Abstract
Summary
Low serum alkaline phosphatase (ALP) was found in 9% of patients attending an osteoporosis clinic, 0.6% of hospital patients, and 2/22 with an atypical femoral fracture. Hypophosphatasia was diagnosed in 3% of osteoporosis clinic patients with low ALP. Low ALP is a screening tool for hypophosphatasia, a condition potentially aggravated by antiresorptive therapy.
Introduction
Hypophosphatasia (HPP) is an inherited disorder associated with impaired primary mineralisation of osteoid (osteomalacia). HPP may be misdiagnosed as osteoporosis, a reduction in the volume of normally mineralized bone. Both illnesses may result in fragility fractures, although stress and atypical fractures are more common in HPP. Antiresorptive therapy, first-line treatment for osteoporosis, is relatively contraindicated in HPP. Misdiagnosis and mistreatment can be avoided by recognising a low serum alkaline phosphatase (ALP). Our aim was to determine the prevalence of a low ALP (< 30 IU/L) in patients attending an osteoporosis clinic, in a hospital-wide setting, and in a group of patients with atypical femoral fractures (AFF).
Methods
This was a retrospective study of patients attending an osteoporosis clinic at a tertiary hospital during 8 years (2012–2020). Patients were categorised into those with a transiently low ALP, those with low ALP on ≥ 2 occasions but not the majority of measurements, and those with a persistently low ALP. ALP levels were also assessed in hospital-wide records and a group of patients with AFF.
Results
Of 1839 patients attending an osteoporosis clinic, 168 (9%) had ≥ 1 low ALP, 50 (2.7%) had low ALP for ≥ 2 months, and seven (0.4%) had persistently low ALP levels. HPP was diagnosed in five patients, four of whom had persistently low ALP levels. The prevalence of HPP was 0.3% in the osteoporosis clinic and 3% in patients with ≥ 1 low ALP. Low ALP occurred in 0.6% of all hospital patients and 2/22 with AFF.
Conclusion
Persistently low ALP in osteoporosis clinic attendees is easy to identify and signals the possibility of hypophosphatasia, a condition that may be mistaken for osteoporosis and incorrectly treated with antiresorptive therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a public health issue due to the significant morbidity and economic burden resulting from fragility fractures [1]. Fracture liaison services and osteoporosis clinics are committed to management of patients with bone fragility. The majority of referred patients have sustained fragility fractures or have low bone mineral density (BMD) [2]. Many diseases may account for bone fragility or reduced BMD including primary hyperparathyroidism, malabsorption, cortisol excess, mastocytosis, and others, making a diagnosis challenging [2, 3]. One rare illness causing secondary osteoporosis is hypophosphatasia (HPP) which may present with fragility, stress, or atypical fractures.
HPP is an inborn error of metabolism inherited in an autosomal dominant or recessive pattern with incomplete penetrance [4, 5]. A loss-of-function mutation within the gene ALPL (alkaline phosphatase liver/bone/kidney isoenzyme [6]) encoding tissue non-specific alkaline phosphatase (TNSALP) impairs hydrolysis of inorganic pyrophosphate, an inhibitor of mineralisation [5]. The mutation results in reduced serum ALP activity and accumulation of inorganic pyrophosphate (PPi), pyridoxal-5′-phosphate (PLP) and phosphoethanolamine [7]. Hence, TNSALP plays a role in vitamin B6 metabolism, with deficiency resulting in high vitamin B6 levels and associated neurological symptoms [7].
Diagnosis of HPP is based on clinical suspicion, laboratory testing, and DNA sequencing, although the latter is not always required. Over 400 defects in TNSALP have been identified with varying presentations relating to the degree of residual ALP activity [7, 8]. HPP can manifest at any age with varying severity [9]. Adults may suffer from stress or fragility fractures with impaired healing. Consequently, misdiagnosis as age-related osteoporosis may occur. Subsequent treatment with bisphosphonates, analogues of pyrophosphate, may exacerbate the inhibitory effect of this accumulated substrate on primary mineralisation. Atypical femoral fractures (AFF) may be the result of HPP [10] and may also be a rare adverse effect of antiresorptive therapy [11].
