Abstract
Multi-drug-resistant (MDR) Enterobacteriaceae pose a global threat to hospitalized patients. We report a series of colistin-resistant Klebsiella pneumoniae blood isolates from Israel and explore their resistance mechanisms using whole genome sequencing (WGS). Patients with colistin-resistant K. pneumoniae bloodstream infection (BSI) were identified during the period between 2006 and 2018. Demographic and clinical data were collected, and antibiotic susceptibility testing (AST) was performed using three commercial platforms. Long and short read sequencing were performed on a PacBio RS II (Pacific Biosciences) and an Illumina Miseq (Illumina), respectively. Thirteen patients with colistin-resistant K. pneumoniae BSI were identified, and seven isolates from seven different patients were successfully revived. Patient records indicated that five of the patients were previously treated with colistin. AST indicated that six of the seven isolates were colistin resistant and four of these isolates were resistant to carbapenems. WGS assigned the isolates to four distinct clusters that corresponded to in silico-derived multi-locus sequence types (MLST). Three isolates carried blaKPC-3 on two different plasmids and one carried blaOXA-48 on a novel IncL/M plasmid. All colistin-resistant isolates carried a variety of different mutations that inactivated the mgrB gene. We report the first comprehensive analysis of a series of colistin-resistant K. pneumoniae from Israel. A diverse set of isolates were obtained and colistin resistance was found to be attributed to different mechanisms that ablated the mgrB gene. Notably, carbapenemase genes were identified in four isolates and were carried on novel plasmids.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multi-drug-resistant (MDR) Enterobacteriaceae pose an increasing threat to patients in health care settings. More than a decade ago, a global epidemic of carbapenemase-producing Enterobacteriaceae (CPE), particularly Klebsiella pneumonia, spread worldwide, and is still associated with increased morbidity and mortality (Xu et al. 2017). Clinical CPE infections are treated with combination therapy that includes colistin as a key component of the regimen.
Recently, acquired colistin resistance has been reported in several studies (Cannatelli et al. 2014; Paterson et al. 2016; Poirel et al. 2016). Acquisition of colistin resistance was found to be mediated by either a plasmid (mcr-1 and mcr-2), or due to alterations in the two-component PhoP/PhoQ and PmrAB regulatory systems or interruption of the mgrB sequence—the latter being the common mechanism of colistin resistance in carbapenem-resistant K. pneumonia (Poirel et al. 2016; Skov et al. 2016; Liu et al. 2016). Colistin resistance has also been reported in non-CPE (Xavier et al. 2016; Antoniadou et al. 2007).
The negatively charged, cell membrane surface layer of Gram-negative bacteria is favorable to the action of polymyxins. Colistin is a polycationic antimicrobial peptide that targets bacterial lipopolysaccharide (LPS), causing cell membrane leakage (Kaye et al. 2016). The PhoP/PhoQ regulatory system activates the PmrAB system which results in neutralization of the negatively charged phospholipids. This electrostatic modification leads to colistin resistance (Moskowitz et al. 2004; Trent et al. 2001; Zhang et al 2000). MgrB is a small transmembrane protein that exerts a negative feedback on the PhoP/PhoQ regulatory system. Hence, disruption of the mgrB gene leads to upregulation of the PmrAB system and neutralization of the negatively charged cell membrane, which leads in turn to colistin resistance.
CPE are considered endemic to Israel. However, since the peak of the outbreak in 2007, infection rates have significantly decreased (largely due to strict cohorting of patients and dedicated staffing), though CPE infections still pose a serious challenge (Leavitt et al. 2007; Schwaber et al. 2011). For example, there are few antimicrobial agents effective against these pathogens. At the Shaare Zedek Medical Center (SZMC), a 1000-bed teaching hospital in Jerusalem, Israel, the annual rate of CPE clinical infections was 28 cases per 100,000 patient days during 2007 and decreased to 3 cases per 100,000 patient days during 2016. Colistin resistance was first reported in Israel only a few years ago. One isolate was from a patient who was a CPE carrier, and further analysis detected colistin resistance attributed to a mutation in the mgrB sequence (Olaitan et al. 2014). In this study, we report a series of colistin-resistant Klebsiella pneumoniae blood isolates from Israel and explore their resistance mechanisms using whole genome sequencing (WGS).
