Abstract
Fullerene whiskers (FLW)s are thin rod-like structures composed of C60 and C70 fullerene (FL). The shape of FLWs suggests potential toxic effects including carcinogenicity to the lung and pleura, similar to effects elicited by asbestos and multi-walled carbon nanotubes (MWCNT)s. However, no long-term carcinogenic studies of FL or FLW have been conducted. In the present study we investigated the pulmonary and pleural carcinogenicity of FL and FLW. Twelve-week-old male F344 rats were administered 0.25 or 0.5 mg FL, FLW, MWCNT-7, and MWCNT-N by intra-tracheal intra-pulmonary spraying (TIPS). Acute lung lesions and carcinogenicity were analyzed at 1 and 104 weeks after 8 doses/15 days TIPS administration. At week 1, FLW, MWCNT-7, and MWCNT-N significantly increased alveolar macrophage infiltration. Expression of Ccl2 and Ccl3, reactive oxygen species production, and cell proliferation were significantly increased by administration of MWCNT-7 and MWCNT-N but not FL or FLW. At week 104, the incidence of bronchiolo-alveolar adenoma plus adenocarcinoma was significantly increased in the MWCNT-7 and MWCNT-N groups, and the incidence of mesothelioma was significantly increased in the MWCNT-7 group. No significant induction of pulmonary or pleural tumorigenesis was observed in the FL or FLW groups. The number of 8-OHdG-positive cells in the alveolar epithelium was significantly increased in the MWCNT-7 and MWCNT-N groups but not in the FL or FLW groups. FL and FLW did not exert pulmonary or pleural carcinogenicity in our study. In addition, oxidative DNA damage was implicated in MWCNT-induced lung carcinogenesis, suggesting that it may be a useful initial marker of carcinogenicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fullerenes (FL), an allotrope of carbon, are stable aggregates of carbon atoms in the form of a truncated icosahedron and classified as nanomaterials (NM) (Hirsch 2010; Johnston et al. 2010; Kuganathan et al. 2019; Terrones and Mackay 1992). Fullerene whiskers (FLW)s are thin rod-like structures composed of C60 and C70 fullerenes. FLWs that are hollow inside are called fullerene tubes and have lengths ranging from micrometers to millimeters (Sayers et al. 2016), and those with a diameter of 1 μm or less are called fullerene nanowhiskers or fullerene nanotubes (FNT)s. The spherical arrangement of carbon atoms and the unique physicochemical properties of fullerenes give C60 and C70 fullerenes and FLW great potential for use in many industrial and medical nanotechnology applications (Baker et al. 2008). They naturally produced as a byproduct of combustion from forest fires and volcanic eruptions: see (Shipkowski et al. 2019). FLW is a fibrous form NM. Consequently, similarly to asbestos and carbon nanotubes, there are concerns about adverse effects on the health of workers during production and handling of FLW. However, currently no long-term toxicity studies on FLW have been reported.
There are several studies on short-term inhalation exposure to fullerene C60. Baker et al. exposed F344 rats by inhalation to micrometer size (2.35 mg/m3, 930 nm) and nanometer size (2.22 mg/m3, 55 nm) C60 fullerene for 3 h a day for 10 consecutive days. Lung histology and analysis of the bronchoalveolar lavage fluid (BALF) immediately after exposure and at 1, 5, and 7 days after the end of exposure indicated that there was no pulmonary inflammatory response with minimal changes in the BALF neutrophils and cytokine profile in rats exposed to micrometer and nanometer sized C60, indicating that C60 has little acute inflammatory effect on the lung (Baker et al. 2008). Morimoto et al. examined the pulmonary toxicity of C60 by both inhalation exposure study (0.12 mg/m3, 96 nm, 6 h/days for 5 days/week, 4 weeks) and intratracheal instillation (0.1–1.0 mg/rat, 33 nm, single treatment) using Wister rats. Though an increased neutrophil count in the BALF and expression of neutrophil chemoattractants was observed in the 1.0 mg group administered C60 by intratracheal instillation, no significant changes were seen in the other groups administered C60 by intratracheal instillation or in any of the inhalation exposed groups (Morimoto et al. 2010). These studies indicate that C60 has little acute inflammatory effect on the lung. In contrast, intratracheal instillation of C60 (0.5–2.0 mg/kg, 46.7 nm, single treatment) to ICR mice increased pro-inflammatory cytokines (IL-1, TNF-α, and IL-6) and Th1 cytokines (IL-12 and IFN-γ) and sub-G1 phase and G1 arrested cells in the BALF, leading the authors to conclude that C60 may have the potential to induce an inflammatory response (Park et al. 2010). In a 13-week subchronic inhalation exposure study with nano-sized C60 (0.5–2 mg/m3, 50 nm, 3 h/days for 5 days/week), concentration-dependent histiocytic infiltration and macrophage pigmentation changes were observed in the lungs of both Wister Han rats and B6C3F1/N mice, but chronic inflammation was not induced in either rats or mice exposed to 50 nm C60 (Sayers et al. 2016). However, in the study by Sayers et al., rats and mice were also exposed to 1 µm C60: the mass exposure concentration of the 50 nm C60 was 0.5 and 2 mg/m3 and the mass exposure concentration of the 1 µm C60 was 2, 15, and 30 mg/m3, and both male and female rats and mice exposed to the high concentration of 30 mg/m3 of 1 µm C60 did develop chronic inflammation. Therefore, the possibility that C60 exerts pulmonary toxicity cannot be ruled out, especially since no long-term exposure studies to C60 have been conducted.
In vitro studies have reported cytotoxicity in human dermal cells and hepatocytes exposed to water-soluble C60 FLs due to the production of reactive oxygen species (ROS) (Sayes et al. 2004) and lipid peroxide (Sayes et al. 2005). Though the DNA damaging effects exerted by FL were not strong, formation of ROS can cause inflammation and genetic damage (Nielsen et al. 2008), and production of lipid peroxide can cause membrane damage and cytotoxicity (Sayes et al. 2004). However, another in vitro study reported that FL has very little influence on formation of ROS (Baierl et al. 1996), and another in vitro study reported that FL was a neuroprotective agent by inhibiting the excitotoxic death of cultured cortical neurons induced by exposure to N-methyl-D-aspartate (NMDA), alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA), or oxygen–glucose deprivation (Dugan et al. 1997). These contrasting results may be caused by the physical properties of the FL particles, which might be interrelated with their toxicity. However, a variety of experimental models assessing the toxicity of fullerenes have also demonstrated the absence of toxic effects of pristine fullerenes (Da Ros and Prato 1999; Jensen et al. 1996; Wainwright 2003). In addition, in vivo studies have not only demonstrated a lack of toxicity, but also beneficial and protective effects of C60 fullerenes (Andrievsky et al. 2005; Dugan et al. 2001; Gharbi et al. 2005; Mori et al. 2006).
