Abstract
Antimuscarinics are the first-line choice of treatment for overactive bladder (OAB). Imidafenacin distributes in the bladder more selectively than in the submaxillary gland and colon, and hence, this drug is considered more useful for OAB than other antimuscarinics. However, the examination of imidafenacin selectivity to bladder over colon using in vivo models is limited. Thus, the author examined whether imidafenacin could induce more selective blockade of the bladder over colon in conscious rats using two pharmacological indices (colonic transit and neostigmine-induced fecal pellet output) and compared its bladder selectivity with propiverine. In the bladder study, the inhibitory doses of antimuscarinics were calculated using the area under the curve of the distension-induced rhythmic contraction in conscious rats. The relative bladder selectivity of imidafenacin to propiverine was 50-fold and 61-fold, respectively, in a dye marker colonic transit model and in a neostigmine-induced fecal pellet output model. This comparative study shows that the functional bladder selectivity of imidafenacin is higher than that of propiverine tested under the present conditions in conscious rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Muscarinic acetylcholine receptors consist of five subtypes (M1 to M5) and are widely expressed in the human body. In particular, M2 muscarinic acetylcholine receptors are predominantly expressed in the urinary bladder and gastrointestinal tract smooth muscle in humans, but M3 muscarinic acetylcholine receptors are expressed at only one third and one fourth of M2 muscarinic acetylcholine receptors in the bladder and the gastrointestinal tract, respectively (Abrams et al. 2006). M3 muscarinic acetylcholine receptors play an obligatory role in detrusor contractile activity in the bladder (Hegde 2006) and a modulatory role in gastrointestinal motility (Eglen et al. 2001; Kondo et al. 2011).
In the bladder, acetylcholine released from the urothelium in response to stretch (Yoshida et al. 2006; Hanna-Mitchell et al. 2007) can act to stimulate urothelial M1 to M5 muscarinic acetylcholine receptors in an autocrine or paracrine manner (Bschleipfer et al. 2007). Out of these subreceptors, Moro et al. (2011) showed endogenous acetylcholine is released from the urothelium through M3 muscarinic acetylcholine receptors, leading to spontaneous bladder contractile activation. Although understanding of the physiological roles of M2 muscarinic acetylcholine receptors in the bladder is still limited, receptor activation suppressed high-conductance Ca2+-activated K+ channels in rat bladder (Nakamura et al. 2002). This effect would be expected to enhance M3 muscarinic acetylcholine receptor-mediated contractions. Indeed, M2 muscarinic acetylcholine receptor activation enhances M3 receptor-mediated bladder contraction in mice through indirect mechanisms (Ehlert et al. 2005): M2-M3 muscarinic acetylcholine receptor interaction is expected to exhibit an M3 profile for pharmacological antagonism because of the conditional nature of the M2 mechanism. A similar process was also demonstrated in the colon (Sawyer and Ehlert 1998). In addition, it has been recently reported that M2 muscarinic acetylcholine receptors regulate the production of prostaglandin E2 in the bladder wall (Nile and Gillespie 2012) and activation of M2 and M3 muscarinic acetylcholine receptors may stimulate the release of ATP through the increase of intracellular Ca2+ (Kullmann et al. 2008; Sui et al. 2014). Nevertheless, the importance of M3 muscarinic acetylcholine receptors in bladder contractions is clear.
Thus, antimuscarinics, which are relatively selective for M3 muscarinic acetylcholine receptors, have been developed for the first-line pharmacotherapy for overactive bladder (OAB), a highly prevalent disorder characterized as a syndrome consisting of urgency with or without urge incontinence and usually together with frequency and nocturia (Abrams et al. 2003). In fact, however, most antimuscarinics act on mainly M3 muscarinic acetylcholine receptors throughout the body and therefore cause a wide variety of adverse effects such as dry mouth, constipation, and blurred vision (Abrams and Andersson 2007; Chapple 2000; Meek et al. 2011). To avoid these adverse effects, a β3 adrenergic receptor agonist, as a new category of drugs, has been recently approved for the treatment of OAB (Andersson et al. 2013). Even so, these antimuscarinics are still the drug of choice and useful for the treatment of OAB because of their high efficacy in preventing pollakisuria.