Methods
Strains used in this study
Colistin resistance was previously determined in SZMC using Kirby Bauer disk diffusion assays and E-tests. Patients with colistin-resistant Klebsiella pneumoniae bloodstream infection (BSI) were identified over a 10-year period (2006–2016) utilizing the electronic medical record at the SZMC in Jerusalem, Israel. Identification of K. pneumonia was performed using standard microbiological methods as well as matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (Bruker™ MALDI-TOF MS).
Demographic and clinical data
Demographic and clinical data of bacteremic patients were retrospectively extracted from electronic medical records, including the variables of age, gender, clinical syndrome, Charlson comorbidity score (CCS), length of stay, previous exposure to colistin, and mortality.
All isolates were tested for carbapenemase production using the CarbaNP test (Nordmann et al. 2019), and antimicrobial-susceptibility testing (AST) was performed using three commercial platforms: thePhoenix (Becton Dickinson), Vitek II (bioMérieux) and MicroScan (Siemens Healthcare).
Whole Genome Sequencing and data analysis (WGS) Long- and short-read sequencing were performed on a PacBio RS II (Pacific Biosciences) and an Illumina Miseq (Illumina), respectively. For short-read sequencing, DNA was extracted using the DNeasy UltraClean Microbial Kit (Qiagen, Germantown, MD, USA) and libraries were constructed using the KAPA Hyperplus Library preparation kit (Roche Diagnostics Indianapolis, Indiana, USA). Libraries were quantified using the KAPA Library Quantification Kit—Illumina/Bio-Rad iCycler™ (Roche Diagnostics) on a CFX96 real-time cycler (Biorad, Hercules, CA, USA). For the Miseq, libraries were normalized to 2 nM, pooled, denatured, and diluted to 20 pM. The pooled samples were further diluted to a final concentration of 14 pM. Samples were sequenced using MiSeq Reagent Kit v3 (600 cycle: 2 × 300 bp) (Illumina, San Diego, CA, USA). For long-read sequencing, High-quality, high-molecular-weighted genomic DNA was isolated using the DNeasy UltraClean Microbial Kit (Qiagen, Germantown, MD, USA). SMRTbell™ libraries were then generated using the SMRTbell™ Template Prep Kit 1.0 (Pacific Biosciences) and size-selected using the BluePippin (Sage Science, Beverly, MA, USA). SMRTbell™ libraries were primer annealed, Magbead and polymerase bound using the MagBead Binding Kit v2 and DNA/Polymerase Binding Kit P6 v2 (Pacific Biosciences) and then sequenced using SMRTcells v3.
Kraken2 (Wood et al. 2019) was used to identify isolate species and check for contamination. Short-read sequencing data were trimmed for adapter sequence content and quality using Btrim64 (Kong et al. 2011). Overlapping sequence reads were merged using FLASH (Magoč et al. 2011). De novo assembly was performed using Newbler (V2.7). Minimum thresholds for contig size and coverage were set at 200 bp and 49.5X, respectively. Long-read sequencing data was de novo assembled using HGAP 2.0 in the SMRT Analysis Portal (Pacific Biosciences, Menlo Park, CA). Overlapping contig ends were removed to circularize individual PacBio contigs, and short-read data were mapped to circularized contigs to detect/correct errors. Comparative genomic analyses were performed using Geneious (Biomatters, Auckland, New Zealand) (Kearse et al. 2012). Antimicrobial resistance genes were annotated using a combination of AMRFinderPlus and ARIBA (Feldgarden et al. 2019; Hunt et al. 2017). MLST assignment was performed using mlst (23). Genomes were annotated using the NCBI Prokaryotic Genome Annotation Pipeline version 4.1
Results
Thirteen patients with colistin-resistant Klebsiella pneumoniae bacteremia were identified via the computerized database from 2006 to 2016. Seven isolates were successfully revived. All isolates were re-tested for colistin resistance and six were found to be colistin resistant. Demographic and clinical data of the bacteremic patients are shown in Table 1. The median age of the patients was 79.5 years (range 25–95), four were males. All patients had prolonged admissions (median 34 days, range 21–109). Five of six cases of bacteremia were hospital acquired. All patients were critically ill, bed ridden, and cognitively impaired and four of the 7 patients died during hospitalization. The median CCS was 10 (range 6–12), and four patients required mechanical ventilation. Three patients were colonized with CPE (rectal swab) during admission. Five of the six patients were exposed to colistin within 90 days prior admission. Antimicrobial testing was performed for each isolate using Phoenix (Becton Dickinson), Vitek II (bioMérieux) and MicroScan (Siemens Healthcare) (Table 2). Multiple antimicrobial resistance genes were detected in all isolates.
