Abstract
Summary
Is osteoporosis related to worst outcomes after fall accidents? After a fall accident, there were no differences in walking and balance between individuals with/without osteoporosis. Gains in fat tissue, higher pain, and difficulty to walk were related to previous falls, regardless of osteoporosis.
Purpose
Impairments are expected after an accidental fall in the older age; whoever, it is still unclear if patients suffering from osteoporosis are in higher risks of fall accidents and if such accidents would cause worst outcomes compared with older adults without osteoporosis. The objective of this study was to discriminate fallers and non-fallers via a combination of physical performance measurements of older adults (65 + years) with and without osteoporosis.
Methods
Older adults (n = 116) were screened for a previous fall accident and tested during (i) quiet stance; (ii) single- and dual-task walking; (iii) 8-Foot Up-and-Go; (iv) Mini BESTest; (v) 2-min step-in-place and (vi) 30-s chair stand. Evaluation of average daily pain intensity and total body fat% were obtained.
Results
Forty-four subjects (38%) reported a previous fall accident. There was, however, no association between osteoporosis and previous fall. Fallers had a higher daily pain intensity, higher body fat%, slower walking speed during a cognitive dual-task test and worse performance at the 8-Foot Up-and-Go test and the Mini BESTest compared to non-fallers.
Conclusions
Although the presence of osteoporosis might not increase the risk of fall accidents, healthcare professionals should expect that accidental falls in older adults are associated with higher body fat%, higher daily pain intensity and problems performing daily activities such as walking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 30% of older adults (65 + years) experience an accidental fall per year [1] where falls are defined as “inadvertently coming to rest on the ground, floor or other lower level, excluding intentional change in position to rest in furniture, wall or other objects” [2]. The consequences of fall accidents in older adults are concerning, considering that it affects the execution of daily activities [3] and occasionally death [3].
Aging affects the static balance, by increasing postural sway [4]. Similarly, a worsened postural control has both been found among fallers, compared to non-fallers, derived through findings of larger sway distance [4]. Some of the mechanisms responsible for the worsened balance are diminishing stretch reflexes [5] and reduced mobility [6]. Among fallers, slower gait speed [7] and larger gait variability [8] were reported when compared with non-fallers, which may be caused by decline in muscle strength, muscle mass, and balance [9]. Pain is common among older adults, as approximately 60% of community-dwelling older adults experiences substantial pain [10]. In accordance with this, pain is being related to increased risk of falling [11], where fallers scores higher pain rating than non-fallers. Muscle strength decreases with age [12] and with a OR of 1.76 between fallers and lower extremity weakness [13].
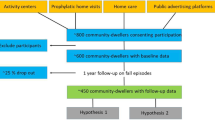
Osteoporosis is characterized by low bone mass, deterioration of bone tissue and disruption of bone architecture [14]. However, it is not clear if older adults with osteoporosis have an increased risk of falling compared with healthy controls [15], even though the increased risk of fractures after accidental falls is increased in individuals with osteoporosis when compared with healthy controls [16]. Individuals with osteoporosis are expected to have less muscle mass [17], increased fear of falling (OR: 2.4) [18], changes in gait characteristics [19], and larger risk of cognitive deterioration [20] compared with healthy controls, which are known factors for increased fall risk in older adults [21]. A direct link between osteoporosis and walking speed is not well tested, but a recent study has found an association between bone turnover markers and walking speed, stating that adults with a slower walking speed had increased bone resorption [22] compared with older adults with a faster 20-feet walking speed. Furthermore, obesity is being found to increase the risk of falling [23]. It is well documented that physical activity can prevent osteoporosis [24] and prevent obesity [25]. Although studies show associations between different factors and fall accidents in healthy older adults and in individuals with osteoporosis, the protocols are usually limited to a few numbers of tests. Therefore, there is a need of studies applying both types of tests (laboratory and clinical), in the same protocol to examine to which extend these tests are sensitive to quantify impairments after an accidental fall. The first aim of this study is to investigate if there is a relationship between patients with osteoporosis and fall accidents. The second aim of this study is to identify among 14 fall-related variables, which tests are the most sensitive to discriminate fallers and non-fallers among older adults with and without osteoporosis. The third aim is to provide new insights into the focus in future preventive intervention/rehabilitation programs concerning long-term consequences within fall accidents. Altogether, the expected results from this study might contribute to the knowledge for preventing recurrent falls, and improving post-fall accident rehabilitation, by enabling new possibility for healthcare workers to better adjust their facilities, training approaches, and evaluation protocols to the needs of older adults that experienced a fall accident. To achieve these aims, the following hypothesis will be tested: (i) older adults with osteoporosis are more likely to experience fall accidents compared to those without osteoporosis; (ii) certain fall-related tests are more sensitive in discriminating fallers from non-fallers among older adults with osteoporosis compared to those without osteoporosis.
