Abstract
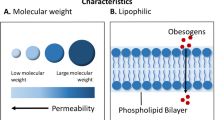
Obesogenic endocrine disruptors, also known as obesogens, are chemicals potentially involved in weight gain by altering lipid homeostasis and promoting adipogenesis and lipid accumulation. They included compounds to which human population is exposed over daily life such as pesticides/herbicides, industrial and household products, plastics, detergents and personal care products. The window of life during which the exposure happens could lead to different effects. A critical window is during utero and/or neonatal period in which the obesogens could cause subtle changes in gene expression and tissue organization or blunt other levels of biological organization leading to increased susceptibility to diseases in the adulthood. Some of the reasons for this increased sensitivity include the lack of the protective mechanisms that are available in adult such as DNA repair mechanisms, a competent immune system, detoxifying enzymes, liver metabolism and the blood/brain barrier still not fully functional in the fetus or newborn. The mechanisms of action of obesogens lay on their ability to increase the number and/or the size of the adipocytes and to alter appetite, satiety and food preferences. The ability of obesogens to increase fat deposition results in an increased capacity for their own retention due to their lipophilic properties; thus prolonging the exposure and increasing the detrimental metabolic consequences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A growing body of evidence reported an increasing prevalence of obesity and obesity-related diseases reaching epidemic proportions (Nguyen et al. 2017; McLaughlin et al. 2004). Genetic background has been identified as the main cause of metabolic diseases along with environmental influences such as excessive food intake and the lack of physical activity (Baudrand et al. 2015; Haluzik et al. 2004). However, these conditions by alone cannot account for the current disease trends leading to hypothesize that other players could take part to the pathogenesis of metabolic diseases. Over recent years a class of chemicals that could interfere with metabolic processes has been identified. These compounds identified as obesogenic endocrine disruptors or “obesogens” include compounds to which the human population is daily exposed through their use in pesticides/herbicides, industrial and household products, plastics, detergents, flame retardants and as ingredients in personal care products (Thayer et al. 2012). Of particular concern is the evidence that the exposure of organs involved in the regulation of metabolisms, such as adipose tissue, pancreas and liver, to metabolic disruptors during utero or neonatal period may have a more detrimental effect compared to the exposure during adulthood (Waalen 2014). This review will summarize the current knowledge on obesogenic endocrine disruptors that may contribute to the pathogenesis of obesity through interfering with regulatory processes in metabolism and in the control of adipocyte function.
Basic evidence
In 2006, Grun and Blumber identified the existence of chemicals that could interfere with energy balance encouraging weight gain and obesity (Grün and Blumberg 2006). These disruptors were called “obesogens” and they have been reported to increase the susceptibility to weight gain in exposed individuals. The mechanisms through which the obesogens act have been identified in the increased adipogenesis and/or the increased storage in preexisting fat cells (Janesick and Blumberg 2011). Further, obesogens could also act indirectly through the change of gut microbiota, by altering basal metabolic rate and hormonal control of appetite and satiety (Lagisz et al. 2015; Snedeker and Hay 2012). The association between chemicals and obesity has been suggested by several studies. Starting from basic viewpoint, the exposure to tributyltin (TBT) during pregnancy leads to offspring that are heavier than not exposed ones (Grun et al. 2006). TBT is an organotin used as fungicide and it is a retinoid acid X receptor and PPAR-γ agonist (Grun et al. 2006). In the murine 3T3-L1 cell model, TBT has been reported to perturb key regulators of adipogenesis and lipogenic pathways in vivo. Moreover, in utero exposure to TBT leads to strikingly elevated lipid accumulation in adipose depots, liver and testis of neonate mice and results in increased epididymal adipose mass in adults (Grun et al. 2006). At the same manner, the exposure to diethylstilbestrol (DES) during neonatal period resulted in increased body weight. Interestingly, this effect was specific for females and did not appear until 4–6 months. In male mice, the exposure to DES was accompanied by an increased number of adipocytes in the gonadal fat pad of mice (Newbold et al. 2005). Recently, bisphenol A (BPA) has been identified as an endocrine and metabolic disruptor. Its presence is ubiquitous since it is a chemical used to make polycarbonate plastic, epoxy resins that line food and beverage cans, and as developer in cash register receipts (Rubin 2011). The effect of the exposure to BPA is controversial. Somm et al. (2009) reported that the exposure to BPA during pregnancy in rats had a determinant effect on the weight of offspring at weaning, thus suggesting that the exposure to BPA at early life plays a crucial role in