Abstract
Streptococcus suis is a major bacterial pathogen of swine and an emerging zoonotic agent that has to date resulted in substantial economic losses to the swine industry worldwide, and can cause persistent infection by forming biofilms. GrpE and histidine protein kinase ComD are important proteins implicated in the pathogenicity of S. suis, although whether they play roles in adhesion and biofilm formation has yet to be sufficiently clarified. In this study, we constructed grpE and comD deletion strains of S. suis by homologous recombination, and examined their cell adhesion and biofilm formation capacities compared with those of the wild-type strain. The pathogenicity of the grpE and comD deletion strains was evaluated using a mouse infection model, which revealed that compared with the wild-type, these deletion strains induced milder symptoms and lower bacteremia, as well as comparatively minor organ (brain, spleen, liver, and lung) lesions, in the infected mice. Moreover, the deletion of grpE and comD significantly reduced the pro-inflammatory cytokine (IL-6, IL-1β, and TNF-α) induction capacity of S. suis. Collectively, the findings of this study indicate that the GrpE and ComD proteins of Streptococcus suis play key roles in the adherence to PK-15 cells and the formation of biofilms, thereby contributing to the virulence of this pathogen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Streptococcus suis is a significant pathogen of swine, it takes pigs as the main host and is mainly colonizes in the upper respiratory tract and tonsil of pigs, causing meningitis, pneumonia, endocarditis, septicemia, and other pathological conditions in infected pigs, and is consequently a source of substantial economic losses to the global swine industry (Yi et al. 2021). The diseases caused by S. suis are difficult to cure, as S. suis can induce persistent in vivo infections as a result of biofilm formation (Zhao et al. 2015). A necessary prerequisite for the continuous infection and dissemination of S. suis is that upon initially colonizing a host, the bacterial cells must evade the host's immune system (Wang et al. 2020a). In this regard, S. suis can gain protection against the antagonistic effects of host defenses by forming biofilms and trapping nutrients (Li et al. 2018). Biofilms are microbial communities that aggregate and attach to the surfaces of living and non-living substrates, and play a key role in the pathogenesis and persistence of certain infectious bacteria (Yang et al. 2018a). In the case of S. suis, it can escape harsh environments by aggregating as biofilms, allowing them to persist and colonize tissues, resist host defense mechanisms and clearance by antimicrobial agents, and facilitate the exchange of genetic information, biofilms contribute to persistent infections and present difficulties in treatment in vivo (Vötsch et al. 2018). The essential initial step in biofilm formation is the adhesion of bacteria to a substrate, which is a non-specific reversible attachment. Having thus attached, the bacteria commence the synthesis of insoluble exopolysaccharides that have the effect of enclosing the adherent bacteria in a three-dimensional matrix (Li et al. 2018). Given that bacterial adhesion to a substrate is non-specific and reversible, interfering with the attachment of S. suis to surfaces might represent an effective means of impeding the formation of biofilms by this bacterium. At the same time, during the infection process, a wide variety of virulence-associated factors enable S. suis to colonize, invade, and spread in the host, thus causing localized infections and/or systemic diseases (Zheng et al. 2020).
In numerous bacterial species, heat shock proteins (HSPs) have been established to play a role in biofilm formation (Zeng et al. 2020; Tripathi et al. 2020). GrpE is the only known type of nucleotide exchange factor for Hsp70 in bacteria and organelles of bacterial origin and plays an essential role in bacterial pathogenic paradigms (Bracher and Verghese 2015). Structurally, GrpE consists of an α-helix dimerization domain and a β-domain that mediates its interaction with DnaK (Bracher and Verghese 2015). In some specific cases, it was found that there had been a connection of GrpE expression and stress conditions during the formation of some bacterial biofilm. In Escherichia coli, DnaK-DnaJ-GrpE was shown to play a significant role on biofilm formation under heat shock conditions only (Grudniak et al. 2015). In Actinomyces naeslundii, GrpE was upregulated in biofilms, especially in membrane damaged cells (Yoneda et al. 2013). And an increase in GrpE and other genes was observed in Staphylococcus aureus biofilms when exposed to macrophages and neutrophils (Scherr et al. 2013). However, our knowledge regarding how GrpE might influence biofilm formation in bacterial species remains limited. According to reports, when bacteria enter the host, they are immediately exposed to different environments, including changes in temperature, osmotic pressure, and pH. Bacteria adhere, invade or escape these stimuli by increasing the expression of virulence factors and stress response proteins, including HSPs and chaperone proteins. Bacteria usually use these chaperones and proteases to facilitate a compensatory response to stress conditions to survive (Wang et al. 2022a). Previous studies have shown that GrpE was significantly down-regulated upon tylosin stress in S. suis and this correlated with the level of drug resistance (Che et al. 2019). It is well known that biofilm formation is one of the important causes of chronic drug-resistant S. suis infection (Zhou et al. 2021). Meanwhile, given that salivary proline-rich proteins mediate group A Streptococcus adherence to pharyngeal epithelial cells via the GrpE chaperone protein (Murakami et al. 2012), we speculated that GrpE could play a role in biofilm formation by mediating the adhesion of S. suis.
In addition to GrpE, the histidine protein kinase ComD has been shown to play a significant role in bacterial biofilm formation, including that of Streptococcus mutans, Streptococcus pneumoniae, and Streptococcus intermedius (Suntharalingam and Cvitkovitch 2005; Yang et al. 2017, 2018b). For example, S. mutans comD and comE mutants are characterized by a reduced ability to adhere to the surfaces of host cells, and S. intermedius comD has been found to be bound and activated by a competence stimulating peptide (CSP) to promote the early accumulation of biofilm cells via CSP-mediated quorum sensing (QS). The QS system has become an attractive target for interventions against biofilm infections because it can control biofilm formation, activate virulence factors, and withstand acidic conditions (Guan et al. 2020). These observations conceivably indicate that in S. mutans and S. intermedius, ComD might influence the initial stages of biofilm growth rather than the latter maturation step (Suntharalingam and Cvitkovitch 2005). In addition, the ability of S. suis to form a biofilm plays an important role in its virulence and the development of drug resistance. S. suis has been reported as the transformable species, ComC/D/E may exist in S. suis and comD gene transcripts were significantly down-regulated correlated with the level of drug resistance (Che et al. 2019). Also, it has been reported that the mutation of CSP receptor gene comD severely attenuates virulence in both mouse models of pneumonia and bacteremia infection (Zhu and Lau 2011). Consequently, based on the above findings, we want to further investigate whether ComD affects biofilm formation by regulating the adhesion and whether comD deficiency has an effect on virulence in S. suis.
