Abstract
Prostaglandins (PGs) are important lipid mediators of numerous physiologic and pathophysiologic processes in the kidney. PGE2, the most abundant renal PG, plays a major role in renal physiology, including renin release and glomerular hemodynamics. We investigated the renoprotective properties of the novel PGE2 EP4 receptor-selective antagonist ASP7657 in 5/6 nephrectomized rats, a chronic kidney disease (CKD) model. Eight weeks of repeated administration of ASP7657 (0.001–0.1 mg/kg) dose-dependently and significantly reduced urinary protein excretion and attenuated the development of glomerulosclerosis and tubulointerstitial damage, including fibrosis and inflammatory cell infiltration, without affecting blood pressure. Additionally, ASP7657 tended to have beneficial effects on renal function, as indicated by the decrease in plasma creatinine and blood urea nitrogen levels and attenuation of the decline in creatinine clearance (Ccr). The angiotensin II receptor blocker losartan (10 mg/kg) also showed these renoprotective effects while significantly reducing blood pressure. ASP7657 dose-dependently and significantly reduced the EP4 receptor agonist-induced increase in plasma renin activity, as assessed by angiotensin I release in normal rats. Additionally, ASP7657 attenuated hyperfiltration assessed by Ccr without changing the renal blood flow or blood pressure in diabetic rats. These results suggest that ASP7657 suppresses the progression of chronic renal failure by modulating renin release and improving renal hemodynamics, and may therefore be a promising therapeutic option for inhibiting the progression of CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease (CKD) is defined as either kidney damage or a decline in renal function as determined by a decrease in glomerular filtration rate. Over 10% of the adult population in developed countries is estimated to have some degree of CKD (Lopez-Novoa et al. 2010). In the general population, a decline in renal function is considered an independent risk factor for both cardiovascular disease and all-cause mortality. However, despite the success of several drugs, including angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), the absolute risk of renal and cardiovascular morbidity and mortality in CKD patients remains devastatingly high (Lambers Heerspink and de Zeeuw 2013). Novel drugs are therefore needed to effectively halt the progression of renal function loss.
Prostaglandins (PGs) are known to play complex roles in renal physiology and pathophysiology. In particular, PGE2, which is the most abundant renal PG, plays a major role in renal physiology, including the regulation of inflammation, volume homeostasis, salt and water balance, renal blood flow, glomerular hemodynamics, and renin release (Yokoyama et al. 2013). The pharmacological activity of PGE2 arises via four well-characterized G protein-coupled receptors known as E-type prostaglandin (EP) receptors, EP1, EP2, EP3, and EP4 (Narumiya et al. 1999). Several reports employing genetic knockout/overexpression and EP receptor-selective agonists/antagonists studies have revealed that these EP receptor subtypes have different physiologic and pathophysiologic effects in the kidney. In particular, many investigations suggest that EP4 receptors, which are most widely expressed in the kidney, play key roles in the pathophysiology of a variety of renal disorders. EP4 receptor mRNA is mainly localized to the glomeruli in normal kidneys and is highly expressed in tubular epithelial cells, interstitial cells, and podocytes under diabetic conditions (Stitt-Cavanagh et al. 2010). In addition, chronic administration of an EP4 receptor-selective agonist exacerbates albuminuria and renal fibrosis in diabetic mice (Mohamed et al. 2013). We previously showed that the newly synthesized EP4 receptor-selective antagonist ASP7657 significantly attenuated albuminuria in type 2 diabetic nephropathy mice (Mizukami et al. 2018). In addition, an EP4 receptor antagonist attenuated renal injury in non-diabetic CKD rats (Thieme et al. 2017). These findings suggest that PGE2 plays a crucial role in the development and progression of various kidney diseases such as diabetic nephropathy and non-diabetic CKD via EP4 receptors. We therefore hypothesized that EP4 receptor-selective antagonists may be beneficial for preventing CKD.
In this study, we evaluated the renoprotective effects of ASP7657 in 5/6 nephrectomized (Nx) rats, a CKD model, and explored the possible mechanisms involved in its renoprotective effects in normal and diabetic rats. In addition, we compared the effects of ASP7657 with those of the ARB losartan.
