Abstract
Summary
In older men, higher high-sensitivity C-reactive protein (hsCRP) concentrations were associated with faster prospectively assessed endocortical expansion (distal radius, distal tibia) and slightly higher cortical bone loss at distal tibia, but not with the fracture risk. High hsCRP level has a limited impact on bone decline in older men.
Purpose
Data on the link of the high-sensitivity C-reactive protein (hsCRP) with bone loss and fracture risk are discordant. We studied the association of the hsCRP with the prospectively assessed decrease in areal bone mineral density (aBMD), bone microarchitecture decline, and fracture risk in older men.
Methods
At baseline, hsCRP was measured in 823 men aged 60–88. Areal BMD and bone microarchitecture (distal radius, distal tibia) were assessed by dual-energy X-ray absorptiometry and high-resolution peripheral QCT, respectively, at baseline and after 4 and 8 years. Data on incident fractures were collected for 8 years.
Results
Higher hsCRP concentration was associated with faster increase in aBMD at the whole body and lumbar spine, but not other sites. Higher hsCRP levels were associated with faster decrease in cortical area and more rapid increase in trabecular area at the distal radius (0.048 mm2/year/SD, p < 0.05) and distal tibia (0.123 mm2/year/SD, p < 0.001). At the distal tibia, high hsCRP level was associated with greater decrease in total and cortical volumetric BMD (vBMD) and in failure load. The hsCRP levels were not associated with the fracture risk, even after accounting for competing risk of death.
Conclusion
Higher hsCRP levels were associated with greater endocortical expansion at the distal radius and tibia. Higher hsCRP was associated with slightly faster decrease in total and cortical vBMD and failure load at distal tibia, but not with the fracture risk. Thus, high hsCRP levels are associated with faster cortical bone loss, but not with fracture risk in older men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis in men is characterized by low areal bone mineral density (aBMD) measured by DXA and poor bone microarchitecture [1]. Low aBMD is associated with high fracture risk [2, 3]; however, it poorly identifies men at high fracture risk [3]. Thus, it is necessary to explore other indices of bone fragility in men.
C-reactive protein (CRP) is an acute phase protein and inflammation marker [4]. Its synthesis is induced by proinflammatory cytokines stimulating bone resorption (interleukin-6, interleukin-1β, tumor necrosis factor α). Blood CRP levels may reflect their effect on bone [5]. Chronic inflammatory diseases are associated with high levels of these cytokines, low aBMD, rapid bone loss, and high fracture risk [6].
Low-grade inflammation may also lead to the development of osteoporosis [7]. However, in this condition, CRP level must be assayed by the high sensitivity CRP (hsCRP) assay [8]. Higher hsCRP levels were associated with higher risk of nontraumatic vertebral and hip fracture in men from the Bruneck study, higher risk of non-vertebral fracture in men from the Tromsø cohort, and with higher risk of clinical vertebral fracture in the MrOS Sweden cohort [9,10,11]. By contrast, hsCRP did not predict fractures in the MrOS cohort (hip, clinical vertebral, non-spine) or in the Cardiovascular Health Study (hip, pelvis, humerus, distal forearm) [12, 13]. However, high hsCRP levels are associated with higher mortality [14]. Thus, the analysis of the fracture risk could be biased by over-mortality of subjects with high hsCRP level.
Moreover, the morphological basis underlying possible association between CRP and fracture is not clear. Data on the link between CRP and aBMD are inconsistent [15, 16]. In men, high hsCRP levels were associated with low aBMD in some [11, 17], but not other cohorts [13, 16, 18]. Bone microarchitecture contributes to the fracture prediction, but the link between hsCRP and bone microarchitecture was weak and limited to trabecular bone microarchitecture in elderly men [18]. High hsCRP was associated with rapid bone loss in inflammatory diseases [19], but data were inconsistent in general population [20, 21]. However, they were obtained in small groups and during short follow-up periods. This link is important because accelerated bone loss is a risk factor for fracture independent of aBMD in men and women [22].
Therefore, our objective is to study the relationship of the hsCRP levels with the subsequent bone loss and with microarchitecture deterioration at the level of radius and tibia, as well as with the prospectively assessed fracture risk in older men followed prospectively for 8 years.
Subjects and methods
Cohort
The STRAMBO study is a single-center, prospective study, focused on fracture prediction by bone microarchitecture measures in men [18]. It was approved by the local ethics committee and performed in agreement with the Helsinki statement (1975, 1983) as collaboration between INSERM (National Institute of Health and Medical Research) and Mutuelle des Travailleurs de la Région Lyonnaise (MTRL). Invitations were sent to a randomly selected sample of clients of MTRL living in Greater Lyon. Between 2006 and 2008, we recruited 1169 men aged 20 to 87 years. Men who were able to give their informed consent, to answer questions, and to participate in diagnostic tests were included. This analysis includes 823 men aged ≥ 60, who had hsCRP measurements at baseline and were followed prospectively for up to 8 years.