In our previous studies, we established that GrpE and ComD are involved in S. suis biofilm formation based on comparative proteomic analyses (Che et al. 2019; Li et al. 2019). We therefore aim to develop GrpE and ComD could serve as an attractive target for the development of novel anti-biofilm drugs.
Materials and methods
Bacterial strains and cells
The Streptococcus suis ATCC 700794 used in this study was purchased from the American Type Culture Collection, and cultured in Todd–Hewitt broth (THB: Summus Ltd, Harbin, Heilongjiang, China) supplemented with 5% (v/v) fetal bovine serum (Sijiqing Ltd, Hangzhou, Zhejiang, China). PK-15 cells (porcine kidney-15) were purchased from the Stem Cell Bank, Chinese Academy of Sciences, and were cultured in 25-cm2 flasks containing high-glucose Dulbecco’s modified Eagle’s medium (DMEM: Gibco, USA) supplemented with 10% fetal bovine serum (PAN Biotech, Germany), 1% (10 mM) MEM nonessential amino acid solution (Solarbio, China), 1% (200 mM) l-glutamine (Hyclone, USA), 100 U/mL penicillin, and 100 μg streptomycin/mL at 37 °C in an atmosphere of 5% CO2.
Construction of the grpE and comD deletion strains
grpE and comD deletion strains of S. suis were constructed via homologous recombination, as described in our previous study (Zhou et al. 2018). At the same time, gfp (green fluorescent protein) gene was introduced as a selection marker (Kong et al. 2020), and the gene deletion strains were screened by flow cytometry. Briefly, the grpE_A, grpE_B, grpE_C, and gfp genes were amplified from the S. suis ATCC 700794 strain using three pairs of primers (Table 1) designed from the sequence of the S. suis NCTC 10234 strain (GenBank accession number LS483418.1). The upstream fragments of the grpE gene, gfp fragments, and downstream fragments of the grpE gene (gfp-grpE) were linked via overlap PCR and cloned into a pClone007 simple vector for ligation. The ligated products were then transformed into Escherichia coli DH5α cells. Subsequently, the constructed gfp-grpE plasmid was transformed into S. suis ATCC 700794 electroporation-competent cells via electro-transformation and thereafter cultured on THB solid medium containing spectinomycin (100 μg/mL) at 28 °C for 48 h. Having identified colonies of the desired strain, the cells were inoculated into THB medium lacking spectinomycin for subculture. Different generations of bacteria were screened by flow cytometry (Fig. 1), and the grpE deletion strain was identified based on PCR analysis. The comD deletion strain was constructed using the same method with primers (Table 1) designed from the sequence of the S. suis R 61 strain (GenBank accession number AEYY01000051.1). Primer synthesis in this study was provided by Comate Bioscience Co., Ltd.
Cell adhesion assays
Cell adhesion assays were performed as described previously, with some modifications (Li et al. 2018; Wang et al. 2020b). Briefly, PK-15 cells were grown on 24-well tissue culture plates and cultivated overnight in high-glucose DMEM supplemented with 10% FBS until typically 80–90% confluence. Then semi-confluent monolayers of PK-15 cells were cultured in 24-well tissue culture plates with 1 mL experimental medium (high-glucose DMEM without FBS) containing 1.0 × 108 CFU/mL of wild-type S. suis or deletion strains (exponential-phase bacteria) at 37 °C for 3 h, by which time the S. suis cells had attached to the PK-15 cells. At the same time, a negative control group containing only PK-15 cells with 1 mL experimental medium (high-glucose DMEM without FBS) at 37 °C for 3 h. After that, having washed the cells six times with PBS, and the semi-confluent monolayers of PK-15 cells were treated with 200 μL 0.25% trypsin–EDTA for 10 min. Then the cell lysates were collected, vortex-mixed for 1 min to release all bacterial cells, and serially diluted with the experimental medium. Appropriate dilutions were plated on THB agar plates for enumeration of viable bacteria. The experiment was performed in three independent biological replicates. The respective bacterial adhesion rates were calculated using the following formula (Li et al. 2018; Zhang et al. 2015).
Biofilm formation assays
Biofilms of the wild-type strain and the grpE and comD deletion strains were formed in 96-well microtiter plates (Polystyrene) and stained with crystal violet (Sularbao Ltd., Beijing, China), as previously described (Wang et al. 2017). Briefly, the wild-type and deletion strains were cultured overnight in THB at 37 °C and thereafter diluted to a concentration of 1 × 105 CFU/mL, 200-μL aliquots of which were added to each well of a 96-well microtiter plate. At the same time, the same amount of THB was added as the negative control. After that, biofilms were incubated without shaking for 12, 24, 36, 48, 60, and 72 h at 37 °C. After rinsing three times with 200 μL PBS, the attached bacteria remaining in each well were fixed with 200 μL of 99% methanol and stained with 200 μL of 0.1% crystal violet at room temperature for 30 min. The CV-stained biofilm was solubilized with 200 μL of 33% (v/v) glacial acetic acid (Sularbao Ltd., Beijing, China), and sample absorbances were measured at 600 nm. The experiment was performed in three independent biological replicates.
Scanning electron microscopy (SEM)
SEM was performed as described previously (Wang et al. 2017). Briefly, 2-mL aliquots of cultures of the wild-type strain and grpE and comD deletion strains were added to each well of a six-well microplate containing 10 × 10 mm sterilized rough organic membrane (Mosutech Co., Ltd., Shanghai, China), respectively, on the bottom and incubated without shaking at 37 °C for 72 h. Biofilms were fixed with fixative solution [2 mM CaCl2 in 0.2 M cacodylate buffer, 2.5% (w/v) glutaraldehyde, 4% (w/v) paraformaldehyde, pH 7.2] for 6 h and washed with PBS. The preparations were then dehydrated in increasing concentrations of ethanol (30%, 50%, 70%, 90%, and twice in 100%) for 15 min each and thereafter fixed in 2% osmium tetroxide containing 6% (w/v) sucrose and 2 mM potassium ferrocyanide in cacodylate buffer. The samples were then dried, gold-sputtered using an ion-sputtering instrument (current 15 mA, 2 min), and observed using an S-3400N scanning electron microscope (Hitachi, Tokyo, Japan).