Finding low ALP may signal the possible diagnosis of HPP [12]. Screening patients for low ALP in an osteoporosis clinic assists in identification of HPP and avoidance of mistreatment with antiresorptive therapy which may aggravate the risk of AFF. This study was undertaken to determine the prevalence of low ALP levels in patients presenting to an osteoporosis clinic, in a whole hospital setting and in patients with AFF.
Methods
This study was performed at The Alfred Hospital, an adult tertiary institution which services a wide catchment area and a large group of lung and heart transplant recipients. Medical records of all adult patients seen in The Alfred Osteoporosis Clinic from its inception in April 2012 until April 2020 were reviewed. Pathology results from January 2008 to April 2020 were accessed and ALP levels reviewed. The electronic medical record was interrogated in all patients with at least one ALP level below 30 IU/L, the lower limit of the reference range in Australia [13].
All ALP levels for each patient were collated to assess the proportion of low levels over time as there was concern that evaluation of the median ALP level alone might misrepresent the individual’s true ALP value. Patients with at least one low ALP were categorised into three groups. Group 1 comprised those with transiently low ALP levels, defined as a low ALP during only one month out of all the months where this was measured. Group 2 comprised those with low ALP during at least two months, but the majority of their measured ALP levels were normal (> 30 IU/L in over half the months when the ALP level was assessed). Group 3 comprised those with a persistently low ALP, defined as a low ALP level in over half of the months when measured. This categorisation was used to minimise over-investigating those with transient periods of low ALP values (when multiple tests were done in short time periods) while not missing recurrent low ALP values in those with fewer pathology tests.
Medical records were reviewed to identify circumstances around low ALP levels in all patients with a low ALP. This included lung and/or cardiac transplantation involving cardiac bypass, plasma exchange, intravenous immunoglobulin, high-dose immunosuppression, surgery, sepsis, chemotherapy, haemorrhage, or bone marrow transplant (Fig. 2). Data collection included previous fragility fractures, AFFs, musculoskeletal pain, dental abnormalities, history of childhood rickets, and family history of osteoporosis. Fractures were recorded as traumatic or minimal trauma and fracture site was documented. Biochemical data assessed included renal function, 25-hydroxy vitamin D level, parathyroid hormone (PTH) level, thyroid stimulating hormone (TSH) level, procollagen type I N-terminal propeptide (PINP), and C-terminal telopeptide of type I collagen (CTx).
Patients with a persistently low ALP level were recalled to clinic for review and repeat blood tests for ALP and a PLP or vitamin B6 level. Genetic testing was subsequently performed to confirm a pathogenic mutation of the ALPL gene in relevant individuals.
The prevalence of low ALP levels across the entire hospital was compared with the prevalence in the osteoporosis clinic in which attendees are at high risk of misdiagnosis as osteoporosis and mistreatment with antiresorptive drugs.
The prevalence of low ALP levels in patients presenting with AFF was also examined in patients enrolled in the TrAFFic study from the same centre, comprising all patients with an AFF referred to the Endocrinology service from 2015 to 2020. ALP values of these patients were reviewed and analysed using the same methodology as described above.
Approval was obtained from the Human Research Ethics Board at Alfred Health prior to study initiation. This project was not funded by the hospital or external grants.
Results
Osteoporosis clinic cohort
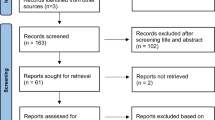
There were 1866 patients seen in the osteoporosis clinic during eight years. Twenty-seven patients were excluded as no ALP result was available. In the remaining 1839, 168 had at least one low ALP, and 118 had a low ALP on one occasion only (group 1); none have been found to have HPP. Fifty patients had at least two low ALP results but the majority of values were within the reference range (group 2) and 7 patients had persistently low ALP levels (group 3) (Fig. 1). Using a low ALP for screening identified two patients already diagnosed with HPP prior to this study. Since the commencement of this study, genetic testing has confirmed HPP in three more patients.
The demographic data of all patients with a low ALP is shown in Table 1, with the median age being 63 years and 51% being male. Of note, 95.2% had received antiresorptive therapy. Isolated low ALP levels were most often encountered in patients having lung and/or cardiac transplantation; followed by plasma exchange or intravenous immunoglobulin, surgery, sepsis, induction chemotherapy, haemorrhage and bone marrow transplantation (Fig. 2).
