Abstract
Summary
Hypophosphatasia (HPP) is a rare bone disease with limited scientific evidence on the tolerability and safety of its novel treatment, Asfotase Alfa (AA). We report 7 HPP patients’ heterogenous presentations and the significant improvement in various clinical outcomes attained with AA shedding light on this highly effective and safe therapy.
Introduction
Hypophosphatasia (HPP) is a rare inherited metabolic bone disorder characterized by a deficiency in the tissue non-specific alkaline phosphatase (TNSALP) due to loss of function mutation in the ALPL gene. HPP is associated with impaired skeletal mineralization due to elevations in inorganic pyrophosphate and altered phosphate : pyrophosphate ratio. Asfotase alfa (AA) “enzyme replacement” was approved for treatment of HPP in 2015. We present 7 patients with HPP, 5 with pediatric-onset, and 2 with adult-onset, who have been treated with AA and describe the efficacy and safety in these patients.
Methods
7 patients (4 females, 3 males) aged 19–68 years with HPP were included in this study. Diagnosis of HPP was confirmed by DNA analysis. AA was administered in doses of 6mg/kg/week with a mean follow-up of 6 months (SD= 5).
Results
Subjective improvement in muscle strength, muscle pain, walking ability, and walking distance with a reduction in the use of gait aids was seen “with AA in HPP patients.” Muscle strength and pain improved by up to 70% from baseline as quantified subjectively by patients. Walking distance improved by up to 100%. Patients also reported improved cognition, mood, and energy levels, with up to 90% improvement in mood and 75% improvement in energy levels. 4 out of 6 patients first noted clinical signs of improvement after 3 months of being on therapy. 1 out of the 7 patients sustained a toe fracture 10 months from being on AA. AA was well-tolerated with injection site reactions being the most reported adverse effect.
Conclusion
HPP treatment with AA in individuals with both pediatric and adult-onset forms resulted in significant subjective improvement in musculoskeletal and cognitive manifestations in addition to patients’ quality of life. The drug was well tolerated in 6 patients. 1 patient discontinued therapy because of minor adverse effects with myalgias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypophosphatasia (HPP) is an inherited metabolic bone disorder characterized by loss of function mutation in the alkaline phosphatase (ALPL) gene resulting in a deficiency in the tissue-nonspecific alkaline phosphatase (TNSALP). Reduced activity of TNSALP results in the systemic accumulation of its substrates including pyridoxal 5′-phosphate (PLP), inorganic pyrophosphate (PPi), and urinary phosphoethanolamine (PEA), with consequent impaired bone mineralization, skeletal defects, and systemic manifestations of the disease [1].
PPi is a potent inhibitor of mineralization that interferes with the formation of hydroxyapatite crystals, resulting in skeletal hypomineralization, and this manifests clinically as rickets in infants and children or osteomalacia in adults [2,3,4]. PLP is the main circulating form of vitamin B6. It acts as an essential cofactor in neurotransmitter synthesis, being able to cross the blood brain barrier only in its dephosphorylated form. TNSALP dephosphorylates PLP to pyridoxal that is then able to enter neuronal cells and is phosphorylated again to PLP. With loss of function mutations in the ALPL gene, reduced concentrations of PLP result in a deficiency in GABA in the central nervous system leading to vitamin B6-dependant seizures in children and various other neurological symptoms including depression, anxiety, and neuropathy [5, 6]. The effects and clinical implications of PEA accumulation are less understood than PPi and PLP.
HPP is inherited in either an autosomal dominant or autosomal recessive manner, with marked variability in clinical expression [7]. Six different clinical forms of HPP have been described, classified based on the age of onset and severity of symptoms: perinatal (age: in utero and at birth, lethal), perinatal (benign), infantile (age <6 months), childhood (age >6 months and <18 years), adult (age >18 years), and odontohypophosphatasia (affects teeth only) [8, 9]. Mornet et al described a genetic-based classification of HPP based on genetic inheritance and their prevalence [10]. Severe HPP is rare, inherited in an autosomal recessive manner, and corresponds to perinatal and most of infantile severe forms. Moderate HPP is more common than severe HPP, can be of autosomal recessive or dominant inheritance, and includes infantile moderate, childhood, odontohypophosphatasia and adults with specific signs. Mild HPP is very common, inherited in an autosomal dominant manner due to a haploinsufficiency mechanism not clearly identified yet, and corresponds to adults (and perhaps children) with less severe and often nonspecific signs. This latter classification is believed to provide a more accurate genotype-phenotype correlation compared to the former where there can be an overlap in the severity among the different clinical forms.