Mouse model of S. suis infection
All procedures used in this experiment were reviewed and approved by the Institutional Animal Care and Use Committee of Northeast Agricultural University (No. NEAUEC20). Mouse challenge experiments using S. suis were conducted under standard laboratory conditions in accordance with National Research Council recommendations (Lavagna et al. 2020). Sixty 6-week-old specific pathogen-free (SPF)-grade female BALB/c mice were obtained from the Experimental Animal Center of the Second Affiliated Hospital of Harbin Medical University. The mice were rendered transiently neutropenic via administration of intraperitoneal injections of cyclophosphamide (Hengrui, Medicine, Jiangsu, China) at 4 days pre-infection at 150 mg/kg and at 1 day pre-infection at 100 mg/kg, as previously described (Guo et al. 2016; Kato et al. 2019; Asempa et al. 2020). Mice were infected with S. suis as described previously, with slight modifications (Wang et al. 2020a, 2019). Briefly, aliquot obtained from overnight bacterial culture was inoculated in fresh THB broth (1:100). The bacterial density was quantified by measuring the absorbance at 600 nm. And then the cultured bacteria were diluted with PBS to determine the optimal infection dose in the infection experiment. The mice were thereafter randomly divided into four groups (15 mice per group), and respectively inoculated with 200 μL (1 × 109 CFU) of the wild-type strain, grpE deletion strain, or comD deletion strain via intraperitoneal injection. A further group of 15 mice, used as negative controls, were treated with an equal volume of aseptic normal saline. In short, BALB/c mice were randomly infected with 1 × 109 CFU of the grpE deletion, comD deletion, or wild-type strain, or were mock-infected with normal saline. Mice were monitored at 6-h intervals until 24 h post-infection (hpi) for clinical signs of sepsis, such as depression, swollen eyes, rough hair coat, and lethargy. Five mice from each group were humanely euthanized at 6, 12, and 24 hpi, and any mice exhibiting extreme lethargy during the course of the experiment were considered moribund and were humanely euthanized (Wang et al. 2020a).
Detection of bacteria in the blood, brain, spleen, liver, and lungs
S. suis that had invaded the blood, brain, spleen, liver, and lungs collected at 6 hpi were assessed using the flat colony counting method. Blood samples were gradient diluted and spread on THB agar plates. In the case of the brain, spleen, liver, and lungs, 0.02 g samples were homogenized in 1 mL of PBS, and the resulting homogenates were then gradient diluted and spread on THB agar plates. The plates were incubated overnight at 37 °C, and the following day, the numbers of single colonies were counted.
Histopathology examinations
Samples of the brain, spleen, liver, and lungs collected at 12 hpi were fixed in 4% formaldehyde solution, embedded in paraffin, and sliced to a thickness of 4 μm. Tissue sections were stained with hematoxylin and eosin and examined blindly by an experienced professional pathologist for the presence of lesions.
Cytokine analysis
Serum samples collected at 6, 12, and 24 hpi were used for the detection of IL-6, IL-1β, and TNF-α using commercial ELISA kits (Mebio, Shanghai, China) according to the manufacturer’s instructions. The amounts of cytokines (pg/mL) within sera were calculated based on reference to a standard curve generated from the recombinant mouse cytokines supplied in the kits.
Statistical analysis
All experimental procedures were conducted in triplicate. All the data were visualized as mean ± standard deviation (M ± SD). The Student’s t test or one-way analysis of variance (ANOVA) followed by Tukey's post hoc test for multiple comparisons was employed by SPSS statistical software package (version 17.0). Different levels of statistical significance were set at P < 0.05 and P < 0.01.
Results
GrpE and ComD facilitate S. suis adherence to PK-15 cells and contribute to biofilm formation
As shown in Fig. 2, grpE and comD deletion strains weakened the adhesion of S. suis to PK-15 cells. Adhesion of grpE and comD deletion strains and the wild-type strain were assessed by culturing lysed PK-15 cells on THB agar plates, and calculating CFU values to compare the adherence capacities of the different S. suis strains. The state of different S. suis strains adhering to the THB agar plates can be intuitively observed and counted. We accordingly determined CFU values of approximately 1 × 105 and 3 × 106 for the grpE and comD deletion strains, respectively, which were significantly lower than the CFU of 8.5 × 106 obtained for the S. suis wild-type strain (P < 0.01) (Fig. 2A). These observations thus provide evidence indicating that both grpE and comD play roles in the S. suis adherent process, and that the deletion of either of these two genes has the effect of weakening the adherence of S. suis to PK-15 cells. On the basis of these findings, we calculated the respective bacterial adhesion rates and accordingly obtained adhesion percentage values of < 2% and < 40% for the grpE and comD deletion strains, respectively (P < 0.01) (Fig. 2B).
The effects of grpE and comD deletion on Streptococcus suis adhesion to PK-15 cells. A Adherent bacteria (CFUs) of a grpE and comD deletion strain. B Percentage adhesion of the grpE and comD deletion strains. For each strain, adhesion assays were performed in triplicate. The results are reported as the means ± SDs. Means that differ significantly (**P < 0.01) from those for the wild-type strain are indicated with asterisks
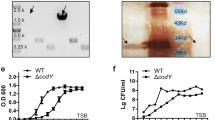
In general, stable mature S. suis biofilms can be detected after culturing for 72 h (Zhao et al. 2015). In the present study, we assessed the effects of GrpE and ComD on S. suis biofilm formation based on crystal violet staining and SEM observations. We accordingly found that after 12, 24, 36, 48, 60 and 72 h of incubation, the OD600 values of crystal violet-stained grpE and comD deletion strains were between 0.2 and 0.4, and 0.1 and 0.3, respectively, which were significantly lower than the values of 0.3 to 0.7 obtained for the wild-type strain of at the same six time points (P < 0.01) (Fig. 3A). These results thus indicate that GrpE and ComD might play important roles in the early stages of biofilm formation, and thus their deletion causes a reduction in S. suis adhesion ability, and consequently hampers biofilm formation. The morphological structures of the respective biofilms were also examined using SEM (Fig. 3B). We established that in the wild-type strain, the complete biofilm structure had developed after 72 h of incubation, and observed that the rough organic membrane surface was almost completely covered by aggregates and micro-colonies. In contrast, after the same length of incubation, the surface of the rough organic membrane of cells co-cultured with the grpE and comD deletion strains was observed to be only sparsely covered by aggregates and micro-colonies, and the gaps in the biofilm formed by the comD deletion strain became large and scattered, and when viewed at high magnification, were found to be surrounded by single or chains of bacterial cells.