Methods
Participants
One hundred sixteen older adults (13/103 M/F, 70.5 ± 4.6 years, 165.3 ± 6.2 cm, and 66.6 ± 12.6 kg) volunteered for this study. Sixty-five of the participants were healthy older adults, whereas fifty-one of the participants were osteoporosis patients. Osteoporosis patients were included if they had verified osteoporosis (− 2.5 ≥ T-score ≥ − 3.5) and were in medical treatment for osteoporosis, whereas healthy participants were included if they had a T-score > − 2.5 and did not receive medical treatment for osteoporosis. All participants were excluded if they were younger than 65 years old, had previous neurological, musculoskeletal (besides osteoporosis) or mental illnesses, or participated in medical trials.
All participants were given a detailed verbal explanation of the experiment and provided written informed consent. The study was conducted in accordance with the Helsinki Declaration, approved by the local ethics committee (N-20180065). This study is a part of a clinical trial [26], investigating the effect of dance as a fall-preventing exercise program. The clinical trial was designed to have 80% power to detect at least a 10% reduction in falls per person-years.
Experimental protocol
All participants had a single test session, lasting approximately three hours. Upon arrival, anthropometric data and history of falls and fall-related fractures (“no fall,” “fall – no fracture,” and “fall – fracture”) were acquired. Bone mineral density (BMD) for lumbar spine (L1-L4), femoral neck, and total hip, as well as body composition, were then examined using a dual-energy X-ray absorptiometry (DXA) scanner. Pain was assessed using a 10-cm visual analogue scale (VAS). Hereafter, postural sway was quantified on a force plate, during quiet stance in four conditions, eyes open and eyes closed on firm surface, eyes open, and eyes closed on a foam surface. Participants had their gait tested during a 25-m walking test, with and without a cognitive challenging dual task. Lastly, the participants functional fitness and postural stability were quantified using the 30-s chair stand test, 2-min step test, 8-Foot Up-and-Go test, and the Mini-BESTest.
Bone mineral density and body composition
Bone mineral density was measured to secure that all participants followed the inclusion and exclusion criteria. The participants were scanned using a Horizon A (Horizon A, Hologic, Marlborough, MA, USA) DXA scanner. The BMD was measured in g/cm2 and computed in a T-score. The radiation from the scanner was less than 100 microSv. Body composition was measured in grams and converted to a bodyfat percentage.
Pain assessment
Pain intensity was assessed using a 10-cm visual analogue scale (VAS), graded for every cm, with the description “no pain,” “moderate pain,” and “worst imaginable pain” at 0, 5, and 10 cm, respectively. The pain intensity was measured with one decimal precision. When assessing pain, participants were asked to rate the average rating of pain they felt in their everyday life. If participants had a VAS score higher than 0, they were asked to draw the painful sites on a body chart. The drawings on the body chart were converted into a percentage measure, describing how large the painful area was, compared to the whole body (pain area%).
Postural control
To quantify the static balance, participant stood on a force plate (Plux Biosignals S.A., Arruda don Vinhos, Portugal) during four conditions: (i) eyes open on a firm surface, (ii) eyes closed on a firm surface, (iii) eyes open on a soft foam surface, and (iv) eyes close on a soft foam surface. Participants were asked to stand in a normal stance, feet with a shoulder width apart and arms resting at their side. In the soft surface condition, a 48 × 40 × 6 cm Airex® Balance-pad (Airex, Sins, Switzerland) were placed on the force plate. All conditions were applied three times in a randomized order, each with a 30-s duration. Ground reaction forces were recorded at 1 kHZ (Opensignals, Plux Biosignals S.A, Arruda dos Vinhos, Portugal) and filtered using a second order Butterworth filter (15 Hz low pass frequency). Center of pressure (CoP) sway velocity and sway area was calculated, with area extracted via principal component analysis and 95% confidence interval for ellipse calculation [27]. A mean of all 12 tests (four conditions with three trials of each) was calculated for velocity and area of the sway, returning a single measure for sway velocity and for sway area. Dynamic balance was assessed using the Mini BESTest [28], which is a test-battery consisting of 14 tests, each rated from 0 to 2, with a total test score ranging from 0 to 28.
Gait stability and dual task
To quantify step length, step time, and gait velocity, participants walked at a self-selected pace in a 25-m path, wearing 17 wireless inertial sensors (Awinda, Xsens Technologies B.V., Enschede, The Netherlands), sampling at 1000 Hz. Through the recordings from the sensors, length of gait cycle (meter), time (milliseconds), and velocity (meter/second) were quantified, by extracting knee joint movement.
To quantify cognitive function, a mathematical dual-task task was administered [29]. Participants had to walk on the same 25-m path as in the single-task gait test, while performing continuously subtractions of seven from a number between 200 and 500. The subtractions should be recited aloud and was then noted.
Both the single-task and dual-task gait test were repeated three times, in a randomized order. An average of the three tests were used for further analysis.