Okuda-Shimazaki, J. et al. compared FLWs with MWCNTs and Titania nanoparticles, and reported weak cytotoxic effects of FLW compared with MWCNTs and Titania nanoparticles (Okuda-Shimazaki et al. 2010). Cui et al. reported that FLW induced the production of the major proinflammatory cytokine IL-1β via a Nod-like receptor pyrin domain containing 3 (NLRP3) inflammasome-mediated mechanism (Cui et al. 2014). However, definitive evidence of the effect of FLW on inflammation and toxicity is lacking.
To assess the pulmonary and pleural toxicity, including carcinogenic effects, of FL and FLW, we administered FL and FLW by intratracheal instillation into the lungs of male F344 rats and observed the animals for 2 years. MWCNT-7 and MWCNT-N, proven carcinogens, were used as positive controls (Grosse et al. 2014; Suzui et al. 2016).
Materials and methods
Preparation of MWCNTs, FL and FLW
MWCNT-N and MWCNT-7 were supplied by NIKKISO (Tokyo, Japan), and Mitsui Chemicals Inc. (Tokyo, Japan), respectively. C60 FL and FLW, composed of C60 FL were synthesized at room temperature by the liquid–liquid interfacial precipitation method (LLIP method) at National Institute for Materials Science. Briefly, FNWs were precipitated and grown by forming a liquid–liquid interface between a C60-saturated toluene solution and isopropyl alcohol (IPA) (Miyazawa et al. 2014). All of the particles (FL, FLW, MWCNT-7, MWCNT-N) were dispersed and diluted into 5% poloxamer 188 solution (Sigma-Aldrich, St. Louis, Mo, USA) at concentrations of 62.5 and 125 μg/mL. The suspensions were homogenized at 20 kHz, 3000 × g for 20 min using an ultrasonic homogenizer (UD-211, TOMY, Tokyo, Japan) before treatment to minimize aggregation of the administered materials.
Animals
Ten-week-old male F344 rats were purchased from Charles River Laboratories Japan, Inc., Yokohama, Japan. They were housed in the Laboratory Animal Facility of Nagoya City University Medical School, maintained on a 12:12 h light: dark cycle, and received Oriental MF Basal diet (Oriental Yeast, Tokyo, Japan) and water ad libitum. The research protocol was recommended by the Animal Care and Use Committee of Nagoya City University Medical School, and the animals were taken care of according to the Guidelines for the Care and Use of Laboratory Animals of Nagoya City University (no. H30M-008).
Experimental design
We used a total of 224 male F344 rats for the experiment. The animals were quarantined and acclimated for 2 weeks before the start of the experiment. The animals were divided by stratified randomization into 10 body weight-matched groups. Group 1 (25 rats) No treatment; Group 2 (22 rats) Vehicle, saline with 0.5% poloxamer-188 solution; Group 3a (20 rats) FL 0.25 mg/rat; Group 3b (24 rats) FL 0.5 mg/rat; Group 4a (20 rats) FLW 0.25 mg/rat; Group 4b (23 rats) FLW 0.5 mg/rat; Group 5a (20 rats) MWCNT-7 0.25 mg/rat; Group 5b (25 rats) MWCNT-7 0.5 mg/rat; Group 6a (20 rats) MWCNT-N 0.25 mg/rat; Group 6b (25 rats) MWCNT-N 0.5 mg/rat. Rats were administered the test solutions by Intra-tracheal intra-pulmonary spraying (TIPS) as previously described (El-Gazzar et al. 2019; Sato et al. 2023). Briefly, rats were anesthetized with 4% isoflurane and given 0.5 ml of vehicle or test substance suspension (62.5 or 125 μg/ml) using a DIMS-type microsprayer aerosolizer (for rats) that was connected to a 1-mL disposable syringe (OSAKA CHEMICAL Co., Ltd., Osaka, Japan). Rats were administered test solutions once every other day for 15 days for a total of 8 doses. The body weight was measured on the weekly basis. Animals were sacrificed by exsanguination from the abdominal aorta under deep isoflurane anesthesia 1 week and 104 weeks after the final TIPS administration. Five rats from the no treatment, vehicle, and high dose groups were sacrificed at 1 week, and the remaining rats were sacrificed after 104 weeks. Rats began to die after 52 weeks, mostly from causes of death unrelated to the procedure. Treatment-related cause of death was mesothelioma, seen only in the MWCNT-7 0.5 mg/rat group, with the earliest death occurring at 80 weeks post-treatment. Animals that died before the final sacrifice were immediately necropsied for quantitative analysis of neoplastic lesions in the lung and pleura. At 104 weeks, 3 animals from each test substance exposure group were used to determine the amount of residual nanomaterial (NM) remaining in the whole lung. Animals that survived for more than 52 weeks and the animals sacrificed at 104 weeks that were not used for determination of residual NM remaining in the lung were used to evaluate carcinogenic lesions in the lungs and pleura.