High-sensitivity C-reactive protein (hsCRP)
Non-fasting blood were collected at 1:00 p.m. and stored at − 80 °C. Serum hsCRP was measured by immunoturbidimetric latex CRP assay (Roche Diagnostics, Mannheim, Germany). Detection limit was 0.15 mg/L [18]. Intra-assay and inter-assay coefficients of variation (CV) were < 10%. The median in 115 men aged 20–35 years was 0.75 mg/L (interquartile range: 0.47; 1.58) [18].
Dual energy X-ray absorptiometry (DXA)
Areal BMD (aBMD) was measured at baseline and then after 4 and 8 years, at lumbar spine, total hip, whole body, and non-dominant distal radius, using a Hologic Discovery A (Hologic, Bedford, MA). Its stability was assessed by the spine phantom measured daily (CV = 0.35%). The in vivo CV was 1.1–1.2%. Body composition was assessed at baseline [23]. Relative appendicular lean muscle mass index (RALM) was calculated as the sum of lean mass of four limbs divided by (body height)2.
High-resolution peripheral quantitative computed tomography (HRpQCT)
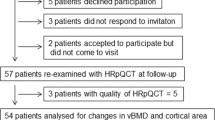
Bone microarchitecture was assessed at the distal non-dominant radius and at distal right tibia using HR-pQCT (XtremeCT, Scanco Medical, Brüttisellin, Switzerland) with a isotropic voxel of 82 μm. A scout view was used to define the reference line at the endplates of radius and tibia. A 3D stack of 110 slices was acquired, starting at 9.5 mm and 22.5 mm from the reference line for radius and tibia. Total volumetric bone density (Tt.vBMD) is the average vBMD in the entire volume of interest (VOI). VOI is separated into trabecular and cortical compartments by a threshold-based algorithm. Cortical area (Ct.Ar) is the average cross-sectional area (CSA) of cortical bone in all slices. Cortical thickness (Ct.Thd) is the mean cortical volume divided by the outer bone surface [24]. Cortical vBMD (Ct.vBMD) is the mean density. Trabecular area (Tb.Ar) is the mean CSA of the trabecular cavity in all slices. Trabecular vBMD (Tb.vBMD) is the mean density. Trabeculae were identified by the mid-axis transformation. Derived trabecular separation (Tb.Spd) and thickness (Tb.Thd) were calculated using the derived trabecular bone volume fraction (Tb.BV/TVd). Intra-individual distribution of trabeculae (Tb.1/N.SDd) is the standard deviation of distances between the mid-axes and reflects the trabecular network heterogeneity. Quality control was performed daily using a phantom containing hydroxyapatite rods. CV for phantom densities was 0.05–0.9% (short term) and 0.5–1.7% (long term). CVs for reproducibility of microarchitectural variables in vivo were 0.7–4.5% [21]. Scans were obtained at baseline and then after 4 and 8 years. Scans were graded for motion artefacts from a scale of 1 (no motion) to 5 (sever streaking artefacts) [25]. Scans with a motion score of ≥ 4 were excluded. The motion scores of 1–3 were considered good quality. Scans overlapping < 85% with scan(s) of same participant was also excluded.
Finite element analysis
Micro finite element (µFE) analysis was performed on the unregistered segmented HR-pQCT images to determine reaction force and estimated failure load of the whole bone. Linear models were generated by the voxel-by-voxel approach, with a Poisson’s ratio of 0.3, and a homogeneous Young’s modulus of 6829 GPa was assigned as bone tissue properties [26]. The model boundary conditions were an axial compression with 1% compressive strain, and resultant reaction force of the bone was measured. Failure load was estimated using a yield criterion of 2% critical volume and 0.7% critical strain [27]. The µFE models were solved using a conjugate gradient approach with a convergence criterion of 1 × 10–6 (FAIM v8.0, Numerics88 Solutions Ltd., Canada) on the University of Calgary’s high-performance computing cluster.
Incident fractures
Information on incident fractures was collected as described previously [28]. We retained low-trauma non-spine fractures (fall from a standing position or less) reported during the follow-up visit or in the yearly questionnaires and confirmed by health professional (medical report, X-ray). Lateral single-energy scans of the spine (Th4 to L4) were obtained in the dorsal decubitus position using a DXA device equipped with rotating C-arm. Scans were performed in all men present at each visit (baseline, 4 and 8 years). An incident spine fracture was diagnosed based on visual analysis (endplate fracture) and/or a decrease in any of the vertebral heights by > 15% versus the previous scan [28]. The vertebrae not correctly visible were considered non-fractured.