determining adult body weight. Yang et al. (2016) demonstrated that the exposure to BPA at increasing doses added to chow diet has been accompanied by an increased body weight and fat mass. This effect seems to be due to the differentiation of white adipocyte progenitors from the stromal vascular fraction, partially through glucocorticoid receptor. Moreover, BPA exposure increased circulating inflammatory factors and the local inflammation in white adipose tissues in both genders and increased circulating inflammatory factors, including leptin and TNFα in lean female subjects but not in male. Phthalates can be found in a variety of products such as cosmetics, shampoos, soaps, lubricants, pesticides and paints. Food is the main tool responsible for the human exposure to phthalates that are often contained in wrapping materials or during the food processing (Wams 1987). Diethylhexyl phthalate (DEHP) has been reported to induce the expression of transcriptional factors peroxisome proliferator-activated receptor (PPAR) gamma, CCAAT/enhancer-binding protein (C/EBP) alpha and sterol regulatory element binding factor 1 (Srebf1) as well as downstream target genes required for adipogenesis in vivo. Further perinatal exposure seems to have detrimental metabolic consequences in the offspring; in fact, body weight, adipose tissue deposition, serum lipids and glucose levels were significantly elevated in offspring at postnatal day 60 (Hao et al. 2013). At the same manner, mono-(2-ethylhexyl) phthalate (MEHP) induced the expression of PPAR-γ as well as its target genes required for adipogenesis in vitro. Moreover, MEHP perturbed key regulators of adipogenesis and lipogenic pathway in vivo. In utero exposure to a low dose of MEHP significantly increased body weight and fat pad weight in male offspring at postnatal day 60. In addition, serum cholesterol, TAG (triacylglycerol) and glucose levels were also significantly elevated (Hao et al. 2012). Polycyclic aromatic hydrocarbons (PAHs) are derived from fossil fuel burning which includes diesel exhaust, air pollution and cigarette smoke (Heindel et al. 2015). The exposure to PAHs leads to increased weight, fat mass and higher PPAR-γ gene expression, fatty acid synthase and adiponectin in mice (Yan et al. 2014). However, exposing adult rats to PAHs resulted in obesity, inflammation and insulin resistance only if they were fed high-fat diet, thus meaning that a second hit is necessary to develop metabolic diseases (Bolton et al. 2014). Further, this detrimental effect was more pronounced in male mice, suggesting that there could be a sexual dimorphic effect (Strakovsky et al. 2015). Female offspring exposed to benzo(a)pyrene during prenatal life developed higher amount of visceral adipose tissue compared to the controls (Ortiz et al. 2013). Persistent organic pollutants (POPs) such as hexachlorobenzene (HCB), DDT and polychlorinated biphenyls may represent a risk of developing obesity later in life (Ghosh et al. 2014). Reduced energy expenditure along with glucose intolerance, dyslipidemia and hyperinsulinemia has been observed in rodents that were exposed to DDT during prenatal life (La Merrill et al. 2014) (Fig. 1).
Summary of mechanism of action of obesogenic endocrine disruptors. Tributyltin (TBT), phthalates, bisphenol A (BPA), diethylstilbestrol (DES), polycyclic aromatic hydrocarbons (PAHs) and organic pollutants (POPs) have been displayed to possess obesogenic properties. The obesogenic activity is due to their ability to increase the number and/or size of fat cells, alter basal metabolic rate and hormones regulating appetite, satiety and food preferences
Clinical evidence
Several human studies suggested an association between obesogens and obesity. Eighty-three human studies have been revised to make the state of the art of the association between smoking and offspring’s outcomes. The maternal smoking has been associated to the predisposition of developing obesity later in life (Behl et al. 2013). Similarly, the prenatal exposure to DES resulted in childhood obesity at age of 7 (Newbold et al. 2009) and increased risk of adult obesity (Kirchner et al. 2010). The American studies reported that over 91% of examined population was exposed to BPA, including children (Newbold et al. 2009). BPA has been identified as a metabolic disruptor that contribute to impair weight regulation, thus promoting obesity and obesity-related complications such as insulin resistance, dyslipidemia, hypertension and peripheral arterial disease (Ropero et al. 2008; Hugo et al. 2008; Shankar and Teppala 2011; Silver et al. 2011; Shankar and Teppala 2012; Shankar et al. 2012a). NHANES 2003–2006 study demonstrated that urinary BPA was associated with general and central obesity. After multivariate adjustments, participants of the three upper quartiles had 39–62% higher odds of being abdominally obese compared to the lowest BPA quartile participants (Carwile and Michels 2011). A direct correlation of urinary BPA level and both BMI and waist circumference has been found in another cross-sectional study based on NHANES 2003–2008 cycle data (Shankar et al. 2012b). This association was not reported only in adulthood but also in childhood. In fact, higher urinary BPA concentrations were detected in children aged 6–11 based on Canadian Health Measure Survey 2007–2009 data (Bushnik et al. 2010).