Colistin resistance
WGS assigned the isolates to four distinct clusters that corresponded to in silico-derived multi-locus sequence types (MLST): ST-11, -14, -15, and -512 (Fig. 1). Both ST-15 strains were essentially identical, differing by just a single nucleotide polymorphism (SNP) and were susceptible to carbapenems. However, both carried extended spectrum beta-lactamase genes (Table 2).
Dendrogram of K. pneumoniae isolates. Dendrogram generated from the whole genome sequence of all seven K. pneumoniae used in this study. Isolates are color-coded by traditional multi-locus sequence type (MLST) and additional K. pneumoniae sequences from NCBI are provided for reference in black text. The number of SNPs separating closely related isolates is shown
Colistin resistance genes were analyzed in the six isolates. All of the isolates were negative for mcr-1 to mcr-10. The mgrB gene was examined in the six colistin-resistant Klebsiella pneumoniae and in one colistin-sensitive isolate. A number of disruptions, mutations, and deletions were identified only in the six resistant strains. Strains 3 and 6 were closely related to one another and to strain 5. However, both strains 3 and 6 had a different mgrB mutation when compared to strain 5 (Table 3). In both strains, ISKpn26 had inserted into the same location in mgrB, disrupting the gene. The characteristic 4 bp target site duplication (TSD) of ISKpn26 movement confirmed that this mobile element had transposed itself into this gene. In contrast, strain 5 had a single base-pair deletion at base 21 (T21Δ) resulting in a STOP codon at amino acid position 9 (Total size of mgrB is 47 amino acids) that is predicted to produce a non-functional MgrB protein.
Similar to strain 5, strain 4 had a single nucleotide polymorphism (SNP) at base 48 (C48A) causing a non-synonymous change from a cysteine residue to a STOP codon (C16STOP). This resulted in a truncated MgrB protein one-third of the total length (16 of 48 amino acids) that was unlikely to function optimally. Both strains 1 and 2 were essentially identical, differing by just a single SNP. Both isolates had completely lost the mgrB sequence, as well as approximately 1608 bp of the surrounding sequence which included two hypothetical genes and part of a gene encoding a cold-shock protein. A schematic illustrating different mgrB mutations is shown in Fig. 2.
Disruption of the mgrB gene. Schematic representation of the various disruptions of the mgrB gene detected in colistin resistant isolates. K. pneumoniae SZMC 1310 is colistin sensitive and contains an intact mgrB gene. Open arrows represent coding sequences with mgrB highlighted in green. Open broken arrows represent truncated genes. Dotted lines indicate regions that have been deleted in K. pneumoniae SZMC 1039 and K. pneumoniae SZMC 1474. The inverted repeats of ISKpn26 are depicted by black vertical lines and the 4 bp target site duplication (TSD) generated upon insertion into mgrB in K. pneumoniae SZMC 1898 and K. pneumoniae SZMC 1368 are shown
Carbapenem resistance
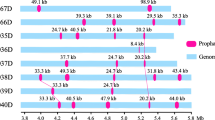
Four isolates, three ST-512 (strains 3, 5, and 6) and one ST-11 (strain 4), were carbapenem resistant and carried blaKPC-3 (strains 3, 5 and 6) and blaOXA-48 (strain 4). A plasmid analysis was performed on the blaKPC-3 (strains 3, 5 and 6) and blaOXA-48 (strain 4). The analysis revealed that blaKPC-3 was carried on an IncFIB plasmid of size 66,188 bp in strain 3 only. In strains 5 and 6, blaKPC-3 was carried on an unknown plasmid. Finally, blaOXA-48 from strain 4 was carried on a 73,424 bp IncL/M plasmid that also carried the blaCTX-M gene (Fig. 3).