Dry mouth and constipation are well-known and common adverse effects of antimuscarinics and are major causes of their treatment discontinuation (Abrams and Andersson 2007). In this connection, we reported that imidafenacin, an antimuscarinic, exhibits a higher selectivity in anticontractile activity to the bladder over the proximal colon than some other antimuscarinics tested in urethane-anesthetized rats (Yamazaki et al. 2011). Except for this previous study, however, the bladder selectivity of imidafenacin has not been studied sufficiently.
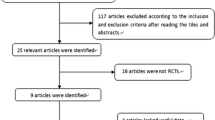
In the present study, the author used two colonic models of conscious rats to study more about the bladder selectivity of imidafenacin by using propiverine, an antimuscarinic for OAB, as a comparative drug. Specifically, one model is to determine the inhibitory effects on colonic transit and the other is to determine the inhibitory effects on the neostigmine-induced fecal pellet output. Then, the inhibitory doses of the two antimuscarinics in each colonic model were compared with the inhibitory doses in the distension-induced rhythmic contraction of the urinary bladder.
Materials and methods
Animals
Male Spradue Dawley rats (Charles River Laboratories Japan, Kanagawa, Japan), weighing 230–426 g, were housed in rooms maintained under controlled conditions: 23 ± 3 °C, 55 ± 15 % relative humidity, and 12–12-h light-dark cycle. The rats were maintained on a solid diet daily with water ad libitum. All animal care/experiments and the study protocol complied with the guidelines of the Committee for the Purpose of Control and Supervision of Experiments on Animals and were approved, prior to the study, by the Institutional Animal Ethics Committee at Kyorin Pharmaceutical Co., Ltd. Our facility is certified as an animal testing research institute by the Japan Health Sciences Foundation, established under the jurisdiction of the Japanese Ministry of Health, Labor and Welfare.
Distension-induced rhythmic contraction in the urinary bladder
Distension-induced rhythmic contractions were measured and analyzed with a modification of the procedures (Kobayashi et al. 2007). Rats anesthetized with 2–4 % isoflurane underwent bladder and stomach surgery. A balloon (about 1 cm in diameter) connected with a polyethylene tube (Hibiki size 5, Japan) was inserted via an incision at the bladder dome into the bladder and ligated at the bladder dome. A polyethylene tube (Hibiki size 5, Japan) for drug administration was inserted through a gastric incision into the stomach. After skin incisions were sutured, the rats were placed in Bollman cages. The other end of the balloon tube was connected to a pressure measurement amplifier (Nihon Kohden, Tokyo, Japan) through a three-way stopcock for measuring bladder rhythmic contractions of the rats in a conscious condition. Thereafter, about 50 μL of distilled water was injected into the balloon through the three-way stopcock and bladder rhythmic contractions were recorded at least for 2 h before dosing. Antimuscarinics or vehicle was dosed through a polyethylene tube inserted into the stomach. Dosing volumes were set at 2 mL/kg. Resultant changes in the bladder pressure after dosing were recorded for 2 h through the bladder tube.
The amplitudes of rhythmic bladder contractions were measured and averaged for each of every 10 min for 30 min before dosing and for each of every 10 min for 2 h after dosing. Specifically, the inhibitory effects on the amplitudes of rhythmic bladder contractions were compared, using the averaged amplitude of 10-min contractions among −30, −20, and −10 min before dosing. To apply to comparison with colonic data, we calculated the relative area under the contractions for the inhibitory effect on the rhythmic bladder contractions for 2 h after dosing in comparison with the control area under contractions for 2 h before dosing. Recording and analysis of rhythmic bladder contractions were made with LabChart version 7.3.7 of PowerLab systems (ADI Instruments, Nagoya, Japan).
Measurements of dye marker colonic transit in conscious rats
The colonic transit of a dye marker was analyzed with a modification of the procedures (Kishibayashi and Karasawa 1995). Rats anesthetized with pentobarbital (50 mg/kg, subcutaneously) underwent abdominal surgery. A polyethylene tube (PE50; Japan Becton Dickinson, Tokyo, Japan) was placed in the colon via the cecum at 1 cm distal to the cecocolic junction and fixed with sutures to the gut wall. The tube was tunneled through the abdominal wall subcutaneously and finally exited from the skin at the nape of the neck. After the midline incision was sutured, the rats were left to recover with warm light in individually separate cages. Six to 10 days later, test drugs were given orally to the rats. At 0.5 h after oral drug dosing, 1 % Evans blue suspended in 0.2 % agar-distilled water solution was carefully injected via the implanted polyethylene tube into the proximal colon at a volume of 0.25 mL/rat. Then, 1.5 h later (at 2 h after oral drug dosing), the rats were euthanized by intravenous injection of excess pentobarbital, and the colon was removed immediately. The length which the dye marker traveled in the colon was measured and is expressed as a percentage of the total length of the colon.
