Abstract
K2P17.1 (TASK-4, TALK-2) potassium channels are expressed in the heart and represent potential targets for pharmacological management of atrial and ventricular arrhythmias. Reduced K2P17.1 expression was found in atria and ventricles of heart failure (HF) patients. Modulation of K2P17.1 currents by antiarrhythmic compounds has not been comprehensively studied to date. The objective of this study was to investigate acute effects of clinically relevant antiarrhythmic drugs on human K2P17.1 channels to provide a more complete picture of K2P17.1 electropharmacology. Whole-cell patch clamp and two-electrode voltage clamp electrophysiology was employed to study human K2P17.1 channel pharmacology. K2P17.1 channels expressed in Xenopus laevis oocytes were screened for sensitivity to antiarrhythmic drugs, revealing significant activation by propafenone (+ 296%; 100 μM), quinidine (+ 58%; 100 μM), mexiletine (+ 21%; 100 μM), propranolol (+ 139%; 100 μM), and metoprolol (+ 17%; 100 μM) within 60 min. In addition, the currents were inhibited by amiodarone (− 13%; 100 μM), sotalol (− 10%; 100 μM), verapamil (− 21%; 100 μM), and ranolazine (− 8%; 100 μM). K2P17.1 channels were not significantly affected by ajmaline and carvedilol. Concentration-dependent K2P17.1 activation by propafenone was characterized in more detail. The onset of activation was fast, and current-voltage relationships were not modulated by propafenone. K2P17.1 activation was confirmed in mammalian Chinese hamster ovary cells, revealing 7.8-fold current increase by 100 μM propafenone. Human K2P17.1 channels were sensitive to multiple antiarrhythmic drugs. Differential pharmacological regulation of repolarizing K2P17.1 background K+ channels may be employed for personalized antiarrhythmic therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Effective and safe pharmacologic treatment of atrial and ventricular arrhythmias remains an unmet need in cardiovascular medicine. Shortening of refractory periods promotes electrical re-entry that underlies atrial fibrillation (AF) and ventricular tachycardia (VT) (Tomaselli and Marbán 1999; Soucek et al. 2012; Trappe et al. 2013). Rhythm control may be achieved by impairment of electrical re-entry through cardiac K+ current inhibition by class III antiarrhythmic drugs. Two-pore-domain potassium (K2P) channels mediate K+ background currents that stabilize the negative resting membrane potential and contribute to action potential (AP) repolarization in excitable cells (Goldstein et al. 2001; Marban 2002). K2P currents are regulated through polymodal mechanisms (Goldstein et al. 2001; Enyedi and Czirják 2010; Sandoz et al. 2011, 2012; Staudacher et al. 2011a, b; Gierten et al. 2012; Schmidt et al. 2012, 2017; Seyler et al. 2014a).
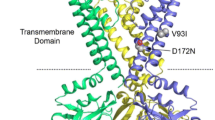
K2P17.1 channels (tandem of P domains in a weak inward rectifying K+ channel (TWIK)-related acid sensitive K+ (TASK) 4 channels, or TWIK-related alkaline pH-activated K+ (TALK) 2 channels) are expressed in the human heart, predominantly in the atria (Decher et al. 2001; Girard et al. 2001; Schmidt et al. 2015). Atrial K2P17.1 abundance is reduced in patients with heart failure (HF) or AF (Schmidt et al. 2017). The association between a genetic K2P17.1 variant and ischemic stroke in Caucasians but not in a Chinese cohort (Domingues-Montanari et al. 2010; Ma et al. 2013) further indicates a potential contribution of K2P17.1 function to AF pathophysiology. In addition, K2P17.1 expression is suppressed in human left ventricular tissue obtained from HF patients compared to patients with preserved cardiac function (Chai et al. 2017). Duration of atrial and ventricular action potentials (AP) is prolonged in patients with HF (Tomaselli and Marbán 1999; Schmidt et al. 2017), consistent with reduction of repolarizing K+ currents. By contrast, cardiac K2P17.1 current was enhanced in patients carrying a K2P17.1 channel gain-of-function mutation associated with cardiac conduction disease (K2P17.1 G88R; Friedrich et al. 2014).
K2P17.1 currents are increased upon extracellular alkalization and blocked by barium (Decher et al. 2001; Kang and Kim 2004; Duprat et al. 2005; Niemeyer et al. 2007). Changes in K2P17.1 expression and function regulate action potential duration (APD) of cardiac myocytes: expression of the K2P17.1 G88R gain-of-function mutant results in APD shortening in HL-1 murine atrial myocytes (Friedrich et al. 2014), whereas siRNA-mediated knockdown of repolarizing K2P17.1 current causes APD prolongation in cardiomyocytes derived from human-induced pluripotent stem cells (Chai et al. 2017). Pharmacologic modulation of K2P17.1 current levels may be employed to suppress atrial and ventricular arrhythmias. The development of this emerging therapeutic principle into clinical practice is limited by the lack of pharmacologic data. This study provides a systematic assessment of K2P17.1 regulation by clinically used antiarrhythmic compounds to close this scientific and translational gap. Activation of the channels by the class I antiarrhythmic drug propafenone was mechanistically studied in detail.
Methods
Patients
A total of 5 patients (mean age, 69 ± 4.1 years; male/female, 4/1) with sinus rhythm (SR) undergoing open heart surgery for coronary artery bypass grafting and/or valve replacement were included (Table 1). Tissue samples were obtained from right atrial appendages.
Molecular biology
Amplification of KCNK17 cDNA encoding human K2P17.1 protein (GenBank accession number EU978944) was described previously (Gierten et al. 2008). For in vitro transcription, human KCNK17 was subcloned into pRAT, a dual-purpose expression vector containing a CMV promoter for mammalian expression and a T7 promoter for cRNA synthesis. Plasmids were linearized with NotI and transcribed using the T7 mMessage mMachine kit (Ambion, Austin, TX, USA). RNA transcripts were quantified by spectrophotometry and cRNA integrity was assessed by agarose gel electrophoresis (Thomas et al. 2008).
Xenopus laevis oocyte preparation
Ovarian lobes were surgically removed in aseptic technique from female Xenopus laevis frogs anesthetized with 1 g/l tricaine solution (pH = 7.5). Frogs were not fed on the day of surgery to avoid emesis during anesthesia. After surgery, the frogs were allowed to recover consciousness, followed by at least 2-month recovery without surgery. Oocyte collection was alternated between left and right ovaries, and no more than four surgeries were performed on one individual frog. After the final collection of oocytes, the anesthetized frog was killed by decerebration and pithing. Following collagenase treatment (collagenase A or D; Roche Diagnostics, Mannheim, Germany), stage V–VI defolliculated oocytes were manually isolated under a stereomicroscope. For electrophysiological recordings, complementary (c)RNA (1.5–5 ng, 46 nl/oocyte) encoding human K2P17.1 was injected. For Western blot studies, 1.5 or 3 ng encoding human KCNK17 cRNA was injected (46 nl/oocyte).