Plasmids carrying carbapenemase genes. Alignment of (a) pMR898KPC and its close relative pIT-FIPP-1 (Genbank Accession HG96999), b pMR2215OXA48 and its close relative pIncL_M_DHQP1400954 (Genbank Accession CP016927) and (c) pMR1368KPC and its relative pCAV1453-208 (Genbank Accession CP018355). Arrows indicate confirmed or putative open reading frames (ORFs), and their orientations. Arrow size is proportional to predicted ORF length. Resistance genes are indicated by red arrows, except for carbapenemases (green arrows). Conjugal transfer genes are indicated by yellow arrows. DNA mobilization genes are indicted by white arrows. Plasmid mobility, replication, and maintenance genes are indicated by blue arrows. Hypothetical and unknown genes are indicted by gray arrows. The blue–gray shaded regions between the different alignments indicate nucleotide identity of 97.5%–100% by BLASTN. For clarification, only a subset of gene names are included. Gene nomenclature was assigned based on the closest BLAST match from NCBI (http://blast.ncbi.nlm.nih.gov/Blast.cgi; last accessed August 2018)
Discussion
We report the first comprehensive analysis of a series of colistin-resistant K. pneumoniae from Israel. A diverse set of isolates was obtained and colistin resistance was found to be attributed to several mechanisms that ablated the mgrB gene, which was likely the cause of colistin resistance in these isolates. Several disruptions, mutations, and deletions were identified as suggested in Fig. 2. No mcr genes were detected. Defects in the mgrB gene have been previously reported as a common mechanism of colistin resistance in K. pneumonia. Those included insertion of sequences (insertional inactivation) such as an IS5-like element, IS903B, IS1F-like ISKpn13, ISKpn14, IS10R, and other insertional elements (Poirel et al. 2016; Olaitan et al. 2014; Cannatelli et al. 2013; López-Camacho et al. 2013; Gaibani et al. 2014) leading to a truncated protein. This alteration is frequently induced by colistin exposure. Missense and non-sense mutations as well as small or complete deletions of the mgrB gene leading to impaired or no synthesis of the protein (Cannatelli et al. 2014; Poirel et al. 2016; Olaitan et al. 2014) had also been observed. Finally, restoration of colistin susceptibility was achieved in complementation studies carried out on some of these mgrB mutant strains (Cannatelli et al. 2013, 2014).
In this study, colistin-resistant K. pneumoniae isolates were identified as early as 2006, and two strains were carbapenem susceptible (Table 2). Five of the six patients with colistin-resistant K. pneumoniae were exposed to colistin within 90 days of bacteremia, in-line with previous reports suggesting that colistin exposure is associated with mgrB gene disruption and colistin resistance (Cannatelli et al. 2013). While there have been case reports and outbreaks involving carbapenem-resistant K. pneumonia resistant to polymyxin B, the carbapenemase genes we identified in four isolates were carried on novel plasmids. Additionally, the MICs to imipenem were unusually high. These higher MIC isolates may be associated with increased resistance to other categories of antimicrobials, as well as infections requiring higher doses of carbapenems.
We did not detect any mcr genes among the resistant isolates. These genes also play a role in the reduction of the negative discharge on the outer membrane, which leads to colistin resistance. Since first identified in 2015 in a transferable plasmid in E. coli isolates from animals and humans in China (Liu et al. 2016), plasmid-borne mcr alleles have been widely reported, most commonly mcr-1 and to less extent mcr-2–9 (Luo et al. 2017; Wang et al. 2020; Kieffer et al. 2019). The emergence and dissemination of mcr genes-associated colistin resistance is attributed to extensive use of colistin as an animal feed additive (growth promoter), primarily in poultry and swine industries (Wang et al. 2020). In Israel, mcr genes have never been reported, perhaps due to the limited swine industry.