Materials and methods
Materials
ASP7657, trans-4-[({[1-(quinolin-2-ylmethyl)-5-(trifluoromethyl)-1H-indol-7 yl] carbonyl} amino) methyl] cyclohexanecarboxylic acid methanesulfonate (1:1) (Mizukami et al. 2018), and the EP4 receptor-selective agonist, ONO-4819 (Kasai et al. 2001), were synthesized at Astellas Pharma Inc. (Ibaraki, Japan). ASP7657 was suspended in 0.5% methylcellulose (MC) solution for oral administration via a stomach tube, or dissolved in saline with 2 mM NaOH for intravenous injection. ONO-4819 was dissolved in saline. Streptozotocin (STZ) was purchased from Sigma-Aldrich (St. Louis, MO, USA). Losartan potassium was purchased from LKT Laboratories, Inc. (St. Paul, MN, USA) and dissolved in 0.5% MC solution.
Animals
Male Wistar rats were purchased from Charles River Laboratories Japan (Kanagawa, Japan) or Japan SLC Inc. (Shizuoka, Japan) at age 7–8 weeks. Six-week-old male Sprague-Dawley rats were purchased from Japan SLC Inc. (Shizuoka, Japan). All animals were housed under conventional conditions with controlled temperature, humidity, and light (12-h light-dark cycle) and were provided a standard commercial diet and water ad libitum. Animal studies were approved by the Institutional Animal Care and Use Committee of Astellas Pharma Inc., Tsukuba Research Center, which is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) International.
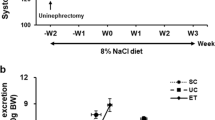
Renal protective effect of ASP7657 in 5/6 nephrectomized rats
Seven-week-old male Wistar rats were used for these experiments. Under pentobarbital anesthesia, 5/6 Nx rats were generated by ablating two thirds of the left kidney followed 1 week later by a right unilateral nephrectomy. Two weeks after the final operation, spontaneously voided urine was collected for 24 h from animals in metabolic cages, and blood samples were taken. Urinary protein concentrations were measured using a protein assay reagent (Bio-Rad Laboratories, Inc., Hercules, CA, USA). Plasma and urine creatinine and blood urea nitrogen (BUN) levels were measured using a Hitachi 7180 automatic analyzer (Hitachi High-Technologies Corporation, Tokyo, Japan). 5/6 Nx rats were grouped such that urinary protein excretion, plasma creatinine and BUN levels, urine volume, and body weight were uniform among the groups. Group compositions were as follows: normal rats, (1) normal (n = 7); 5/6 Nx rats, (2) vehicle (n = 15), (3) ASP7657 (0.001 mg/kg, n = 15), (4) ASP7657 (0.01 mg/kg, n = 15), (5) ASP7657 (0.1 mg/kg, n = 15), and (6) losartan (10 mg/kg, n = 15). ASP7657 and losartan were orally administered to 5/6 Nx rats once daily for 8 weeks. Body weight was measured every week. At weeks 2, 4, 6, and 8, 24-h urinary protein excretion and creatinine concentration were measured. At weeks 6 and 8, levels of plasma creatinine and BUN were measured. At week 5, systolic blood pressure (SBP) was recorded using the tail-cuff method (BP-98AL; Softron Inc., Tokyo, Japan). About 24 h after the final drug administration at week 8, blood samples were collected from the abdominal vena cava under isoflurane anesthesia, and the left kidney was isolated and weighed. The renal tissue was immersed in 10% neutral-buffered formalin for histological evaluation.
Histology
Specimen preparation and histopathological examination were performed at the Drug Safety Research Laboratories of Astellas Pharma Inc. Slices of renal tissue fixed in 10% neutral-buffered formalin were embedded in paraffin, and 2-μm-thick sections were cut for morphological examination. These sections were stained with hematoxylin and eosin (H&E) and periodic acid-Schiff (PAS). All glomeruli and the entire microscopic area of each specimen were examined. To determine the degree of glomerulosclerosis, a semi-quantitative score was obtained from PAS-stained sections by multiplying the grades for mesangial expansion, dilation of Bowman’s capsule, and segmental and global sclerosis (grade 0: no damage, 1: damage in 25%, 2: damage in half, 3: damage in 75%, 4: damage in the whole area of the glomeruli in the visual field). To determine the degree of tubulointerstitial damage, a semi-quantitative score was obtained from H&E-stained sections by multiplying the grades for thickening and dilation of tubule basement membrane, urinary cast, basophilic change in tubular epithelium, hyaline droplet deposition, interstitial fibrosis, and inflammatory cell infiltration (grade 0: no damage, 1: damage in 25%, 2: damage in half, 3: damage in 75%, 4: damage in the whole area of the renal cortex in the visual field).
