to 439 million globally by 2030 (Shaw et al. 2010). A major concern of diabetes is its propensity to be associated with macrovascular complications, such as stroke and cardiovascular disease, and microvascular complications, such as nephropathy, retinopathy, and neuropathy. Diabetic nephropathy is one of the most common complications of diabetes and the leading cause of end-stage renal disease. It is also associated with high cardiovascular risk and significant morbidity and mortality worldwide (Gilbertson et al. 2005). It is estimated that one third of diabetic patients have diabetic nephropathy (Akmal 2001). Known risk factors for diabetic nephropathy include hyperglycemia, hypertension, dyslipidemia, and obesity (Hall 2006). Therefore, current standard therapies to prevent and slow the progression of diabetic nephropathy are based on the control of blood glucose and blood pressure. While current antidiabetic therapies to control blood glucose, and administration of renin-angiotensin-aldosterone system inhibitors, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin II receptor blockers (ARBs) to control blood pressure can slow the progression of diabetic nephropathy, they do not sufficiently prevent it (Fioretto et al. 2010). There is therefore a strong need to explore alternative therapies to prevent the progression of diabetic nephropathy.
Prostaglandins (PGs) are important lipid mediators of numerous physiological and pathophysiological processes in the kidney. PGE2, which is the most abundant renal PG, plays a major role in renal physiological processes including inflammation, volume homeostasis, regulation of salt and water balance, renal blood flow, glomerular hemodynamics, and renin release (Breyer et al. 1996). PGE2 signals through four well-characterized G protein-coupled receptors known as E-type prostaglandin (EP) receptors: EP1, EP2, EP3, and EP4. EP1 and EP3 are generally regarded as being vasoconstrictive while EP2 and EP4 are usually associated with vasorelaxation (Narumiya et al. 1999). Several genetic knockout and overexpression studies have revealed that these EP receptor subtypes have different physiological and pathophysiological effects in the kidney. The results of many investigations strongly suggest that EP4 receptors, which are most widely expressed in the kidney, play key roles in the pathophysiology of a variety of renal disorders. EP4 receptor mRNA is localized mainly to the glomeruli in normal kidneys and is highly induced in tubular epithelial cells, interstitial cells, and podocytes under diabetic conditions (Stitt-Cavanagh et al. 2010). Overexpression of EP4 receptors in podocytes reportedly exacerbates glomerular injury and albuminuria in chronic kidney disease rats (Stitt-Cavanagh et al. 2010). In addition, chronic administration of an EP4 receptor-selective agonist exacerbates albuminuria and renal fibrosis in diabetic mice (Mohamed et al. 2013). These findings suggest that PGE2 may play a crucial role in the development and progression of various kidney diseases including diabetic nephropathy via EP4 receptors. We therefore hypothesized that a selective EP4 receptor antagonist may be beneficial for preventing diabetic nephropathy.
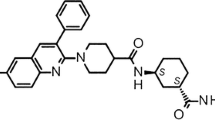
In this study, we characterized the pharmacological properties of ASP7657 (trans-4-[({[1-(quinolin-2-ylmethyl)-5-(trifluoromethyl)-1H-indol-7 yl] carbonyl} amino) methyl] cyclohexanecarboxylic acid methanesulfonate (1:1); Fig. 1), a newly synthesized EP4 receptor antagonist, and investigated the efficacy of ASP7657 in diabetic nephropathy.
Materials and methods
Materials
ASP7657, trans-4-[({[1-(quinolin-2-ylmethyl)-5-(trifluoromethyl)-1H-indol-7 yl] carbonyl} amino) methyl] cyclohexanecarboxylic acid methanesulfonate (1:1), was synthesized at Astellas Pharma Inc. (Ibaraki, Japan). For in vitro studies, ASP7657 was initially dissolved in dimethyl sulfoxide (DMSO) and diluted to the desired concentration with assay buffer. The final concentration of DMSO in assay buffer did not exceed 1%. For in vivo studies, ASP7657 was dissolved in 0.1 M sodium hydrogen carbonate solution for oral and intravenous administration in the pharmacokinetic study and suspended in 0.5% methylcellulose solution for oral administration in other experiments. [3H]PGE2 was purchased from PerkinElmer Inc. (Waltham, MA, USA), and membrane fractions expressing the recombinant human EP4 receptor were purchased from Chemicon International Inc. (Billerica, MA, USA). Lipopolysaccharide (LPS) and PGE2 were purchased from Sigma-Aldrich (St. Louis, MO, USA) and Funakoshi (Tokyo, Japan), respectively.