Western blot analysis
Protein immunodetection was performed by sodium dodecyl sulfate (SDS) gel electrophoresis and Western blotting as described (Bikou et al. 2011; Trappe et al. 2013; Schmidt et al. 2015). Tissue sections obtained from human right atrial samples were rinsed in phosphate-buffered saline (PBS), rapidly frozen in liquid nitrogen and stored at − 80 °C. Aliquots were then homogenized (TissueRuptor, QIAGEN, Hilden, Germany) in radioimmunoprecipitation (RIPA) lysis buffer containing 50 mM Tris-HCl (pH 7.4), 0.5% NP-40, 0.25% sodium deoxycholate, 150 mM NaCl, 1 mM EDTA, 1 mM Na3VO4, 1 mM NaF, and protease inhibitors (Complete; Roche, Indianapolis, IN, USA).
To obtain Xenopus oocyte protein, 150 oocytes of each study group were harvested. Protein extracts were homogenized in a buffer containing 100 mM NaCl, 40 mM KCl, 1 mM ethylene-diamine-tetraacetic acid (EDTA), Complete Protease Inhibitor Cocktail (Roche Diagnostics, Indianapolis, USA), 10% glycerol, 1% 3-[(3-cholamidopropyl)dimethylammonio]-1-propanesulfonate (CHAPS), 20 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) (pH 7.4), and clarified by repeated centrifugations. The supernatant was diluted with 2-mercaptoethanol-containing loading buffer and subjected to Western blotting.
The protein concentration was determined using the bicinchoninic acid (BCA) protein assay (Thermo Scientific, Rockford, IL, USA), and equal amounts of protein were separated on SDS polyacrylamide gels. Nitrocellulose membranes were developed by sequential exposure to blocking reagent containing 5% dry milk (supplemented with 3% bovine serum albumin for oocyte experiments), primary antibodies directed against K2P17.1 (1:200; ab198043, Abcam, Cambridge, UK), and appropriate HRP-conjugated secondary antibodies (1:3000; ab6802; Abcam). Signals were developed using the enhanced chemiluminescence assay (ECL Western Blotting Reagents, GE Healthcare, Buckinghamshire, UK) and quantified with ImageJ 1.41 Software (National Institutes of Health, Bethesda, MD, USA). Protein content was normalized to glyceraldehyde 3-phosphate dehydrogenase (GAPDH) using anti-GAPDH primary antibodies (1:10,000; G8140-01; US Biological, Swampscott, MA, USA for human tissue; 1:10,000; ab181602; Abcam for oocyte protein) and corresponding secondary antibodies (1,3000; sc-2005; Santa Cruz Biotechnology) for quantification of optical density.
Cell culture
Chinese hamster ovary (CHO) cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM; Invitrogen, Karlsruhe, Germany) supplemented with 10% fetal bovine serum (Invitrogen), 100 U/ml penicillin G sodium, and 100 μg/ml streptomycin sulfate in an atmosphere of 95% humidified air and 5% CO2 at 37 °C. Cells were passaged regularly and subcultured prior to treatment. KCNK17 was expressed using transient transfections in CHO cells. The total DNA transfected was equal to 2.0 μg for both conditions (1.8 μg of KCNK17 + 0.2 μg of yellow fluorescent protein (YFP) to identify transfected cells). Transfection of CHO cells was accomplished using Lipofectamine 2000 (Life Technologies, Grand Island, NY, USA) according to the manufacturer’s protocol, using 35-mm dishes.
Electrophysiology
Two-electrode voltage clamp measurements were performed to record whole cell currents from Xenopus laevis oocytes 3–4 days after cRNA injection as described (Thomas et al. 2008; Gierten et al. 2012). Two-electrode voltage clamp electrodes were pulled from 1 mm borosilicate glass tubes (Science Products, Hofheim, Germany) using a P-87 micropipette puller (Sutter Instruments, Novato, CA, USA). Macroscopic currents were recorded using an Oocyte Clamp amplifier OC-725C (Warner Instruments, Hamden, CT, USA) and pClamp software (Molecular Devices, Sunnyvale, CA, USA). Data were sampled at 2 kHz and low-pass filtered at 1 kHz. Leak currents were not subtracted. Current amplitudes were determined at the end of + 20-mV voltage pulses unless stated otherwise. Voltage clamp measurements were carried out at room temperature (20–22 °C). Voltage clamp electrodes filled with 3 M KCl solution had tip resistances of 1.5–3 MΩ. Experiments were performed under constant perfusion by a gravity-driven perfusion system. The standard extracellular bath solution contained 96 mM NaCl, 4 mM KCl, 1.1 mM CaCl2, 1 mM MgCl2, and 5 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES). The pH was adjusted with NaOH to pH 8.5 to activate human K2P17.1 currents (Decher et al. 2001; Seyler et al. 2014a).
Currents were recorded from CHO cells with the whole cell patch-clamp technique using an Axopatch 200B amplifier and a Digidata 1440A (both from Molecular Devices). Voltage-clamp command pulses were inputted using pCLAMP version 10 (Molecular Devices). Patch-clamp pipettes were pulled from 8161 Corning borosilicate capillary glass (Dow-Corning, Midland, MI, USA) and polished. Tip resistances ranged from 1.0 to 2.2 MΩ. The extracellular bath solution contained (in mM at pH 8.5 adjusted with NaOH) 140 NaCl, 5 KCl, 1 MgCl2, 1.8 CaCl2, 10 HEPES, and 10 glucose. The intracellular pipette solution contained (in mM at pH 7.2 adjusted with KOH) 100 K-aspartate, 20 KCl, 2 MgCl2, 1 CaCl2, 10 EGTA, 2 ATP, and 10 HEPES. Of note, no difference in K2P17.1 current density was observed using HEPES or AMPSO (((1,1-dimethyl-2-hydroxyethyl)amino)-2-hydroxypropanesulfonic acid sodium salt) to adjust extracellular pH to 8.5, respectively (data not shown). Patch clamp recordings were performed at 23 °C.
Drugs
Drugs were obtained from Sigma-Aldrich (Steinheim, Germany), unless indicated otherwise. Ajmaline (abcr, Karlsruhe, Germany), amiodarone, carvedilol, mexiletine, propafenone, propranolol, sotalol, and quinidine were dissolved in dimethyl sulfoxide (DMSO) to 100 mM stock solutions. Metoprolol was dissolved in H2O to a 100 mM stock solution. Ranolazine was dissolved in H2O to a 10 mM stock solution. Amitriptyline and verapamil were dissolved in methanol to 100 mM stock solutions. Stock solutions were stored at − 20 °C. Aliquots of the stock solutions were diluted to the desired concentration with the bath solution on the day of experiments.