Low ALP levels and surrounding circumstances. a Low ALP levels at time of lung transplantation in 92 (54.8%) patients, heart transplantation in 2 (1.2%) patients, and combined heart–lung transplantation in 1 (0.6%). b Individuals with a low ALP on the day of treatment with plasma exchange, intravenous immunoglobulin, and/or or pulse intravenous methylprednisolone. c Operations included coronary artery bypass graft, left ventricular assist device insertion, total hip replacement for fractured neck of femur, laparoscopic anterior resection and endoscopic procedures. d Haemorrhage was defined as significant bleeding requiring blood transfusion
The group with persistently low ALP levels is described further in Table 2. All patients had elevated vitamin B6 levels. Bone densitometry \(T\) scores were normal in two patients, within the osteopaenic range in two (− 1.0 to − 2.5) and within the osteoporotic range in three (< − 2.5).
As shown in Table 3, fragility fractures were present in 41 of 118 (35%) patients with an isolated low ALP, 16 of 43 (37%) patients with multiple low ALP levels, and 3 of 7 (43%) with persistently low ALP levels (Table 3). In the latter group, fractures of the feet, hands, femur, wrist, and ribs were observed, not vertebral or hip fractures. Vertebral and hip fractures were present in groups 1 and 2. Two patients with persistently low ALP levels sustained an AFF, both of whom had received antiresorptive therapy prior the fracture, one with a bisphosphonate and the other with denosumab.
Hospital-wide ALP testing
In 2021, the hospital performed 175,047 ALP tests in 49,336 individuals, with 696 measurements < 30 U/L (0.4%) in 284 patients (0.6%).
TrAFFic study
Two of 22 individuals with an AFF had at least one ALP level below 30 IU/L. Both had received prolonged bisphosphonate therapy and were referred to the osteoporosis clinic for assessment after cessation of bisphosphonate therapy. One was been found to have a pathogenic ALPL mutation.
Discussion
This study reports that 9% of osteoporosis clinic attendees (168 of 1839) had ALP < 30 U/L and 4.2% (7 patients) of these had persistently low ALP levels. Five patients have been diagnosed with HPP, four in the group with persistently low ALP levels. The prevalence of HPP was 0.3% of patients in the osteoporosis clinic and 3% of patients with at least one low ALP.
The 9% prevalence of at least one low ALP in this study of osteoporosis clinic attendees is higher than that reported previously. A study in an ambulatory care endocrinology practice identified 315 of 20,000 patients (~ 1.6%) seen during one year had an ALP ≤ 40 U/L [14]. Ten patients had histories suggestive of HPP but genetic testing was not reported. An osteoporosis clinic in Edinburgh reported 16 of 3285 (0.49%) patients had an ALP level ≤ 40 U/L on at least two occasions [15]. Eight of the 16 individuals had ALPL mutations associated with HPP and six had potentially pathogenic ALPL mutations.
Hospital-wide ALP results from this study found ALP < 30 U/L in 0.4% of all tests and 0.6% of all patients who had an ALP tested in 2021, higher than reported in 0.19% of tests at a veteran centre (cut-off < 30 U/L) and 0.36% of tests in a tertiary centre in Brazil (cut-off < 40 U/L) [16, 17].
The significance of a low ALP level may not be appreciated in the clinic or hospital setting; thus, delay in diagnosis is common [12, 21, 22]. In this and other studies, patients with persistently low ALP levels form a small subset of all patients with a low ALP [23, 24].
ALPL mutations have been reported in over half of adults with low ALP levels [25,26,27]. A Danish study of an Endocrinology unit over 12 years described a 0.20% prevalence of persistently low ALP levels (51/26,121), and HPP was confirmed in 13 of the 24 who underwent genetic testing [25]. In another study, ALPL mutations were identified in 21 of 42 adults with low ALP levels [26]. Four of seven patients with persistently low ALP levels in this study have been confirmed to have HPP. One of the five patients diagnosed with HPP was classified into group 2, with multiple low ALP levels but less than half of his measured ALP < 30 U/L (the majority of his 157 ALP measurements were < 35 U/L, with a median of 34 U/L). The remaining 3 out of 7 patients with persistently low ALP levels have not undergone genetic testing; thus, there remains potential for the diagnosis of HPP to be made (Table 2).