Fitness assessment
To assess fitness of the older adults, three physical fitness tests were used, the 30-Second Chair Stand, 2-Minute Step-in-Place, and the 8-Foot Up-and-Go test, all from Rikli and Jones Fullerton Battery test for older adults [30]. The 30-Second Chair stand tests the leg strength and endurance and is measured as the number of times the participant can raise from the chair, without using the arms to push off. The 2-Minute Step-in-Place test is used to test aerobic endurance among older adults and is measured by the number of knees raises with the right knee. The 8-Foot Up-and-Go test measures speed, agility, and balance while moving, and is scored by the nearest 1/10th second.
Statistics
Independent samples T-tests were performed between the three demographic set of data (age, height, and weight), regarding fall accidents, to secure that a possible difference between groups was not due to differences within demographic data. A 2 × 2 contingency table with a Pearson chi-square test was performed between the variables Osteoporosis and falls. A Pearson chi-square test was calculated for the variables Osteoporosis and fall-related fractures (“no fall,” “fall – no fracture,” and “fall – fracture”). For all of the variables, a MANOVA with a Bonferroni-corrected pairwise comparisons test used to analyze if there were differences within any of the 14 dependent variables (VAS, CoP sway area, CoP sway velocity, walking speed with and without dual-task, gait cycle length with and without dual-task, gait cycle time with and without dual-task, mini-BESTest, 30-Second Chair Stand, 2-Minute Step-in-Place, 8-Foot Up-and-Go, body fat percentage) and the fixed factors (previous falls and osteoporosis), as well as a MANOVA with a Tukey post hoc test for the 14 dependent variables and the fixed factors (fall-related fractures and osteoporosis). For each variable in the MANOVA tests, the observed power was calculated. For the Bonferroni-corrected pairwise comparisons, the partial ETA squared was calculated. A Walds forward stepwise logistic regression test was used to calculate if there were any statistical association between the groups of fallers and non-fallers, within each of the 14 parameters. If pain levels differed significantly in the MANOVA or were included in the logistic regression model, an independent T-test were calculated for the body chart drawings between fallers and non-fallers. Statistical significance is set to P < 0.05.
Results
Falling and osteoporosis
Of the 116 participants, 51 were individuals with osteoporosis. There were significant differences in T-score (L1-L4: t-test (114) = 13.599, P < 0.001; hip: t-test (113) = 14.128, P < 0.001) between osteoporosis patients (T-score L1-L4 − 2.01 ± 0.89; T-score hip − 1.64 ± 0.61) and healthy older adults (T-score L1-L4 -0.35 ± 1.55; T-score Hip − 0.65 ± 0.98). Forty-four of the 116 participants had previously had a fall accident. There were no differences between fallers and non-fallers within age, height and weight (All, P > 0.25; Table 1).
There were no statistical significant associations between falling (yes/no) and osteoporosis (yes/no), (Table 2, chi-square (1) = 3.221, P = 0.07). There were no significant association between fall-related fractures (“no fall,” “fall – no fracture,” and “fall – fracture”) and osteoporosis (yes/no) (chi-square (2) = 5.617, P = 0.06).
Fall accidents and fall-related factors
The MANOVA indicated a significant main effect of fall accidents (MANOVA (14, 90) = 2.214, P = 0.01, power = 0.95), but no differences for osteoporosis (Table 3, MANOVA (14, 90) = 0.999, P = 0.46, power = 0.58) and no interaction effect (MANOVA (14, 90) = 0.487, P = 0.94, power 0.277). The post hoc test for the effect of fall accidents showed (i) higher in pain intensity (Bonferroni, P < 0.01, partial-eta-squared = 0.076) for fallers (VAS 2.5 cm ± 2.6 cm) compared with non-fallers (VAS 1.5 cm ± 2.1 cm); (ii) longer gait cycle time during a cognitive dual-task (Bonferroni, P = 0.02, partial-eta-squared = 0.052) in fallers (1202 ms ± 252 ms) compared with non-fallers (1113 ms ± 119 ms); (iii) slower mean step velocity during a cognitive dual-task (Bonferroni, P = 0.04, partial-eta-squared = 0.04) in fallers (1.18 m/s ± 0.23 m/s) compared with non-fallers (1.26 m/s ± 0.19 m/s); (iv) slower time for the 8-Foot Up-and-Go test (Bonf., P < 0.01, partial-eta-squared = 0.094) among fallers (6.3 s ± 1.2 s) compared with non-fallers (5.7 s ± 1.2 s); (v) lower Mini-BESTest score (Bonferroni, P = 0.03, partial-eta-squared = 0.044) in the fallers (23.8 ± 3.8) compared with the non-fallers (25.2 ± 3.1) group; and (vi) higher body fat % (Bonf., P < 0.01, partial-eta-squared = 0.065) among fallers (39.0% ± 5.4%) than non-fallers (36.3% ± 5.4%).
