Abstract
Summary
Poor physical function and body composition my partly predict the risk of falls leading to fracture regardless of bone mineral density.
Introduction
To examine the relationship between body composition, physical function, and other markers of health with hip fractures in older community-dwelling Icelandic adults.
Methods
A prospective cohort of 4782 older adults from the AGES-Reykjavik study. Baseline recruitment took place between 2002 and 2006, and information on hip fractures occurring through 2012 was extracted from clinical records. Using multivariate regression analyses, baseline measures of bone health, physical function, and body composition were compared between those who later experienced hip fractures and to those who did not. Associations with the risk of fractures were quantified using Cox regression.
Results
Mean age was 76.3 years at baseline. After adjustment for age, regression showed that male hip fracture cases compared with non-cases had (mean (95% confidence interval)) significantly lower thigh muscle cross-sectional area − 5.6 cm2 (− 10.2, − 1.1), poorer leg strength – 28 N (− 49, − 7), and decreased physical function as measured by longer timed up and go test 1.1 s (0.5, 1.7). After adjustment for age, female cases had, compared with non-cases, lower body mass index − 1.5 kg/m2 (− 2.1, − 0.9), less lean mass − 1.6 kg (− 2.5, − 0.8), thigh muscle cross-sectional area − 4.4 cm2 (− 6.5, − 2.3), and worse leg strength − 16 N (− 25, − 6). These differences largely persisted after further adjustment for bone mineral density (BMD), suggesting that body composition may contribute to the risk of fracture independent of bone health. When examining the association between these same factors and hip fractures using Cox regression, the same conclusions were reached.
Conclusions
After accounting for age and BMD, older adults who later experienced a hip fracture had poorer baseline measures of physical function and/or body composition, which may at least partly contribute to the risk of falls leading to fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures constitute a major health problem for the elderly in terms of reduced quality of life and life expectancy [1]. The associated financial burden for society is also substantial with estimated health care costs per fracture ranging between $3500 and $25,000 [2]. At an older age, the increased incidence of hip fractures can largely be explained by the critical loss of bone mass combined with a deterioration of physical function resulting in an increased propensity for falls [3]. Although a number of risk factors for hip fractures have been identified, many of them such as age, height, and sex [4,5,6] are non-modifiable and of limited use for prevention. Modifiable risk factors that directly influence BMD include vitamin D and calcium [7,8,9,10]. Other factors such as smoking [11], low body weight [12], exercise [10, 13, 14], physical function [15, 16], and balance [17, 18] appear to have a more dual role as they may affect both BMD and propensity of falls.
Many previous studies have often focused on quantifying fracture risk for a single or a few selected risk factors only. This approach is somewhat limited, as it largely ignores the fact that risk factors tend to emerge in clusters at an older age when health deteriorates [19, 20]. In terms of prevention, a better understanding of how individual risk factors for hip fractures cluster and identifying through which pathway they may operate is likely to achieve better results than focusing on individual risk factors alone.
In a large prospective cohort of elderly subjects who underwent detailed clinical examination, we examined the baseline characteristics of individuals who subsequently had hip fractures (cases) compared with those who did not (non-cases) in relation to measures of bone health, body composition, physical function, lifestyle, and health. We aimed to identify and separate risk factors for hip fractures associated with an increased propensity for falls on the one hand and those associated with poor bone health on the other.
Methods
Study participants
This study is based on Age, Gene/Environment Susceptibility-Reykjavik Study (AGES-Reykjavik) that has been described in detail elsewhere [21]. Between 2002 and 2006, a total of 5764 subjects were recruited, 3326 female and 2438 male. A total of 933 subjects did not undergo QCT scanning either because they did not want to attend or because they excluded for reasons including extreme body weight, being unable to lie flat on the scanner bed, and having metal implants at the scan site. In addition, information on hip fracture status during follow-up was missing for 49 subjects leaving 4782 subjects (84% of those enrolled) available for analyses. The subjects not included in our analyses were on average 4 years older. After adjustment for age, those who were not included had poorer physical function as measured by the timed up and go test and leg strength. There were, however, no marked differences in clinical biomarkers (including serum 25(OH)D) and body composition (see Supplemental Table 1).
All participants provided written informed consent. The study was approved by the Icelandic National Bioethics Committee (VSN: 00-063) and the National Institute on Aging Intramural Institutional Review Board (MedStar IRB for the Intramural Research Program, Baltimore, MD).