There are many causes of a transiently low ALP level including use of antiresorptive agents, nutritional deficiencies, and acute severe illness [18,19,20]. Such causes are likely to be more common than HPP and so should be considered early in the evaluation of a low ALP. A large proportion of patients with transiently low ALP levels in this study were undergoing cardiac and/or lung transplantation. Cardiac bypass during these procedures is a recognised cause of low ALP. Low ALP in transplant recipients may also be multifactorial, as they receive high-dose glucocorticoid therapy.
Evidence for HPP is supported by finding a high urinary phosphoethanolamine level and serum PLP (main circulating form of vitamin B6), as these substrates of TNSALP accumulate in HPP [7, 25, 26]. These biomarkers differentiate HPP from other causes of a low ALP, with serum PLP being a more sensitive and specific biomarker than urinary PEA [8]. Patients with a persistently low ALP in this study were found to have an elevated vitamin B6 after withdrawal of vitamin supplementation. These supporting biomarkers may be especially useful where antiresorptive therapy has preceded the finding of a low ALP.
Distinguishing HPP from age-related bone fragility is important due to the potential for inappropriate use of antiresorptive therapy. Bisphosphonates exacerbate the impaired mineralisation seen in HPP by compromising residual TNSALP activity [8]. Of the seven patients with persistently low ALP levels, six had received antiresorptive therapy and two sustained fragility fractures after their administration. A bone biopsy may have identified failed primary mineralisation (osteomalacia) which occurs in adults with HPP in the presence or absence of antiresorptive therapy [28,29,30,31]. The group with persistently low ALP levels had a high number of atypical fractures (Table 3). There is an increased risk of subtrochanteric and diaphyseal atypical femoral fractures in adult HPP patients, as well as metatarsal fractures [32, 33]. The evaluation of low ALP levels in the TrAFFic study cohort with AFF looks only at one subset of fracture that is more common in HPP.
This study has several limitations. As this was a retrospective survey of ALP levels in clinic and hospital patients, it was not possible to perform a systematic interrogation of all possible causes of a low ALP or to detect temporal associations between antiresorptive use and low ALP levels [19, 27]. In addition, generalisability is limited by the large transplant population and high proportion of males. Moreover, while fractures were documented, any causal relationship to underlying bone fragility, HPP, or drug therapy could not be determined. In those with low ALP, the prevalence of HPP is likely to be underestimated as genetic testing has not been undertaken in all patients. Additionally, the cut-off of ALP < 30 U/L was utilised as it is the lower limit of normal at our institution and across Australia. A higher cut-off such as that used internationally and in previous studies might have identified more patients with HPP. The case for this is supported by one of the five patients with HPP who would have been considered to have persistently low ALP (group 3 rather than group 2) if the ALP cut-off was < 35 U/L. Thus, a “low” ALP, defined as a level below the lower limit of the reference range, may benefit from further clarification.
Although HPP is a rare illness, assessment of ALP is appropriate given the illness may be misdiagnosed as osteoporosis. The potential harm lies in the prescription of antiresorptive therapy. The assessment of ALP is therefore especially relevant to patients presenting with fragility or atypical femur fractures. Persistently low ALP in osteoporosis clinic attendees should signal consideration of the diagnosis of HPP. The occurrence of a serially low ALP level is uncommon, but when found, investigating for HPP has a relatively high yield, justifying serial measurement whenever a single low level is detected.