Effect of ASP7657 on plasma renin activity in normal rats
Six-week-old male SD rats were used for these experiments. ASP7657 (0.003, 0.01, 0.03 mg/kg) was orally administered to rats, and the EP4 receptor-selective agonist ONO-4819 (0.01 mg/kg) was subcutaneously injected 1 h after drug administration. Blood samples were collected by decapitation 10 min after the ONO-4819 injection. Plasma concentrations of angiotensin I were measured using an in-house enzyme-linked immunosorbent assay as an indicator of plasma renin activity (PRA).
Effect of ASP7657 on renal hemodynamics in diabetic rats
Eight-week-old male Wistar rats were used for this study. STZ was dissolved in 1.5 mM citric acid buffer before intravenous administration at 50 mg/kg. Two or three weeks after the STZ injection, rats were anesthetized with an intraperitoneal injection of inactin (100 mg/kg), and the left femoral artery was catheterized for blood sampling and blood pressure monitoring using a pressure transducer (AP-612G, Nihon Koden, Tokyo, Japan). Another catheter was inserted into the left femoral vein for drug administration. Creatinine (100 mg/kg) was subsequently intravenously injected followed by infusion of a 1% creatinine, 2.5% glucose, and 0.45% NaCl solution (1.2 mL/h/100 g body weight) throughout the remainder of the study period. After making a flank incision, the left renal artery was isolated from the surrounding tissue and 5% phenol solution was applied to the artery for denervation. An electromagnetic flow probe was attached to the artery to monitor renal blood flow (RBF) using a magnetic blood flow meter (MVF-3100, Nihon Koden). A catheter for urine collection was placed into the left ureter. After a 1-h stabilization period, urine was collected for 20 min (from − 20 to 0 min). Blood samples were taken 10 min before drug administration. These urine and blood data were used as baseline values. ASP7657 (0.1 mg/kg) or vehicle was intravenously administered (at 0 min) followed by two consecutive sets of urine collections for 20 min (from 0 to 20 min and 20 to 40 min). Blood samples were taken 10 and 30 min after drug administration. RBF, systolic blood pressure (SBP), and diastolic blood pressure (DBP) were continuously monitored throughout the study period. Mean blood pressure (MBP) was calculated using SBP and DBP values. Renal vascular resistance (RVR) was calculated by dividing the mean arterial pressure by RBF. Group composition was as follows: normal rats, (1) normal (n = 7); diabetic rats, (2) vehicle (n = 8), (3) ASP7657 (0.1 mg/kg, n = 7). Plasma and urine creatinine concentrations were measured using CRE-EN KAINOS® (KAINOS Laboratories Inc., Tokyo, Japan). The areas under the curve (AUCs) were calculated from the percent change in creatinine clearance (Ccr), RBF, and MBP over time.
Statistical analysis
The experimental results are expressed as mean ± standard error of the mean (SEM) or standard deviation (SD). Significant differences between two groups were assessed using Student’s t test, while those among multiple groups were assessed using one-way ANOVA followed by Dunnett’s multiple comparisons test as a post hoc test. Histopathological scores were compared using a Mann-Whitney test to analyze differences between two groups, while nonparametric Kruskal-Wallis ANOVA followed by Dunn’s multiple comparisons test was used for comparisons among multiple groups. A value of p < 0.05 was considered significant. Statistical and data analyses were conducted using the SAS 9.1.3 software package (SAS Institute Japan, Ltd., Tokyo, Japan) or GraphPad Prism 7 (GraphPad Software, La Jolla, CA, USA).