Measurements of neostigmine-induced fecal pellet output in conscious rats
Rats were acclimated in cages for 1–3 days before experiment. On the day of the experiment, test drugs were given orally to rats, and 0.5 h later, neostigmine (0.1 mg/kg) was injected subcutaneously. The number of fecal pellets excreted for the subsequent 1.5 h (at 2 h after oral drug dosing) was counted.
Data analysis and statistics
The 50 % inhibition doses (defined as ED50s) against dye marker colonic transit, neostigmine-induced fecal pellet count, amplitude of rhythmic bladder contraction, and area under the bladder contractions were determined by non-linear regression analysis, using GraphPad Prism version 6.01 for Windows (GraphPad Software, San Diego, USA). Each control value was defined as one hundredth of the minimum dose, for use in all analyses, of either antimuscarinic. In the amplitude of rhythmic bladder contraction analysis, the maximum inhibition value in post-dose contraction amplitude was adopted as analysis data at each dose.
All data are expressed as mean ± standard error (SE) of the mean. The statistical differences of effects were analyzed between drug and vehicle groups, using Dunnett’s multiple comparison test. Students’ t test was used to determine the statistical significance between dose ratio of propiverine and imidafenacin. Probability values of 0.05 or less were considered statistically significant.
Drugs
Propiverine hydrochloride (propiverine) and imidafenacin were synthesized in our laboratories. Atropine sulfate (atropine) and neostigmine bromide (neostigmine) were obtained from Sigma-Aldrich Co. (St. Louis, MO, USA). Imidafenacin was suspended in 0.3 % carboxymethylcellulose sodium solution and diluted with 0.3 % carboxymethylcellulose sodium solution. Other drugs were dissolved in distilled water. The solutions were diluted with distilled water except for imidafenacin suspension solution.
Results
Effects of propiverine and imidafenacin on rhythmic bladder contraction in conscious rats
Propiverine and imidafenacin effectively inhibited the amplitude of rhythmic bladder contractions in a dose-dependent manner (Fig. 1a, b). The ED50s of propiverine and imidafenacin over rhythmic bladder contraction amplitude were 11 and 0.15 mg/kg, respectively (Table 1). These data were close to their half-inhibitory doses (ID30; propiverine 15 mg/kg and imidafenacin 0.17 mg/kg) of the distension-induced rhythmic bladder contraction amplitudes (Kobayashi et al. 2007). For comparison with post-dose 2-h colonic data, we used the inhibitory ratio of the area under the contractions of the bladder for 2 h after oral treatment with each antimuscarinic. Based on the area under the contraction analyses, propiverine and imidafenacin inhibited the area under the rhythmic bladder contractions in a dose-dependent manner, with the ED50s of 15 and 0.15 mg/kg, respectively (Fig. 1c, d; Table 1).
Dose-response relation of propiverine and imidafenacin on distension-induced rhythmic bladder contractions in conscious rats. Propiverine (a, c) and imidafenacin (b, d) at each dose were given intragastrically. a, b Averaged maximum change value of rhythmic bladder contraction amplitudes at each dose was plotted. c, d Area under the rhythmic bladder contractions for 2 h after each dose was calculated. Each symbol and vertical bar represents the mean ± SE of the data from six rats. Each line means the result of non-linear regression analysis. **P < 0.01 and ***P < 0.001 vs. control (Dunnett’s test for multiple comparison)
Effects of propiverine and imidafenacin on colonic transit in conscious rats
Propiverine and imidafenacin inhibited the length of dye marker colonic transit in a dose-dependent manner, with the ED50s of 34 and 17 mg/kg, respectively (Fig. 2 and Table 2). In contrast, there were no significant differences in dye marker colonic transit length between two control groups (53.8 ± 3.6 and 59.1 ± 2.1 %) independently obtained for propiverine and imidafenacin. At the maximum effective doses (60 and 100 mg/kg, respectively), propiverine and imidafenacin inhibited the control colonic transit by 39.4 ± 4.5 and 44.4 ± 8.8 %, respectively.