Animals
Male Sprague-Dawley (SD) rats were purchased from Charles River Laboratories Japan (Kanagawa, Japan) or Japan SLC Inc. (Shizuoka, Japan) at age 7–8 weeks. db/db type 2 diabetic and db/m+ normal control mice were purchased from CLEA Japan Inc. (Tokyo, Japan) at age 7 weeks. The diabetic mice were grouped such that each group had similar blood glucose levels. All animals were housed under conventional conditions with controlled temperature, humidity, and light (12-h light-dark cycle) and were provided a standard commercial diet and water ad libitum. Animal studies were approved by the Institutional Animal Care and Use Committee of Astellas Pharma Inc., Tsukuba Research Center, which is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) International.
Binding assay
Radioligand binding studies for human EP4 receptors
This study was performed according to the standard assay procedures specified by Sekisui Medical Co., Ltd. [3H]PGE2 (3 nM) was added to membrane preparations of human EP4 receptors, which were subsequently incubated with various concentrations of ASP7657 in assay buffer (50 mM HEPES-NaOH, 5 mM MgCl2, 1 mM CaCl2, and 0.5% bovine serum albumin [BSA]). Binding reactions were initiated by adding the membrane preparations. After the incubation period (room temperature for 1 h), the reaction was terminated by adding wash buffer (50 mM HEPES-NaOH (pH 7.4) containing 500 mM NaCl and 0.1% BSA) followed immediately by rapid filtration through 96-well GF/B UniFilter Plates using a Cell Harvester (PerkinElmer Inc., MA, USA). The filters were rinsed and the radioactivity retained on the filters was counted using a TopCount Microplate Scintillation Counter (PerkinElmer Inc., MA, USA). Nonspecific binding was determined using 10 μM PGE2. The concentration of drug that caused 50% inhibition (IC50) of the specific binding of [3H]PGE2 was determined using regression analysis of displacement curves. The inhibition constant (Ki) was calculated using the following formula: Ki = IC50/(1 + [L]/Kd), where [L] is the concentration of the radioligand and Kd is the dissociation constant of radioligand obtained from the Scatchard plot.
Radioligand binding studies for rat EP4 receptors
[3H]PGE2 (0.3 nM) was added to membrane preparations of human embryonic kidney (HEK) 293 cells transiently expressing rat EP4 receptors, which were subsequently incubated with various concentrations of ASP7657 in assay buffer (50 mM HEPES, 10 mM MgCl2, 0.5% BSA). Nonspecific binding was determined using 1 μM PGE2. Measurement of other parameters was conducted as described above.
Measurement of intracellular Ca2+ concentration ([Ca2+]i)
HEK293 cells expressing rat EP1 or EP3 receptors were cultured in Dulbecco’s Modified Eagle’s medium (DMEM) with 10% fetal bovine serum (FBS), 50 units/mL penicillin, 50 μg/mL streptomycin, and 0.2 mg/mL G418 at 37 °C in a humidified atmosphere of 5% CO2. These cells were seeded at 10,000 cells per well into black-walled, clear-base 96-well poly-d-lysine coated plates, and cultured overnight. On the day of the measurement, the cells were incubated for 3 h at room temperature in Hank’s Balanced Salt Solution (HBSS) buffer containing 20 mM HEPES (pH 7.5), 0.5% BSA, and 2.5 mM probenecid (HBSS buffer) with Calcium 3 reagent (Molecular Devices Corporation Japan, Tokyo, Japan) in the dark. The plates were then placed into a fluorometric imaging plate reader (FLIPR) TETRA (Molecular Devices Corporation Japan). The cells were incubated with the compound for 5 min and then with 100 nM PGE2 for 3 min. The total change in intracellular fluorescence, an index of Ca2+ concentration, was monitored for these 8 min. The maximum fluorescence signal after adding PGE2 was subtracted from the fluorescence signal before adding PGE2 for each well. The IC50 value was estimated using Sigmoid-Emax nonlinear regression analysis.