Results
Renal protective effect of ASP7657 in 5/6 nephrectomized rats
Compared to normal rats, 5/6 Nx rats showed a progressive increase in urinary protein excretion (Fig. 1). Repeated administration of ASP7657 (0.01–0.1 mg/kg) dose-dependently improved the elevated urinary protein excretion, and this effect was significant at doses of 0.01 mg/kg or higher at week 8.
Effects of repeated administration of ASP7657 on urinary protein excretion in 5/6 nephrectomized (Nx) rats. ASP7657 and losartan were orally administered to 5/6 Nx rats once daily for 8 weeks. Values are mean ± SEM for 7–15 animals per group. *P < 0.05 vs. normal group, #P < 0.05 vs. vehicle group, $P < 0.05 vs. vehicle group
Losartan (10 mg/kg) also significantly improved urinary protein excretion, almost as effectively as high doses of ASP7657. 5/6 Nx rats exhibited significant increases in plasma levels of creatinine and BUN and decreases in Ccr (Fig. 2). ASP7657 and losartan significantly improved or showed a trend towards improving these parameters. In addition, 5/6 Nx rats exhibited a significant decrease in body weight and increase in urine volume, kidney weight, and SBP (Table 1). Losartan significantly reduced kidney weight and blood pressure. ASP7657 also significantly reduced kidney weight and slightly decreased blood pressure. However, this antihypertensive effect was not significant and was much weaker than that of losartan. Neither drug significantly affected body weight or urine volume (Table 1).
Effects of repeated administration of ASP7657 on a plasma creatinine, b blood urea nitrogen (BUN), and c creatinine clearance in 5/6 nephrectomized (Nx) rats. ASP7657 and losartan were orally administered to 5/6 Nx rats once daily for 8 weeks. Values are mean ± SEM for 7–15 animals per group. *P < 0.05 vs. normal group, $P < 0.05 vs. vehicle group
5/6 Nx rats exhibited significant glomerulosclerosis and tubulointestinal lesions (Fig. 3a–c). Renal tubules around the glomeruli were severely degenerated, and the tubular lumen was dilated. Marked infiltration of inflammatory cells was observed in the interstitium, and severe fibrosis was present. ASP7657 attenuated these pathological changes. In addition, ASP7657 dose-dependently and significantly reduced histopathological glomerulosclerosis and tubulointerstitial damage scores including fibrosis and inflammatory cell infiltration (Fig. 3d, e). Losartan also significantly attenuated these kidney injury parameters.
Improvement in renal injury by repeated administration of ASP7657 in 5/6 nephrectomized (Nx) rats. Representative light micrographs of renal tissues obtained from a normal, b vehicle-treated 5/6 Nx rats, and c ASP7657 (0.1 mg/kg)-treated 5/6 Nx rats. Top panels: periodic acid-Schiff (PAS) stain (magnification: × 200), bottom panels: hematoxylin and eosin (H&E) stain (magnification: × 100). Effects of ASP7657 on histopathological scores for d glomerulosclerosis and e tubulointerstitial damage. Values are mean ± SD for 7–15 animals per group. *P < 0.05 vs. normal group, #P < 0.05 vs. vehicle group, $P < 0.05 vs. vehicle group
Effect of ASP7657 on plasma renin activity in normal rats
Subcutaneous administration of the EP4 receptor-selective agonist ONO-4819 significantly increased the PRA as assessed by angiotensin I production (Fig. 4). ASP7657 (0.003–0.03 mg/kg) dose-dependently suppressed the increase in PRA and this effect was significant at doses of 0.01 mg/kg or higher.
Effect of ASP7657 on the EP4 receptor agonist-induced increase in plasma renin activity (PRA) in normal rats. ASP7657 (0.003–0.03 mg/kg) was orally administered to rats, and the EP4 receptor-selective agonist ONO-4819 (0.01 mg/kg) was subcutaneously injected 1 h post-dose. Blood samples were collected 10 min after the ONO-4819 injection. PRA was assessed by angiotensin I release. Values are mean ± SEM for 8 animals per group. *P < 0.05 vs. vehicle group, #P < 0.05 vs. ONO-4819-treated group
Effect of ASP7657 on renal hemodynamics in diabetic rats
Administration of streptozotocin induces various typical diabetic abnormalities, including hyperglycemia and complications such as albuminuria (Tahara et al. 2014). Diabetic rats exhibited a significant or trend towards a significant increase in Ccr (hyperfiltration) and RBF, and a significant decrease in RVR and MBP (Table 2). Intravenous administration of ASP7657 (0.1 mg/kg) attenuated hyperfiltration without affecting RBF, RVR, or MBP (Fig. 5).
