Abstract
Green tea (GT), obtained from the leaves of Camellia sinensis (L.) Kuntze (Fam. Theaceae), is largely used for its potential health benefits such as reduction in risk of cardiovascular diseases and weight loss. Nevertheless, it is suspected to induce liver damage. Present work reviews the hepatic adverse reactions associated with GT-based herbal supplements, published by the end of 2008 to March 2015. A systematic research was carried out on PubMed, MedlinePlus, Scopus and Google Scholar databases, without any language restriction. Moreover, some accessible databases on pharmacovigilance or phytovigilance were consulted. The causality assessment was performed using the CIOMS/RUCAM score. Nineteen cases of hepatotoxicity related to the consumption of herbal products containing GT were identified. The hepatic reactions involved mostly women (16/19); the kind of liver damage was generally classified as hepatocellular (16/19). The causality assessment between consumption of herbal preparation and hepatic reaction resulted as probable in eight cases and as possible in eleven cases. In seven cases, patients used preparations containing only GT, while twelve reactions involved patients who took multicomponent preparations (MC). The reactions induced by GT had a generally long latency (179.1 ± 58.95 days), and the outcome was always resolution, with recovery time of 64.6 ± 17.78 days. On the contrary, liver injury associated with MC had a shorter latency (44.7 ± 13.85 days) and was more serious in four cases that required liver transplantation and, when resolution occurred, the recovery time was longer (118.9 ± 38.79). MC preparations contained numerous other components, many of which are suspected to induce liver damage, so it is difficult to ascribe the toxicity to one specific component, e.g., GT. Present data confirm a certain safety concern with GT, even if the number of hepatic reactions reported is low considering the great extent of use of this supplement. The mechanism of GT hepatotoxicity remains unclear, but factors related to the patient are becoming predominant. A major safety concern exists when GT is associated with other ingredients that can interact between them and with GT, enhancing the risk of liver damage. Patients should be discouraged from using herbal or dietary supplements containing complex mixtures and should be encouraged to use herbal and dietary supplement possibly under supervision of healthcare professionals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tea is a universal beverage consumed by billions of people around the world since thousands of years owing to its aroma, taste and health-promoting properties. It is prepared by infusion from the leaves of Camellia sinensis (L.) Kuntze (Fam. Theaceae). Depending on the postharvest processing treatment, particularly the “degree of fermentation,” several commercial types of tea can be obtained, which differ in terms of flavor, color and composition (Dias et al. 2014; Wu et al. 2014; Tenore et al. 2015). The term “fermentation” refers to how much a tea is allowed to undergo enzymatic oxidation. Classically, the most known types of tea are: black tea (fully fermented), oolong tea (semifermented) and green tea (unfermented). To produce black tea, leaves are allowed to wither for about 20 h, rolled, fermented in a humid atmosphere and then dried with hot air. Oolong tea is only partially fermented. To produce green tea, freshly harvested leaves are stabilized by dry heating or steaming to inactivate polyphenol oxidase enzymes and then rolled and dried rapidly. More recently, special attention is drawn to white tea, which is now worldwide on the market. White tea is prepared from young leaves or buds, harvested before being fully opened; the leaflets, covered by silvery hairs, are picked and allowed to wither lightly before being dried; during the withering, a very light fermentation occurs (Dias et al. 2014; Tenore et al. 2015).
Black tea is the type of tea most largely consumed worldwide (about 80 % of the market) and is very popular in North America and Europe: Green tea is mainly consumed in China and Japan. White tea is the rarest and the least handled tea.
Besides methylxanthine alkaloids (caffeine, theophylline, theobromine), the polyphenols are considered the major bioactive molecules of tea (up to 30 % of tea leaf dry weight), among which are the catechins epigallocatechin-3-gallate (EGCG), epicatechin (EC), epicatechin-3-gallate (ECG) and epigallocatechin (EGC). EGCG is the most abundant (up to 50 % of total polyphenols) and possesses the highest antioxidant potential, so it is considered the most biologically active substance. The high catechin levels have been indicated as the base of the tea antioxidant properties and its protective role in pathological conditions caused by reactive oxygen species, such as cancer, cardiovascular and neurological diseases (Rietveld and Wiseman 2003). During fermentation, catechins undergo oxidization by polyphenol oxidase so they are transformed into theaflavins and thearubigins, condensed polymeric compounds, considered responsible for the typical organoleptic characteristics (taste and color) of black tea. Green tea is the major source of catechins, although it is suggested that white tea presents higher levels of antioxidants than green tea (Dias et al. 2014).
In the last decade, the consumption of tea, particularly green tea, has been largely increased for its reputed health benefits (obesity, diabetes mellitus, cardiovascular disorders, cancer and neurodegenerative diseases) even if the preventive effect of tea has not been confirmed yet (Butt et al. 2015; Keske et al. 2015; Wierzejska 2014; Wang et al. 2014). Green tea use is encouraged by a myriad of Internet Web sites and by the over-the-counter availability of a large variety of green tea products on Internet as well as on health food stores. Based on reputed healthy properties, today green tea is marketed in the form of innumerable herbal supplements, whose composition differs largely for content in catechins.
As the consumption of green tea increased, some safety issues appeared. Particularly, green tea has been associated with hepatotoxic reactions, mainly when used for the weight control (Mazzanti et al. 2009; Sarma et al. 2008). In this context, a green tea preparation, Exolise® (Arkopharma, Carros, France), marketed as herbal supplement for weight loss, was withdrawn in 2003 after 13 cases of hepatotoxicity due to its consumption (Gloro et al. 2005). After this, the US Pharmacopoeia (USP) Dietary Supplement Information Expert Committee (DSI EC) systematically reviewed the safety information for green tea products in order to re-evaluate the current safety class to which these products were assigned (Sarma et al. 2008). As a result of this safety review, DSI EC decided to assign to green tea extract a Class 2 safety (Articles for which the DSI EC is unaware of significant safety issues that would prohibit monograph development when the article is used and formulated appropriately, provided there is a warning statement in the labelling section). As labelling statement was suggested, “Take with food. Discontinue use and consult a healthcare practitioner if you have a liver disorder or develop symptoms of liver trouble such as abdominal pain, dark urine, or jaundice” (Sarma et al. 2008). However, after reviewing additional information, in June 2008, the DSI EC decides to defer approval of this cautionary labelling requirement (Update on the USP Green Tea Extract Monograph; www.usp.org/usp-nf/notices/retired-compendial-notices/update-usp-green-tea-extract-monograph). In May 2009, Hydroxycut®, a multi-ingredient herbal supplement containing green tea along with other components, had issued a public recall and a health advisory by FDA (FDA Warns Consumers to Stop Using Hydroxycut Products; www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149575.htm), owing to a case series of hepatotoxicity. Despite this, other green tea-based supplements appeared on the market, sometimes near identically to those withdrawn and other case reports of liver damage after consumption of green tea appeared in the literature.
Aim of the present work was to review the green tea hepatotoxicity on the basis of the more recent literature data.
Methods
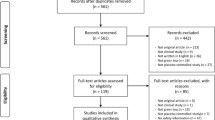
A systematic research of case reports of hepatotoxicity induced by green tea and its preparations was carried out on PubMed, MedlinePlus, Scopus and Google Scholar databases using the key words: green tea, C. sinensis, catechins, epigallocatechin gallate, EGCG, polyphenols, herbal supplements, dietary supplements and herbal medicine. Each term was matched with the key words typical for liver damage: hepatotoxicity, liver failure, liver injury, liver damage, hepatitis, hepatic necrosis, hepatic fibrosis, cirrhosis and cholestasis. Moreover, some accessible databases on pharmacovigilance or phytovigilance such as RELIS (http://relis.arnett.no/Utredning_Ekstern.aspx?Relis=3&S=4390&R=X) were examined. The search started from November 2008 (because we desired to update our previous work on green tea hepatotoxicity, Mazzanti et al. 2009) and extended to March 2015, without any language restriction. Cases of hepatotoxicity induced by Hydroxycut® published in this period (Fong et al. 2010; Sharma et al. 2010; Kaswala et al. 2014; Haimowitz et al. 2015) were not included in this review, owing to the withdrawal of the product from the market in July 2009; nevertheless, they have been mentioned in the Discussion section.
All papers selected were retrieved and carefully examined to perform a causality assessment between herbal supplement ingestion and liver injury. A causality assessment process that is specific for herbal-induced liver injury has not been developed, so a variety of scales can be used (Teschke et al. 2008). We chose the CIOMS/RUCAM score (Danan and Benichou 1993; Benichou et al. 1993) that assigns points to specific categories. It is a well-standardized method used in the assessment of drug-induced liver injuries which has been applied to both drugs and dietary supplement (Chalasani et al. 2008). To classify the type of liver injury and then to calculate the RUCAM score, the upper normal values of alanine aminotransferase (ALT), and alkaline phosphatase (ALP) are needed. However, in our cases the range of normal values of ALT and ALP was described only in few reports, so we used those reported by US National Library of Medicine—NIH—Health Topics (http://www.nlm.nih.gov/medlineplus/healthtopics.html).
Results
In our search, nineteen cases of hepatotoxicity related to the consumption of herbal products containing green tea were identified. The hepatic reactions involved mostly females (16/19 = 84 %), between 24 and 63 years old; males (3/19 = 16 %) were between 16 and 76 years old. The characteristics of cases are reported in Table 1.