Collection of tissue samples and pleural lavage
Blood samples collected from the abdominal aorta were centrifuged at 3000×g, 4 °C for 10 min and then the serum was collected. 10 ml of RPMI1640 (Thermo Fisher Scientific, Rockford, IL) was injected into the pleural cavity through the left side of the diaphragm, the entire chest cavity was shaken from side to side, and the lavage was collected. The pleural lavage was centrifuged at 1000 × g, 4 °C for 10 min and the supernatant were used for biochemical analysis. Precipitates after centrifugation were fixed with 4% paraformaldehyde solution and paraffin-embedded for histological analysis. Myeloperoxidase (MPO) levels were measured using an Amplite Fluorimetric Myeloperoxidase Assay Kit (AAT Bioquest, Inc., Sunnyvale, CA) and ROS levels were measured using the dichloro-dihydro-fluorescein diacetate (DCFH-DA) assay (Thermo Fisher Scientific) as previously described (Naiki et al. 2012). The left lobe of the lung was cut into small pieces and immediately frozen at -80⁰C for RNA extraction or ROS detection, and the 4 right lobes were fixed with 4% paraformaldehyde solution and paraffin-embedded for light microscopic examination, scanning electron microscopy (SEM), and immunohistochemical analysis. SEM was performed as previously described (Saleh et al. 2020). The heart, trachea, paratracheal lymph node, liver, kidney, spleen, and chest wall were removed and fixed with 10% formalin, paraffin-embedded and used for histological evaluation.
Pathological examination and Immunohistochemistry
Three µm-thick sections were prepared from the fixed, paraffin-embedded specimens and stained with Hematoxylin and Eosin (H&E). Underlying sections were immunohistochemically stained with antibodies against CD68 (Bio-Rad Cat# MCA341R, RRID:AB_2291300, Cambridge, UK), Ki67 (Abcam Cat# ab16667, RRID:AB_302459, Hercules, CA), and 8-hydroxydeoxy guanosine (8-OHdG) (Japan Institute for Control of Aging Cat# MOG-020P, RRID:AB_3096485, Shizuoka, Japan). H&E slides were evaluated by two experts in pathology (A.N-I. and H.T.) and diagnosis of hyperplasia, adenoma, adenocarcinoma in lung, and mesothelioma was done according to the INHAND criteria.
Detection of ROS production
Six µm thick slices were cut from the frozen lung tissues of rats sacrificed at 1 week after TIPS administration and incubated in 5 μM dihydroethidium (Thermo Fisher Scientific) for 15 min in the dark. The slides were washed with phosphate buffered saline and ROS was detected at 518/605 nm using an image analyzer (BZ 9000 Fluorescence Microscope, RRID:SCR_015486, Keyence, Osaka, Japan). Five images per rat were randomly taken with the same exposure time at 400 × magnification, and the average fluorescence intensity in the alveolar epithelial nuclei was quantified using BZ-analysis application software (Keyence).
RNA extraction and quantitative reverse transcription–PCR
Total RNA was isolated from frozen lung tissues by phenol–chloroform extraction (Isogen; Nippon Gene Co. Ltd., Tokyo, Japan). One microgram of RNA was converted to cDNA using PrimeScript™ RT Master Mix (Takara). The cDNA was subjected to quantitative real-time PCR (qRT-PCR) using TB Green™ Premix Ex Taq™ II (Takara) and detected by the AriaMx Real-Time PCR System (g8830a, RRID:SCR_019469, Agilent Technologies). The primers used are listed in Table S1. GAPDH mRNA levels were used as internal controls.
Total protein and albumin in the pleural lavage
The levels of total protein and albumin in the pleural lavage at week 1 were measured using standard procedures on an autoanalyzer by a commercial laboratory (DIMS Institute of Medical Science, Aichi, Japan).
Measurement of FLW and MWCNTs in the lung
MWCNT concentration in the lung was measured as previously described (Ohnishi et al. 2013, 2016). Briefly, the formalin-fixed lungs (n = 3 per group) containing MWCNT were digested by a strong alkali solution (Clean 99 K200; Clean Chemical, Osaka, Japan), and after removing organic matter with sulfuric acid, benzo[ghi]perylene (B(ghi)P) (FUJIFILM Wako Pure Chemical Corporation, Osaka, Japan) was added to the sample solution. The sample solution was immediately sonicated by an ultrasonic homogenizer (VP-30S, Taitec, Saitama, Japan) to allow the MWCNT to adsorb the B(ghi)P. The solution was filtrated through a membrane filter (Whatman® Nuclepore, 111,109, Cytiva). The B(ghi)P on the filter was desorbed from the MWCNT into acetonitrile. Finally, the B(ghi)P was analyzed by an UPLC system (Waters, Milford, MA) coupled to a fluorescence detector with a reversed phase column (ACQUITY UPLC BEH C18, Waters).
FL and FLW in the formalin-fixed lungs (n = 3 per group) was measured as below with reference to JIS Z 8981:2010 (Quantitative analysis methods for [60]fullerene and [70]fullerene by high performance liquid chromatography). The digested lung samples by a strong alkali solution passed thorough the liquid–liquid extraction column (EXtrelut NT, Merck, Darmstadt, Germany). The adsorbed FLWs in the column were eluted using toluene. The elution was concentrated by nitrogen and filled to 1 mL by toluene: methanol = 1:1. The FLW concentrations were analyzed by an HPLC system (LC-10; Shimadzu Corporation, Kyoto, Japan). Absorbance was detected at 325 nm. The flow rate of the mobile phases (toluene: methanol = 1:1) was 0.8 mL/min. A reversed phase column (Inertsil ODS-2, GL Sciences Inc., Tokyo, Japan) was used at 35 °C.
Statistical analysis
Differences in quantitative data, expressed as mean ± standard deviation (SD), between groups were compared by one-way ANOVA and the Turkey’s multiple comparison test using the software package GraphPad Prism 8 (GraphPad Software, Inc., La Jolla, CA, USA). P < 0.05 was considered significant.