Data analysis and statistics
PCLAMP 8.2 (Axon Instruments, Foster City, USA), Origin 8 (OriginLab, Northampton, MA, USA), Prism 6.0 (GraphPad, La Jolla, CA, USA) and Excel (Microsoft, Redmond, WA, USA) software was used for data acquisition and analysis. Concentration-response relationships for drug-induced activation were fit with a Hill equation of the following form: y = Imin + (Imax − Imin) × EC50n/(EC50n + xn), where I indicates current, n is the Hill coefficient, and EC50 is the concentration necessary for half-maximal activation. Data are expressed as mean ± standard error of the mean (SEM). Paired and unpaired Student’s t tests (two-tailed tests) were applied to compare statistical significance of the results. P < 0.05 was considered as statistically significant.
Results
K2P17.1 expression in human atrium
K2P17.1 protein was expressed in human atrium (Fig. 1a). This finding is consistent with previous studies reporting predominant atrial expression of KCNK17 mRNA or K2P17.1 protein (Decher et al. 2001; Girard et al. 2001; Schmidt et al. 2015, 2017) and highlights potential physiological significance of K2P17.1 currents in atrial electrophysiology and arrhythmogenesis. Specific detection of recombinant human K2P17.1 protein expressed in Xenopus laevis oocytes and the lack of anti-K2P17.1 immunoreactivity in uninjected oocytes, indicating specificity of the antibodies used (Fig. 1b).
Western blot analysis of K2P17.1 protein. a Representative immunoblots obtained from right atrial appendages (RAA) of five patients undergoing cardiac surgery, probed with anti-K2P17.1 antibodies. b Protein lysates from Xenopus oocytes heterologously expressing human K2P17.1 protein (1.5 or 3 ng RNA/oocyte as indicated) and from uninjected (uninj.) control oocytes served as positive and negative controls, respectively. Lower panels, anti-glyceraldehyde 3-phosphate dehydrogenase (GAPDH) antibodies were applied to confirm equal protein load
Regulation of K2P17.1 function by antiarrhythmic drugs
Electropharmacology of K2P17.1 channels was assessed using the Xenopus laevis oocyte system and two-electrode voltage-clamp electrophysiology. For screening experiments, supratherapeutic concentrations were applied to ensure the detection of any potential drug-channel interactions. From a holding potential of − 80 mV, test pulses were applied for 500 ms to voltages between − 140 and + 80 mV in 20 mV increments (0.5 Hz) (Fig. 2). Current amplitudes were measured at the end of the + 20 mV pulse before and after drug application for 60 min (Fig. 2a–n). K2P17.1 currents were activated by antiarrhythmic drugs quinidine (+ 57.7 ± 12.2%; n = 5; p = 0.009; 100 μM), mexiletine (+ 20.6 ± 4.0%; n = 6; p = 0.0002; 100 μM), propafenone (+ 296.1 ± 39.2%; n = 6; p = 0.001; 100 μM), metoprolol (+ 17.3 ± 3.6%; n = 6; p = 0.009; 100 μM), and propranolol (+ 139.2 ± 22.7%; n = 6; p = 0.005; 100 μM), respectively (Figs. 2b–d, f, g and 3). By contrast, K2P17.1 current amplitudes were reduced upon application of sotalol (− 9.8 ± 1.8%; n = 5; p = 0.008; 100 μM), amiodarone (− 12.5 ± 4.2%; n = 6; p = 0.010), verapamil (− 20.5 ± 4.5%; n = 5; p = 0.013; 100 μM), and ranolazine (− 8.3 ± 1.1%; n = 6; p = 0.012; 100 μM) (Figs. 2h–k and 3). For comparison, the antidepressant amitriptyline that harbors proarrhythmic potential through inhibition of cardiac K+ currents (Witchel et al. 2003) was studied. Amitriptyline did not significantly affect K2P17.1 current amplitudes (− 7.9 ± 3.8%; n = 5; p = 0.088; 100 μM) (Figs. 2l and 3). Application of the solvent DMSO (60 min; 0.1% v/v) did not significantly affect mean K2P current amplitudes (+ 0.8 ± 3.2%; n = 5; p = 0.47) (Figs. 2m and 3), while the solvent methanol (0.1% v/v) resulted in weak current activation (+ 9.7 ± 2.5%; n = 6; p = 0.008) within 60 min (Figs. 2n and 3). Of note, methanol was used as solvent for verapamil and amitriptyline only. Considering 9.7% activation of K2P17.1 currents after 60 min methanol application and 20.5% (verapamil) or 7.9% (amitriptyline) inhibition compared with drug-free control conditions, the total degree of K2P17.1 inhibition amounts to 30.2% (verapamil; p = 0.001 versus methanol) or 17.6% (amitriptyline; p = 0.006 vs. methanol), respectively.
Pharmacology of human K2P17.1 potassium channels expressed in Xenopus oocytes. Representative macroscopic currents recorded under control conditions and after drug application (60 min, left panels) with time courses of K2P17.1 current modulation at + 20 mV membrane potential (right panels) are displayed for ajmaline (a), quinidine (b), mexiletine (c), propafenone (d), carvedilol (e), metoprolol (f), propranolol (g), sotalol (h), amiodarone (i), verapamil (j), ranolazine (k), and amitriptyline (l). The solvents dimethyl sulfoxide (DMSO; m) and methanol (n) were studied for comparison
Comparison of activating and inhibitory drug effects on K2P17.1. Currents recorded from Xenopus oocytes were quantified at + 20 mV membrane voltage after application of indicated compounds for 60 min. Values are provided normalized to control conditions prior to administration of the respective drugs. Data are given as mean ± SEM; *p < 0.05, **p < 0.01, ***p < 0.001 versus drug-free control measurements (n = 5 to 6 cells)
Biophysical analysis of K2P17.1 activation by propafenone
Biophysical characteristics of K2P17.1 current enhancement by propafenone, the drug-K2P17.1 channel interaction with most pronounced functional effects, were studied in more detail using the Xenopus oocyte expression system. Currents were recorded as described in Fig. 2 and quantified at + 20 mV after propafenone administration for 60 min. The onset of activation is shown in Fig. 2d (n = 6). After a control period of 30 min showing stable current levels, K2P17.1 current activation by 100 μM propafenone developed rapidly. To assess the concentration dependence of hK2P17.1 activation by propafenone, currents in the presence of the drug were normalized to their respective control values and plotted as relative current amplitudes in Fig. 4a (n = 3 to 6 cells were investigated at each concentration). The half-maximal effective concentration (EC50) for activation of K2P17.1 channels was 75.4 ± 0.53 μM with a Hill coefficient nH of 9.1 ± 0.15.
Pharmacological and biophysical analysis of K2P17.1 activation by propafenone. a Concentration-response relationships for the effect of propafenone on human K2P17.1 currents measured in Xenopus oocytes at the end of the + 20 mV voltage step after 60 min drug application (n = 3 to 6 cells). The EC50 value yielded 75.4 μM. b–e Effects of propafenone on hK2P17.1 voltage-dependence of activation. Control measurement (b) and the effect of 100 μM propafenone (60 min; c) are shown in one representative oocyte; d and e display activation curves, i.e., step current amplitudes as function of test potentials, recorded under isochronal conditions (d original current amplitudes; e values normalized to maximum currents) (n = 6). Data are provided as mean ± SEM
Drug effects on K2P17.1 current voltage (I-V) relationship were investigated under isochronal recording conditions using the protocol described above. Representative families of current traces from one cell are shown for control conditions (Fig. 4b) and after application of 100 μM propafenone for 60 min (Fig. 4c). The current-voltage relationship was not affected by propafenone administration (Fig. 4d, e). Mean half-maximal activation voltage (V1/2) normalized to current amplitudes recorded at + 60 mV was 11.2 ± 1.1 mV under control conditions and yielded 11.7 ± 1.4 mV (n = 5; p = 0.84) in the presence of propafenone.