Green tea preparations used by the patients who experienced a reaction consisted of green tea alone, as infusion or dried leaves (4/19), or its derivatives (simple or decaffeinated extract, water soluble powder: 3/19). In most preparations (12/19), green tea extracts were associated with other components that consist of botanicals, pure phytochemicals, vitamins, amino acids, alkaloids, minerals and others (Table 1).
The reason for use of green tea products, reported in 15/19 cases, dealt mainly with weight loss (six cases) and hair loss (four cases), followed by energy or well-being enhancement and beverage; in one case, a green tea infusion was used even to treat constipation. The duration of treatment was very variable being between 2 days and more than 1 year. The latency of the reaction varied within a broad range too: from 14 days to more than 1 year. All patients presented symptoms that required hospitalization; they consist of jaundice, malaise, fatigue, abdominal pain, nausea, vomiting, fever; sometimes discoloration of stool and urine and pruritus were present. The reaction occurred generally during the treatment, but in two cases (4, 5), it happened 14 days after the treatment discontinuation.
Laboratory investigations, reported as mean ± standard error (SE), showed liver enzyme levels several times higher than the upper level of normal (ULN); particularly, ALT were from 3.6 to 96 times ULN (mean 36.9 ± 6.01) and AST from 4.9 to 99 times ULN (mean 35.8 ± 5.84). ALP values ranged from normal (6 cases) to 5.5 times ULN.
The kind of liver damage was classified, according to Danan and Benichou (1993), as hepatocellular in 16/19 cases and as cholestatic in two cases. In case 16 the type of liver injury could not be classified as hepatocellular or cholestatic, owing to the lack of ALP value in the report. However, the causality assessment resulted as possible, when the liver injury was considered both as hepatocellular and cholestatic. Liver biopsy was performed in 15/19 cases and highlighted mostly necrosis (massive, submassive, multifocal or focal) and inflammatory cell infiltrates. In some cases, cholestasis was pointed out. Slight fibrosis was present occasionally.
Serologic tests for viral hepatitis (generally HAV, HBV, HCV, CMV, EBV and sometimes HEV, HSV, HIV) when performed were always negative. Occasionally, on the basis of specific tests, other diseases excluded were hereditary haemochromatosis (cases 2, 3, 14 and 16), Wilson disease (cases 4, 9, 11, 14 and 16), Leishmania infection (case 2) and Toxoplasma infection (case 13). Serology for autoimmune hepatitis, particularly assay for ANA, AMA ASMA and anti-LKM, was within normal values, except for a positivity for ANA antibodies in cases 10 (1:160) and 12 (1:320), for ASMA in cases 17 (1:40) and 19 (1:80) and for ANCA in case 19 (1:160). In most cases (13/19), consumption of green tea was associated with other medications consisting both in conventional drugs (ACE inhibitors, selective serotonin reuptake inhibitors, oral contraceptives, antibiotics, benzodiazepines, calcium antagonists, etc.) and in dietary supplements (vitamins, minerals, fibers, whey protein, GNC Mega Men® Sport, Nopal®, Somalyz®). Pathological conditions predisposing the subject to liver injury were generally excluded, except for a case with previous hepatic steatosis (case 2). Risk factors related to the age were present in six subjects. Abuse of alcohol was always excluded.
Outcome consisted mostly in resolution but four cases of liver transplantation occurred (4, 5, 14 and 16). Recovery occurred mainly between 20 and 90 days, but rapid (5 days) and long-lasting (180 and 540 days) times of recovery were also observed. In some cases (6, 10 and 11), corticoid therapy was required to obtain resolution. Rechallenge was never reported.
The causality assessment between consumption of herbal preparation and hepatic reaction, carried out according to CIOMS/RUCAM method, resulted as probable in eight cases (42 %) and as possible in 11 cases (58 %). It is obvious that when herbal supplement contained green tea in association with other components, the causality assessment concerned the whole supplement and not green tea only.
Other details on adverse reactions are described in Table 1.
Discussion
Consumption of herbal dietary supplements has become a major heath trend in wealthy societies worldwide (Bardia et al. 2007; Cavaliere et al. 2010; Denison et al. 2012). A recent survey (Garcia-Alvarez et al. 2014) carried out in six European countries (Finland, Germany, Italy, Romania, Spain and the United Kingdom) found an usage prevalence rate of herbal supplements of 18.8 %, being the majority of consumers educated to medium level. The rising popularity of herbal dietary supplements probably originates from an increased awareness of consumers toward well-being and health in general and then from the desire to prevent illness by an optimal nutritional status. A relevant reason for the favor these products enjoy with the public is the belief that they are not only effective but also safe because herbal remedies are of natural origin and used for long time (Snyder et al. 2009; Chauhan et al. 2013). This lack of criticism is surprising, particularly as there is no shortage of criticism for conventional medicine. Actually, the efficacy and safety of herbal dietary supplements are questionable for several reasons, first of all because current regulatory framework for natural products differs from that of conventional drugs in that nonclinical and clinical assessments of safety and efficacy are not required to market herbal products, so safety concerns are not known until postmarketing surveillance (Silano et al. 2011; Licata et al. 2013; Ehrenpreis et al. 2013).
In recent years, there is an increasing evidence of adverse reactions to these products (Menniti-Ippolito et al. 2008; Vitalone et al. 2011, 2012; Koncic and Tomczyk 2013; Seeff et al. 2014). Herbal supplements are prone to induce toxicity firstly because of their complexity and variability. They originate from a living organism (the plant) by different steps: harvesting, drying, processing, etc. From a single plant, very different products can be obtained depending on time of harvesting, part of plant used, drying method and extraction procedure. These parameters likely cause batch-to-batch and product-to-product variability in the final product. Other open questions are represented by plant misidentification, contamination and adulteration. Consequently, quality aspects of herbal products should be considered in evaluating their safety and, eventually, their adverse affects.
The liver, by its nature, is an organ prone to suffer toxic effects of xenobiotics. Among drug-induced liver injury cases, herbal and dietary supplements (HDS) are the second most common cause (Chalasani et al. 2008). In the USA, reports from the Drug-Induced Liver Injury Network (DILIN) indicate that HDS are responsible for an increasing proportion of hepatotoxicity cases. Among 109 patients in whom HDS were implicated in their liver injury, most (33 %) used products intended for bodybuilding, followed by products for weight loss (26 %) (Rossi and Navarro 2014).
Green tea, besides its use as beverage, is one of the most widely used herbal supplements. Some studies have shown the potential health benefit associated with green tea consumption (e.g., reduction in risk of cardiovascular diseases and cancer, weight loss), but in the literature, there are also several reports of adverse hepatic reactions associated with green tea.
In our previous review (Mazzanti et al. 2009), 34 cases of hepatotoxicity associated with green tea preparations were identified, including six cases related to Exolise®, which had been withdrawn from the market owing to its hepatotoxicity. Present search identified 19 cases of suspected hepatotoxicity associated with the consumption of green tea-based products.
The assessment causality, carried out by the CIOMS/RUCAM method, resulted in most cases (58 %) as possible and in 42 % as probable. Sometimes the causality level assigned by us on the basis of data described in case reports resulted lower than that assigned by authors; this fact can be due to the different opinion among evaluators that remains a concern with all causality assessment methods (Arimone et al. 2005). However, often the score was penalized by the lack of sufficient information in case reports; just as an example, for case 1, authors describe only results about markers for HBV and HCV without data regarding HAV, HEV and CMV. In the absence of these data, the CIOMS/RUCAM score is 5 so the causality assessment results as possible; conversely, the exclusion of the above viral infections would bring the score to 7 and the causality assessment would result as probable. Furthermore, in several cases (e.g., case 10), the course of liver parameters is not reported: Also this lack decreases the score and then the causality level. Finally, among “non-drug causes,” CIOMS/RUCAM score takes into account also an “acute hypotension history” but this event is never mentioned in cases reports, so it has been considered as not excluded and the score is reduced. These facts highlight the importance of comprehensively evaluating an adverse reaction and of reporting it correctly.
As already specified, seven cases (1, 2, 3,10, 13, 15 and 19) regarded use of preparations containing only green tea or its derivatives, while twelve reactions (4–9, 11, 12, 14, 16–18) involved multicomponent preparations. This point has to be kept in mind to avoid misleading conclusions. In fact, in a multicomponent preparation, each ingredient has its own pharmacological and toxicological profile, inducing desired and undesired effects; moreover, it can interact both with other components of the mixture and with conventional drugs possibly co-administered, leading to unpredictable effects. In these cases, as stated, the causality assessment between herbal supplement and reaction deals with the whole supplement, not with its single ingredients (i.e., green tea). In line with this consideration, the cases involving preparations containing only green tea will be discussed separately from those involving multicomponent preparations.
As regards patients who took only green tea, they consumed infusions (from two cups to three L/day, corresponding to about 186 and 1395 mg polyphenols/die, as calculated according to Arzenton et al. 2014) or its derivatives such as micronized powder (1 g/day catechins) and decaffeinated extract (710 mg/day polyphenols of which 320 mg/day catechins). The latency of the reaction ranged from ten to more than 365 days, being mean ± SE 179.1 ± 58.95, and the outcome was always resolution, with recovery time of 5–120 days (mean 64.6 ± 17.78).