Covariates
Men replied to a reviewer-assisted epidemiological questionnaire. Smoking was assessed as a current smoker vs. non-smoker. Alcohol intake was calculated as the average amount of alcohol consumed weekly. Current leisure physical activity comprised the time spent walking or sport activity. Self-reported occupational physical activity was classified as low, medium, high, or very high. Comorbidities (ischemic heart disease, hypertension, diabetes mellitus, stroke, Parkinson’s disease, chronic obstructive pulmonary disease, rheumatoid arthritis, cancer) were self-reported (yes/no) and not further ascertained. Weight and height were measured in light clothes without shoes. Grip strength was measured 3 times at the dominant hand by a hand dynamometer (Martin Vigorimeter, Germany). Clinical tests were performed and the score of lower limb physical function was calculated as previously described.
Mortality
Data on the date of death was obtained from proxies or physician indicated by the participant at the moment of the recruitment.
Biochemical measurements
Testosterone, 17β-estradiol (17β-E2), and sex hormone-binding globulin (SHBG) were measured as previously described [23]. Calculated free testosterone (cFT) and bioavailable 17β-E2 (bio-17β-E2) were calculated [23]. 25-Hydroxycholecalciferol (25OHD) and parathyroid hormone (PTH) were measured as previously described [23]. Glomerular filtration rate (GFR) was estimated with the Chronic Kidney Disease Epidemiology Collaboration Eq. [29].
Statistical analysis
The analyses were performed using R-3.6.3 software (R Foundation for Statistical Computing, Austria; https://www.r-project.org). Correlations were assessed using Pearson’s correlation coefficient. Comparisons were performed by analysis of covariance (ANCOVA) for continuous variable without and with age adjustment. Chi-square test or Fisher’s exact test was used for class variables. The evolution of bone microarchitecture was explored using linear mixed effect models. Bivariate analysis explored the association between independent variables and each bone index with a simple linear regression and α risk of 10%. Selection of the variables was based on previously published data, biological plausibility, and the analysis of the link between bone microarchitectural variables and potential confounders. Model assumptions were checked by histograms and quantile–quantile plots of residuals. Quality of statistical model for a given set of variables was assessed with the coefficient of determination. Conditions for validity of fixed effect models have been verified graphically. Random coefficient models were added to characterize individual trajectories to allow individual prediction. Percentage changes were assessed using log-transformed variables. All final models were adjusted for age, BMI, bio-17β-E2, PTH, and GFR. In addition, the models for distal radius (DXA, HR-pQCT) were adjusted for grip strength and those for distal tibia, hip, lumbar spine, and whole body for the score of lower limb physical function. Interactions between the variables were checked. The analyses in various classes identified post hoc the level of 1 mg/L as the most discriminating threshold. Fracture-free survival related to HR-pQCT indices was analyzed by the Cox model after checking the assumption of proportional hazards using the Schoenfeld residues. Follow-up time was censored at the first fracture, death, last news, or 8 years after baseline, whichever came first. The link between hsCRP and fracture risk was assessed by a multivariable model adjusted for age, BMI, prior falls and fractures, and femoral neck aBMD. As hsCRP may be associated with increased mortality, men with higher hsCRP may develop fewer fractures because of higher competing risk of mortality. The Fine and Gray model was integrated into multivariable models to calculate HR (95% CI), allowing for competing mortality risks [30].
Results
Associations between hsCRP and other variables at baseline
The median hsCRP was 1.67 mg/L (interquartile range: 0.87; 3.28). 240 men (29%) had hsCRP ≤ 1 mg/L, 354 (43%) had hsCRP 1–3 mg/L, 100 (12%) had hsCRP 3–5 mg/L, and 129 (16%) men had hsCRP > 5 mg/L. The hsCRP concentrations correlated positively with age, weight, and BMI, but negatively with height (Table 1). After adjustment for age and weight, higher hsCRP correlated with less time spent outdoors, lower grip strength, and lower RALM. Higher hsCRP correlated with lower testosterone (total, cFT) and higher total and bio-17β-E2 levels. These correlations persisted after adjustment for age and weight. Higher hsCRP correlated with higher PTH and lower GFR; however, both associations became non-significant after adjusting for age and weight.
After adjustment for age and weight, ever smokers (current, former) had higher hsCRP levels vs. the never-smokers (Table 2). Higher occupational physical activity and prior fractures were associated with higher hsCRP. Men who self-reported prior stroke, Parkinson’s disease, diabetes mellitus treated with oral medications, COPD, or cancer had higher hsCRP concentrations. All the differences remained significant after adjustment for age and weight.
Associations between baseline hsCRP and bone loss assessed by DXA
Among 823 men who had the hsCRP assay, 820, 646, and 492 had good quality DXA scans at baseline, 4, and 8 years, respectively, for least one skeletal site. The causes of attrition were death (61 and 168), poor health status (32 and 126), relocation (3 and 7), second hip prosthesis (4 and 3), or poor quality of the scans. Men who were lost to follow-up before the last visit were older (76.5 versus 70.2 years, p < 0.001) and had higher hsCRP levels (median: 2.10 versus 1.44 mg/L, p < 0.001, after adjustment for age: p = 0.005).