Adults with HPP may therefore have onset in childhood or adulthood and commonly present with recurrent/poorly healing metatarsal and long bone fractures, pseudofractures, pseudogout, muscle weakness, loss of secondary teeth, and bone, joint, and muscle pain [11,12,13].
In October 2015, the FDA approved asfotase alfa (AA), a human recombinant enzyme replacement of TNSALP, for use in all ages in childhood-onset HPP (symptom onset less than 18 years of age). Studies have shown significant improvement in bone mineralization, growth, mobility, survival, reduced skeletal abnormalities, and respiratory symptoms, with benefits persisting for up to 7 years in infants and children [14]. In adults, studies are limited with regard to efficacy and safety of AA. Kishnani et al. looked at the efficacy and safety of AA in adolescents and adults with HPP over a 5-year treatment period [15]. Significant improvement was observed in functional measures (walking distance, reliance on walking assistive devices, and proximal muscle strength) and substrate levels—PLP and PPi. Out of the 19 patients randomized to AA, 5 did not complete the study, 1 of which was attributed to serious adverse events (anaphylactoid reaction) indicating it to be generally well tolerated.
In another case report, 2 adult patients with pediatric-onset HPP with poor fracture healing in 4 long bone fractures and pseudofractures were treated with AA [16]. Clinical and radiographic improvement in bone healing was noted a few months after starting therapy without any reported adverse effects.
We present 7 patients with known HPP that we commenced on AA. This report highlights the heterogeneity in their clinical presentations and their response to therapy with AA.
Subjects and methods
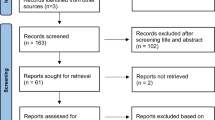
Patients who had a confirmed molecular diagnosis of HPP were identified by medical records at the Department of Medicine, McMaster University, Hamilton, Ontario, Canada. Medical records were reviewed, and only patients with HPP treated with AA were included. 7 patients (4 females, 3 males) aged 19–68 years were referred to our clinic between 2017 and 2021 with either known or possible HPP for further evaluation and management. The characteristics and clinical features of those patients are outlined in Table 1. The laboratory measurements of both serum and urine parameters were performed following standards set by Canadian laboratories. These parameters include alkaline phosphatase, vitamin B6, urine PEA, serum/plasma calcium and phosphate, 24-hour urine calcium, 25-hydorxyvitamin D, and estimated glomerular filtration rate (eGFR). With regard to imaging, DXA was done on either Hologic or Lunar machines, and conventional X-rays were used to perform skeletal surveys. Patients also underwent renal ultrasounds to assess for complications including nephrolithiasis and nephrocalcinosis. DNA analysis via extraction of genomic DNA by peripheral blood leukocytes and subsequent analysis of the ALPL gene was carried out in patients with no prior genetic testing.
Clinical cases
Patient 1
A 46-year-old Japanese female with no significant past medical history was referred to our clinic for evaluation of skeletal health in the setting of low bone mineral density (BMD). DXA showed a lumbar spine BMD of 0.637 g/cm2 (Z-score of −3.3) and femoral neck BMD of 0.538 g/cm2 (Z-score of −2.4). She had several low-trauma fractures including a radial fracture at age 12 years, rib fractures after a coughing bout at age 32 years and 3 toe fractures. She denied any clinical features of osteogenesis imperfecta (OI) but was noted on physical examination to have mild joint laxity. Alkaline phosphatase (ALP) was in the low normal range of 40–54 U/L (normal range 45–120 U/L). DNA analysis was pursued to rule out OI and revealed a heterozygous mutation in the ALPL gene, with a c.979T>C (p.Phe327Leu) variant that is known to be pathogenic. No mutation in COL1A1 or COL1A2 genes was identified. 24-hour urine calcium was high; renal ultrasound showed only milk of calcium cyst on the right side. She was deemed to have pediatric onset HPP, and considering her mild degree of disease, she was not initiated on AA immediately. Low BMD was managed with hormone replacement therapy (HRT) as she was perimenopausal at the time of presentation. She was followed on an annual basis in our clinic during which time she started developing left lower back and thigh pain. This progressed to difficulty ambulating, muscle fatigue, balance problems, and restricted mobility to avoid falls. BMD was also declining despite HRT, and a decision was subsequently made to start AA, 4 years from the time of molecular diagnosis. She was seen in follow-up 1 month later and reported notable improvement in her muscle fatigue, balance, and energy levels (Tables 3, 4, and 5). The injections were well tolerated with no reported adverse events. Regarding family history, she has 2 children aged 6 (boy) and 9 years (girl) who had no concerning features at the time of presentation (no fractures or dental issues). At age 12 years, her daughter started having several fractures (elbow and forearm while playing soccer) and at age 13 sustained a hip fracture after a sprint and evaluated by a pediatric HPP specialist in Japan, and ALP levels were normal. No genetic testing was done. Her son continues to be asymptomatic.