Fall-related fractures and fall-related factors
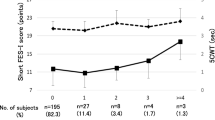
Figure 1 serves as an overview of these results indicating that fallers without fractures compared with no-fallers showed: (i) higher body fat, (ii) longer time for 8-foot Up-and-Go, (iii) worst Mini BESTest, (iv) longer gait cycle time during dual-task, and (v) lower gait velocity during dual-task. Pain intensity was also higher in the fallers with fracture compared to non-fallers. Finally, fallers with fracture showed shorter gait cycle time compared with fallers with no-fracture. The MANOVA indicated a significant main effect of fall-related fractures (MANOVA (28, 178) = 1.601, P = 0.04, power = 0.98), but no differences for osteoporosis (MANOVA (14, 88) = 1.005, P = 0.46, power = 0.56) and no interaction effect (MANOVA (28, 176) = 1.148, P = 0.29, power = 0.89). The post hoc test showed higher pain ratings (Tukey, P = 0.03) within fallers with a fracture (VAS 2.5 cm ± 2.9 cm) compared to non-fallers (VAS 1.5 cm ± 2.1 cm). There were no further differences between non-fallers and fallers with a fracture. Fallers without a fall-related fracture had a significant longer dual-task gait cycle time (1262 ms ± 323 ms) than fallers with a fall-related fracture (1133 ms ± 98 ms) (Tukey, P = 0.047) and non-fallers (1113 ms ± 119 ms) (Tukey, P < 0.01). Furthermore, there were a significant slower mean step velocity with a cognitive dual-task (Tukey, P = 0.02) within fallers without a fall-related fracture (1.13 m/s ± 0.25 m/s) and non-fallers (1.26 m/s ± 0.19 m/s). Finally, the completion time for the 8-Foot Up-and-Go test was significantly (Tukey, P < 0.01) slower among fallers without a fracture (6.3 s ± 1.1 s) than in non-fallers (5.7 s ± 1.2 s), the score in the Mini-BESTest was significantly lower (Tukey, P = 0.03) in the fallers without a fall-related fracture (23.7 ± 3.3) than the non-fallers (25.2 ± 3.1) and the body fat % was higher (Tukey, P = 0.03) among fallers without a fall-related fracture (39.5% ± 5.1%) than non-fallers (36.3% ± 5.4%).
Mean (± standard deviation) for the non-fallers, fallers with no fall-related fracture and fallers with a fall-related fracture for body fat, 8-Foot Up-and-Go, Mini BESTest, Pain rating, and dual-task gait cycle time and velocity. A Body fat % measured by a DEXA scanner. Significant larger body fat % within fallers with no fall-related fractures compared to non-fallers (*, Tukey, P = 0.03). B Completion time in seconds for the 8-Foot Up-and-Go test. Significant longer completion time within fallers with no fall-related fractures compared to non-fallers (*, Tukey, P < 0.01). C Score on the Mini BESTest. Significant lower scores within fallers with no fall-related fractures compared to non-fallers (*, Tukey, P = 0.03). D Pain ratings on the Visuel Analogue Scale (VAS). Significant higher pain ratings within fallers with a fall-related fracture compared to non-fallers (#, Tukey, P = 0.03). E Gate cycle time during a cognitive dual-task walking test. Significant longer gait cycle time within fallers with no fall-related fractures compared to non-fallers (*, Tukey, P < 0.01). Significant longer gait cycle time within fallers with no fall-related fractures compared to fallers with a fall-related fracture (¤, Tukey, P = 0.05). F Gait velocity during a cognitive dual-task walking test. Significant slower gait velocity within fallers with no fall-related fractures compared to non-fallers (*, Tukey, P = 0.02)
Fall accidents and associations with physical performance tests
When performing a Walds forward logistic regression test, the 8-Foot Up-and-Go test (P < 0.01) and the pain rating was significant (P = 0.01) between fallers and non-fallers, with a coefficient of 0.710 and 0.244, respectively. The model was statistically significant (chi-square (2) = 18.130, P < 0.001). The model explained 21.2% (Nagelkerke R-squared) of the variance and correctly classified 70.1% of the cases. The test shows that older adults who experiences a fall accident will have significantly increased pain rating and a slower completion time of the 8-Foot Up-and-Go test.
As pain levels differed between fallers and non-fallers in the MANOVA and was included in the logistic regression model, differences in pain area% from the body chart was calculated. Fifty-nine of the participants had a VAS score above 0 cm (fallers, N = 28; non-fallers, N = 31). A significant difference in pain area% (t-test (57) = 6.392, P = 0.014) were found between fallers (3.33% ± 3.94%; range 0.2–16.7%) and non-fallers (2.15% ± 1.53%; range 0.3–6.5%). As shown in Fig. 2, the most dominant areas for pain in both fallers and non-fallers were lower back, neck, and shoulder pain.