Higher hsCRP concentrations were associated with more rapid increase in aBMD at lumbar spine and whole body (Table 3). The increase in aBMD was faster in men with hsCRP > 1 mg/L versus men who had lower hsCRP levels. The associations between hsCRP concentrations and bone loss at the hip and distal radius were not significant regardless of the statistical model.
Association between hsCRP and changes in bone microarchitecture at distal radius
Among 823 men who had the hsCRP assay, 789 (96%), 640 (81%), and 446 (57%) had good quality HR-pQCT scans at baseline, 4, and 8 years, respectively, for least one skeletal site. After adjustment for confounders, higher hsCRP levels were associated with faster decrease in Ct.Ar and Ct.Thd (absolute values) and more rapid increase in Tb.Ar (Table 4). In men with hsCRP > 1 mg/L, Ct.Ar, Ct.Thd, and Tt.vBMD (absolute values) decreased and Tb.Ar increased faster vs. men with hsCRP ≤ 1 mg/L. Serum hsCRP did not correlate with changes in trabecular measures and in the µFEA estimates of bone strength.
Association between hsCRP and changes in bone microarchitecture at distal tibia
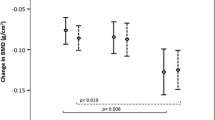
After adjustment for confounders, higher hsCRP levels were associated with faster decrease in Ct.Ar, Ct.Thd, and Ct.vBMD as well as faster increase in Tb.Ar (Table 5). In men with hsCRP > 1 mg/L, Ct.Ar, Ct.Thd, Ct.vBMD, and Tt.vBMD decreased and Tb.Ar increased more rapidly versus men with hsCRP ≤ 1 mg/L (Fig. 1). Higher hsCRP levels were associated with a faster decrease in failure load and with a non-significant trend to faster decline in reaction force. By contrast, hsCRP levels did not correlate with changes in trabecular indices.
Comparison of the bone microarchitecture measures at the distal tibia in men with hsCRP concentration > 1 mg/L vs. < 1 mg/L: Tt.vBMD, total volumetric bone mineral density (vBMD); Ct.Ar, cortical area; Ct.Th, cortical thickness; Ct.vBMD, cortical vBMD; Tb.Ar, trabecular area; failure load. The model adjusted for age, BMI, bio-17β-estradiol, parathyroid hormone, glomerular filtration rate, and the score of lower limb physical function
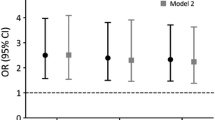
hsCRP and fracture risk
During the follow-up, 102 men had at least one incident fracture (spine fractures in 47 men, non-spine fractures in 62 men). After adjustment for the confounders, higher hsCRP levels were not associated with the risk of fracture (Table 6). After adjustment for age, BMI, and comorbidities, higher hsCRP was associated with higher risk of death (HR = 1.21 per SD, 95% CI: 1.05–1.40, p < 0.01). However, the association between hsCRP and fracture risk did not change after adjustment for competing risk of mortality. The results were similar for other cut-offs of the hsCRP concentrations. The results were similar for spine and non-spine fractures.
Discussion
In a cohort of older men followed prospectively for 8 years, higher hsCRP levels were associated with more rapid endocortical expansion and cortical thinning. The decrease in bone strength estimated by µFEA was observed at the distal tibia, a load-bearing site. High hsCRP levels were not associated with the bone loss assessed by DXA or with the fracture risk.
In our cohort, hsCRP level correlated positively with age and BMI. After adjustment for age, high hsCRP level was associated with smoking, low testosterone, and lower grip strength. Men with poor health (morbidities, treatments) had higher hsCRP levels. Our data are consistent with the concept of “inflammaging,” ageing-related chronic subclinical inflammation characterized by high secretion of inflammatory cytokines and high activity of T lymphocytes [7, 13]. The inflammatory cytokines stimulate bone resorption and may contribute to the bone loss. Higher hsCRP levels may reflect activated inflammatory status and higher levels of proinflammatory cytokines and of derivatives of reactive oxygen metabolites [31, 32].
Data on the association between hsCRP levels and aBMD loss are discordant, but mostly non-significant [16, 20, 21, 33]. Elderly women with persistently elevated hsCRP concentration had faster aBMD loss at the hip [20]. In late postmenopausal women, greater increase in hsCRP level was associated with more rapid bone loss [33]. In our cohort, hsCRP was not associated with the bone loss at the hip or distal radius. By contrast, higher hsCRP was associated with greater aBMD gain at the lumbar spine and whole body. This increase is not straightforward. However, higher hsCRP level may be associated with greater weight gain or development of osteoarthritis which result in bone gain [34, 35].