Clinical conditions predisposing to liver damage were absent except for case 2 in which a preexisting hepatic steatosis occurred. Four patients (3, 10, 13 and 19) were taking other medications, some of which are known to be potentially hepatotoxic, among these are anastrozole (Inno et al. 2011; Lacey and Evans 2014; case 3), oral contraceptives (Elouni et al. 2010; case 10), irbesartan (Andrade et al. 2002; case 10), ramipril (Douros et al. 2013; cases 3 and 19) and atorvastatin (Perdices et al. 2014; Chang et al. 2015; case 19). However, in all cases, these medications were consumed since almost 2 years without any side effect, so they cannot be directly related to the hepatic adverse event. In some cases, it has been hypothesized that the consumption of green tea triggered the reaction as, for example, for the autoimmune-like hepatitis reported by Gallo et al. (2013). In this case, the patient, who consumed irbesartan and a combination of gestodene and 17α-ethynilestradiol (besides green tea in dose of 1 g/day catechins), carried various genetic variants, being heterozygote for the CYP3A4 gene IVS10 + 12G > A polymorphism (rs2242480) and for the UGT1A1 gene*22 polymorphism, associated with a decreased enzymatic activity; moreover, he was homozygote for the UGTA9*22 polymorphism, associated with a reduced transcriptional activity. It was hypothesized that these genetic variants of his hepatic metabolism made the patient particularly susceptible to oxidative stress possibly induced by the high doses of catechins (1 g/day), particularly by EGCG (Lambert et al. 2010). Moreover, the peculiar hepatic metabolism of the patient increased the concentration of oral contraceptives intermediates so favoring the haptenization of liver proteins and leading to the development of an autoimmune hepatitis, supported by a positivity of ANA antibodies and by the normalization of liver function tests after steroid therapy with prednisone (Gallo et al. 2013).
On the whole, based on the temporal relationship between the consumption of green tea and onset of reaction (“suggestive” or “compatible” according to CIOMS/RUCAM) and the positive rechallenge and the general absence of non-drug-related causes, these data point green tea as the main cause of the hepatic reactions reported. Nevertheless, only in some cases (Pillukat et al. 2014; Gallo et al. 2013), a laboratory analysis of the product ingested was carried out to exclude the presence of contaminants, a recurrent problem with herbal products.
Considering the reactions that involved multicomponent preparations of green tea, in some cases (SlimQuick™, Green Tea Fat Burner®, Euforia®, Lipoliz®, Exilis®, Lotus-f3®), their composition appears very complex owing to the presence, besides green tea, of several herbal ingredients, minerals, amino acids and others. The doses of green tea active constituents taken by patients were reported only in four cases and were expressed as EGCG (270 and 400 mg/day) or as polyphenols (140 and about 700 mg/day). The latency of the reaction, expressed as mean ± SE, was 44.7 ± 13.85 days. When the outcome consisted in resolution, the recovery time was 118.9 ± 38.79 days. The most striking datum is the severity of reactions in that all cases of liver transplantation (four = 33 %) occurred after consumption of multicomponent preparations.
One of the patients who underwent liver transplantation (case 4) consumed SlimQuick™; the product had been taken for 2 days. Several other causes for hepatitis (e.g., viral and autoimmune hepatitis, Wilson disease, primary biliary cirrhosis) were excluded; a toxicity due to metoprolol consumed by the patient was excluded too, owing to incompatible time of onset. The daily dosage of catechins taken by the patient, according to the manufacturer, was 270 mg: This dosage is considered as safe (Boehm et al. 2009), even if a quality control of the supplement has not been performed so the content of catechins has not been checked. However, it has to be considered that the supplement was taken fasting, a condition that increases the bioavailability of catechins (Chow et al. 2005; Isbrucker et al. 2006) and then their possible toxicity. Moreover, components of SlimQuick™ other than green tea are to be considered. For most of them, hepatotoxicity issues have not been reported; however, a speculation about Polygonum cuspidatum Siebold & Zucc. (Polygonaceae family) can be made. This medicinal plant is widely used in traditional Chinese medicine along with the species P. multiflorum Thunb.; the latter is known to be involved in numerous cases of hepatotoxicity (Dong et al. 2014; Lei et al. 2015). The chemical composition of these two species is similar, the major compounds being stilbenes and anthraquinone derivatives (Frédérich et al. 2011). They can be differentiated by identification of their stilbene derivatives; however, some confusion exists within the pharmaceutical market regarding P. multiflorum and P. cuspidatum (Frédérich et al. 2011), so we cannot exclude that in our case, P. multiflorum had been used instead of P. cuspidatum.
In the other case of liver injury after SlimQuick™ (case 11), several causes for hepatitis (viral and autoimmune hepatitis, Wilson disease, primary biliary cirrhosis) were excluded too, as well as a toxicity due to the concomitant medication with tetracycline, owing to the lack of consistent documentation and the incompatible time of onset. In this case, the patient was heterozygous for alpha-1 antitrypsin and the alpha-1 antitrypsin MZ phenotype has been suggested, which might be a risk factor for chronic liver disease or liver failure (Graziadei et al. 1998).
The second case of liver transplantation (case 5) regarded a 35-year-old woman who took Saba Appetite Control and Energy (ACE) for 2 days. She was also taking sertraline, norethindrone acetate and ethinyl estradiol for 3 years, without any recent change in doses; all other causes of hepatitis were ruled out. Besides green tea, the supplement ACE, in the previous formula, contained geranium extract also known as 1,3-dimethylpentylamine or DMAA. In July 2013, FDA banned DMAA-containing dietary supplements and any marketing practices promoting them, following several adverse reactions including liver failure (http://www.fda.gov/Food/DietarySupplements/QADietarySupplements/ucm346576.htm). Many DMAA-containing supplements were reformulated as “DMAA free”; however, geranium extract is still present in some ACE supplements marketed online. In light of this, we do not know which was the exact composition of the supplement taken by the patient, because it is not described in the case report. Among ACE ingredients, chromium is also reported. Trivalent chromium compounds are used to enhance weight loss due to purported effects of decreasing body fat and increasing basal rate (Anderson 1998); however, there have been reports of chromium hepatotoxicity, due to dietary supplements (Cerulli et al. 1998; Lança et al. 2002). In conclusion, which is the exact hepatotoxic agent in Saba Appetite Control and Energy (ACE) and whether a possible contamination with DMAA played a role in liver toxicity remain unclear.
The third case of liver transplantation (case 14) regarded a young 28-year-old female bodybuilder. This woman, besides the green tea-based supplement Lipolyz®, took several other dietary supplements, among which is Somalyz®. Both these supplements contain usnic acid, a substance derived from the lichen Usnea barbata. Usnic acid is a component of dietary supplements promoted for weight loss and has been associated with several levels of liver damage, ranging from mild hepatitis to liver failure requiring transplantation (Stickel et al. 2011; Sanchez et al. 2006; Neff et al. 2004). After numerous reports of liver toxicity related to the ingestion of dietary supplements containing usnic acid, the FDA in 2001 issued a warning about one such supplement, LipoKinetix (Guo et al. 2008). Usnic acid acts as an uncoupler of mitochondrial oxidative phosphorylation leading to an increase in fat metabolism and desired weight loss; however, with this effect, there is a concomitant increase in oxidative stress and cellular injury, resulting in loss of mitochondrial respiratory control and inhibition of ATP synthesis (Moreira et al. 2013; Guo et al. 2008). Usnic acid showed also to be a potent inhibitor of CYP2C19 and CYP2C9 with less potent inhibitor of CYP2C8 and CYP2C18 (Foti et al. 2008), so having a significant potential to interact with other medication. In this case, usnic acid may have been predominantly responsible for the liver damage even if its effect was possibly perpetuated by other components of the mixtures, among green tea.
The last case of liver transplantation (case 16) involved a 25-year-old man who took the dietary supplement Exilis®. He had neither other medications nor other clinical conditions possibly responsible for liver failure, so the dietary supplement remains the main suspect. Exilis®contains, besides green tea, Garcinia cambogia, Gymnema sylvestre, chromium chelate, conjugated linoleic and others. G. cambogia has been hypothesized to have a synergistic hepatotoxic effect with montelukast in a fatal case of liver failure (Actis et al. 2007) and in laboratory experiments has been shown to increase hepatic collagen accumulation, lipid peroxidation and mRNA levels of genes related to oxidative stress, as well as plasma alanine transaminase and aspartate transaminase levels (Kim et al. 2013). G. sylvestre has been reported to induce hepatitis too (Shiyovich et al. 2010). Possible hepatotoxicity of chromium compounds has been described above. Conjugated linoleic acid, an ingredient included in several weight loss dietary supplements because reputed as having some potential benefit for weight loss (Egras et al. 2011), has been recently involved in two cases of hepatotoxicity, one of which required liver transplantation (Ramos et al. 2009; Nortadas and Barata 2012). Last but not least, we cannot overlook the fact that most of the components of Exilis® (Garcinia cambogia, Gymnema sylvestre, chromium, calcium, l-carnitine and green tea) are identical to those of Hydroxycut®, the above-mentioned food supplement recalled by FDA in 2009. In this context, it is worth to emphasize that after Hydroxycut® recall, other cases of hepatotoxicity involving this supplement have been published. Seventeen cases were reported by Fong et al. (2010); they probably were collected before Hydroxycut® recall; in any case, it deserved to be mentioned that four out of them required liver transplantation. A further case, reported by Sharma et al. (2010), involved a 19-year-old man who took the product for fat burning and muscle building. More recently, Kaswala et al. (2014) reported the case of a 27-year-old man who was studying to be a physical trainer and had been taking Hydroxycut® along with other supplements (black powder, mitotropin, xenadrine, etc.). Finally, Haimowitz et al. (2015) described a fulminant liver failure in a 23-year-old man after consumption of Hydroxycut® for 2 months. In this case, the supplement was considered to be the cause of initial liver injury in the setting of an underlying porphyria. All these cases about Hydroxycut® highlight, besides the lack of information on the safety of herbal supplements, the fact that, even after withdrawal from the market, they are easily available through the other distribution channels as, for example, online sales.