Discussion
CKD is currently a serious problem in nephrology and its incidence is steadily increasing. Both experimental and clinical studies have shown that ACE inhibitors and ARBs are highly effective for halting the progression of CKD (Macconi 2010; Berl 2009). Therefore, these renin-angiotensin-aldosterone system (RAAS) blocking agents are currently accepted as the gold standard in therapies. However, current management strategies are insufficient to prevent the progression of CKD (Lambers Heerspink and de Zeeuw 2013). Therefore, identifying new add-on therapies to standard RAAS therapies remains a major challenge. In recent years, a large body of experimental evidence has suggested that PGE2 plays diverse and important roles in the regulation of renal function including glomerular hemodynamics and renin release via EP4 receptors. The PGE2-EP4 receptor pathway may therefore be a suitable target for the treatment of kidney disease including diabetic nephropathy and CKD. The present work was conducted to examine the protective effect of the EP4 receptor-selective antagonist ASP7657 on progressive renal dysfunction in 5/6 Nx CKD rats and to explore the possible mechanisms involved in its renoprotective effects.
The 5/6 Nx model is often used to study the mechanisms of CKD and potential therapeutic approaches to prevent the progression of CKD with renal mass reduction. In this model, systemic hypertension and proteinuria contribute to kidney injury as indicated by glomerulosclerosis and interstitial fibrosis, and to the expression of proinflammatory and profibrotic molecules by kidney cells (Helal et al. 2012). Renal damage in this CKD rat model is induced by hemodynamic changes associated with an increase in renin release, hyperfiltration in residual nephrons, and podocyte loss. In this study, proteinuria and impaired renal function, as estimated by a rise in plasma levels of creatinine and BUN and reduction in Ccr in 5/6 Nx rats, were progressively exacerbated. This was accompanied by hypertension, renal hypertrophy, and typical pathological changes such as proliferation of glomerular mesangial cells and accumulation of mesangial matrix, focal segmental glomerulosclerosis and glomerular tuft adhesion, tubular epithelial cell degeneration, atrophy, and interstitial fibrosis. These abnormalities were consistent with those reported in previous studies in rodent CKD models (Kondo et al. 2014) and are similar to those observed in CKD patients (Kliem et al. 1996). ASP7657 attenuated the increase in proteinuria, plasma creatinine and BUN levels, and improved impaired renal function. In addition, ASP7657 ameliorated renal hypertrophy, glomerulosclerosis, and tubulointerstitial injury including fibrosis. These renal pathological injury events are highly correlated with the progression of CKD and are regarded as the final common pathways towards end-stage renal disease (ESRD) (Hodgkins and Schnaper 2012; Fine and Norman 2008). Therefore, the renoprotective effect of ASP7657 could be associated with an improvement in histopathological changes and ASP7657 may suppress the progression of CKD towards ESRD. Moreover, losartan also exhibited significant renoprotective effects and had similar efficacy on proteinuria and renal injury to that of high doses of ASP7657. These renoprotective effects of losartan are consistent with the results of previous studies (Jian et al. 2013). These results suggest that ASP7657 may suppress the progression of chronic renal failure with a potency that is comparable to that of losartan.