We have previously shown that in elderly men, higher hsCRP concentration was associated with poor trabecular bone status (lower Tb.N, higher TB.1/N.SDd) at distal radius [18]. Thus, high hsCRP levels may be associated with higher bone resorption which is not matched by a similar increase in bone formation. Prospective data on the link between bone structural decline and inflammation are scarce. In patients with rheumatoid arthritis or ankylosing spondylitis, severe disease (assessed by hsCRP or clinical score) was associated with faster prospectively assessed bone loss [19, 36]. Potential mechanisms include stimulatory effect of inflammatory cytokines on bone resorption on the endocortical surface. Interestingly, this endocortical bone loss may be partly offset by periosteal apposition as suggested by higher outer perimeter of bones in patients with rheumatoid arthritis [37]. Moreover, sirtuin 1 (SIRT1), NAD + -dependent deacetylase, may inhibit osteoclastogenesis and induce osteoblast differentiation [38]. Inflammation is associated with low SIRT1 level which may contribute to the progressive bone loss [39]. Proinflammatory cytokines disrupt osteocyte function and increase the secretion of RANKL (stimulating bone resorption) and of sclerostin (inhibiting bone formation) [40]. These mechanisms of the inflammation-related bone decline are consistent with our findings.
In our study, high hsCRP was not associated with fracture risk after adjustment for confounders including aBMD, prior falls, and fractures. Previously, high hsCRP levels were not associated with higher fracture risk in older men (and in the mixed cohorts) or this association was weak and limited to some skeletal sites (e.g., spine) [10,11,12,13, 16, 41, 42]. By contrast, higher hsCRP levels were associated with higher fracture risk in the models poorly controlled for confounders such as aBMD or prior falls [9, 43]. Higher hsCRP level was associated with higher risk of non-vertebral fracture in women from the Tromsø study, higher risk of nontrauma fracture in women from the Bruneck study, and with the higher risk of limb or vertebral fracture in elderly women from the Muramatsu study [9, 11, 44]. By contrast, hsCRP levels were not associated with the risk of fracture (major osteoporotic, hip) in elderly women from the OPRA study [20]. However, women have lower aBMD and their bone may be more sensitive to the inflammation-induced bone loss, because estrogen deficit activates the Th17 proinflammatory cytokines. Moreover, fracture risk was higher in subjects with long-term (or recurrent) active inflammation and higher hsCRP levels, e.g., in patients with rheumatoid arthritis [6]. Fracture risk was also increased in individuals who had elevated levels of several inflammatory markers simultaneously [13]. These data show that active inflammatory status can be associated with increased fracture risk. By contrast, in older men aged 60–87 years from cohort, hsCRP levels were low (median: 1.67 mg/L) and only 16% of men has hsCRP > 5 mg/L. Thus, we could be unable to detect a mild increase in fracture risk related to the low-grade ageing-related inflammatory syndrome.
Our study has limitations. It is a single-center cohort composed of home-dwelling Caucasian men. Our results may not be extrapolated to women or other ethnic groups. We had one hsCRP value per man and we could not differentiate between chronic stable and acute inflammation. However, men refused to come when they had an acute disease; thus, few high hsCRP levels are supposed to be associated with acute inflammation. Blood was collected in the non-fasting status in early afternoon; however, there is no diurnal variation of serum hsCRP in humans [45]. The attrition rate was high. Men who were lost to follow-up were older and had higher hsCRP levels (also when adjusted for age). Men who were lost to follow-up could have faster bone loss and higher fracture risk. It shows that we underestimate the rate of bone loss, fracture incidence, and also the strength of the links between variables. Ct.Thd and Tb.Thd were calculated, not measured. The assessment of cortical bone may be erroneous in the oldest men with thin cortex. Bone microarchitecture assessment may be inaccurate because of the partial volume effect. HR-pQCT cannot detect age-related microdamage, posttranslational protein modification, or mineral imperfection. µFEA assesses bone compression, not other deformations [46]. Endocortical trabecularization leads to inclusion of remnants of internal cortical layer into the trabecular bone and results in underestimation of trabecular bone loss and overestimation of cortical bone loss. Dichotomization cortical/trabecular is to be interpreted cautiously. Microradiographic analyses performed in the bones collected post mortem in elderly women show no clear-cut endocortical edge, but gradual transition between the compartments [47, 48]. Perforations of subendocortical cortical pores lead to overestimation of endocortical expansion as well as to underestimation of the rise in cortical porosity and of the decrease in Ct.vBMD [47, 48]. We checked self-reported non-spine fractures, but false negatives are possible. Incident spine fractures were assessed only in men who returned for follow-up visits and had DXA. Medical records of the participants were not scrutinized. It may underestimate the number of incident spine fractures, especially because older and sicker men, who did not return, could have higher spine fracture incidence. Prior non-spine fractures, falls, and morbidities were self-reported and not checked. In an observational study, residual confounding is possible.