Dose-response relation of propiverine and imidafenacin on dye marker colonic transit in conscious rats. Propiverine (a) and imidafenacin (b) at each dose were given orally. Colonic transit (%) was measured as individual transit lengths of a dye marker. Each symbol and vertical bar represents the mean ± SE of the data from eight rats. Each line means the result of non-linear regression analysis. **P < 0.01 vs. control (Dunnett’s test for multiple comparison)
Effects of propiverine and imidafenacin on neostigmine-induced fecal pellet output in conscious rats
It has been shown that neostigmine increases fecal output in rats in a dose-dependent manner (Campbell-Dittmeyer et al. 2009). Thus, we examined effects of the test compounds on neostigmine-induced fecal output in conscious rats. Propiverine and imidafenacin inhibited neostigmine-induced fecal pellet output in a dose-dependent manner, with the ED50s of 23 and 14 mg/kg, respectively (Fig. 3 and Table 2). In contrast, there were no significant differences in the number of fecal pellets between two independent control groups (average values of the control group for propiverine and imidafenacin were 8.1 ± 0.8 and 7.3 ± 0.8, respectively). At the maximum doses (100 and 100 mg/kg, respectively), propiverine and imidafenacin inhibited the control fecal pellet output by 79.0 ± 8.0 and 76.7 ± 8.4 %, respectively.
Dose-response relation of propiverine and imidafenacin on neostigmine-induced fecal pellet output in conscious rats. Propiverine (a) and imidafenacin (b) at each dose were given orally. Each symbol and vertical bar represents the mean ± SE of the data from ten rats. Each line means the result of non-linear regression analysis. *P < 0.05 and ***P < 0.001 vs. control (Dunnett’s test for multiple comparison)
Comparative bladder selectivity of propiverine and imidafenacin over the colon in conscious rats
Using the ED50 values shown in Tables 1 and 2, the bladder selectivity of imidafenacin over the colon was calculated to be 50-fold higher than that of propiverine in the dye marker colonic transit model (Table 2). In addition, the bladder selectivity of imidafenacin over the colon was calculated to be 61-fold higher than that of propiverine in the neostigmine-induced fecal pellet output model (Table 2).
Effects of atropine on two colonic models in conscious rats
To examine the effects of the prototype antimuscarinics on the colon, we used atropine. Atropine inhibited dye marker colonic transit in a dose-dependent manner, with the ED50 of 30 mg/kg (95 % confidence interval, 13–69 mg/kg) (Fig. 4), and the maximum inhibitory effect was 44.3 ± 7.9 % at a dose of 300 mg/kg. Atropine inhibited the neostigmine-induced fecal pellet output in a dose-dependent manner and, at the maximum dose of 30 mg/kg, inhibited the control fecal pellet output by 91.9 ± 8.1 % (Fig. 4), with the ED50 of 3.8 mg/kg (95 % confidence interval, 1.9–7.8 mg/kg). The maximum inhibitory effects of atropine, imidafenacin, and propiverine found in this dye marker colonic transit model of rats were approximately 40–50 % even when their relatively high doses were given orally. In particular, the inhibitory effects of atropine and propiverine were saturated at a dose of 300 and 120 mg/kg (Figs. 2 and 4), respectively, and remained at about 50 % or lower levels.
Dose-response relation of atropine on dye marker colonic transit and on neostigmine-induced fecal pellet output in conscious rats. Atropine at each dose was given orally. a Colonic transit (%) is the mean of individual transit lengths of a dye marker. b Fecal pellet output was induced by neostigmine. Each symbol and vertical bar represents the mean ± SE of the data from six to eight rats. Each line means the result of non-linear regression analysis. *P < 0.05, **P < 0.01, and ***P < 0.001 vs. control (Dunnett’s test for multiple comparison)
Discussion
In this study, to examine the relative bladder selectivity of propiverine and imidafenacin, the author measured colonic transit and neostigmine-induced fecal pellet output from 0.5 to 2 h after oral dosing of propiverine and imidafenacin. The rationale for selection of this evaluation timing in propiverine is based on available literature. Specifically, the known Tmax of propiverine given to rats was ≤1 h in a dose range of 24.8–248 μmol/kg (Yamada et al. 2010), after oral treatment. On the other hand, the Tmax of imidafenacin was 0.25–1 h in rats when imidafenacin at 6–30 mg/kg was orally given (unpublished data). These Tmax data support the evaluation timing and are well compatible with the pharmacological findings in the present study, in which, in distension-induced rhythmic contractions of rat urinary bladder, the peak inhibitory effects of propiverine and imidafenacin given intragastrically appeared at 0.5–0.7 h after dosing. In addition, these effects were substantially noted for 2 h after dosing. Furthermore, ED50s (11 and 0.15 mg/kg, respectively; Table 1) of propiverine and imidafenacin on the maximum change in rhythmic contraction amplitudes were close to the ED50s (15 and 0.15 mg/kg, respectively; Table 1) of them on the area under the contractions for 2 h. Therefore, the timing of our measurements in our colonic test after dosing is close to the Tmax of each antimuscarinic, and thus, the effective time duration of either antimuscarinic is considered being at least 2 h. Nevertheless, the author cannot exclude another possibility that the bladder selectivity of imidafenacin is caused by different plasma concentrations between propiverine and imidafenacin during experiments.