Results
Histological analysis of the lung at week 1
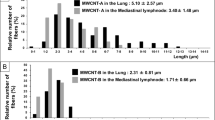
The diameters of FLW, MWCNT-7, and MWCNT-N were 0.261 ± 0.064 μm, 0.053 ± 0.018 μm, and 0.048 ± 0.023 μm, respectively (Fig. 1a). No clinical symptoms were found in the treated groups at the 1-week sacrifice. The body and organ weights at 1-week are shown in Table 1. There was no significant change in body weights or liver and kidneys weights in the FL, FLW, MWCNT-7, and MWCNT-N treated groups compared to the vehicle group. Lung weights in the vehicle group were significantly higher than in the no treatment group, possibly due to the residual effect of 8 doses of 0.5 ml vehicle solution. FLW and both MWCNTs significantly increased lung weight compared to vehicle, but no changes in the FL groups were observed. SEM images of the NM-treated groups are shown in Fig. 1b. MWCNT-7 and MWCNT-N were found engulfed by macrophages in the lung. Fibrous MWCNT-7 penetrated the plasma membrane of the macrophages. Only a very small amount of FLW incorporated into alveolar macrophages was observed in SEM (Fig. 1b). This was probably due to easy solubility of fullerenes in organic solvents, such as xylene treatment after paraformaldehyde fixation (Fan et al. 2020). In frozen sections without xylene treatment, FLW was readily deposited in the alveoli (Fig. 1c). H&E staining revealed that MWCNTs deposited in the lungs of rats treated with MWCNT-7 and MWCNT-N, and induced higher neutrophil infiltration into the alveoli, while there was less neutrophil infiltration in the lungs of rats treated with FLW and no increased neutrophil infiltration into the alveoli in the FL group (Fig. 2a). CD68 immunohistochemistry showed significantly increased infiltration of alveolar macrophage in the FLW, MWCNT-7 and MWCNT-N groups. There was no change in the FL group compared to the vehicle group (Fig. 2a,b). Treatment with MWCNTs also increased the Ki67 labeling index of alveolar epithelia, with a statistically significant increase in the MWCNT-N group (Fig. 2a,c). These results suggest that MWCNTs-induced lung carcinogenicity may correlated with increased Ki67 labeling index of alveolar epithelial cells.
Fibers of FLW, MWCNT-7 and MWCNT-N. a, b Scanning electron microscopic images of FLW fibers (a), and FLW, MWCNT-7 and MWCNT-N fibers in lung (b). Arrows indicate MWCNT or FLW fibers phagocytosed by alveolar macrophages. c FLW fibers in paraformaldehyde fixed frozen lung section. Deposition of FLWs is indicated by arrowheads
Infiltration of neutrophils, alveolar macrophages and proliferation activity in the lung at week 1. a Representative hematoxylin and eosin (H&E) staining, macrophage recruitment by CD68 immunohistochemistry, and cell proliferation by Ki67 immunohistochemistry of lung sections from the vehicle, FL, FLW, MWCNT-7 and MWCNT-N groups at week 1. Deposition of MWCNTs is indicated by arrowheads. b Percentage of the CD68 positive area. c The labeling index of Ki67 in alveolar epithelia. Data are presented as mean ± SD, n = 5 per group, ***P < 0.001 statistically significant from the vehicle group
ROS production and cytokines expression in the lung at week 1
We previously reported positive correlations between carcinogenicity and oxidative stress in the liver and prostate (Naiki-Ito et al. 2020; Sagawa et al. 2015; Suzuki et al. 2013). Therefore, we compared ROS production and inflammatory cytokine levels in the lung after FL, FLW, and MWCNTs administration. Dihydroethidium staining assays indicated a significant elevation of ROS in the lungs of the MWCNT-7 and MWCNT-N treated rats compared to the vehicle control. There was no significant change in the lungs of FL and FLW treated rats compared to the vehicle control (Fig. 3a, b). The mRNA expression of the chemokines, Ccl2 and Ccl3, was significantly up-regulated by MWCNT-7 and MWCNT-N, while these levels were not changed by FL and FLW.
Intracellular reactive oxygen species (ROS) levels in the lung at week 1. a Representative dihydroethidium (DHE) staining of lung sections from the vehicle, FL, FLW, MWCNT-7 and MWCNT-N groups at week 1. b The signal intensity of DHE staining is presented as the mean ± SD, n = 5 per group, ***P < 0.001 statistically significant from the vehicle group
The expression levels of other inflammatory cytokines, Tnf-α, Il6, Il-1β, Il18, Tgf-β1 and Ifn-γ, were not significantly altered by administration of FL, FLW, or MWCNTs (Fig. 4). The results of oxidative stress induction by both MWCNTs, positive lung carcinogens, suggest that oxidative stress and carcinogenicity may be closely related in the lung.
mRNA expression of inflammatory cytokines in the lung. mRNA level for inflammatory cytokines Ccl2, Ccl3, Tnf-α, Il-6, Il-1β, Il-18, Tgf-β1, Il-18, Ifn-γ, and Ctgf at week 1 as measured by quantitative RT-PCR. Data are presented as mean ± SD, n = 5 per group, ***P < 0.001 statistically significant from the vehicle group
Histological analysis of the mesothelium at week 1
Toxic effects of FL, FLW, and MWCNTs on the mesothelium were analyzed. The recruitment of macrophages in the precipitates of the pleural lavage were significantly increased in all treatment groups compared to the vehicle group (Fig. 5a, b). A significant increase in Ki67 labeling index of visceral pleural mesothelial cells was observed only in the MWCNT-N-treated group and not in FL, FLW, or MWCNT-7 groups (Fig. 5a, c). The ROS and MPO levels in the pleural lavage were not changed in any of the treatment groups compared to the vehicle group (Fig. 5d, e). FLW and the two MWCNTs slightly increased protein and albumin levels in the pleural lavage, but there were not any significant changes (Table 2). These results indicated that significant changes in several toxicity parameters were observed in the alveolar epithelium after 1 week of MWCNTs administration, whereas no significant toxicity was observed in the pleura. FL and FLW did not induce any apparent toxicity in the lung or pleura.
Infiltration of macrophages and proliferation activity in the pleura at week 1. a Representative macrophage recruitment by CD68 immhonohistochemistry of the pleural lavage, and cell proliferation by Ki67 immhonohistochemistry of lung sections from the vehicle, FL, FLW, MWCNT-7 and MWCNT-N group at week 1. b Percentage of the CD68 positive area. c The labeling index of Ki67 in the pleural mesothelium. d Intracellular ROS levels in the pleural lavage was measured by DCFH-DA assay. e Myeloperoxidase (MPO) level in the pleural lavage was measured by Amplite Fluorimetric Myeloperoxidase Assay Kit. Data are presented as mean ± SD, n = 5 per group, *P < 0.05, **P < 0.01, ***P < 0.001 statistically significant from the vehicle group
Histological analysis at week 104
Eight rats from the no treatment group, 4 rats from the vehicle group, 5 rats from the FL 0.25 mg group, 7 rats from the FL 0.5 mg group, 5 rats from the FLW 0.25 mg group, 5 rats from the FLW 0.5 mg group, 5 rats from the MWCNT-7 0.25 mg group, 5 rats from the MWCNT-7 0.5 mg group, 3 rats from the MWCNT-N 0.25 mg group, and 8 rats from the MWCNT-N 0.5 mg group survived for more than 52 weeks after treatment but died before the final sacrifice at 104 weeks. Only one rat of treated related causes. One rat in the MWCNT-7 0.5 mg group died of treatment-related pleural mesothelioma at 80 weeks post-treatment. The causes of death before 104 weeks of the other rats were unrelated to the treatments, and included malignant lymphoma and leukemia. At the 104-week sacrifice, there was no significant difference in body, liver, kidney, or lung weights among the groups (Table 3).