Discussion
One of the aims of this study was to investigate if there was a relationship between osteoporosis and fall accidents. No association was found between falling and osteoporosis. This is in line with the literature, stating that older adults with osteoporosis does not have an increased risk of falling, but an increased risk of getting fall-related fractures [15, 16].
This study further aimed to investigate which tests are the most sensitive to discriminate fallers and non-fallers among older adults with and without osteoporosis. Previous fall accident led to (i) higher body fat %, (ii) higher pain intensity; (iii) longer gait cycle time and slower walking speed during a cognitive task; and (iv) slower time in the 8-Foot Up-and-Go test and lower scores in the Mini BEST test in the group with fallers compared with non-fallers group. Furthermore, higher pain ratings and increased completion time for the 8-Foot Up-and-Go test was the only parameters who had a significant contribution to the difference within fallers and non-fallers, when using the Walds forward logistic regression test. This suggests that a reduced completion time for the 8-Foot Up-and-Go test and increased pain in everyday living are the leading consequences of fall accidents.
-
I.
Body fat %
Participants who had previously had a fall accident, had a significantly higher body fat % compared with those with no history of falls. As obesity has been found to increase the risk of falling [31], it is relevant to try to prevent obesity, to minimize the risk of turning the faller into a recurrent faller. Healthcare workers should pay attention to this problem, in order to potentially reduce the risk of falling, but also other overweight associated diseases, such as type 2 diabetes, cardiovascular disease, stroke, and hypertension [32].
-
II.
Pain intensity
Participants who had experienced a fall-related fracture had a higher level of pain throughout their everyday life compared with the non-fallers. Broken bones may lead to chronic pain, as shown among rib fracture patients [33], which could be the case in this study too. Surprisingly, the group of participants with a fall-related fracture did not differ from the non-fallers in any other of the parameters, though pain, in previous studies, has been associated with slower walking speed [34] and decreased amount of physical activity [35]. In this study, the difference in pain rating between fallers and non-fallers was 1.0 cm. Compared with chronic pain patients [36], this is within the range of minimal clinically important differences, though this small difference between the groups may explain the similarities between fallers with a fracture and non-fallers in every other parameter. The small difference shall not be neglected, as the fallers have a more widespread pain than the non-fallers.
Fallers experienced more pain, walked slower during a cognitive dual-task and performed worse in the 8-Foot Up-and-Go test, which combines dynamic balance and walking speed. Previously, experimental calf muscle pain has been found to decrease the postural control during perturbations [37], which is a more dynamic balance task than quite stance, making it more comparable to the dynamic balance in the 8-Foot Up-and-Go test. Experimental pain has likewise been found to affect the trunk muscles, by changing the feedforward postural responses of these [38]. As trunk control capacity has previously been found to correlate with turning difficulties [39], this may explain the pain-altering mechanisms.
-
III.
Walking speed during a cognitive task
Impaired cognition has previously been found to increase the risk of falling [40], with an odds ratio for falls ranging from 2.13 [41] to more than 3 [42]. In a 5-year follow-up study [40], executive function derived from cognitive function assessment was able to predict future fallers. As the fallers in this study had a slower walking speed in the cognitive dual-task walking test, but not in the single-task walking test, compared to the non-fallers, this may indicate a reduced executive function among the fallers. If so, this reduced executive function may increase the risk of future falls. However, these findings are in contrast to previous meta-analysis [7], indicating that both single- and dual-task walking tests were able to discriminate between fallers and non-fallers, when using gait speed as a parameter. In this study, no difference within single task walking speed was found. Participants in this study tends to be more fit than the background population, in regard to walking speed, as mean gait speed of the participants in this study (1.43–1.48 m/s) is within the 4th quartile of the gait speed found within a cross-sectional study on walking speed [43]. This may explain the discrepancy within the findings, although still clinically relevant by indicating that such test is able to discriminate potential increased fall risk in older adults with high fitness levels. The possibility of including only relative fit participants in this study is mentioned within limitations of the protocol paper [26].
-
IV.
8-Foot Up-and-Go test and the Mini BEST test
The Mini BESTest and the 8-Foot Up-and-Go test are both designed to test dynamical balance [28, 30]. In this study, the fallers and non-fallers had a mean Mini BESTest score of 23.8 and 25.2, respectively, showing a much better performance than previous studies. Gait and balance deficits have both been found to be a large contributor to fall risk, with an odds ratio of 2.9 [21]. As the combination of gait and balance deficits (i) contributes to fall risk [21], (ii) is an activity performed during most fall accidents [44], and (iii) being parameters worsened among fallers compared to non-fallers after a fall accident, physicians, and health care workers should include this as a focus in the post-fall accident rehabilitation training. This is in line with a recent update on a meta-analysis, stating that exercise as fall prevention should aim to challenge balance and may include walking training [45].