References
Harvey N, Dennison E, Cooper C (2010) Osteoporosis: impact on health and economics. Nat Rev Rheumatol 6(2):99–105. https://doi.org/10.1038/nrrheum.2009.260
Ebeling PR, Nguyen HH, Aleksova J, Vincent AJ, Wong P, Milat F (2022) Secondary osteoporosis. Endocr Rev 43(2):240–313
Stein E, Shane E (2003) Secondary osteoporosis. Endocrinol Metab Clin North Am 32(1):115–134. https://doi.org/10.1016/S0889-8529(02)00062-2
Mornet E (2007) Hypophosphatasia. Orphanet J Rare Dis 2:40. https://doi.org/10.1186/1750-1172-2-40
Whyte MP (2008) Chapter 73 - Hypophosphatasia: nature’s window on alkaline phosphatase function in humans. In: Bilezikian JP, Raisz LG, Martin TJ (eds) Principles of bone biology, 3rd edn. Academic Press, San Diego, pp 1573–1598
Swallow DM, Povey S, Parkar M, Andrews PW, Harris H, Pym B, Goodfellow P (1986) Mapping of the gene coding for the human liver/bone/kidney isozyme of alkaline phosphatase to chromosome 1. Ann Hum Genet 50(3):229–235. https://doi.org/10.1111/j.1469-1809.1986.tb01043.x
Hofmann C, Girschick HJ, Mentrup B, Graser S, Seefried L, Liese J, Jakob F (2013) Clinical aspects of hypophosphatasia: an update. Clin Rev Bone Miner Metab 11(2):60–70. https://doi.org/10.1007/s12018-013-9139-0
Whyte MP (2016) Hypophosphatasia - aetiology, nosology, pathogenesis, diagnosis and treatment. Nat Rev Endocrinol 12(4):233–246. https://doi.org/10.1038/nrendo.2016.14
Conti F, Ciullini L, Pugliese G (2017) Hypophosphatasia: clinical manifestation and burden of disease in adult patients. Clin Cases Miner Bone Metab 14(2):230 4. https://doi.org/10.11138/ccmbm/2017.14.1.230
Nguyen HH, van de Laarschot DM, Verkerk AJMH, Milat F, Zillikens MC, Ebeling PR (2018) Genetic risk factors for atypical femoral fractures (AFFs): a systematic review. JBMR Plus 2(1):1–11. https://doi.org/10.1002/jbm4.10024
Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster DW, Ebeling PR, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O’Keefe R, Papapoulos S, Howe TS, van der Meulen MC, Weinstein RS, Whyte MP (2014) Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 29(1):1–23. https://doi.org/10.1002/jbmr.1998
Schmidt T, Mussawy H, Rolvien T, Hawellek T, Hubert J, Rüther W, Amling M, Barvencik F (2017) Clinical, radiographic and biochemical characteristics of adult hypophosphatasia. Osteoporos Int 28(9):2653–2662. https://doi.org/10.1007/s00198-017-4087-z
Koerbin G, Sikaris K, Jones GRD, Flatman R, Tate JR (2018) AACB Harmonization Committee for Common Reference Intervals An update report on the harmonization of adult reference intervals in Australasia. Clin Chem Lab Med 57(1):38–41. https://doi.org/10.1515/cclm-2017-0920
Quinn HB, Busch RS, Kane MP (2021) The occurrence and burden of hypophosphatasia in an ambulatory care endocrinology practice. Endocr Pract 27(12):1189–1192. https://doi.org/10.1016/j.eprac.2021.07.005
Alonso N, Larraz-Prieto B, Berg K, Lambert Z, Redmond P, Harris SE, Deary IJ, Pugh C, Prendergast J, Ralston SH (2020) Loss-of-function mutations in the ALPL gene presenting with adult onset osteoporosis and low serum concentrations of total alkaline phosphatase. J Bone Miner Res 35(4):657–661. https://doi.org/10.1002/jbmr.3928
Lum G (1995) Significance of low serum alkaline phosphatase activity in a predominantly adult male population. Clin Chem 41(4):515–518
Vieira LHR, Peixoto KC, Flósi CL, de Farias MLF, Madeira M (2021) Active search of adult patients with persistently low serum alkaline phosphatase levels for the diagnosis of hypophosphatasia. Arch Endocrinol Metab. 65(3):289–294. https://doi.org/10.20945/2359-3997000000347
McKiernan FE, Berg RL, Fuehrer J (2014) Clinical and radiographic findings in adults with persistent hypophosphatasemia. J Bone Miner Res 29(7):1651–1660. https://doi.org/10.1002/jbmr.2178