Returning to our cases, four (6, 7, 8 and 18) out of 12 involved catechin-based supplements taken to counteract the hair loss. The two supplements involved in these reactions had a very similar composition consisting in catechins from green tea and grape seeds, taurine, zinc gluconate. In cases 6, 7 and 8, the causal relationship, according to CIOMS/RUCAM scale, resulted probable because of the temporal relationship between supplement consumption and reaction and the absence of other causes. In particular, patients 6 and 7 had no other medications while patient 7 had been taking acetyl salicylic acid and fenofibrate but for years, without any reaction. In case 18, the causality was possible owing to fact that the patient had been taking paracetamol as concomitant drug. Taurine and zinc gluconate are not suspected of liver damage to our knowledge, so catechins and the other components of the green tea and grape seeds remain the main responsible.
The case 9 (Patel et al. 2013) regarded a 16-year-old Hispanic male who was taking several dietary supplements as a part of an unsupervised weight loss planning. The patient was consuming the supplement Green Tea Fat Burner®, whose components, other than green tea, are not known as causing hepatotoxicity; on the contrary, some of them are considered to possess hepatoprotective effects (Fan et al. 2015; Huang et al. 2011). However, the young man was consuming also other supplements such as Nopal®, an extract from cactus of Opuntia genus, used as source of dietary fibers in the management of overweight (Grube et al. 2013), GNC Mega Men Sport®, a complex mixture containing numerous vitamins, minerals among which are chromium, branched chain amino acids, l-carnitine, lycopene, choline, zeaxanthin, astaxanthin, alpha-lipoic acid and others and, finally, whey protein. The latter, even if reputed a hepatoprotective substance (Gad et al. 2011), has been shown to cause liver damage in humans and in laboratory experiments (Vilella et al. 2013; Gürgen et al. 2014; Whitt et al. 2008). Moreover, chromium has been suspected of hepatotoxicity as already stated. So, on the whole, it is very difficult to establish which is the component responsible for the liver injury in this subject, but probably a unique culprit cannot be found.
Case 12 (Jiménez-Encarnación et al. 2012) deals with a 45-year-old woman with hypothyroidism and systemic sclerosis who had hepatitis after taking the preparation Euforia®. The patient was positive for antinuclear antibodies ANA (1:320), suggesting an autoimmune hepatitis; however, ANA are present in up to 98 % of systemic sclerosis patients (Villalta et al. 2012); authors concluded that the mechanism of the liver injury was unknown. As regards the components of the supplement, other than green tea, possibly involved in liver damage, aloe (Aloe vera L.) is one of defendants in that it has been associated with several cases of hepatitis (Lee et al. 2014; Yang et al. 2010; Curciarello et al. 2008; Belfrage and Malmström 2008; Bottenberg et al. 2007; Kanat et al. 2006). Anthraquinones, the chemical components of aloe, are reputed toxic that lead to the production of oxygen-derived free radicals that eventually induce apoptosis (Kågedal et al. 1999). Goji berry, the fruit of Lycium barbarum L., has been recently involved in hepatitis too (Franco et al. 2012; Arroyo-Martinez et al. 2011). Finally, many reports of suspected liver injuries from noni (Morinda citrifolia L.) are reported (Waldman et al. 2013; Yu et al. 2011; Stadlbauer et al. 2008; López-Cepero Andrada et al. 2007; Yuce et al. 2006; Stadlbauer et al. 2005; Millonig et al. 2005), even if hepatotoxicity of noni juice remains speculative (Mrzljak et al. 2013; West and Deng 2011). In this scenario, which component of Euforia® induced liver injury remains to be established.
The case 17 (Bergman and Schjøtt 2009) involved a 55-year-old man with a history of psoriatic arthritis who took Lotus-f3®. This is the unique published report of hepatotoxicity from this supplement; however, other unpublished cases are reported in Norwegian Adverse Drug Reaction database (RELIS) (http://relis.arnett.no/Utredning_Ekstern.aspx?Relis=3&S=4390&R=X). According to the authors, the content of green tea in Lotus-f3® had been reduced just after the reports of adverse effects. Non-drug-related cases of hepatitis were excluded; conversely, the patient was taking etanercept, an antagonist of tumor necrosis factor-alpha (TNFα), which is used widely in severe forms of rheumatoid arthritis and psoriasis. This drug has been associated with some cases of drug-induced liver injury (Ghabril et al. 2013); however, in our case, after resolution of the reaction, the drug was reintroduced and the dose was increased, without any adverse effect. None of the components of Lotus-f3®, other than green tea, are reported to be toxic to liver, except for chromium so, probably, green tea and chromium are the main suspected components.
Present data, particularly those from green tea alone, confirm that a certain safety concern with green tea exists. The number of hepatic reactions reported is low if we consider the great extent of use of green tea, nevertheless, has to be taken into account that there is a tendency for underreporting the ingestion of herbal supplements by patients and the magnitude of their use and, as a consequence, their adverse reactions are underrecognized by physicians (Bunchorntavakul and Reddy 2013). The liver damage occurs mostly after ingestion of green tea in high quantity or for long periods of time and the pattern of liver injury is almost always of hepatocellular type.
How and why green tea can induce liver injury is still under debate.
-
Safety and efficacy of herbal medicines and herbal supplements strongly depend on the quality, i.e., on the concentration of effective ingredients, the purity and a constant batch-to-batch composition. In principle, we can never exclude that hepatotoxicity can depend on lack of quality of the product suspected (contamination, adulteration, misidentification); however, in this case, the reaction probably should involve many people at the same time. In case of green tea extracts, hepatotoxicity could be consequence of the particular procedure applied for extraction and concentration that alter the original composition of green tea.
-
Green tea catechins, particularly EGCG, were found to be cytotoxic toward isolated hepatocytes being the major cytotoxic mechanism the mitochondrial membrane potential collapse and reactive oxygen species formation (Galati et al. 2006). The clinical relevance of in vitro data is difficult to establish, because the majority of published studies employ concentrations of EGCG in the range of 10–100 μM, while pharmacokinetic studies of EGCG in healthy subjects have established the achievable upper peak of plasma catechins as approximately 8 μM (Schönthal 2011). Nevertheless, other studies have shown that, under specific conditions such as fasting and repeated administration, catechins plasma level rises and induces toxicity (Wu et al. 2001; Chow et al. 2005; Ullmann et al. 2003).
-
Green tea components can interact with prescription drugs or other co-administered compounds by modulating the activity of P-glycoprotein (Zhou et al. 2004; Jodoin et al. 2002). Inhibition of human hepatic and intestinal microsomal CYP2C8, CYP2B6, CYP3A4, CYP2D6 and CYP2C19 by GTE catechins was observed in vitro; however, a clinical study of bioavailability highlighted a small risk of increased plasma drug levels only for substrates metabolized by CYP3A4, without clinical relevance (Teschke et al. 2014).
-
There is considerable evidence for a genetic basis of drug-induced liver injury; the human leukocyte antigen (HLA) genotype has been demonstrated to be a strong risk factor for drug-induced liver injury, as well as polymorphisms in genes encoding cytochromes P450, UDP-glucuronosyltransferase (UGT), ABS drug transporters and, finally, enzymes that protect against reactive oxygen species (ROS) (Urban et al. 2014). It has been suggested that host genetic factors can be important in modulating susceptibility to green tea too (Jimenez-Saenz and Martinez-Sanchez 2007). In support of this, recently, an experiment was carried out in Diversity Outbred mice, a newly derived heterogeneous strain of mice developed to maximize genetic variation within the population. In these mice, an equal exposure to EGCG (50 mg/Kg; daily for 3 days) was found to be tolerated in the majority of animals; however, a small fraction of mice (16 %) exhibited a severe hepatotoxicity that was analogous to the clinical cases (Church et al. 2015).
In this context, it has also to be noted that the green tea liver injury involves mostly females. This can be due to the more wide use made by this gender of herbal supplements, particularly those for body weight control, but it is known that females appear to be at higher risk of liver injury from some medications (Chalasani et al. 2014). Moreover it is surprising that a significant portion of subjects who experienced hepatitis after green tea (seven of the nineteen our cases) were Hispanic. An intriguing hypothesis is a genetic predisposition, even if other causes as prevalence of overweight among this population (being green tea often used for weight loss) or a wider use of green tea by this population cannot be excluded. It has to be noted that a genetic basis has been hypothesized in some of our cases (Gallo et al. 2013; Weinstein et al. 2012).