Neoplastic lesions of lung and pleura are shown in Table 4 and Fig. 6. The incidence of hyperplasia in the lung was increased by administration of MWCNT-7 and MWCNT-N, and significantly elevated in the MWCNT-7 0.5 mg group. Hyperplasia or adenoma occurred in 1–2 animals in the FL and FLW treatment groups and also in the no treatment and vehicle groups, so these lesions were not considered to be caused by treatment with FL or FLW. The incidence of adenocarcinoma was increased in the MWCNT-treated groups but not in FL or FLW-treated groups. Adenocarcinoma was significantly increased in the MWCNT-N 0.5 mg group. The combined incidence of adenomas and adenocarcinomas was significantly increased in the 0.25 and 0.5 mg MWCNT-7 groups and in the 0.25 mg MWCNT-N group. The level of 8-OHdG formation in the lung was significantly elevated the MWCNT-7 and MWCNT-N groups, suggesting an association with lung tumorigenesis (Fig. 7a, b).
8-hydroxydeoxy guanosine (8-OHdG) levels in lung at week 104. a Representative 8-OHdG immunohistochemistry of lung sections from the vehicle, FL, FLW, MWCNT-7 and MWCNT-N group at week 104. b The number of 8-OHdG positive alveolar cells per 1,000 cells is presented as the mean ± SD, n = 14–17 per group, ***P < 0.001 statistically significant from the vehicle group
Pleural mesothelioma occurred in the visceral pleura (lungs) and parietal pleura (chest wall, pericardium, and diaphragm) and was observed only in the MWCNT-treated groups (Table 4 and Fig. 6b). Induction of mesothelioma in the visceral pleura was observed in the MWCNT-7 high-dose group, and induction of mesothelioma in the parietal pleura was observed in both the low and high dose MWCNT-7 groups and the MWCNT-N high-dose group. The incidence of mesothelioma in both visceral and parietal pleura was significantly increased in the MWCNT-7 high-dose group. FL or FLW did not show any carcinogenic potential to either the lung or mesothelium.
Residuals of NMs in the lung at week 104
Residual FL, FLW, and MWCNTs in the lung at 104 week were measured using the whole lung. Very little FL remained in the lungs at 104 weeks, and only about 1% of the initial dose of FLW remained in the lung at 104 weeks. In contrast, MWCNT-7 and MWCNT-N had high residual levels, ranging from 18.0 to 57.0%, of the initial dose, indicating biological persistence of MWCNTs in the lungs (Table 5).
Discussion
Due to the dramatic improvements in the functions and properties obtained by nanosizing materials, NMs are attracting attention as new materials for industrial and medical technologies. In particular, CNTs have excellent electrical, mechanical, and thermal properties, and various types of CNTs have been commercialized and used for numerous applications in industrial fields. With the increased use and production of CNTs, adverse health effects due to inhalation exposure of workers in the manufacturing and handling processes of CNTs and to consumers of products manufactured from CNTs have become a serious problem. Intraperitoneal administration of MWCNTs has been reported to induce malignant mesothelioma in mice and rats (Sakamoto et al. 2009; Takagi et al. 2008). However, the route of administration of MWCNTs in these studies was different from the actual inhalation exposure expected in humans, and evaluation of MWCNTs with matched exposure routes is required. Kasai et al. developed an exposure system for whole-body inhalation exposure to MWCNTs (Kasai et al. 2014). Inhalation exposure of F344 rats to MWCNT-7 (0, 0.02, 0.2, and 2 mg/m3) resulted in deposition of MWCNT-7 in the alveoli as well as in the thoracic cavity and diaphragm, and significantly induced alveolar adenocarcinoma at doses of 0.2 and 2 mg/m3 in males and 2 mg/m3 in females (Kasai et al. 2016). The evaluation of MWCNTs by inhalation exposure would be ideal, but an inhalation exposure study is extremely difficult to conduct because of the extensive equipment and high cost involved. Currently, the study by Kasai et al. is the only long-term inhalation exposure carcinogenicity study of MWCNTs. Therefore, we developed a trans-airway intrapulmonary spraying study design called the TIPS method, a simple alternative to inhalation exposure studies of NMs. MWCNT-7 by the TIPS method induced broncho-alveolar adenoma, adenocarcinoma in the lung, and malignant mesothelioma in the pleura (Abdelgied et al. 2019a, 2019b; Numano et al. 2019; Saleh et al. 2022). The carcinogenicity of another MWCNT, MWCNT-N, to the lung and pleural mesothelium was also assessed using TIPS administration (Suzui et al. 2016). Therefore, in the present study, we evaluated the pleural toxicity of FL and FLW using TIPS, and using MWCNT-7 and MWCNT-N as positive controls for pulmonary and pleural toxicity and carcinogenicity.
The final results of this 2-year study showed that a few bronchiolo-alveolar hyperplasia and bronchiolo-alveolar adenomas developed in the lungs of FL or FLW-treated rats, but the incidence was not statistically different from that in the no treatment and vehicle groups, and no dose-dependency was observed. On the other hand, MWCNT-7 and MWCNT-N significantly increased the incidence of bronchiolo-alveolar adenocarcinoma or adenoma plus adenocarcinoma (Table 4). In the pleural mesothelium, the incidence of malignant mesothelioma was significantly increased in the MWCNT-7 high-dose group. No tumor formation was observed after TIPS administration of FL or FLW. The results of the lung and pleural carcinogenicity of MWCNT-7 in the current experiment were consistent with the results of previous studies (Abdelgied et al. 2019b; Numano et al. 2019). On the other hand, MWCNT-N differed from the previous study in that it showed significant lung carcinogenicity but no evidence of pleural mesothelioma development (Suzui et al. 2016). This may be due to the fact that the doses of MWCNT-N administered in the current experiment were 0.25 and 0.5 mg, whereas the dose in the previous study was 1.0 mg. Based on these results, we conclude that FL and FLW are not carcinogenic to the lung. This is the first 2-year toxicity study to evaluate the carcinogenic potential of FL and FLW in the rat lung after TIPS administration.