Biofilm formation of wild-type and grpE and comD deletion strains of Streptococcus suis. A Biofilm formation of the wild-type, grpE deletion, and comD deletion strains at different periods stained by the crystal violet. Quantification of biofilm formation ability of the wild-type, grpE deletion, and comD deletion strains at 12, 24, 36, 48, 60, and 72 h. B Structures of the biofilms produced by wild-type S. suis and the grpE and comD deletion strains were directly observed by scanning electron microscopy (Scale bars: 2 μm). For each strain, adhesion assays were performed in triplicate. The results are reported as the means ± SDs. Means that differ significantly (**P < 0.01) from those for the wild-type strain are indicated with asterisks
GrpE and comD deletions reduce the severity of S. suis-induced infection symptoms and lower bacteremia in a mouse model
In this study, we used a mouse infection model to assess the contribution of the grpE and comD genes to bacterial virulence. Mice infected with the wild-type S. suis showed prominent clinical signs at 6 h post-inoculation (hpi), including lethargy, arched back, lower body temperature, anorexia, emaciation, rough appearance of hair coat, and swollen eyes. Apart from those mice showing the most pronounced symptoms, which were humanely euthanized mice at 6 or 12 hpi, the remaining mice exhibited extreme lethargy during the period from 18 to 24 hpi, and were likewise humanely euthanized. In contrast, those mice inoculated with either the grpE- or comD-deletion strain were characterized by mild symptoms during the course of the experiment, including a slightly arched back, rough appearance of hair coat, and swollen eyes. With the exception of those mice humanely euthanized at 6 and 12 hpi, others survived to 24 hpi, and after 18 hpi, there was a gradual reduction in clinical symptoms and recovery to a normal appearance and stability, which were maintained until the experiment was terminated.
The bacterial burdens associated with three different strains were monitored by counting colonies after plating blood and organ suspension (in PBS) on THB agar plates. At 6 hpi, we obtained colony counts of approximately 1.15 × 104 CFU/mL and 2.06 × 106 CFU/mL for the grpE and comD deletion strain-infected mice, respectively, on the blood THB agar plates, which were significantly lower than the mean 9.20 × 107 CFU/mL count obtained for the wild-type strain-infected mice (Fig. 4A). Correspondingly, the mean bacterial burdens in organs of the grpE and comD deletion strain-infected mice were respectively as follows: 1.95 × 104 CFU/g and 4.15 × 104 CFU/g (brain) (Fig. 4B), 2.03 × 106 CFU/g and 2.65 × 106 CFU/g (liver) (Fig. 4C), 5.89 × 106 CFU/g and 5.70 × 106 CFU/g (spleen) (Fig. 4D), and 5.50 × 103 CFU/g and 8.9 × 106 CFU/g (lung) (Fig. 4E). In each case, these counts were significantly lower than those obtained for the wild-type strain-infected mice, the means of which are as follows: 1.07 × 105 CFU/g (brain) (P < 0.01) (Fig. 4B), 1.17 × 107 CFU/g (liver) (P < 0.01) (Fig. 4C), 2.85 × 107 CFU/g (spleen) (P < 0.01) (Fig. 4D), and 1.05 × 108 CFU/g (lung) (P < 0.01) (Fig. 4E). These results accordingly indicate that knockout of the grpE and comD genes can effectively reduce the bacterial burden of S. suis.
The bacterial burden in the blood, brain, liver, spleen, and lungs of mice infected with wild-type, grpE deletion, and comD deletion strains at 6 h post-infection. Tissues were collected, homogenized, and plated on THB agar plates for the assessment of CFU counts (n = 5). Bacterial burdens in the blood (A), brain (B), liver (C), spleen (D), and lungs (E) of deletion strain-infected mice were lower than those detected wild-type-infected mice. The results are reported as the means ± SDs. Means that differ significantly (**P < 0.01) from those for the wild-type strain are indicated with asterisks
Deletion of GrpE and ComD attenuated the organ-invasive capacity of S. suis
The main gross lesions in the brain, lungs, liver, and spleen of infected mice were evaluated using mice that were humanely euthanized at 12 hpi (Fig. 5A–C). Compared with the negative control mice, the wild-type strain-infected mice showed slight bleeding in the brain, obvious bleeding or congestion in the lungs, a deeper pigmentation in the liver, and no obvious lesions in the spleen. Correspondingly, all the changes observed upon autopsy of mice infected with the grpE and comD gene deletion strains were less pronounced than those seen in the wild-type strain-infected mice. These observations accordingly indicate that knockout of the grpE and comD genes can attenuate the organ-invasive capacity of S. suis.
Clinical necropsy observations of Streptococcus suis-infected mice. Pathological changes in vision in the strains. For comparison, the brain, lung, liver, and spleen from mice infected with the wild-type strain (A) and gene deletion strains (B, C) are shown at 12 h post-infection. Compared with the wild-type-infected mice, those infected with the gene deletion strains were characterized by slight bleeding in the brain; minor bleeding in the lung or congestion when the chest was opened; and a lighter liver pigmentation (Arrows: the appearance of infected with wild-type strain was characterized by bleeding in the brain and lung). However, no obvious changes were detected in the spleen
To further evaluate the pathological changes induced by infection with the different S. suis strains, we examined the most prominent histopathological lesions at 12 hpi. The brain cells of wild-type strain-infected or gene deletion strain-infected mice were in each case found to be regularly arranged, the meningeal structure was clear, and we detected no obvious histopathological lesions (Fig. 6A). However, the lungs of wild-type strain-infected mice were characterized by broken alveolar walls, and large cavities had developed in the alveoli, which was accompanied by evidence of emphysema (red arrows). Notably, these changes were more pronounced than those observed in the lungs of mice infected with the gene deletion strains (Fig. 6B). The spleen of the wild-type strain-infected mice was thickened, and a large number of hemosiderin-containing particles were detected in the red pulp (red arrows), whereas no comparable abnormalities were observed in the spleens of mice infected with the deletion strains (Fig. 6C). The livers of mice infected with all three strains were found to be characterized by diffuse hydropic degeneration, which may have been attributable to the accumulation of water or fat. Moreover, the cytoplasm of liver cells was observed to be loose and slightly stained. Liver degeneration was, however, more severe in those mice infected with the wild-type strain (Fig. 6D). Thus, the data obtained for both the clinical symptoms and gross histopathological lesions provide evidence to indicate that the grpE and comD genes are both important virulence factors for S. suis, the deletion of either of which will attenuate the ability of this bacterium to invade host organs.