If a safety concern with green tea exists, a bigger safety concern exists when green tea is associated with other ingredients. People seeking to remain in good health, as well as patients seeking self-medicate, oftentimes consume a variety of herbal and other type of dietary supplements in addition to green tea thinking that “if one is good two is better.” On the contrary, present data clearly show that green tea hepatotoxicity is greatly enhanced when it is consumed in association with other herbal or dietary ingredients. Comparing the adverse events induced by only green tea-based preparations with those by multicomponent mixtures, it is apparent that in general, the first ones have a latency that is generally longer and the damage is generally milder because outcome was always resolution. On the contrary, liver injury associated with multicomponent preparations had a shorter latency and was more serious in that resulted in four cases of liver transplantation and, when resolution occurred, the recovery time was longer. As above described, almost all multicomponent green tea preparations contain ingredients other than green tea which are suspected to induce liver injury (Garcinia cambogia, Aloe vera, goji berries, chromium, usnic acid, etc.): These can act synergistically between them and with green tea, so enhancing the risk of liver damage. Moreover considering the possible quality problems related to a single herbal drug (plant variability, plant misidentification, contamination, adulteration, lack of standardization, etc.), it is obvious that more a mixture is complex, the greater the possibility of lack of quality. In addition, in a multicomponent herbal preparation, there are hundreds of molecules that may interact pharmacologically in a manner totally unpredictable with serious health risk. Finally, we cannot overlook the fact that often these products are used to increase the physical performance or in body building. It is known that physical exercise results in oxidative stress and free radical-mediated damage to tissues (Powers and Jackson 2008). For this reason, body builders use supplements containing antioxidants, such as green tea. Always thinking that “if one is good two is better,” they consume several other antioxidant-based supplements such as, for example, Mega Men Sport® that contains, besides green tea, vitamins C and E, selenium, lycopene, lutein, zeaxanthin, astaxanthin, etc, so exposing themselves to heath risks because it is equally well known that an excessive intake of antioxidants may promote oxidative stress (Rietjens et al. 2002) inducing several kind of damages among which is liver injury.
Conclusions
The popularity of herbal remedies is increasing worldwide. Being marketed as dietary supplements, they are not subjected to the evaluation for safety and efficacy so the harmful effects are reported only after they are placed on the market. Herbal supplements are emerging as a major cause of drug-induced liver injury, supplements used for body building and weight loss are the most common types implicated in the damage.
There is general agreement that herbal supplements hepatotoxicity represents a major diagnostic challenge, since markers for its diagnosis are not commonly available and there are only a few agents in which common and repeating patterns of injury have been observed (Chalasani et al. 2014). Moreover, a causality assessment process that is specific for herbal-induced liver injury has not been developed, although a preliminary attempt was made by DILIN (Hayashi et al. 2014).
On the whole, the cases here described show a positive trend in reporting herbal hepatotoxicity since numerous cases were published in 2014 (eight out of nineteen); this fact may depend on an increasing consumption of green tea products or herbal supplements in general, or an increasing attention by healthcare professionals to the safety of herbal supplements and, as consequence, an increasing reporting.
In previous cases of hepatotoxicity, green tea preparations were mostly used as slimming supplements, in cases here described weight loss was the reason of use in the minority of cases and, surprisingly, sometimes green tea preparations were taken to counteract hair loss. This shows that use of these preparations is changing and spreading in different fields.
Use of green tea infusion can be considered as safe when consumed as a beverage in normal quantity (1–2 cups/day), provided that quality concerns and other risk factors do not exist; nevertheless, an idiosyncratic reaction remains always possible. When using green tea derivatives such as extracts, safety concerns can rise, depending on the type of preparation and the dose of active components. In some extracts, EGCG content can reach up to 95 %: Such a product cannot be still named “green tea,” it is a pure substance, so we cannot rely on its long-lasting use as safety warranty (Ernst et al. 1998). Use of multicomponent preparations appears much more dangerous with respect to green tea alone.
Physician and patient awareness remains central to the early identification of herbal toxicity. Clinicians should ask their patients about consumption of herbal products and patients should be advised about possible adverse effects and encouraged to report them as soon as possible.
Whenever an adverse reaction occurs, attempts to obtain the suspected product should be made, in order to analyze it and so exclude any problem of quality (adulteration, contamination, etc.). Patients should be encouraged to use herbal and dietary supplements possibly under supervision of healthcare professionals. Healthcare professionals should be encouraged to report adverse effects of herbal supplements in order to implement their knowledge, to collect signals and, when necessary, to take regulatory measures.
References
Actis GC, Bugianesi E, Ottobrelli A, Rizzetto M (2007) Fatal liver failure following food supplements during chronic treatment with montelukast. Dig Liver Dis 39:953–955. doi:10.1016/j.dld.2006.10.002
Amariles P, Angulo N, Agudelo-Agudelo J, Gaviria G (2009) Hepatitis associated with aqueous green tea infusions: a case study. Farm Hosp 33:289–291. doi:10.1016/S1130-6343(09)72471-7
Anderson RA (1998) Effects of chromium on body composition and weight loss. Nutr Rev 56:266–270. doi:10.1111/j.1753-4887.1998.tb01763.x
Andrade RJ, Lucena MI, Fernández MC, Vega JL, García-Cortés M, Casado M, Guerrero-Sanchez E, Pulido-Fernandez F (2002) Cholestatic hepatitis related to use of irbesartan: a case report and a literature review of angiotensin II antagonist-associated hepatotoxicity. Eur J Gastroenterol Hepatol 14:887–890. doi:10.1097/00042737-200208000-00014
Arimone Y, Bégaud B, Miremont-Salamé G, Fourrier-Réglat A, Moore N, Molimard M, Haramburu F (2005) Agreement of expert judgment in causality assessment of adverse drug reactions. Eur J Clin Pharmacol 61:169–173. doi:10.1007/s00228-004-0869-2
Arroyo-Martinez Q, Sáenz MJ, Argüelles Arias F, Acosta MS (2011) Lycium barbarum: a new hepatotoxic “natural” agent? Dig Liver Dis 43:749. doi:10.1016/j.dld.2011.04.010
Arzenton E, Magro L, Paon V, Capra F, Apostoli P, Guzzo F, Conforti A, Leone R (2014) Acute epatitis caused by green tea infusion: a case report. Adv Pharmacoepidemiol Drug Saf 3:170. doi:10.4172/2167-1052.1000170
Bardia A, Nisly NL, Zimmerman MB, Gryzlak BM, Wallace RB (2007) Use of herbs among adults based on evidence-based indications: findings from the National Health Interview Survey. Mayo Clin Proc 82:561–566. doi:10.4065/82.5.561
Belfrage B, Malmström R (2008) Several cases of liver affected by Aloe vera. Lakartidningen 105:45
Benichou C, Danan G, Flahault A (1993) Causality assessment of adverse reactions to drugs–II. An original model for validation of drug causality assessment methods: case reports with positive rechallenge. J Clin Epidemiol 46:1331–1336. doi:10.1016/0895-4356(93)90102-7
Bergman J, Schjøtt J (2009) Hepatitis caused by Lotus-f3? Basic Clin Pharmacol Toxicol 104:414–416. doi:10.1111/j.1742-7843.2009.00385.x
Boehm K, Borrelli F, Ernst E, Habacher G, Hung SK, Milazzo S, Horneber M (2009) Green tea (Camellia sinensis) for the prevention of cancer. Cochrane Database Syst Rev 8:CD005004. doi:10.1002/14651858.CD005004.pub2
