Abstract
Brucellosis is an infectious disease that affects practically all species of mammals, including human, and is a major zoonosis worldwide. Brucella spp. are facultative intracellular pathogens that have the ability to survive and multiply in phagocytic and nonphagocytic cells such as trophoblast and epithelial cells. Among the six recognized species of the genus Brucella, Brucella melitensis is the main etiological agent involved in goat brucellosis and is also the most pathogenic for human. It causes significant losses in livestock production as a result of abortions, metritis, infertility, and birth of weak animals. Outer membrane proteins (OMPs) are exposed on the bacterial surface and are in contact with cells and effectors of the host immune response, whereby they could be important virulence factors of Brucella species. To evaluate this hypothesis, the gene encoding for the major outer membrane protein Omp31 was amplified, cloned into pUC18 plasmid, and inactivated by inserting a kanamycin cassette, rendering pLVM31 plasmid which was transformed into B. melitensis wild-type strain to obtain LVM31 mutant strain. The Outer membrane (OM) properties of the mutant strain were compared with B. melitensis Bm133 wild-type and B. melitensis Rev1 vaccine strains, in assessing its susceptibility to polymyxin B, sodium deoxycholate, and nonimmune serum. The mutant strain was assessed in vitro with survival assays in murine macrophages J774.A1 and HeLa cells. Our results demonstrate that LVM31 mutant is more susceptible to polymyxin B, sodium deoxycholate, and nonimmune serum than control strains; moreover, Omp31 mutation caused a decrease in the internalization and a significant decrease in the intracellular survival compared with the reference strains in both cell lines. These results allow us to conclude that Omp31 is important for maintaining OM integrity, but also it is necessary for bacterial internalization, establishment and development of an optimal replication niche, and essential for survival and intracellular multiplication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microorganisms belonging to the genus Brucella are Gram-negative, facultative intracellular bacteria causing infections in many animal species and humans (Boschiroli et al. 2001). Ten species, classified on the basis of differences in pathogenicity and host preference, are recognized within the genus Brucella: B. melitensis, B. abortus, B. suis, B. ovis, B. canis and B. neotomae, B. pinnipedialis, B. ceti, B. microti, and B. inopinata (Moreno et al. 2002; Scholz et al. 2010). Brucella melitensis, besides its important zoonotic aspect, is the most relevant etiologic agent of ovine and caprine brucellosis, a disease that causes abortion in ewes and goats resulting in huge economic losses, particularly in Mediterranean countries (Blasco 1997). Vaccination is the most suitable way to control both infections in sheep in endemic situations. The live attenuated B. melitensis Rev.1 strain is considered the best vaccine available for the prophylaxis of brucellosis in sheep and goats (Garin-Bastuji et al. 1997). However, this vaccine may cause abortion if used in animals in late pregnancy and its use is known to induce antibody responses indistinguishable by the current conventional serological tests from those observed in B. melitensis infected animals, this fact limits the extended use of Rev.1 in countries applying eradication programs based on serological testing and slaughtering of seropositive animals (de Bagüés et al. 1992; Schurig et al. 2002). Finally, this vaccine strain is fully virulent for humans and many accidental injection infections have been documented. To solve these problems, several strategies have been used to improve current vaccines. For safety improvement, the deletion of virulence-related genes, reduced-dose vaccination, and vaccination via the oral and conjunctival routes have widely been used (Barrio et al. 2009; Wang and Wu 2013; Yang et al. 2013). Outer membrane proteins (OMPs) are exposed on the bacterial surface and are in direct contact with cells effectors of the host immune response, whereby they could be important virulence factors of Brucella species (Martín-Martín et al. 2011). The Brucella spp. Omp25/Omp31 family is formed by seven homologous OMPs (Salhi et al. 2003). Regarding virulence, mutant strains of B. melitensis, B. abortus, and B. ovis by omp25 inactivation have been found to be attenuated in mice, goats (B. melitensis) (Edmonds et al. 2002a, b), and cattle (B. abortus) (Edmonds et al. 2001, 2002). In addition, Omp25 has been shown to inhibit the production of tumor necrosis factor alpha (TNF-α) by human macrophages (Jubier-Maurin et al. 2001) and to be involved in the permeability of Brucella membrane, allowing for secretion of periplasmic proteins, in acidic medium (Boigegrain et al. 2004). Several reports showed that the inactivation of the genes coding for the five OMPs of this family in virulent B. ovis PA, and demonstrated that the absence of Omp25d or Omp22 proteins leads to a striking decrease on virulence of B. ovis PA in mice (Caro-Hernández et al. 2007; Vizcaíno et al. 2004). Furthermore, it was demonstrated that Omp25d and Omp22 are essential for invasion and survival of B. ovis inside host cells, justifying the strong attenuation of the Δomp25d and Δomp22 mutants. In contrast, little is known about the role of the Omp31 on virulence in smooth strains (Martín-Martín et al. 2008). The aim of this work was to generate an omp31 mutant of B. melitensis Bm 133 strain and evaluate its effect on OM properties and intracellular survival of bacteria in murine macrophages J774.A1 and HeLa cells.