Measurement of cyclic adenosine monophosphate levels
Chinese hamster ovary (CHO) cells expressing rat EP2 or EP4 receptors were cultured in α-minimum essential medium (MEM) with 10% FBS, 50 units/mL penicillin, 50 μg/mL streptomycin, and 0.5 mg/mL G418 at 37 °C in a humidified atmosphere of 5% CO2. These cells were seeded at 50,000 cells per well into 96-well plates and cultured overnight. On the day of the measurement, the medium was replaced first with α-MEM containing 2 μM indomethacin and 0.5% BSA and then α-MEM-IBMX buffer (α-MEM containing 2 μM indomethacin, 1 mM 3-isobutyl-1-methylxanthine [IBMX], and 0.5% BSA). The cells were incubated with 100 nM PGE2 in the presence or absence of the compound in α-MEM-IBMX buffer at 37 °C for 30 min. The medium was removed, and the cells were lysed with 0.2% TritonX-100/phosphate-buffered saline (PBS). Cyclic adenosine monophosphate (cAMP) levels in the lysate were measured using a homogeneous time resolved fluorescence-based assay kit (Cisbio Bioassays, Bagnols, France). The IC50 value was estimated using Sigmoid-Emax nonlinear regression analysis.
Effect on PGE2-induced cAMP production in Jurkat cells
Human Jurkat T cells (clone E6-1; Dainippon Sumitomo Pharma, Osaka, Japan) were cultured in Roswell Park Memorial Institute (RPMI)-1640 with 10% FBS, 50 units/mL penicillin, and 50 μg/mL streptomycin at 37 °C in a humidified atmosphere of 5% CO2. Cells were incubated in HBSS buffer containing 20 mM HEPES, pH 7.5, 0.5 mM IBMX, 0.02% CHAPS, 2 μM indomethacin, and 0.5% BSA with ASP7657 and PGE2 (100 nM) in a 384-well plate (5000 cells/well) for 30 min. Intracellular cAMP concentrations were measured as described above. The IC50 value was estimated using Sigmoid-Emax nonlinear regression analysis.
Specificity assay
Pharmacological screening assays for various receptors, ion channels, and transporters were performed using 1 μM ASP7657 according to standard assay procedures specified by Sekisui Medical Co., Ltd.
Pharmacokinetics
ASP7657 (0.1 mg/kg) was administered intravenously and orally to conscious SD rats. Under isoflurane anesthesia, blood samples were drawn from the abdominal aorta at 0.1 (intravenous dosing only), 0.25, 0.5, 1, 2, 4, 6, 8, and 10 h after dosing. The drug plasma concentration was measured using liquid chromatography-tandem mass spectrometry (LC-MS/MS) with liquid-liquid extraction. Pharmacokinetic parameters were calculated from mean plasma ASP7657 concentrations using the noncompartmental analysis model of Phoenix WinNonlin version 6.1 software (Pharsight Co., St. Louis, MO, USA).
Effect of single administration of ASP7657 on the PGE2-mediated inhibition of LPS-induced tumor necrosis factor (TNF)-α release from rat whole blood culture
ASP7657 (0.003–0.1 mg/kg) was orally administered to rats, and blood was drawn under isoflurane anesthesia 1 h after dosing. Blood samples were diluted twofold in RPMI1640 medium into 48-well plates and incubated at 37 °C for 10 min in a CO2 incubator. LPS (1 μg/mL) and PGE2 (100 nM) were added and the samples were incubated for 4 h. The assay mixture was centrifuged (3000 rpm, 10 min) and the supernatant was collected for use as the assay sample. Concentrations of TNF-α in the assay sample were measured using an enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems, Inc., Minneapolis, MN, USA).