It is essential to discuss the factors involved in the carcinogenic potential of NMs. In this study, we examined histological changes in factors involved in inflammation, oxidative stress, and cell proliferation observed in the first week after NM administration. Absolute and relative lung weights did not change in the FL group, but significantly increased in the FLW group, along with lung weights of the positive controls, MWCNT-7 and MWCNT-N. MWCNT-7 and MWCNT-N induced recruitment of CD68-positive alveolar macrophages and infiltration of neutrophils into the lung lobes. Similar but more mild increases were observed in the FLW group. In contrast, no changes were observed in the FL groups. This result is consistent with results reported in a previous study in which only a small neutrophil infiltrate was observed in the acute phase after inhalation exposure or intratracheal administration of FL (Baker et al. 2008; Morimoto et al. 2010). Lung weight can increase due to neutrophil infiltration in response to acute lung injury in Wegener’s granulomatosis model (Hattar et al. 2010). In the present study, lung weight correlated with the extent of alveolar macrophage and neutrophil infiltration 1 week after administration, suggesting an increase in lung weight due to inflammation induced by NMs.
MWCNT-7 and MWCNT-N also induced ROS production in alveolar epithelial cells and an increase cell proliferative activity. In contrast, FLW did not induce ROS production in alveolar epithelial cells or an increase in cell proliferative activity. There are both positive and negative reports of ROS production by FL in vitro (Baierl et al. 1996; Sayes et al. 2004), however, our present study did not show a significant increase in ROS production after administration of FL or FLW (Fig. 3).
Various types of NMs demonstrated to induce inflammation and this reaction is considered to be a common response associated with exposure to certain types of NMs (Donaldson et al. 2005). Gene expression analysis of inflammatory cytokines in the lung at 1 week showed that Ccl2 and Ccl3 were significantly up-regulated by both MWCNT-7 and MWCNT-N, but Tnf-α, Il-6, Il-1β, Il-18, Tgf-β1, and Ifn-γ were not changed by either MWCNT-7 and MWCNT-N. There were no expression changes in these cytokines after exposure to FL or FLW (Fig. 4). These results indicated that FL and FLW exhibited no inflammatory potential. Thus, overall, FL and FLW did not affect lung cell proliferative activity, inflammatory responses, or oxidative stress 1 week after treatment, but these toxicity markers were elevated in the positive control groups and may predict carcinogenicity at 2 years.
Residual rates of NMs after deposition in the lungs may also affect the toxicity of NMs. In this study, we quantified the residual levels of the administered materials in the lungs 2 years after administration, we found that the residual levels of FL and FLW were markedly lower than those of the MWCNTs. Notably, retention of MWCNTs in the lungs correlated with early proliferative activity, ROS production, and inflammatory cytokine expression in the lungs of the rats.
In contrast to analysis of the lungs, analysis of the pleural lavage fluid after 1 week showed no significant changes in the MWCNT groups. These results indicate that no early indicators of carcinogenicity to the pleural mesothelium were found. This remains an issue for future studies, including what is analyzed and the time period after administration of the analysis.
In conclusion, our 2-year observation with 8 doses/15 days of FL and FLW by TIPS administration revealed that neither FL or FLW caused alterations of inflammatory responses or cell proliferation in the lung or pleura and no carcinogenic changes occurred. In addition, proliferative activity and ROS levels in the alveolar epithelium 1 week after TIPS administration were associated with carcinogenicity, which may contribute to improved carcinogenicity detection in future studies.
Data availability
The data generated or analysed during this study are included in this published article and its supplementary information files. Any other data sets that support the findings of this study are available on request from the corresponding author [A.N.-I.].
Abbreviations
- BALF:
-
Bronchoalveolar lavage fluid
- DCFH-DA:
-
Dichloro-dihydro-fluorescein diacetate
- FL:
-
Fullerene
- FLW:
-
Fullerene whisker
- FNT:
-
Fullerene nanotube
- H&E:
-
Hematoxylin and eosin
- TIPS:
-
Intra-tracheal intra-pulmonary spraying
- MPO:
-
Myeloperoxidase
- MWCNT:
-
Multi-walled carbon nano tube
- NM:
-
Nanomaterial
- qRT-PCR:
-
Quantitative real-time PCR
- ROS:
-
Reactive oxygen species
- SEM:
-
Scanning electron microscopy
- 8-OHdG:
-
8-Hydroxydeoxy guanosine
References
Abdelgied M, El-Gazzar AM, Alexander DB et al (2019a) Pulmonary and pleural toxicity of potassium octatitanate fibers, rutile titanium dioxide nanoparticles, and MWCNT-7 in male Fischer 344 rats. Arch Toxicol 93(4):909–920. https://doi.org/10.1007/s00204-019-02410-z
Abdelgied M, El-Gazzar AM, Alexander WT et al (2019b) Carcinogenic effect of potassium octatitanate (POT) fibers in the lung and pleura of male Fischer 344 rats after intrapulmonary administration. Part Fibre Toxicol 16(1):34. https://doi.org/10.1186/s12989-019-0316-2
Andrievsky G, Klochkov V, Derevyanchenko L (2005) Is the C60 fullerene molecule toxic?! Fullerenes, Nanotubes Carbon Nanostruct 13(4):363–376. https://doi.org/10.1080/15363830500237267