Materials and methods
Bacterial strains, growth conditions, and cloning vectors
The strains used in this work are listed in Table 1. Brucella strains were cultured at 37 °C in a 5% CO2 atmosphere for 72 h. They were typically propagated in Brucella broth (BB; Difco Laboratories, Detroit, MI) or Brucella agar (BA; Difco Laboratories), both supplemented with 0.3% yeast extract (YE; Difco Laboratories) and 5% fetal bovine serum (FBS; GIBCO-BRL Life Technologies, Germany) (BB-YE-FBS and BA-YE-BFS).
Plasmids pCR2.1 TOPO (Invitrogen, USA), pUC4K, and pUC18 were used as cloning vectors. pUC18 does not replicate in Brucella spp., so it works as a suicide plasmid required for homologous recombination. Plasmids were propagated in Escherichia coli DH5α. Recombinant E. coli cells were grown in Luria–Bertani (LB; Difco Laboratories) medium supplemented with 50 µg/ml of the required antibiotic(s) depending on plasmid resistance. Brucella and E. coli strains were provided by LMM (Molecular Microbiology Laboratory, Immunology and Microbiology Department, FMVZ-UNAM, Mexico).
Primers and DNA techniques
Chromosomal DNA of Brucella melitensis Bm133 was obtained by the guanidine thiocyanate method, as directed by the protocol described by Sambrook and Russell 2001. Prior to DNA extraction, biomass of bacteria was suspended in 5 ml of sterile distilled water and incubated in a water bath at 80 °C for 45 min for inactivation.
The omp31 nucleotide sequence was retrieved from the genome sequence of B. melitensis reference strain 16 M (GenBank accession no. JF918757.1). Primers were designed to amplify the entire omp31 gene (723 bp). The primers were omp31Fw (forward primer 5′ATGAAATCCGTAATTTTGGCG 3′) and omp31Rv (reverse primer 5′ TTAGAACTTGTAGTTCAGACC 3′). Primers were purchased from Sigma Genosys (United States). PCR was performed on extracted DNAs as follows: 35 cycles of PCR, with 1 cycle consisting of 1 min at 95 °C for DNA denaturation, 1 min at 50 °C for DNA annealing, and 1 min at 72 °C for polymerase-mediated primer extension. The last cycle included incubation of the sample at 72 °C for 5 min. Five microliters of the amplified product were analyzed by electrophoresis in 1.5% agarose gels in TAE buffer (20-mM Tris base, acetate acid, 2-mM EDTA [pH 8.0]) (Sigma–Aldrich).
Inactivation of omp31 gene in B. melitensis Bm 133 by homologous recombination
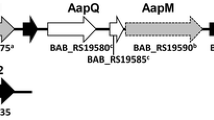
Construction of recombinant pLV plasmid was carried out using the amplification product of omp31 and cloned into plasmid pCR2.1-TOPO (Invitrogen, USA). The ligation mixture was transformed into electrocompetent E. coli DH5 α cells, plated on LB agar with kanamycin (100 µg/ml), and incubated at 37 °C overnight. Subsequently, plasmid extraction was performed. pLV plasmid was digested with Hind III (Thermo-SCIENTIFIC) and Xba I (Thermo-SCIENTIFIC) enzymes and omp31 was subcloned into pUC18 plasmid previously digested with both enzymes, rendering pLVM. The pLVM plasmid was digested with SalI (Thermo-SCIENTIFIC) and omp31 inactivation was performed by inserting a kanamycin resistance cassette obtained from pUC4K to render pLVM31. This plasmid was transformed by electroporation into the B. melitensis strain, obtaining the mutant strain B. melitensis LVM31 (Fig. 1).