Overall, in a cohort of older men followed prospectively for 8 years, high hsCRP was associated with greater endocortical expansion at distal radius and distal tibia. Higher hsCRP level was also associated with more rapid decrease in Tt.vBMD, Ct.vBMD, and failure load at distal tibia and with a greater increase in aBMD at the lumbar spine and whole body. After adjustment for potential confounders including the competing risk of death, higher hsCRP was not associated with the fracture risk. Thus, ageing-related low-grade inflammatory syndrome may results in slightly greater bone loss, probably mainly at the endocortical surface. However, bone loss is not generalized and its impact on bone strength is minor. Thus, in our cohort, higher hsCRP level does not seem to be a major predictor of bone decline and fragility in older men. However, given the loss to follow-up of the oldest men with the highest hsCRP concentrations, we could have underestimated the existing links. Thus, further studies are necessary to explore this topic.
References
Martel D, Monga A, Chang G (2022) Osteoporosis imaging. Radiol Clin North Am 60:537–545. https://doi.org/10.1016/j.rcl.2022.02.003
Cummings SR, Cawthon PM et al (2006) BMD and risk of hip and nonvertebral fractures in older men: a prospective study and comparison with older women. J Bone Miner Res 21:1550–6. https://doi.org/10.1359/jbmr.060708
Szulc P, Munoz F, Duboeuf F, Marchand F, Delmas PD (2005) Bone mineral density predicts osteoporotic fractures in elderly men: the MINOS study. Osteoporos Int 16:1184–1192. https://doi.org/10.1007/s00198-005-1970-9
Pathak A, Agrawal A (2019) Evolution of C-reactive protein. Front Immunol 10:943. https://doi.org/10.3389/fimmu.2019.00943
Chedid VG, Kane SV (2020) Bone health in patients with inflammatory bowel diseases. J Clin Densitom 23:182–189. https://doi.org/10.1016/j.jocd.2019.07.009
Jin S, Hsieh E, Peng L, Yu C, Wang Y, Wu C, Wang Q, Li M, Zeng X (2018) Incidence of fractures among patients with rheumatoid arthritis: a systematic review and meta-analysis. Osteoporos Int 29:1263–1275. https://doi.org/10.1007/s00198-018-4473-1
Pietschmann P, Mechtcheriakova D, Meshcheryakova A, Föger-Samwald U, Ellinger I (2016) Immunology of osteoporosis: a mini-review. Gerontology 62:128–137. https://doi.org/10.1159/000431091
Eda S, Kaufmann J, Roos W, Pohl S (1998) Development of a new microparticle-enhanced turbidimetric assay for C-reactive protein with superior features in analytical sensitivity and dynamic range. J Clin Lab Anal 12:137–144. https://doi.org/10.1002/(sici)1098-2825(1998)12:3%3c137::aid-jcla2%3e3.0.co;2-6
Schett G, Kiechl S (2006) Weger S et al High-sensitivity C-reactive protein and risk of nontraumatic fractures in the Bruneck study. Arch Intern Med 166:2495–501
Eriksson AL, Movérare-Skrtic S, Ljunggren O, Karlsson M, Mellström D, Ohlsson C (2014) High-sensitivity CRP is an independent risk factor for all fractures and vertebral fractures in elderly men: the MrOS Sweden study. J Bone Miner Res 29:418–423. https://doi.org/10.1002/jbmr.2037
Dahl K, Ahmed LA, Joakimsn RM, Jorgensen L, Eggen AE, Eriksen EF, ABjornerem (2015) High-sensitivity C-reactive protein is an independent risk factor for non-vertebral fractures in women and men: the Tromsø study. Bone 72:65–70
Stojanović D, Bůžková P, Mukamal KJ et al (2018) Soluble inflammatory markers and risk of incident fractures in older adults: the cardiovascular health study. J Bone Miner Res 33:221–228. https://doi.org/10.1002/jbmr.3301
Cauley JA et al (2016) Inflammatory markers and the risk of hip and vertebral fractures in men: the osteoporotic fractures in men (MrOS). J Bone Miner Res 31:2129–2138. https://doi.org/10.1002/jbmr.2905
Emerging Risk Factors Collaboration, Kaptoge S, Di Angelantonio E, Lowe G, Pepys MB, Thompson SG, Collins R, Danesh J (2010) C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet 375:132–40. https://doi.org/10.1016/S0140-6736(09)61717-7
Koh JM, Khang YH, Jung CH, Bae S, Kim DJ, Chung YE, Kim GS (2005) Higher circulating hsCRP levels are associated with lower bone mineral density in healthy pre- and postmenopausal women: evidence for a link between systemic inflammation and osteoporosis. Osteoporos Int 16:1263–71. https://doi.org/10.1007/s00198-005-1840-5