Baierl T, Drosselmeyer E, Seidel A, Hippeli S (1996) Comparison of immunological effects of Fullerene C60 and raw soot from Fullerene production on alveolar macrophages and macrophage like cells in vitro. Exp Toxicol Pathol 48(6):508–511. https://doi.org/10.1016/s0940-2993(96)80068-6
Baker GL, Gupta A, Clark ML et al (2008) Inhalation toxicity and lung toxicokinetics of C60 fullerene nanoparticles and microparticles. Toxicol Sci 101(1):122–131. https://doi.org/10.1093/toxsci/kfm243
Cui H, Wu W, Okuhira K et al (2014) High-temperature calcined fullerene nanowhiskers as well as long needle-like multi-wall carbon nanotubes have abilities to induce NLRP3-mediated IL-1beta secretion. Biochem Biophys Res Commun 452(3):593–599. https://doi.org/10.1016/j.bbrc.2014.08.118
Da Ros T, Prato M (1999) Medicinal chemistry with fullerenes and fullerene derivatives. Chem Commun. https://doi.org/10.1039/A809495K
Donaldson K, Tran L, Jimenez LA et al (2005) Combustion-derived nanoparticles: a review of their toxicology following inhalation exposure. Part Fibre Toxicol 2(1):10. https://doi.org/10.1186/1743-8977-2-10
Dugan LL, Turetsky DM, Du C et al (1997) Carboxyfullerenes as neuroprotective agents. Proc Natl Acad Sci U S A 94(17):9434–9439. https://doi.org/10.1073/pnas.94.17.9434
Dugan LL, Lovett EG, Quick KL, Lotharius J, Lin TT, O’Malley KL (2001) Fullerene-based antioxidants and neurodegenerative disorders. Parkinsonism Relat Disord 7(3):243–246. https://doi.org/10.1016/s1353-8020(00)00064-x
El-Gazzar AM, Abdelgied M, Alexander DB et al (2019) Comparative pulmonary toxicity of a DWCNT and MWCNT-7 in rats. Arch Toxicol 93(1):49–59. https://doi.org/10.1007/s00204-018-2336-3
Fan X, Soin N, Li H, Li H, Xia X, Geng J (2020) Fullerene (C60) nanowires: the preparation, characterization, and potential applications. Energy Environ Mater 3(4):469–491. https://doi.org/10.1002/eem2.12071
Gharbi N, Pressac M, Hadchouel M, Szwarc H, Wilson SR, Moussa F (2005) [60]fullerene is a powerful antioxidant in vivo with no acute or subacute toxicity. Nano Lett 5(12):2578–2585. https://doi.org/10.1021/nl051866b
Grosse Y, Loomis D, Guyton KZ et al (2014) Carcinogenicity of fluoro-edenite, silicon carbide fibres and whiskers, and carbon nanotubes. Lancet Oncol 15(13):1427–1428. https://doi.org/10.1016/S1470-2045(14)71109-X
Hattar K, Oppermann S, Ankele C et al (2010) c-ANCA-induced neutrophil-mediated lung injury: a model of acute Wegener’s granulomatosis. Eur Respir J 36(1):187–195. https://doi.org/10.1183/09031936.00143308
Hirsch A (2010) The era of carbon allotropes. Nat Mater 9(11):868–871. https://doi.org/10.1038/nmat2885
Jensen AW, Wilson SR, Schuster DI (1996) Biological applications of fullerenes. Bioorg Med Chem 4(6):767–779. https://doi.org/10.1016/0968-0896(96)00081-8
Johnston HJ, Hutchison GR, Christensen FM, Aschberger K, Stone V (2010) The biological mechanisms and physicochemical characteristics responsible for driving fullerene toxicity. Toxicol Sci 114(2):162–182. https://doi.org/10.1093/toxsci/kfp265
Kasai T, Gotoh K, Nishizawa T et al (2014) Development of a new multi-walled carbon nanotube (MWCNT) aerosol generation and exposure system and confirmation of suitability for conducting a single-exposure inhalation study of MWCNT in rats. Nanotoxicology 8(2):169–178. https://doi.org/10.3109/17435390.2013.766277
Kasai T, Umeda Y, Ohnishi M et al (2016) Lung carcinogenicity of inhaled multi-walled carbon nanotube in rats. Part Fibre Toxicol 13(1):53. https://doi.org/10.1186/s12989-016-0164-2
Kuganathan N, Srikaran R, Chroneos A (2019) Stability of coinage metals interacting with C(60). Nanomaterials (Basel). https://doi.org/10.3390/nano9101484
Miyazawa Ki, Hirata C, Wakahara T (2014) Influence of the solution volume on the growth of C60 nanowhiskers. J Cryst Growth 405:68–72. https://doi.org/10.1016/j.jcrysgro.2014.07.036
Mori T, Takada H, Ito S, Matsubayashi K, Miwa N, Sawaguchi T (2006) Preclinical studies on safety of fullerene upon acute oral administration and evaluation for no mutagenesis. Toxicology 225(1):48–54. https://doi.org/10.1016/j.tox.2006.05.001
Morimoto Y, Hirohashi M, Ogami A et al (2010) Inflammogenic effect of well-characterized fullerenes in inhalation and intratracheal instillation studies. Part Fibre Toxicol 7:4. https://doi.org/10.1186/1743-8977-7-4
Naiki T, Asamoto M, Toyoda-Hokaiwado N et al (2012) Organ specific Gst-pi expression of the metastatic androgen independent prostate cancer cells in nude mice. Prostate 72(5):533–541. https://doi.org/10.1002/pros.21455
Naiki-Ito A, Naiki T, Kato H et al (2020) Recruitment of miR-8080 by luteolin inhibits androgen receptor splice variant 7 expression in castration-resistant prostate cancer. Carcinogenesis 41(8):1145–1157. https://doi.org/10.1093/carcin/bgz193
Nielsen GD, Roursgaard M, Jensen KA, Poulsen SS, Larsen ST (2008) In vivo biology and toxicology of fullerenes and their derivatives. Basic Clin Pharmacol Toxicol 103(3):197–208. https://doi.org/10.1111/j.1742-7843.2008.00266.x
Numano T, Higuchi H, Alexander DB et al (2019) MWCNT-7 administered to the lung by intratracheal instillation induces development of pleural mesothelioma in F344 rats. Cancer Sci 110(8):2485–2492. https://doi.org/10.1111/cas.14121
Ohnishi M, Yajima H, Kasai T et al (2013) Novel method using hybrid markers: development of an approach for pulmonary measurement of multi-walled carbon nanotubes. J Occup Med Toxicol 8(1):30. https://doi.org/10.1186/1745-6673-8-30