Here, the author showed that the functional bladder selectivity of imidafenacin is higher than propiverine in conscious rats under the present conditions. Specifically, the relative bladder selectivity of imidafenacin, when compared to propiverine in terms of relative dose ratio (mg/kg basis), was 50-fold in a dye marker colonic transit model and 61-fold in a neostigmine-induced fecal pellet output model. Thus, imidafenacin is selective for the bladder over colon. Using rhythmical contractions of the proximal colon in rats, we previously showed that imidafenacin has high bladder selectivity over the colon (Yamazaki et al. 2011). The present study using two in vivo models also provides evidence that imidafenacin is functionally more selective to the bladder over colon, and this strongly supports the previous study (Yamazaki et al. 2011). One possible interpretation about this selectivity is that imidafenacin may have the ability to bind selectively to bladder muscarinic acetylcholine receptors, thereby resulting in direct blockade of these receptors by imidafenacin excreted in the bladder, although there is still room for elucidating precisely more about the detailed mechanisms involved in this bladder selectivity. Muscarinic acetylcholine receptors have been identified in the urothelium and structures in the suburothelium (Bschleipfer et al. 2007; Chess-Williams 2002; Tyagi et al. 2006). All five muscarinic acetylcholine receptors (M1 to M5 subtypes) are expressed in urothelial cells from rats (Kullmann et al. 2008) and in the urothelium of the human bladder (Bschleipfer et al. 2007). Intravesical instillation of tolterodine, oxybutynin, and trospium suppressed carbachol-induced detrusor muscle contractions in rats (Kim et al. 2005). Yamada et al. (2011) showed that when orally given, imidafenacin distributed in the rat bladder much more selectively than in the submaxillary gland and colon; that when orally given at 1.57 μmol/kg, approximately 200 nM of imidafenacin was excreted in urine of rats; and that when instilled intravesically at concentrations of 30 to 3000 nM, imidafenacin bound to bladder muscarinic acetylcholine receptors. Indeed, since the ED50 of imidafenacin in the present bladder study is 0.5 μmol/kg, we interpret this suggests that imidafenacin (the unchanged form) excreted in urine is interacting with muscarinic acetylcholine receptors on the urothelial cells. As in agreement with these observations, the present study showed that the relative effective dose levels of imidafenacin were quite different from propiverine in the bladder (Fig. 1; 60–1200-fold), whereas their pharmacologically effective doses are not so different or similar to each other in the colon (colonic transit, 1.2- to 5-fold different; fecal pellet output, 1-fold different). In addition, Kim et al. (2006) reported that while intravesical injection of human urine from volunteers who took orally trospium prevented the carbachol-induced reduction in bladder capacity and shortening of intercontraction intervals in a rat OAB model, intravesical injection of human urine from volunteers who took orally oxybutynin or tolterodine was unable to inhibit the carbachol-induced detrusor overactivity. Approximately 7.8 % of an imidafenacin dose is excreted into the urine in healthy volunteers (Ohno et al. 2007), and this urinary excretion rate is higher than that of trospium, darifenacin, oxybutynin, and propiverine (Mansfield 2010; Kugimiya et al. 1990). Taken together, it is possible that the preferable distribution of imidafenacin into the bladder explains the higher bladder selectivity, and if this is the case, such selectivity is probably a big advantage for the treatment of OAB.