Our study presents data showing that not only does colistin-resistant K. pneumoniae continue to cause serious infections in hospitalized patients, but also the bacteria appear to be creating novel ways to evade our shrinking armamentarium of available antibiotic options. Infection control and antibiotic stewardship programs have become an important fixture of medical centres, and for good reason. At the SZMC, cohorting of colistin-resistant K. pneumonia began in 2012. We identified 10 colistin-resistant K. pneumonia isolates prior to 2013, and only 6 from 2013 to the present. Also affecting this possible decline may be the way colistin had been used in the recent past at our facility. Over the past few years, empiric use of low dose colistin has slowed dramatically, possibly exerting less selective pressure on the resistome. This decline in resistant isolates may even be an underestimate, as they were diagnosed by the E-test method, not always a reliable method of susceptibility testing (Katz et al. 2016). However, as of 2020, colistin-resistant K. pneumonia strains are still being detected at our medical centre. As whole genome sequencing becomes more mainstream, further studies should utilize this developing technology to describe the epidemiology of these resistant organisms and their clinical impact.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Antoniadou A, Kontopidou F, Poulakou G et al (2007) Colistin-resistant isolates of Klebsiella pneumoniae emerging in intensive care unit patients: first report of a multiclonal cluster. J Antimicrob Chemother 59:786–790
Cannatelli A, D’Andrea MM, Giani T et al (2013) In vivo emergence of colistin resistance in Klebsiella pneumoniae producing KPC-type carbapenemases mediated by insertional inactivation of the PhoQ/PhoP mgrB regulator. Antimicrob Agents Chemother 57:5521–5526
Cannatelli A, Giani T, D’Andrea MM et al (2014) COLGRIT Study Group. MgrB inactivation is a common mechanism of colistin resistance in KPC-producing Klebsiella pneumoniae of clinical origin. Antimicrob Agents Chemother. 58:5696–5703
Feldgarden M, Brover V, Haft DH et al (2019) Validating the AMRFinder tool and resistance gene database by using antimicrobial resistance genotype-phenotype correlations in a collection of isolates. Antimicrob Agents Chemother 63:e00483-e519
Gaibani P, Lombardo D, Lewis RE et al (2014) In vitro activity and post-antibiotic effects of colistin in combination with other antimicrobials against colistin-resistant KPC-producing Klebsiella pneumoniae bloodstream isolates. J Antimicrob Chemother 69:1856–1865
Hunt M, Mather AE, Sánchez-Busó L et al (2017) ARIBA: rapid antimicrobial resistance genotyping directly from sequencing reads. Microb Genom 3:e000131
Katz DE, Marchaim D, Assous MV et al (2016) Ten years with colistin: a retrospective case series. Int J Clin Pract 70:706–711
Kaye KS, Pogue JM, Tran TB et al (2016) Last Resort: polymyxin resistance. Infect Dis Clin North Am 30:391–414
Kearse M, Moir R, Wilson A et al (2012) Geneious Basic: an integrated and extendable desktop software platform for the organization and analysis of sequence data. Bioinformatics 28:1647–1649
Kieffer N, Royer G, Decousser JW et al (2019) mcr-9, an inducible gene encoding an acquired Phosphoethanolamine Transferase in Escherichia coli, and its origin. Antimicrob Agents Chemother 63:e00965-e1019
Kong Y (2011) Btrim: A fast, lightweight adapter and quality trimming program for next-generation sequencing technologies. Genomics 98:152–153
Leavitt A, Navon-Venezia S, Chmelnitsky I et al (2007) Emergence of KPC-2 and KPC-3 in carbapenem-resistant Klebsiella pneumoniae strains in an Israeli hospital. Antimicrob Agents Chemother 51:3026–3029
Liu YY, Wang Y, Walsh TR et al (2016) Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis 16:161–168
López-Camacho E, Gómez-Gil R, Tobes R et al (2013) Genomic analysis of the emergence and evolution of multidrug resistance during a Klebsiella pneumoniae outbreak including carbapenem and colistin resistance. J Antimicrob Chemother. 69:632–636