Propafenone-induced K2P17.1 current enhancement in mammalian cells
We expressed hK2P17.1 potassium channels in Chinese hamster ovary (CHO) cells to demonstrate modulation of K2P17.1 currents in mammalian cells (Fig. 5). From a holding potential of − 80 mV, depolarizing pulses were applied for 500 ms to voltages between − 120 and + 80 mV in 20-mV increments (Fig. 5a, b). Propafenone (100 μM, 30 min) activated K2P17.1 currents by 7.8-fold (n = 6–13; p < 0.0001) (Fig. 5c). Concentration-dependent activation was analyzed at + 20 mV after propafenone application for 30 min (Fig. 5d). The half-maximal activating concentration could not be calculated as maximum activation was not reached with the highest concentration applied without compromising CHO cell integrity.
Propafenone-induced activation of human K2P17.1 channels expressed in Chinese hamster ovary (CHO) cells. Families of current traces recorded under control conditions and after superfusion with 100 μM propafenone were normalized to capacitance and are displayed in a and b, respectively. c Mean activation curves obtained under control conditions and after application of 100 μM propafenone (n = 5). d Concentration-response relationships for the effect of propafenone on hK2P17.1 currents measured at + 20 mV (n = 3 to 7 cells; mean ± SEM)
Discussion
Cardiovascular pharmacology of human K2P17.1 K+ channels: comparison with previous studies
The present work reveals that human cardiac K2P17.1 background K+ channels are previously unrecognized targets for multiple antiarrhythmic drugs. K2P17.1 currents were activated by class I antiarrhythmic compounds (quinidine, mexiletine, propafenone) and by β-blockers (metoprolol, propranolol). By contrast, class III drugs (amiodarone, sotalol), a class IV compound (verapamil), and the late sodium current inhibitor, ranolazine, inhibited K2P17.1. There is, however, no uniform class effect of antiarrhythmics on K2P17.1 function, as other class I (ajmaline, flecainide) or III drugs (dronedarone) as well as β-blockers (carvedilol) did not affect K2P17.1 current amplitudes or even induced opposite effects (e.g., K2P17.1 activation by the class III drug vernakalant) here and in prior studies (Table 2). Among drugs investigated, quinine and quinidine displayed both inhibitory and activating actions on K2P17.1 channels in independent studies (Table 2). While these differences cannot be fully resolved based on available data, we may speculate that different experimental conditions determined whether quinine and quinidine caused activation or inhibition of K2P17.1, respectively.
K2P17.1 channel activation or inhibition occurred at concentrations exceeding free plasma levels (Table 2), indicating low clinical significance of K2P17.1 modulation during clinical application of the respective drugs with current dosing recommendations. Therefore, associations between in vitro modulation of K2P17.1 and clinical effects cannot be established at the present, early stage of K2P17.1 pharmacology research. However, impaired metabolism may result in significantly higher plasma levels and in modulation of K2P17.1 channel function during drug administration. Although novel pharmacological interactions reported here may not affect cardiac cellular electrophysiology in routine clinical practice, differential actions of antiarrhythmic drugs on K2P17.1 channels provide the basis for future research and development aimed at the identification of more potent and selective K2P17.1 modulators. A comparison of multiple different chemical structures described here as K2P17.1 blockers or activators is expected to support the targeted design of novel compounds.
Mechanism of K2P17.1 current activation by propafenone
The rapid onset of activation indicates a direct drug–channel interaction and provides evidence against decreased protein turnover or impaired protein degradation as molecular mechanism of action. The Hill coefficient of 9.1 may indicate multiple binding sites for propafenone within the K2P17.1 channel protein with positively cooperative binding. K2P17.1 current–voltage relationships were not altered by propafenone, indicating that protein domains responsible for voltage sensing were not directly affected. Of note, biophysical characteristics of K2P17.1 activation by propafenone are shared with those observed with vernakalant, a class III drug previously reported to activate K2P17.1 (Seyler et al. 2014b), suggesting a common molecular mechanism of current activation that remains to be elucidated in more detail in future studies.
Clinical significance of pharmacologic K2P17.1 current activation and inhibition—implications for therapy
Complex and heterogenous mechanisms of cardiac arrhythmia require differential antiarrhythmic therapy with appropriate approaches. The “classical” mechanism of atrial arrhythmogenesis in AF involves reduced electrical conduction velocity and shortening of atrial action potential duration (APD) and effective refractory periods (AERPs) that perpetuate AF through promotion of electrical reentry (Schotten et al. 2011). These alterations are observed in patients with persistent or permanent AF that do not exhibit severe HF (Schmidt et al. 2017). At the molecular level, increased potassium currents are primarily responsible for shortening of refractoriness (Schotten et al. 2011; Schmidt et al. 2015, 2017). In these cases, inhibition of repolarizing K2P17.1 currents that are substantially expressed in human atrium may be effective to suppress AF. By contrast, atrial action potentials are shortened and K2P17.1 expression is reduced in patients with HF (Schmidt et al. 2017). Furthermore, ventricular electrical remodeling is similarly characterized by prolonged ventricular refractoriness and reduced K+ channel abundance including K2P17.1 (Tomaselli and Marbán 1999; Nattel et al. 2007; Chai et al. 2017). Here, activation of K2P17.1 channels may be employed as antiarrhythmic principle. Whether in vitro membrane hyperpolarization through K2P17.1 activation may suppress automaticity and triggered activity in vivo remains to be confirmed in future studies using specific, high-affinity activators and appropriate animal models.
Conclusion
Cardiac K2P17.1 channels are differentially regulated by multiple antiarrhythmic drugs. This work highlights a mechanistic link between modulation of cardiac K2P17.1 K+ currents and antiarrhythmic therapy. In addition, the data provide a molecular starting point for the development of future, mechanism-derived antiarrhythmic concepts targeting individual K2P17.1 dysfunction in cardiac arrhythmia. The therapeutic significance of cardiac K2P17.1 channel blockade or activation in specific heart rhythm disorders requires validation in translational and clinical investigations.