Growth kinetics of bacterial strains
To determine B. melitensis 133 biovar 1, Brucella melitensis Rev1, and Brucella melitensis LVM31 growth rates, five colonies of fresh cultures were taken and inoculated into a tube with 5 ml of Brucella broth, which were incubated at 37 °C to 150 rpm for 22 h. Thus, a 1/50 dilution of each culture in 200 ml of Brucella broth was made and cultures were incubated at 37 °C at 150 rpm for 120 h. To determine the number of CFU, absorbance was measured at 4, 6, 8, 12, 16, 24, 48, 72, 96, and 120 h of culture and 20 ml of a 10−6 dilution were platted in triplicate on Brucella agar with or without antibiotic to count colony-forming units (CFUs).
Susceptibility assays
To evaluate the susceptibility of Brucella strains to polymyxin B (Sigma–Aldrich) and sodium deoxycholate (Sigma–Aldrich), bacterial suspensions containing 1 × 105 CFU/ml were prepared, and 1 ml of them was mixed in wells of a 24-well sterile plate with 1 ml of 2-mg/ml polymyxin B or 0.2-mg/ml sodium deoxycholate (final concentrations in the wells, 1 and 0.1 mg/ml, respectively). After a 2-h incubation at 37 °C in a 5% CO2 atmosphere, the content of each well was mixed, and 50 µl were spread by triplicate on BA-YE-FBS plates supplemented with antibiotic(s) when required. The CFU obtained after each treatment were counted, and the percentages of survival were established with respect to a control culture of bacteria incubated in PBS (100% survival) (De Tejada et al. 1995). To determinate the susceptibility to nonimmune serum, 5 ml of serum was obtained from a specific free pathogens (SPF) goat. Half of the serum was heated at 56 °C for 30 min to remove complement (control serum) and the other half was used fresh. Briefly, 1 ml of bacterial suspensions with approximately 1 × 105 CFU/ml in PBS were mixed in wells of a 24-well sterile plate with 200 µl of either fresh serum or heated serum. After a 4-h incubation at 37 °C in a 5% CO2 atmosphere, the content of each well was gently mixed by pipetting and 50 µl of each bacterial suspension were spread in triplicate on BA-YE-SFB plates supplemented with antibiotic(s) when required. The CFU obtained after exposure to fresh serum were counted, and the percentages of survival were established with respect to the CFU obtained with the heated serum (100% survival) (Corbeil et al. 1988).
Cell culture and infection of HeLa and J774.A1 cells
Prior to infection, cell suspensions were prepared in the basal medium Dulbecco’s Modified Eagle [Dulbecco’s Modified Eagle Medium (DMEM)] (Gibco-BRL), supplemented with fetal bovine serum (FBS); 5% (v/v) for HeLa cells and 10% (v/v) for murine macrophages, and with 4-mM l-glutamine (complete DMEM medium) at a concentration of 1 × 105 cells/ml. Subsequently, cells were distributed in 24-well culture plates (1 ml/well) and incubated for 18 h in the case of HeLa cells, and 24 h for macrophages J774.A1. To perform infection assays, Brucella melitensis Bm133 and Brucella melitensis LVM31 were grown on Brucella agar plates (supplemented or not with antibiotic as required) for 48 h, and thus, five colonies were grown in 5 ml of Brucella broth, at 37 °C, 150 rpm for 22 h. A 1/50 dilution of each culture in 200 ml of Brucella broth was performed, with incubation at 37 °C, 150 rpm for 26 h. From this culture, serial dilutions 1/2 to 1/10 of the bacteria in Brucella broth were made for a multiplicity of infection (MOI) of 100:1 for murine macrophages and 300: 1 for HeLa cells.