Moreover, in the cross-sectional study in the children from 2003 to 2004, 2005 to 2006, and 2007 to 2008 NHANES cycles statistically significant direct correlation was found between urinary BPA levels and BMI in gender and age adjusted models of the whole population and in non-Hispanic white boys, while non-significant among other subgroups (Bhandari et al. 2013). After multivariate adjustments of NHANES 2003–2008 data, the three upper quartiles had 10–22% higher odds of being obese compared to the lowest BPA quartile but only among the white race participants the positive statistical association remained after dividing in subgroups (Trasande et al. 2012). A study based on the data pooled from the NHANES 2003–2010 cycles for children reported higher odds of being obese and having an abnormal waist circumference-to-height ratio in three upper quartiles in comparison with the first one (Eng et al. 2013). The same results were achieved in China where a study was conducted in school-age children reporting that the increased BPA levels among female students entering puberty (9–12 years) increased the risk of developing obesity (Li et al. 2013). Similarly, high levels of urinary BPA have been detected in the obese group of Chinese children (8–15 years) (Wang et al. 2012).
However, negative associations have been also reported between BPA and obesity in studies performed in India and US. These latter should be discussed carefully due to the small sample size that could interfere with the final results (Xue et al. 2015; Wolff et al. 2007).
Phthalates are one of the most studied metabolic disruptors. Several observational studies suggested that phthalates could be determinant in the pathogenesis of obesity. Most of the results come from the NHANES studies and surveys carried out in the USA to obtain a random sample of the civilian noninstitutionalized population for a given survey cycle. Several phthalate metabolites mono-butyl phthalate (MBP), mono-benzylphthalate (MBzP), mono-(2-ethylhexyl) phthalate (MEHP), mono-ethylphthalate (MEP), mono-(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP) and mono-(2-ethyl-5-oxohexyl) phthalate (MEOHP) were investigated in relation to waist circumference (WC) in adult US male enrolled in the National Health and Nutrition Examination Survey (NHANES) 1999–2002. Mono-benzylphthalate (MBzP), mono-(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP), mono-(2-ethyl-5-oxohexyl) phthalate (MEOHP) and mono-ethylphthalate (MEP) levels were closely related to abdominal obesity, thus leading to hypothesize that they could contribute to the pathogenesis of abdominal obesity (Stahlhut et al. 2007). However, the limit of this study was that only males were included while Hatch et al. (2008) subsequently analyzed the same NHANES database but taking into account both genders. The endpoints of interest in Hatch’s study were BMI and WC. They found that MBzP, MEOHP, MEHHP, MEP and MBP correlated to BMI and WC in males aged 20–59 while MEP correlated to BMI and WC in adolescent girls (Stahlhut et al. 2007). Based on the 2003–2008 National Health and Nutrition Examination Survey, a cross-sectional analysis of 2884 children (aged 6–19 years) was conducted (Trasande et al. 2013a, b). The endpoints of interest were 2000 CDC reference-based BMI z-scores and binary variables of overweight and obesity that were defined using BMI z-score cutoffs of 85th and 95th percentile, respectively. The interesting result was that the association between anthropometric measures and phthalate metabolites is race/ethnicity specific. In fact, each log unit increase in low molecular weight metabolites was associated with 21 and 22% increases in odds (95% CI 1.05–1.39 and 1.07–1.39, respectively) of overweight and obesity, and a 0.090-SD unit increase in BMI z-score (95% CI 0.003–0.18), among non-Hispanic blacks but not in other racial/ethnic subgroup (Trasande et al. 2013a, b). Lind et al. (2012) assessed data from the Prospective Investigation of the Vasculature in Uppsala Seniors (PIVUS) study aiming to investigate the association between circulating concentrations of phthalates and indices of obesity. Serum phthalate metabolites levels were assessed at baseline, and dual-energy X-ray absorptiometry (DXA) and abdominal magnetic resonance imaging (MRI) assessments were performed 2 years later. The results of Lind et al. were presented separately by gender. In women, mono-isobutyl phthalate MiBP (mono-isobutyl phthalate) levels were positively correlated with WC, total fat mass and trunk fat mass assessed by DXA, as well as to subcutaneous adipose tissue assessed by MRI while monomethyl phthalate (MMP) concentrations were related to trunk fat mass and the trunk/leg ratio assessed by DXA, although this association was less powerful than the association with MiBP. This association was not confirmed in males. Since exposure assessment was performed 2 years before the outcome ascertainment, this study could not be considered as a truly longitudinal study; thus, the follow-up status of participants could not correspond to the status at baseline. In contrast to phthalates, limited data in humans are available regarding the association between TBT and obesity. The placental levels of TBT seem to be determinant for the onset of obesity only during the first three months of life while this association was not significant for the other periods of life (Rantakokko et al. 2015). At the same way, limited data are currently available regarding to the association of PAHs and obesity. Rundle et al. (2012) found that higher body weight both at 5 and 7 years of age was associated to PAHs exposure during prenatal life. At the same way, the exposure to POPs during prenatal life is associated with rapid growth in the first 6 months of life and obesity in infancy and childhood (Valvi et al. 2014; Diamanti-Kandarakis et al. 2009). Both the Endocrine Society and United States Environmental Protection Agency identified several endocrine disruptors that could interfere with weight control such as BPA, DES, organotin compounds, such as TBT and triphenyltin and phytoestrogens. They concluded that the dangerous effect of these compounds is more severe when it happens in perinatal time. They encouraged screening tests and research programs to draw final recommendation on endocrine disruptor exposure (https://www.epa.gov/endocrine-disruption; Smink et al. 2008). In conclusion, data regarding the association of chemicals with obesity are of little high quality. This is due to the fact that chemicals have often short physiologic half-lives; thus, the single measurement performed in most of the studies cannot provide information on long-term exposure. Further, since chemicals have a large number of metabolites and the investigators that conducted studies on chemicals measured not the effects of the same metabolites, it is hard to get a comparison of the results across the studies. Moreover, the majority of the studies are based upon population-based surveys or pharmacovigilance studies, i.e., studies that were not designed to address the effect of chemicals on obesity.