Assessment of hip fractures
Hip fractures were defined according to the International Classification of Diseases version 10, diagnostic codes S72.0, S72.1, and S72.2 [22]. Based on this definition, information on hip fractures were extracted, verified, and confirmed by medical and radiological records. The exact procedures have been described previously, where it was estimated that around 97% of all hip fractures occurring among participants were captured [23]. Information on hip fractures included all events occurring from participants’ enrollment (2002–2006) into the study until 31 December 2012.
Clinical examination
Blood chemistry
During the clinical examination, fasting blood samples were drawn, and biomarkers reflecting general health and nutrition were quantified, i.e., serum 25-hydroxy vitamin D (25(OH)D), albumin, and hemoglobin using standard methods [7].
Body composition
Body weight was measured in light underwear on a calibrated scale (model no. 708, Seca, Hamburg, Germany), and height was measured with a calibrated stadiometer (model no. 206; Seca, Hamburg, Germany). Based on these two measures, sex-specific fat- and fat-free mass were estimated using bioelectric impedance analysis (BIA). Body mass index (BMI) was calculated as weight in kg divided by height in meters squared.
Muscular strength, physical function, and balance
Leg strength and grip strength were quantified using a computerized dynamometer chair (Good Strength, Metitur Ltd., Finland). Leg strength was measured in the right knee and quantified in terms of the maximal isometric extension force, as described previously [24]. Grip strength was quantified in terms of the maximum force the participants could squeeze as has been described before [25]. For both leg and grip strength, the best performance out of three measures was used. Physical function was assessed as the timed up and go test, which measures the time it takes to stand up from a chair, walk 3 m, return, and sit down [26, 27]. Participants also underwent a balance test [28], where they were asked to stand in an eased upright position with hands beside the body. The test consisted of following a computer monitor that showed a moving frame of reference that should be followed without losing balance or taking an extra step. The maximal distance achieved was then recorded for leaning backwards and forward and when leaning to the sides from left to right.
Assessment of bone health and muscle thigh area
Bone health was measured using quantitative computerized tomography (QCT) measuring bone mineral content, volume, and density of the femoral neck and trochanter. The integral bone mineral density was then calculated from those measures. The exact procedures and quality control for these scannings have been described in detail elsewhere [29].
Information on lifestyle and health
During the clinical examination, participants filled out a questionnaire covering medical history, lifestyle, and socioeconomic status. To summarize the health status of participants, we used the Charlson comorbidity index (CCI) [30] defined as the binary sum over the following comorbidities: myocardial infarction, congestive heart failure, peripheral vascular disease, chronic obstructive pulmonary disease, diabetes, and chronic renal failure as described by Austin et al. [31]. Current alcohol consumption was categorized as higher or lower than moderate intake of ≤ 25 g/day or > 25 g/day [32]. Current smoking was categorized as yes/no. Physical activity was categorized as ≤ 30 or > 30 min of moderate or vigorous physical activity per day. The number of falls during the last 12 months before AGES recruitment was categorized as ≤ 3 or > 3 falls.
Statistical analyses
Statistical analysis was conducted using SPSS for Windows version 24.0 (SPSS, Chicago, IL, USA), and the level of significance was set at P < 0.05. Data were checked for normality using visual inspection of histograms and quantile-quantile plots. The mean and standard deviation (SD) were used to describe continuous variables, and percentages were used to describe dichotomous variables.
Differences between hip fracture and non-fracture cases were examined using multivariable linear regression analyses, run separately for males and females. For these analyses, adjusted models accounting for either (1) age or (2) age and BMD of the femoral neck were used. Differences between hip fracture cases and non-cases were formally tested using the t test that was for continuous variables and chi-square test for dichotomous variables.
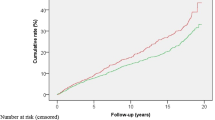
In addition to examining differences in characteristics of hip fracture cases and non-cases at baseline, Cox regression analysis was also used to quantify the association between baseline measures of body composition, clinical biomarkers, physical function, and later fracture status. As mentioned above, adjustments for either (1) age or (2) age and BMD of the femoral neck were made. The underlying time scale in these models was the time from recruitment (baseline) until fracture, death, or end of follow-up. The hazard ratio was estimated in relation to a 1-SD increase in the independent variable.