Luo Q, Yu W, Zhou K et al (2017) Molecular Epidemiology and Colistin Resistant Mechanism of mcr-Positive and mcr-Negative Clinical Isolated Escherichia coli. Front Microbiol 8:2262
Magoč T, Salzberg SL (2011) FLASH: fast length adjustment of short reads to improve genome assemblies. Bioinformatics 27:2957–2963
Moskowitz SM, Ernst RK, Miller SI (2004) PmrAB, a two-component regulatory system of Pseudomonas aeruginosa that modulates resistance to cationic antimicrobial peptides and addition of aminoarabinose to lipid A. J Bacteriol 186:575–579
Nordmann P, Poirel L (2019) Epidemiology and diagnostics of carbapenem resistance in gram-negative bacteria. Clin Infect Dis 69:S521–S528
Olaitan AO, Diene SM, Kempf M et al (2014) Worldwide emergence of colistin resistance in Klebsiella pneumoniae from healthy humans and patients in Lao PDR, Thailand, Israel, Nigeria and France owing to inactivation of the PhoP/PhoQ regulator mgrB: an epidemiological and molecular study. Int J Antimicrob Agents 44:500–507
Paterson DL, Harris PN (2016) Colistin resistance: a major breach in our last line of defense. Lancet Infect Dis 16:132–133
Poirel L, Kieffer N, Liassine N et al (2016) Plasmid-mediated carbapenem and colistin resistance in a clinical isolate of Escherichia coli. Lancet Infect Dis 16:281
Schwaber MJ, Lev B, Israeli A et al (2011) Israel Carbapenem-Resistant Enterobacteriaceae Working Group. Containment of a country-wide outbreak of carbapenem-resistant Klebsiella pneumoniae in Israeli hospitals via a nationally implemented intervention. Clin Infect Dis. 52:848–855
Skov R, Monnet D (2016) Plasmid-mediated colistin resistance (mcr-1 gene): three months later, the story unfolds. Euro Surveill 21:30155
Trent MS, Ribeiro AA, Lin S et al (2001) An inner membrane enzyme in Salmonella and Escherichia coli that transfers 4-amino-4-deoxy-L-arabinose to lipid A: induction on polymyxin-resistant mutants and role of a novel lipid-linked donor. J Biol Chem 276:43122–43131
Wang Y, Xu C, Zhang R et al (2020) Changes in colistin resistance and mcr-1 abundance in Escherichia coli of animal and human origins following the ban of colistin-positive additives in China: an epidemiological comparative study. Lancet Infect Dis 20:1161–1171
Wood DE, Lu J, Langmead B (2019) Improved metagenomic analysis with Kraken 2. Genome Biol 20:257
Xavier BB, Lammens C, Ruhal R et al (2016) Identification of a novel plasmid-mediated colistin-resistance gene, mcr-2, in Escherichia coli, Belgium, June 2016. Euro Surveill. 21:30280
Xu L, Sun X, Ma X (2017) Systematic review and meta-analysis of mortality of patients infected with carbapenem-resistant Klebsiella pneumoniae. Ann Clin Microbiol Antimicrob 16:18
Zhang L, Dhillon P, Yan H et al (2000) Interactions of bacterial cationic peptide antibiotics with outer and cytoplasmic membranes of Pseudomonas aeruginosa. Antimicrob Agents Chemother 44:3317–3321
Funding
We received no funding for this study.
Author information
Authors and Affiliations
Contributions
EB-C (clinical data collection and analysis, manuscript formation), PM (whole genome sequencing and report formation, manuscript formation), Rosslyn Maybank (whole genome sequencing), Jason Stam (whole genome sequencing), MVA (microbiology sample acquisition, preparation, and initial testing), DEK (clinical data collection and analysis, manuscript formation).
Corresponding author
Ethics declarations
Conflict of interest
All authors have passed final approval on the manuscript that is currently being submitted. No conflicts of interests were declared by any of the authors regarding the content of this report.
Additional information
Communicated by Erko Stackebrandt.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ben-Chetrit, E., Mc Gann, P., Maybank, R. et al. Colistin-resistant Klebsiella pneumoniae bloodstream infection: old drug, bad bug. Arch Microbiol 203, 2999–3006 (2021). https://doi.org/10.1007/s00203-021-02289-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00203-021-02289-4