Effect of repeated administration of ASP7657 on albuminuria in type 2 diabetic mice
ASP7657 (0.001–0.1 mg/kg) was administered to diabetic mice once daily for 4 weeks. At weeks 2 and 4, mice were transferred to metabolic cages and spontaneously voided urine was collected for 24 h. Blood samples were collected at week 4. Blood glucose levels were measured using the Glucose CII test reagent (Wako Pure Chemical Industries, Osaka, Japan). Creatinine concentrations of plasma and urine were measured using an automatic analyzer (Hitachi 7180, Hitachi High-Technologies Corporation, Tokyo, Japan). Urinary albumin concentrations were measured using an ELISA kit (Shibayagi, Gunma, Japan).
Statistical analysis
Data analyses for calculating IC50 and Ki values were conducted using the SAS 9.1.3 software package (SAS Institute Japan, Ltd., Tokyo, Japan), except those for the human EP4 receptor binding study, which were conducted using EXSUS 7.7 (CAC Croit Corporation, Tokyo, Japan). Experimental results are expressed as mean ± standard error of the mean (SEM), standard deviation (SD), or with 95% confidence limits. Student’s t test was used to analyze the difference between two groups; Dunnett’s multiple comparisons test was used for comparisons among multiple groups. A value of p < 0.05 was considered significant. Statistical and data analyses were conducted using SAS 9.1.3 software package (SAS Institute Japan, Ltd., Tokyo, Japan) or GraphPad Prism 7 (GraphPad Software, La Jolla, CA, USA).
Results
In vitro pharmacological characterization of ASP7657
ASP7657 potently inhibited the specific binding of [3H]PGE2 to rat and human EP4 receptors, with Ki values of 6.02 nM and 2.21 nM, respectively (Table 1). ASP7657 potently inhibited the PGE2-induced cAMP increase in rat EP4 receptor-expressing CHO cells and human EP4 receptor-expressing Jurkat cells, with IC50 values of 0.86 (0.24–3.08) nM and 0.29 (0.03–2.46) nM, respectively (Table 2). In contrast, ASP7657 did not inhibit the PGE2-induced cAMP increase in rat EP2 receptor-expressing CHO cells or the [Ca2+]i increase in rat EP1 and EP3 receptor-expressing HEK293 cells (IC50 > 1000 nM). ASP7657 (1 μM) did not interact with other examined receptors including human PG CRTH2, DP, EP2, and EP3 receptor subtypes (Table 3). In addition, ASP7657 did not inhibit various ion channels, transporters, and enzymes (data not shown).
Pharmacokinetics
After oral administration of ASP7657 (0.1 mg/kg) to rats, the plasma concentration of the unchanged drug rapidly reached maximum at 0.25 h and decreased with a t1/2 value of 1.38 h (Fig. 2). The corresponding Cmax was 22.4 ng/mL and AUC0–10 h was 22.3 ng·h/mL. Bioavailability, calculated from the results of the oral administration study, was 46.2%.
Effect of single administration of ASP7657 on PGE2-mediated inhibition of LPS-induced TNF-α release from rat whole blood culture
Compared to the vehicle alone group, LPS (1 μg/mL) treatment significantly increased TNF-α release from rat whole blood culture, and PGE2 (100 nM) treatment significantly inhibited LPS-induced TNF-α release (Fig. 3). ASP7657 (0.003–0.1 mg/kg) dose-dependently antagonized the PGE2-mediated inhibition of LPS-induced TNF-α release from rat whole blood.