Bottenberg MM, Wall GC, Harvey RL, Habib S (2007) Oral Aloe vera-induced hepatitis. Ann Pharmacother 41:1740–1743. doi:10.1345/aph.1K132
Bunchorntavakul C, Reddy KR (2013) Review article: herbal and dietary supplement hepatotoxicity. Aliment Pharmacol Ther 37:3–17. doi:10.1111/apt.12109
Butt MS, Ahmad RS, Sultan MT, Qayyum MM, Naz A (2015) Green tea and anticancer perspectives: updates from last decade. Crit Rev Food Sci Nutr 55:792–805. doi:10.1080/10408398.2012.680205
Cavaliere C, Rea C, Lynch ME, Blumenthal M (2010) Herbal supplement sales rise in all channels in 2009. HerbalGram 86:62–65
Cerulli J, Grabe DW, Gauthier I, Malone M, McGoldrick MD (1998) Chromium picolinate toxicity. Ann Pharmacother 32:428–431. doi:10.1345/aph.17327
Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J, Drug Induced Liver Injury Network (DILIN) (2008) Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 135: 1924–1934, 1934.e1–1934.e4. doi: 10.1053/j.gastro.2008.09.011
Chalasani NP, Hayashi PH, Bonkovsky HL, Navarro VJ, Lee WM, Fontana RJ (2014) ACG Clinical Guideline: the diagnosis and management of idiosyncratic drug-induced liver injury. Am J Gastroenterol 109:950–966. doi:10.1038/ajg.2014.131
Chang CH, Chang YC, Lee YC, Liu YC, Chuang LM, Lin JW (2015) Severe hepatic injury associated with different statins in patients with chronic liver disease: a nationwide population-based cohort study. J Gastroenterol Hepatol 30:155–162. doi:10.1111/jgh.12657
Chauhan B, Kumar G, Kalam N, Ansari SH (2013) Current concepts and prospects of herbal nutraceutical: a review. J Adv Pharm Technol Res 4:4–8. doi:10.4103/2231-4040.107494
Chow HH, Hakim IA, Vining DR, Crowell JA, Ranger-Moore J, Chew WM, Celaya CA, Rodney SR, Hara Y, Alberts DS (2005) Effects of dosing condition on the oral bioavailability of green tea catechins after single-dose administration of polyphenon E in healthy individuals. Clin Cancer Res 11:4627–4633. doi:10.1158/1078-0432.CCR-04-2549
Church RJ, Gatti DM, Urban TJ, Long N, Yang X, Shi Q, Eaddy JS, Mosedale M, Ballard S, Churchill GA, Navarro V, Watkins PB, Threadgill DW, Harrill AH (2015) Sensitivity to hepatotoxicity due to epigallocatechin gallate is affected by genetic background in diversity outbred mice. Food Chem Toxicol 76:19–26. doi:10.1016/j.fct.2014.11.008
Curciarello J, De Ortúzar S, Borzi S, Bosia D (2008) Severe acute hepatitis associated with intake of Aloe vera tea. Gastroenterol Hepatol 31:436–438. doi:10.1157/13125590
Danan G, Benichou C (1993) Causality assessment of adverse reactions to drugs-I. A novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuries. J Clin Epidemiol 46:1323–1330. doi:10.1016/0895-4356(93)90101-6
Dela Cruz AC, Patel TT, Maynard E, Shah M, Lee EY, Angulo P (2014) Fulminant liver failure secondary to “Saba appetite control and energy” weight loss supplement. Gastroenterology 146:S-1002. doi:10.1016/S0016-5085(14)63644-1
Denison HJ, Jameson KA, Syddall HE, Dennison EM, Cooper C, Sayer AA, Robinson SM (2012) Patterns of dietary supplement use among older men and women in the UK: findings from the Hertfordshire Cohort Study. J Nutr Health Aging 16:307–311. doi:10.1007/s12603-012-0016-1
Dias TR, Alves MG, Tomás GD, Socorro S, Silva BM, Oliveira PF (2014) White tea as a promising antioxidant medium additive for sperm storage at room temperature: a comparative study with green tea. J Agric Food Chem 62:608–617. doi:10.1021/jf4049462
Dong H, Slain D, Cheng J, Ma W, Liang W (2014) Eighteen cases of liver injury following ingestion of Polygonum multiflorum. Complement Ther Med 22:70–74. doi:10.1016/j.ctim.2013.12.008
Douros A, Kauffmann W, Bronder E, Klimpel A, Garbe E, Kreutz R (2013) Ramipril-induced liver injury: case report and review of the literature. Am J Hypertens 26:1070–1075. doi:10.1093/ajh/hpt090
Egras AM, Hamilton WR, Lenz TL, Monaghan MS (2011) An evidence-based review of fat modifying supplemental weight loss products. J Obes. doi:10.1155/2011/297315
Ehrenpreis ED, Kulkarni P, Burke C (2013) What gastroenterologists should know about the gray market, herbal remedies, and compounded pharmaceuticals and their regulation by the Food and Drug Administration. Am J Gastroenterol 108:642–646. doi:10.1038/ajg.2012.348
Elouni B, Ben Salem C, Zamy M, Ganne N, Beaugrand M, Bouraoui K, Biour M (2010) Cytolytic hepatitis possibly related to levonorgestrel/ethinylestradiol oral contraceptive use: 2 case reports. Ann Pharmacother 44:2035–2037. doi:10.1345/aph.1P201
Ernst E, De Smet PA, Shaw D, Murray V (1998) Traditional remedies and the “test of time”. Eur J Clin Pharmacol 54:99–100. doi:10.1007/s002280050428
Fan X, Chen P, Jiang Y, Wang Y, Tan H, Zeng H, Wang Y, Qu A, Gonzalez FJ, Huang M, Bi H (2015) Therapeutic efficacy of Wuzhi tablet (Schisandra sphenanthera extract) on acetaminophen-induced hepatotoxicity through a mechanism distinct from N-acetylcysteine. Drug Metab Dispos 43:317–324. doi:10.1124/dmd.114.062067
FDA (2013) DMAA in Dietary Supplements. US Food and Drug Administration. http://www.fda.gov/Food/DietarySupplements/QADietarySupplements/ucm346576.htm. Accessed 5 Mar 2015
FDA Warns Consumers to Stop Using Hydroxycut Products. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149575.htm. Accessed 31 Mar 2015
Fernández J, Navascués C, Albines G, Franco L, Pipa M, Rodríguez M (2014) Three cases of liver toxicity with a dietary supplement intended to stop hair loss. Rev Esp Enferm Dig 106:552–555
Fong TL, Klontz KC, Canas-Coto A, Casper SJ, Durazo FA, Davern TJ II, Hayashi P, Lee WM, Seeff LB (2010) Hepatotoxicity due to hydroxycut: a case series. Am J Gastroenterol 105:1561–1566. doi:10.1038/ajg.2010.5
Foti RS, Dickmann LJ, Davis JA, Greene RJ, Hill JJ, Howard ML, Pearson JT, Rock DA, Tay JC, Wahlstrom JL, Slatter JG (2008) Metabolism and related human risk factors for hepatic damage by usnic acid containing nutritional supplements. Xenobiotica 38:264–280. doi:10.1080/00498250701802514
Franco M, Monmany J, Domingo P, Turbau M (2012) Autoimmune hepatitis triggered by consumption of Goji berries. Med Clin 139:320–321. doi:10.1016/j.medcli.2012.02.009
Frédérich M, Wauters JN, Tits M, Jason C, de Tullio P, Van der Heyden Y, Fan G, Angenot L (2011) Quality assessment of Polygonum cuspidatum and Polygonum multiflorum by 1H NMR metabolite fingerprinting and profiling analysis. Planta Med 77:81–86. doi:10.1055/s-0030-1250132
Gad AS, Khadrawy YA, El-Nekeety AA, Mohamed SR, Hassan NS, Abdel-Wahhab MA (2011) Antioxidant activity and hepatoprotective effects of whey protein and Spirulina in rats. Nutrition 27:582–589. doi:10.1016/j.nut.2010.04.002
Galati G, Lin A, Sultan AM, O’Brien PJ (2006) Cellular and in vivo hepatotoxicity caused by green tea phenolic acids and catechins. Free Radic Biol Med 40:570–580. doi:10.1016/j.freeradbiomed.2005.09.014
Gallo E, Maggini V, Berardi M, Pugi A, Notaro R, Talini G, Vannozzi G, Bagnoli S, Forte P, Mugelli A, Annese V, Firenzuoli F, Vannacci A (2013) Is green tea a potential trigger for autoimmune hepatitis? Phytomedicine 20:1186–1189. doi:10.1016/j.phymed.2013.07.004
Garcia-Alvarez A, Egan B, de Klein S, Dima L, Maggi FM, Isoniemi M, Ribas-Barba L, Raats MM, Meissner EM, Bade M, Bruno F, Salmenhaara M, Milà-Villarroel R, Knaze V, Hodgkins C, Marculescu A, Uusitalo L, Restani P, Serra-Majem L (2014) Usage of plant food supplements across six European countries: findings from the PlantLIBRA Consumer Survey. PLoS One 9:e92265. doi:10.1371/journal.pone.0092265
Ghabril M, Bonkovsky HL, Kum C, Davern T, Hayashi PH, Kleiner DE, Serrano J, Rochon J, Fontana RJ, Bonacini M, US Drug-Induced Liver Injury Network (2013) Liver injury from tumor necrosis factor-α antagonists: analysis of thirty-four cases. Clin Gastroenterol Hepatol 11(558–564):e3. doi:10.1016/j.cgh.2012.12.025
Gloro R, Hourmand-Ollivier I, Mosquet B, Mosquet L, Rousselot P, Salamé E, Piquet MA, Dao T (2005) Fulminant hepatitis during self-medication with hydroalcoholic extract of green tea. Eur J Gastroenterol Hepatol 17:1135–1137. doi:10.1097/00042737-200510000-00021
Graziadei IW, Joseph JJ, Wiesner RH, Therneau TM, Batts KP, Porayko MK (1998) Increased risk of chronic liver failure in adults with heterozygous alpha1-antitrypsin deficiency. Hepatol 28:1058–1063. doi:10.1002/hep.510280421