Statistical analysis
Analyses were performed using the commercial package for statistical analysis R®, using the Chi-square method with a normal distribution of data by time, achieving greater significance of 99% (P < 0.01). Statistical analysis took into account the absolute UFC values obtained in survival tests to determine whether the observed variation in the number of CFU is attributed to the dependent variable; for purposes of our studies, it was the intracellular survival of B. melitensis LVM31 mutant strain in HeLa cells and murine macrophages.
Results
Amplification and inactivation of the gene encoding Omp31 in B. melitensis Bm 133 by homologous recombination
The omp31 gene was amplified and interrupted as described in methodology. Thus, to obtain the mutant strain, the pLVM31 plasmid was transformed in B. melitensis. Bacteria were spread on Brucella agar plates supplemented with 5% FBS, 3% YE, and 50 µg of kanamycin, which were incubated at 37 °C for 48 h. Kanamycin-resistant and ampicillin sensitive transformants were selected. DNA extraction was performed to verify, by PCR, the integration of the inactivated omp31 gene by homologous recombination into the genome of the wild strain (Fig. 2).
Agarose gel electrophoresis of PCR-amplified omp31 gene fragments from Brucella prototype strains. Lane M 1 kb “ladder” plus. Lane 1 amplified omp31 fragment (723 bp) from B. melitensis Bm133 strain (Wild-Type). Lane 2 amplified omp31 fragment (2000 bp) from B. melitensis LVM31 (mutant strain). Lane 3 amplified omp31 fragment (2000 bp) from pLVM31 plasmid
Growth rate of Brucella strains
To determine the effect of interrupt omp31 on the growth rate, growth kinetics using control and mutant strains were performed and CFU/ml were determined by the method of Miles and Misra at different times during 120 h (Slack and Wheldon 1978). A significant decrease (P < 0.01) in the growth rate of the mutant strain B. melitensis LVM31 was observed at 4, 12, 16, 24, 48, 72, 96, and 120 h as compared to the field B. melitensis 133 and B. melitensis Rev1 vaccine strains (Fig. 3).
Role of the Omp31 on the OM properties of Brucella melitensis
To indirectly evaluate the OM integrity of the B. melitensis strains under study, the susceptibility of them to polymyxin B (1 mg/ml), sodium deoxycholate (0.1 mg/ml), and serum was determined. A 100% survival for each strain was assessed, as described in “Materials and methods” section. A statistically significant decrease (P < 0.001) in mutant survival exposed to polymyxin B and sodium deoxycholate (42.32 and 50.71% respectively) compared with both B. melitensis Bm133 (77.15 and 86.52 respectively) and B. melitensis Rev1 (68.57 and 74.28% respectively) strains was observed. In contrast, LVM31 mutant strain was only more susceptible (P < 0.01) (59.53%) to serum than B. melitensis Bm133 strain (70.59%) (Fig. 4). Therefore, Omp31 could be involved in maintaining outer membrane integrity and bacterial virulence.
Role of the Omp31 protein in intracellular survival of Brucella melitensis
To determine the effect of omp31 mutation, the intracellular survival of B. melitensis 133 and B. melitensis LVM31 strains in HeLa cells and murine macrophages was evaluated. The number of viable bacteria in the assay was determined at 0-, 4-, 8-, 12-, 24-, 48-, and 72-h postinfection. The number of CFU for B. melitensis LVM31 mutant strain invading the macrophage and HeLa cells (time zero) was lower statistically significant (P < 0.001) (1.5 × 103 and 4.1 × 103 CFU/ml respectively) as compared with B. melitensis 133 strain (3.8 × 104 and 5.4 × 104 CFU/ml respectively). Intracellular survival of B. melitensis LVM31 was lower statistically significant (P < 0.001) in both HeLa cells and murine macrophages at any sampling time as compared with B. melitensis Bm133 wild-type strain (Fig. 5).