Patient 2
A 53-year-old male was referred to our clinic for evaluation of possible HPP. This was in the setting of recurrent fractures and low ALP of 9 U/L (normal range 40–129 U/L). He had bilateral femoral stress fractures at age 51 years requiring intramedullary nail fixation and left ulnar fracture at age 52 years after slipping and falling from his own height. He had loss of 2 deciduous teeth at age 2 years, no other dental issues. He had generalized musculoskeletal pain and bilateral knee pain. Laboratory testing confirmed low ALP in 9–14 U/L range (normal range 35–125 U/L). DNA analysis revealed heterozygous ALPL gene mutations in 2 variants: c.881A>C (p.Asp294Ala) pathogenic gene variant and c.571G>A (p.Glu191Lys) likely pathogenic gene variant—the latter later classified as pathogenic. The patient was deemed to have pediatric-onset HPP and was initiated on AA. He was evaluated in follow-up and admitted to improvement in the generalized musculoskeletal pain and knee pain (Tables 3, 4, and 5). There were no reported adverse events. Regarding family history, he has 2 daughters whose screen for HPP was negative.
Patient 3
A 47-year-old female was referred to our clinic for management of known HPP. She was diagnosed with HPP at age 44 years in the setting or recurrent bilateral atraumatic metatarsal fractures. She had premature loss of deciduous teeth at 13 months of age, with roots intact. She also reported a 20-year history of upper thoracic and lumbar back pain, generalized arthralgia, myalgia, and muscle weakness. The review of the genetic report showed her to be heterozygous for a pathogenic variant, c571G>A (pGlu191Lys), and a likely pathogenic variant, c1250A>G (p.Asn417Ser) in the ALPL gene. She was deemed to have pediatric-onset HPP. On presentation, ALP was low at 8–10 U/L (normal range 35-120 U/L) and phosphate was high at 1.50 mmol/L (normal range 0.8–1.45mmolL). Vitamin B6 was high at 560 nmol/L (normal range 20–96 nmol/L). Urine PEA returned high at 20 mmol/mol (normal range 0–12 mmol/mol). DXA scan showed normal BMD, and spinal X-rays showed multilevel degenerative changes. A request for AA was submitted, however, denied. The patient was managed conservatively with pain medications and physical therapy. In clinic follow-up, the patient endorsed new left hip pain and a bone scan was pursued revealing bilateral atypical femoral fracture (AFF). AA was subsequently approved and initiated 1 month following the AFF. After the first injection, she developed redness and itching at the injection site. Symptoms resolved a few days later. The second injection was delayed for a few days then resumed at half the dose; she received 3 half doses and then resumed on full dose again. She continued to have minor skin reactions following the injections, generally tolerating the AA well. 10 months after starting AA, she developed left shoulder pain, ultrasound showed calcific tendinopathy in the subscapularis muscle, and this was deemed secondary to HPP. Since starting AA there have been no new fractures. She reported dramatic improvement in walking and is now able to run, muscle pain also improved (Tables 3, 4, and 5). Due to ongoing injection skin reactions, AA was reduced in frequency from 2mg/kg three times weekly to 3mg/kg twice weekly. Regarding family history, both parents were identified as carriers of the ALPL gene mutations. She has 1 younger brother with low ALP, but no DNA analysis has been done yet. Her 2 children are without clinical features of HPP. A maternal cousin’s daughter has confirmed HPP.