References
Altomare C, Barbuti A, Viscomi C, Baruscotti M, DiFrancesco D (2000) Effects of dronedarone on acetylcholine-activated current in rabbit SAN cells. Br J Pharmacol 130:1315–1320
Baker JG (2005) The selectivity of beta-adrenoceptor antagonists at the human beta1, beta2 and beta3 adrenoceptors. Br J Pharmacol 144:317–322
Bébarová M, Matejovic P, Pásek M, Simurdová M, Simurda J (2005) Effect of ajmaline on action potential and ionic currents in rat ventricular myocytes. Gen Physiol Biophys 24:311–325
Bengtsson C, Johnsson G, Regårdh CG (1975) Plasma levels and effects of metoprolol on blood pressure and heart rate in hypertensive patients after an acute dose and between two doses during long-term treatment. Clin Pharmacol Ther 17:400–408
Bigot MC, Debruyne D, Bonnefoy L, Grollier G, Moulin M, Potier JC (1991) Serum digoxin levels related to plasma propafenone levels during concomitant treatment. J Clin Pharmacol 31:521–526
Bikou O, Thomas D, Trappe K, Lugenbiel P, Kelemen K, Koch M, Soucek R, Voss F, Becker R, Katus HA, Bauer A (2011) Connexin 43 gene therapy prevents persistent atrial fibrillation in a porcine model. Cardiovasc Res 92:218–225
Björkman A, Willcox M, Marbiah N, Payne D (1991) Susceptibility of Plasmodium falciparum to different doses of quinine in vivo and to quinine and quinidine in vitro in relation to chloroquine in Liberia. Bull World Health Organ 69:459–465
Cahill SA, Gross GJ (2004) Propafenone and its metabolites preferentially inhibit IKr in rabbit ventricular myocytes. J Pharmacol Exp Ther 308:59–65
Chai S, Wan X, Nassal DM, Liu H, Moravec CS, Ramirez-Navarro A, Deschenes I (2017) Contribution of two pore potassium channels to cardiac ventricular action potential revealed using human iPSC-derived cardiomyocytes. Am J Physiol Heart Circ Physiol 312:H1144–H1153
Chatelain P, Meysmans L, Mattéazzi JR, Beaufort P, Clinet M (1995) Interaction of the antiarrhythmic agents SR 33589 and amiodarone with the beta-adrenoceptor and adenylate cyclase in rat heart. Br J Pharmacol 116:1949–1956
Chen Y, Herness MS (1997) Electrophysiological actions of quinine on voltage-dependent currents in dissociated rat taste cells. Pflugers Arch 434:215–226
Decher N, Maier M, Dittrich W, Gassenhuber J, Bruggemann A, Busch AE, Steinmeyer K (2001) Characterization of TASK-4, a novel member of the pH-sensitive, two-pore domain potassium channel family. FEBS Lett 492:84–89
Delgado C, Tamargo J, Henzel D, Lorente P (1993) Effects of propafenone on calcium current in guinea-pig ventricular myocytes. Br J Pharmacol 108:721–727
Dobrev D, Hamad B, Kirkpatrick P (2010) Vernakalant. Nat Rev Drug Discov 9:915–916
Domingues-Montanari S, Fernández-Cadenas I, Del Río-Espinola A, Mendioroz M, Fernandez-Morales J, Corbeto N, Delgado P, Ribó M, Rubiera M, Obach V, Martí-Fàbregas J, Freijo M, Serena J, Montaner J (2010) KCNK17 genetic variants in ischemic stroke. Atherosclerosis 208:203–209
Dorian P (2010) Clinical pharmacology of dronedarone: implications for the therapy of atrial fibrillation. J Cardiovasc Pharmacol Ther 15(4 Suppl):15S–18S
Du CY, El Harchi A, Zhang YH, Orchard CH, Hancox JC (2011) Pharmacological inhibition of the hERG potassium channel is modulated by extracellular but not intracellular acidosis. J Cardiovasc Electrophysiol 22:1163–1170
Du C, Zhang Y, El Harchi A, Dempsey CE, Hancox JC (2014) Ranolazine inhibition of hERG potassium channels: drug-pore interactions and reduced potency against inactivation mutants. J Mol Cell Cardiol 74:220–230
Duan D, Fermini B, Nattel S (1993) Potassium channel blocking properties of propafenone in rabbit atrial myocytes. J Pharmacol Exp Ther 264:1113–1123
Duprat F, Girard C, Jarretou G, Lazdunski M (2005) Pancreatic two P domain K+ channels TALK-1 and TALK-2 are activated by nitric oxide and reactive oxygen species. J Physiol 562(Pt 1):235–244
Enyedi P, Czirják G (2010) Molecular background of leak K+ currents: two-pore domain potassium channels. Physiol Rev 90:559–605
Estes NA, Manolis AS, Greenblatt DJ, Garan H, Ruskin JN (1989) Therapeutic serum lidocaine and metabolite concentrations in patients undergoing electrophysiologic study after discontinuation of intravenous lidocaine infusion. Am Heart J 117:1060–1064
Fedida D (2007) Vernakalant (RSD1235): a novel, atrial-selective antifibrillatory agent. Expert Opin Investig Drugs 16:519–532
Fedida D, Orth PM, Chen JY, Lin S, Plouvier B, Jung G, Ezrin AM, Beatch GN (2005) The mechanism of atrial antiarrhythmic action of RSD1235. J Cardiovasc Electrophysiol 16:1227–1238
Fischer F, Vonderlin N, Zitron E, Seyler C, Scherer D, Becker R, Katus HA, Scholz EP (2013) Inhibition of cardiac Kv1.5 and Kv4.3 potassium channels by the class Ia anti-arrhythmic ajmaline: mode of action. Naunyn Schmiedeberg's Arch Pharmacol 386:991–999
Friedrich C, Rinné S, Zumhagen S, Kiper AK, Silbernagel N, Netter MF, Stallmeyer B, Schulze-Bahr E, Decher N (2014) Gain-of-function mutation in TASK-4 channels and severe cardiac conduction disorder. EMBO Mol Med 6:937–951
Gehr TW, Tenero DM, Boyle DA, Qian Y, Sica DA, Shusterman NH (1999) The pharmacokinetics of carvedilol and its metabolites after single and multiple dose oral administration in patients with hypertension and renal insufficiency. Eur J Clin Pharmacol 55:269–277
Gierten J, Ficker E, Bloehs R, Schloemer K, Kathoefer S, Scholz E, Zitron E, Kiesecker C, Bauer A, Becker R, Katus HA, Karle CA, Thomas D (2008) Regulation of two-pore-domain (K2P) potassium leak channels by the tyrosine kinase inhibitor genistein. Br J Pharmacol 154:1680–1690
Gierten J, Hassel D, Schweizer PA, Becker R, Katus HA, Thomas D (2012) Identification and functional characterization of zebrafish K2P10.1 (TREK2) two-pore-domain K+ channels. Biochim Biophys Acta 1818:33–41
Girard C, Duprat F, Terrenoire C, Tinel N, Fosset M, Romey G, Lazdunski M, Lesage (2001) Genomic and functional characteristics of novel human pancreatic 2P domain K+ channels. Biochem Biophys Res Commun 282:249–256