Histopathological lesions in the organs of mice infected with wild-type Streptococcus suis and grpE and comD deletion strains. Histopathological analysis in the strains. Mice were infected with 1 × 109 CFU of S. suis and samples were collected at 12 h post-infection for histopathological lesion observations (Scale bars: 50 μm). A Brain tissue showing no significant changes in the brain cells. B Lung alveoli developed large cavities, which was accompanied by evidence of emphysema; however, less emphysema was observed in deletion strain-infected mice compared with those infected with the wild-type strain (Red arrows: the appearance of emphysema). C Spleen tissue from a wild-type-infected mouse, showing an increase in hemosiderin-containing particles in the red pulp (red arrow), whereas no significant differences were detected between negative control mice and the gene deletion strain-infected mice. D Livers were characterized by diffuse hydropic degeneration, although less pronounced differences were observed in the livers of mice infected with the gene deletion strains
Deletion of the S. suis grpE and comD genes modulates serum cytokine dynamics
To assess the effects of grpE and comD deletion on host pro-inflammatory responses, we evaluated the serum levels of the cytokines IL-6, IL-1β, and TNF-α at 6, 12, and 24 hpi using enzyme-linked immunosorbent assay (ELISA) kits. We accordingly found that the serum IL-6 levels of mice infected with the wild-type strain had increased to 107.40 pg/mL at 6 hpi and subsequently peaked at 115.00 pg/mL at 12 hpi, which were found to be significantly higher than the levels detected in the sera of mice infected with the grpE and comD deletion strains, with respective values of 6 68.53 pg/mL and 90.00 pg/mL being obtained at 6 hpi, and 75.34 pg/mL and 93.28 pg/mL at 12 hpi (P < 0.05). Comparatively we obtain serum IL-6 levels ranging from approximately 59.49 to 65.78 pg/mL within samples collected from negative control mice at the designated time points (Fig. 7A). Serum IL-1β levels in wild-type strain-infected mice had increased to 127.93 pg/mL at 6 hpi, with similar expression levels being detected at 12 hpi, which again was significantly higher than the values of 110.69 pg/mL at 6 hpi and 77.96 pg/mL at 12 hpi measured in the sera of mice infected with the grpE deletion strain (P < 0.05). Contrastingly, however, we detected no significant difference regarding the values obtained from mice infected with the comD deletion strain at 6 hpi or 12 hpi (P > 0.05). For the negative control mice, the levels of serum IL-1β levels measured in all samples were between approximately 68.41 and 76.09 pg/mL (Fig. 7B). The expression of serum TNF-α in the wild-type strain-infected mice had increased to 715.92 pg/mL at 6 hpi, with comparable expression levels being detected at 12 hpi, which is higher significantly higher than the values obtained for mice infected with the grpE and comD deletion strains at 6 hpi, measured as 370.85 and 606.71 pg/mL at 6 hpi, and 393.79 and 570.92 pg/mL at 12 hpi, respectively (P < 0.05). Values obtained for serum TNF-α levels in the negative control mice were within the range of 369.66 to 380.09 pg/mL (Fig. 7C).
Cytokine levels in the blood of mice infected with wild-type Streptococcus suis and grpE and comD deletion strains. Levels of the cytokines IL-6 (A), IL-1β (B), and TNF-α (C) in the blood of infected mice were evaluated by ELISA (n = 5). Data were expressed as the mean ± SD (n = 5); the significant difference between groups was shown by the different letters above the histogram. a,b,c,d Significant differences at P < 0.05
Discussion
Streptococcus suis is difficult to treat and responsible for various infections in humans and pigs. It can also form biofilms and induce persistent infections (Li et al. 2018). Therefore, the research on the regulation mechanism of biofilm and the search for new drug targets to improve the prevention and treatment of streptococcus disease have become one of the focuses of S. suis research community scientific researchers. Although the protein GrpE and histidine protein kinase ComD have been reported to regulate biofilm formation factors in several species of pathogenic bacteria, there have been relatively few studies on the function of these two proteins in Streptococcus suis. In this study, we examined the functions of GrpE and ComD based on the construction of grpE and comD deletion strains of S. suis, which were duly found to be characterized by weakened adhesion to PK-15 cells, irregular biofilm formation, attenuated ability to invade host organs, and modulated host serum cytokine dynamics compared with the wild-type strain. These observations not only provide convincing evidence of the involvement of S. suis GrpE and ComD in bacterial adherence to PK-15 cells and biofilm formation but also of an association with virulence of this pathogen.
The adhesion of S. suis to host tissues or cells represents a critical step in the invasion of host cells. It has previously been proven that certain bacterial adhesins, such as the glyceraldehyde phosphate dehydrogenase, fibronectin binding protein, and glucose 6-phosphate dehydrogenase of S. suis, play important roles in adhesion, and it is thus speculated that they are functionally active in the infection and invasion processes of this bacterium (Li et al. 2018; Wang et al. 2020b). Consistently, in the present study, we demonstrated that GrpE and ComD contribute to the adherence of S. suis to PK-15 cells. In both bacteria and eukaryotes, GrpE, together with DnaJ and DnaK proteins, are required for the normal functioning of the heat shock protein Hsp70 in biochemical paradigms. For example, in Mycobacterium tuberculosis, molecular chaperones play roles associated with extracellular functions, including bacterial adhesion to host cells (Hickey et al. 2010). GrpE has been shown function as a nucleotide exchange factor involved in cellular protein folding (Murakami et al. 2012). Consequently, we speculate that GrpE might target unfolding proteins and thereby modify surface proteins or the proteins associated with the cell structures to facilitate the adherence of S. suis to PK-15 cells. In pathogenic bacteria, such as Group1 Streptococcus pneumoniae and Streptococcus mutans, ComD has been identified as a transmembrane receptor, which, when activated by CSP, functions in regulating the number of microorganisms in biofilms via CSP-mediated quorum sensing (QS) (Yifang and Yftah 2019). In the present study, we established that a comD deletion strain of S. suis is characterized by a comparatively low level of adhesion, which is conceivably attributable to a genetic defect that leads to reduced expression of a CSP receptor encoded by the comD gene on the bacterial cell surface. By perturbing the bacterial surface CSP-mediated regulation of the QS signaling system, this would thus have the effect of hampering bacterial adhesion (Rowe et al. 2019). On the basis of our collective observations, we accordingly speculate that GrpE and ComD contribute to the adherent properties of S. suis, and can accordingly identify these proteins as putative adhesin proteins. However, the detailed molecular mechanisms underlying the activities of these two proteins warrant further investigation.