In this study, half of the measured colonic transit response was resistant to the antimuscarinics employed, including atropine. Similarly, atropine-independent contraction components and propulsion have been detected in the mid and distal areas of the colon (Hata et al. 1990; Gonzalez and Sarna 2001). Moreover, half-inhibitory doses of the antimuscarinics against distension-induced rhythmic bladder contraction in this study were close to their ID30s by linear regression analysis reported in a study (Kobayashi et al. 2007) in which the contraction also had resistant components to even higher doses of antimuscarinics. In contrast, the neostigmine-induced fecal pellet output in conscious rats was more sensitive to antimuscarinics in the present study, suggesting that endogenous acetylcholine, which is increased by treatment with neostigmine, is involved in the mechanism of this fecal pellet output as reported (Kirkpatrick and Rooney 1982). Moreover, these results imply that each of propiverine and imidafenacin at the maximum dose used this time is enough to block muscarinic acetylcholine receptors activated by endogenous acetylcholine (Fig. 3). It has been known that non-cholinergic systems are a component of the excitatory innervations of both rat colon and bladder. Tachykinin and 5-hydroxytryptamine (5HT), for example, produce longitudinal muscle contractions in rat distal colon (Grider 2003; Ono et al. 2005). There have been such responses in which bladder or its tissue shows to adenosine 5′-triphosphate in guinea pigs (Kennedy et al. 2007), tachykinin in rat bladder detrusor muscle (Meini and Maggi 1994), and 5HT in rabbit low urinary tract (Chen 1990). Furthermore, an unknown transmitter from urothelium/lamina propria by electrical field stimulation induces non-cholinergic contractions in pig bladder (Moro and Chess-Williams 2012).
In the detrusor contractile activity, M3 muscarinic acetylcholine receptors play an obligatory role in the bladder (Hegde 2006). Bladder motility is evaluated by measuring intravesical pressure (as a measure of spontaneous detrusor contraction) and would be affected mainly via M3 muscarinic acetylcholine receptor-related bladder excitability. The in vivo colonic motor activity (motility) in rats is characterized by rhythmic contraction, tone, and giant migrating contractions, which are all associated with uninterrupted migration over long distances, mass movement, and defecation in the living body (Gonzalez et al. 2001). Muscarinic receptors, especially the M3 subtype, have an important role in colonic propulsion in MR-KO mice (Kondo et al. 2011). Thus, a combination of all these colon contractions leads to colonic propulsion in vivo. In this study, therefore, colonic motility was evaluated by measuring dye marker colonic transit and neostigmine-induced fecal pellet output (as a measure of colonic propulsion). The colonic propulsion and the bladder contraction are somewhat different in motility quality, and some limitation may remain in comparing data between the colon and bladder. Nevertheless, we think that this type of comparative evaluation of bladder selectivity is pharmacologically useful because the inhibition of colonic propulsion is linked with constipation, a major adverse event of antimuscarinics.
Further studies will be needed to elucidate more detailed mechanisms of bladder selectivity over other smooth muscle organs related to antimuscarinic adverse reactions.
Conclusion
The author has shown imidafenacin-induced selective inhibition of distension-induced bladder contraction over both of the colonic transit and neostigmine-induced fecal pellet output in conscious rats. The relative bladder selectivity of imidafenacin to propiverine was 50-fold and 61-fold, respectively, in a dye marker colonic transit model and in a neostigmine-induced fecal pellet output model. In conclusion, this study indicates that the functional bladder selectivity of imidafenacin is higher than that of propiverine in conscious rats under the present conditions employed.