Goldstein SA, Bockenhauer D, O'Kelly I, Zilberberg N (2001) Potassium leak channels and the KCNK family of two-P-domain subunits. Nat Rev Neurosci 2:175–184
Gross GJ, Castle NA (1998) Propafenone inhibition of human atrial myocyte repolarizing currents. J Mol Cell Cardiol 30:783–793
Guillemare E, Marion A, Nisato D, Gautier P (2000) Inhibitory effects of dronedarone on muscarinic K+ current in guinea pig atrial cells. J Cardiovasc Pharmacol 36:802–805
Haffajee CI, Love JC, Alpert JS, Asdourian GK, Sloan KC (1983) Efficacy and safety of long-term amiodarone in treatment of cardiac arrhythmias: dosage experience. Am Heart J 106:935–943
Hancox JC (1997) Amiodarone blocks L-type calcium current in single myocytes isolated from the rabbit atrioventricular node. Gen Pharmacol 29:429–435
Hancox JC, Mitcheson JS (1997) Inhibition of L-type calcium current by propafenone in single myocytes isolated from the rabbit atrioventricular node. Br J Pharmacol 121:7–14
Harmer AR, Valentin JP, Pollard CE (2011) On the relationship between block of the cardiac Na+ channel and drug-induced prolongation of the QRS complex. Br J Pharmacol 164:260–273
Hirota M, Ohtani H, Hanada E, Sato H, Kotaki H, Uemura H, Nakaya H, Iga T (2000) Influence of extracellular K+ concentrations on quinidine-induced K+ current inhibition in rat ventricular myocytes. J Pharm Pharmacol 52:99–105
Hoffmann C, Leitz MR, Oberdorf-Maass S, Lohse MJ, Klotz KN (2004) Comparative pharmacology of human beta-adrenergic receptor subtypes—characterization of stably transfected receptors in CHO cells. Naunyn Schmiedeberg's Arch Pharmacol 369:151–159
Husser D, Binias KH, Stridh M, Sornmo L, Olsson SB, Molling J, Geller C, Klein HU, Bollmann A (2005) Pilot study: Noninvasive monitoring of oral flecainide’s effects on atrial electrophysiology during persistent human atrial fibrillation using the surface electrocardiogram. Ann Noninvasive Electrocardiol 10:206–210
Jerling M (2006) Clinical pharmacokinetics of ranolazine. Clin Pharmacokinet 45:469–491
Jonkers R, van Boxtel CJ, Koopmans RP, Oosterhuis B (1989) A nonsteady-state agonist antagonist interaction model using plasma potassium concentrations to quantify the beta-2 selectivity of beta blockers. J Pharmacol Exp Ther 249:297–302
Kamiya K, Nishiyama A, Yasui K, Hojo M, Sanguinetti MC, Kodama I (2001) Short- and long-term effects of amiodarone on the two components of cardiac delayed rectifier K+ current. Circulation 103:1317–1324
Kang D, Kim D (2004) Single-channel properties and pH sensitivity of two-pore domain K+ channels of the TALK family. Biochem Biophys Res Commun 315:836–344
Karle CA, Kreye VA, Thomas D, Röckl K, Kathöfer S, Zhang W, Zhang W, Kiehn J (2001) Antiarrhythmic drug carvedilol inhibits HERG potassium channels. Cardiovasc Res 49:361–370
Keefe DL, Yee YG, Kates RE (1981) Verapamil protein binding in patients and in normal subjects. Clin Pharmacol Ther 29:21–26
Kiesecker C, Zitron E, Lück S, Bloehs R, Scholz EP, Kathöfer S, Thomas D, Kreye VA, Katus HA, Schoels W, Karle CA, Kiehn J (2004) Class Ia anti-arrhythmic drug ajmaline blocks HERG potassium channels: mode of action. Naunyn Schmiedeberg's Arch Pharmacol 370:423–435
Köppel C, Wagemann A, Martens F (1989) Pharmacokinetics and antiarrhythmic efficacy of intravenous ajmaline in ventricular arrhythmia of acute onset. Eur J Drug Metab Pharmacokinet 14:161–167
Koumi S, Sato R, Hayakawa H, Okumura H (1991) Quinidine blocks cardiac sodium current after removal of the fast inactivation process with chloramine-T. J Mol Cell Cardiol 23:427–438
Läer S, Neumann J, Scholz H (1997) Interaction between sotalol and an antacid preparation. Br J Clin Pharmacol 43:269–272
Lalevée N, Nargeot J, Barrére-Lemaire S, Gautier P, Richard S (2003) Effects of amiodarone and dronedarone on voltage-dependent sodium current in human cardiomyocytes. J Cardiovasc Electrophysiol 14:885–890
Larsson-Backström C, Arrhenius E, Sagge K (1985) Comparison of the calcium-antagonistic effects of terodiline, nifedipine and verapamil. Acta Pharmacol Toxicol (Copenh) 57:8–17
Latini R, Tognoni G, Kates RE (1984) Clinical pharmacokinetics of amiodarone. Clin Pharmacokinet 9:136–156
Lish PM, Weikel JH, Dungan KW (1965) Pharmacological and toxicological properties of two new beta-adrenergic receptor antagonists. J Pharmacol Exp Ther 149:161–173
Ma Q, Wang Y, Shen Y, Liu X, Zhu X, Zhang H, Liu L, Tan X, Wang L, Wang X (2013) The rs10947803 SNP of KCNK17 is associated with cerebral hemorrhage but not ischemic stroke in a Chinese population. Neurosci Lett 539:82–85
Marban E (2002) Cardiac channelopathies. Nature 415:213–218
McPhillips JJ, Schwemer GT, Scott DI, Zinny M, Patterson D (1988) Effects of carvedilol on blood pressure in patients with mild to moderate hypertension. A dose response study. Drugs 36(Suppl 6):82–91
Michel D, Wegener JW, Nawrath H (2002) Effects of quinine and quinidine on the transient outward and on the L-type Ca2+ current in rat ventricular cardiomyocytes. Pharmacology 65:187–192
Mitcheson JS, Hancox JC (1997) Modulation by mexiletine of action potentials, L-type Ca current and delayed rectifier K current recorded from isolated rabbit atrioventricular nodal myocytes. Pflugers Arch 434:855–858
Mo ZL, Faxel T, Yang YS, Gallavan R, Messing D, Bahinski A (2009) Effect of compound plate composition on measurement of hERG current IC50 using PatchXpress. J Pharmacol Toxicol Methods 60:39–44
Morgan T, Anderson A, Cripps J, Adam W (1990) Pharmacokinetics of carvedilol in older and younger patients. J Hum Hypertens 4:709–715
Nattel S, Maguy A, Le Bouter S, Yeh YH (2007) Arrhythmogenic ion-channel remodeling in the heart: heart failure, myocardial infarction, and atrial fibrillation. Physiol Rev 87:425–456
Nayak TK, Harinath S, Nama S, Somasundaram K, Sikdar SK (2009) Inhibition of human two-pore domain K+ channel TREK1 by local anesthetic lidocaine: negative cooperativity and half-of-sites saturation kinetics. Mol Pharmacol 76:903–917