den Uyl D, van Schoor NM, Bravenboer N, Lips P, Lems WF (2015) Low grade inflammation is associated with lower velocity of sound and broadband ultrasound attenuation in older men, but not with bone loss or fracture risk in a longitudinal aging study. Bone 81:270–276. https://doi.org/10.1016/j.bone.2015.07.017
de Pablo P, Cooper MS, Buckley CD (2012) Association between bone mineral density and C-reactive protein in a large population-based sample. Arthritis Rheum 64:2624–2631. https://doi.org/10.1002/art.34474
Rolland T, Boutroy S, Vilayphiou N, Blaizot S, Chapurlat R, Szulc P (2012) Poor trabecular microarchitecture at the distal radius in older men with increased concentration of high-sensitivity C-reactive protein—the Strambo study. Calcif Tissue Int 90:496–506. https://doi.org/10.1007/s00223-012-9598-1
Pye SR, Adams JE, Ward KA, Bunn DK, Symmons DPM, O’Neill TW (2010) Disease activity and severity in early inflammatory arthritis predict hand cortical bone loss. Rheumatology (Oxford) 49:1943–1948. https://doi.org/10.1093/rheumatology/keq181
Berglundh S, Malmgren L, Luthman H, McGuigan F, Åkesson K (2015) C-reactive protein, bone loss, fracture, and mortality in elderly women: a longitudinal study in the OPRA cohort. Osteoporos Int 26:727–735. https://doi.org/10.1007/s00198-014-2951-7
Ding C, Parameswaran V, Udayan R, Burgess J, Jones G (2008) Circulating levels of inflammatory markers predict change in bone mineral density and resorption in older adults: a longitudinal study. J Clin Endocrinol Metab 93:1952–1958. https://doi.org/10.1210/jc.2007-2325
Cawthon PM, Ewing SK, Mackey DC et al (2012) Change in hip bone mineral density and risk of subsequent fractures in older men. J Bone Miner Res. 27:2179–88. https://doi.org/10.1002/jbmr.1671
Szulc P, Schoppet M, Goettsch C, Rauner M, Dschietzig T, Chapurlat R, Hofbauer LC (2012) Endocrine and clinical correlates of myostatin serum concentration in men – the STRAMBO study. J Clin Endocrinol Metab 97:3700–3708. https://doi.org/10.1210/jc.2012-1273
Whittier DE, Boyd SK, Burghardt AJ et al (2020) Guidelines for the assessment of bone density and microarchitecture in vivo using high-resolution peripheral quantitative computed tomography. Osteoporos Int 31:1607–1627. https://doi.org/10.1007/s00198-020-05438-5
Pauchard Y, Liphardt A-M, Macdonald HM, Hanley DA, Boyd SK (2012) Quality control for bone quality parameters affected by subject motion in high-resolution peripheral quantitative computed tomography. Bone 50:1304–1310. https://doi.org/10.1016/j.bone.2012.03.003
MacNeil JA, Boyd SK (2008) Bone strength at the distal radius can be estimated from high-resolution peripheral quantitative computed tomography and the finite element method. Bone 42:1203–1213. https://doi.org/10.1016/j.bone.2008.01.017
Pistoia W, Van Rietbergen B, Lochmüller EM, Lill CA, Eckstein F, Rüegsegger P (2004) Image-based micro-finite-element modeling for improved distal radius strength diagnosis: Moving from bench to bedside. J Clin Densitom 7:153–160. https://doi.org/10.1385/jcd:7:2:153
Szulc P, Boutroy S, Chapurlat R (2018) Prediction of fractures in men using bone microarchitectural parameters assessed by high-resolution peripheral quantitative computed tomography - the prospective STRAMBO study. J Bone Miner Res 33:1470–1479. https://doi.org/10.1002/jbmr.3451
Levey AS, Stevens LA, Schmid CH, Zhang Y, Castro AF, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–12. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Kamezaki F, Yamashita K, Kubara T, Suzuki Y, Tanaka S, Rkouzuma R, Okazaki M, Tasaki H, Otuji Y (2008) Derivatives of reactive oxygen metabolites correlates with high-sensitivity C-reactive protein. J Atheroscler Thromb 15:206–212. https://doi.org/10.5551/jat.e538
Schaap LA, Pluijm SM, Deeg DJ, Harris TB, Kritchevsky SB, Newman AB, Colbert LH, Pahor M, Rubin SM, Tylavsky FA, Visser M (2009) Higher inflammatory marker levels in older persons: associations with 5-year change in muscle mass and muscle strength. J Gerontol A Biol Sci Med Sci 64:1183–1189. https://doi.org/10.1093/gerona/glp097
Greendale GA, Jackson NJ, Han W, Huang M, Cauley JA, Karvonen-Gutierrez C, Karlamangla AS (2021) Increase in C-reactive protein predicts increase in rate of bone mineral density loss: the study of women’s health across the nation. JBMR Plus 5:e10480. https://doi.org/10.1002/jbm4.10480