One of the novel findings in this study was that older adults who had experienced a fall accident without a fracture, performed worse in numerous tests than the non-fallers. With exception of pain, participants with a fall-related fracture did not differ in performance in any of the tests, compared to non-fallers. In the Municipality of Aalborg, where the majority of the participants of this study were recruited, citizens are offered fall-preventing training, but inclusion criteria are that the person has to (1) meet the criteria for maintenance training, which is for persons who are weakened after a long illness, or (2) have a rehabilitation plan. An older adult experiencing a fall accident that does not lead to a fracture, will in many cases not be offered fall prevention training, which may explain these findings and possibly highlighting the importance of physical training post-fall accidents. However, the present study cannot directly address this statement, which should be further investigated in future studies.
As all the negative consequences, with exception of pain, was present in the group of fallers who has not experienced a fall-related fractures, there may be a potential to decrease the number of fallers who become recurrent fallers, if fall prevention exercise programs could be offered to adults who does not necessarily belong to the group of persons who are eligible to maintenance training or a rehabilitation plan.
The 8-Foot Up-and-Go test was the most sensitive physical test for quantifying impairments after a fall accident. In the test, participants need to go from seated to standing position, walk 8 feet, turn around a cone and return to the chair in shortest possible time. This test is therefore a composite measure of four parameters: (i) lower body strength and power, (ii) speed, (iii) agility, and (iv) dynamic balance. Future studies dividing the test into measurement of each parameter individually are need, in order to incorporate this in future preventive intervention programs.
-
V.
Future preventive intervention/rehabilitation programs concerning long-term fall consequences in older adults with and without osteoporosis
This study highlights which long-term effects of a fall could increase the likelihood of future falls in older adults. To mitigate this additional risk, it is paramount to have a multi-focus preventive approach to not just increase, for example, muscle strength but also on weight control and muscle power to potentially enhance gait speed and dynamic balance. Pain management approaches are also recommended, especially if fractures were present in previous falls. Additionally, interventions that simultaneously challenge both physical and cognitive abilities (dual-task training) are potentially beneficial. One could try to combine these elements in one approach involving physical exercise. These emerges as a comprehensive approach, which currently can also be delivered online, as it not only addresses these physical and cognitive needs but also improves mental health and social wellbeing among older adults [46].
Conclusion
This study found no association between number of accidental falls and the presence of osteoporosis. The overall results suggest that individuals with a history of fall accidents may experience more pain, have impaired balance and gait, and may face challenges when performing cognitive dual tasks while walking. Early identification of these issues using simple clinical tests could potentially help in developing targeted interventions and reducing the risk of future falls. Healthcare workers may therefore use these tests when evaluating progress during rehabilitation or post-fall accident training.
Data availability
Requests for access to the data generated in this study should be directed to the corresponding author, who will evaluate the requests based on relevant criteria.
References
Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL (1990) Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing 19:136–141. https://doi.org/10.1093/ageing/19.2.136
World Health Organization (2008) WHO Global report on falls prevention in older age. https://www.who.int/publications/i/item/9789241563536. Visited: 19 Aug 2024
Tinetti ME, Williams CS (1997) Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 337:1279–1284. https://doi.org/10.1056/NEJM199710303371806
Maki BE, Holliday PJ, Topper AK (1994) A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol 49:72–84
Pyykko I, Jantti P, Aalto H (1990) Postural control in elderly subjects. Age Ageing 19:215–21. https://doi.org/10.1093/ageing/19.3.215
Freitas SMSF, Wieczorek SA, Marchetti PH, Duarte M (2005) Age-related changes in human postural control of prolonged standing. Gait Posture 22:322–330. https://doi.org/10.1016/j.gaitpost.2004.11.001
Menant JC, Schoene D, Sarofim M, Lord SR (2014) Single and dual task tests of gait speed are equivalent in the prediction of falls in older people: a systematic review and meta-analysis. Ageing Res Rev 16:83–104. https://doi.org/10.1016/j.arr.2014.06.001