Effect of single administration of ASP7657 on prostaglandin (PG)E2-mediated inhibition of lipopolysaccharide (LPS)-induced tumor necrosis factor (TNF)-α release from whole blood culture. ASP7657 was orally administered to rats, and blood was withdrawn 1 h after dosing. LPS (1 μg/mL) and PGE2 (100 nM) were added to cultured whole blood and TNF-α release was measured. The values are the mean ± SD for eight animals in each group. *p < 0.05 vs. normal group, #p < 0.05 vs. LPS group
Effect of repeated administration of ASP7657 on albuminuria in type 2 diabetic mice
Compared to normal control mice, type 2 diabetic mice exhibited hyperglycemia, obesity, and glomerular hyperfiltration as assessed by increased creatinine clearance (Table 4). Repeated administration of ASP7657 (0.001–0.1 mg/kg) for 4 weeks did not affect these parameters. In contrast, ASP7657 dose-dependently attenuated urinary albumin excretion; these effects were significant at doses of 0.01 mg/kg or higher (Fig. 4). No deaths or serious adverse events were observed during the entire study period. In addition, ASP7657 did not affect general parameters including body weight, blood glucose level, and locomotor activity. Furthermore, serious toxicity due to ASP7657 has not been observed in safety studies using rats (data not shown).
Effect of repeated administration of ASP7657 on albuminuria in type 2 diabetic db/db mice. ASP7657 was orally administered to diabetic mice for 4 weeks. a Time course of changes in urinary albumin excretion and b scatter plot of urinary albumin excretion at week 4. The values are the mean ± (a) SEM or (b) SD for five animals in the normal group and eleven animals in all other groups. *p < 0.05 vs. normal group, #p < 0.05 vs. vehicle group
Discussion
The present study characterized the pharmacological profile of ASP7657, a newly discovered potent and selective EP4 receptor antagonist. In receptor binding studies, ASP7657 exhibited high affinity for rat and human EP4 receptors with IC50 values in the nanomolar range. In addition, ASP7657 potently inhibited the PGE2-induced cAMP increase in rat and human EP4 receptor-expressing cells. In contrast, ASP7657 did not inhibit PGE2-induced signal transduction in EP1, EP2, or EP3 receptor-expressing cells. Furthermore, ASP7657 did not interact with other examined receptors including human EP2 and EP3 receptor subtypes, ion channels, transporters, and enzymes. These results indicate that ASP7657 possesses potent affinity and selectivity for EP4 receptors.
ASP7657 showed good oral bioavailability in rats. PGE2 has been shown to suppress LPS-induced TNF-α release via EP4 receptors (Wall et al. 2009). To evaluate the antagonistic activity of ASP7657 in vivo, we examined the effects of ASP7657 on this physiological response. Oral administration of ASP7657 significantly and dose-dependently antagonized the PGE2-mediated inhibition of LPS-induced TNF-α release from rat whole blood culture. This suggests that ASP7657 potently antagonized the PGE2-induced physiological response via EP4 receptors in vivo, which agrees with our pharmacokinetic results for ASP7657.
We also investigated the effects of ASP7657 on nephropathy in type 2 diabetic db/db mice, which exhibit not only typical diabetic symptoms, such as hyperglycemia, insulin resistance, hyperlipidemia, inflammation, and obesity, but also incipient nephropathy with glomerular hyperfiltration and albuminuria (Park et al. 2006; Sharma et al. 2003). Four weeks repeated administration of ASP7657 significantly and dose-dependently attenuated albuminuria without affecting blood glucose levels. This suggests that ASP7657 suppresses the progression of diabetic nephropathy without direct effects on hyperglycemia. Despite our pharmacokinetic analysis showing that ASP7657 was rapidly eliminated from plasma with a half-life of about 1 h, once-daily administration of ASP7657 showed significant pharmacologic effects in type 2 diabetic mice. One explanation for these findings may be that ASP7657 possesses potent EP4 receptor inhibitory activity. Our findings indicate that ASP7567 possesses high affinity (Ki = 0.86 nM, equivalent to 3.1 ng/mL) for rat EP4 receptors and a potent inhibitory effect (IC50 = 0.86 nM, equivalent to 0.44 ng/mL) on the PGE2-induced increase in cAMP. After oral administration, plasma concentrations of ASP7657 were rapidly eliminated but remained at approximately 0.5 ng/mL until 8 h after dosing. Additionally, in pharmacokinetic studies using rats, oral administration resulted in approximately threefold higher concentrations of ASP7657 in the kidneys than in plasma (data not shown), suggesting that ASP7657 is highly concentrated in its target organ, the kidneys. These characteristics may underlie the significant pharmacologic effects of ASP7657 in a once-daily dosing regimen. In contrast, we did not investigate the pharmacologic effects of ASP7657 in a multiple-daily dosing regimen. Therefore, the once-daily dosing effects of ASP7657 shown in this study may not reflect the compound’s maximum efficacy. Future studies on the detailed pharmacologic effects of ASP7657 including in various dosing regimens are needed.