At present, the pathogenic mechanism of S. suis is still not well characterized, but the adhesion of S. suis to host tissues or cells is an important step for S. suis to invade and infect host cells. The ability of bacteria to adhere is one of the important manifestations of virulence (Fittipaldi et al. 2012). However, whether the adhesion ability of bacteria can be used as a marker of bacterial pathogenicity, the molecular mechanism in adhesion ability of S. suis has not been well elucidated. This study preliminarily clarified the ability of GrpE and ComD to adhere to PK-15 cells, the ability of bacterial adhesion may be an important manifestation of its virulence, but it is not a decisive factor. This is a follow-up to study the adhesion mechanism of GrpE and ComD and to lay the foundation for a preliminary understanding of the pathogenic mechanism after S. suis infection. The process of bacterial biofilm formation is initiated following the adhesion of cells to a substrate, and we accordingly investigated whether the deletion of GrpE and ComD would have a detrimental effect on biofilm formation by S. suis. Our observations duly indicated that at the assessed time points, the grpE and comD deletion strains of S. suis were characterized by a lower extracellular matrix biomass and biofilm formation capacity compared with the wild-type strain, whereas the comparatively low adhesion percentages confirmed that GrpE and ComD play functional roles in the adhesion phase of biofilm formation. The phenomena observed in the present study are similar to those previously described by Murakami et al., who speculated that the nucleotide exchange factor GrpE might target unfolding protein and thereby modifying cell morphology (Murakami et al. 2012), that is, by interacting with GrpE, DnaK can control the homoeostasis of curli biogenesis at multiple stages to organize the biofilm matrix (Sugimoto et al. 2018). Consequently, GrpE may play a pivotal role in modulating cell surface or structural proteins, thereby influencing bacterial adhesion and biofilm formation. Furthermore, the density sensing system controlled by ComC/D/E encoded proteins is more effective in modifying bacterial density, and inactivation of any single gene encoding the comC/D/E QS system can weaken the biofilm formation capacity of S. mutans and S. gordonii (Suntharalingam and Cvitkovitch 2005). Accordingly, the absence of comD might have the effect of delaying the response to bacterial density, thereby reducing adhesion and biofilm formation. These observations thus indicate that GrpE and ComD play important roles in the adhesion phase of S. suis and consequently the subsequent biofilm formation process. However, the mechanisms whereby these two proteins contribute to this process await further elucidation.
Given that biofilms play a key role in the pathogenesis and persistence of certain infectious bacteria, we also investigated whether the deletion of GrpE and ComD has an effect on the virulence of S. suis, based on a previously described mouse infection model (Wang et al. 2020b). Mice have been used as a suitable model for predicting the pathogenicity and virulence of S. suis isolates (Wang et al. 2020b). In the present work, we aim to characterize the role of GrpE and ComD in pathogenicity to deepen our insights of the zoonotic pathogen streptococcus suis by investigating changes between the wild-type strain and grpE and comD deletion strains. Bacterial invasion and colonization capacities in host tissues and bloodstream are considered as critical events in S. suis pathogenesis (Li et al. 2021). Bacterial Burden was measured on related tissues and blood, as expected, we found that compared with mice infected with the wild-type S. suis, those infected with the grpE or comD deletion strain developed lower bacterial burdens, as well as incurring less severe organ lesions, thus providing evidence that GrpE and ComD are important virulence factors of S. suis, and that inhibition of these two proteins might weaken the adhesion of S. suis, thereby affecting the formation of biofilms and attenuating virulence. These observations would thus tend to confirm our speculation that grpE and comD may be virulence factors or play important roles in virulence and can be considered candidate vaccine antigens (Kim et al. 2018) and drug targets that could be used in the treatment of S. suis infection. Further in vivo assays showed that deletion of grpE and comD significantly inhibited the histopathological lesions in a S. Suis infection model in BALB/c mice. In the tissues examined by clinical autopsy, the deletion of grpE and comD attenuated the organ-invasive capacity of S. suis. Moreover, in order to better understand the histopathological changes, we used histopathological examination. Histopathological examination revealed that deletion of grpE and comD reduced the severity of pathological progression in a mouse model of S. suis infection. These results clearly indicate that GrpE and ComD are necessary for successful infection of S. suis and they play an important role in the virulence of S. suis.
The inhibition of bacterial growth by cytokines is an important facet of the host defense mechanism. It has been reported that pro-inflammatory immune response dominates in the early stages of S. Suis infection (Wang et al. 2022b; Li et al. 2023). Among these cytokines, IL-1β, the major secreted form of IL-1, is a regulatory protein that plays an important role in inflammation and autoimmune diseases, and TNF-α is an important pro-inflammatory cytokine produced primarily by activated monocyte macrophages, whereas IL-6 is a pro-inflammatory cytokine that stimulates B cells to produce a variety of inflammatory mediators involved in immune regulation, three of which are most closely associated the inflammation caused by bacterial infection. S. suis infection modulates pro-inflammatory cytokine dynamics (Wang et al. 2020a), and upon infection, we observed rapid increases on the production of the inflammatory factors IL-1β, TNF-α, and IL-6 in model mice. However, whereas grpE and comD deletion strains also induced the expression of IL-1β, TNF-α, and IL-6, the levels were significantly lower than those detected in the wild-type-infected mice until 12 hpi. These observations thus revealed that deletion of the grpE and comD genes significantly reduced the pro-inflammatory cytokine induction capacity of S. suis. Taken together, GrpE and ComD was essential for the virulence of the zoonotic pathogen S. suis in mouse infection model.
The present study firmed that GrpE and ComD play important roles in bacterial adherence, biofilm formation, they are required for the virulence of S. suis. Our results provide useful insights into the biological functions of GrpE and ComD in the pathogenesis of S. suis infection. Among these, future in vitro studies using porcine cells and in vivo studies in pigs will be necessary to confirm the results obtained herein using mice. Further studies are needed to explore the molecular mechanism of GrpE and ComD, and provide new ideas for the treatment of S. suis biofilm.
Conclusions
In this study, we investigated the roles of GrpE and ComD during the process of S. suis infection, and accordingly found that these two proteins play important roles in bacterial adherence, biofilm formation, virulence, and pro-inflammatory cytokine modulation, thereby indicating their potential utility as suitable drug targets and candidate vaccine antigens. But much work remains to be done to understand their pathogenicity in S. suis.