Mechanism of action of obesogens
Obesogens play an important role in the onset of obesity acting through several pathways that promote adipogenesis and lipid accumulation. Usually the exposure to obesogens during prenatal life resulted in an increasing number of adipocytes. The main mechanism involved in adipogenesis acts through PPAR-γ function. TBT has been reported to bind RXR–PPAR-γ heterodimer promoting adipogenesis (Grün et al. 2006; Kanayama et al. 2005; Kirchner et al. 2010). Masuno et al. (2002) reported that BPA accelerated the conversion of 3T3-L1 fibroblasts when incubated with insulin. Mono-(2-ethylhexyl) phthalate (MEHP) has been found to directly activate PPARgamma and promote adipogenesis inducing a selective activation of different PPARgamma target genes (Masuno et al. 2002). Benzyl butyl phthalate (BBP) promoted the differentiation of 3T3-L1 through the activation of the adipogenic pathway and metabolic disturbances. In particular, BBP significantly induced mRNA expression of transcriptional factors C/EBPα and PPARγ, their downstream genes, and numerous adipogenic proteins in a dose and time-dependent manner. Furthermore, GC/MC metabolomic analysis revealed that BBP exposure perturbed the metabolic profiles that are associated with glyceroneogenesis and fatty acid synthesis (Feige et al. 2007). Parabens also have been reported to promote adipogenesis (or adipocyte differentiation) in murine 3T3-L1 cells, as revealed by adipocyte morphology, lipid accumulation, and mRNA expression of adipocyte-specific markers. Further, the adipogenic potency of parabens is increased with increasing length of the linear alkyl chain (Yin et al. 2016). Another mechanism that has been hypothesized to be involved in the pathogenesis of obesity by obesogens is the alteration of appetite, satiety and food preferences. BPA may exert its effects through developmental programming of the hypothalamic melanocortin circuitry, permanently altering the neurobiology of metabolic homeostasis. In fact, both male and female BPA-exposed mice showed a reduced density of pro-opiomelanocortin (POMC) projections into the paraventricular nucleus of the hypothalamus (PVN). BPA-exposed pups had, respectively, delayed and blunted postnatal leptin surges, and POMC projections into the PVN were rescued in female BPA-exposed animals given daily injections of supplemental leptin (Hu et al. 2013). In humans, BPA was associated positively with adiponectin and leptin but negatively with ghrelin, following adjustments for sex, height, fat mass, lean mass, smoking, alcohol consumption, physical activity, energy intake and educational levels (MacKay et al. 2017). In 3T3-L1, adipocytes differentiated in the presence of BPA mRNA levels of leptin, interleukin 6 (IL6) and interferon gamma (IFNgamma) were significantly increased (Rönn et al. 2014). Further, methylparaben exposure by daily oral gavage (100 mg/kg/day) increased adiposity and serum leptin levels compared to the controls when fed the chow diet (Ariemma et al. 2016). Both leptin and ghrelin are secreted both by adipose tissue and regulate hunger, with leptin being inhibitory and ghrelin being stimulatory. An interesting hypothesis is based on the fact that obesogens could trigger a vicious pathological cycle. In fact, obesogens could promote the onset of obesity. In turn, obesity is characterized by an increased amount of adipose tissue that could act as reservoir for obesogens that it is well known to have lipophilic properties. The prolonged exposure to obesogens could result in an increased development of metabolic diseases. Further, obesogens could also have a local toxicity. Some xenobiotics have been reported to form fatty acid conjugates at adipose tissue level (Hu et al. 2016). Conjugate mechanism has the aim to increase hydrophilicity and aid to the elimination of toxic substances from the body. Usually, common conjugates are with sulfate, glucuronic acid, glutathione or amino acids, and this result in a negation of biological activity (Ansari et al. 1995). However, sometimes it could happen that this process lead to an enhancement of activity. In fact, although BPA glucuronide loses estrogenic activity, it preserves the ability of promoting adipogenesis (Pugazhendhi et al. 2008). A further consideration is that although adipose tissue could act as reservoir, it could be that not all the adipose tissue could have the same ability to accumulate obesogens. For example, females differ dramatically from male in subcutaneous fat deposition as well as in the endocrine function of adipocytes. These differences could result in a different retention of obesogens according to the specific fat composition laid down in the adipocytes.