In CKD rat models, subtotal nephrectomy leads to a compensatory hyperfiltration of the remaining nephrons to initially maintain overall renal function. This glomerular hyperfiltration leads to glomerular hypertension and subsequent glomerulosclerosis with progressive renal function decline (Fogo 2007). Therefore, renal hemodynamic abnormalities that result in glomerular hyperfiltration are likely to play a crucial role in the initiation and progression of CKD. While the mechanisms of glomerular hyperfiltration in CKD conditions are variable and not well established, vasodilation of afferent arterioles by several endogenous molecules such as atrial natriuretic peptide (ANP), nitric oxide, and PGE2 (Kikkawa et al. 1993; Sugimoto et al. 1998; Nasrallah et al. 2016) and/or vasoconstriction of efferent arterioles by RAAS (Nangaku and Fujita 2008) are implicated as contributing pathways. Indeed, ANP receptor antagonists and RAAS inhibitors attenuate glomerular hyperfiltration (Kikkawa et al. 1993; Helal et al. 2012). In particular, renal injury associated with glomerular hyperfiltration is known to be strongly correlated with activation of RAAS, which leads to maladaptive renal and systemic hemodynamic responses (Fogo 2007). Many animal experiments suggest that ACE inhibitors or ARBs attenuate the progression of renal injury by improving glomerular hyperfiltration. This suggests that the most effective intervention would be targeting glomerular hyperfiltration and RAAS. In addition, PGE2 reportedly induces vasodilatory actions on the afferent arteriole via EP4 receptors and is correlated with induction of glomerular hyperfiltration (Purdy and Arendshorst 2000; Tang et al. 2000). In the present study, ASP7657 attenuated hyperfiltration under diabetic conditions, suggesting that the renoprotective effect of ASP7657 in CKD rats may also be mediated by attenuation of glomerular hyperfiltration in remnant glomeruli. In addition, previous studies suggest that the PGE2-EP4 receptor pathway might be necessary for stimulation of renin release from juxtaglomerular cells (Friis et al. 2013) and activation of RAAS in kidneys (Pöschke et al. 2012). Indeed, we showed that ASP7657 suppressed the EP4 receptor agonist-induced increase in PRA, a finding that is consistent with those of previous studies (Schweda et al. 2004). Therefore, the renoprotective effects of ASP7657 may at least in part be mediated by inhibition of renal RAAS activation. However, given that we only investigated the acute effects of ASP7657 on typical parameters in normal and diabetic rats, additional studies are needed to examine the chronic effects of ASP7657 on more detailed parameters, including glomerular hyperfiltration and renal RAAS activation in CKD models, to confirm this pharmacologic mechanism. In addition, measurement of creatinine clearance is insufficient for investigating the direct effects of a drug on renal glomerular function. Therefore, additional studies including measurement of inulin clearance in CKD models are needed. We also showed that losartan markedly reduced high blood pressure while ASP7657 only slightly decreased blood pressure and to a lesser extent than losartan. Hypertension is a key independent risk factor for kidney diseases and accelerates the progression of CKD, and control of blood pressure using antihypertensive drugs containing RAAS blocking agents is effective in the treatment of CKD (Ravera et al. 2006). Therefore, the renoprotective effects of losartan may at least in part be mediated by its hypotensive actions. In contrast, ASP7657 exhibited renoprotective effects without potently reducing systemic blood pressure, suggesting that ASP7657 may have kidney-selective pharmacologic effects, such as on local renal RAAS, for CKD. However, we only measured blood pressure at one point (week 7) during the 8-week repeated administration period; therefore, multiple measurements of blood pressure are needed to confirm the pharmacologic effects of ASP7657 on systemic blood pressure in CKD models.
Recent studies have shown that podocyte-specific deletion of the EP4 receptor or EP4 receptor antagonists attenuate podocyte injury and improve renal function and pathological changes in 5/6 Nx animal models (Stitt-Cavanagh et al. 2010; Thieme et al. 2017). In addition, EP4 receptor agonists increase the production of proinflammatory cytokines, including tumor necrosis factor (TNF)-α and monocyte chemoattractant protein (MCP-1), and the profibrotic cytokine transforming growth factor (TGF)-β1, which play important roles in the pathogenesis of kidney injury including glomerulosclerosis and interstitial fibrosis (Mohamed et al. 2013). Therefore, EP4 receptor-selective antagonists may attenuate kidney injury through these mechanisms. In this study, we only investigated the effects of ASP7657 on the main parameters of renal function and pathophysiology. Therefore, additional detailed examinations and comparisons with other EP4 receptor antagonists, including ONO-AE3-208 (Thieme et al. 2017), as well as with existing drugs such as ACE inhibitors and ARBs in several CKD models are needed to confirm and expand these potentially important therapeutic and novel biological findings associated with the PGE2-EP4 receptor pathways in CKD.