Patient 4
A 48-year-old Mennonite male with primary hypothyroidism, depression, and anxiety was referred to our clinic for further evaluation of possible HPP in the setting of low ALP and musculoskeletal complaints. He reported muscle pain and weakness ongoing for the preceding 6 years since age 42 years, to which he was using a cane for stability with a fear of falling. He also had extreme fatigue, lethargy and “brain fog.” He was diagnosed with polymyositis in Mexico a few years back and was put on 100mg of prednisone, tapered off upon his return to Canada due to disputable muscle biopsy results insufficient to support this diagnosis. There was no prior history of fractures, renal stones, or premature dental loss. He had generalized back pain since age 13 years. ALP was low at <20 U/L (normal range 36–144 U/L). 24-hour urine calcium was high but no renal stones identified on renal ultrasound. DNA analysis showed him to be heterozygous for the pathogenic variant c.1001G>A (p.Gly334Asp) in the ALPL gene. This variant in the homozygous state was reported in Canadian Mennonite HPP families. He was deemed to have adult-onset HPP and was started on AA. In the first clinic visit after the injection, 3 months later, he noted significant improvement in cognitive function. Over the subsequent year he noted improvement in muscle strength with increased walking tolerance (Tables 3, 4, and 5). Prior to therapy, he was able to walk half a block before he had to stop due to muscle weakness and fatigue. Since therapy, he has been able to walk for 2–3 blocks without the use of any gait aid. He continues to have generalized myalgias after more strenuous activity, but overall, his tolerance to activity is better and recovery time is significantly shortened. He had mild fatigue after the first injection; there were no other reported adverse events. Regarding family history, both parents were of Mennonite descent. While they did not go genetic testing, his sister and her daughter both carry the same ALPL gene mutation. He does not have any biological children.
Patient 5
A 23-year-old female with known HPP, diagnosed in childhood, was referred to our clinic for transitioning from pediatric to adult care. She was born full term, with no respiratory difficulties at birth, and muscle tone was normal. There were no skeletal deformities, and she started walking at age 1 year, with normal developmental milestones. There were no seizures either. At age 2 years, she lost 3 deciduous teeth with the roots intact. At age 4 years, she was diagnosed with HPP based on DNA analysis. She is heterozygous for the mutation N400S in the ALPL gene and thus has pediatric-onset HPP. After diagnosis, family screening revealed her father and younger sister (patient 6) to have HPP and harbor the same pathogenic variant in the ALPL gene. On further inquiry, her father had infantile HPP and had corrective skull surgery for craniosynostosis, no dental issues. On presentation to our clinic, she noted arm and knee pain since age 11 years and lumbar back pain since age 13 years, headaches, and fatigue. She was having ongoing dental issues with significant mobility in her teeth and periodontitis; however, no further teeth loss. Other than HPP, medical history was significant for depression, anxiety, and psoriasis. Laboratory testing showed low ALP at 15–17 U/L (normal range 35–122 U/L). Vitamin B6 was high at 45.6 mcg/L (normal range 2.0–32.8 mcg/L). AA was started, and following the first injection, she had redness at the injection site with no other associated symptoms, this resolved after 4–5 days. Subsequent injections have been well tolerated with no adverse events. 6 months later, the patient noticed improvement in her cognition, mood, and energy levels. Significant improvement in the myalgias and muscle strength was noted 12 months since being on AA (Tables 3, 4, and 5).
Patient 6
A 19-year-old female with known HPP, diagnosed in childhood, was referred to our clinic for transitioning from pediatric to adult care. She was diagnosed at 11 months of age as part of family screening following the diagnosis of her older sister (patient 5) and was deemed to have pediatric-onset HPP. She was born full-term without respiratory difficulty at birth. She had normal muscle tone and developmental milestones and walked at 11 months. There were no skeletal deformities, fractures, or infantile seizures. She lost her deciduous teeth at age 6 years with roots out. She had learning disability with reading and writing; no formal psychological diagnosis was made. On presentation, she was reporting generalized fatigue, intermittent thoracic back pain since age 14 years, and frequent headaches since age 14 as well. She also reported recurrent bouts of vomiting after dinner meals since age 3 to present that has not been investigated. DNA analysis showed her to be heterozygous for the mutation N400S in the ALPL gene. Laboratory testing was remarkable for low ALP at 15–19 U/L (normal range 35–122 U/L) and high vitamin B6 of 69 mcg/L (normal range 2.0–32.8 mcg/L). AA was initiated, and 1 month later, she noted improvement in her headaches and vomiting up to 50% and 75% improvement at 12 months of therapy, respectively. There was no significant improvement in musculoskeletal symptoms or energy levels (Tables 3, 4, and 5). She reported increased pain in both hands since starting AA; there was no other reported adverse effect. She also sustained an atraumatic toe fracture after 10 months of being on AA.