Conclusions
The obesogens have a relevant role in the pathogenesis of obesity. Although overeating coupled with the lack of physical activity could play a key role to the onset of obesity, it could be that obesogens could contribute to the predisposition to develop obesity. The strength of this review is to provide the most current evidence on the association between obesogens and obesity although there are several limits of the reported studies that prevent to draw final conclusion. This could be due to the fact that most of the studies were retrospective and were not designed aiming to investigate the association between obesogens and obesity. Further, they provide a proxy evaluation of obesogens that could not be a parameter to assess the chronic exposure. Thus, it will be mandatory to perform randomized clinical trials to assess to the link between suspected obesogens and obesity and to take political action to make the population aware about the exposure to obesogens. Since the effect of exposure to obesogens is expected to increase, future work mandate investigations into the specific disease-promoting mechanisms by which these toxicants work to devise targeted interventions to stem the global tide of metabolic deterioration.
References
Ansari GAS, Bhupendra S, Kaphalia M et al (1995) Fatty acid conjugates of xenobiotics. Toxicol Lett 75:1–17. doi:10.1016/0378-4274(94)03171-3
Ariemma F, D’Esposito V, Liguoro D, Oriente F, Cabaro S, Liotti A et al (2016) Low-dose bisphenol-A impairs adipogenesis and generates dysfunctional 3T3-L1 adipocytes. PLoS One 11:e0150762. doi:10.1371/journal.pone.0150762
Baudrand R, Goodarzi MO, Vaidya A, Underwood PC, Williams JS, Jeunemaitre X et al (2015) A prevalent caveolin-1 gene variant is associated with the metabolic syndrome in Caucasians and Hispanics. Metabolism 64(12):1674–1681
Behl M, Rao D, Aagaard K, Davidson TL, Levin ED, Slotkin TA et al (2013) Evaluation of the association between maternal smoking, childhood obesity, and metabolic disorders: a national toxicology program workshop review. Environ Health Perspect 121:170–180. doi:10.1289/ehp.1205404
Bhandari R, Xiao J, Shankar A (2013) Urinary bisphenol A and obesity in U.S. children. Am J Epidemiol 177:1263–1270. doi:10.1093/aje/kws391
Bolton JL, Auten RL, Bilbo SD (2014) Prenatal air pollution exposure induces sexually dimorphic fetal programming of metabolic and neuroinflammatory outcomes in adult offspring. Brain Behav Immun 37:30–44. doi:10.1016/j.bbi.2013.10.029
Bushnik T, Haines D, Levallois P, Levesque J, Van Oostdam J, Viau C (2010) Lead and bisphenol A concentrations in the Canadian population. Health Rep 21:7–18
Carwile JL, Michels KB (2011) Urinary bisphenol A and obesity: nHANES 2003–2006. Environ Res 111:825–830. doi:10.1016/j.envres.2011.05.014
Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, Hauser R, Prins GS, Soto AM, Zoeller RT, Gore AC (2009) Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr Rev 30(4):293–342
Li DK, Miao M, Zhou Z, Wu C, Shi H, Liu X et al (2013) Urine bisphenol-A level in relation to obesity and overweight in school-age children. PLoS One 8:e65399. doi:10.1371/journal.pone.0065399s
Eng DS, Lee JM, Gebremariam A, Meeker JD, Peterson K, Padmanabhan V (2013) Bisphenol A and chronic disease risk factors in US children. Pediatrics 132:e637–e645. doi:10.1542/peds.2013-0106
Feige JN, Gelman L, Rossi D, Zoete V, Métivier R, Tudor C, Anghel SI, Grosdidier A, Lathion C, Engelborghs Y, Michielin O, Wahli W, Desvergne B (2007) The endocrine disruptor monoethyl-hexyl-phthalate is a selective peroxisome proliferator-activated receptor gamma modulator that promotes adipogenesis. J Biol Chem 282:19152–19166
Ghosh S, Murinova L, Trnovec T, Loffredo CA, Washington K, Mitra PS et al (2014) Biomarkers linking PCB exposure and obesity. Curr Pharm Biotechnol 15:1058–1068