Results
Among 2104 males and 2678 females with BMD data, a total of 114 and 273 hip fractures occurred between recruitment (2002–2006) and end of follow-up (31 December 2012), respectively. The mean (SD) age at hip fracture was 79.8 years (5.5) for males and 79.2 years (5.2) for females with mean (SD) follow-up time of 4.6 years (2.3) and 5.3 (2.4) for males and females, respectively. The mean follow-up time for non-cases was 7.4 (2.4) and 7.9 (2.1) for males and females, respectively. No clear seasonal variation in hip fractures was observed (data not shown).
Crude measures of bone health, body composition, clinical biomarkers, physical function, and other characteristics recorded at baseline among those who later experienced hip fractures and those who did not are presented in Table 1. After accounting for age (age-adjusted P values), males and females who later experienced hip fractures had significantly lower baseline serum 25(OH)D and BMD of the femoral neck compared with non-cases. More pronounced differences in BMD were observed for the trabecular compared with the cortical part of the bone. For both sexes, hip fracture cases also had poorer leg strength and were more likely to experience several falls (> 3) during the previous 12 months prior to recruitment. No differences in Charlson comorbidity index and smoking were observed. With respect to sex-specific differences, male cases had significantly worse balance, lower albumin concentrations, and performed worse in the timed up and go test compared with non-cases. On the other hand, more pronounced and significant differences in body composition were observed between female cases and non-cases.
Adjusted differences between hip fracture cases and non-cases are shown in Table 2. Compared with the age-adjusted model, further adjustment for BMD had only a minor impact on the observed differences between hip fracture cases and non-cases for females. That is, after adjustment for age and BMD significant differences in measures of body composition, serum 25(OH)D and leg strength were still clearly present. For males, significant differences in serum 25(OH)D, albumin, timed up and go test, and balance were also still present after adjustment for BMD, while differences in muscle thigh area and leg strength were no longer formally significant.
Table 3 shows the corresponding risk of fracture from the Cox regression analysis for all variables shown in Table 2. Overall, conclusions remained largely consistent, although some of the mean differences in Table 2 that were borderline significant (e.g. leg strength, hemoglobin, and balance left-right for males) or showed non-significant small differences (timed up and go test and grip strength) were formally significant in the Cox regression analyses (Table 3).
In the results presented in Tables 1, 2, and 3, a total of 1500 subjects, of which 183 were hip fracture cases, died during the follow-up period. Examining the influence of mortality during follow-up, we observed similar differences as presented in Table 1, and the same conclusions were reached when excluding those who died during the follow-up period (see Supplemental Table 2).
Discussion
In this cohort of 4782 older adults, we examined baseline characteristics of participants who later experienced a hip fracture during a mean follow-up time of 7.4 years versus those who did not. Participants who experienced hip fracture were generally older and frailer. After adjusting for age, the differences between the two groups can be summarized as reduced thigh muscle cross-sectional area, lower leg strength, and decreased physical function in terms of timed up and go and balance among males. Female cases, on the other hand, had lower BMI, less lean mass and fat mass, as well as reduced thigh muscle cross-sectional area and lower leg strength. These differences largely persisted after further adjustment for bone mineral density, suggesting that they may at least partly contribute to the risk of fracture independent of bone health.
Consistent with findings from other studies [3, 14, 33], hip fracture cases in our study scored lower in most baseline characteristics related to bone health and body composition. Apart from BMD, one of the most pronounced and consistent differences between hip fracture cases and non-cases for both sexes were observed for thigh muscle area and leg strength. Both measures are determinants of mobility and physical function in older adults. Several sex-specific differences were also observed. For example, after adjustment for age and BMD, differences in clinical biomarkers and physical function were more pronounced in males, while differences in body composition were more pronounced in females. Similar differences in body composition have been observed in other studies as well [3].
In line with our findings, the EPIDOS study [33] reported that both poor balance and physical function were, after adjustment for age and BMD, significantly associated with an increased risk of subsequent hip fractures. Two other studies [15, 34] have also suggested that limitations in physical functioning are related to increased hip fracture risk. With respect to body composition, the Health ABC study found high subcutaneous fat thickness to be protective against hip fracture risk in both males and females [16]. This observation is also supported by more experimental work by Robinovitch et al. (1995). They showed that when applying the same impact, the measured peak force to the hip was reduced with increased trochanteric soft tissue thickness [34].