Hausdorff JM, Rios DA, Edelberg HK (2001) Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil 82:1050–1056. https://doi.org/10.1053/apmr.2001.24893
Xie YJ, Liu EY, Anson ER, Agrawal Y (2017) Age-related imbalance is associated with slower walking speed: an analysis from the National Health and Nutrition Examination Survey. J Geriatr Phys Ther 40:183–189. https://doi.org/10.1519/JPT.0000000000000093
Herr KA, Garand L (2001) Assessment and measurement of pain in older adults. Clin Geriatr Med 17:457–478. https://doi.org/10.1016/S0749-0690(05)70080-X
Blyth FM, Cumming R, Mitchell P, Wang JJ (2007) Pain and falls in older people. Eur J Pain 11:564–571. https://doi.org/10.1016/j.ejpain.2006.08.001
Tieland M, Trouwborst I, Clark BC (2018) Skeletal muscle performance and ageing. J Cachexia Sarcopenia Muscle 9:3–19. https://doi.org/10.1002/jcsm.12238
Moreland JD, Richardson JA, Goldsmith CH, Clase CM (2004) Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc 52:1121–1129. https://doi.org/10.1111/j.1532-5415.2004.52310.x
Resnick B, Nahm ES, Zhu S, Brown C, An M, Park B, Brown J (2014) The impact of osteoporosis, falls, fear of falling, and efficacy expectations on exercise among community-dwelling older adults. Orthop Nurs 33:277–286. https://doi.org/10.1097/NOR.0000000000000084
Smulders E, van Lankveld W, Laan R, Duysens J, Weerdesteyn V (2011) Does osteoporosis predispose falls? A study on obstacle avoidance and balance confidence. BMC Musculoskelet Disord 12:1. https://doi.org/10.1186/1471-2474-12-1
Aitken JM (1984) Relevance of osteoporosis in women with fracture of the femoral neck. Br Med J (Clin Res Ed) 288:597–601. https://doi.org/10.2307/29514179
Gentil P, Lima RM, Jacó de Oliveira R, Pereira RW, Reis VM (2007) Association between femoral neck bone mineral density and lower limb fat-free mass in postmenopausal women. J Clin Densitom 10:174–178. https://doi.org/10.1016/j.jocd.2007.01.004
Meyer F, König HH, Hajek A (2019) Osteoporosis, fear of falling, and restrictions in daily living. Evidence from a nationally representative sample of community-dwelling older adults. Front Endocrinol 10:1–6. https://doi.org/10.3389/fendo.2019.00646
Eldeeb AM, Khodair AS (2014) Three-dimensional analysis of gait in postmenopausal women with low bone mineral density. J Neuroeng Rehabil 11:1–7. https://doi.org/10.1186/1743-0003-11-55
Lui L, Stone K, Cauley JA, Hillier T, Yaffe K (2003) Bone loss predicts subsequent cognitive decline in older women: the study of osteoporotic fractures. J Am Geriatr Soc 51:38–43. https://doi.org/10.1034/j.1601-5215.2002.51007.x
American Geriatrics Society, Geriatrics Society, American Academy Of, Orthopaedic Surgeons Panel On Falls Prevention (2001) Guideline for the prevention of falls in older persons. J Am Geriatr Soc 49:664–672. https://doi.org/10.1046/j.1532-5415.2001.49115.x
Orces CH (2021) The association between walking speed and bone turnover markers in older adults. Cureus. https://doi.org/10.7759/cureus.18019
Himes CL, Reynolds SL (2012) Effect of obesity on falls, injury, and disability. J Am Geriatr Soc 60:124–129. https://doi.org/10.1111/j.1532-5415.2011.03767.x
Borer KT (2005) Physical activity in the prevention and amelioration of osteoporosis in women: interaction of mechanical, hormonal and dietary factors. Sports Med 35:779–830. https://doi.org/10.2165/00007256-200535090-00004
Wareham NJ, van Sluijs EMF, Ekelund U (2005) Physical activity and obesity prevention: a review of the current evidence. Proc Nutr Soc 64:229–247. https://doi.org/10.1079/pns2005423
Thomsen MJ, Liston M, Christensen MG, Vestergaard P, Hirata RP (2021) Dancing against falls iN Community-dwElling older adults (DANCE): a study protocol of a stratified, block-randomised trial. Injury Prevention :injuryprev-044224. https://doi.org/10.1136/injuryprev-2021-044224
Duarte M, Zatsiorsky VM (2002) Effects of body lean and visual information on the equilibrium maintenance during stance. Exp Brain Res 146:60–69. https://doi.org/10.1007/s00221-002-1154-1
Franchignoni F, Horak F, Godi M, Nardone A, Giordano A (2010) Using psychometric techniques to improve the Balance Evaluation Systems Test: the mini-BESTest. J Rehabil Med 42:323–331. https://doi.org/10.2340/16501977-0537
Montero-Odasso M, Almeida QJ, Bherer L, Burhan AM, Camicioli R, Doyon J, Fraser S, Muir-Hunter S, Li KZH, Liu-Ambrose T, McIlroy W, Middleton L, Morais JA, Sakurai R, Speechley M, Vasudev A, Beauchet O, Hausdorff JM, Rosano C, Studenski S, Verghese J (2019) Consensus on shared measures of mobility and cognition: From the Canadian Consortium on Neurodegeneration in Aging (CCNA). J Gerontol A Biol Sci Med Sci 74:897–909. https://doi.org/10.1093/gerona/gly148
Rikli RE, Jones CJ (2013) Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 53:255–267. https://doi.org/10.1093/geront/gns071
Fjeldstad C, Fjeldstad AS, Acree LS, Nickel KJ, Gardner AW (2008) The influence of obesity on falls and quality of life. Dyn Med 7:1–6. https://doi.org/10.1186/1476-5918-7-4