Grün F, Blumberg B (2006) Environmental obesogens: organotins and endocrine disruption via nuclear receptor signaling. Endocrinology 147:S50–S55. doi:10.1210/en.2005-1129
Grün F, Watanabe H, Zamanian Z, Maeda L, Arima K, Cubacha R et al (2006) Endocrine-disrupting organotin compounds are potent inducers of adipogenesis in vertebrates. Mol Endocrinol 20:2141–2155. doi:10.1210/me.2005-0367
Haluzik M, Colombo C, Gavrilova O, Chua S, Wolf N, Chen M et al (2004) Genetic background (C57BL/6J versus FVB/N) strongly influences the severity of diabetes and insulin resistance in ob/ob mice. Endocrinology 145:3258–3264. doi:10.1210/en.2004-0219
Hao C, Cheng X, Xia H, Ma X (2012) The endocrine disruptor mono-(2-ethylhexyl)phthalate promotes adipocyte differentiation and induces obesity in mice. Biosci Rep 32:619–629. doi:10.1042/BSR20120042
Hao C, Cheng X, Guo J, Xia H, Ma X (2013) Perinatal exposure to diethyl-hexyl-phthalate induces obesity in mice. Front Biosci (Elite Ed) 5:725–733
Hatch EE, Nelson JW, Qureshi MM, Weinberg J, Moore LL et al (2008) Association of urinary phthalate metabolite concentrations with body mass index and waist circumference: a cross-sectional study of NHANES data, 1999–2002. Environ Health 7:27. doi:10.1186/1476-069X-7-27
Heindel JJ, Newbold R, Schug TT (2015) Endocrine disruptors and obesity. Nat Rev Endocrinol 11:653–661. doi:10.1038/nrendo.2015.163
Hu P, Chen X, Whitener RJ, Boder ET, Jones JO, Porollo A et al (2013) Effects of parabens on adipocyte differentiation. Toxicol Sci 131:56–70. doi:10.1093/toxsci/kfs262
Hu P, Kennedy RC, Chen X, Zhang J, Shen CL, Chen J, Zhao L (2016) Differential effects on adiposity and serum marker of bone formation by post-weaning exposure to methylparaben and butylparaben. Environ Sci Pollut Res Int 23:21957–21968
Hugo ER, Brandebourg TD, Woo JG, Loftus J, Alexander JW, Ben-Jonathan N (2008) Bisphenol A at environmentally relevant doses inhibits adiponectin release from human adipose tissue explants and adipocytes. Environ Health Perspect 116:1642–1647. doi:10.1289/ehp.1153749
Janesick A, Blumberg B (2011) Endocrine disrupting chemicals and the developmental programming of adipogenesis and obesity. Birth Defects Res C Embryo Today 93:34–50. doi:10.1002/bdrc.20197
Kanayama T, Kobayashi N, Mamiya S, Nakanishi T, Nishikawa J (2005) Organotin compounds promote adipocyte differentiation as agonists of the peroxisome proliferator-activated receptor gamma/retinoid X receptor pathway. Mol Pharmacol 67:766–774. doi:10.1124/mol.104.008409
Kirchner S, Kieu T, Chow C, Casey S, Blumberg B (2010) Prenatal exposure to the environmental obesogen tributyltin predisposes multipotent stem cells to become adipocytes. Mol Endocrinol 24:526–539. doi:10.1210/me.2009-0261
La Merrill M, Karey E, Moshier E, Lindtner C, La Frano MR, Newman JW et al (2014) Perinatal exposure of mice to the pesticide DDT impairs energy expenditure and metabolism in adult female offspring. PLoS One 9:e103337. doi:10.1371/journal.pone.0103337
Lagisz M, Blair H, Kenyon P, Uller T, Raubenheimer D, Nakagawa S (2015) Littleappetite for obesity: meta-analysis of the effects of maternal obesogenic diets on offspring food intake and body mass in rodents. Int J Obes (Lond) 39:1669–1678. doi:10.1038/ijo.2015.160
Lind PM, Roos V, Rönn M, Johansson L, Ahlström H, Kullberg J et al (2012) Serum concentrations of phthalate metabolites are related to abdominal fat distribution two years later in elderly women. Environ Health 11:21. doi:10.1186/1476-069X-11-21
MacKay H, Patterson ZR, Abizaid A (2017) Perinatal exposure to low-dose bisphenol-A disrupts the structural and functional development of the hypothalamic feeding circuitry. Endocrinology 158:768–777. doi:10.1210/en.2016-1718
Masuno H, Kidani T, Sekiya K, Sakayama K, Shiosaka T, Yamamoto H et al (2002) Bisphenol A in combination with insulin can accelerate the conversion of 3T3-L1fibroblasts to adipocytes. J Lipid Res 43:676–684