Grube B, Chong PW, Lau KZ, Orzechowski HD (2013) A natural fiber complex reduces body weight in the overweight and obese: a double-blind, randomized, placebo-controlled study. Obesity 21:58–64. doi:10.1002/oby.20244
Guo L, Shi Q, Fang JL, Mei N, Ali AA, Lewis SM, Leakey JE, Frankos VH (2008) Review of usnic acid and Usnea barbata toxicity. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev 26:317–338. doi:10.1080/10590500802533392
Gürgen S, Yücel A, Karakuş A, Ceçen D, Ozen G, Koçtürk S (2014) Usage of whey protein may cause liver damage via inflammatory and apoptotic responses. Hum Exp Toxicol. doi:10.1177/0960327114556787
Haimowitz S, Hsieh J, Shcherba M, Averbukh Y (2015) Liver failure after hydroxycut™ use in a patient with undiagnosed hereditary coproporphyria. J Gen Intern Med. doi:10.1007/s11606-014-3153-x
Hayashi PH, Barnhart HX, Fontana RJ, Chalasani N, Davern TJ, Talwalkar JA, Reddy KR, Stolz AA, Hoofnagle JH, Rockey DC (2014) Reliability of causality assessment for drug, herbal and dietary supplement hepatotoxicity in the Drug-Induced Liver Injury Network (DILIN). Liver Int. doi:10.1111/liv.12540
Huang L, Zhao H, Huang B, Zheng C, Peng W, Qin L (2011) Acanthopanax senticosus: review of botany, chemistry and pharmacology. Pharmazie 66:83–97. doi:10.1691/ph.2011.0744
Inno A, Basso M, Vecchio FM, Marsico VA, Cerchiaro E, D’Argento E, Bagalà C, Barone C (2011) Anastrozole-related acute hepatitis with autoimmune features: a case report. BMC Gastroenterol 11:32. doi:10.1186/1471-230X-11-32
Isbrucker RA, Edwards JA, Wolz E, Davidovich A, Bausch J (2006) Safety studies on epigallocatechin gallate (EGCG) preparations. Part 2: dermal, acute and short-term toxicity studies. Food Chem Toxicol 44:636–650. doi:10.1691/ph.2011.0744
Jiménez-Encarnación E, Ríos G, Muñoz-Mirabal A, Vilá LM (2012) Euforia-induced acute hepatitis in a patient with scleroderma. BMJ Case Rep. doi:10.1136/bcr-2012-006907
Jimenez-Saenz M, Martinez-Sanchez C (2007) Green tea extracts and acute liver failure: the need for caution in their use and diagnostic assessment. Liver Transpl 13:1067. doi:10.1002/lt.21127
Jodoin J, Demeule M, Beliveau R (2002) Inhibition of the multidrug resistance P-glycoprotein activity by green tea polyphenols. Biochim Biophys Acta 1542:149–159. doi:10.1016/S0167-4889(01)00175-6
Kågedal K, Bironaite D, Ollinger K (1999) Anthraquinone cytotoxicity and apoptosis in primary cultures of rat hepatocytes. Free Radic Res 31:419–428. doi:10.1080/10715769900300981
Kanat O, Ozet A, Ataergin S (2006) Aloe vera-induced acute toxic hepatitis in a healthy young man. Eur J Intern Med. 17:589. doi:10.1016/j.ejim.2006.04.017
Kaswala D, Shah S, Patel N, Raisoni S, Swaminathan S (2014) Hydroxycut-induced liver toxicity. Ann Med Health Sci Res 4:143–145. doi:10.4103/2141-9248.126627
Keske MA, Ng HL, Premilovac D, Rattigan S, Kim JA, Munir K, Yang P, Quon MJ (2015) Vascular and metabolic actions of the green tea polyphenol epigallocatechin gallate. Curr Med Chem 22:59–69. doi:10.2174/0929867321666141012174553
Kim YJ, Choi MS, Park YB, Kim SR, Lee MK, Jung UJ (2013) Garcinia cambogia attenuates diet-induced adiposity but exacerbates hepatic collagen accumulation and inflammation. World J Gastroenterol 19:4689–4701. doi:10.3748/wjg.v19.i29.4689
Koncic MZ, Tomczyk M (2013) New insights into dietary supplements used in sport: active substances, pharmacological and side effects. Curr Drug Targets 4:1079–1092. doi:10.2174/1389450111314090016
Lacey R, Evans A (2014) An unusual cause of jaundice in a patient with breast cancer. BMJ Case Rep. doi:10.1136/bcr-2014-205764
Lambert JD, Kennett MJ, Sang S, Reuhl KR, Ju J, Yang CS (2010) Hepatotoxicity of high oral dose (-)-epigallocatechin-3-gallate in mice. Food Chem Toxicol 48:409–416. doi:10.1016/j.fct.2009.10.030
Lança S, Alves A, Vieira AI, Barata J, de Freitas J, de Carvalho A (2002) Chromium-induced toxic hepatitis. Eur J Intern Med 13:518–520. doi:10.1016/S0953-6205(02)00164-4
Lee J, Lee MS, Nam KW (2014) Acute toxic hepatitis caused by an Aloe vera preparation in a young patient: a case report with a literature review. Korean J Gastroenterol 64:54–58. doi:10.4166/kjg.2014.64.1.54
Lei X, Chen J, Ren J, Li Y, Zhai J, Mu W, Zhang L, Zheng W, Tian G, Shang H (2015) Liver damage associated with polygonum multiflorum thunb: a systematic review of case reports and case series. Evid Based Complement Altern Med. doi:10.1155/2015/459749
Licata A, Macaluso FS, Craxì A (2013) Herbal hepatotoxicity: a hidden epidemic. Intern Emerg Med 8:13–22. doi:10.1007/s11739-012-0777-x
López-Cepero Andrada JM, Lerma Castilla S, Fernández Olvera MD, Amaya Vidal A (2007) Hepatotoxicity caused by a Noni (Morinda citrifolia) preparation. Rev Esp Enferm Dig 99:179–181
Lorenzo-Almorós A, Polo-Sabau J, Barrio-Dorado MD, Ruggiero García M (2015) Acute liver injury induced by green tea extracts. Gastroenterol Hepatol 38:44–45. doi:10.1016/j.gastrohep.2014.07.004
Mazzanti G, Menniti-Ippolito F, Moro PA, Cassetti F, Raschetti R, Santuccio C, Mastrangelo S (2009) Hepatotoxicity from green tea: a review of the literature and two unpublished cases. Eur J Clin Pharmacol 65:331–341. doi:10.1007/s00228-008-0610-7
Mc Donnell WM, Bhattacharya R, Halldorson JB (2009) Fulminant hepatic failure after use of the herbal weight-loss supplement Exilis. Ann Intern Med 151:673–674. doi:10.7326/0003-4819-151-9-200911030-00021
Menniti-Ippolito F, Mazzanti G, Vitalone A, Firenzuoli F, Santuccio C (2008) Surveillance of suspected adverse reactions to natural health products: the case of propolis. Drug Saf 31:419–423. doi:10.2165/00002018-200831050-00007
Millonig G, Stadlmann S, Vogel W (2005) Herbal hepatotoxicity: acute hepatitis caused by a Noni preparation (Morinda citrifolia). Eur J Gastroenterol Hepatol 17:445–447
Moreira CT, Oliveira AL, Comar JF, Peralta RM, Bracht A (2013) Harmful effects of usnic acid on hepatic metabolism. Chem Biol Interact 203:502–511. doi:10.1016/j.cbi.2013.02.001
Mrzljak A, Kosuta I, Skrtic A, Kanizaj TF, Vrhovac R (2013) Drug-induced liver injury associated with Noni (Morinda citrifolia) juice and phenobarbital. Case Rep Gastroenterol 7:19–24. doi:10.1159/000343651
Neff GW, Reddy KR, Durazo FA, Meyer D, Marrero R, Kaplowitz N (2004) Severe hepatotoxicity associated with the use of weight loss diet supplements containing ma huang or usnic acid. J Hepatol 41:1062–1064. doi:10.1016/j.jhep.2004.06.028
Nortadas R, Barata J (2012) Fulminant hepatitis during self-medication with conjugated linoleic acid. Ann Hepatol 11:265–267
Patel SS, Beer S, Kearney DL, Phillips G, Carter BA (2013) Green tea extract: a potential cause of acute liver failure. World J Gastroenterol 19:5174–5177. doi:10.3748/wjg.v19.i31.5174
Perdices EV, Medina-Cáliz I, Hernando S, Ortega A, Martín-Ocaña F, Navarro JM, Peláez G, Castiella A, Hallal H, Romero-Gómez M, González-Jiménez A, Robles-Díaz M, Lucena MI, Andrade RJ (2014) Hepatotoxicity associated with statin use: analysis of the cases included in the Spanish Hepatotoxicity Registry. Rev Esp Enferm Dig 106:246–254
Pillukat MH, Bester C, Hensel A, Lechtenberg M, Petereit F, Beckebaum S, Müller KM, Schmidt HH (2014) Concentrated green tea extract induces severe acute hepatitis in a 63-year-old woman—a case report with pharmaceutical analysis. J Ethnopharmacol 155:165–170. doi:10.1016/j.jep.2014.05.015
Powers SK, Jackson MJ (2008) Exercise-induced oxidative stress: cellular mechanisms and impact on muscle force production. Physiol Rev 88(4):1243–1276. doi:10.1152/physrev.00031.2007
Radha Krishna Y, Mittal V, Grewal P, Fiel MI, Schiano T (2011) Acute liver failure caused by ‘fat burners’ and dietary supplements: a case report and literature review. Can J Gastroenterol 25:157–160
Ramos R, Mascarenhas J, Duarte P, Vicente C, Casteleiro C (2009) Conjugated linoleic acid-induced toxic hepatitis: first case report. Dig Dis Sci 54:1141–1143. doi:10.1007/s10620-008-0461-1
RELIS database (2007) CLA, Lotus-f3 og hepatitt. RELIS Vest. http://relis.arnett.no/Utredning_Ekstern.aspx?Relis=3&S=4390&R=X. Accessed 11 Mar 2015