Discussion
The resistance of Brucella spp. to oxygen-independent mechanisms has not been explained on a structural basis. Oxygen-independent mechanisms include the synergistic actions of several cationic proteins and peptides which, in a first step, bind to OM anionic targets and render the cell envelope permeable and susceptible to lytic enzymes, thereby blocking cell functions that depend on membrane integrity (Groisman 1994; Lehrer et al. 1993). The previous studies have shown that Brucella envelope has permeability properties and sensitivities to anionic detergents (de Tejada and Moriyon 1993) that are different from those common to Gram-negative bacteria, and on this basis, it has been suggested a relationship between Brucella OM properties and its pathogenicity. In this work, B. melitensis LVM31 mutant strain was studied for its resistance to polymyxin B, sodium deoxycholate, and nonimmune serum compared to control strains. Polymyxin B and sodium deoxycholate were used to determine OM stability and also as an indicator of B. melitensis LVM31 mutant susceptibility to the bactericidal effect mediated by cationic peptides in the host. In this case, B. melitensis LVM31 mutant was more susceptible to polymyxin B and sodium deoxycholate (P < 0.001) as compared with wild-type and vaccine strains. Brucella spp. are also at least partially resistant to killing mediated by the action of host nonimmune serum (Corbeil et al. 1988; Eisenschenk et al. 1999; Estein et al. 2004), which may contribute to virulence. Thus, B. melitensis LVM31 mutant survival was evaluated in the presence of nonimmune goat serum. Our results showed that mutant strain is more susceptible to serum action as compared with the wild-type strain (P < 0.01). These results suggest that Omp31 might be involved in maintaining the integrity of B. melitensis OM. As mentioned, Brucella is a facultative intracellular bacterium. Importantly, smooth Brucella species are able to enter, survive, and multiply in professional phagocytic cells as macrophages and dendritic cells as well as in nonphagocytic cells such as trophoblastic cells and epithelial cells (HeLa cells) (Billard et al. 2007; Pizarro-Cerdá et al. 2000). Accordingly, we set out to determine the effect of mutate omp31 in B. melitensis by evaluating internalization and intracellular survival of the mutant strain in HeLa cells and murine macrophages. Our results indicated that omp31 mutation caused a significant decrease in Brucella intracellular survival, both in murine macrophages and HeLa cells. These results differ from those obtained in other studies (Martín-Martín et al. 2008), where different mutant strains of B. ovis PA on genes belonging to the omp25/omp31 family were evaluated. On that instance, only the absence of Omp25d or Omp22 severely affected bacterial intracellular replication. Thus, while Δomp25d mutant strain was able to survive in macrophages, Δomp22 mutant strain was completely eliminated at 24-h postinfection. Therefore, these contradictory results could be explained considering that the O chains in S-LPS mask other surface antigens such as outer membrane proteins (OMPs), preventing both a specific immune response against them and antibodies accessibility (Bowden et al. 1995; Cloeckaert et al. 1991). Conversely, rough strains of Brucella, such as B. ovis and B. canis, do not have this problem, since they lack of O-polysaccharide, and thus, OMPs are exposed on the bacterial surface (Bowden et al. 2000; Vizcaíno et al. 2004; Vizcaı́no et al. 2001). Based on these results it is necessary to evaluate the role of the OMP25/31 family in B. melitensis to clarify differences between smooth and rough phase species of Brucella.
Achieving a replication niche in macrophages, the main host cells for this pathogen, provides protection to complement and antibodies action, allowing for dissemination into the host, and to remain for longer periods of time in the organism, resulting in subsequent chronic infection. This ability of Brucella smooth phase strains involves a complex process in which this pathogen interferes with host cell functions even to control their own intracellular trafficking. Thus, when a smooth Brucella strain is phagocytized by the macrophage, it starts an endocytic pathway in which prevents hydrolytic degradation by fusion with lysosomes, favoring in early stages of infection and intracellular survival (Celli 2006). Brucella virulence is associated with survival in phagocytic cells. The results obtained in this study highlight a relationship between a decrease in intracellular survival and replication of B. melitensis LVM31 mutant strain in both murine macrophages in HeLa cells and the absence of Omp31. Therefore, Omp31 is involved on maintaining outer membrane integrity, but also could be relevant to virulence of B. melitensis 133 by exerting important roles in intracellular survival and multiplication, although studies must be done in mice to test this hypothesis.