One of the principal mechanisms by which glomerular injury occurs in diabetes is through glomerular hyperfiltration (Pistrosch et al. 2005). Many studies have reported that the beneficial effects of ACE inhibitors and ARBs on diabetic nephropathy may be, at least in part, mediated by the attenuation of glomerular hyperfiltration (Parving et al. 2001). There is a large body of evidence indicating that PGE2 also affects glomerular hyperfiltration via EP4 receptors. PGE2 induces vasodilation of renal afferent arterioles via EP4 receptors (Purdy and Arendshorst 2000). In addition, PGE2 induces renin release in juxtaglomerular cells, which leads to an increase in angiotensin II production (Jensen et al. 1996), and in turn induces constriction of renal efferent arterioles. Based on these mechanisms, PGE2 may induce glomerular hyperfiltration via EP4 receptors. In this study, diabetic db/db mice exhibited glomerular hyperfiltration, as assessed by increased creatinine clearance and decreased plasma creatinine levels. However, ASP7657 did not affect these parameters. The EP4 receptor antagonist ONO-AE3-208 also attenuates diabetic nephropathy in db/db mice without affecting renal hemodynamics (Thieme et al. 2017). These results suggest that, unlike ACE inhibitors and ARBs, the beneficial effects of ASP7657 on diabetic nephropathy in this model may not occur through renal hemodynamic actions. EP4 receptor agonists have also been suggested to induce large increases in inflammatory cytokine production, which plays an important role in the pathogenesis of diabetic nephropathy (Mohamed et al. 2013).
Podocyte-selective deletion of EP4 receptors reportedly protects against renal injury in chronic kidney disease rats (Stitt-Cavanagh et al. 2010). In addition, chronic administration of an EP4 receptor agonist enhanced the expression of profibrotic cytokine transforming growth factor (TGF)-β1 (Mohamed et al. 2013), which is strongly correlated with glomerulosclerosis and interstitial fibrosis in diabetic kidney diseases. Moreover, an EP4 receptor antagonist prevented TGF-β1-induced podocyte differentiation (Thieme et al. 2017). Furthermore, mouse mesangial cells overexpressing EP4 receptors had increased TGF-β1-induced accumulation of extracellular matrix (ECM), type I collagen and fibronectin, and heterozygous EP4 receptor knockout mice showed an attenuation of nephrectomy-induced reduction in renal function and pathological changes including fibrosis. PGE2 may contribute to the accumulation of ECM in glomerular mesangial cells and renal fibrosis via EP4 receptors (Yang et al. 2014). EP4 receptor-selective antagonists may therefore attenuate diabetic nephropathy through these mechanisms. As such, additional and detailed examinations are needed to confirm and expand these potentially important therapeutic and novel biological findings associated with the PGE2-EP4 receptor pathway.
In summary, our in vitro and in vivo experiments indicate that ASP7657 is an orally active, high affinity, potent, and selective EP4 receptor antagonist. In addition, ASP7657 attenuated albuminuria in type 2 diabetic mice. EP4 receptor antagonists may represent a promising therapeutic option to slow the progression of nephropathy in the management of type 2 diabetes.