McLaughlin T, Allison G, Abbasi F, Lamendola C, Reaven G (2004) Prevalence of insulin resistance and associated cardiovascular disease risk factors among normal weight, overweight, and obese individuals. Metabolism 53(4):495–499
Newbold RR, Padilla-Banks E, Snyder RJ, Jefferson WN (2005) Developmental exposure to estrogenic compounds and obesity. Birth Defects Res A Clin Mol Teratol 73:478–480. doi:10.1002/bdra.20147
Newbold RR, Padilla-Banks E, Jefferson WN (2009) Environmental estrogens andobesity. Mol Cell Endocrinol 304:84–89. doi:10.1016/j.mce.2009.02.024
Nguyen QC, Meng H, Li D, Kath S, McCullough M, Paul D et al (2017) Social media indicators of the food environment and state health outcomes. Public Health 148:120–128. doi:10.1016/j.puhe.2017.03.013
Ortiz L, Nakamura B, Li X, Blumberg B, Luderer U (2013) In utero exposure to benzo[a]pyrene increases adiposity and causes hepatic steatosis in female mice, and glutathione deficiency is protective. Toxicol Lett 223:260–267. doi:10.1016/j.toxlet.2013.09.017
Pugazhendhi D, Watson KA, Mills S, BottingN Pope GS, Darbre PD (2008) Effect of sulphation on the oestrogen agonist activity of the phytoestrogens genistein and daidzein in MCF-7 human breast cancer cells. J Endocrinol 197:503–515. doi:10.1677/JOE-07-0384
Rantakokko M, Iwarsson S, Portegijs E, Viljanen A, Rantanen T (2015) Associationsbetween environmental characteristics and life-space mobility in community-dwelling older people. J Aging Health 27:606–621. doi:10.1177/0898264314555328
Rönn M, Lind L, Örberg J, Kullberg J, Söderberg S, Larsson A et al (2014) Bisphenol A is related to circulating levels of adiponectin, leptin and ghrelin, but not to fat mass or fat distribution in humans. Chemosphere 112:42–48. doi:10.1016/j.chemosphere.2014.03.042
Ropero AB, Alonso-Magdalena P, García-García E, Ripoll C, Fuentes E, Nadal A (2008) Bisphenol-A disruption of the endocrine pancreas and blood glucose homeostasis. Int J Androl 31:194–200
Rubin BS (2011) Bisphenol A: an endocrine disruptor with widespread exposure and multiple effects. J Steroid Biochem Mol Biol 127:27–34. doi:10.1016/j.jsbmb.2011.05.002
Rundle A, Hoepner L, Hassoun A, Oberfield S, Freyer G, Holmes D et al (2012) Association of childhood obesity with maternal exposure to ambient air polycyclic aromatic hydrocarbons during pregnancy. Am J Epidemiol 175:1163–1172. doi:10.1093/aje/kwr455
Shankar A, Teppala S (2011) Relationship between urinary bisphenol A levels and diabetes mellitus. J Clin Endocrinol Metab 96:3822–3826. doi:10.1210/jc.2011-1682
Shankar A, Teppala S (2012) Urinary bisphenol A and hypertension in a multiethnic sample of US adults. J Environ Public Health 2012:481641. doi:10.1155/2012/481641
Shankar A, Teppala S, Sabanayagam C (2012a) Bisphenol a and peripheral arterial disease: results from the NHANES. Environ Health Perspect 120:1297–1300. doi:10.1289/ehp.1104114
Shankar A, Teppala S, Sabanayagam C (2012b) Urinary bisphenol a levels and measures of obesity: results from the national health and nutrition examination survey 2003–2008. ISRN Endocrinol 2012:965243. doi:10.5402/2012/965243
Silver MK, O’Neill MS, Sowers MR, Park SK (2011) Urinary bisphenol A and type-2 diabetes in U.S. adults: data from NHANES 2003-2008. PLoS One 6:e26868. doi:10.1371/journal.pone.002686851
Smink A, Ribas-Fito N, Garcia R, Torrent M, Mendez MA, Grimalt JO et al (2008) Exposure to hexachlorobenzene during pregnancy increases the risk of overweight in children aged 6 years. Acta Paediatr 97:1465–1469. doi:10.1111/j.1651-2227.2008.00937.x
Snedeker SM, Hay AG (2012) Do interactions between gut ecology and environmental chemicals contribute to obesity and diabetes? Environ Health Perspect 120:332–339. doi:10.1289/ehp.1104204
Somm E, Schwitzgebel VM, Toulotte A, Cederroth CR, Combescure C, Nef S et al (2009) Perinatal exposure to bisphenol a alters early adipogenesis in the rat. Environ Health Perspect 117:1549–1555. doi:10.1289/ehp.11342