References
Barrio MB, Grilló MJ, Muñoz PM, Jacques I, González D, de Miguel, MJ, Gorvel J-P (2009) Rough mutants defective in core and O-polysaccharide synthesis and export induce antibodies reacting in an indirect ELISA with smooth lipopolysaccharide and are less effective than Rev 1 vaccine against Brucella melitensis infection of sheep. Vaccine 27(11):1741–1749
Billard E, Dornand J, Gross A (2007) Brucella suis prevents human dendritic cell maturation and antigen presentation through regulation of tumor necrosis factor alpha secretion. Infect Immun 75(10):4980–4989
Blasco JM (1997) A review of the use of B. melitensis Rev 1 vaccine in adult sheep and goats. Prev Vet Med 31(3):275–283
Boigegrain R-A, Salhi I, Alvarez-Martinez, M-T, Machold J, Fedon Y, Arpagaus M, Rouot B (2004) Release of periplasmic proteins of Brucella suis upon acidic shock involves the outer membrane protein Omp25. Infect Immun 72(10):5693–5703
Boschiroli ML, Foulongne V, O’Callaghan D (2001) Brucellosis: a worldwide zoonosis. Curr Opin Microbiol 4(1):58–64
Bowden RA, Cloeckaert A, Zygmunt MS, Bernard S, Dubray G (1995) Surface exposure of outer membrane protein and lipopolysaccharide epitopes in Brucella species studied by enzyme-linked immunosorbent assay and flow cytometry. Infect Immun 63(10):3945–3952
Bowden RA, Estein SM, Zygmunt MS, Dubray G, Cloeckaert A (2000) Identification of protective outer membrane antigens of Brucella ovis by passive immunization of mice with monoclonal antibodies. Microbes Infect 2(5):481–488
Caro-Hernández P, Fernández-Lago L, de Miguel M-J, Martín-Martín AI, Cloeckaert A, Grilló M-J, Vizcaíno N (2007) Role of the Omp25/Omp31 family in outer membrane properties and virulence of Brucella ovis. Infect Immun 75(8):4050–4061
Celli J (2006) Surviving inside a macrophage: the many ways of Brucella. Res Microbiol 157(2):93–98
Cloeckaert A, Jacques I, Bosseray N, Limet JN, Bowden R, Dubray G, Plommet M (1991) Protection conferred on mice by monoclonal antibodies directed against outer-membrane-protein antigens of Brucella. J Med Microbiol 34(3):175–180
Corbeil LB, Blau K, Inzana TJ, Nielsen KH, Jacobson RH, Corbeil RR, Winter AJ (1988) Killing of Brucella abortus by bovine serum. Infect Immun 56(12):3251–3261
de Tejada MG, Moriyon I (1993) The outer membranes of Brucella spp. are not barriers to hydrophobic permeants. J Bacteriol 175(16):5273–5275
de Bagüés MP, Marin CM, Blasco JM, Moriyon I, Gamazo C (1992) An ELISA with Brucella lipopolysaccharide antigen for the diagnosis of B. melitensis infection in sheep and for the evaluation of serological responses following subcutaneous or conjunctival B. melitensis strain Rev 1 vaccination. Vet Microbiol 30(2):233–241
De Tejada MG, Pizarro-Cerda J, Moreno E, Moriyon I (1995) The outer membranes of Brucella spp. are resistant to bactericidal cationic peptides. Infect Immun 63(8):3054–3061
Edmonds MD, Cloeckaert A, Booth NJ, Fulton WT, Hagius SD, Walker JV, Elzer PH (2001) Attenuation of a Brucella abortus mutant lacking a major 25 kDa outer membrane protein in cattle. Am J Vet Res 62(9):1461–1466
Edmonds MD, Cloeckaert A, Elzer PH (2002a) Brucella species lacking the major outer membrane protein Omp25 are attenuated in mice and protect against Brucella melitensis and Brucella ovis. Vet Microbiol 88(3):205–221
Edmonds MD, Cloeckaert A, Hagius SD, Samartino LE, Fulton WT (2002b) Pathogenicity and 21 protective activity in pregnant goats of a Brucella melitensis Deltaomp25 deletion 22 mutant. Res Vet Sci 72:235–239
Eisenschenk FC, Houle JJ, Hoffmann EM (1999) Mechanism of serum resistance among Brucella abortus isolates. Vet Microbiol 68(3):235–244
Estein SM, Cheves PC, Fiorentino MA, Cassataro J, Paolicchi FA, Bowden RA (2004) Immunogenicity of recombinant Omp31 from Brucella melitensis in rams and serum bactericidal activity against B. ovis. Vet Microbiol 102(3):203–213