Patient 7
A 68-year-old male with known dyslipidemia, obstructive sleep apnea, prediabetes, and newly diagnosed hypogonadism, was referred to our clinic for evaluation of possible HPP in the setting of low ALP. He was noted to have low ALP since age 63 years and no dental issues during childhood but was having loose teeth and recurrent teeth abscesses and had lost 5 teeth over the preceding 2 years at age 66–68 years. There were no fractures, seizures, or mood disorder. Since age 65 years, he has had increasing fatigue, lumbar back pain, and progressive pain the in the knees, hips, and ankles. Laboratory testing showed low ALP 23–25 U/L (normal range 40–129 U/L). DXA scan sowed osteoporosis, multifactorial with history of hypogonadism, and vitamin D insufficiency. DNA analysis showed him to be heterozygous for a pathogenic variant in the ALPL gene-c.575T>C (p.Met192Thr). He was deemed to have adult-onset HPP. We recommended treatment with AA; however, he was reluctant to start therapy. Due to persistence of arthralgias and new myalgias, he agreed on therapy. 10 days after initiation of therapy, he developed the following symptoms: shortness of breath, irritability, nausea, generalized body aches, dry and itchy eyes, left leg and ankle numbness, and sharp lumbar back pain. He subsequently stopped therapy with AA and was treated with teriparatide for the osteoporosis. Family history is negative for HPP.
Discussion
HPP is a rare inherited disorder of bone and mineral metabolism. Due to its low prevalence, HPP is often misdiagnosed as other more common bone disorders. A thorough history, physical examination, and laboratory studies including ALP, calcium, phosphate, and vitamin B6 are crucial to avoid delays in diagnosis or misdiagnosis.
Clinical presentation is also highly variable in both children and adults. Of the 7 patients included in this case series, 5 were deemed to have pediatric-onset HPP with the first symptoms manifesting before age 18 years and 2 adult-onset HPP. All patients reported musculoskeletal pain, 3 had fractures associated with minimal to no trauma, 3 had premature loss of primary teeth, 1 had loss of secondary teeth, 2 had limited mobility, and 2 had “brain fog” or memory problems. 1 patient presented with osteoporosis, later deemed to be low bone density secondary to HPP, and 1 had osteoporosis secondary to multiple other factors. Patients 5 and 6 were part of the same family and harbored the same pathogenic variants in the ALPL gene, yet their clinical symptoms were different.
It is important to note that low bone mass can be a presenting feature of HPP, and misdiagnosis with osteoporosis and subsequent treatment with bisphosphonates further undermines the defective mineralization [17]. This is because bisphosphonates can inhibit the effect of and reduce ALP levels [18]. It is therefore empiric to ensure HPP is excluded prior to diagnosing osteoporosis and starting therapy in patients noted to have low ALP or other features suggestive of HPP. HPP can also result in the extracellular accumulation of PPi that compounds with calcium forming calcium pyrophosphate crystals, and these deposit in joints resulting in chondrocalcinosis or pseudogout [19, 20]. They can also deposit in the kidneys and result in nephrolithiasis [8, 10, 21]. Screening for these conditions was undertaken in our patients, and 3 patients were found to have low bone density. None of our patients had renal stones or chondrocalcinosis.
All patients included in this report had genetically confirmed HPP. 7 different pathogenic variants in the ALPL gene were identified, 6 of which were previously reported in HPP patients and known to be pathogenic (Table 2). 5 patients had heterozygous variants (a pathogenic variant on 1 allele), and 2 patients had compound heterozygous variants (2 different pathogenic variants on opposite alleles).
AA is the first-in-class treatment approved for HPP [22]. Prior to it its FDA approval in 2015, treatment of HPP consisted largely of supportive care [23]. AA works by replacing the deficient TNSALP therefore reducing the extracellular accumulation of its substrates. It is administered as a subcutaneous injection at the recommended dose of 6mg/kg/week, commonly administered as 3mg/kg twice a week. This dose was based on studies mostly in the pediatric population [12, 24, 25]. In adults, a 13-week, open-label study was undertaken in those with pediatric-onset HPP. They evaluated variable doses of AA and findings confirmed that the 6mg/kg/week dose was more effective in reducing TNSALP substrates to within normal range than the lower dose of 1.5mg/kg/week [26]. This was the dose administered to our patients.