Burton BT, Foster WR (1985) Health implications of obesity: an NIH Consensus Development Conference. J Am Diet Assoc 85:1117–1121. https://doi.org/10.1016/S0002-8223(21)03768-8
Gordy S, Fabricant L, Ham B, Mullins R, Mayberry J (2014) The contribution of rib fractures to chronic pain and disability. Am J Surg 207:659–663. https://doi.org/10.1016/j.amjsurg.2013.12.012
Patel KV, Guralnik JM, Dansie EJ, Turk DC (2013) Prevalence and impact of pain among older adults in the United States: findings from the 2011 National Health and Aging Trends Study. Pain 154:2649–2657. https://doi.org/10.1016/j.pain.2013.07.029
Larsson C, Ekvall Hansson E, Sundquist K, Jakobsson U (2016) Impact of pain characteristics and fear-avoidance beliefs on physical activity levels among older adults with chronic pain: a population-based, longitudinal study. BMC Geriatr 16:1–8. https://doi.org/10.1186/s12877-016-0224-3
Stauffer ME, Taylor SD, Watson DJ, Peloso PM, Morrison A (2011) Definition of nonresponse to analgesic treatment of arthritic pain: an analytical literature review of the smallest detectable difference, the minimal detectable change, and the minimal clinically important difference on the pain visual analog scale. Int J Inflamm 2011:1–6. https://doi.org/10.4061/2011/231926
Hirata RP, Arendt-Nielsen L, Graven-Nielsen T (2010) Experimental calf muscle pain attenuates the postural stability during quiet stance and perturbation. Clin Biomech 25:931–937. https://doi.org/10.1016/j.clinbiomech.2010.06.001
Hodges PW, Moseley GL, Gabrielsson A, Gandevia SC (2003) Experimental muscle pain changes feedforward postural responses of the trunk muscles. Exp Brain Res 151:262–271. https://doi.org/10.1007/s00221-003-1457-x
Kobayashi M, Takahashi K, Sato M, Usuda S (2015) Association of performance of standing turns with physical impairments and walking ability in patients with hemiparetic stroke. J Phys Ther Sci 27:75–78. https://doi.org/10.1589/jpts.27.75
Mirelman A, Herman T, Brozgol M, Dorfman M, Sprecher E, Schweiger A, Giladi N, Hausdorff JM (2012) Executive function and falls in older adults: new findings from a five-year prospective study link fall risk to cognition. PLoS One 7:1–8. https://doi.org/10.1371/journal.pone.0040297
Muir SW, Gopaul K, Montero Odasso MM (2012) The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing 41:299–308. https://doi.org/10.1093/ageing/afs012
Vassallo M, Mallela SK, Williams A, Kwan J, Allen S, Sharma JC (2009) Fall risk factors in elderly patients with cognitive impairment on rehabilitation wards. 41–6. https://doi.org/10.1111/j.1447-0594.2008.00506.x
Busch TDA, Duarte YA, PiresNunes D, Lebrão ML, Satya Naslavsky M, Dos Santos RA, Amaro E (2015) Factors associated with lower gait speed among the elderly living in a developing country: a cross-sectional population-based study. BMC Geriatr 15:1–9. https://doi.org/10.1186/s12877-015-0031-2
Robinovitch SN, Feldman F, Yang Y, Schonnop R, Leung PM, Sarraf T, Sims-Gould J, Loughi M (2013) Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. Lancet 381:47–54. https://doi.org/10.1016/S0140-6736(12)61263-X
Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, Cumming RG, Herbert RD, Close JCT, Lord SR (2017) Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med 51:1750–1758. https://doi.org/10.1136/bjsports-2016-096547
Hansen RK, Jochum E, Egholm D, Villumsen M, Hirata RP (2024) Moving together - benefits of an online dance program on physical and mental health for older women: an exploratory mixed-method study. BMC Geriatr 24:392–396. https://doi.org/10.1186/s12877-024-04983-6
Acknowledgements
A thank you to Ms Mette Brodersen, Ms Line Rosengreen Kaldahl, Ms Katrine Bruhn Vogensen, and Ms Ingelise Leegaard, all from Steno Diabetes Center North Jutland, Aalborg, Denmark, for their expertise and help performing DXA scans.
Funding
Open access funding provided by Aalborg University Author RPH was funded by Trygfonden (grant number 124404), the Obel family foundation, Augustinus fonden (grant number 18–4708), and Dansk Oplysnings Forbund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study is conducted in accordance with the Helsinki Declaration and approved by the local Ethics Committee of The North Denmark Region (N-20180065) in October 2018 and registered at ClinicalTrials.gov (NCT03683849). test. All participants provided informed written consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rogerio Pessoto Hirata and Mikkel Jacobi Thomsen share first authorship.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hirata, R.P., Thomsen, M.J., Liston, M. et al. Clinical features of fallers and non-fallers: finding best-performing combinations of physical performance measurements to discriminate physical impairments between fallers and non-fallers among older adults with and without osteoporosis. Osteoporos Int (2024). https://doi.org/10.1007/s00198-024-07233-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00198-024-07233-y