Nicholas J, Boyle DM, Kinney CD, Salathia K, Shanks RG (1986) Plasma concentrations and acceptability of mexiletine given by intramuscular injection in patients admitted to a coronary care unit. J Cardiovasc Pharmacol 8:21–28
Niemeyer MI, González-Nilo FD, Zúñiga L, González W, Cid LP, Sepúlveda FV (2007) Neutralization of a single arginine residue gates open a two-pore domain, alkali-activated K+ channel. Proc Natl Acad Sci U S A 104:666–671
Orth PM, Hesketh JC, Mak CK, Yang Y, Lin S, Beatch GN, Ezrin AM, Fedida D (2006) RSD1235 blocks late INa and suppresses early afterdepolarizations and torsades de pointes induced by class III agents. Cardiovasc Res 70:486–496
Otani M, Fukuda T, Naohara M, Maune H, Senda C, Yamamoto I, Azuma J (2003) Impact of CYP2D6*10 on mexiletine pharmacokinetics in healthy adult volunteers. Eur J Clin Pharmacol 59:395–399
Penniman JR, Kim DC, Salata JJ, Imredy JP (2010) Assessing use-dependent inhibition of the cardiac Na+ current (INa) in the PatchXpress automated patch clamp. J Pharmacol Toxicol Methods 62:107–118
Pine M, Favrot L, Smith S, McDonald K, Chidsey CA (1975) Correlation of plasma propranolol concentration with therapeutic response in patients with angina pectoris. Circulation 52:886–893
Rajamani S, El-Bizri N, Shryock JC, Makielski JC, Belardinelli L (2009) Use-dependent block of cardiac late Na+ current by ranolazine. Heart Rhythm 6:1625–1631
Reiter MJ, Higgins SL, Payne AG, Mann DE (1986) Effects of quinidine versus procainamide on the QT interval. Am J Cardiol 58:512–516
Ridley JM, Milnes JT, Witchel HJ, Hancox JC (2004) High affinity HERG K+ channel blockade by the antiarrhythmic agent dronedarone: resistance to mutations of the S6 residues Y652 and F656. Biochem Biophys Res Commun 325:883–891
Rigby JW, Scott AK, Hawksworth GM, Petrie JC (1985) A comparison of the pharmacokinetics of atenolol, metoprolol, oxprenolol and propranolol in elderly hypertensive and young healthy subjects. Br J Clin Pharmacol 20:327–331
Roy D, Rowe BH, Stiell IG, Coutu B, Ip JH, Phaneuf D, Lee J, Vidaillet H, Dickinson G, Grant S, Ezrin AM, Beatch GN, Investigators CRAFT (2004) A randomized, controlled trial of RSD1235, a novel anti-arrhythmic agent, in the treatment of recent onset atrial fibrillation. J Am Coll Cardiol 44:2355–2361
Sandoz G, Bell SC, Isacoff EY (2011) Optical probing of a dynamic membrane interaction that regulates the TREK1 channel. Proc Natl Acad Sci U S A 108:2605–2610
Sandoz G, Levitz J, Kramer RH, Isacoff EY (2012) Optical control of endogenous proteins with a photoswitchable conditional subunit reveals a role for TREK1 in GABAB signaling. Neuron 74:1005–1014
Schmidt C, Wiedmann F, Schweizer PA, Becker R, Katus HA, Thomas D (2012) Novel electrophysiological properties of dronedarone: inhibition of human cardiac two-pore-domain potassium (K2P) channels. Naunyn Schmiedeberg's Arch Pharmacol 385:1003–1016
Schmidt C, Wiedmann F, Voigt N, Zhou XB, Heijman J, Lang S, Albert V, Kallenberger S, Ruhparwar A, Szabo G, Kallenbach K, Karck M, Borggrefe M, Biliczki P, Ehrlich JR, Baczko I, Lugenbiel P, Schweizer PA, Donner BC, Katus HA, Dobrev D, Thomas D (2015) Upregulation of K2P3.1 K+ current causes action potential shortening in patients with chronic atrial fibrillation. Circulation 132:82–92
Schmidt C, Wiedmann F, Zhou XB, Heijman J, Voigt N, Ratte A, Lang S, Kallenberger S, Campana C, Weymann A, De Simone R, Szabo G, Ruhparwar A, Kallenbach K, Karck M, Ehrlich JR, Baczkó I, Borggrefe M, Ravens U, Dobrev D, Katus HA, Thomas D (2017) Inverse remodeling of K2P3.1 K+ channel expression and action potential duration in left ventricular dysfunction and atrial fibrillation—implications for patient-specific antiarrhythmic drug therapy. Eur Heart J 38:1764–1774
Schotten U, Verheule S, Kirchhof P, Goette A (2011) Pathophysiological mechanisms of atrial fibrillation: a translational appraisal. Physiol Rev 91:265–325
Seki A, Hagiwara N, Kasanuki H (1999) Effects of propafenone on K currents in human atrial myocytes. Br J Pharmacol 126:1153–1162
Seyler C, Li J, Schweizer PA, Katus HA, Thomas D (2014a) Inhibition of cardiac two-pore-domain K+ (K2P) channels by the antiarrhythmic drug vernakalant – comparison with flecainide. Eur J Pharmacol 724:51–57
Seyler C, Schweizer PA, Zitron E, Katus HA, Thomas D (2014b) Vernakalant activates human cardiac K2P17.1 background K+ channels. Biochem Biophys Res Commun 451:415–420
Sheldon R, Duff H, Koshman ML (1995) Antiarrhythmic activity of quinine in humans. Circulation 92:2944–2950
Slawsky MT, Castle NA (1994) K+ channel blocking actions of flecainide compared with those of propafenone and quinidine in adult rat ventricular myocytes. J Pharmacol Exp Ther 269:66–74
Soucek R, Thomas D, Kelemen K, Bikou O, Seyler C, Voss F, Becker R, Koenen M, Katus HA, Bauer A (2012) Genetic suppression of atrial fibrillation using a dominant-negative ether-a-go-go-related gene mutant. Heart Rhythm 9:265–272
Staudacher K, Baldea I, Kisselbach J, Staudacher I, Rahm AK, Schweizer PA, Becker R, Katus HA, Thomas D (2011a) Alternative splicing determines mRNA translation initiation and function of human K2P10.1 K+ channels. J Physiol 589:3709–3720
Staudacher K, Staudacher I, Ficker E, Seyler C, Gierten J, Kisselbach J, Rahm AK, Trappe K, Schweizer PA, Becker R, Katus HA, Thomas D (2011b) Carvedilol targets human K2P3.1 (TASK1) K+ leak channels. Br J Pharmacol 163:1099–1110
Supanaranond W, Davis TM, Pukrittayakamee S, Silamut K, Karbwang J, Molunto P, Chanond L, White NJ (1991) Disposition of oral quinine in acute falciparum malaria. Eur J Clin Pharmacol 40:49–52
Tamura A, Ogura T, Uemura H, Reien Y, Kishimoto T, Nagai T, Komuro I, Miyazaki M, Nakaya H (2009) Effects of antiarrhythmic drugs on the hyperpolarization-activated cyclic nucleotide-gated channel current. J Pharmacol Sci 110:150–159
Tanabe T, Yoshikawa H, Furuya H, Goto Y (1988) Therapeutic effectiveness and plasma levels of single or combination use of class I antiarrhythmic agents for ventricular arrhythmias. Jpn Circ J 52:298–305