Rietjens IM, Boersma MG, Haan Ld, Spenkelink B, Awad HM, Cnubben NH, van Zanden JJ, Hv Woude, Alink GM, Koeman JH (2002) The pro-oxidant chemistry of the natural antioxidants vitamin C, vitamin E, carotenoids and flavonoids. Environ Toxicol Pharmacol 11(3–4):321–333
Rietveld A, Wiseman S (2003) Antioxidant effects of tea: evidence from human clinical trials. J Nutr 133:3285S–3292S
Rohde J, Jacobsen C, Kromann-Andersen H (2011) Toxic hepatitis triggered by green tea. Ugeskr Laeger 173:205–206
Rossi S, Navarro VJ (2014) Herbs and liver injury: a clinical perspective. Clin Gastroenterol Hepatol 12:1069–1076. doi:10.1016/j.cgh.2013.07.030
Sanchez W, Maple JT, Burgart LJ, Kamath PS (2006) Severe hepatotoxicity associated with use of a dietary supplement containing usnic acid. Mayo Clin Proc 81:541–544. doi:10.4065/81.4.541
Sarma DN, Barrett ML, Chavez ML, Gardiner P, Ko R, Mahady GB, Marles RJ, Pellicore LS, Giancaspro GI, Low Dog T (2008) Safety of green tea extracts: a systematic review by the US Pharmacopeia. Drug Saf 31:469–484. doi:10.2165/00002018-200831060-00003
Schönthal AH (2011) Adverse effects of concentrated green tea extracts. Mol Nutr Food Res 55:874–885. doi:10.1002/mnfr.201000644
Seeff LB, Bonkovsky HL, Navarro VJ, Wang G (2014) Herbal products and the liver: a review of adverse effects and mechanisms. Gastroenterology. doi:10.1053/j.gastro.2014.12.004
Sharma T, Wong L, Tsai N, Wong RD (2010) Hydroxycut(®) (herbal weight loss supplement) induced hepatotoxicity: a case report and review of literature. Hawaii Med J 69:188–190
Shiyovich A, Sztarkier I, Nesher L (2010) Toxic hepatitis induced by Gymnema sylvestre, a natural remedy for type 2 diabetes mellitus. Am J Med Sci 340:514–517. doi:10.1097/MAJ.0b013e3181f41168
Silano V, Coppens P, Larrañaga-Guetaria A, Minghetti P, Roth-Ehrang R (2011) Regulations applicable to plant food supplements and related products in the European Union. Food Funct 2:710–719. doi:10.1039/c1fo10105f
Snyder FJ, Dundas ML, Kirkpatrick C, Neill KS (2009) Use and safety perceptions regarding herbal supplements: a study of older persons in southeast Idaho. J Nutr Elder 28:81–95. doi:10.1080/01639360802634043
Stadlbauer V, Fickert P, Lackner C, Schmerlaib J, Krisper P, Trauner M, Stauber RE (2005) Hepatotoxicity of NONI juice: report of two cases. World J Gastroenterol 11:4758–4760
Stadlbauer V, Weiss S, Payer F, Stauber RE (2008) Herbal does not at all mean innocuous: the sixth case of hepatotoxicity associated with Morinda citrifolia (Noni). Am J Gastroenterol 103:2406–2407. doi:10.1111/j.1572-0241.2008.02010_8.x
Stickel F, Kessebohm K, Weimann R, Seitz HK (2011) Review of liver injury associated with dietary supplements. Liver Int 31:595–605. doi:10.1111/j.1478-3231.2010.02439.x
Tenore GC, Daglia M, Ciampaglia R, Novellino E (2015) Exploring the nutraceutical potential of polyphenols from black, green and white tea infusions—an overview. Curr Pharm Biotechnol 16:264–271. doi:10.2174/1389201016666150118133604
Teschke R, Schwarzenboeck A, Hennermann KH (2008) Causality assessment in hepatotoxicity by drugs and dietary supplements. Br J Clin Pharmacol 66:758–766. doi:10.1111/j.1365-2125.2008.03264.x
Teschke R, Zhang L, Melzer L, Schulze J, Eickhoff A (2014) Green tea extract and the risk of drug-induced liver injury. Expert Opin Drug Metab Toxicol 10:1663–1676. doi:10.1517/17425255.2014.971011
Ullmann U, Haller J, Decourt JP, Girault N, Girault J, Richard-Caudron AS, Pineau B, Weber P (2003) A single ascending dose study of epigallocatechin gallate in healthy volunteers. J Int Med Res 31:88–101
Update on the USP Green Tea Extract Monograph. http://www.usp.org/usp-nf/notices/retired-compendial-notices/update-usp-green-tea-extract-monograph. Accessed 31 Mar 2015
Urban TJ, Daly AK, Aithal GP (2014) Genetic basis of drug-induced liver injury: present and future. Semin Liver Dis 34:123–133. doi:10.1055/s-0034-1375954
US National Library of Medicine—NIH http://www.nlm.nih.gov/medlineplus/healthtopics.html. Accessed 16 Feb 2015 (bisogna indicare il documento consultato)
Vanstraelen S, Rahier J, Geubel AP (2008) Jaundice as a misadventure of a green tea (Camellia sinensis) lover: a case report. Acta Gastroenterol Belg 71:409–412
Verhelst X, Burvenich P, Van Sassenbroeck D, Gabriel C, Lootens M, Baert D (2009) Acute hepatitis after treatment for hair loss with oral green tea extracts (Camellia sinensis). Acta Gastroenterol Belg 72:262–264
Vilella AL, Limsuwat C, Williams DR, Seifert CF (2013) Cholestatic jaundice as a result of combination designer supplement ingestion. Ann Pharmacother 47:e33. doi:10.1345/aph.1R405
Villalta D, Imbastaro T, Di Giovanni S, Lauriti C, Gabini M, Turi MC, Bizzaro N (2012) Diagnostic accuracy and predictive value of extended autoantibody profile in systemic sclerosis. Autoimmun Rev 12:114–120. doi:10.1016/j.autrev.2012.07.005
Vitalone A, Menniti-Ippolito F, Moro PA, Firenzuoli F, Raschetti R, Mazzanti G (2011) Suspected adverse reactions associated with herbal products used for weight loss: a case series reported to the Italian National Institute of Health. Eur J Clin Pharmacol 67:215–224. doi:10.1007/s00228-010-0981-4
Vitalone A, Menniti-Ippolito F, Raschetti R, Renda F, Tartaglia L, Mazzanti G (2012) Surveillance of suspected adverse reactions to herbal products used as laxatives. Eur J Clin Pharmacol 8:231–238. doi:10.1007/s00228-011-1128-y
Waldman W, Piotrowicz G, Sein Anand J (2013) Hepatoxic effect of a noni juice consumption—a case report. Przegl Lek 70:690–692
Wang L, Zhang X, Liu J, Shen L, Li Z (2014) Tea consumption and lung cancer risk: a meta-analysis of case–control and cohort studies. Nutrition 30:1122–1127. doi:10.1016/j.nut.2014.02.023
Weinstein DH, Twaddell WS, Raufman JP, Philosophe B, Mindikoglu AL (2012) SlimQuick™-associated hepatotoxicity in a woman with alpha-1 antitrypsin heterozygosity. World J Hepatol 4:154–157. doi:10.4254/wjh.v4.i4.154
West BJ, Deng S (2011) Ingredients other than noni may be culprits in acute hepatotoxicity in 14-year-old boy. J Pediatr Gastroenterol Nutr 53:469–470. doi:10.1097/MPG.0b013e31822b77e2
Whitsett M, Halegoua-De Marzio D, Rossi S (2014) SlimQuick™-associated hepatotoxicity resulting in fulminant liver failure and orthotopic liver transplantation. ACG Case Rep J 1:220–222
Whitt KN, Ward SC, Deniz K, Liu L, Odin JA, Qin L (2008) Cholestatic liver injury associated with whey protein and creatine supplements. Semin Liver Dis 28:226–231. doi:10.1055/s-2008-1073122
Wierzejska R (2014) Tea and health—a review of the current state of knowledge. Przegl Epidemiol 68(501–6):595–599
Wu KM, Yao J, Boring D (2001) Green tea extract-induced lethal toxicity in fasted but not in nonfasted dogs. Int J Toxicol 30:19–20. doi:10.1177/1091581810387445
Wu QJ, Dong QH, Sun WJ, Huang Y, Wang QQ, Zhou WL (2014) Discrimination of Chinese teas with different fermentation degrees by stepwise linear discriminant analysis (S-LDA) of the chemical compounds. J Agric Food Chem 62:9336–9344. doi:10.1021/jf5025483
Yang HN, Kim DJ, Kim YM, Kim BH, Sohn KM, Choi MJ, Choi YH (2010) Aloe-induced toxic hepatitis. J Korean Med Sci 25:492–495. doi:10.3346/jkms.2010.25.3.492
Yu EL, Sivagnanam M, Ellis L, Huang JS (2011) Acute hepatotoxicity after ingestion of Morinda citrifolia (Noni Berry) juice in a 14-year-old boy. J Pediatr Gastroenterol Nutr 52:222–224. doi:10.1097/MPG.0b013e3181eb69f0
Yuce B, Gulberg V, Diebold J, Gerbes AL (2006) Hepatitis induced by Noni juice from Morinda citrifolia: a rare cause of hepatotoxicity or the tip of the iceberg? Digestion 73:167–170
Zhou S, Lim LY, Chowbay B (2004) Herbal modulation of P-glycoprotein. Drug Metab Rev 36:57–104. doi:10.1081/DMR-120028427
Acknowledgments
A. Di Sotto and A. Vitalone were supported by “Enrico and Enrica Sovena Foundation” Rome, Italy. We thank Dr. Patrizia Parisi and Dr. Silvia Di Giacomo for their assistance in retrieving some articles.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Antonella Di Sotto and Annabella Vitalone have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Mazzanti, G., Di Sotto, A. & Vitalone, A. Hepatotoxicity of green tea: an update. Arch Toxicol 89, 1175–1191 (2015). https://doi.org/10.1007/s00204-015-1521-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-015-1521-x