Concerning the sex-specific differences observed in our study, the higher incidence of hip fractures in females is, at least partly, explained by increased survival to older age, enhanced rate of bone loss after menopause [35], and smaller bone size compared with males [29]. These differences may explain the pattern observed in our study (Tables 2 and 3) with the protective role of body composition being more pronounced females [17, 35], while physical function, a marker of frailty and propensity of falls [36], being more pronounced for males who tend not to live as long as females.
In older adults’ measures of physical function such as muscle thigh area, leg strength, timed up and go, and balance can be improved through resistance training and exercise. What impact such improvements may have on fracture risk must be examined in an intervention setting. When comparing cases and non-cases, absolute differences in the timed up and go test were stronger for males than females (Table 3). However, in terms of risk of fracture, a 1-SD increase in timed up and go was, after adjustment for age and BMD, significantly associated with around 50% and 25% higher risk of hip fracture in males and females, respectively. The strength of this association was similar or stronger to what was observed for other more advanced measures examined in our study. These results suggest that timed up and go test may be a relevant method to use when identifying older adults who are at increased fracture risk due to impaired functional mobility [37]. The advantages of using the timed up and go test are that it is non-invasive and less expensive than more advanced image techniques (e.g., DXA, CT, MRI).
The beneficial effect of sufficient vitamin D status on BMD is well established [38, 39], and both uses of vitamin D containing supplements and serum 25(OH)D status have been observed to be a predictor of bone health in this cohort [7, 40]. In our study, serum 25(OH)D also remained significantly different between hip fracture cases and non-fracture cases after adjustment for BMD, which is in line with findings from other studies [41, 42]. These associations may suggest a possible role of vitamin D in fracture prevention beyond bone density.
Regarding interpretation of our results, we presented both absolute mean differences in baseline characteristics of subjects who later (~ 5 years) experienced hip fractures compared with those who did not (Table 2) as well as examining the associations for these characteristics with time until fracture using Cox-regression analyses (Table 3). As the Cox regression analyses takes time to event into consideration, it provides a more direct and precise estimate of the underlying association. The absolute differences, however, provide information on how different the two groups were in absolute term at baseline. Overall same conclusions were reached for both analyses but difference that were borderline significant in Table 2 (e.g., leg strength, hemoglobin, and balance left-right for males) reached formal significance when associations with time to event were examined (Table 3). For females, the timed up and go test and grip strength were significantly associated with increased risk of fractures (Table 3), while only modest and non-significant differences were observed for the mean differences at baseline (Table 2). In both cases the associations with risk of fractures appeared to be driven by few subjects with poor performance for these two measurements, which were slightly overrepresented among hip fracture cases (see Table 1).
Our study had several strengths, including its longitudinal design with a large number of participants who underwent a detailed, standardized clinical evaluation at baseline. After a relatively long follow-up period, hip fracture cases were extracted from clinical records and additionally verified. The study sample is representative of the elderly population in Iceland, which is reflected by a similar incidence of hip fractures compared with the general population [43]. Concerning limitations, despite the strength of the longitudinal design compared with other observational designs, these types of studies are still prone to biases due to improper confounder control and/or residual confounding. As a result, replication of our findings in another independent data source and further support from carefully designed interventions are needed.
Conclusions
Community-dwelling older adults who later experienced a hip fracture were generally older and frailer at the baseline evaluation, compared with those who did not subsequently suffer a fracture. After accounting for age and BMD, hip fracture cases had poorer baseline measures of physical function and/or body composition, which may at least partly contribute to the risk of falling, leading to fracture. A simple test of physical function, such as the timed up and go test, seems to compare favorably with more advanced methods using image analyses. In terms of preventive measures for hip fractures, more focus on improved physical function explored in intervention setting seems justified.
Change history
21 October 2020
The original version of this article, published on 18 august 2020 contained a mistake. An author’s name was misspelled.