Stahlhut RW, Van Wijngaarden E, Dye TD, Cook S, Swan SH (2007) Concentrations of urinary phthalate metabolites are associated with increased waist circumference and insulin resistance in adult U.S. males. Environ Health Perspect 115:876–882. doi:10.1289/ehp.9882
Strakovsky RS, Lezmi S, Shkoda I, Flaws JA, Helferich WG, Pan YX (2015) In utero growth restriction and catch-up adipogenesis after developmental di(2-ethylhexyl) phthalate exposure cause glucose intolerance in adult male rats following a high-fat dietary challenge. J Nutr Biochem 26:1208–1220. doi:10.1016/j.jnutbio.2015.05.012
Thayer KA, Heindel JJ, Bucher JR, Gallo MA (2012) Role of environmental chemicals in diabetes and obesity: a National Toxicology Program workshop review. Environ Health Perspect 120:779–789. doi:10.1289/ehp.1104597
Trasande L, Attina TM, Blustein J (2012) Association between urinary bisphenol A concentration and obesity prevalence in children and adolescents. JAMA 308:1113–1121. doi:10.1001/2012.jama.11461
Trasande L, Attina TM, Sathyanarayana S, Spanier AJ, Blustein J (2013a) Race/ethnicity-specific associations of urinary phthalates with childhood body mass in a nationally representative sample. Environ Health Perspect 121:501–506. doi:10.1289/ehp.1205526
Trasande L, Sathyanarayana S, Spanier AJ, Trachtman H, AttinaTM Urbina EM (2013b) Urinary phthalates are associated with higher blood pressure in childhood. J Pediatr 163(747–53):e1. doi:10.1016/j.jpeds.2013.03.072
Valvi D, Mendez MA, Garcia-Esteban R, Ballester F, Ibarluzea J, Goñi F et al (2014) Prenatalexposure to persistent organic pollutants and rapid weight gain and overweight ininfancy. Obesity (Silver Spring) 22:488–496. doi:10.1002/oby.20603
Waalen J (2014) The genetics of human obesity. Transl Res 164:293–301. doi:10.1016/j.trsl.2014.05.010
Wams TJ (1987) Diethylhexylphthalate as an environmental contaminant—a review. Sci Total Environ 66:1–16
Wang HX, ZhouY Tang CX, Wu JG, Chen Y, Jiang QW (2012) Association between bisphenol A exposure and body mass index in Chinese school children: a cross-sectional study. Environ Health 11:79. doi:10.1186/1476-069X-11-79
Wolff MS, Teitelbaum SL, WindhamG Pinney SM, Britton JA, Chelimo C et al (2007) Pilot study of urinary biomarkers of phytoestrogens, phthalates, and phenols in girls. Environ Health Perspect 115:116–121
Xue J, Wu Q, Sakthivel S, Pavithran PV, Vasukutty JR, Kannan K (2015) Urinary levels of endocrine-disrupting chemicals, including bisphenols, bisphenol A diglycidyl ethers, benzophenones, parabens, and triclosan in obese and non-obese Indian children. Environ Res 137:120–128. doi:10.1016/j.envres.2014.12.007
Yan Z, Zhang H, Maher C, Arteaga-Solis E, Champagne FA, Wu L et al (2014) Prenatal polycyclic aromatic hydrocarbon, adiposity, peroxisome proliferator-activated receptor (PPAR) γ methylation in offspring, grand-offspring mice. PLoS One 9:e110706. doi:10.1371/journal.pone.0110706
Yang M, Chen M, Wang J, Xu M, Sun J, Ding L et al (2016) Bisphenol A promotes adiposity and inflammation in a nonmonotonic dose-response way in 5-week-old male and female C57BL/6J mice fed a low-calorie diet. Endocrinology 157:2333–2345. doi:10.1210/en.2015-1926
Yin L, Yu KS, Lu K, Yu X (2016) Benzyl butyl phthalate promotes adipogenesis in3T3-L1 preadipocytes: a high content cellomics and metabolomic analysis. Toxicol In Vitro 32:297–309. doi:10.1016/j.tiv.2016.01.010
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest, neither any grants nor other financial supports regarding the publication of this article.
Rights and permissions
About this article
Cite this article
Muscogiuri, G., Barrea, L., Laudisio, D. et al. Obesogenic endocrine disruptors and obesity: myths and truths. Arch Toxicol 91, 3469–3475 (2017). https://doi.org/10.1007/s00204-017-2071-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-017-2071-1