Garin-Bastuji B, Blasco JM, Grayon M, Verger JM (1997) Brucella melitensis infection in sheep: present and future. Vet Res 29(3–4):255–274
Groisman EA (1994) How bacteria resist killing by host-defense peptides. Trends Microbiol 2(11):444–449
Jubier-Maurin V, Boigegrain R-A, Cloeckaert A, Gross A, Alvarez-Martinez M-T, Terraza A, Dornand J (2001) Major outer membrane protein Omp25 of Brucella suis is involved in inhibition of tumor necrosis factor alpha production during infection of human macrophages. Infect Immun 69(8):4823–4830
Lehrer RI, Lichtenstein AK, Ganz T (1993) Defensins: antimicrobial and cytotoxic peptides of mammalian cells. Annu Rev Immunol 11(1):105–128
Martín-Martín AI, Caro-Hernández P, Orduña A, Vizcaíno N, Fernández-Lago L (2008) Importance of the Omp25/Omp31 family in the internalization and intracellular replication of virulent B. ovis in murine macrophages and HeLa cells. Microbes Infect 10(6):706–710
Martín-Martín AI, Sancho P, Tejedor, C, Fernández-Lago L, Vizcaíno N (2011) Differences in the outer membrane-related properties of the six classical Brucella species. Vet J 189(1):103–105
Moreno E, Cloeckaert A, Moriyón I (2002) Brucella evolution and taxonomy. Vet Microbiol 90(1):209–227
Pizarro-Cerdá J, Moreno E, Gorvel J-P (2000) Invasion and intracellular trafficking of Brucella abortus in nonphagocytic cells. Microbes Infect 2(7):829–835
Salhi I, Boigegrain R-A, Machold J, Weise C, Cloeckaert A, Rouot B (2003) Characterization of new members of the group 3 outer membrane protein family of Brucella spp. Infect Immun 71(8):4326–4332
Scholz HC, Nöckler K, Göllner C, Bahn P, Vergnaud G, Tomaso H, Maquart M (2010) Brucella inopinata sp. nov., isolated from a breast implant infection. Int J Syst Evol Microbiol 60(4):801–808
Schurig GG, Sriranganathan N, Corbel MJ (2002) Brucellosis vaccines: past, present and future. Vet Microbiol 90(1):479–496
Slack MP, Wheldon DB (1978) A simple and safe volumetric alternative to the method of Miles, Misra and Irwin for counting viable bacteria. J Med Microbiol 11(4):541–545
Vizcaíno N, Kittelberger R, Cloeckaert A, Marín CM, Fernández-Lago L (2001) Minor nucleotide substitutions in the omp31 gene of Brucella ovis result in antigenic differences in the major outer membrane protein that it encodes compared to those of the other Brucella Species. Infect Immun 69(11):7020–7028
Vizcaíno N, Caro-Hernández P, Cloeckaert A, Fernández-Lago L (2004) DNA polymorphism in the omp25/omp31 family of Brucella spp.: identification of a 1.7-kb inversion in Brucella cetaceae and of a 15.1-kb genomic island, absent from Brucella ovis, related to the synthesis of smooth lipopolysaccharide. Microbes Infect 6(9):821–834
Wang Z, Wu Q (2013) Research progress in live attenuated Brucella vaccine development. Curr Pharm Biotechnol 14(10):887–896
Yang X, Skyberg JA, Cao L, Clapp B, Thornburg T, Pascual DW (2013) Progress in Brucella vaccine development. Front Biol 8(1):60–77
Acknowledgements
This work was supported by PAPIIT IN212610, PAPIIT IN-221513, and PAPIIT IN-222516, UNAM. The authors acknowledge Beatriz Arellano for her technical support and Mrs. Francisca Muñoz for her administrative support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Erko Stackebrandt.
Rights and permissions
About this article
Cite this article
Verdiguel-Fernández, L., Oropeza-Navarro, R., Basurto-Alcántara, F.J. et al. Omp31 plays an important role on outer membrane properties and intracellular survival of Brucella melitensis in murine macrophages and HeLa cells. Arch Microbiol 199, 971–978 (2017). https://doi.org/10.1007/s00203-017-1360-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00203-017-1360-7