In conclusion, the present findings suggest that PGE2 plays an important role in CKD via EP4 receptors, and that the EP4 receptor-selective antagonist ASP7657 suppresses the progression of chronic renal failure by improving glomerular hemodynamics resulting from amelioration of hyperfiltration and renin release. ASP7657 may be potentially useful in the treatment of CKD patients.
References
Berl T (2009) Review: renal protection by inhibition of the renin-angiotensin-aldosterone system. J Renin-Angiotensin-Aldosterone Syst 10:1–8
Fine LG, Norman JT (2008) Chronic hypoxia as a mechanism of progression of chronic kidney diseases: from hypothesis to novel therapeutics. Kidney Int 74:867–872
Fogo AB (2007) Mechanisms of progression of chronic kidney disease. Pediatr Nephrol 22:2011–2022
Friis UG, Madsen K, Stubbe J, Hansen PB, Svenningsen P, Bie P, Skøtt O, Jensen BL (2013) Regulation of renin secretion by renal juxtaglomerular cells. Pflugers Arch 465:25–37
Helal I, Fick-Brosnahan GM, Reed-Gitomer B, Schrier RW (2012) Glomerular hyperfiltration: definitions, mechanisms and clinical implications. Nat Rev Nephrol 21:293–300
Hodgkins KS, Schnaper HW (2012) Tubulointerstitial injury and the progression of chronic kidney disease. Pediatr Nephrol 27:901–909m
Jian DY, Chao YW, Ting CH, Huang SW, Chang CF, Juan CC, Chen JY (2013) Losartan ameliorates renal injury, hypertension, and adipocytokine imbalance in 5/6 nephrectomized rats. Eur J Pharmacol 709:85–92
Kasai K, Sato S, Suzuki K (2001) A novel prostaglandin E receptor subtype agonist, 0N0-4819, attenuates acute experimental liver injury in rats. Hepatol Res 21:252–260
Kikkawa R, Haneda M, Sakamoto K, Koya D, Shikano T, Nakanishi S, Matsuda Y, Shigeta Y (1993) Antagonist for atrial natriuretic peptide receptors ameliorates glomerular hyperfiltration in diabetic rats. Biochem Biophys Res Commun 193:700–705
Kliem V, Johnson RJ, Alpers CE, Yoshimura A, Couser WG, Koch KM, Floege J (1996) Mechanisms involved in the pathogenesis of tubulointerstitial fibrosis in 5/6-nephrectomized rats. Kidney Int 49:666–678
Kondo M, Tahara A, Hayashi K, Abe M, Inami H, Ishikawa T, Ito H, Tomura Y (2014) Renoprotective effects of novel interleukin-1 receptor-associated kinase 4 inhibitor AS2444697 through anti-inflammatory action in 5/6 nephrectomized rats. Naunyn Schmiedeberg's Arch Pharmacol 387:909–919
Lambers Heerspink HJ, de Zeeuw D (2013) Novel drugs and intervention strategies for the treatment of chronic kidney disease. Br J Clin Pharmacol 76:536–550
Lopez-Novoa JM, Martinez-Salgado C, Rodriguez-Pena AB, Lopez-Hernandez FJ (2010) Common pathophysiological mechanisms of chronic kidney disease: therapeutic perspectives. Pharmacol Ther 128:61–81
Macconi D (2010) Targeting the renin angiotensin system for remission/regression of chronic kidney disease. Histol Histopathol 25:655–668
Mizukami K, Kamada H, Yoshida H, Ishii I, Nozawa E, Wada K, Ugawa T (2018) Pharmacological properties of ASP7657, a novel, potent and selective prostaglandin EP4 receptor antagonist. Naunyn Schmiedeberg's Arch Pharmacol 391:1319–1326
Mohamed R, Jayakumar C, Ramesh G (2013) Chronic administration of EP4-selective agonist exacerbates albuminuria and fibrosis of the kidney in streptozotocin-induced diabetic mice through IL-6. Lab Investig 93:933–945
Nangaku M, Fujita T (2008) Activation of the renin-angiotensin system and chronic hypoxia of the kidney. Hypertens Res 31:175–184
Narumiya S, Sugimoto Y, Ushikubi F (1999) Prostanoid receptors: structures, properties, and functions. Physiol Rev 79:1193–1226