References
Asempa TE, Motos A, Abdelraouf K, Bissantz C, Zampaloni C, Nicolau DP (2020) Meropenem-nacubactam activity against AmpC-overproducing and KPC-expressing Pseudomonas aeruginosa in a neutropenic murine lung infection model. Int J Antimicrob Agents 55:105838. https://doi.org/10.1016/j.ijantimicag.2019.10.019
Bracher A, Verghese J (2015) The nucleotide exchange factors of Hsp70 molecular chaperones. Front Mol Biosci 2:1–9. https://doi.org/10.3389/fmolb.2015.00010
Che RX, Xing XX, Liu X, Qu QW, Chen M, Yu F, Ma JX, Chen XR, Zhou YH, God’Spower BO et al (2019) Analysis of multidrug resistance in Streptococcus suis ATCC 700794 under tylosin stress. Virulence 10:58–67. https://doi.org/10.1080/21505594.2018.1557505
Fittipaldi N, Segura M, Grenier D, Gottschalk M (2012) Virulence factors involved in the pathogenesis of the infection caused by the swine pathogen and zoonotic agent Streptococcus suis. Future Microbiol 7:259–279. https://doi.org/10.2217/fmb.11.149
Grudniak AM, Wlodkowska J, Wolska KI (2015) Chaperone DnaJ influences the formation of biofilm by Escherichia coli. Pol J Microbiol 64:279–283. https://doi.org/10.5604/01.3001.0009.2123
Guan C, Che F, Zhou H, Li Y, Li Y, Chu J (2020) Effect of rubusoside, a natural sucrose substitute, on Streptococcus mutans biofilm cariogenic potential and virulence gene expression in vitro. Appl Environ Microbiol. https://doi.org/10.1128/aem.01012-20
Guo C, Liao X, Wang M, Wang F, Yan C, Xiao X, Sun J, Liu Y (2016) In Vivo Pharmacodynamics of cefquinome in a neutropenic mouse thigh model of Streptococcus suis serotype 2 at varied initial inoculum sizes. Antimicrob Agents Chemother 60:1114–1120. https://doi.org/10.1128/aac.02065-15
Hickey TBM, Ziltener HJ, Speert DP, Stokes RW (2010) Mycobacterium tuberculosis employs Cpn60.2 as an adhesin that binds CD43 on the macrophage surface. Cell Microbiol 12:1634–1647. https://doi.org/10.1111/j.1462-5822.2010.01496.x
Kato H, Hagihara M, Yokoyama Y, Suematsu H, Asai N, Koizumi Y, Yamagishi Y, Mikamo H (2019) Comparison of the in vivo activities of garenoxacin and levofloxacin in a murine model of pneumonia by mixed-infection with Streptococcus pneumoniae and Parvimonas micra. Jpn J Infect Dis 72:407–412. https://doi.org/10.7883/yoken.JJID.2019.109
Kim WS, Kim J-S, Kim HM, Kwon KW, Eum S-Y, Shin SJ (2018) Comparison of immunogenicity and vaccine efficacy between heat-shock proteins, HSP70 and GrpE, in the DnaK operon of Mycobacterium tuberculosis. Sci Rep 8:1–12. https://doi.org/10.1038/s41598-018-32799-z
Kong J, Wang Y, Qi W, Huang M, Su R, He Z (2020) Green fluorescent protein inspired fluorophores. Adv Colloid Interface Sci 285:102286. https://doi.org/10.1016/j.cis.2020.102286
Lavagna A, Auger JP, Giradin SE, Gisch N, Segura M, Gottschalk M (2020) Recognition of lipoproteins by toll-like receptor 2 and DNA by the AIM2 inflammasome is responsible for production of interleukin-1 beta by virulent suilysin-negative Streptococcus suis serotype 2. Pathogens 9(2):147. https://doi.org/10.3390/pathogens9020147
Li Y, Zhou Y, Ren Y, Xu C, Liu X, Liu B, Chen J, Ding W, Zhao Y, Yang Y (2018) Inhibition of Streptococcus suis adhesion and biofilm formation in vitro by water extracts of rhizoma coptidis. Front Pharmacol 9:371. https://doi.org/10.3389/fphar.2018.00371
Li J, Wang J, Liu Y, Yang J, Guo L, Ren S, Chen Z, Liu Z, Zhang Y, Qiu W et al (2019) Porcine reproductive and respiratory syndrome virus NADC30-like strain accelerates Streptococcus suis serotype 2 infection in vivo and in vitro. Transbound Emerg Dis 66:729–742. https://doi.org/10.1111/tbed.13072
Li Q, Fei X, Zhang Y, Guo G, Shi H, Zhang W (2021) The biological role of MutT in the pathogenesis of the zoonotic pathogen Streptococcus suis serotype 2. Virulence 12:1538–1549. https://doi.org/10.1080/21505594.2021.1936770
Li S, Wang C, Tang YD, Qin L, Chen T, Wang S, Bai Y, Cai X, Wang S (2023) Interaction between porcine alveolar macrophage-tang cells and Streptococcus suis strains of different virulence: phagocytosis and apoptosis. Microorganisms. https://doi.org/10.3390/microorganisms11010160
Murakami J, Terao Y, Morisaki I, Hamada S, Kawabata S (2012) Group A streptococcus adheres to pharyngeal epithelial cells with salivary proline-rich proteins via GrpE chaperone protein. J Biol Chem 287:22266–22275. https://doi.org/10.1074/jbc.M112.350082
Rowe HM, Karlsson E, Echlin H, Chang T-C, Wang L, van Opijnen T, Pounds SB, Schultz-Cherry S, Rosch JW (2019) Bacterial factors required for transmission of Streptococcus pneumoniae in mammalian hosts. Cell Host Microbe 25(884–891):e886. https://doi.org/10.1016/j.chom.2019.04.012
Scherr TD, Roux CM, Hanke ML, Angle A, Dunman PM, Kielian TL (2013) Global transcriptome analysis of Staphylococcus aureus biofilms in response to innate immune cells. Infect Immun 81:4363–4376. https://doi.org/10.1128/IAI.00819-13
Sugimoto S, Arita-Morioka K-I, Terao A, Yamanaka K, Ogura T, Mizunoe Y (2018) Multitasking of Hsp70 chaperone in the biogenesis of bacterial functional amyloids. Commun Biol 1:1–14. https://doi.org/10.1038/s42003-018-0056-0
Suntharalingam P, Cvitkovitch DG (2005) Quorum sensing in streptococcal biofilm formation. Trends Microbiol. https://doi.org/10.1016/j.tim.2004.11.009
Tripathi P, Singh LK, Kumari S, Hakiem OR, Batra JK (2020) ClpB is an essential stress regulator of Mycobacterium tuberculosis and endows survival advantage to dormant bacilli. Int J Med Microbiol 310:151402. https://doi.org/10.1016/j.ijmm.2020.151402
Vötsch D, Willenborg M, Weldearegay YB, Valentin-Weigand P (2018) Streptococcus suis - The “Two Faces” of a pathobiont in the porcine respiratory tract. Front Microbiol 9:480. https://doi.org/10.3389/fmicb.2018.00480