References
Akmal M (2001) Hemodialysis in diabetic patients. Am J Kidney Dis 38:S195–S199
Breyer MD, Jacobson HR, Breyer RM (1996) Functional and molecular aspects of renal prostaglandin receptors. J Am Soc Nephrol 7:8–17
Fioretto P, Dodson PM, Ziegler D, Rosenson RS (2010) Residual microvascular risk in diabetes: unmet needs and future directions. Nat Rev Endocrinol 6:19–25
Gilbertson DT, Liu J, Xue JL, Louis TA, Solid CA, Ebben JP, Collins AJ (2005) Projecting the number of patients with end-stage renal disease in the United States to the year 2015. J Am Soc Nephrol 16:3736–3741
Hall PM (2006) Prevention of progression in diabetic nephropathy. Diabetes Spectr 19:18–24
Jensen BL, Schmid C, Kurtz A (1996) Prostaglandins stimulate renin secretion and renin mRNA in mouse renal juxtaglomerular cells. Am J Phys 271:F659–F669
Mohamed R, Jayakumar C, Ramesh G (2013) Chronic administration of EP4-selective agonist exacerbates albuminuria and fibrosis of the kidney in streptozotocin-induced diabetic mice through IL-6. Lab Investig 93:933–945
Narumiya S, Sugimoto Y, Ushikubi F (1999) Prostanoid receptors: structures, properties, and functions. Physiol Rev 79:1193–1226
Park CW, Zhang Y, Zhang X, Wu J, Chen L, Cha DR, Su D, Hwang MT, Fan X, Davis L, Striker G, Zheng F, Breyer M, Guan Y (2006) PPARalpha agonist fenofibrate improves diabetic nephropathy in db/db mice. Kidney Int 69:1511–1517
Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S, Arner P (2001) Irbesartan in patients with type 2 diabetes and microalbuminuria study group. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med 345:870–878
Pistrosch F, Herbrig K, Kindel B, Passauer J, Fischer S, Gross P (2005) Rosiglitazone improves glomerular hyperfiltration, renal endothelial dysfunction, and microalbuminuria of incipient diabetic nephropathy in patients. Diabetes 54:2206–2211
Purdy KE, Arendshorst WJ (2000) EP1 and EP4 receptors mediate prostaglandin E2 actions in the microcirculation of rat kidney. Am J Phys 279:F755–F764
Sharma K, McCue P, Dunn SR (2003) Diabetic kidney disease in the db/db mouse. Am J Phys 284:F1138–F1144
Shaw JE, Sicree RA, Zimmet PZ (2010) Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 87:4–14
Stitt-Cavanagh EM, Faour WH, Takami K, Carter A, Vanderhyden B, Guan Y, Schneider A, Breyer MD, Kennedy CR (2010) A maladaptive role for EP4 receptors in podocytes. J Am Soc Nephrol 21:1678–1690
Thieme K, Majumder S, Brijmohan AS, Batchu SN, Bowskill BB, Alghamdi TA, Advani SL, Kabir MG, Liu Y, Advani A (2017) EP4 inhibition attenuates the development of diabetic and non-diabetic experimental kidney disease. Sci Rep 7:3442
Wall EA, Zavzavadjian JR, Chang MS, Randhawa B, Zhu X, Hsueh RC, Liu J, Driver A, Bao XR, Sternweis PC, Simon MI, Fraser ID (2009) Suppression of LPS-induced TNF-alpha production in macrophages by cAMP is mediated by PKA-AKAP95-p105. Sci Signal 16:ra28
Yang GX, Xu YY, Fan YP, Wang J, Chen XL, Zhang YD, Wu JH (2014) A maladaptive role for EP4 receptors in mouse mesangial cells. PLoS One 9:e104091
Acknowledgments
The authors thank Drs. Akiyoshi Shimaya, Yuichi Tomura, and Atsuo Tahara (Astellas Pharma Inc.) for their valuable comments and continuing encouragement.
Author information
Authors and Affiliations
Contributions
KM, HK, HY, II, EN, KW, and TU conceived and designed the research. KM, HK, HY, II, and TU performed experiments and analyzed the data. EN contributed to the synthesis of ASP7657. KM and KW wrote the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Animal studies were approved by the Institutional Animal Care and Use Committee of Astellas Pharma Inc., Tsukuba Research Center, which is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) International.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mizukami, K., Kamada, H., Yoshida, H. et al. Pharmacological properties of ASP7657, a novel, potent, and selective prostaglandin EP4 receptor antagonist. Naunyn-Schmiedeberg's Arch Pharmacol 391, 1319–1326 (2018). https://doi.org/10.1007/s00210-018-1545-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-018-1545-x