McKiernan FE, Shrestha LK, Berg RL, Fuehrer J (2014) Acute hypophosphatasemia. Osteoporos Int 25(2):519–523. https://doi.org/10.1007/s00198-013-2447-x
Napal J, Amado JA, Riancho JA, Olmos JM, Gonzàlez-Macìas J (1993) Stress decreases the serum level of osteocalcin. Bone Miner 21(2):113–118. https://doi.org/10.1016/S0169-6009(08)80013-X
Berkseth KE, Tebben PJ, Drake MT, Hefferan TE, Jewison DE, Wermers RA (2013) Clinical spectrum of hypophosphatasia diagnosed in adults. Bone 54(1):21–27. https://doi.org/10.1016/j.bone.2013.01.024
Maman E, Borderie D, Roux C, Briot K (2016) Absence of recognition of low alkaline phosphatase level in a tertiary care hospital. Osteoporos Int 27:1251–1254. https://doi.org/10.1007/s00198-015-3346-0
Deeb A, Elfatih A (2018) Could alerting physicians for low alkaline phosphatase levels be helpful in early diagnosis of hypophosphatasia? J Clin Res Pediatr Endocrinol 10(1):19–24. https://doi.org/10.4274/jcrpe.4426
Saraff V, Narayanan VK, Lawson AJ, Shaw NJ, Preece MA, Högler W (2016) A diagnostic algorithm for children with low alkaline phosphatase activities: lessons learned from laboratory screening for hypophosphatasia. J Pediatr 172:181–186. https://doi.org/10.1016/j.jpeds.2016.01.045
Hepp N, Frederiksen AL, Duno M, Præst Holm J, Rye Jørgensen N, Beck Jensen JE (2021) Biochemical, clinical and genetic characteristics in adults with persistent hypophosphatasaemia; data from an endocrinological outpatient clinic in Denmark. Bone Rep 15:101101. https://doi.org/10.1016/j.bonr.2021.101101
Riancho-Zarrabeitia L, García-Unzueta M, Tenorio JA, Gómez-Gerique JA, Ruiz Pérez VL, Heath KE, Lapunzina P, Riancho JA (2016) Clinical, biochemical and genetic spectrum of low alkaline phosphatase levels in adults. Eur J Intern Med 29:40–45. https://doi.org/10.1016/j.ejim.2015.12.019
McKiernan FE, Dong J, Berg RL, Scotty E, Mundt P, Larson L, Rai I (2017) Mutational and biochemical findings in adults with persistent hypophosphatasemia. Osteoporos Int 28(8):2343–2348. https://doi.org/10.1007/s00198-017-4035-y
Cundy T, Michigami T, Tachikawa K, Dray M, Collins JF, Paschalis EP, Gamsjaeger S, Roschger A, Fratzl-Zelman N, Roschger P, Klaushofer K (2015) Reversible deterioration in hypophosphatasia caused by renal failure with bisphosphonate treatment. J Bone Miner Res 30(9):1726–1737. https://doi.org/10.1002/jbmr.2495
Gagnon C, Sims NA, Mumm S, McAuley SA, Jung C, Poulton IJ, Ng KW, Ebeling PR (2010) Lack of sustained response to teriparatide in a patient with adult hypophosphatasia. J Clin Endocrinol Metab 95(3):1007–1012. https://doi.org/10.1210/jc.2009-1965
Lawrence JE, Saeed D, Bartlett J, Carrothers AD (2017) Adult-onset hypophosphatasia diagnosed following bilateral atypical femoral fractures in a 55-year-old woman. Clin Cases Miner Bone Metab. 14(3):347–53. https://doi.org/10.11138/ccmbm/2017.14.3.347
Rassie K, Dray M, Michigami T, Cundy T (2019) Bisphosphonate use and fractures in adults with hypophosphatasia. JBMR Plus 3(10):e10223. https://doi.org/10.1002/jbm4.10223
Desborough R, Nicklin P, Gossiel F, Balasubramanian M, Walsh JS, Petryk A, Teynor M, Eastell R (2021) Clinical and biochemical characteristics of adults with hypophosphatasia attending a metabolic bone clinic. Bone 144:115795. https://doi.org/10.1016/j.bone.2020.115795
Genest F, Seefried L (2018) Subtrochanteric and diaphyseal femoral fractures in hypophosphatasia - not atypical at all. Osteoporos Int 29(8):1815–1825. https://doi.org/10.1007/s00198-018-4552-3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
PRE has received research funding from Alexion. All other authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ng, E., Ashkar, C., Seeman, E. et al. A low serum alkaline phosphatase may signal hypophosphatasia in osteoporosis clinic patients. Osteoporos Int 34, 327–337 (2023). https://doi.org/10.1007/s00198-022-06597-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06597-3