Notable subjective improvements in muscle strength, muscle pain, walking ability, and walking distance with a reduction in the use of gait aids were seen. Cognition and mood also improved. These effects were seen as early as 1 month from initiation of therapy. For some, it took as long as long as 1 year for significant clinical improvement to be observed. As no objective measure was utilized to assess improvement in symptoms, the possibility of a placebo effect can also be considered. ALP levels were elevated in the thousands on AA. While we do not have post-therapy vitamin B6 levels to assess and compare to pre-therapy values, we highly suspect that these values have returned to normal consistent with the subjective symptom improvement observed.
Patients were asked to quantify the improvement in their walking distance, muscular function, mood, and energy levels at 3, 6, 9, 12, and 24 months, when applicable, from starting treatment with AA. The results are shown in Tables 3, 4, 5 and 6 . 5 out of the 6 patients did not notice any subjective improvement before 6 months of being on AA. It is therefore crucial that this expectation be discussed with patients starting therapy.
With regard to safety of AA, injection site reactions are the most frequently reported adverse effects on review of literature [24, 25, 27, 28]. The most commonly reported side effects in our patients included: injection site reactions in 2 patients, tiredness in 1 patient, bilateral hand pain in 1 patient, and no adverse effects in 2 patients (Table 3). 1 patient reported nonspecific symptoms within 10 days of initiating AA and subsequently discontinued therapy. None of the patients developed tooth abscesses as a complication.
In conclusion, the clinical presentation of HPP is highly variable, even among family members harboring the same pathogenic variants of the ALPL gene. Treatment with AA is proven to be well tolerated with only minor adverse effects and significant improvement in symptoms and prognosis, especially in pediatric-onset HPP. With regard to adult-onset HPP, our patient had subjective improvement in muscle strength, walking distance, and cognition on therapy. Further studies are still warranted to explore the effect of treatment in adult-onset HPP and the unknown long-term safety profile of AA, in addition to its resultant elevation in ALP levels. Development of anti-asfotase alfa antibodies is a potential complication of enzyme replacement therapy that also warrants further evaluation. These antibodies can exert a neutralizing effect to the AA; while it has not been seen to hinder or make therapy less effective after 7 years of treatment in several studies [12, 25, 28], further evaluation is essential to better understand the lack or limited clinical response that might be seen in some patients.
References
Fedde KN, Whyte MP (1990) Alkaline phosphatase (tissue-nonspecific isoenzyme) is a phosphoethanolamine and pyridoxal-5′-phosphate ectophosphatase: normal and hypophosphatasia fibroblast study. Am J Hum Genet 47(5):767–775
Addison WN, Azari F, Sorensen ES, Kaartinen MT, McKee MD (2007) Pyrophosphate inhibits mineralization of osteoblast cultures by binding to mineral, up-regulating osteopontin, and inhibiting alkaline phosphatase activity. J Biol Chem 282(21):15872–15883
Fleisch H (1981) Diphosphonates: history and mechanisms of action. Metab Bone Dis Relat Res 3(4-5):279–287
Whyte MP (2010) Physiological role of alkaline phosphatase explored in hypophosphatasia. Ann N Y Acad Sci 1192:190–200
Wilson MP, Plecko B, Mills PB, Clayton PT (2019) Disorders affecting vitamin B(6) metabolism. J Inherit Metab Dis 42(4):629–646
Baumgartner-Sigl S, Haberlandt E, Mumm S, Scholl-Burgi S, Sergi C, Ryan L et al (2007) Pyridoxine-responsive seizures as the first symptom of infantile hypophosphatasia caused by two novel missense mutations (c.677T>C, p.M226T; c.1112C>T, p.T371I) of the tissue-nonspecific alkaline phosphatase gene. Bone 40(6):1655–1661
Nunes ME (1993) Hypophosphatasia. In: Adam MP, Everman DB, Mirzaa GM, Pagon RA, Wallace SE, LJH B et al (eds) GeneReviews((R)), Seattle (WA)