References
Abrams P, Andersson KE (2007) Muscarinic receptor antagonists for overactive bladder. BJU Int 100:987–1006
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A (2003) The standardisation of terminology in lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Urology 61:37–49
Abrams P, Andersson KE, Buccafusco JJ, Chapple C, de Groat WC, Fryer AD, Kay G, Laties A, Nathanson NM, Pasricha PJ, Wein AJ (2006) Muscarinic receptors: their distribution and function in body systems, and the implications for treating overactive bladder. Br J Pharmacol 148:565–578
Andersson KE, Martin N, Nitti V (2013) Selective β3-adrenoceptor agonists in the treatment of the overactive bladder. J Urol 190:1173–1180
Bschleipfer T, Schukowski K, Weidner W, Grando SA, Schwantes U, Kummer W, Lips KS (2007) Expression and distribution of cholinergic receptors in the human urothelium. Life Sci 80:2303–2307
Campbell-Dittmeyer K, Hicks GA, Earnest DL, Greenwood-Van Meerveld B (2009) Increased colonic transit in rats produced by a combination of a cholinesterase inhibitor with a 5-HT4 receptor agonist. Neurogastroenterol Motil 21:1197-e108
Chapple CR (2000) Muscarinic receptor antagonists in the treatment of overactive bladder. Urology 55(suppl):33–46
Chen HI (1990) Evidence for the presynaptic action of 5-hydroxytryptamine and the involvement of purinergic innervation in the rabbit lower urinary tract. Br J Pharmacol 101:212–216
Chess-Williams Z (2002) Muscarinic receptors of the urinary bladder: detrusor, urothelial and prejunctional. Auton Autacoid Pharmacol 22:133–145
Eglen RM, Choppin A, Watson N (2001) Therapeutic opportunities from muscarinic receptor research. Trends Pharmacol Sci 22:409–414
Ehlert FJ, Griffin MT, Abe DM, Vo TH, Taketo MM, Manabe T, Matsui M (2005) The M2 muscarinic receptor mediates contraction through indirect mechanisms in mouse urinary bladder. J Pharmacol Exp Ther 313:368–378
Gonzalez A, Sarna SK (2001) Neural regulation of in vitro giant contractions in the rat colon. Am J Physiol Gastrointest Liver Physiol 281:G275–G282
Grider JR (2003) Reciprocal activity of longitudinal and circular muscle during intestinal peristaltic reflex. Am J Physiol Gastrointest Liver Physiol 284:G768–G775
Hanna-Mitchell AT, Beckel JM, Barbadora S, Kanai AJ, de Groat WC, Birder LA (2007) Non-neuronal acetylcholine and urinary bladder urothelium. Life Sci 80:2298–2302
Hata F, Kataoka T, Takeuchi T, Yagasaki O, Yamano N (1990) Differences in control of descending inhibition in the proximal and distal regions of rat colon. Br J Pharmacol 101:1011–1015
Hegde SS (2006) Muscarinic receptors in the bladder: from basic research to therapeutics. Br J Pharmacol 147:S80–S87
Kennedy C, Tasker PN, Gallacher G, Westfall TD (2007) Identification of atropine- and P2X1 receptor antagonist-resistant, neurogenic contractions of the urinary bladder. J Neurosci 27:845–851
Kim Y, Yoshimura N, Masuda H, de Miguel F, Chancellor MB (2005) Antimuscarinic agents exhibit local inhibitory effects on muscarinic receptors in bladder-afferent pathways. Urology 65:238–242
Kim Y, Yoshimura N, Masuda H, De Miguel F, Chancellor MB (2006) Intravesical instillation of human urine after oral administration of trospium, tolterodine and oxybutynin in a rat model of detrusor overactivity. BJU Int 97:400–403
Kirkpatrick CT, Rooney PJ (1982) Contractures produced by carbamate anticholinesterases in bovine tracheal smooth muscle. Clin Exp Pharmacol Physiol 9:603–611
Kishibayashi N, Karasawa A (1995) Stimulating effects of KW-5092, a novel gastroprokinetic agent, on the gastric emptying, small intestinal propulsion and colonic propulsion in rats. Jpn J Pharmacol 67:45–50
Kobayashi F, Yageta Y, Yamazaki T, Wakabayashi E, Inoue M, Segawa M, Matsuzawa S (2007) Pharmacological effects of imidafenacin (KRP-197/ONO-8025), a new bladder selective anti-cholinergic agent, in rats. Comparison of effects on urinary bladder capacity and contraction, salivary secretion and performance in the Morris water maze task. Arzneim Forsch 57:147–154
Kondo T, Nakajima M, Teraoka H, Unno T, Komori S, Yamada M, Kitazawa T (2011) Muscarinic receptor subtypes involved in regulation of colonic motility in mice: functional studies using muscarinic receptor-deficient mice. Eur J Pharmacol 670:236–243