Ohnishi M, Suzuki M, Yamamoto M et al (2016) Improved method for measurement of multi-walled carbon nanotubes in rat lung. J Occup Med Toxicol 11:44. https://doi.org/10.1186/s12995-016-0132-7
Okuda-Shimazaki J, Takaku S, Kanehira K, Sonezaki S, Taniguchi A (2010) Effects of titanium dioxide nanoparticle aggregate size on gene expression. Int J Mol Sci 11(6):2383–2392. https://doi.org/10.3390/ijms11062383
Park EJ, Kim H, Kim Y, Yi J, Choi K, Park K (2010) Carbon fullerenes (C60s) can induce inflammatory responses in the lung of mice. Toxicol Appl Pharmacol 244(2):226–233. https://doi.org/10.1016/j.taap.2009.12.036
Sagawa H, Naiki-Ito A, Kato H et al (2015) Connexin 32 and luteolin play protective roles in non-alcoholic steatohepatitis development and its related hepatocarcinogenesis in rats. Carcinogenesis 36(12):1539–1549. https://doi.org/10.1093/carcin/bgv143
Sakamoto Y, Nakae D, Fukumori N et al (2009) Induction of mesothelioma by a single intrascrotal administration of multi-wall carbon nanotube in intact male Fischer 344 rats. J Toxicol Sci 34(1):65–76. https://doi.org/10.2131/jts.34.65
Saleh DM, Alexander WT, Numano T et al (2020) Comparative carcinogenicity study of a thick, straight-type and a thin, tangled-type multi-walled carbon nanotube administered by intra-tracheal instillation in the rat. Part Fibre Toxicol 17(1):48. https://doi.org/10.1186/s12989-020-00382-y
Saleh DM, Luo S, Ahmed OHM et al (2022) Assessment of the toxicity and carcinogenicity of double-walled carbon nanotubes in the rat lung after intratracheal instillation: a two-year study. Part Fibre Toxicol 19(1):30. https://doi.org/10.1186/s12989-022-00469-8
Sato K, Fukui H, Hagiwara Y et al (2023) Difference in carcinogenicities of two different vapor grown carbon fibers with different physicochemical characteristics induced by intratracheal instillation in rats. Part Fibre Toxicol 20(1):37. https://doi.org/10.1186/s12989-023-00547-5
Sayers BC, Germolec DR, Walker NJ et al (2016) Respiratory toxicity and immunotoxicity evaluations of microparticle and nanoparticle C60 fullerene aggregates in mice and rats following nose-only inhalation for 13 weeks. Nanotoxicology 10(10):1458–1468. https://doi.org/10.1080/17435390.2016.1235737
Sayes CM, Fortner JD, Guo W et al (2004) The differential cytotoxicity of water-soluble fullerenes. Nano Lett 4(10):1881–1887. https://doi.org/10.1021/nl0489586
Sayes CM, Gobin AM, Ausman KD, Mendez J, West JL, Colvin VL (2005) Nano-C60 cytotoxicity is due to lipid peroxidation. Biomaterials 26(36):7587–7595. https://doi.org/10.1016/j.biomaterials.2005.05.027
Shipkowski KA, Sanders JM, McDonald JD, Walker NJ, Waidyanatha S (2019) Disposition of fullerene C60 in rats following intratracheal or intravenous administration. Xenobiotica 49(9):1078–1085. https://doi.org/10.1080/00498254.2018.1528646
Suzui M, Futakuchi M, Fukamachi K et al (2016) Multiwalled carbon nanotubes intratracheally instilled into the rat lung induce development of pleural malignant mesothelioma and lung tumors. Cancer Sci 107(7):924–935. https://doi.org/10.1111/cas.12954
Suzuki S, Pitchakarn P, Ogawa K et al (2013) Expression of glutathione peroxidase 2 is associated with not only early hepatocarcinogenesis but also late stage metastasis. Toxicology 311(3):115–123. https://doi.org/10.1016/j.tox.2013.07.005
Takagi A, Hirose A, Nishimura T et al (2008) Induction of mesothelioma in p53+/- mouse by intraperitoneal application of multi-wall carbon nanotube. J Toxicol Sci 33(1):105–116. https://doi.org/10.2131/jts.33.105
Terrones H, Mackay AL (1992) The geometry of hypothetical curved graphite structures. Carbon 30(8):1251–1260. https://doi.org/10.1016/0008-6223(92)90066-6
Wainwright M (2003) A microbiologist looks at panspermia. Astrophys Space Sci 285(2):563–570. https://doi.org/10.1023/A:1025494005689
Acknowledgements
The authors would like to acknowledge Dr. Makoto Onishi for measurement of FL, FLW and MWCNTs.
Funding
This work was supported by MHLW Association for Promotion of Research on Risk Assessment Program Grant Number JPMH16769893 (2016–2018) to H.T. and MHLW Association for Promotion of Research on Risk Assessment Program Grant Number JPMH20316858 (2020–2022) to A.N-I.
Author information
Authors and Affiliations
Contributions
Asraful Nahar Sheema: Validation, Formal analysis, Investigation, Visualization, Writing—Original Draft, Aya Naiki-Ito: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Writing—Original Draft, Review & Editing, Visualization, Supervision, Project administration, Funding acquisition, Anna Kakehashi: Validation, Formal analysis, Investigation, Omnia Hosny Mohamed: Validation, Formal analysis, Investigation, David B. Alexander: Investigation, William T. Alexander: Investigation, Takamasa Numano: Investigation, Hiroyuki Kato: Investigation, Hiroshi Takase: Investigation, Yuko Goto: Investigation, Akihiko Hirose: Resources, Takatsugu Wakahara: Resources, Kun’ichi Miyazawa: Resources, Satoru Takahashi: Methodology, Writing—Review & Editing, Hiroyuki Tsuda: Conceptualization, Methodology, Resources, Supervision, Project administration, Funding acquisition.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sheema, A.N., Naiki-Ito, A., Kakehashi, A. et al. Fullerene and fullerene whisker are not carcinogenic to the lungs and pleura in rat long-term study after 2-week intra-tracheal intrapulmonary administration. Arch Toxicol (2024). https://doi.org/10.1007/s00204-024-03863-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00204-024-03863-7