Thomas D, Plant LD, Wilkens CM, McCrossan ZA, Goldstein SAN (2008) Alternative translation initiation in rat brain yields K2P2.1 potassium channels permeable to sodium. Neuron 58:859–870
Tomaselli GF, Marbán E (1999) Electrophysiological remodeling in hypertrophy and heart failure. Cardiovasc Res 42:270–283
Trappe K, Thomas D, Bikou O, Kelemen K, Lugenbiel P, Voss F, Becker R, Katus HA, Bauer A (2013) Suppression of persistent atrial fibrillation by genetic knockdown of caspase 3: a pre-clinical pilot study. Eur Heart J 34:147–157
Volz M, Mitrovic V, Thiemer J, Schlepper M (1995) Steady-state plasma kinetics of slow-release propafenone, its two isomers and its main metabolites. Arzneimittelforschung 45:246–249
Waelbroeck M, Taton G, Delhaye M, Chatelain P, Camus JC, Pochet R, Leclerc JL, De Smet JM, Robberecht P, Christophe J (1983) The human heart beta-adrenergic receptors. II. Coupling of beta 2-adrenergic receptors with the adenylate cyclase system. Mol Pharmacol 24:174–182
Wang Z, Fermini B, Nattel S (1995) Effects of flecainide, quinidine, and 4-aminopyridine on transient outward and ultrarapid delayed rectifier currents in human atrial myocytes. J Pharmacol Exp Ther 272:184–196
Wanwimolruk S, Denton JR (1992) Plasma protein binding of quinine: binding to human serum albumin, alpha 1-acid glycoprotein and plasma from patients with malaria. J Pharm Pharmacol 44:806–811
Watanabe Y, Hara Y, Tamagawa M, Nakaya H (1996) Inhibitory effect of amiodarone on the muscarinic acetylcholine receptor-operated potassium current in guinea pig atrial cells. J Pharmacol Exp Ther 279:617–624
Wettwer E, Christ T, Endig S, Rozmaritsa N, Matschke K, Lynch JJ, Pourrier M, Gibson JK, Fedida D, Knaut M, Ravens U (2013) The new antiarrhythmic drug vernakalant: ex vivo study of human atrial tissue from sinus rhythm and chronic atrial fibrillation. Cardiovasc Res 98:145–154
Witchel HJ, Hancox JC, Nutt DJ (2003) Psychotropic drugs, cardiac arrhythmia, and sudden death. J Clin Psychopharmacol 23:58–77
Yan M, Fan P, Shi Y, Feng L, Wang J, Zhan G, Li B (2016) Stereoselective blockage of quinidine and quinine in the hERG channel and the effect of their rescue potency on drug-induced hERG trafficking defect. Int J Mol Sci 17:1648
Yang T, Snyders DJ, Roden DM (1997) Rapid inactivation determines the rectification and [K+]o dependence of the rapid component of the delayed rectifier K+ current in cardiac cells. Circ Res 80:782–789
Yatani A, Akaike N (1985) Blockage of the sodium current in isolated single cells from rat ventricle with mexiletine and disopyramide. J Mol Cell Cardiol 17:467–476
Zhang S, Zhou Z, Gong Q, Makielski JC, January CT (1999) Mechanism of block and identification of the verapamil binding domain to HERG potassium channels. Circ Res 84:989–998
Zhang YH, Colenso CK, Sessions RB, Dempsey CE, Hancox JC (2011) The hERG K+ channel S4 domain L532P mutation: characterization at 37°C. Biochim Biophys Acta 1808:2477–2487
Acknowledgements
We thank Simone Bauer, Christine Jeckel, Jennifer Kleist, Axel Schöffel, Kai Sona and Nadine Weiberg for excellent technical assistance. This work was supported in part by research grants from the University of Heidelberg, Faculty of Medicine (Physician Scientist Program to I.S. and to A.K.R.), from the German Cardiac Society (German Cardiac Society Scholarship to I.S. and to A.K.R., Otto Hess Scholarship to S.S.), from the German Heart Foundation/German Foundation of Heart Research (Kaltenbach Scholarship to D.G., project F/08/14 to D.T.), from the Else Kröner-Fresenius-Stiftung (2014_A242 to D.T.), from the Joachim Siebeneicher Foundation (to D.T.), from the Deutsche Forschungsgemeinschaft (German Research Foundation; SCHW 1611/1-1 to P.A.S., TH 1120/8-1 to D.T.), and from the Ministry of Science, Research and the Arts Baden-Wuerttemberg (Sonderlinie Medizin to D.T.). C.I. and T.W. were supported by the Cardiology Career Program of the Department of Cardiology, University of Heidelberg. P.A.S was supported by the Heidelberg Research Centre for Molecular Medicine (Senior Career Fellowship). Additionally, portions of this work were supported by NIH/NHLBI 1R01HL124245 (to I.D.) and an American Heart Association Pre-Doctoral Fellowship from the Great Rivers Affiliate 15PRE25700037 (to S.C.).
Author contribution statement
IS, CI, ID, AKR and DT conceived and designed research. IS, CI, SC, ID, SS, DG, MEM, TW and AKR conducted experiments. CM contributed new analytical tools. IS, CI, SC, ID, DG, MEM, TW, AKR, PAS, HAK and DT analyzed data and participated in data interpretation. IS, CI, DG, MEM, TW, AKR and DT wrote the manuscript. IS, CI, SC, ID, SS, DG, MEM, TW, AKR, PAS, HAK and DT critically revised the manuscript for important intellectual content. All authors read and approved the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics statement
This study has been carried out in accordance with the Guide for the Care and Use of Laboratory Animals as adopted and promulgated by the US National Institutes of Health (NIH publication no. 85-23, revised 1985), and the current version of the German Law on the Protection of Animals was followed. The investigation conforms to the Directive 2010/63/EU of the European Parliament. The study protocol involving human tissue samples was approved by the ethics committee of the University of Heidelberg (Germany; Medical Faculty Heidelberg, S-017/2013). Written informed consent was obtained from all patients, and the study was conducted in accordance with the Declaration of Helsinki. Approval for experiments involving Xenopus laevis was granted by the local Animal Welfare Committee (institutional approval numbers A-38/11 and G-221/12).
Rights and permissions
About this article
Cite this article
Staudacher, I., Illg, C., Chai, S. et al. Cardiovascular pharmacology of K2P17.1 (TASK-4, TALK-2) two-pore-domain K+ channels. Naunyn-Schmiedeberg's Arch Pharmacol 391, 1119–1131 (2018). https://doi.org/10.1007/s00210-018-1535-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-018-1535-z