References
Peeters CM, Visser E, Van de Ree CL et al (2016) Quality of life after hip fracture in the elderly: a systematic literature review. Injury 47(7):1369–1382
Davis JC, Robertson MC, Ashe MC et al (2010) International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporos Int 21(8):1295–1306
Nasiri M, Luo Y (2016) Study of sex differences in the association between hip fracture risk and body parameters by DXA-based biomechanical modeling. Bone 90:90–98
Briot K, Maravic M, Roux C (2015) Changes in number and incidence of hip fractures over 12 years in France. Bone 81:131–137
Finsterwald M, Sidelnikov E, Orav EJ et al (2014) Gender-specific hip fracture risk in community-dwelling and institutionalized seniors age 65 years and older. Osteoporos Int 25(1):167–176
Xiao Z, Ren D, Feng W, Chen Y, Kan W, Xing D (2016) Height and risk of hip fracture: a meta-analysis of prospective cohort studies. Biomed Res Int 2016:2480693
Steingrimsdottir L, Halldorsson TI, Siggeirsdottir K et al (2014) Hip fractures and bone mineral density in the elderly - importance of serum 25-hydroxyvitamin D. PLoS One:9(3)
Guerra MTE, Feron ET, Viana RD et al (2016) Elderly with proximal hip fracture present significantly lower levels of 25-hydroxyvitamin D. Rev Bras Ortop (Engl Ed) 51(5):583–588
Fiatarone Singh MA (2014) Exercise, nutrition and managing hip fracture in older persons. Curr Opin Clin Nutr Metab Care 17(1):12–24
Lang T, Cauley JA, Tylavsky F et al (2010) Computed tomographic measurements of thigh muscle cross-sectional area and attenuation coefficient predict hip fracture: the health, aging, and body composition study. J Bone Miner Res 25(3):513–519
Marques EA, Elbejjani M, Gudnason V et al (2018) Cigarette smoking and hip volumetric bone mineral density and cortical volume loss in older adults: the AGES-Reykjavik study. Bone 108:186–192
Waugh EJ, Lam MA, Hawker GA et al (2009) Risk factors for low bone mass in healthy 40-60 year old women: a systematic review of the literature. Osteoporos Int 20(1):1–21
Benetou V, Orfanos P, Benetos IS et al (2011) Anthropometry, physical activity and hip fractures in the elderly. Injury 42(2):188–193
Malkov S, Cawthon PM, Peters KW et al (2015) Hip fractures risk in older men and women associated with DXA-derived measures of thigh subcutaneous fat thickness, cross-sectional muscle area, and muscle density. J Bone Miner Res 30(8):1414–1421
Chun SH, Cho B, Yang H-K et al (2017) Performance on physical function tests and the risk of fractures and admissions: findings from a national health screening of 557,648 community-dwelling older adults. Arch Gerontol Geriatr 68(Supplement C):174–180
Frank-Wilson AW, Farthing JP, Chilibeck PD et al (2016) Lower leg muscle density is independently associated with fall status in community-dwelling older adults. Osteoporos Int 27(7):2231–2240
Marks R (2011) Physical activity and hip fracture disability: a review. J Aging Res 2011:741918
Lundin H, Saaf M, Strender LE, Nyren S, Johansson SE, Salminen H (2014) One-leg standing time and hip-fracture prediction. Osteoporos Int 25(4):1305–1311
Pekkarinen T, Löyttyniemi E, Välimäki M (2013) Hip fracture prevention with a multifactorial educational program in elderly community-dwelling Finnish women. Osteoporos Int 24(12):2983–2992
Cummings SR, Nevitt MC, Browner WS et al (1995) Risk factors for hip fracture in white women. N Engl Med 332:767–774
Harris TB, Launer LJ, Eiriksdottir G et al (2007) Age, Gene/Environment Susceptibility-Reykjavik Study: multidisciplinary applied phenomics. Am J Epidemiol 165(9):1076–1087
WHO (2017) The International Classification of Diseases and Related Health Problems 10th Revision (ICD-10)-WHO
Siggeirsdottir K, Aspelund T, Sigurdsson G et al (2007) Inaccuracy in self-report of fractures may underestimate association with health outcomes when compared with medical record based fracture registry. Eur J Epidemiol 22(9):631–639
Aalto H, Pyykko I, Starck J (1988) Computerized posturography, a development of the measuring system. Acta Otolaryngol Suppl 449:71–75
Mijnarends DM, Koster A, Schols JM et al (2016) Physical activity and incidence of sarcopenia: the population-based AGES-Reykjavik Study. Age Ageing 45(5):614–620
Podsiadlo D, Richardson S (1991) The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39(2):142–148