Wang S, Wang C, Gao L, Cai H, Zhou Y, Yang Y, Xu C, Ding W, Chen J, Muhammad I et al (2017) Rutin inhibits Streptococcus suis biofilm formation by affecting CPS biosynthesis. Front Pharmacol 8:379. https://doi.org/10.3389/fphar.2017.00379
Wang Z, Ma J, Wang J, Yang D, Kong L, Fu Q, Cheng Y, Wang H, Yan Y, Sun J (2019) Application of the phage lysin Ply5218 in the treatment of Streptococcus suis infection in piglets. Viruses. https://doi.org/10.3390/v11080715
Wang S, Lyu C, Duan G, Meng F, Yang Y-B, Yu Y, He X, Wang Z, Gottschalk M, Li G et al (2020a) Streptococcus suis serotype 2 infection causes host immunomodulation through induction of thymic atrophy. Infect Immun. https://doi.org/10.1128/iai.00950-19
Wang Y, Yi L, Sun L-Y, Liu Y-C, Wen W-Y, Li X-K, Mei J-J, Ding K, Wu T-C, Grenier D (2020b) Identification and characterization of a Streptococcus suis immunogenic ornithine carbamoytransferase involved in bacterial adherence. J Microbiol Immunol Infect 53:234–239. https://doi.org/10.1016/j.jmii.2018.05.004
Wang B, Song CR, Zhang QY, Wei PW, Wang X, Long YH, Yang YX, Liao SG, Liu HM, Xu GB (2022a) The fusaric acid derivative qy17 inhibits Staphylococcus haemolyticus by disrupting biofilm formation and the stress response via altered gene expression. Front Microbiol 13:822148. https://doi.org/10.3389/fmicb.2022.822148
Wang S, Wang G, Tang YD, Li S, Qin L, Wang M, Yang YB, Gottschalk M, Cai X (2022b) Streptococcus suis serotype 2 infection induces splenomegaly with splenocyte apoptosis. Microbiol Spectr 10:e0321022. https://doi.org/10.1128/spectrum.03210-22
Yang Y, Koirala B, Sanchez LA, Phillips NR, Hamry SR, Tal-Gan Y (2017) Structure-activity relationships of the competence stimulating peptides (CSPs) in Streptococcus pneumoniae reveal motifs critical for intra-group and cross-group ComD receptor activation. ACS Chem Biol 12:1141–1151. https://doi.org/10.1021/acschembio.7b00007
Yang W, Hong Y, Zhang Y, Wang D, Li D, Hou Y (2018a) A potential substrate binding pocket of BdcA plays a critical role in NADPH recognition and biofilm dispersal. Biochem Biophys Res Commun 497:863–868. https://doi.org/10.1016/j.bbrc.2018.02.143
Yang Y, Cornilescu G, Tal-Gan Y (2018b) Structural characterization of competence-stimulating peptide analogues reveals key features for ComD1 and ComD2 receptor binding in streptococcus pneumoniae. Biochemistry 57:5359–5369. https://doi.org/10.1021/acs.biochem.8b00653
Yi L, Fan Q, Wang Y, Mao C, Li J, Jin M, Zhang X, Ding K, Wang Y (2021) Evaluation of immune effect of Streptococcus suis biofilm-associated protein PDH. Vet Microbiol 263:109270. https://doi.org/10.1016/j.vetmic.2021.109270
Yifang Y, Yftah T-G (2019) Exploring the competence stimulating peptide (CSP) N-terminal requirements for effective ComD receptor activation in group1 Streptococcus pneumoniae. Bioorg Chem 89:102987. https://doi.org/10.1016/j.bioorg.2019.102987
Yoneda S, Kawarai T, Narisawa N, Tuna EB, Sato N, Tsugane T, Saeki Y, Ochiai K, Senpuku H (2013) Effects of short-chain fatty acids on Actinomyces naeslundii biofilm formation. Mol Oral Microbiol 28:354–365. https://doi.org/10.1111/omi.12029
Zeng B, Wang C, Zhang P, Guo Z, Chen L, Duan K (2020) Heat shock protein DnaJ in Pseudomonas aeruginosa affects biofilm formation via pyocyanin production. Microorganisms 8(3):395. https://doi.org/10.3390/microorganisms8030395
Zhang X, Jiang X, Yang L, Fang L, Shen H, Lu X, Fang W (2015) DnaJ of Streptococcus suis type 2 contributes to cell adhesion and thermotolerance. J Microbiol Biotechnol 25:771–781. https://doi.org/10.4014/jmb.1408.08085
Zhao Y, Zhou Y, Chen J, Huang Q, Han Q, Liu B, Cheng G, Li Y (2015) Quantitative proteomic analysis of sub-MIC erythromycin inhibiting biofilm formation of S. suis in vitro. J Proteomics 116:1–14. https://doi.org/10.1016/j.jprot.2014.12.019
Zheng C, Wei M, Jia M, Cao M (2020) Involvement of various enzymes in the physiology and pathogenesis of Streptococcus suis. Vet Sci. https://doi.org/10.3390/vetsci7040143
Zhou L, Kang R, Zhang Y, Ding M, Xie B, Tian Y, Wu X, Zuo L, Yang X, Wang H (2018) Whole genome analysis of two novel type 2 porcine reproductive and respiratory syndrome viruses with complex genome recombination between lineage 8, 3, and 1 strains identified in southwestern China. Viruses 10:328. https://doi.org/10.3390/v10060328
Zhou Y, Yu F, Chen M, Zhang Y, Qu Q, Wei Y, Xie C, Wu T, Liu Y, Zhang Z et al (2021) Tylosin inhibits Streptococcus suis biofilm formation by interacting with the O-acetylserine (thiol)-lyase B CysM. Front Vet Sci 8:829899. https://doi.org/10.3389/fvets.2021.829899
Zhu L, Lau GW (2011) Inhibition of competence development, horizontal gene transfer and virulence in Streptococcus pneumoniae by a modified competence stimulating peptide. PLoS Pathog 7:e1002241. https://doi.org/10.1371/journal.ppat.1002241
Funding
This work was supported by the China Agriculture Research System of MOF and MARA, the National Nature Science Foundation of China (Grant No. 31772787) and the Natural Science Foundation of Heilongjiang Province, China (Grant No. LH2020C024).
Author information
Authors and Affiliations
Contributions
YHL and GW designed the whole study. FY and CLD directed the completion of the experiment and drafted the manuscript. YFZ, RXC, CMX, YYL, ZYZ, LL, XYC, XHC were supportive during the experiment. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Yusuf Akhter.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yu, F., Dong, C., Zhang, Y. et al. GrpE and ComD contribute to the adherence, biofilm formation, and pathogenicity of Streptococcus suis. Arch Microbiol 205, 159 (2023). https://doi.org/10.1007/s00203-023-03503-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00203-023-03503-1