Barzilay JI, Forsberg C, Heckbert SR, Cushman M, Newman AB (2006) The association of markers of inflammation with weight change in older adults: the cardiovascular health study. Int J Obes (Lond) 30:1362–1367. https://doi.org/10.1038/sj.ijo.0803306
SaberiHosnijeh F, Siebuhr AS, Uitterlinden AG, Oei EH, Hofman A, Karsdal MA, Bierma-Zeinstra SM, Bay-Jensen AC, van Meurs JB (2016) Association between biomarkers of tissue inflammation and progression of osteoarthritis: evidence from the Rotterdam study cohort. Arthritis Res Ther 18:81. https://doi.org/10.1186/s13075-016-0976-3
Deminger A, Klingberg E, Lorentzon M, Hedberg M, Carlsten H, Jacobsson LTH, Forsblad-d’Elia H (2022) Factors associated with changes in volumetric bone mineral density and cortical area in men with ankylosing spondylitis: a 5-year prospective study using HRpQCT. Osteoporos Int 33:205–216. https://doi.org/10.1007/s00198-021-06049-4
Kocijan R, Finzel S, Englbrecht M, Engelke K, Rech J, Schett G (2014) Decreased quantity and quality of the periarticular and nonperiarticular bone in patients with rheumatoid arthritis: a cross-sectional HR-pQCT study. J Bone Miner Res 29:1005–1014. https://doi.org/10.1002/jbmr.2109
Chen Y, Zhou F, Liu H, Li J, Che H, Shen J, Luo E (2021) SIRT1, a promising regulator of bone homeostasis. Life Sci 269:119041. https://doi.org/10.1016/j.lfs.2021.119041
Yang Y, Liu Y, Wang Y, Chao Y, Zhang J, Jia Y, Tie J, Hu D (2022) Regulation of SIRT1 and its roles in inflammation. Front Immunol 13:831168. https://doi.org/10.3389/fimmu.2022.831168
Zhou M, Shuyi Li S, Pathak JL (2019) Pro-inflammatory cytokines and osteocytes. Curr Osteoporos Rep 17:97–104. https://doi.org/10.1007/s11914-019-00507-z
Apalset EM, Gjesdal CG, Ueland PM, Øyen J, Meyer K, Midttun Ø, Eide GE, Tell GS (2014) Interferon gamma (IFN-γ)-mediated inflammation and the kynurenine pathway in relation to risk of hip fractures: the Hordaland health study. Osteoporos Int 25:2067–2075
Oei L, Campos-Obando N, Dehghan A, Oei EH, Stolk L, van Meurs JB, Hofman A, Uitterlinden AG, Franco OH, Zillikens MC, Rivadeneira F (2014) Dissecting the relationship between high-sensitivity serum C-reactive protein and increased fracture risk: the Rotterdam study. Osteoporos Int 25:1247–1254. https://doi.org/10.1007/s00198-013-2578-0
Mun H, Liu B, Pham THA, Wu Q (2021) C-reactive protein and fracture risk: an updated systematic review and meta-analysis of cohort studies through the use of both frequentist and Bayesian approaches. Osteoporos Int 32:425–435. https://doi.org/10.1007/s00198-020-05623-6
Nakamura K, Saito T, Kobayashi R, Oshiki R, Oyama M, Nishiwaki T, Nashimoto M, Tsuchiya Y (2011) C-reactive protein predicts incident fracture in community-dwelling elderly Japanese women: the Muramatsu study. Osteoporos Int 22:2145–2150. https://doi.org/10.1007/s00198-010-1425-9
Meier-Ewert HK, Ridker PM, Rifai N, Price N, Dinges DF, Mullington JM (2001) Absence of diurnal variation of C-reactive protein concentrations in healthy human subjects. Clin Chem 47:426–30
Walle M, Marques FC, Ohs N, Blauth M, Müller R, Collins CJ (2021) Bone mechanoregulation allows subject-specific load estimation based on time-lapsed micro-CT and HR-pQCT in vivo. Front Bioeng Biotechnol 9:677985. https://doi.org/10.3389/fbioe.2021.677985
Zebaze R, Ghasem-Zadeh A, Bohte A, Iuliano-Burns A, Mirams M, Prime RI, Mackie EJ, Seeman E (2010) Intracortical remodelling and porosity in the distal radius and post-mortem femurs of women: a cross-sectional study. Lancet 375:1729–1736. https://doi.org/10.1016/S0140-6736(10)60320-0
Zebaze R, Seeman E (2015) Cortical bone: a challenging geography. J Bone Miner Res 30:24–29. https://doi.org/10.1002/jbmr.2419
Funding
Grants are from the Roche pharmaceutical company, Basel, Switzerland, Agence Nationale de la Recherche (ANR-07-PHYSIO-023, ANR-10-BLAN-1137), Abondement ANVAR (E1482.042), and Hospices Civils de Lyon (50564).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
NonE.
Disclaimer
The supporting sponsors played no role in the study design collection, analysis, or interpretation of data.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Girard, D., Wagner, P.P., Whittier, D.E. et al. C-reactive protein predicts endocortical expansion but not fracture in older men: the prospective STRAMBO study. Osteoporos Int 34, 539–550 (2023). https://doi.org/10.1007/s00198-022-06652-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06652-z