Siggeirsdottir K, Jonsson BY, Jonsson H Jr, Iwarsson S (2002) The timed ‘up & go’ is dependent on chair type. Clin Rehabil 16(6):609–616
Rasku J, Pyykko I, Juhola M et al (2012) Evaluation of the postural stability of elderly persons using time domain signal analysis. J Vestib Res 22(5-6):243–252
Sigurdsson G, Aspelund T, Chang M et al (2006) Increasing sex difference in bone strength in old age: the Age, Gene/Environment Susceptibility-Reykjavik study (AGES-REYKJAVIK). Bone 39(3):644–651
Armitage JN, van der Meulen JH (2010) Identifying comorbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson Score. Br J Surg 97(5):772–781
Austin SR, Wong YN, Uzzo RG, Beck JR, Egleston BL (2015) Why summary comorbidity measures such as the Charlson comorbidity index and Elixhauser score work. Med Care 53(9):e65–e72
Zhang X, Yu Z, Yu M, Qu X (2015) Alcohol consumption and hip fracture risk. Osteoporos Int 26(2):531–542
Dargent-Molina P, Favier F, Grandjean H et al (1996) Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet 348(9021):145–149
Robinovitch SN, McMahon TA, Hayes WC (1995) Force attenuation in trochanteric soft tissues during impact from a fall. J Orthop Res 13(6):956–962
Riis BJ, Hansen MA, Jensen AM et al (1996) Low bone mass and fast rate of bone loss at menopause: equal risk factors for future fracture: a 15-year follow-up Study. Bone 19(1):9–12
Kamińska MS, Brodowski J, Karakiewicz B (2015) Fall risk factors in community-dwelling elderly depending on their physical function, cognitive status and symptoms of depression. Int J Environ Res Public Health 12(4):3406–3416
Kear BM, Guck TP, McGaha AL (2017) Timed up and go (TUG) test: normative reference values for ages 20 to 59 years and relationships with physical and mental health risk factors. J Prim Care Community Health 8(1):9–13
EFSA NDA Panel (2016) Scientific opinion on dietary reference values for vitamin D. EFSA J 14:4547. https://doi.org/10.2903/j.efsa.2016.4547
Zarca K, Durand-Zaleski I, Roux C et al (2014) Cost-effectiveness analysis of hip fracture prevention with vitamin D supplementation: a Markov micro-simulation model applied to the French population over 65 years old without previous hip fracture. Osteoporos Int 25(6):1797–1806
Eysteinsdottir T, Halldorsson TI, Thorsdottir I (2015) Cod liver oil consumption at different periods of life and bone mineral density in old age. Br J Nutr 114(2):248–256
Salamon A, Toldy E, Biro C et al (2017) Vitamin D and calcium supplementation in elderly patients with hip fracture. Orv Hetil 43:1699–1707
Choi S-W, Kweon S-S, Choi J-S et al (2015) The association between vitamin D and parathyroid hormone and bone mineral density: the Dong-gu Study. J Bone Miner Metab 34:555–563
Skuladottir SS, Gudmundsdottir E, Mogensen B, et al (2018) Hip fractures among older people in Iceland between 2008 and 2012. Int J Orthop Trauma Nurs
Funding
The original work was funded by the National Institutes of Health, USA, contract N01-AG-12100, and the National Institute on Aging Intramural Research Program, the National Eye Institute, USA (ZIAEY000401), Hjartavernd (The Icelandic Heart Association), and Althingi (Icelandic Parliament). Work on this study was in part funded by The St. Josef’s Hospital Fund, Reykjavik, Iceland, the Landspitali University Hospital Research Fund, the Icelandic Gerontological Society Research Fund, and the Helga Jonsdottir and Sigurlidi Kristjánsson Geriatric Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All participants provided written informed consent. The study was approved by the Icelandic National Bioethics Committee (VSN: 00-063) and the National Institute on Aging Intramural Institutional Review Board (MedStar IRB for the Intramural Research Program, Baltimore, MD).
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: An author’s name was misspelled
Electronic supplementary material
ESM 1
(DOCX 31 kb)
Rights and permissions
About this article
Cite this article
Skuladottir, S.S., Ramel, A., Hjaltadottir, I. et al. Characteristics of incidence hip fracture cases in older adults participating in the longitudinal AGES-Reykjavik study. Osteoporos Int 32, 243–250 (2021). https://doi.org/10.1007/s00198-020-05567-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05567-x