Bianchi ML (2015) Hypophosphatasia: an overview of the disease and its treatment. Osteoporos Int 26(12):2743–2757
Whyte MP, Zhang F, Wenkert D, McAlister WH, Mack KE, Benigno MC et al (2015) Hypophosphatasia: validation and expansion of the clinical nosology for children from 25 years experience with 173 pediatric patients. Bone (New York, NY) 75:229–239
Mornet E, Taillandier A, Domingues C, Dufour A, Benaloun E, Lavaud N et al (2021) Hypophosphatasia: a genetic-based nosology and new insights in genotype-phenotype correlation. Eur J Hum Genet 29(2):289–299
Berkseth KE, Tebben PJ, Drake MT, Hefferan TE, Jewison DE, Wermers RA (2013) Clinical spectrum of hypophosphatasia diagnosed in adults. Bone 54(1):21–27
Shapiro JR, Lewiecki EM (2017) Hypophosphatasia in adults: clinical assessment and treatment considerations. J Bone Miner Res 32(10):1977–1980
Khan AA, Josse R, Kannu P, Villeneuve J, Paul T, Van Uum S et al (2019) Hypophosphatasia: Canadian update on diagnosis and management. Osteoporos Int 30(9):1713–1722
Whyte MP, Simmons JH, Moseley S, Fujita KP, Bishop N, Salman NJ et al (2019) Asfotase alfa for infants and young children with hypophosphatasia: 7 year outcomes of a single-arm, open-label, phase 2 extension trial. Lancet Diabetes Endocrinol 7(2):93–105
Kishnani PS, Rockman-Greenberg C, Rauch F, Bhatti MT, Moseley S, Denker AE et al (2019) Five-year efficacy and safety of asfotase alfa therapy for adults and adolescents with hypophosphatasia. Bone 121:149–162
Klidaras P, Severt J, Aggers D, Payne J, Miller PD, Ing SW (2018) Fracture healing in two adult patients with hypophosphatasia After Asfotase Alfa Therapy. JBMR Plus 2(5):304–307
Lefever E, Witters P, Gielen E, Vanclooster A, Meersseman W, Morava E et al (2020) Hypophosphatasia in adults: clinical spectrum and its association with genetics and metabolic substrates. J Clin Densitom 23(3):340–348
Vaisman DN, McCarthy AD, Cortizo AM (2005) Bone-specific alkaline phosphatase activity is inhibited by bisphosphonates: role of divalent cations. Biol Trace Elem Res 104(2):131–140. https://doi.org/10.1385/BTER:104:2:131
Chuck AJ, Pattrick MG, Hamilton E, Wilson R, Doherty M (1989) Crystal deposition in hypophosphatasia: a reappraisal. Ann Rheum Dis 48(7):571–576
Guañabens N, Mumm S, Möller I, González-Roca E, Peris P, Demertzis JL et al (2014) Calcific periarthritis as the only clinical manifestation of hypophosphatasia in middle-aged sisters. J Bone Miner Res 29(4):929–934
Conti F, Ciullini L, Pugliese G (2017) Hypophosphatasia: clinical manifestation and burden of disease in adult patients. Clin Cases Miner Bone Metab 14(2):230–234
Whyte MP (2016) Hypophosphatasia - aetiology, nosology, pathogenesis, diagnosis and treatment. Nat Rev Endocrinol 12(4):233–246
Millan JL, Plotkin H (2012) Hypophosphatasia - pathophysiology and treatment. Actual osteol 8(3):164–182
Kitaoka T, Tajima T, Nagasaki K, Kikuchi T, Yamamoto K, Michigami T et al (2017) Safety and efficacy of treatment with asfotase alfa in patients with hypophosphatasia: results from a Japanese clinical trial. Clin Endocrinol (Oxf) 87(1):10–19
Whyte MP, Greenberg CR, Salman NJ, Bober MB, McAlister WH, Wenkert D et al (2012) Enzyme-replacement therapy in life-threatening hypophosphatasia. N Engl J Med 366(10):904–913
Seefried L, Kishnani PS, Moseley S, Denker AE, Watsky E, Whyte MP et al (2021) Pharmacodynamics of asfotase alfa in adults with pediatric-onset hypophosphatasia. Bone 142:115664
Whyte MP, Madson KL, Phillips D, Reeves AL, McAlister WH, Yakimoski A et al (2016) Asfotase alfa therapy for children with hypophosphatasia. JCI insight 1(9):e85971–e85971
Kishnani PS, Rush ET, Arundel P, Bishop N, Dahir K, Fraser W et al (2017) Monitoring guidance for patients with hypophosphatasia treated with asfotase alfa. Mol Genet Metab 122(1-2):4–17
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alsarraf, F., Ali, D., Almonaei, K. et al. Hypophosphatasia: presentation and response to asfotase alfa. Osteoporos Int 35, 717–725 (2024). https://doi.org/10.1007/s00198-023-06943-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06943-z