Nasrallah R, Hassouneh R, Hébert RL (2016) PGE2, kidney disease, and cardiovascular risk: beyond hypertension and diabetes. J Am Soc Nephrol 27:666–676
Pöschke A, Kern N, Maruyama T, Pavenstädt H, Narumiya S, Jensen BL, Nüsing RM (2012) The PGE2-EP4 receptor is necessary for stimulation of the renin-angiotensin-aldosterone system in response to low dietary salt intake in vivo. Am J Physiol Renal Physiol 503:F1435–F1442
Purdy KE, Arendshorst WJ (2000) EP1 and EP4 receptors mediate prostaglandin E2 actions in the microcirculation of rat kidney. Am J Physiol Renal Physiol 279:F755–F764
Ravera M, Re M, Deferrari L, Vettoretti S, Deferrari G (2006) Importance of blood pressure control in chronic kidney disease. J Am Soc Nephrol 17:S98–S103
Schweda F, Klar J, Narumiya S, Nüsing RM, Kurtz A (2004) Stimulation of renin release by prostaglandin E2 is mediated by EP2 and EP4 receptors in mouse kidneys. Am J Physiol Renal Physiol 287:F427–F433
Stitt-Cavanagh EM, Faour WH, Takami K, Carter A, Vanderhyden B, Guan Y, Schneider A, Breyer MD, Kennedy CR (2010) A maladaptive role for EP4 receptors in podocytes. J Am Soc Nephrol 21:1678–1690
Sugimoto H, Shikata K, Matsuda M, Kushiro M, Hayashi Y, Hiragushi K, Wada J, Makino H (1998) Increased expression of endothelial cell nitric oxide synthase (ecNOS) in afferent and glomerular endothelial cells is involved in glomerular hyperfiltration of diabetic nephropathy. Diabetologia 41:1426–1434
Tahara A, Kurosaki E, Yokono M, Yamajuku D, Kihara R, Hayashizaki Y, Takasu T, Imamura M, Li Q, Tomiyama H, Kobayashi Y, Noda A, Sasamata M, Shibasaki M (2014) Effects of sodium-glucose cotransporter 2 selective inhibitor ipragliflozin on hyperglycaemia, oxidative stress, inflammation and liver injury in streptozotocin-induced type 1 diabetic rats. J Pharm Pharmacol 66:975–987
Tang L, Loutzenhiser K, Loutzenhiser R (2000) Biphasic actions of prostaglandin E2 on the renal afferent arteriole: role of EP3 and EP4 receptors. Circ Res 86:663–670
Thieme K, Majumder S, Brijmohan AS, Batchu SN, Bowskill BB, Alghamdi TA, Advani SL, Kabir MG, Liu Y, Advani A (2017) EP4 inhibition attenuates the development of diabetic and non-diabetic experimental kidney disease. Sci Rep 7(3442):3442
Yokoyama U, Iwatsubo K, Umemura M, Fujita T, Ishikawa Y (2013) The prostanoid EP4 receptor and its signaling pathway. Pharmacol Rev 65:1010–1052
Acknowledgments
The authors thank Drs. Akiyoshi Shimaya, Yuichi Tomura, and Atsuo Tahara (Astellas Pharma Inc.) for their valuable comments and continuing encouragement.
Author information
Authors and Affiliations
Contributions
KM, HY, EN, KW, and TU conceived and designed the research. KM, HY, and TU performed experiments and analyzed the data. EN contributed to the synthesis of ASP7657. KM and KW wrote the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Animal studies were approved by the Institutional Animal Care and Use Committee of Astellas Pharma Inc., Tsukuba Research Center, which is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) International.
Conflict of interest
The authors have no conflict of interest other than being employees of Astellas Pharma Inc.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mizukami, K., Yoshida, H., Nozawa, E. et al. Renoprotective effects of the novel prostaglandin EP4 receptor-selective antagonist ASP7657 in 5/6 nephrectomized chronic kidney disease rats. Naunyn-Schmiedeberg's Arch Pharmacol 392, 451–459 (2019). https://doi.org/10.1007/s00210-018-01600-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-018-01600-3