Kugimiya T, Hanaoka K, Inada Y, Yamamoto Y, Marunaka T, Kawaguchi Y (1990) Phase I study of propiverine hydrochloride—the 1st report: single oral dosing study. Jpn J Clin Pharmacol Ther 21:555–565
Kullmann FA, Artim D, Beckel J, Barrick S, de Groat WC, Birder LA (2008) Heterogeneity of muscarinic receptor-mediated Ca2+ responses in cultured urothelial cells from rat. Am J Physiol Renal Physiol 294:F971–F981
Mansfield KJ (2010) Muscarinic receptor antagonists, the overactive bladder and efficacy against urinary urgency. Clin Med Insights Ther 2:471–480
Meek PD, Evang SD, Tadrous M, Roux-Lirange D, Triller DM, Gumustop B (2011) Overactive bladder drugs and constipation: a meta-analysis of randomized, placebo-controlled trials. Dig Dis Sci 56:7–18
Meini S, Maggi CA (1994) Evidence for a capsaicin-sensitive, tachykinin-mediated, component in the NANC contraction of the rat urinary bladder to nerve stimulation. Br J Pharmacol 112:1123–1131
Moro C, Chess-Williams R (2012) Non-adrenergic, non-cholinergic, non-purinergic contractions of the urothelium/lamina propria of the pig bladder. Auton Autacoid Pharmacol 32:53–59
Moro C, Uchiyama J, Chess-Williams R (2011) Urothelial/lamina propria spontaneous activity and the role of M3 muscarinic receptors in mediating rate responses to stretch and carbachol. Urology 78:1442.e9-e15
Nakamura T, Kimura J, Yamaguchi O (2002) Muscarinic M2 receptors inhibit Ca2+-activated K+ channels in rat bladder smooth muscle. Int J Urol 9:689–696
Nile CJ, Gillespie JI (2012) Interactions between cholinergic and prostaglandin signaling elements in the urothelium: role for muscarinic type 2 receptors. Urology 79:240.e17-e23
Ohno T, Nakade S, Nakayama K, Kitagawa J, Ueda S, Miyabe H, Masuda Y, Miyata Y (2007) Absolute bioavailability of imidafenacin after oral administration to healthy subjects. Br J Clin Pharmacol 65:197–202
Ono S, Mitsui R, Karaki S, Kuwahara A (2005) Muscarinic and 5-HT4 receptors participate in the regulation of the frequency of spontaneous contractions of the longitudinal muscle in rat distal colon. Biomed Res 26:173–177
Sawyer GW, Ehlert FJ (1998) Contractile roles of the M2 and M3 muscarinic receptors in the guinea pig colon. J Pharmacol Exp Ther 284:269–277
Sui G, Fry CH, Montgomery B, Roberts M, Wu R, Wu C (2014) Purinergic and muscarinic modulation of ATP release from the urothelium and its paracrine actions. Am J Physiol Renal Physiol 306:F286–F298
Tyagi S, Tyagi P, Van-le S, Yoshimura N, Chancellor MB, de Miguel F (2006) Qualitative and quantitative expression profile of muscarinic receptors in human urothelium and detrusor. J Urol 176:1673–1678
Yamada S, Ito Y, Taki Y, Seki M, Nanri M, Yamashita F, Morishita K, Komoto I, Yoshida K (2010) The N-oxide metabolite contributes to bladder selectivity resulting from oral propiverine: muscarinic receptor binding and pharmacokinetics. Drug Metab Dispos 38:1314–1321
Yamada S, Seki M, Ogoda M, Fukata A, Nakamura M, Ito Y (2011) Selective binding of bladder muscarinic receptors in relation to the pharmacokinetics of a novel antimuscarinic agent, imidafenacin, to treat overactive bladder. J Pharmacol Exp Ther 336:365–371
Yamazaki T, Muraki Y, Anraku T (2011) In vivo bladder selectivity of imidafenacin, a novel antimuscarinic agent, assessed by using an effectiveness index for bladder capacity in rats. Naunyn-Schmiedeberg’s Arch Pharmacol 384:319–329
Yoshida M, Inadome A, Maeda Y, Satoji Y, Masunaga K, Sugiyama Y, Murakami S (2006) Non-neuronal cholinergic system in human bladder urothelium. Urology 67:425–430
Acknowledgments
The author thanks Mr. Fumiyoshi Kobayashi, Mr. Kunio Someya, Mr. Takanobu Yamazaki, Mr. Tsuyoshi Anraku, and Mr. Tokutarou Yasue (Kyorin Pharmaceutical Co., Ltd.) for their helpful comments and advice.
Conflict of interest
The author declares that he has no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muraki, Y. Comparative functional selectivity of imidafenacin and propiverine, antimuscarinic agents, for the urinary bladder over colon in conscious rats. Naunyn-Schmiedeberg's Arch Pharmacol 388, 1171–1178 (2015). https://doi.org/10.1007/s00210-015-1155-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-015-1155-9